Abstract
Background
Physical tests are usually preferred to assess rotator-cuff syndrome but are insufficient to predict the morphology and size of the rotator-cuff. The objective of the study was to rate the ultrasound findings for patients with sudden shoulder pain and to determine potential predictors of the same.
Material/Methods
A total of 112 patients with sudden shoulder pain with rotator-cuff syndrome, suspected by orthopedic doctors, were subjected to ultrasonography. Real-time ultrasonography was done for the acromioclavicular joint, biceps, infraspinatus, posterior labrum, subscapularis, supraspinatus, teres minor tendon, and the sub-acromial-subdeltoid bursa. Each tendon was assessed via scanning planes in orientation as per longer and shorter axis, and from their myotendinous junction shoulder to bony insertions. Linear and logistic regression analysis were performed to predict the associations of medical history with rotator-cuff injury.
Results
Ultrasonography identified that 82% of the enrolled patients had at least one particular cause of the rotator-cuff disorder. Among the rotator-cuff disorders, calcific tendonitis (54%) was observed more frequently followed by tendinopathy (32%), subacromial-subdeltoid bursitis (22%), and partial thickness tear (21%). Also, 46 patients (41%) had multiple findings. Older age (older than 40 years) was a strong predicting factor of rotator-cuff disorder (r2=0.36, P=0.0004).
Conclusions
Ultrasonography is a vital diagnostic procedure used by orthopedic surgeons for diagnosis of the rotator-cuff disorder(s) in patients with sudden shoulder pain.
MeSH Keywords: Bursitis; Rotator Cuff; Shoulder Dislocation; Tendinopathy; Ultrasonography; Ultrasonography, Doppler
Background
Sudden pain in shoulders is generally due to uncoordinated movements of structures in the subacromial space [1] and is difficult to understand [2]. A stiff or painful shoulder is often caused intrinsically by periarticular or articular rheumatoid conditions in shoulder joint [3]. It could also be extrinsically as reflective neurological pain or vascular diseases, neoplasms, internal organs, and cervical spine disease [4,5]. Suggested treatment for all orthopaedical medicine patients comprises of step-wise therapy despite particular fundamental cause [6]. The rotator cuff is a natural reduction of the muscle-tendon unit in old adults [7]. Many of the patients with pain in the shoulder are treated under medicine by orthopedic surgeons [8,9] because 30–70% of painful shoulders patients are related cases of rotator cuff disorders [7]. Physical tests like the external rotation lag test and positive painful arc test [10] are utilized to assess the rotator-cuff syndrome but usually insufficient to predict the morphology and size of rotator-cuff [2,11].
The downside of this step-wise treatment is that it may lead to overtreatment and delayed recuperation [12] because the rotator cuff disorders are often asymptomatic. Therefore, real events are very difficult to diagnose rotator cuff disorders [7]. The most accurate diagnostic imaging methods are magnetic resonance imaging (MRI), ultrasound, and magnetic resonance angiography (MRA) [10]. Among them, MRI and MRA are limited for partial tears [7] and have poor interobserver agreements for diagnosis of the rotator-cuff syndrome [13]. Also, if the patient is to be implanted, then that condition does not allow the MRI to be executed [7]. Shoulder ultrasound has turned into an acceptable diagnosis for assessing rotator-cuff syndrome, that directed to personalized therapy depending on subdivisions of diagnosis [6,14]. Based on this foundation, it appeared to be valuable to identify disease frequencies from the range of rotator-cuff disorder on a prospective basis in orthopaedical medicine patients having shoulder pain [15]. A prospective observational study on patients with a 3-months history of shoulder pain showed that ultrasound diagnosis makes treatment plausible [8]. All in all, it is essential to have the best, most valid imaging tests, and such tests are influenced by many factors such as operators’ experiences, accuracy, sensitivity, and image analysis.
The objective of this observational study was to rate ultrasound findings of rotator-cuff syndrome in patients who had sudden pain in the shoulder. The secondary endpoint of the study was to identify potential predictors of sudden pain in the shoulder.
Material and Methods
Ethical consideration and consent to participate
The study was registered in the Research Registry (www.researchregistry.com), UID No.: researchregistry4568 dated May 13, 2016. The protocol (SGH/CL/01/16 dated May 11, 2016) was approved by the Shanghai General Hospital of Nanjing Medical University Review Board. An informed consent form was signed by every participant (or authorized guardian) before enrollment, and covered pathology, diagnosis, and publication of the work in all formats (hard and/or electronics) including patients’ images and personal data (if any) irrespective of language and time. The study adhered to the law of China, the STROBE (strengthening the reporting of observational studies in epidemiology) statement, and the 2008 Declarations of Helsinki (Chinese version). Confidentiality of patients’ data was strictly preserved.
Inclusion criteria
Inclusion criteria for the study included: patients age 18 years and older with sudden pain (last 5-days; as per institutional review board guideline) in the shoulder.
Exclusion criteria
Exclusion criteria included patients who had 3 months prior therapy/consultation for shoulder pain, less than 45° motion range of glenohumeral rotation (which might be due to glenohumeral diseases like adhesive capsulitis or osteoarthritis), fracture history of acromion or humerus bone, affected shoulder surgery/dislocation, shoulder problems due to cause by rheumatic disorder, referred pain or extraneous causes, medical history of psychiatric diseases, depression, anxiety, diabetes mellitus, hemiparesis from stroke, or catastrophizing pain.
Ultrasonography technique and diagnosis
A rotating stool was used to seat the patient so that the elbow was positioned in 90° flection with an unsupported hand in the supine position (neutral position). The arm of patient was kept in that position so that all structures could be evaluated. Real-time ultrasonography was done utilizing an iU22 Ultrasound Machine with L12-5 50 mm transducer (Koninklijke Philips N.V., China) for the acromioclavicular joints, biceps, infraspinatus, posterior labrum, subscapularis, supraspinatus, teres minor tendon, and the sub-acromial-subdeltoid (SASD) bursa. Each tendon was assessed via scanning planes in orientation as per longer axis, shorter axis, and by the myotendinous junction of shoulder to bony insertions. Color Doppler (Koninklijke Philips N.V., China) was used to access neovascularity and hyperemia into 4 grades (0 to 3). Standardized ultrasonography technique and diagnosis were used. All tests were conducted by ultra-sonographers (3 years of experience) of the participating institutes, utilizing a scanning approach as shown in Table 1 [4]. The criteria for rotator-cuff diseases are presented in Table 2 [2].
Table 1.
Ultrasonography technique and diagnosis.
| Site | Position of arm |
|---|---|
| Acromioclavicular joint | Arm in a neutral position with the transducer in a coronal plane, also shifting/rotating the transducer atop the acromion |
| Biceps tendon-long head | Arm in a neutral position |
| Infraspinatus tendon | Forearm in a supine position on the ipsilateral thigh or across the front of patient chest, with the hand resting on opposing shoulder. Visualization was enhanced by passive internal and external rotation, during real-time dynamic imaging |
| Subscapularis tendon | Arm in a neutral position as well as during external rotation |
| Supraspinatus tendon | Arms behind patients backs, with hand near the opposing scapular tip (Crass position). In case this position was not possible patient’s hand palm was stationed on iliac wing’s superior aspect with a flexed elbow, headed posterior and in the direction of midline (Modified Crass or Middleton position) |
| The sub-acromial-subdeltoid bursa | Arm in a neutral position with patients arm behind back and during testing for subacromial impingement |
| Subacromial impingement | The transducer was stationed in the coronal plane with medial margin in the acromion lateral margin. Patient’s arm was abducted during internal rotation. The sub-acromial-subdeltoid bursa and supraspinatus tendon was easily glid under acromion till the higher tuberosity touched it closely. Next, this procedure was also performed during flexion, with transducer stationed sagittal with posterior margin near the acromion anterior margin |
Table 2.
Criteria for rotator-cuff diseases.
| Rotator-cuff diseases | Criteria |
|---|---|
| The acromioclavicular osteoarthritis | Joint space narrowing, irregularities and/or osteophytes of the articular bone surfaces, and/or para-articular cysts |
| Biceps tendon tear (partial or complete) | The tendon contains respectively an anechoic cleft and fluid in the sheath or full anechoic cleft via tendon or torn tendon retracted ends separated by the fluid-filled sheath |
| Calcific tendinitis | The tendon contains hyperechoic foci. Calcium deposit was graded as: Type 1: Hyperechoic foci with well-defined acoustic shadow, Type 2: Hyperechoic foci with a faint shadow, Type 3: Hyperechoic foci without shadow. Dynamic examination to reveal impingement and local hyperemia was assessed |
| Full-thickness rotator cuff tear | Tendon focal thinning, full tendon non-visualization, focal discontinuities in the homogeneous tendon echogenicity with no focal thinning, or superficial bursa contour inversion and/or hyperechoic material in tendon location that fails to shift with humeral head amid real-time dynamic imaging |
| Os acromiale | Well defined cortical discontinuity of the superior aspect of the acromion, often mimicking a double the acromioclavicular joint |
| Partial-thickness rotator cuff tear | Hypoechoic discontinuities in the tendon where lesions involve articular or bursal sides of the tendon or hyperechoic and hypoechoic mixed regions in the tendon. The area did not alter appearances on shorter as well as longer axis scans and during transducer tilting atop tendon |
| The sub-acromial-subdeltoid bursitis | A thin hypoechoic layer of more than 2 mm in sandwich manner across hyperechoic peri bursal fat, that was in sandwich manner across hypoechoic deltoid muscles and supraspinatus tendon with hyperemia and/or a teardrop-shaped structure with the most distended segment of the bursa most distal and most dependent. Fluid in the bursa had also considered as a secondary signal of partial thickness rotator cuff tear at the bursal side or a full thickness tear |
| Subacromial impingement | Supraspinatus tendon catches on or bunches up anterior or lateral to the acromion. Presence of bursal thickening with no inflammatory arthropathy history and/or movement of fluid into most lateral part of the sub-acromial-subdeltoid bursa during abduction were secondary signs of impingement |
| Tendinopathy | The tendon was locally or diffusely swollen and had a heterogeneous hypoechoic appearance |
Statistical analysis
The analysis was performed utilizing SPSS Statistics version 24.0-window (IBM Corporation, NY, USA). Fisher’s exact test was used for statistical analysis of categorical data [16]. Linear and logistic regression analysis were performed to predict the associations of independent variables (the medical history of patients, e.g., gender, occupational parameters, and age) with the dependent variable (rotator-cuff disease). At the most discriminating 60 months age cut-off, age was dichotomized [17]. The results were considered significant at 95% of confidence level (CI).
Results
Medical history of patients
From May 15, 2016 to July 1, 2018, a total of 247 patients with sudden pain in the shoulder were recruited from an outpatient setting of the Shanghai General Hospital of Nanjing Medical University, China and the First Affiliated Hospital of XinXiang Medical University, China. Among the study patients, 3 patients were 18 years of age, 32 patients had 3-months prior therapy or consultation for shoulder pain, 5 patients had less than 45° motion range of glenohumeral rotation, 21 patients had osteoarthritis, 23 patients had fracture history of acromion/humerus bone, 14 patients had affected shoulder surgery or dislocation, 9 patients had shoulder problems (by rheumatic disorder, referred pain, and/or extraneous causes), 6 patients had history of psychiatric diseases, 4 patients had depression, 6 patients had anxiety, 12 patients had diabetes mellitus, 1 patient had hemiparesis from stroke, and 2 patients had catastrophizing pain. Therefore, these patients were excluded from the study. A total of 112 patients with sudden shoulder pain with rotator-cuff syndrome suspected by an orthopedic surgeon were included in the study. The flow diagram of the study is presented in Figure 1. The enrolled patients had a median age of 48.8±10.2 years. The analysis included 44 female patients (39%) and 68 male patients (61%). Only 34 patients (30%) had an occupational risk.
Figure 1.
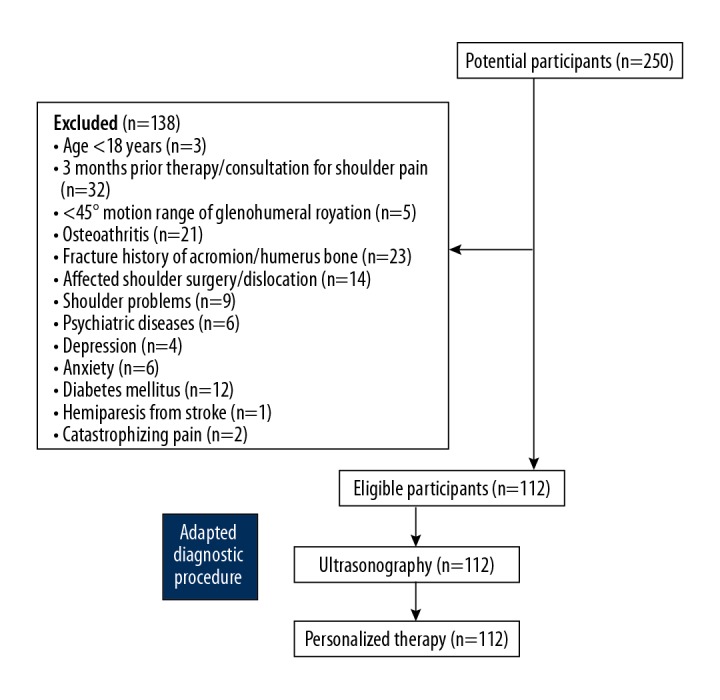
Flow diagram of the study.
Frequencies of rotator-cuff disease
Impingement was found to coexisted with specific rotator-cuff disorders. Ultrasonography aided in the diagnosis of at least one specific cause of rotator-cuff disorder in 92 study patients (82%). Among the rotator-cuff disorders, calcific tendonitis (54%) was observed more frequently followed by tendinopathy in supraspinatus tendon (32%), SASD bursitis (22%), and partial thickness tear (21%). Among the rotator-cuff diseased patients, 46 patients (41%) had found multiple disorders. The frequencies of multiple rotator-cuff disorder in patients is presented in Table 3.
Table 3.
Frequencies of multiple diseases in patients with rotator cuff disease.
| Characteristics | Populations | |
|---|---|---|
| Patients with rotator-cuff disease | 92 | |
| Two diseases | Calcific tendonitis and tendinopathy | 14 (15) |
| Calcific tendonitis and SASD bursitis | 5 (5) | |
| SASD bursitis and tendinopathy | 2 (2) | |
| ACJ osteoarthritis and tendinopathy | 2 (2) | |
| Calcific tendonitis and partial thickness tear | 2 (2) | |
| Partial thickness tear and SASD bursitis | 2 (2) | |
| ACJ osteoarthritis and calcific tendonitis | 2 (2) | |
| Calcific tendonitis and full thickness tear | 2 (2) | |
| Full thickness tear and SASD bursitis | 1 (1) | |
| ACJ osteoarthritis and SASD bursitis | 1 (1) | |
| Three diseases | Calcific tendonitis, partial thickness tear, and tendinopathy | 4 (4) |
| Calcific tendonitis, partial thickness tear, and SASD bursitis | 2 (2) | |
| Partial thickness tear, SASD bursitis, and tendinopathy | 2 (2) | |
| ACJ osteoarthritis, calcific tendonitis, and SASD bursitis | 1 (1) | |
| ACJ osteoarthritis, partial thickness tear, and SASD bursitis | 1 (1) | |
| ACJ osteoarthritis, full thickness tear, and calcific tendonitis | 1 (1) | |
| Four diseases | Calcific tendonitis, partial thickness tear, SASD bursitis, and tendinopathy | 1 (1) |
| ACJ osteoarthritis, calcific tendonitis, tendinopathy, and SASD bursitis | 1 (1) | |
ACJ – acromioclavicular joint; SASD – subacromial subdeltoid.
Potential predictors of sudden pain in the shoulder
Age was association with detection of rotator-cuff disorder (P=0.0004). The frequencies of ultrasonography diagnosed rotator-cuff disorder and predictor factors are presented in Table 4. Linear-regression analysis demonstrated a significant increase in the number of disorders with advancing age (r2=0.86). The univariate analyses demonstrated a significant association of age with the presence of rotator-cuff disorder, which was affirmed by the multivariate analyses’ outcome (OR: 0.239, 95% CI: 0.118–0.485).
Table 4.
Frequencies of ultrasonography diagnosed rotator-cuff disease and predictor factors in the enrolled patients.
| Characteristics | Populations | p-Value# | OR (95% CI) | ||
|---|---|---|---|---|---|
| Patients enrolled in the study | 112 | ||||
| RCD | Absent | 20 (18) | – | – | |
| Present | Age <40 years | 11 (10) | 0.0004* | 0.239 (0.118–0.485) | |
| Age ≥40 years | 81 (72) | ||||
| Gender | Male | 68 (61) | 0.826 | 0.98 (0.28–2.31) | |
| Female | 44 (39) | ||||
| Occupational risk | 34 (30) | 0.841 | 0.97 (0.26–2.42) | ||
| Non-occupational risk | 78 (70) | ||||
| Specific disease | |||||
| ACJ Osteoarthritis | With the other RCD | 9 (8) | |||
| Without the other RCD | 4 (4) | ||||
| Age ≥40 years | 13 (12) | 0.002* | 2 (1.29–3.1) | ||
| Age <40 years | 0 (0) | ||||
| Calcific tendonitis | With the other RCD | 34 (30) | |||
| Without the other RCD | 24 (21) | ||||
| Age ≥40 years | 53 (47) | <0.001* | 1.96 (1.26–3.05) | ||
| Age <40 years | 1 (1) | ||||
| Full-thickness tear | With the other RCD | 3 (3) | |||
| Without the other RCD | 0 (0) | ||||
| Age ≥40 years | 3 (3) | 0.229 | 2 (1.29–3.1) | ||
| Age <40 years | 0 (0) | ||||
| Partial thickness tear | With the other RCD | 14 (13) | |||
| Without the other RCD | 7 (6) | ||||
| Age ≥40 years | 18 (16) | 0.782 | 2.14 (0.58–6.97) | ||
| Age <40 years | 3 (3) | ||||
| SASD bursitis | With the other RCD | 19 (17) | |||
| Without the other RCD | 3 (3) | ||||
| Age ≥40 years | 22 (20) | 0.02* | 1.71 (1.07–2.75) | ||
| Age <40 years | 0 (0) | ||||
| Tendinopathy | With the other RCD | 26 (23) | |||
| Without the other RCD | 8 (7) | ||||
| Age ≥40 years | 31 (28) | 0.0001* | 1.94 (1.24–3.02) | ||
| Age <40 years | 1 (1) | ||||
| Impingement | Age ≥40 years | 16 (14) | 0.004* | 1.88 (1.2–2.97) | |
| Age <40 years | 1 (1) | ||||
Variables were presented as number (percentage). ACJ – acromioclavicular joint; RCD – rotator-cuff disorder; SASD – subacromial subdeltoid.
Fisher’s Exact Test was used for statistical analysis.
A p<0.05 was considered significant. Linear and logistic regression analysis were used to predict the associations. OR – odd ratio; CI – confidence interval.
Significant association.
Discussion
This observational study reported 92 patients (82%) with at least one specific cause of rotator-cuff disorder among the patients who had sudden pain in the shoulder(s) irrespective of age and sex. The painful arc test is considered the most specific test for the detection of the rotator-cuff syndrome [1], but it has inconclusive sensitivity and specificity [2]. Also, physiological tests are not capable of delineating the morphology and size of rotator-cuff [18]. Ultrasonography provides excellent visualization of upper limb muscles [15] and surrounding connective soft tissues [19], and it has several advantages, e.g., no radiation and portability [15]. Also, ultrasonography has excellent inter-observer agreement for synovial effusion, cartilage erosion, and synovial thickening [20]. Musculoskeletal ultrasonography is an appropriate and non-invasive method for the evaluation of rotator-cuff syndrome.
The ultrasonographic investigation by orthopedic surgeons for patients with sudden pain in the shoulder was also performed for calcific tendonitis and thickness tears in our study. The results demonstrated greater frequency of calcific tendonitis with a comparatively lower tear proportion when compared with studies conducted in secondary care settings [8,14]. The results from our study suggest a potential diagnostic methods for patients with sudden shoulder pain who are considered for surgical treatment.
Our observational study demonstrated that older age (older than 40 years) was a stronger predictor of rotator-cuff disorder in patients with sudden pain in the shoulder(s). The results of our study were in line with available published studies [8,17,21]. The outcomes in the present study revealed that ultrasonography allows orthopedic doctors to streamline therapy, particularly for patients 40 years of age or older.
Sudden pain in the shoulder typically presents with at least one specific cause of rotator-cuff disorder (e.g., calcific tendonitis, tendinopathy, SASD bursitis, or partial thickness tear). In addition, 41% of patients have been found to have multiple disorders. Subacromial impingement and shoulder stiffness predicted by physical tests are poor prognostic factors for initial success of treatment [1]. Ultrasonography gives clarification to the patient complaints and advises physicians regarding prognosis. For example, intermittent excruciating episodes are characteristic of calcific tendonitis [22]. In day to day practice, it is necessary to always weigh the ultrasonography results and other findings from the clinical setting, as asymptomatic discoveries might be noted [8]. Patients having a musculoskeletal disease should be treated as per the disease which is more symptomatically likely, e.g., resorption phase calcification or bursitis might profit by corticosteroid injections [1]. Ultrasonography might be helpful to inform treatment strategies for multiple causes of rotator-cuff disorders.
This study was able to differentiate calcific tendonitis, tendinopathy, SASD bursitis, and thickness tears among the rotator-cuff disorders in patients with sudden shoulder pain by using ultrasonography. For the diagnosis of the rotator-cuff disorders, early detection by physical tests [2], arthroscopy [23], and open surgery [24] are helpful to prevent further pathology of the disease. Besides these, MRI [25], computed tomography [26], MRA [25,27], and traditional radiology [28] are commonly used methods for detection of the rotator-cuff disorders. It is important to note that for further diagnosis of patients with sudden shoulder pain, physical tests have high sensitivity but have no specificity [29], and arthroscopy and open surgery are tedious, invasive, non-dynamic, and expensive methods [2]. Ultrasonography can facilitate side-by-side comparisons of joints [19]. Ultrasonography is the best option to diagnose rotator-cuff disorder compared to other available modalities for patients with sudden shoulder pain.
Certain intrinsic limitations of this study require consideration when interpreting the study outcomes. Because ultrasonography is operator-dependence [19], this study would have benefited from comparisons with the contralateral shoulder as a control cohort, a reliability study, and a greater number of ultra-sonographers. In our study, scanning of the contralateral shoulder was done only when results were ambivalent. As this was a 2-center study with very limited patient numbers, we should be cautious in generalizing the results. The clinical value of ultrasonography will rely upon whether patient results are altered. Patient history also can have an effect on results outcomes [30] but this study did not evaluate patient history. We did not have rheumatoid factor test results [31] to evaluate for musculoskeletal disorders, which was somewhat unorthodox, but the study did not include laboratory test. Acute cuff tears and chronic cuff tear analysis was not performed. Results of ultrasound finding should have been compared to arthroscopic findings or the findings by musculoskeletal radiologists. A further comparative diagnostic study is required to assess and prove that an earlier ultrasonography in diagnostic modality improves patients’ outcomes. Long-term health outcomes were not evaluated in this study. Subcutaneous thickness has been reported to be a major influence on echo intensity values [32]. Echo intensity values were not adjusted in the present study. The possible justification for this exclusion was that there was a light touch of the transducer on the upper limb skin. Only 82% of patients were diagnosed with positive rotator-cuff disorder(s). However, all patients had sudden pain in the shoulder. The possible reason for the failure of ultrasonography in the remaining patients could be the presence of excessively soft tissues over the glomerular joint space, which interferes with the sensitivity of ultrasonography for detection of the rotator-cuff disorder [33].
Conclusions
Ultrasonography equipment is the best way for orthopedic surgeons to assess patients for rotator-cuff disorders who have sudden pain in the shoulders, particularly for elderly patients.
Acknowledgments
Authors are thankful to all medical and non-medical staff of the Shanghai General Hospital of Nanjing Medical University, Shanghai, China, and the First Affiliated Hospital of XinXiang Medical University, Weihui, Henan, China.
Abbreviations
- MRI
magnetic resonance imaging
- MRA
magnetic resonance angiography
- STROBE
the strengthening the reporting of observational studies in epidemiology
- SASD
sub-acromial-subdeltoid
- OR
odd ratio
- Cl
confidence interval
Footnotes
Source of support: This study was supported by the National Natural Science Foundation of China (No: 81571679.81771838) and the Interdisciplinary Major Program of Shanghai Jiao Tong University, China (No: YG2015ZD09)
Conflict of interest
None.
References
- 1.Chang KV, Wu WT, Han DS, Ozcakar L. Static and dynamic shoulder imaging to predict initial effectiveness and recurrence after ultrasound-guided subacromial corticosteroid injections. Arch Phys Med Rehabil. 2017;98:1984–94. doi: 10.1016/j.apmr.2017.01.022. [DOI] [PubMed] [Google Scholar]
- 2.Kelly SM, Brittle N, Allen GM. The value of physical tests for subacromial impingement syndrome: A study of diagnostic accuracy. Clin Rehabil. 2010;24:149–58. doi: 10.1177/0269215509346103. [DOI] [PubMed] [Google Scholar]
- 3.Lewis JS, Raza SA, Pilcher J, et al. The prevalence of neovascularity in patients clinically diagnosed with rotator cuff tendinopathy. BMC Musculoskelet Disord. 2009;10:163. doi: 10.1186/1471-2474-10-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Park J, Chai JW, Kim DH, Cha SW. Dynamic ultrasonography of the shoulder. Ultrasonography. 2018;37:190–99. doi: 10.14366/usg.17055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Parentis MA, Glousman RE, Mohr KS, Yocum LA. An evaluation of the provocative tests for superior labral anterior posterior lesions. Am J Sports Med. 2006;34:265–68. doi: 10.1177/0363546505279911. [DOI] [PubMed] [Google Scholar]
- 6.Ottenheijm RP, Joore MA, Walenkamp GH, et al. The Maastricht Ultrasound Shoulder pain trial (MUST): Ultrasound imaging as a diagnostic triage tool to improve management of patients with non-chronic shoulder pain in primary care. BMC Musculoskelet Disord. 2011;12:154. doi: 10.1186/1471-2474-12-154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oliva F, Piccirilli E, Bossa M, et al. I.S.Mu.L.T – rotator cuff tears guidelines. Muscles Ligaments Tendons J. 2016;5:227–63. doi: 10.11138/mltj/2015.5.4.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ottenheijm RP, Cals JW, Weijers R, et al. Ultrasound imaging for tailored treatment of patients with acute shoulder pain. Ann Fam Med. 2015;13:53–55. doi: 10.1370/afm.1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ottenheijm RP, Cals JW, Winkens B, et al. Ultrasound imaging to tailor the treatment of acute shoulder pain: A randomised controlled trial in general practice. BMJ Open. 2016;6:e011048. doi: 10.1136/bmjopen-2016-011048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jancuska J, Matthews J, Miller T, et al. A systematic summary of systematic reviews on the topic of the rotator cuff. Orthop J Sports Med. 2018;6(9) doi: 10.1177/2325967118797891. 2325967118797891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hanchard NC, Lenza M, Handoll HH, Takwoingi Y. Physical tests for shoulder impingements and local lesions of bursa, tendon or labrum that may accompany impingement. Cochrane Database Syst Rev. 2013;30:CD007427. doi: 10.1002/14651858.CD007427.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Randelli P, Randelli F, Ragone V, et al. Regenerative medicine in rotator cuff injuries. Biomed Res Int. 2014;2014 doi: 10.1155/2014/129515. 129515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spencer EE, Jr, Dunn WR, Wright RW, et al. Shoulder Multicenter Orthopaedic Outcomes Network. Interobserver agreement in the classification of rotator cuff tears using magnetic resonance imaging. Am J Sports Med. 2008;36:99–103. doi: 10.1177/0363546507307504. [DOI] [PubMed] [Google Scholar]
- 14.Ottenheijm RP, Jansen MJ, Staal JB, et al. Accuracy of diagnostic ultrasound in patients with suspected subacromial disorders: A systematic review and meta-analysis. Arch Phys Med Rehabil. 2010;91:1616–25. doi: 10.1016/j.apmr.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 15.Chang KV, Wu WT, Huang KC, et al. Limb muscle quality and quantity in elderly adults with dynapenia but not sarcopenia: An ultrasound imaging study. Exp Gerontol. 2018;108:54–61. doi: 10.1016/j.exger.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 16.Hackett DJ, Jr, Hsu JE, Matsen FA., 3rd Primary shoulder hemiarthroplasty: What can be learned from 359 cases that were surgically revised? Clin Orthop Relat Res. 2018;476:1031–40. doi: 10.1007/s11999.0000000000000167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Louwerens JK, Sierevelt IN, van Hove RP, et al. Prevalence of calcific deposits within the rotator cuff tendons in adults with and without subacromial pain syndrome: Clinical and radiologic analysis of 1219 patients. J Shoulder Elbow Surg. 2015;24:1588–93. doi: 10.1016/j.jse.2015.02.024. [DOI] [PubMed] [Google Scholar]
- 18.Wu WT, Chang KV, Mezian K, et al. Basis of shoulder nerve entrapment syndrome: An ultrasonographic study exploring factors influencing cross-sectional area of the suprascapular nerve. Front Neurol. 2018;9:902. doi: 10.3389/fneur.2018.00902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Razek AA, Fouda NS, Elmetwaley N, Elbogdady E. Sonography of the knee joint. J Ultrasound. 2009;12:53–60. doi: 10.1016/j.jus.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Razek AA, El-Basyouni SR. Ultrasound of knee osteoarthritis: Interobserver agreement and correlation with Western Ontario and McMaster Universities Osteoarthritis. Clin Rheumatol. 2016;35:997–1001. doi: 10.1007/s10067-015-2990-2. [DOI] [PubMed] [Google Scholar]
- 21.Schmidt CC, Jarrett CD, Brown BT. Management of rotator cuff tears. J Hand Surg Am. 2015;40:399–408. doi: 10.1016/j.jhsa.2014.06.122. [DOI] [PubMed] [Google Scholar]
- 22.Carcia CR, Scibek JS. Causation and management of calcific tendonitis and periarthritis. Curr Opin Rheumatol. 2013;25:204–49. doi: 10.1097/BOR.0b013e32835d4e85. [DOI] [PubMed] [Google Scholar]
- 23.Ladermann A, Denard PJ, Collin P. Massive rotator cuff tears: Definition and treatment. Int Orthop. 2015;39:2403–14. doi: 10.1007/s00264-015-2796-5. [DOI] [PubMed] [Google Scholar]
- 24.Lenza M, Buchbinder R, Takwoingi Y, et al. Magnetic resonance imaging, magnetic resonance arthrography and ultrasonography for assessing rotator cuff tears in people with shoulder pain for whom surgery is being considered. Cochrane Database Syst Rev. 2013;9:CD009020. doi: 10.1002/14651858.CD009020.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roy JS, Braen C, Leblond J, et al. Diagnostic accuracy of ultrasonography, MRI and MR arthrography in the characterisation of rotator cuff disorders: A systematic review and meta-analysis. Br J Sports Med. 2015;49:131628. doi: 10.1136/bjsports-2014-094148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Oh JH, Kim JY, Choi JA, Kim WS. Effectiveness of multidetector computed tomography arthrography for the diagnosis of shoulder pathology: Comparison with magnetic resonance imaging with arthroscopic correlation. J Shoulder Elbow Surg. 2010;19:14–20. doi: 10.1016/j.jse.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 27.Zhao G, Liu YJ. [Latest progress on diagnosis and treatment of glenohumeral instability]. China J Orthopaed Traumatol. 2014;27:172–76. [in Chinese] [PubMed] [Google Scholar]
- 28.Liu T, Ma J, Cao H, et al. Evaluation of the diagnostic performance of the simple method of computed tomography in the assessment of patients with shoulder instability: A prospective cohort study. BMC Med Imaging. 2018;18:45. doi: 10.1186/s12880-018-0290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.van Kampen DA, van den Berg T, van der Woude HJ, et al. The diagnostic value of the combination of patient characteristics, history, and clinical shoulder tests for the diagnosis of rotator cuff tear. J Orthop Surg Res. 2014;9:70. doi: 10.1186/s13018-014-0070-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tangrood ZJ, Gisselman AS, Sole G, Ribeiro DC. Clinical course of pain and disability in patients with subacromial shoulder pain: A systematic review protocol. BMJ Open. 2018;8:e019393. doi: 10.1136/bmjopen-2017-019393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rezaei H, Torp-Pedersen S, Klint E, et al. Diagnostic utility of musculoskeletal ultrasound in patients with suspected arthritis – a probabilistic approach. Arthritis Res Ther. 2014;16:448. doi: 10.1186/s13075-014-0448-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Young HJ, Jenkins NT, Zhao Q, Mccully KK. Measurement of intramuscular fat by muscle echo intensity. Muscle Nerve. 2015;52:963–71. doi: 10.1002/mus.24656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Razek AA, Al Mahdy Al Belasy F, et al. Assessment of articular disc displacement of temporomandibular joint with ultrasound. J Ultrasound. 2014;18:159–63. doi: 10.1007/s40477-014-0133-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


