Abstract
Retrograde jejuno-jejunal intussusception is a rare complication of bariatric surgeries. It causes acute sudden symptoms that require immediate surgical intervention. We report a case of a 46-year-old female who underwent Roux-en-Y gastric bypass (REYGP) 3 years prior. The patient presented to the emergency department with acute sudden abdominal pain, nausea and vomiting. Laparoscopically, intussuscepting small bowel segment was found gangrenous, and it was resected and end-to-end anastomoses were fashioned. The postoperative course was uneventful, and the patient remained asymptomatic for the 12 months of follow-up. Patients with retrograde intussusception experience an intolerable severe pain that necessitates surgical intervention. The etiology of intussusception as a complication after REYGP is unclear, yet theoretically some possible etiologies exist. The initial diagnosis of retrograde intussusception is made based on abdominal computed tomography. Early intervention significantly reduces morbidity and mortality.
INTRODUCTION
Bariatric surgeries are being performed with a significantly increasing rate every year [1]. The advancement of this surgical field has allowed more options and types of procedures to evolve. Roux-en-Y gastric bypass (REYGB) is considered the most common bariatric procedure performed for weight loss [2]. REYGB procedure bypasses the absorption that occurs in the lower part of the stomach, duodenum and first 100–150 cm of the small bowel. This procedure usually involves two anastomosis sites: the gastro-jejunal and the jejuno-jejunal. Intussusception as a complication for REYGB has been described for the first time in 1986 by Agha [3]. Despite being uncommon, intussusception post RYGB is considered a potentially life-threatening condition that must be expected in order to be treated early. Here, we report a case of retrograde jejuno-jejunal intussusception that occurred 3 years after REYGB.
PRESENTATION
This is a case of a 46-year-old female, 3 years post REYGB. She presented to the emergency department with sudden abdominal pain as well as nausea and vomiting, which started the day before presentation (30 minutes post prandial). Moreover, on physical examination, the abdomen was soft with pain out of proportion (severe pain with minimal tenderness) and no other signs of peritoneal irritation. Furthermore, laboratory data were unremarkable. Abdominal computed tomography (CT) revealed a long segment of obstructed retrograde small bowel obstruction adjacent to the jejuno-jejunal anastomosis associated with a complete proximal small bowel obstruction (Fig. 1). Therefore, the patient was immediately taken to the operating room, and laparoscopic exploration of the abdomen was performed. A segment of retrograde jejuno-jejunal intussusception was encountered with dilated small bowel proximal to the intussusception and a collapsed part distal to it. Decision was made to convert the procedure to an open surgery through a small midline laparotomy (Fig. 2), and a trial was performed to undo the intussusception. There was a gangrenous segment of about 23 cm, necessitating resection and anastomosis (Fig. 3). The anastomosis was performed using a gastrointestinal anastomosis stapler device. Consequently, the patient tolerated the procedure well, and she was sent for recovery in a good condition. Pathology confirmed a gangrenous jejunal segment with features consistent with external venous compression (intussusception related) with viable surgical resection margins. Afterwards, the patient was discharged on postoperative day 3 in a good condition, and she remained asymptomatic during the follow-up period of 1 year.
Figure 1.
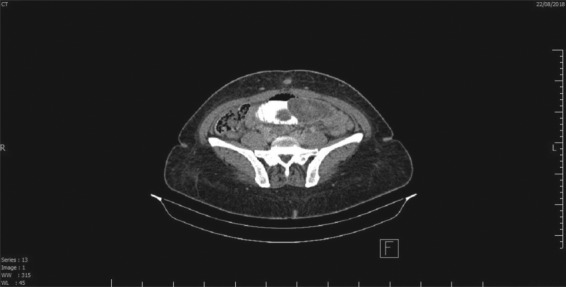
CT scan showing a segment of intestine telescoping into another, which is suggestive of intussusception.
Figure 2.
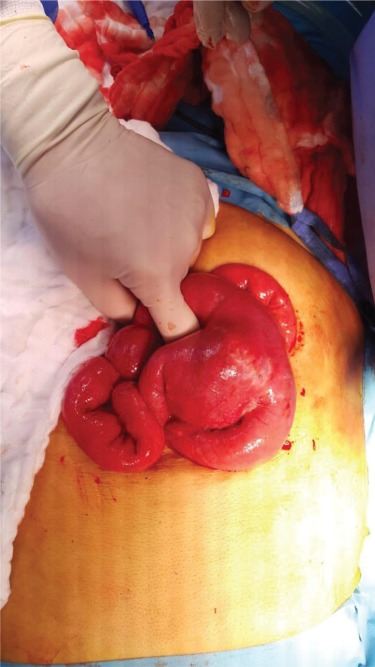
Intussusception of small intestine toward jejuno-jejunal anastomosis.
Figure 3.

Intussuscepted gangrenous part of the small intestine after reduction of intussusception.
DISCUSSION
Retrograde jejuno-jejunal intussusception is a rare, underappreciated complication of REYGB. In a single-center study with more than 15 000 patients having REYGB, 23 patients developed intussusception [4]. The etiology of intussusception as a complication after a surgical procedure, specifically REYGP, is unclear. However, Hocking et al. [5] hypothesized a motility disorder from the divided bowel as opposed to a known pathological lead point. Patients usually present with sudden unspecific symptoms, such as severe abdominal pain, nausea and vomiting, though physical examination is usually normal. CT is considered the most reliable investigation in diagnosing intussusception secondary to surgical exploration [6]. Then, intussusception is recognized, and it can be diagnosed grossly by its pathognomonic appearance as a complex soft tissue mass consisting of outer and inner portions of the intussuscepting (telescoping) bowel segments. A crescent-shaped piece of mesenteric fat is often appreciated within the intussusception [7]. Early intervention significantly reduces morbidity and mortality, so it should be ruled out whenever suspected.
Conclusion
Intussusception as a complication for REYGB is still a rare complication that may occur even after years of the procedure. Due to its unspecific signs and symptoms, it may be difficult to diagnose. Therefore, this complication should be suspected clinically in patients after REYGB, and the use of CT scan is very valuable in the diagnosis of such complications. In addition, the swift diagnosis is important for such cases as early intervention reduces morbidity and mortality.
Conflict of interest statement
None declared.
REFERENCES
- 1. English WJ, DeMaria EJ, Brethauer SA, Mattar SG, Rosenthal RJ, Morton JM. American Society for Metabolic and Bariatric Surgery estimation of metabolic and bariatric procedures performed in the United States in 2016. Surg Obes Relat Dis 2018;14:259–63. [DOI] [PubMed] [Google Scholar]
- 2. Khan S, Rock K, Baskara A, Qu W, Nazzal M, Ortiz J. Trends in bariatric surgery from 2008 to 2012. The American Journal of Surgery, 211:1041–46. [DOI] [PubMed] [Google Scholar]
- 3. Agha F. Review intussusception in adults. AJR Am J Roentgenol 1986;146:527–31 [DOI] [PubMed] [Google Scholar]
- 4. Simper SC, Erzinger JM, McKinlay RD, Smith SC. Retrograde (reverse) jejunal intussusception might not be such a rare problem: a single group’s experience of 23 cases. Surg Obes Relat Dis 2008;4:77–83. [DOI] [PubMed] [Google Scholar]
- 5. Hocking MP, McCoy DM, Vogel SB, Kaude JV, Sninsky CA. Antiperistaltic and isoperistaltic intussusception associated with abnormal motility after Roux-en-Y gastric bypass: a case report. Surgery 1991;110:109–12. [PubMed] [Google Scholar]
- 6. Gayer G, Apter S, Hofmann C, Nass S, Amitai M, Zissin R, et al. Intussusception in adults: CT diagnosis. Clin Radiol 1998;53:53–7. [DOI] [PubMed] [Google Scholar]
- 7. Gayer G, Zissin R, Apter S, Papa M, Hertz M. Pictorial review: adult intussusception--a CT diagnosis. Br J Radiol 2002;75:185–90. [DOI] [PubMed] [Google Scholar]


