Summary
Background
The last comprehensive systematic review of the incidence of psychotic disorders was published in 2004. New epidemiological data from different settings now permit a broader understanding of global variation. We examined the variation in psychosis by demographic characteristics and study method.
Methods
For this systematic review and meta-analysis, we searched PubMed, Embase, Web of Science, PsycINFO, and bibliographies, and directly contacted first authors. We sought to obtain citations of original research published between Jan 1, 2002, and Dec 31, 2017, on incidence of non-organic adult-onset psychotic disorder. We included papers that were published or in grey literature and had no language restrictions. Data were extracted from published reports, where possible, by sex, age, and ethnic group. Quality of yield was assessed. Data were assessed using univariable random-effects meta-analysis and meta-regression. We registered our systematic review on PROSPERO, number CRD42018086800.
Findings
From 56 721 records identified, 177 met inclusion criteria. The pooled incidence of all psychotic disorders was 26·6 per 100 000 person-years (95% CI 22·0–31·7). Heterogeneity was high (I2≥98·5%). Men were at higher risk of all psychotic disorders (incidence rate ratio 1·44 [1·27–1·62]) and non-affective disorders (1·60 [1·44–1·77]) than women, but not affective psychotic disorders (0·87 [0·75–1·00]). Ethnic minorities were also at excess risk of all psychotic disorders (1·75 [1·53–2·00]), including non-affective disorders (1·71 [1·40–2·09]). Meta-regression revealed that population registers reported higher rates of non-affective disorders (9·64 [2·72–31·82]), schizophrenia (2·51 [1·24–5·21]), and bipolar disorder (4·53 [2·41–8·51]) than first contact study designs.
Interpretation
We found marked variation in incidence of psychotic disorders by personal characteristics and place. Some geographical variation could be partially explained by differences in case ascertainment methods.
Funding
None.
Introduction
Psychotic disorders are associated with substantial premature mortality,1, 2 morbidity,3 and a large social and financial burden.4 Yet, research into their distribution and determinants has only in the past decade extended beyond North America5 and northern Europe6, 7, 8 to southern Europe,9, 10, 11, 12 South America,13 Africa,14, 15 and other low-income and middle-income countries (LMICs).15, 16 These new data might provide new clues to the determinants of the heterogeneity in the incidence of psychotic disorders between and within different populations reported in previous studies,17, 18 aiding both service planning and our understanding of cause; both are crucial for planning effective public mental health responses. The most recent comprehensive systematic review and meta-analysis17 was published in 2004 and was restricted to schizophrenia. Further meta-analyses have limitations in terms of single country coverage,18 search scope, yield and assessment of heterogeneity,19 specific population group coverage20, 21 or coverage of a particular risk factor,22, 23, 24, 25, 26 or were also restricted to schizophrenia.27
Together, these reviews showed that estimates of the incidence of psychotic disorders vary across replicable demographic, geographical, and social characteristics. Men and young people appear to have an excess risk,27, 28 as do migrants and their descendants.20, 29, 30 Settings at higher latitude and more urban settings also yield higher incidences.26, 31 Socioeconomic deprivation, inequality, and instability are also associated with increased incidence.14, 32, 33, 34 Earlier meta-analyses17, 18, 35 found no evidence of variation in incidence by study quality or other methodological features. Research suggests36, 37 that higher incidences are derived from population registers (which cover all health-care contacts within an entire health system) than from first-contact studies (which rely on individuals making contact with appropriate services). These comparisons notwithstanding, methodological heterogeneity as an explanation for variation in incidences has not been investigated widely.
We sought to synthesise the accumulating research on the incidence of adult-onset psychotic disorders (including affective psychotic disorders) and investigate whether sociodemographic factors or methodological heterogeneity accounted for any observed variation. Consistent with available evidence, we hypothesised that incidences would be higher in men, younger people, and those from ethnic minority groups, and in register-based studies.
Research in context.
Evidence before this study
We searched PubMed and Web of Science (appendix p 4) for international systematic reviews and meta-analyses of the incidence of non-organic psychotic disorders in the general population, published since the last major review of the evidence (published in 2004). Our search yielded 156 results, of which 14 were meta-analyses. However, these commonly examined a single risk factor for psychotic disorders, such as migrant status, or synthesised evidence of incidence in a particular segment of the population, such as the elderly. Only one meta-analysis met all inclusion criteria and summarised incidence in the general population, but this study provided no assessment of heterogeneity.
Added value of this study
To the best of our knowledge, this study is the first comprehensive systematic review and meta-analysis of the incidence of non-organic adult-onset psychotic disorders done in 16 years and provides an update on the epidemiological landscape. For the first time, we also formally assessed if incidence of psychotic disorders varies by study type. Incidence varied substantially between settings: a 10 times variation in incidence was observed across diagnostic categories. We also found that studies with routine registers reported higher incidences of disorder than studies with a service-based design.
Implications of all the available evidence
Variance in the incidence of psychotic disorders worldwide arises from both replicable social, demographic, and environmental determinants, and from methodological heterogeneity. Although most studies continue to be done in a handful of countries, future studies across more diverse settings will benefit from standardised methods to facilitate comparable estimates of incidence across the globe.
Methods
Search strategy and selection criteria
This systematic review and meta-analysis followed PRISMA guidelines38 (appendix pp 2–3), including preregistering our protocol with PROSPERO (CRD42018086800) before extraction of data. Our method is based on a previous systematic review.18
We systematically searched PubMed, PsycINFO, Web of Science, and Embase, adapting a previously used search strategy18 based on Cochrane Systematic Reviewing guidelines.39 This strategy used terms covering psychotic disorders and incidence and was adapted for each database (appendix p 4). We searched bibliographies of included citations and directly contacted authors to request data, where appropriate. We restricted our review to studies published between Jan 1, 2002, and Dec 31, 2017. We had no restriction on language of publication, study design, or publication status, although grey literature was only identified via published conference proceedings, author correspondence, and bibliographical searches.
Citations were considered eligible if they contained incidence data or data from which incidence could be derived (numerator and denominator); included patients (aged 18–64 years) diagnosed with a first episode of any psychotic disorder; were published between Jan 1, 2002, and Dec 31, 2017, and were published in the scientific or grey literature, online, or in print.
Two authors (HEJ, CT) carried out searches and screened the titles found to assess whether they met eligibility criteria, with definite or possible titles forwarded to duplicate independent abstract review and, if appropriate, full text review. Uncertainties about inclusion were resolved in agreement with two senior authors with experience in epidemiological research and systematic reviewing (JBK, PBJ). The study protocol is available online.
Data analysis
Two authors (HEJ, CT) extracted data. Study-level data about study characteristics, rate-level data about incidences, and meta-level data on time period, study quality, study design, and diagnostic criteria (see below) were included.
The primary outcome was incidence per 100 000 person-years of all psychotic disorders (International Classification of Disease tenth edition [ICD-10] = equivalent, F20–33), non-affective disorders (F20–29), schizophrenia (F20), affective disorders (F30–33), bipolar disorder with psychosis (F30–31), psychotic depression (F32–33), or substance-induced psychosis (F1X.5). Included studies used a range of diagnostic classifications, including ICD-8, ICD-9, and ICD–10, and the Diagnostic and Statistical Manual of Mental disorders (DSM) versions 3-R and 4, and we assumed sufficient commonalities to pool citations (appendix p 5).
Where possible, we extracted summary-level incidence data on the exposures age, sex, ethnicity, and migrant status. Meta-level data on study design, study quality, and time period were recorded. Study design was divided into first-contact studies (which count the number of people attending the relevant service, and include first presentation, first diagnosis, first GP record, first admission, and first treatment), cohort studies, case-register studies (with a dedicated national patient register), and studies with a general population register covering an entire health system. Time period was defined as the median year of the case ascertainment period. Where incidences were not directly reported, we derived them from ancillary information wherever possible. Where citations reported overlapping data from the same study or population, we used set criteria to establish inclusion (appendix p 4).
The full spreadsheet containing all study-level, rate-level, and meta-level data is available online.
Two independent raters (HEJ, JBK or CT) assessed study quality according to seven previously published criteria:18 designation of a defined catchment area, accurate reporting and reliable source of denominator data, population-based case finding, standardised research diagnosis used, masking (of the clinician) to demographic variables, inclusion criteria stated, and inclusion of a leakage study (appendix p 4).
We first did a narrative synthesis of the yield. Based on previous meta-analyses,17, 18 we anticipated high levels of heterogeneity and therefore specified use of random-effects meta-analysis and meta-regression a priori to quantify this heterogeneity. When five or more incidences could be pooled, we did random-effects meta-analyses using the DerSimonian and Laird method,40 grouping citations by study design. We transformed incidence rates to their natural logarithm and entered into meta-analyses with corresponding standard errors (SE)s. If no SE could be derived, we retained studies for narrative synthesis only. For assessments of differences in incidence by sex and ethnicity, we estimated incidence rate ratios (IRRs), transformed them to their natural logarithm, and entered them into meta-analyses with their corresponding SEs.
We assessed statistical heterogeneity using the Q test and quantified using the I2 statistic, which identifies the proportion of the observed variance that reflects real differences in effect size. We examined evidence of small study effects (including publication bias) by visual inspection of funnel plots and formal testing using Egger's test for which at least 10 estimates were available.41 We did random-effects meta-regression to explore whether heterogeneity was associated with study quality, study design, or time period.
We did meta-analyses in Stata (version 13)42 using the metan and admetan commands. We did meta-regressions using the metareg package, and we did funnel plots and Egger's tests using the metafunnel and metabias packages.
We chose to display pooled estimates to prevent ad-hoc summaries of data but considering the high expected heterogeneity, the emphasis in interpretation of results is on the variation in incidences.
Role of the funding source
There was no funding source for this study.
Results
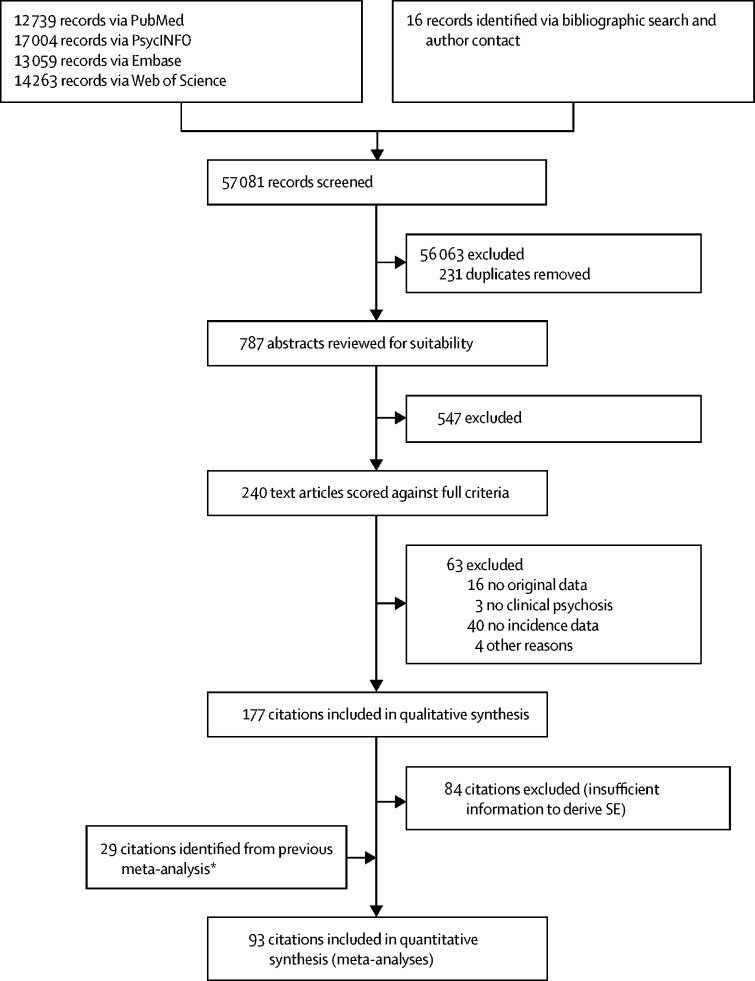
We retrieved 56 721 records of which 177 met inclusion criteria (figure 1; table); 93 (53%) of 177 had sufficient data available for meta-analysis and meta-regression. Most studies (140 [79%] of 177) were done in Europe, with 14 (8%) done in North America. Few studies were done in Asia (11 [6%]), the Middle East (seven [4%]), Australia, Latin or South America (four [2%] each), or Africa (two [1%]). Two citations covered more than one continent.15, 55 Citations examining psychosis in young people (26 [15%]), comorbid groups (12 [7%]), the army (seven [4%]), a prison population (one [<1%]), and post-partum psychosis (five [3%]) are synthesised in the appendix (pp 8–12) because they are not representative of the general population. The most frequently studied diagnostic outcome was schizophrenia (86 [49%]), followed by all non-affective disorders (66 [37%]) and all psychotic disorders (59 [33%]). Any affective psychotic disorder as an outcome was less frequently studied (32 [18%]), although we identified 40 (22%) citations of bipolar disorder with psychosis and 15 (8%) citations of psychotic depression. Six (3%) citations examined substance-induced psychosis.
Figure 1.
PRISMA flowchart
*Citations derived from Kirkbride and colleagues,18 which cover England only from 2002–09.
Table.
Study characteristics of included citations
| Country | Period | Type | Diagnostic confirmation | Diagnostic classification | Diagnostic outcomes | Number of cases | |
|---|---|---|---|---|---|---|---|
| Tsuchiya et al 200261* | Denmark | 1980–97 | First admission | .. | ICD-8, ICD-10 | Schz | Unknown |
| Hanoeman et al 200262* | Surinam | 1992–93 | First admission | Medical records | DSM-3-R | Schz, schzp | 73 |
| Selten et al 200263† | Netherlands | 1970–92 | Case register | None | ICD-8, ICD-9 | Schz | Unknown |
| Baldwin et al 200264‡ | Ireland | 1995–2000 | First contact | SCID or medical records | DSM-4 | FEP | 69 |
| Scully et al 200265* | Ireland | 1995–2000 | First contact | SCID or medical records | .. | FEP | 69 |
| Boydell et al 200366* | England | 1965–97 | Case register | Case notes plus OPCRIT | Combination | Schz | 623; 385 |
| Smith et al 200367‡ | Canada | 1907–13 | First admission | Clinical records | DSM-4 | Schz, schzp, bpd | 831 |
| Singh et al 200368 | England | 2000 | First contact | Interview, questionnaire, case notes | .. | FEP | 295 |
| Selten et al 200369 | Netherlands | 1990–96 | Case register | Discharge summary | ICD-9 | Bpd, pd | 14 749 |
| Cantor-Graae et al 200370‡ | Denmark | 1970–98 | Population register | None | ICD-8, ICD-10 | Schz | 10 244 |
| Baldwin et al 200371‡ | Ireland | 1995–2002 | First contact | SCID or clinical records | DSM-4 | FEP, non-aff, schiz, aff, bp, pd, other | 146 |
| Proctor et al 200472 | England | 1998–2001 | Case register | Chart diagnosis | ICD-10 | FEP, non-aff, schz, aff, bp, pd, sip, other | 227 |
| Sipos et al 200473 | Sweden | 1989–2001 | First admission | None | ICD-9, ICD-10 | Non-aff, schz | 1950 |
| Chien et al 200474‡ | Taiwan | 1997–2001 | First contact | None | ICD-9 | Schz | 419 |
| Boydell et al 200475* | England | 1988–97 | Combination | Case records using OCCPI | RDC | Schz | 222 |
| Veen et al 200476 | Netherlands | 1997–99 | First contact | Diagnostic meeting | DSM-4 | FEP, non-aff, aff, oth | 181 |
| Singh et al 200477 | England | 1992–94 | First contact | Interview, SCAN or SANS and OCCPI or OPCRIT | ICD-10 | FEP, non-aff, schz, aff, sip, oth | 168 |
| Sailas et al 200578§ | Finland | 1984–94 | Cohort | None | Other | FEP | 71 |
| Harris et al 200579*† | Australia | .. | First presentation | Consensus | DSM-4, ICD-10 | FEP, schz, aff | 94 |
| Sundquist et al 200580‡ | Sweden | 1997–99 | Population register | None | ICD-9, ICD-10 | FEP, pd | 6163 |
| Nager et al 200581¶ | Sweden | 1986–97 | Cohort | None | ICD-9, ICD-10 | FEP | 339 |
| Laursen et al 200582‡ | Denmark | 1952–87 | Population register | None | ICD-8, ICD-10 | Schz, schza, bp | 18 147 |
| Selten et al 200583 | Surinam | 2002–03 | First contact | CASH interview, panel discussion | DSM-4 | FEP | 64 |
| Nixon et al 200584 | England | 1881–1994 | Combination | Case notes | RDC | Schz | 41 |
| Qin et al 200585‖ | Denmark | 1950–87 | Population register | None | ICD-8, ICD-10 | Non-aff, schz | 795 |
| Allardyce et al 200586 | Scotland | 1989–93 | First admission | Case record | ICD-9 | FEP | 5838 |
| Cantor-Graae et al 200587 | Sweden | 1999–2001 | First contact | Clinical, case records, additional data | DSM-4 | FEP, non-aff | 150 |
| Baldwin et al 200543 | Ireland | 1995–2003 | First contact | SCID or clinical diagnosis | DSM-4 | FEP, non-aff, schz, aff, bpd, pd, oth | 194 |
| Kennedy et al 2005a88 | England | 1965–99 | Combination | Case notes plus OPCRIT | DSM-4 | Bpd | 246 |
| Kennedy et al 2005b89* | England | 1965–99 | Combination | Case notes plus OPCRIT | DSM-4, ICD-10 | Bpd | 246; 235 |
| Lloyd et al 200590‡ | England | 1997–99 | First contact | Interview (SCAN, SANS, modified PPHS), consensus diagnosis | ICD-10 | Bpd | 75 |
| Leão et al 20068† | Sweden | 1992–99 | Population register | None | ICD-9, ICD-10 | Non-aff | Unknown |
| Bray et al 200691† | Canada | 1975–85 | First contact | None | ICD-10 | Schz | 1962 |
| Payne et al 200692 | Canada | 1993–95 | First admission | Clinical records | .. | Non-aff | 146 |
| Drukker et al 200693 | Netherlands | 1993–2002 | Case register | None | DSM-4 | Schz | 98 |
| Turner et al 200694** | England | 1999–2002 | First admission | Case notes, ratified by psychiatrist | ICD-10 | Non-aff, schz | 62 |
| Mahmmood et al 200695 | England | 2005–05 | First contact | Unknown | .. | FEP | 303 |
| Westman et al 200696‡ | Sweden | 1997–98 | Population register | None | ICD-9, ICD-10 | FEP | 10 800 |
| Munk-Olsen et al 200697¶ | Denmark | 1955–90 | Population register | None | ICD-8, ICD-10 | Non-aff, schz | 166 |
| Smith et al 200644 | Canada | 1902–13 | First admission | Clinical records | DSM-4 | Schz, schza, schp, oth | 807 |
| Amminger et al 200698† | Australia | 1997–2000 | First treatment | Youth assessment team, random sample SCID or RPMIP | DSM-4 | FEP | 1019 |
| Veling et al 20067 | Netherlands | 1997–2005 | First contact | Diagnostic meeting | DSM-4 | Non-aff | 181 |
| Morgan et al 200699‡ | England | 1997–99 | First contact | Interview (SCAN), case notes, consensus meeting | ICD-10 | FEP, schz | 592 |
| Fearon et al 2006100* | England | 1997–99 | First contact | Interview (PSE SCAN), case notes (IGC SCAN) | ICD-10 | FEP, schz, bpd, pd, oth | 568 |
| Gould et al 2006101 | England | 1997–99 | First presentation | WHO screening for psychosis plus OPCRIT | ICD-10 | FEP | 111 |
| Kirkbride et al 20066 | England | 1997–99 | First contact | SCAN, consensus panel | DSM-4 | FEP, non-aff, schz, aff, sip | 568 |
| Zipursky et al 2006102 | England | 1997–99 | First contact | SCAN, consensus panel | DSM-4 | FEP, schz | Unknown |
| Li et al 2007103 | Sweden | 1984–2004 | Population register | None | ICD-9, ICD-10 | FEP | 40 228 |
| Schimmelmann et al 2007104* | Australia | 1998–2000 | First admission | SCID and clinical diagnosis comparison | DSM-4 | FEP | 636 |
| Laursen et al 2007105 | Denmark | 1995–87 | Population register | None | ICD9, ICD-10 | Schz, bpd | 17 787 |
| Ajdacic-Gross et al 2007106† | Switzerland | 1977–2005 | Case register | None | ICD-8, ICD-9 | FEP, schz | 7230 |
| Andersen et al 2007107 | Norway | 1887–2005 | First admission | Case records | ICD-10 | Schz, aff | 64 |
| Harlow et al 2007108 | Sweden | 1987–2001 | Cohort | None | ICD-8, ICD-9 | Non-aff, schz, schza, bpd | 2134 |
| Juvonen et al 2007109‖ | Finland | 1950–59 | Population register | Case notes (2 experts) | DSM-4 | Schz | 807 |
| Cantor-Graae et al 2007a110‡ | Denmark | 1986–2006 | Population register | None | ICD-8, ICD-10 | Schz | 4609 |
| Cantor-Graae et al 2007b111‡ | Denmark | 1970–2001 | Population register | None | ICD-8, ICD-10 | Schz | 10 779 |
| Leão et al 2007112*† | Sweden | 1995–98 | Population register | None | ICD-9, ICD-10 | Non-aff, aff | Unknown |
| Kikbride et al 2007a113 | England | 1997–99 | First contact | SCAN, consensus panel | ICD-10 | FEP, non-aff, aff | 295 |
| Menezes et al 200713 | Brazil | 2002–2004 | First contact | SCID-I or case notes | DSM-4 | FEP, non-aff, aff | 367 |
| Kirkbride et al 2007b114‡ | England | 1997–99 | First contact | SCAN, consensus panel | ICD-10 | Non-aff, schz, oth | 218 |
| Stain et al 2008115† | Australia | 2001–2005 | First contact | Case notes | Other | Oth | 308 |
| Boonstra et al 2008116 | Netherlands | 2002 | First contact | Clinical diagnosis | DSM-4 | Non-aff | 75 |
| Crebbin et al 2008117* | England | 1998–2005 | Case register | Chart diagnosis | ICD-10 | FEP, schz, pd | 540 |
| Farquhar et al 200845 | Wales | 1875–2005 | First admission | Case records | ICD-10 | Schz, schza, aff, bpd, pd, oth | 579 |
| Pelayo-Teran et al 200810 | Spain | 2001–05 | First contact | SCID-I | DSM-4 | Non-aff | 174 |
| Castagnini et al 2008118* | Denmark | 1996 | Case register | None | ICD-8 | Schz, bpd, oth | 11 126 |
| Burns et al 200814 | South Africa | 2005 | First presentation | Case records | DSM-4 | FEP | 160 |
| Weiser et al 2008119 | Israel | .. | Population register | None | ICD-9, ICD-10 | Schz | 1686 |
| Veling et al 2008120 | Netherlands | 1997–2005 | First contact | Diagnostic meeting | DSM-4 | FEP, non-aff, bpd, pd, oth | 466 |
| Kirkbride et al 2008a121‡ | England | 1997–99 | First contact | SCAN, consensus panel | ICD-10 | Schz | 148 |
| Kirkbride et al 2008b122 | England | 1996–2000 | First contact | SCAN, consensus panel | DSM-4 | FEP, schz, non-aff, oth | 484 |
| Coid et al 200123 | England | 1996–2000 | First contact | SCAN, consensus panel | DSM-4 | FEP, non-aff, schz, aff, oth | 484 |
| Grant et al 200124†† | USA | 2004–05 | Cohort | Not stated | DSM-4 | Bpd | 263 |
| Crebbin et al 2009125* | England | 1998–2005 | Case register | Chart diagnosis | ICD-10 | Schz, sip | 430 |
| Bih et al 2009126*†† | Taiwan | 1996–2003 | Cohort | None | ICD-9 | Bpd | 532 |
| Corcoran et al 2009127† | Israel | 1964–97 | Cohort | None | ICD-10 | Non-aff | 637 |
| Osby et al 2009128* | Sweden | 1997–2005 | Case register | None | ICD-10 | Bpd | 4117 |
| Valdimarsdottir et al 2009129¶ | Sweden | 1983–2000 | Cohort | None | ICD-8, ICD-9 | FEP | 4557 |
| Harlap et al 2009130 | Israel | 1964–76 | Cohort | None | ICD-10 | Schz | 637 |
| Reay et al 2009131 | England | 1998–2005 | First contact | Chart diagnosis | ICD-10 | FEP, non-aff, schz, aff, bpd, pd | 540 |
| Norredam et al 2009132 | Denmark | 1994–2003 | Cohort | None | ICD-10 | Non-aff | 1127 |
| Bogren et al 2009133 | Sweden | 1947–97 | First contact | Key informants, case files | DSM-4 | Non-aff, schz, schza, aff, bpd | 61 |
| Kirkbride et al 2009134‡ | England | 1978–99 | Combination | SCAN, consensus agreement | ICD-9, ICD-10 | FEP, non-aff, schz, aff, bpd, pd, sip, oth | 347 |
| Coid et al 2009123 | .. | .. | .. | .. | .. | .. | .. |
| Cheng et al 2010135† | England | 2002–2007 | First contact | Unsure | ICD-10 | FEP | 285 |
| Bogren et al 201046 | Sweden | 1947–97 | First presentation | Key informants, case files | DSM-4 | Non-aff, aff, bpd | 108 |
| Zammit et al 2010136‡ | Sweden | 1972, 1977 | First admission | None | ICD-8, ICD-9 | Non-aff, schz | 881 |
| Tseng et al 2010137 | Taiwan | 1996–2001 | First hospitalisation | None | ICD-9 | Schz | Unknown |
| Zandi et al 2010138 | Netherlands | 2002–04 | First contact | CASH or CASH-CS, medical files, consensus diagnosis | DSM-4 | FEP, schz | 77 |
| Norredam et al 2010139‡ | Denmark | 1994–2003 | Cohort | None | ICD-10 | Non-aff | 791 |
| Goodman et al 201147** | USA | .. | First contact | Not stated | ICD-9 | FEP | 8 |
| Cowan et al 2011140** | USA | 2000–09 | First hospitalisation | None | ICD-9 | Non-aff | 2722 |
| Harris et al 2011141* | Wales | 1875–2005 | First admission | Panel assessment of case notes | ICD-10 | Pd | 800 |
| Jorgensen et al 2011142 | Sweden | 2005 | Case register | Random sample checked by psychiatrist | ICD-10 | Non-aff, schz | 416 |
| Cheng et al 2011143† | England | 2002–07 | First contact | Multidisciplinary diagnostic meeting | ICD-10 | FEP | 285 |
| Kleinhaus et al 2011144† | Israel | 1964–76 | Cohort | None | ICD-10 | Non-aff | 860 |
| Benros et al 2011145‖ | Denmark | 1945–96 | Population register | None | ICD-8, ICD-10 | Non-aff | 39 076 |
| Salokangas et al 2011146 | Finland | .. | Case register | None | ICD-8, DSM-3-R, ICD-10 | Schz | 30 032 |
| Schofield et al 2011147 | England | 1996–2006 | First GP record | Patient records | READ codes | FEP | 508 |
| Veling et al 2011148 | Netherlands | 1997–2005 | First contact | Diagnostic meeting | DSM-4 | FEP | 618 |
| Healy et al 2012149* | Wales | 1875–2005 | First admission | Case records, clinical diagnosis | ICD-10 | Schz, oth | 3523 |
| Callaghan et al 2012150* | USA | 1990–2000 | First hospitalisation | Not stated | ICD-9 | Schz | 1499 |
| Anderson et al 2012151† | Canada | 2000–06 | First contact | None | .. | Non-aff | 546 |
| Manrique-Garcia et al 2012152** | Sweden | 1969–70 | First admission | None | ICD-8, ICD-9 | Non-aff, schz | 674 |
| Turola et al 2012153 | Italy | 1979–2008 | First diagnosis | Case notes | DSM-4, ICD-10 | Schz | 1759 |
| Werbeloff et al 2012154 | Israel | 1979–92 | Case register | None | ICD-9 | Schz | 2335 |
| Nosarti et al 2012155† | Sweden | 1973–85 | First admission | None | ICD-8 and ICD-9 | Non-aff, bpd | 886 |
| Gigantesco et al 2012156 | Italy | 2008 | First contact | SCID-I, BPRS, GAF in duplicate | DSM-4 | FEP, bpd | 247 |
| Tarricone et al 201211 | Italy | 2002–09 | First contact | SCAN, consensus diagnosis | ICD-10 | FEP, Non-aff, schz, aff | 163 |
| Kirkbride et al 2012157† | England | 2009–11 | First presentation | Clinical diagnoses | ICD-10 | FEP | .. |
| Hung et al 2013158‖†† | Taiwan | 2000–05 | Cohort | None | ICD-9 | Bpd | 9711 |
| Peritogiannis et al 2013159 | Greece | 2008–09 | First contact | None | ICD-10 | FEP | 132 |
| Sutterland et al 2013160 | Netherlands | 1996–2006 | First GP record | Medical records | ICPC | Non-aff, schz | 293 |
| Cantor-Graae et al 2013161†‡ | Denmark | 1995–2010 | Population register | None | ICD-8, ICD-10 | Non-aff, schz, schza, bpd | 13 729 |
| Kroon et al 2013162 | Netherlands | 1996–2007 | First GP record | Medical records | ICPC | Bpd | 649 |
| Castagnini et al 2013163‡ | Denmark | 1995–2008 | First diagnosis | None | ICD-10 | Oth | 11 126 |
| Hardoon et al 2013164 | England | 2000–10 | First record or diagnosis | GP records | READ | Schz, bpd, oth | 10 520 |
| Weibell et al 2013165 | Norway | 2007–11 | First presentation | SCID | DSM-4 | Non-aff, sip | 321 |
| Cocchi et al 2014166 | Italy | 2007–09 | First contact | ERIaos-CL, sociodemographic form, HoNOS, BPRS, WHO-DAS III | ICD-10 | Non-aff | 43 |
| Tortelli et al 2014167 | France | 2005–09 | First admission | Case notes | ICD-10 | FEP | 258 |
| Hogerzeil et al 201437 | Netherlands | 2000–05 | First contact and case register | Diagnostic meeting and clinical regularly audited) | DSM-4 | Schz | 254; 843 |
| Pedersen et al 2014168* | Denmark | 1995–2006 | Case register | None | ICD-10 | Oth | Unknown |
| Sørensen et al 2014169* | Denmark | 1993–95 | Population register | None | ICD-8, ICD-10 | Schz | 17 389 |
| Munk-Olsen et al 2014170¶ | Denmark | 1960–95 | First treatment | None | ICD-8, ICD-9 | Oth | Unknown |
| Szoke et al 2014171 | France | 2010–12 | First contact | Identical procedures, regular meetings | DSM-4 | FEP, non-aff, aff | 133 |
| Bhavsar et al 2014172† | England | 2000–07 | First contact | Case notes | RDC | Schz | 405 |
| Omer et al 2014173‡ | Ireland | 1995–2000 | First contact | SCID or clinical records | DSM-4 | FEP | 336 |
| Lasalvia et al 20149 | Italy | 2005–07 | First contact | Interview, consensus diagnosis | ICD-10 | FEP, non-aff, schz, aff, bpd, pd | 558 |
| Veling et al 2014174 | Netherlands | 1997–2005 | First contact | Diagnostic meeting | DSM-4 | FEP, schz, aff, bpd, pd, oth | 618 |
| Kirkbride et al 201434‡ | England | 1996–2000 | First contact | SCAN, consensus diagnosis | DSM-4 | Non-aff, aff | 484 |
| Anderson et al 20155† | Canada | 1999–2008 | Population register | Medical records or billing claims | Non-aff | Unknown | |
| Paksarian et al 2015a175† | Denmark | 1986–2010 | Population register | None | ICD-8, ICD-10 | Non-aff, schz, bpd | 15 811 |
| Sørensen et al 2015176 | Denmark | 1955–67 | Population register | None | ICD-8, ICD-10 | Non, aff, schz, aff | 15 074; 7562 |
| Paksarian et al 2015b177 | Denmark | 1986–2011 | Population register | None | ICD-8, ICD-10 | Non-aff, schz, bpd | 14 285 |
| Soderlund et al 2015178† | Sweden | 1955–67 | Population register | None | ICD-10 | Non-aff, schz, aff | 2322 |
| Medici et al 2015179†† | Denmark | 1995–2012 | Case register | None | ICD-10 | Bpd | 15 334 |
| Carlborg et al 2015180†† | Sweden | 1991–2010 | Case register | None | ICD-10 | Bpd | 10 273 |
| Tsai et al 2016181‖†† | Taiwan | 2000–07 | Cohort | None | ICD-9 | Bpd | 202 |
| Chen et al 2015182‖†† | Taiwan | 2000–06 | Cohort | None | ICD-9-CM | Bpd, pd | 118 |
| Latvala et al 2016183** | Sweden | 1969–2010 | Case register | None | ICD-8/9/10 | Schz, bpd | 14 840 |
| Jensen et al 2016184*†† | Denmark | 1995–2010 | Case register | None | ICD-10 | Bpd | 12 034 |
| Kuhl et al 2016185* | Denmark | 2000–12 | Population register | None | ICD-10 | Non-aff, schz | 23 479 |
| Filatova et al 2016186† | Finland | 1966–2013 | Cohort | None | ICD-8, ICD-10 | Non-aff, schz, bpd, oth | 295 |
| Chiang et al 201648 | Taiwan | 1998–2007 | First admission | None | ICD-9-CM | FEP | 69 690 |
| Nielsen et al 2016187‡ | Denmark | 1997–2002 | Population register | None | ICD-8, ICD-10 | Schz | 6927 |
| Kendler et al 201649 | Sweden | 1972–90 | Population register | None | ICD-9, ICD-10 | Non-aff, schz, bpd | 22 589 |
| Levine et al 2016a188* | Israel | 1950–2004 | Cohort | None | ICD-10 | Schz | 2278 |
| Levine et al 2016b189* | Israel | 1950–2014 | Cohort | None | ICD-10 | Schz | 665 |
| Vassos et al 201650‡ | Denmark | 1995–2006 | Population register | None | ICD-10 | FEP, non-aff, bpd | 32 983 |
| Sørensen et al 2016190* | Denmark | 1930–76 | Cohort | None | ICD-8, ICD-10 | Schz | 4936 |
| Hollander et al 2016191† | Sweden | 1998–2011 | Population register | None | ICD-10 | Non-aff | 3704 |
| O'Donoghue et al 2016192 | Ireland | 2006–11 | First presentation | SCID | DSM-4 | FEP | 292 |
| Morgan et al 201615 | India, Nigeria, Trinidad | .. | First contact | SSP, consensus diagnosis | ICD-10 | FEP | 147 |
| Tarricone et al 2016193 | Italy | 2002–10 | First contact | SCAN | ICD-10 | FEP | 187 |
| Szoke et al 2016194 | France | 2010–14 | First contact | Unclear—senior review if uncertain | DSM-4 | Non-aff, aff | 212 |
| Mulé et al 201612 | Italy | 2008–11 | First contact | SCAN | ICD-10 | FEP, schz, aff, oth | 204 |
| Ramsey et al 201751** | USA | 2001–14 | Cohort | None | ICD-9 | Schz, bpd | 24 714 |
| Okkels et al 2017195‖ | Denmark | 1985–2001 | Population register | None | ICD-8, ICD-10 | Non-aff, schz, bpd | 9329 |
| Vikstrom et al 2017196¶ | Sweden | 1988–2012 | Cohort | None | ICD-8, ICD-10 | Non-aff, bpd | 91 |
| Wang et al 2017197‖ | Taiwan | 1997–2007 | Cohort | None | ICD-9 | Schz | 238 |
| Lin et al 2017198‖†† | Taiwan | 2001–06 | Cohort | None | ICD-9 CM | Bpd | 183 |
| Marrie et al 2017a199‖ | Canada | 1989–2012 | Case register | None | ICD-9 CM | Schz, bpd | Unknown |
| Marrie et al 2017b200‖ | Canada | 1984–2013 | Case register | None | ICD-9 CM | Schz, bpd | Unknown |
| Hogerzeil et al 2017201 | Netherlands | 2000–05 | First contact or case register | Structured interview or clinical, then consensus | DSM-4 | Schz | 254; 843 |
| Hoeffding et al 2017202 | Denmark | 1995–2013 | Population register | None | ICD-8, ICD-10 | Non-aff | 31 647 |
| Kim et al 201752 | South Korea | 2002–13 | Cohort | None | ICD-10 | Non-aff | 9387 |
| Markkula et al 201753 | Finland | 2011–14 | Population register | None | ICD-10 | Non-aff, bpd | 2905 |
| Nielsen et al 2017203‖ | Denmark | 1955–99 | Population register | None | ICD-8, ICD-10 | Schz | 21 305 |
| Schofield et al 2017204 | Denmark | 1965–97 | Population register | None | ICD-8, ICD-10 | Non-aff | 26 891 |
| Simon et al 201754 | USA | 2007–13 | First contact | None, subset case records | ICD-9 | FEP | 37 843 |
| Kirkbride et al 2017a205† | England | 2009–13 | First contact | OPCRIT | ICD-10 | FEP, non-aff, schz, aff, bpd, pd, sip | 687 |
| Kirkbride et al 2017b206† | England | 2009–13 | First contact | OPCRIT | ICD-10 | FEP, non-aff, schz, aff | 687 |
| Schofield et al 2018207‡ | Denmark | 1965–2013 | Population register | None | ICD-8, ICD-10 | Non-aff | Unknown |
| Nyberg et al 2018208**‡‡ | Sweden | 1968–2005 | Cohort | None | ICD-8, ICD-9, ICD-10 | Non-aff | 4641 |
| Barghadouch et al 2018209†‡‡ | Denmark | 1993–2000 | Cohort | None | ICD-10 | Non-aff | 392 |
| Richardson et al 2018210†‡‡ | England | 2009–13 | First contact | OPCRIT | ICD-10 | FEP, non-aff, schz, aff | 0687 |
| Jongsma et al 201855 | England, Netherlands, France, Spain, Italy, Brazil | 2005–15 | First contact | SCAN, CASH, DIGS, SID, or case notes—OPCRIT | ICD-10 | FEP, non-aff, aff | 2774 |
All references up to and including 60 are found in the reference list of the main article. References from 61 onwards are found in the appendix (pp 35–43). Aff=affective psychosis. Bpd=bipolar disorder. BPRS=Brief Psychiatric Rating Scale. CASH=Comprehensive Assessment of Symptoms and History. CASH-CS=CASH-Culturally Sensitive. DIGS=Diagnostic Interview for Genetic Studies. DSM=Diagnostic and Statistical Manual. ERIaos-CL=Early Recognition Inventory Retrospective Assessment of Symptoms checklist. FEP=all first episode psychosis. GAF=Global Assessment of Functioning. HoNOS=Health of the Nations Outcome Scale. ICD=International Classification of Disease. Non-aff=non-affective psychosis. OCCPI=Operational Criteria Checklist for Psychotic Illness. OPCRIT=Operational Criteria Checklist for Psychotic Illness. Oth=other. Pd=psychotic depression. PPHS=Personal and Psychiatric History Schedule. PSE=Present State Examination. RDC=Research Diagnostic Criteria. RPMIP=Royal Park Multidiagnostic Instrument for Psychosis. SANS=Scale for the Assessment of Negative Symptoms. SCAN=Schedules Clinical Assessment Neuropsychiatry. Schz=schizophrenia. Schzp=schizophreniform disorder. Schza=schizoaffective disorder. SCID=Structural Clinical Interview for DSM-4. SCID-I=SCID-Axis I disorders. Sip=substance-induced psychosis. SID=Structured Interview for DSM-4. SSP=Screening Schedule for Psychosis. WHO-DAS III=WHO Disability Assessment Schedule.
Citations with insufficient data to include in quantitative analyses.
Citations only covering young people (<40 years).
Citations only containing information covered in more detail in other citations.
Citations covering a prison population.
Citations covering post-partum psychosis.
Citations covering comorbid populations.
Citations covering the army only.
Citations including psychotic bipolar disorder, but where this can't be clearly differentiated from bipolar disorder more widely (not included in analyses).
Published online in 2017.
The largest study in this Article48 included 69 690 cases, and the smallest study47 identified eight cases. The middle year of recruitment varied from 190844 to 2012,53 with most citations (105 [59%]) recruiting between approximately 1995 and 2006. Most studies reported a clearly defined catchment area (174 [98%]), clearly listed their inclusion criteria (166 [94%]), used accurate denominator data (157 [89%]), and employed population-based case-finding (135 [76%]). Few studies done used a standardised research diagnosis (50 [28%]), did a leakage study (28·5 [16%]), or used blinding to demographic variables (18 [10%]; appendix pp 6–8). 92 (52%) citations reflected first contact designs and 76 (43%) used a cohort, case, or population register. The remaining nine (5%) studies used a combination. 40 (23%) citations used a version of the DSM for diagnoses and 118 (67%) used a version of ICD. The remaining 19 (11%) used a combination, used a different diagnostic system, such as the Research Diagnostic Criteria, or it was not reported (three [2%]; table). To confirm clinical diagnoses, 21 (12%) citations used a structured interview instrument only, 19 (11%) reviewed medical records, 14 (8%) used a structured interview followed by consensus diagnosis, 13 (7%) used only an interview without specifying whether an instrument was used, ten (6%) used only a consensus or panel discussion, and five (2%) used a chart or clinical diagnoses. The remaining citations either relied solely on clinical diagnoses in registry data (85 [48%]), or information was not stated (ten [6%]; table).
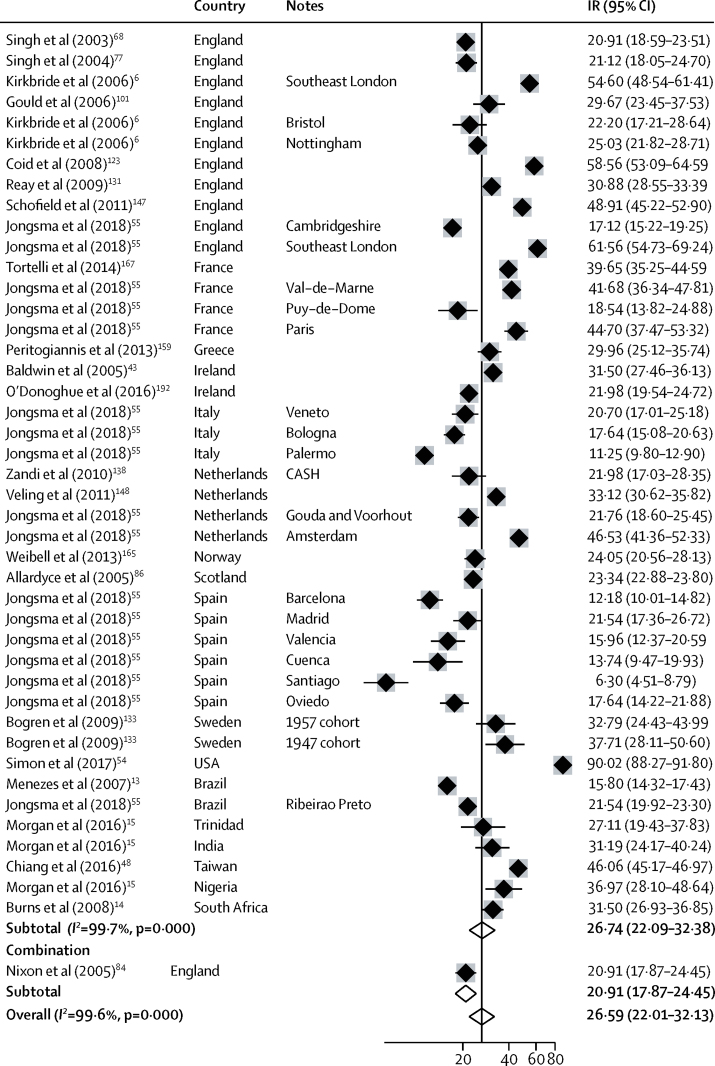
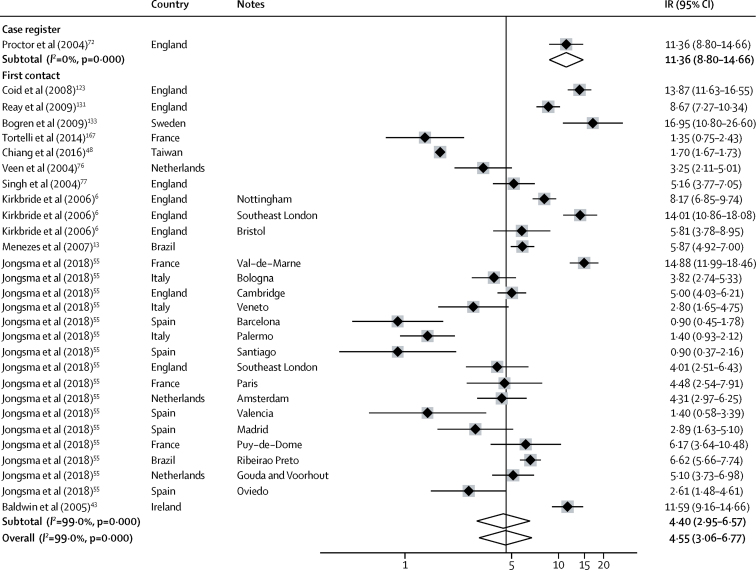
We included 44 separate estimates of the incidence of all psychotic disorders derived from 27 citations, including estimates from multicentre studies (figure 2). Incidence varied around 15 times, from 6·3 per 100 000 person-years (95% CI 4·5–8·8) in Santiago (Spain)55 to 90·0 (88·3–91·8) in the USA.54 The overall pooled incidence of all psychotic disorders was 26·6 per 100 000 person-years (22·0–31·7).
Figure 2.
Incidence of all psychotic disorders
References from 61 onwards are found in the appendix (pp 35–43). IR=incidence rates. Note: weights are from random effects analysis.
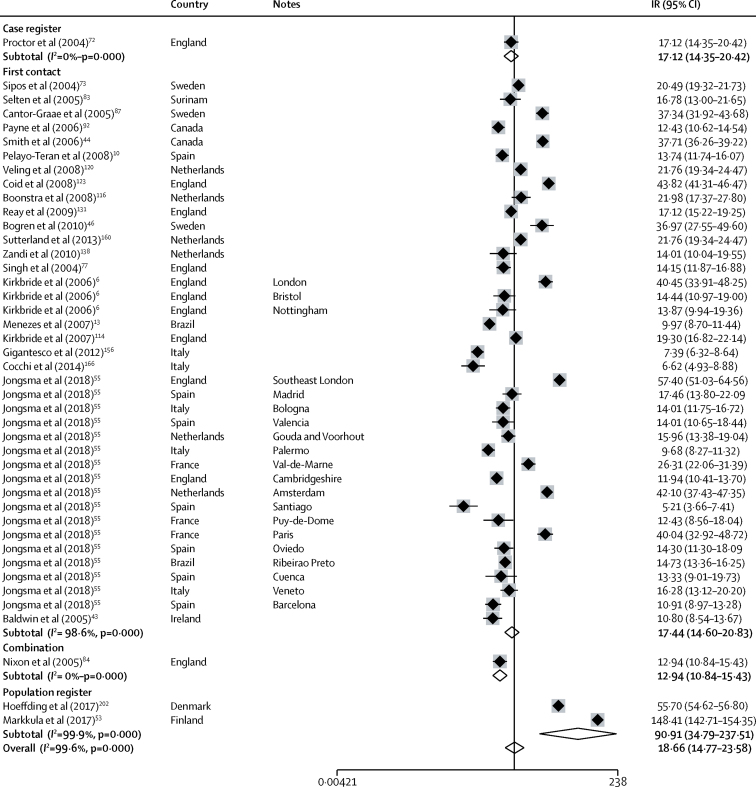
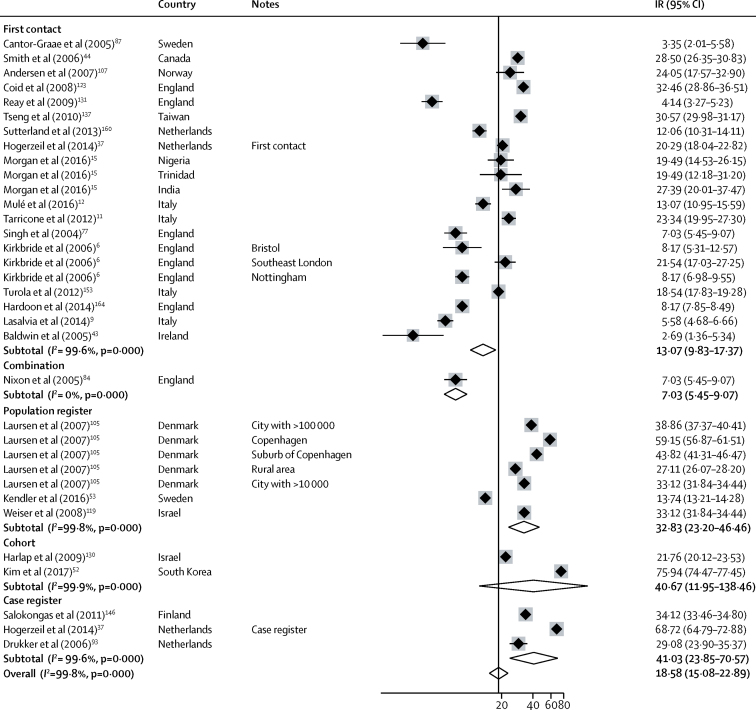
Incidence of non-affective disorders was available from 47 incidences derived from 28 citations (figure 3). Incidence varied almost 30 times, from 5·2 per 100 000 years (95% CI 3·7–7·4) in Santiago55 to 148·4 (142·7–154·4) in Finland.53 The overall pooled incidence was 18·7 per 100 000 person-years (14·8–23·6), but this incidence was lower in first-contact studies at 17·4 (14·6–20·8) compared with population register studies (pooled incidence rate 90·9 [34·5–237·5]; figure 3). The incidence of schizophrenia was available from 36 incidences from 26 citations and varied from 2·7 per 100 000 person-years (1·4–5·3) in Cavan-Monaghan (Ireland)43 to 75·9 (74·4–77·5) in South Korea.52 Pooled incidence was lower in first contact studies (13·1 per 100 000 person-years [9·0–15·0]) than in population registers (32·8 [23·2–46·5]; figure 4).
Figure 3.
Incidence of non-affective disorders
References from 61 onwards are found in the appendix (pp 35–43). IR=incidence rates. Note: weights are from random effects analysis.
Figure 4.
Incidence of schizophrenia
References from 61 onwards are found in the appendix (pp 35–43). IR=incidence rates. Note: weights are from random effects analysis.
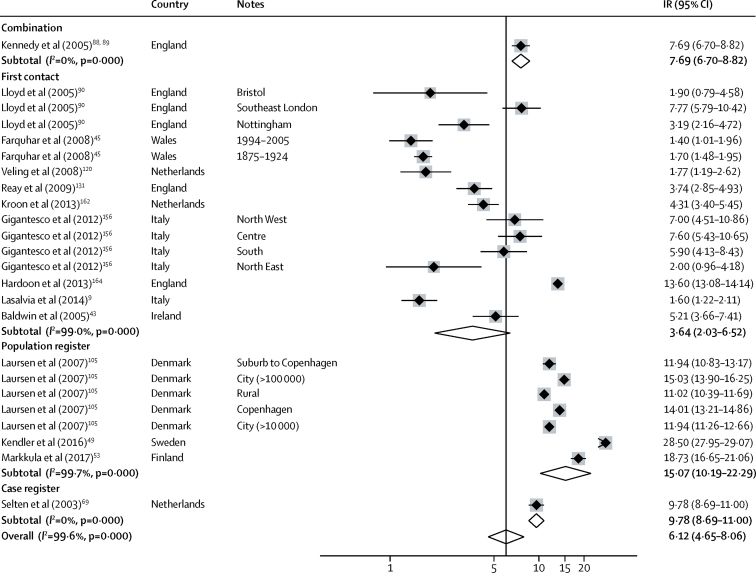
We pooled 34 estimates of the incidence of affective psychotic disorders from 16 citations. Incidence varied from 0·9 per 100 000 person-years (95% CI 0·4–2·2) in Santiago55 to 17·0 (10·8–26·6) in Lundby (Sweden).46 The overall pooled rate was 4·6 per 100 000 person-years (3·1–6·8; figure 5). 24 estimates of the incidence of bipolar disorder were included in a meta-analysis, derived from 15 citations. Incidence varied from 1·4 per 100 000 person-years (1·0–2·0) in Wales45 to 28·5 (28·0–29·1) in Sweden,49 and was higher in population registers (15·1 [10·2–22·3]) than first contact studies (3·6 [2·0–6·5]; figure 6). Insufficient citations were available to pool rates for other outcomes.
Figure 5.
Incidence of affective disorders
References from 61 onwards are found in the appendix (pp 35–43). IR=incidence rates. Note: weights are from random effects analysis.
Figure 6.
Incidence of bipolar disorder
References from 61 onwards are found in the appendix (pp 35–43). IR=incidence rates. Note: weights are from random effects analysis.
Pooled estimates of the incidence of all psychotic disorders were similar across high-income and LMICs (appendix pp 11–16), though heterogeneity was substantial in both sets of data; formal comparisons were hampered by insufficient studies in LMICs.
For all psychotic disorders, 26 estimates of IRRs in men compared with women were available from 10 citations, with a pooled IRR of 1·44 (95% CI 1·27–1·62). A similar pattern was observed for non-affective psychoses (1·60 [1·44–1·77]; derived from 27 estimates using 11 citations) and schizophrenia (1·70 [1·46–1·97]; derived from 11 estimates using 11 citations). No excess risk in men was found for affective disorders (IRR 0·87 [0·75–1·00]; p=0·07; derived from 20 estimates using six citations) or for psychotic bipolar disorder (0·90 [0·73–1·11]; derived from five estimates; appendix p 17). Insufficient citations were available to pool IRRs for other outcomes.
Migrants and their descendants were at excess risk of all psychotic disorders, non-affective disorders, and schizophrenia (insufficient citations were available to synthesise results for other diagnostic outcomes). When pooling all migrant groups to a binary majority or minority division, 22 estimates from seven citations were available to pool IRRs for all psychotic disorders (pooled IRR 1·75 [95% CI 1·53–2·00]). The pooled IRR for non-affective disorders was 1·71 (1·40–2·09), derived using 28 estimates from thirteen citations. The pooled IRR for schizophrenia was 1·41 (1·15–1·75), derived using six estimates (appendix p 18). Risk was not equitably distributed across ethnic minority groups (appendix pp 19–21).
We did not pool estimates by age group because of the large variety of age groups used. Nonetheless, we observed an overall pattern of higher incidence in younger age groups (appendix pp 22–24). For example, in the multinational EU-GEI study55 incidence of all first episode psychosis ranged from 44·2 per 100 000 person-years (95% CI 42·2–46·2) in people aged 18–24 years to 5·5 (3·2–7·7) in people aged 60–64 years.55
We found some evidence that study design was associated with variation in incidence. Population registers had higher incidences of non-affective disorders (IRR 9·64 [2·72–31·82]), schizophrenia (2·54 [1·24–5·21]), and bipolar disorder (4·53 [2·41–8·51]) than first contact studies. Incidence of schizophrenia was also elevated in cohort studies (3·10 [1·12–8·53]) and case registers (3·12 [1·33–7·29]). Cohort studies (0·43 [0·20–0·93]) and population registers (0·42 [0·22–0·83]) recorded lower IRRs by minority status for non-affective disorders than first contact designs, but we found no differences by study design in IRRs for any other exposure or outcome association. We found little evidence that study quality and time period were associated with changes in incidence or IRR (appendix pp 25–28).
Heterogeneity was high across study outcomes (I2 ≥98·5%; Figure 2, Figure 3, Figure 4, Figure 5, Figure 6). Small study effects, as evidenced by Egger's test, were shown in the overall meta-analyses of incidences of all psychotic disorders (β −7·53 [SE 3·14]; p=0·021), non-affective disorders (–14·55 [2·46]; p<0·001), schizophrenia (–11·78 [5·52]; p=0·041), affective disorders (7·72 [1·60]; p<0·001), and bipolar disorder (–14·97 [2·78]; p<0·001). They were also found in analyses by sex for all psychotic disorders (2·16 [0·44]; p<0·001) and affective disorders (0·90 [0·24]; p=0·001), but not for other diagnostic outcomes or for analyses by ethnic group (appendix pp 29–32). Post-hoc sensitivity analyses supported some remaining small study effects within first contact designs (appendix p 32).
Discussion
Our systematic review identified 177 citations containing data on the incidence of psychotic disorders published since 2002. This yield is considerably higher than reported in another systematic review19 and was marked by substantial heterogeneity in incidence across all major psychotic disorders. Although we found no evidence that incidences varied with study quality or time period, we did observe strong evidence of higher incidence rates reported in register-based or cohort-based study designs than in first-contact studies. Given that register-based or cohort-based studies are often done with whole population samples (ie, the USA,51, 54 Sweden,49 Denmark,50 Taiwan48), this difference was consistent with our evidence of small study effects, whereby smaller studies tended to estimate lower incidence rates. Together with the high levels of statistical heterogeneity observed in our meta-analyses, our results suggest that methodological variation might partially obscure true heterogeneity in the incidence of psychotic disorders. Nonetheless, as previously established, we found strong evidence of higher incidences of all first episode psychosis and non-affective psychotic disorders in men and ethnic minority groups, with less evidence of such differences for affective psychotic disorders.
The strength of our study is that our search strategy was inclusive and based on a previously used strategy with good reliability.18 We searched multiple databases without restriction by place or language of publication. Although individual studies might have been missed, given the size of our yield we consider it unlikely that these missing data would have substantially altered our main conclusions.
One limitation of our Article was that some citations provided incidence estimates from multiple catchment areas (notably Jongsma and colleagues, 2018),55 which we included as separate estimates in meta-analyses. We acknowledge this inclusion might have conservatively biased SEs around effect sizes. Nonetheless, it would not have affected our observation of substantial interestimate heterogeneity in incidence, which was the primary focus of our Article. Future studies should consider adopting individual-participant data approaches, which account for clustering by design.56 We used a previously published, clinician-informed algorithm to group estimates into major psychotic disorder categories.18 However, for non-affective disorders particularly, the use of this algorithm led to the categorisation of studies that used several overlapping diagnostic outcomes (appendix pp 33–34), which might have contributed to heterogeneity. Although our quality assessment tool was based on epidemiological good practice, we acknowledge it might have been skewed towards first-contact studies given it is not feasible to assess some criteria (ie, blinding) in register-based designs. Despite this, our quality assessment aided in assessing the gaps in the published literature.
The most recent systematic review and meta-analysis of all psychotic disorders19 identified substantially fewer citations (N=33) than our Article and provided no assessment or investigation of heterogeneity, despite similar inclusion criteria and time frames. The estimates of our more comprehensive review are aligned: we found a pooled estimate of non-affective disorders of 18·7 per 100 000 person-years (95% CI 14·8–23·7) and of affective disorders of 4·8 (3·3–6·9) compared with their estimates of 22·5 (16·5–28·5) for non-affective and 7·1 (1·4–12·2) for affective disorders.19 Our findings on the excess of psychoses in men were nuanced: the overall excess found in both reviews appears to be primarily driven by an excess in non-affective disorders in line with other meta-analytic evidence.27, 28
The median incidence of schizophrenia in our Article (21·7 per 100 000 person-years [IQR 5·6–52·0]) was higher than in the last major systematic review17 on this topic by McGrath and colleagues (15·2 [7·7–43·0]), with greater variation around these estimates. The only systematic review57 pertaining to mood disorders solely synthesised incidence of major depressive disorder and as such is not directly comparable to the present Article. The excess risk of (non-affective) psychotic disorders in migrants and their descendants is long-established,58 well-reported,20, 29 and covered elaborately in one publication.30
The present Article presents a varied epidemiological landscape, which partly appears to reflect methodological differences in study design. We found substantial heterogeneity both within and between study designs, with incidences of non-affective disorders, schizophrenia, and bipolar disorder higher in registry-based studies than in first contact studies. Different study designs were more common for different outcomes; for instance, a large proportion of schizophrenia studies were population registers, potentially contributing to this pooled estimate being higher than the pooled estimate of non-affective disorders (a broader category). Although individual studies36, 37 have done direct comparisons between different study designs, to our knowledge this study is the first systematic review to have investigated such differences. From a public mental health perspective, our results highlight the importance of parsing out potentially causally-relevant signals in geographical variance in incidence from noise generated through varying study designs used in different settings; individual studies16, 55, 59 that have done so suggest substantive variation in the global burden of psychotic disorders remains.
Nevertheless, more research is required to understand heterogeneity in incidence produced by different study designs. One possible explanation is that register-based studies primarily (though not exclusively) originate from Scandinavian countries, and higher incidences might indicate an association between latitude and psychotic disorders (which is well-reported, but poorly understood).31 Alternatively, although registry-based studies might ascertain new cases of psychotic disorder across an entire (usually secondary and tertiary) health-care system, not limited to contact with mental health providers, they also rely heavily on diagnoses made in clinical practice. Although such diagnoses are reliable,60 first-contact studies are often able to include standardised diagnostic assessments, which might reduce the number of false positives, leading to lower reported incidence. Small study effects are not necessarily due to publication bias41 and in our Article are consistent with the possibility of lower incidence rates reported in first contact designs; registry-based or insurance database-based studies tended to include a larger number of cases (table). However, sensitivity analyses (appendix p 32) suggest some within-type small study effects remained, which might reflect real variance between for instance urban (where a large number of cases accrue) and rural areas. In this Article, we were unable to assess effects of urbanicity, latitude, or other socioeconomic variables due to the preponderance of country-wide estimates for which no meaningful values could be assigned.
The geographical spread of studies in this Article remained mostly limited to Europe, Northern America, or Australia. One public health implication of our findings is the continued dearth of evidence outside of these settings, which might have profound consequences; for example, a cross-sectional study16 suggested the well established link between urbanicity and psychosis might not apply in LMICs. To fully understand and provide effective public mental health responses to the global burden of psychotic disorders, we will require methodologically-rigorous and culturally-appropriate epidemiological studies to delineate the incidence of psychotic disorders in a broader range of settings than has thus far been considered.
Finally, our findings also suggest that developing international guidelines for investigation of the incidence of psychotic disorders in different settings could help minimise methodological heterogeneity in the reporting of psychosis incidence across the globe.
Acknowledgments
Acknowledgments
HEJ and PBJ are funded by the National Institute of Health Research (NIHR) Collaboration of Leadership in Applied Health Research and Care, East of England. HEJ is funded by the Economic and Social Research Council (grant ES/S011714/1). JBK is funded by the Wellcome Trust (grant 101272/Z/13/Z). This work was in part supported by the University College London (UCL)Hospital NIHR Biomedical Research Centre, which provided funding to the Division of Psychiatry, UCL.
Contributors
HEJ, JBK, and PBJ conceived the project and designed the protocol. HEJ and CT carried out the database searches, screened titles, abstracts, and full texts, extracted data from citations, prepared data for analyses, and carried out statistical analyses. HEJ provided supervision to CT and prepared the manuscript. HEJ, JBK, and CT quality scored all articles. JBK carried out the database searches, screened titles, abstracts and full texts, extracted data from citations (for all studies from England published before 2011), and provided the template spreadsheet. PBJ screened abstracts. JBK and PBJ resolved conflicts regarding inclusion of articles, provided supervision to HEJ and CT, and critically revised the manuscript at all stages.
Declaration of interests
PBJ has received honoraria from Janssen and Ricordati. HEJ, CT, and JBK declare no competing interests.
Supplementary Material
References
- 1.Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry. 2017;4:295–301. doi: 10.1016/S2215-0366(17)30078-0. [DOI] [PubMed] [Google Scholar]
- 2.Hayes JF, Marston L, Walters K, King MB, Osborn DP. Mortality gap for people with bipolar disorder and schizophrenia: UK-based cohort study 2000–2014. Br J Psychiatry. 2017;211:175–181. doi: 10.1192/bjp.bp.117.202606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2017 Disease and Injury Incidence and Prevalence Collaborators Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knapp M, Mangalore R, Simon J. The global costs of schizophrenia. Schizophr Bull. 2004;30:279–293. doi: 10.1093/oxfordjournals.schbul.a007078. [DOI] [PubMed] [Google Scholar]
- 5.Anderson KK, Cheng J, Susser E, McKenzie KJ, Kurdyak P. Incidence of psychotic disorders among first-generation immigrants and refugees in Ontario. Can Med Assoc J. 2015;187:E279–E286. doi: 10.1503/cmaj.141420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kirkbride JB, Fearon P, Morgan C. Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings from the 3-center AeSOP study. Arch Gen Psychiatry. 2006;63:250–258. doi: 10.1001/archpsyc.63.3.250. [DOI] [PubMed] [Google Scholar]
- 7.Veling W, Selten JP, Veen N, Laan W, Blom JD, Hoek HW. Incidence of schizophrenia among ethnic minorities in the Netherlands: a four-year first-contact study. Schizophr Res. 2006;86:189–193. doi: 10.1016/j.schres.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 8.Leão TS, Sundquist J, Frank G, Johansson L-M, Johansson S-E, Sundquist K. Incidence of schizophrenia or other psychoses in first- and second-generation immigrants: a national cohort study. J Nerv Ment Dis. 2006;194:27–33. doi: 10.1097/01.nmd.0000195312.81334.81. [DOI] [PubMed] [Google Scholar]
- 9.Lasalvia A, Bonetto C, Tosato S. First-contact incidence of psychosis in north-eastern Italy: Influence of age, gender, immigration and socioeconomic deprivation. Br J Psychiatry. 2014;205:127–134. doi: 10.1192/bjp.bp.113.134445. [DOI] [PubMed] [Google Scholar]
- 10.Pelayo-Terán JM, Pérez-Iglesias R, Ramírez-Bonilla ML. Epidemiological factors associated with treated incidence of first-episode non-affective psychosis in Cantabria: insights from the Clinical Programme on Early Phases of Psychosis. Early Interv Psychiatry. 2008;2:178–187. doi: 10.1111/j.1751-7893.2008.00074.x. [DOI] [PubMed] [Google Scholar]
- 11.Tarricone I, Mimmi S, Paparelli A. First-episode psychosis at the West Bologna Community Mental Health Centre: results of an 8-year prospective study. Psychol Med. 2012;42:2255–2264. doi: 10.1017/S0033291712000335. [DOI] [PubMed] [Google Scholar]
- 12.Mulè A, Sideli L, Capuccio V. Low incidence of psychosis in Italy: confirmation from the first epidemiological study in Sicily. Soc Psychiatry Psychiatr Epidemiol. 2017;52:155–162. doi: 10.1007/s00127-016-1322-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Menezes P, Scazufca M. Incidence of first-contact psychosis in São Paulo, Brazil. Br J Psychiatry. 2007;191:s102–s106. doi: 10.1192/bjp.191.51.s102. [DOI] [PubMed] [Google Scholar]
- 14.Burns JK, Esterhuizen T. Poverty, inequality and the treated incidence of first-episode psychosis. An ecological study from South Africa. Soc Psychiatry Psychiatr Epidemiol. 2008;43:331–335. doi: 10.1007/s00127-008-0308-2. [DOI] [PubMed] [Google Scholar]
- 15.Morgan C, John S, Esan O. The incidence of psychoses in diverse settings, INTREPID (2): a feasibility study in India, Nigeria, and Trinidad. Psychol Med. 2016;46:1923–1933. doi: 10.1017/S0033291716000441. [DOI] [PubMed] [Google Scholar]
- 16.DeVylder JE, Kelleher I, Lalane M, Oh H, Link BG, Koyanagi A. Association of urbanicity with psychosis in low- and middle-income countries. JAMA Psychiatry. 2018;75:679–686. doi: 10.1001/jamapsychiatry.2018.0577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McGrath J, Saha S, Welham J, El Saadi O, MacCauley C, Chant D. A systematic review of the incidence of schizophrenia: the distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med. 2004;2:13. doi: 10.1186/1741-7015-2-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kirkbride JB, Errazuriz A, Croudace TJ. Incidence of schizophrenia and other psychoses in England, 1950–2009: a systematic review and meta-analyses. PLoS One. 2012;7:e31660. doi: 10.1371/journal.pone.0031660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Castillejos MC, Martín-Pérez C, Moreno-Küstner B. A systematic review and meta-analysis of the incidence of psychotic disorders: the distribution of rates and the influence of gender, urbanicity, immigration and socio-economic level. Psychol Med. 2018;22:1–15. doi: 10.1017/S0033291718000235. [DOI] [PubMed] [Google Scholar]
- 20.Bourque F, van der Ven E, Malla A. A meta-analysis of the risk for psychotic disorders among first- and second-generation immigrants. Psychol Med. 2011;41:897–910. doi: 10.1017/S0033291710001406. [DOI] [PubMed] [Google Scholar]
- 21.Stafford J, Howard R, Kirkbride JB. The incidence of very late-onset psychotic disorders: a systematic review and meta-analysis, 1960–2016. Psychol Med. 2018;48:1775–1786. doi: 10.1017/S0033291717003452. [DOI] [PubMed] [Google Scholar]
- 22.Esterberg ML, Trotman HD, Holtzman C, Compton MT, Walker EF. The impact of a family history of psychosis on age-at-onset and positive and negative symptoms of schizophrenia: a meta-analysis. Schizophr Res. 2010;120:121–130. doi: 10.1016/j.schres.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 23.Matheson SL, Shepherd AM, Pinchbeck RM, Laurens KR, Carr VJ. Childhood adversity in schizophrenia: a systematic meta-analysis. Psychol Med. 2012;43:1–13. doi: 10.1017/S0033291712000785. [DOI] [PubMed] [Google Scholar]
- 24.Moore THM, Zammit S, Lingford-Hughes A. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370:319–328. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- 25.Varese F, Smeets F, Drukker M. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vassos E, Pedersen CB, Murray RM, Collier DA, Lewis CM. Meta-analysis of the association of urbanicity with schizophrenia. Schizophr Bull. 2012;38:1118–1123. doi: 10.1093/schbul/sbs096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.van der Werf M, Hanssen M, Köhler S. Systematic review and collaborative recalculation of 133 693 incident cases of schizophrenia. Psychol Med. 2014;44:9–16. doi: 10.1017/S0033291712002796. [DOI] [PubMed] [Google Scholar]
- 28.Aleman A, Kahn RS, Selten J-P. Sex differences in the risk of schizophrenia. Arch Gen Psychiatry. 2003;60:565. doi: 10.1001/archpsyc.60.6.565. [DOI] [PubMed] [Google Scholar]
- 29.Cantor-Graae E, Selten J-P. Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry. 2005;162:12–24. doi: 10.1176/appi.ajp.162.1.12. [DOI] [PubMed] [Google Scholar]
- 30.Selten J-P, van der Ven E, Termorshuizen F. Migration and psychosis: a meta-analysis of incidence studies. Psychol Med. 2019;6:1–11. doi: 10.1017/S0033291719000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Saha S, Chant DC, Welham JL, McGrath JJ. The incidence and prevalence of schizophrenia varies with latitude. Acta Psychiatr Scand. 2006;114:36–39. doi: 10.1111/j.1600-0447.2005.00742.x. [DOI] [PubMed] [Google Scholar]
- 32.Faris R, Dunham H. The University of Chicago Press; Chicago, IL: 1939. Mental disorders in urban areas: an ecological study of schizophrenia and other psychoses. [Google Scholar]
- 33.Hare EH. Mental illness and social conditions in Bristol. J Ment Sci. 1956;102:349–357. doi: 10.1192/bjp.102.427.349. [DOI] [PubMed] [Google Scholar]
- 34.Kirkbride JB, Jones PB, Ullrich S, Coid JW. Social deprivation, inequality, and the neighborhood-level incidence of psychotic syndromes in East London. Schizophr Bull. 2014;40:169–180. doi: 10.1093/schbul/sbs151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Castillejos MC, Martín-Pérez C, Moreno-Küstner B. Incidence of psychotic disorders and its association with methodological issues. A systematic review and meta-analyses. Schizophr Res. 2018;204:458–459. doi: 10.1016/j.schres.2018.07.031. [DOI] [PubMed] [Google Scholar]
- 36.Anderson KK, Norman R, MacDougall AG. Disparities in access to early psychosis intervention services: comparison of service users and non-users in health administrative data. Can J Psychiatry. 2018;63:395–403. doi: 10.1177/0706743718762101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hogerzeil SJ, van Hemert AM, Rosendaal FR, Susser E, Hoek HW. Direct comparison of first-contact versus longitudinal register-based case finding in the same population: early evidence that the incidence of schizophrenia may be three times higher than commonly reported. Psychol Med. 2014;44:3481–3490. doi: 10.1017/S003329171400083X. [DOI] [PubMed] [Google Scholar]
- 38.Moher D, Liberati A, Tetzlaff J, Altman DG, Group TP. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.The Cochrane Collaboration . In: Cochrane Handbook for Systematic Reviews of Interventions. Higgins JP, Green S, editors. John Wiley & Sons; Chichester: 2008. [Google Scholar]
- 40.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 41.Harbord R, Harris R, Sterne J. Updated tests for small-study effects in meta-analyses. In: Sterne JA, editor. Meta-analysis in stata: an updated collection from the Stata Journal. Stata Press; College Station, TX: 2009. pp. 138–150. [Google Scholar]
- 42.StataCorp . StataCorp LP; College Station, TX: 2013. Stata Statistical Software: Release 13. [Google Scholar]
- 43.Baldwin P, Browne D, Scully PJ. Epidemiology of first-episode psychosis: illustrating the challenges across diagnostic boundaries through the cavan-monaghan study at 8 years. Schizophr Bull. 2005;31:624–638. doi: 10.1093/schbul/sbi025. [DOI] [PubMed] [Google Scholar]
- 44.Smith GN, Boydell J, Murray RM. The incidence of schizophrenia in European immigrants to Canada. Schizophr Res. 2006;87:205–211. doi: 10.1016/j.schres.2006.06.024. [DOI] [PubMed] [Google Scholar]
- 45.Farquhar F, Le Noury J, Tschinkel S, Harris M, Kurien R, Healy D. The incidence and prevalence of manic-melancholic syndromes in North West Wales: 1875–2005. Acta Psychiatr Scand. 2007;115:37–43. doi: 10.1111/j.1600-0447.2007.00961.x. [DOI] [PubMed] [Google Scholar]
- 46.Bogren M, Mattisson C, Isberg P-E, Munk-Jørgensen P, Nettelbladt P. Incidence of psychotic disorders in the 50 year follow up of the Lundby population. Aust N Z J Psychiatry. 2010;44:31–39. doi: 10.3109/00048670903393647. [DOI] [PubMed] [Google Scholar]
- 47.Goodman GP, DeZee KJ, Burks R, Waterman BR, Belmont PJ. Epidemiology of psychiatric disorders sustained by a U.S. Army brigade combat team during the Iraq War. Gen Hosp Psychiatry. 2011;33:51–57. doi: 10.1016/j.genhosppsych.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 48.Chiang C-L, Chen P-C, Huang L-Y. Time trends in first admission rates for schizophrenia and other psychotic disorders in Taiwan, 1998–2007: a 10-year population-based cohort study. Soc Psychiatry Psychiatr Epidemiol. 2017;52:163–173. doi: 10.1007/s00127-016-1326-0. [DOI] [PubMed] [Google Scholar]
- 49.Kendler KS, Ohlsson H, Mezuk B, Sundquist K, Sundquist J. A Swedish national prospective and co-relative study of school achievement at age 16, and risk for schizophrenia, other nonaffective psychosis, and bipolar illness. Schizophr Bull. 2015;42:sbv103. doi: 10.1093/schbul/sbv103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vassos E, Agerbo E, Mors O, Pedersen CB. Urban–rural differences in incidence rates of psychiatric disorders in Denmark. Br J Psychiatry. 2016;208:435–440. doi: 10.1192/bjp.bp.114.161091. [DOI] [PubMed] [Google Scholar]
- 51.Ramsey C, Dziura J, Justice AC. Incidence of mental health diagnoses in veterans of operations Iraqi freedom, enduring freedom, and new dawn. Am J Public Health. 2017;107:329–335. doi: 10.2105/AJPH.2016.303574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim W, Jang SY, Chun SY, Lee TH, Han KT, Park EC. Mortality in schizophrenia and other psychoses: data from the South Korea national health insurance cohort, 2002–2013. J Korean Med Sci. 2017;32:835–842. doi: 10.3346/jkms.2017.32.5.835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Markkula N, Lehti V, Gissler M, Suvisaari J. Incidence and prevalence of mental disorders among immigrants and native Finns: a register-based study. Soc Psychiatry Psychiatr Epidemiol. 2017;52:1523–1540. doi: 10.1007/s00127-017-1432-7. [DOI] [PubMed] [Google Scholar]
- 54.Simon GE, Coleman KJ, Yarborough BJH. First presentation with psychotic symptoms in a population-based sample. Psychiatr Serv. 2017;68:456–461. doi: 10.1176/appi.ps.201600257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jongsma HE, Gayer-Anderson C, Lasalvia A. Treated incidence of psychotic disorders in the Multinational EU-GEI Study. JAMA Psychiatry. 2018;75:36. doi: 10.1001/jamapsychiatry.2017.3554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Abo-Zaid G, Guo B, Deeks JJ. Individual participant data meta-analyses should not ignore clustering. J Clin Epidemiol. 2013;66:865–873. doi: 10.1016/j.jclinepi.2012.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Waraich P, Goldner EM, Somers JM, Hsu L. Prevalence and incidence studies of mood disorders: a systematic review of the literature. Can J Psychiatry. 2004;49:124–138. doi: 10.1177/070674370404900208. [DOI] [PubMed] [Google Scholar]
- 58.Ødegaard Ø. Emigration and insanity. Acta Psychiatr Neurol Scand. 1932;4:1–206. [Google Scholar]
- 59.Morgan C, John S, Esan O. The incidence of psychoses in diverse settings, INTREPID (2): a feasibility study in India, Nigeria, and Trinidad. Psychol Med. 2016;46:1923–1933. doi: 10.1017/S0033291716000441. [DOI] [PubMed] [Google Scholar]
- 60.Dalman C, Broms J, Cullberg J, Alleback P. Young cases of schizophrenia identified in a national inpatient register. Are the diagnoses valid? Soc Psychiatry Psychiatr Epidemiol. 2002;37:527–531. doi: 10.1007/s00127-002-0582-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.