Abstract
Background:
Shared decision making (SDM) is increasingly recognized as an important facet of patient-centered care. Despite growing interest in SDM in the emergency department (ED), little is known about emergency physicians’ (EPs’) motivations for using SDM. Understanding current patterns of SDM use and EP’s rationale for using SDM is essential for the development of interventions to increase use.
Objectives:
Recognizing the EP as an important stakeholder in SDM research, we sought to identify and explore factors that may motivate EPs’ engagement in SDM.
Methods:
In this qualitative study, informed by the Theory of Planned Behavior and Social Cognitive Theory, we conducted semistructured interviews with a purposeful sample of EPs. Interviews were recorded and transcribed verbatim. Using a directed qualitative content analysis approach, three members of the research team performed open coding of the transcripts in an iterative process, building a provisional code book as coding progressed. Respondent validation was employed to ensure methodologic rigor.
Results:
Fifteen EPs, ages 31–65, from both academic and community practice settings, were interviewed. Several had not heard of the specific phrase “shared decision making,” but all understood the concept and felt that they used SDM techniques to some degree. Most noted they had often had an agenda when they used SDM, which often motivated them to have the conversation. Agendas described included counteracting an algorithmic or defensive approach to diagnosis and treatment, avoiding harmful tests, or sharing uncertainty. All participants believed that patients benefited from SDM in terms of satisfaction, engagement, or education. Nearly all participants identified research outcomes that they felt would encourage their use of SDM (e.g., improvements in patient engagement, mitigation of risk) and many prioritized patient-centered outcomes over systems outcomes such as improved resource utilization. Little consensus was seen, however, regarding the importance of individual outcomes: of eight potential research outcomes participants endorsed, no single outcome was endorsed by even half of the physicians interviewed.
Conclusion:
Emergency physicians identified many factors that motivated them to use SDM. This study informs current research on SDM in the ED, particularly regarding the motivations of the physician-as-stakeholder.
Shared decision making (SDM) improves patient engagement and knowledge, facilitates communication, and improves resource utilization.1–7 Defined as “a collaborative process that allows patients and their providers to make health care decisions together, taking into account the best scientific evidence available, as well as the patient’s values and preferences,”8 SDM has been called the “pinnacle of patient-centered care” and promoted as an ethical imperative based on principles of patient autonomy.9,10
Despite increasing interest in the impact of SDM in the emergency department (ED),11–16 little research has focused on the emergency physician (EP) as a stakeholder in SDM research. “Stakeholders” are defined as “Individuals, organizations or communities that have a direct interest in the process and outcomes of a project, research or policy endeavor.”17 While there are many stakeholders in SDM research, including patients and families, policy-makers, and payers, EPs are possibly the most critical stakeholders regarding the translation of SDM research into clinical practice. Therefore, understanding the perspectives and needs of this group is essential. Specifically, an understanding of the factors that may contribute to an EP’s motivation to engage or not engage in SDM could help policy-makers promote SDM as well as help researchers study SDM. Additionally, the early involvement of stakeholders “helps to ensure that the research reflects the various needs of all diverse users.”18,19 Although two surveys about EPs’ views on SDM were recently published,15,20 neither study examined why EPs engage in SDM or explored factors that may encourage physicians’ use of SDM, such as attitudes, beliefs, or local practice norms. Because factors that may contribute to motivation have not previously been studied in an exploratory manner, qualitative research provides the necessary foundation for further investigation.
The purpose of this study was to explore EPs’ views on SDM in the emergency department (ED). Specifically, we sought to examine what motivated individual providers to use SDM, what benefits they perceived from the use of SDM, and what effect various research findings might have on providers’ motivation to use of SDM. These data may then inform future research seeking to study and implement SDM in the ED by identifying factors and outcomes that EPs find “motivating.”
METHODS
Study Design
This was a qualitative study utilizing semistructured interviews with practicing EPs. The study was granted exempt status by the local institutional review board, but utilized written informed consent due to recording of participants. Participants were reimbursed $25 for their time. The study was designed to comply with published standards for reporting qualitative research.21–23
Interview Guide
The initial interview guide was developed using an integrative theoretical model that combined the Theory of Planned Behavior and Social Cognitive Theory (Figure 1).24 The theoretical framework organizes the factors that potentially influence an individual’s performance of a behavior, such as initiating a SDM conversation. For example, the decision of whether or not to engage in SDM (behavior) may be influenced by the provider perceiving that they communicate well (skills and self-efficacy), that the behavior is expected of them (Norms), or that the ED is too busy to take the time (environmental constraints). We also incorporated findings from qualitative studies of non-EPs, due to the paucity of related studies with EPs.25–28 Table 1 demonstrates how the theoretical framework guided the development of the interview guide. The interview guide was piloted and was then iteratively revised during the interview process (Data Supplement S1, available as supporting information in the online version of this paper). No changes were made to the guide after the fifth interview. Since the interviews were semistructured, however, the content and questions of each interview diverged from the guide as needed during interviews. Both interviewers took field notes during interviews and discussed these notes after interviews. Interviews were designed to be 20–45 minutes long.
Figure 1.
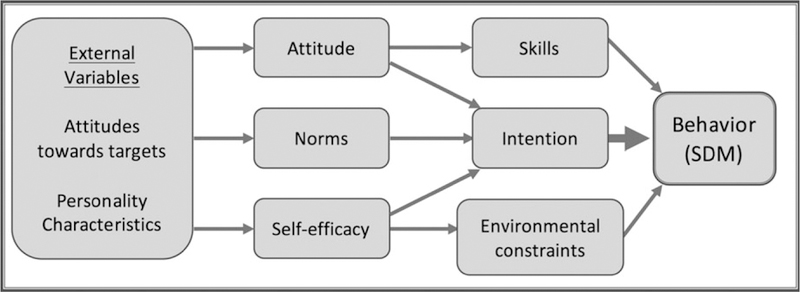
The theoretical framework (Integrative Model: Social Cognitive Theory & Theory of Planned Behavior24) demonstrating how various factors affect a behavior (shared decision making).
Table 1.
Factors Derived from the Theoretical Framework, Resultant Interview Questions, and Example Responses
| Factor | Domain/Question | Example Response |
|---|---|---|
| Intention | Facilitators: What made you decide to use SDM in that scenario? |
“it was ... that sort of almost flip of the coin decision point, and I really could have gone either way.” (Female academic EP) “often it’s where I’m going down a path I don’t want to go down ... We’re gonna get a CTA, I don’t want to get a CTA. We’re going to tube (intubate) you, I don’t want to do it. So it’s when I’m not convinced it’s the right path and so I often will present it to them.” (Male academic EP) |
| Attitude | Benefits: How do you think using SDM effects your patient encounters? |
“... you often end up doing the right thing, or doing what will make the patient understand and sort of embrace the right work up.” (Female academic EP) “I think it’s almost always appreciated. I think the patients feel understood, they feel listened to.” (Male academic EP) |
| Norms | Barrier/facilitator: Do you think your colleagues use SDM? Have you ever received training? | “I think they probably, many, most of them use shared decision making whether they call it that or not. I think there might be a few outliers that sort of feel they can decide and instruct the patient, but I think it’s being sort of widely used.” (Female academic EP) |
| Skills/self-efficacy | Barrier/facilitator: How comfortable do you feel using SDM techniques? | “I think pretty comfortable.” (Female community EP) |
| Environmental constraints | Barriers: What stands in the way of using SDM more? |
“Hallway beds.” (Male academic EP) “Time.” (Noted by nearly all EPs) |
| External variables | Facilitator: What research findings or policies would encourage you to use SDM? | “I don’t know... if [SDM] somehow increased my productivity...” (Male community/academic EP) |
We asked participants to first discuss a scenario where they needed to make a decision, how they made that decision, and who they involved in that decision-making process. We then asked participants if they were familiar with the term “shared decision making” and shared an accepted definition.8 We then asked participants to discuss scenarios where they used SDM, rather than asking directly, “what motivates you to use SDM?” This allowed further discussion of the motivators in the scenarios the participants provided. They were then asked to discuss scenarios where they could have used SDM but chose not to. Finally, they were presented with a verbal summary of the Chest Pain Choice trial as an example of SDM research in the ED2 and asked what the findings meant to them. This led into a discussion of whether various research findings (particular outcomes) were meaningful to them in a way that would potentially influence their behavior.
Study Setting, Participants, and Recruitment
A purposeful sample seeks to intentionally sample based on criteria that may be important to a particular study, under the presumption that a homogenous cohort may limit the breadth of responses.29 We chose a purposeful sample of EP physicians based on sex, years in practice since residency, region (rural/suburban vs. urban) of primary employment, academic versus community practice setting, and location of training (inside versus outside of the state). Physicians meeting these predetermined criteria were identified by convenience sampling and by utilization of networks to identify physicians likely to have different perspectives, similar to snowball sampling techniques.30 For example, professional networks were used to identify several physicians new to the region, with the expectation that they may contribute new perspectives. Physicians were initially contacted by the investigators via an e-mail asking to conduct an interview about “clinical decision making.” Initial study design planned for at least 12 interviews, with the option to conduct additional interviews if thematic saturation had not been reached.29 (Thematic saturation refers to the point where new interviews fail to generate new ideas.) Previous research has shown that 15 interviews is generally enough to reach thematic sat-uration.31
Data Collection
After agreeing to meet for an interview, participants provided written informed consent and filled out a demographics form. Interviews were conducted in person at private residences or private offices per participants’ choice. The interview team consisted of two female, practicing EPs (EMS and TRE) who trained and piloted interviews under a senior investigator with qualitative methods experiences (SLG). One interviewer served as the primary interviewer for each interview, with all but one interview having a team member present as an observer, taking notes and asking additional questions at the end. All interviews were recorded via audio recording device and transcribed. After the interviews, member checking was performed by providing participants with a short summary of the major points they discussed and asking them for their agreement, disagreements, or comments.23
Data Analysis
Transcripts were entered into Dedoose qualitative data management and analysis software (Dedoose Version 7.0.18, SocioCultural Research Consultants, LLC). Coding was performed in an iterative fashion by three research team members (EMS, ERK, KEP), all of whom had either qualitative research experience or recent training pertaining to coding. The codebook was developed using a directed approach to content analysis: that is, we combined a priori codes drawn from previous literature and our theoretical framework with emergent codes that came directly from line by line coding of the transcripts.29,32 Iterative coding was done, where transcripts were recoded as the codebook was refined. Each transcript was coded at least twice by at least two coders. We calculated agreement based on excerpt coding as well as by overall codes identified per transcript. Disagreements were discussed until consensus was reached. The codebook is available in Data Supplement S2 (available as supporting information in the online version of this paper). While the goal of the interview was to explore the physicians’ use (or lack of use) of SDM and explore the factors that motivated or discouraged their use, our analysis focuses on their intrinsic motivation and the factors that they felt encouraged them to use SDM (or would potentially encourage their use of SDM).
Research Team and Reflexivity
Qualitative inquiry attempts to recognize and reflect on the effect of the researcher on the participants and the analysis of the information gathered, particularly in an interview-based study. This concept is known as reflex-ivity.23 The research team must acknowledge the role that they may have played in introducing bias and make attempts to recognize and mitigate that bias.
The interviewers knew many, but not all, of the participants prior to the interviews. Most of the participants did not know the goals of the research prior to the interview, but the goals were stated during the semistructured interview and it was made clear that the interviewers sought honest responses (Data Supplement S1).
RESULTS
Between June 2015 and November 2015, we interviewed 15 EPs currently working in Massachusetts. One additional EP was contacted but we were unable to schedule an interview and he was not included. Theoretical saturation was reached as no distinct new codes emerged from the last three interviews.23 Participant characteristics are described in Table 2.
Table 2.
Participant Demographics
| Participant Characteristics (N = 15) | N (%) |
|---|---|
| Age (y), mean (range) | 46 (31–65) |
| Female | 6 (40) |
| Race/ethnicity | |
| White | 10 (67) |
| Black | 1 (7) |
| Asian/Indian | 2 (13) |
| Did not answer | 2 (13) |
| 100% Academic | 6 (40) |
| 100% Community | 4 (27) |
| Combined academic/community | 5 (33) |
| Years since residency, mean (range) | 13.1 (1–30) |
| Residency in emergency medicine | 13 (87) |
| Residency (training) location | |
| Regional academic hospital (one site) | 4 (27) |
| In current state of practice but not at regional training site | 3 (20) |
| Outside current state of practice | 8 (53) |
| Total different practice sites where participants had worked within past year | 14 |
In the year prior to their interview, participants worked at 14 different practice locations (both within and outside of Massachusetts), with nearly half working at more than one site. Regarding participants’ practice locations at the time of the interview, two are considered to be urban, five are considered to be suburban/ rural, with one site considered to be rural. One site is academic, two sites have some academic affiliation (occasional residents or medical students), and the others are considered to be community hospitals.
Regarding familiarity with the term “shared decisionmaking,” six participants were not familiar with the term, but once given a definition, each expressed familiarity with the concept, and every participant was able to give examples of instances when they used SDM. The types of clinical scenarios discussed are noted in Table 3; this included scenarios that were discussed in detail as well the answers to the question, “In what other scenarios do you use SDM?”
Table 3.
Scenarios Where EPs Noted Using SDM*
| Scenario | Number of Participants Who Noted This Scenario When Asked About Use of SDM (N = 15) |
|---|---|
| Admission versus discharge for chest pain at low risk for ACS | 13 |
| CT scans in general | 12 |
| CT scans for abdominal pain (diverticulitis, renal colic, “nonspecific”) | 11 |
| End-of-life scenarios | 7 |
| Pediatrics in general | 6 |
| Head CT after minor injury | 5 |
| Admission versus discharge for nonspecific neurologic complaints | 5 |
| Admission versus discharge or antibiotics versus watchful waiting for infections | 5 |
| Lumbar puncture after negative head CT for ruling out subarachnoid hemorrhage | 4 |
| Opioid prescribing | 2 |
| When patient is considering leaving AMA | 2 |
| tPA for stroke | 1 |
ACS = acute coronary syndrome; AMA = against medical advice; CT = computed tomography; SDM = shared decision-making; tPA = tissue plasminogen activator.
Scenarios were not presented, but participants were asked, “Any other scenarios where you use SDM?”
Measures of Validity
Member checking yielded only two comments from participants, clarifying thoughts but not changing the content of their codes. Intercoder agreement for excerpt coding and for total individual codes found in a transcript ranged from 60% to 90% for the second round of coding, with a mean of 75%.
Themes and Subthemes Identified, Related to Motivation
Many of the factors from the theoretical framework fell under the domains of “barriers” and “facilitators.” Because we sought to examine the attitudes of the physicians specifically in light of their position as stake-holders in SDM research, our analysis emphasized how the factors identified related to motivation. Themes and subthemes, along with representative quotations, are listed in Table 4.
Table 4.
Themes and Subthemes Related to Physicians’ Motivations, With Representative Quotations
| Theme | Subthemes | Representative Quotations |
|---|---|---|
| The Physician’s Agenda (“Intention”) | To avoid the “medicolegal” path (defensive medicine) or to avoid tests/treatments that harm |
“[I use SDM when there might be] the need for further testing in which the testing carries some risk and expense, for example an abdominal CT.” (Male academic EP) “[sometimes] we’re recommending things just to be complete and protect ourselves and do everything ... unless the patient doesn’t want everything done, and appropriately say, ‘Hey, can I go home and see if my abdominal pain gets worse instead of staying here 6 hours for a CAT scan?’ [and I would say] ‘yes, you can do that.’“ (Male community/academic EP) “[regarding low-risk chest pain patient and SDM] I don’t think they really benefit from that admission too much.” (Male community/academic EP) “What is the harm of hospitalization? There’s always a harm in hospitalization. So, when I go into these conversations, I usually for myself would feel that the harm of hospitalization outweighs the potential harm of whatever disease process they may be presenting with and therefore I personally would choose not to stay.” (Male community/academic EP) |
| To manage uncertainty |
“I use it (SDM) because I want them to be aware that although the risk is low, there is some little bit of risk there that something bad could happen to this person and family.” (Male community/academic EP) “I think the benefit of the discussion with shared decision making is to involve the other people in the room, because I want them to know that I’m actually thinking about it, because I recognize that there are certainly limitations to my intellect or skill set... that if something goes in the wrong direction then they knew that I was open to the idea that I wanted them to come back.” (Male community EP) “There is a benefit to the system. In general I think it provides decreased, in my feeling, decreased risk, so it’s a risk mitigation technique as well.” (Male academic EP) |
|
| “Guided” SDM |
“... then there’s sort of this shared decision making with some heavy advertising of my end where .. .I’ve really put a lot of emphasis on what I think is right.” (Male community EP) “In abdominal pain in a young kid ... I don’t want to really radiate the child so a little bit of shared decision making—helping them understand why I don’t want to do it, and hoping that they agree.” (Female community/academic EP) “I think in this case, because I was on the fence ... [I] didn’t lead her down one path per se. Although, I kind of talk people into one way, subtly presenting the other. I can’t really help but do that.” (Male community/academic EP) “[as part of the SDM conversation] I... try to have a PECARN [sheet] with me and hand it right to the parents ... and say “look, take this, this is why I’m doing this” and they’re like “oh, ok” so I think that helps a lot.” (Female community EP) “I’ll give options, but I’ll say that’s probably not an option you want to pursue and just mention it in passing.” (Male academic EP) |
|
| Attitudes | Toward the importance of patient satisfaction |
“I want people to be happy, I want people to feel like they got good care, that we are doing a good job.” (Male community/academic EP) “The patient comes first... and [that] they’re content with the service that is being supplied to them is paramount. You want to make sure that they feel better, but that they also, since we’re not always able to make them feel better, that they at least feel the process was appropriate and the care was appropriate and that they’re satisfied with the outcome.” (Male academic EP) [Where does patient satisfaction fit in your priorities?] “Getting the diagnosis right probably has to be first, getting teaching done ... getting through the waiting room ... They don’t have to like me, they have to just get better.” (Male academic EP) |
| Toward the importance of resource utilization |
“It [SDM] may provide some benefit to the system, the healthcare system, in the sense that I’ve had people take me up on no scans and that’s saved me a CT and labs, which also affects flow and so on and so forth.” (Male academic EP) [What external factors influence your use of SDM?] “Resources of the institution. Honestly, at [Hospital], where resources were at a premium, I engaged in SDM more (i.e. ‘Would you rather wait 6 hours for a CT or go home ... ?’)” (Male community/academic EP) |
|
| The importance of research outcomes or policy | Attitudes toward guidelines |
Pro-guidelines: “. . .having guidelines. . .there’s at least some buy-in from other providers and a practice approach where you can feel protected both medicolegally and reputation-wise.. .so consistency in the practice.” (Female community EP) Anti-guidelines: “1 think too many guidelines get in the way, personally. 1 think like we’re inundated with the guidelines. They feel more like rules than guidelines most of the time, so 1 don’t think 1 would ... that would not work for me ... Not looking for more guidelines.” (Male community/academic EP) |
| Medicolegal protection | [Interviewer: What might encourage you to use SDM more?] “... tort reform, tort reform would help me use it more .. “ (Male academic EP) |
|
| Patient satisfaction |
“ Well, if we want to keep our jobs, patient satisfaction has to be somewhat prominent, so 1 take it seriously and 1 try to treat almost all of my patients very well. But 1 think it’s part of the flaw of the American medical system that in the highly technical, complex, scientific job that we do, we’re being evaluated on patient satisfaction ... 1 find that, the whole idea, pretty offensive, but 1 play the game just like everyone else does.” (Male community/academic EP) “1 think both decreasing chest pain admissions would be a worthy outcome, and increase(ing) patient engagement or satisfaction is a very important part of it.” (Female academic EP) |
|
| Norms | SDM as part of the culture | [Interviewer: Do you think your colleagues are using SDM?] “1 think some of them would say it’s hard, 1 think there’s definitely a larger... growing percentage that seem to do it and are interested in doing it. But there is definitely a percentage that are like, ‘I’m the doctor, 1 know better’ you know, it’s not shared decision making it’s like shared convincing of my plan.” (Male community/academic EP) “I think what is more powerful is the culture of the institution ... it was a younger population, probably slightly less risk than what we have here, but at the same time that was what the institution, and kind of the population, expected ... I think it’s a lot harder to ... have the impetus to engage and kind of put yourself at risk (at a different institution).” (Male community/academic EP) |
| Patient characteristics | “If they seem open to that [alternatives] I’m much more likely to engage in that way (SDM).” (Male community/academic EP) | |
CT = computed tomography; SDM = shared decision making.
The Physician’s Agenda (“Intention”).
While the initial interview guide sought to elicit perceived benefits, facilitators, downsides, and barriers, the issue of the physician’s agenda emerged as a previously unrecognized theme. All physicians, in discussing their use of SDM, noted that although they recognized that there were two reasonable options (as some degree of clinical equipoise is necessary for SDM), and therefore presented these options to the patients, they usually had either an agenda or at least an opinion regarding which option they felt was best. This theme was noted at least once in every interview. What their agenda or opinion was, in each different scenario, helps shed light on what motivates EPs to use SDM.
Avoiding the “Medicolegal Path” or Algorithmic Care.
The physician’s agenda was often to avoid tests that harm (computed tomography [CT] scans) or treatments/admissions that were thought to have minimal benefit, but that constituted the “appropriate medicolegal care” based on the patients’ complaint. (Appropriate “medicolegal” care referring to tests and treatment that minimized medicolegal risk but involved a greater use of testing and admission than the physician thought was actually warranted.) An example of this would be using SDM to attempt to avoid a CT scan in a patient with abdominal pain and a very low likelihood of a pathologic finding or using SDM to decide on admission versus discharge in a chest pain patient at low-risk for acute coronary syndrome.
“[I use SDM when I’m thinking] this is not a path we want to go down ... but the medicolegal side says we should.” (Male academic EP)
“[When do I use SDM?] I mean CT for PE is a big one. Especially in those poor pregnant women ... I’m just like, I really don’t want to scan you, but I’m really being forced to scan you.” (Female academic EP)
“It [using SDM, avoiding algorithmic care] feels like you’re actually being a doctor as opposed to just, you know, a monkey.” (Male community/academic EP)
The Management of Uncertainty and Perceived Mitigation of Risk.
Physicians also used SDM to manage uncertainty. Physicians noted that not only was SDM a way of sharing uncertainty and possibly decreasing the risk of litigation, but also that some degree of risk tolerance (by both the physician and the patient) was necessary to have any SDM. Several noted that they believed that their risk-averse colleagues were less likely to engage in SDM, and that as they themselves had become more comfortable with uncertainty (through the progression of their careers), they engaged in SDM more often. While many participants used SDM to share uncertainty, nearly half noted that SDM may lead to “missing something” or increasing medicolegal risk. Finally, several physicians lamented the cultural intolerance of uncertainty and noted that this was a barrier to SDM.
“I don’t know if this pans out in actual data, but it feels like you’re protected from bad outcomes better if the patient feels like they had a say in that choice.” (Female academic EP)
“I hope that shared decision making is accepted by the public, and, selfishly, legally that it’s accepted ... because ... right or wrong, there has to be ... some acceptable level of risk, there has to be. If we train to 100% right, or we try to do that, it’s non-sustainable ... it probably hurts people.” (Male community/academic EP)
“Guided” SDM.
The physicians’ agenda was, at times, an outcome specific to that clinical scenario, such as avoiding a CT in minor head injury or avoiding blood tests in a young person with a viral illness. Nearly all participants described scenarios where their agenda or opinion was so strong that the conversation could be called “guided shared decision making” or possibly not “shared” decision making at all. An example of this would be a physician telling a patient with bronchitis that they are willing to give them a prescription for antibiotics, but then taking the time to explain why they don’t recommend that “option.” Most physicians noted that they only expressed options they were willing to offer, even if they believed strongly that there was a best choice for the patient. Physicians felt that this was SDM and probably improved communication and engagement, although the risk existed that the patient would make the “wrong” choice.
“Then there are other times when there’s SDM but I’ve already decided what I’m going to do—like, a football player gets his bell rung [head injury] and he comes in ... and then the SDM is kind of educating the mother on why we don’t want to fry this kid’s brain when we can clearly just observe him.” (The physician went on to explain that if the parents insisted, after the explanation, that they wanted the head CT, he would oblige, but that this rarely happened.) (Male community EP)
“[regarding low risk chest pain] ... so I’ll spin [it] in one direction or another, and if it’s a super low-risk patient then I will definitely spin it hard in the other direction. Like ‘you have no risk factors ... your pain is not suggestive of that [MI] ... we could bring you into the hospital, but I don’t really think you need to come in. If you were my brother I wouldn’t admit you to the hospital.’“ [But physician is still giving the patient the options.] (Female community EP)
Attitudes That May Affect Motivation to use SDM (“Attitudes”).
Participants expressed a multitude of differing attitudes, often in direct opposition to opinions expressed by other EPs. In light of recent research on SDM,2,20 physicians’ attitudes toward patient satisfaction and resource utilization stood out as particularly important.
Attitudes Regarding Patient Satisfaction.
Nearly all participants noted that SDM likely increases patient satisfaction. They noted that SDM probably improves communication and engagement, as well as giving patients and families a sense of control and feeling cared about.
“I think, in general, patients who like to be involved, and that’s probably the majority, appreciate it. It makes for patient satisfaction, especially when it involves family and the whole room. If you have them help to decide that a CT scan of the abdomen with PO contrast is something that should be done now, then they can’t complain about a three hour wait.” (Female academic EP)
“I think a number of patients have clearly expressed to me that they appreciate that I was giving them the information and the choice.” (Male academic EP)
Although nearly all participants felt that SDM increased patient satisfaction, the importance that physicians placed on increasing patient satisfaction as a motivator varied. Only four subjects identified patient satisfaction as a research outcome that would encourage their use of SDM, and over half of participants expressed reservations about patient satisfaction—noting that the competing priorities of a busy shift are often more important than patient satisfaction and that many factors out of the physicians’ control contribute to lower satisfaction (such as wait times).
“[regarding priorities that come before patient satisfaction] I hope everybody lives, I hope that I don’t miss anything big, I hope that I give good care, and I hope that I teach the residents how to do something well that day. The rest is gravy.” (Female academic EP)
“Patient satisfaction is secondary to appropriate medical care. This is not Applebees, you cannot have ranch/dilaudid with that and I will not supersize you to a CT scan.” (Male community EP)
Attitudes Regarding SDM as a Modality to Affect Resource Utilization.
Previous literature suggests that EPs see SDM as a viable method to decrease unnecessary testing in the ED.20 However, it is unclear whether, in the context of the competing priorities of a busy shift, improving resource utilization is important to physicians and whether it actually motivates physicians to use SDM. Our interviews suggested that while the scenarios offered by participants would often lead to improved resource utilization, improving resource utilization was only occasionally described as the primary goal, or motivator, of an SDM conversation. While several physicians noted that they attempted to be cognizant of resource utilization issues, many noted that improving resource utilization wasn’t a top priority or a motivating factor for using SDM.
[Interviewer: What are the benefits of SDM?] “I think it often saves the system... resources and ultimately money.” (Male community/academic EP)
“[The] shared decision making would be that I don’t think that we need to do ... more tests, that you’re safe to go home ... limiting the amount of testing.” (Male community EP)
“I don’t think that my primary reason not to CT scan someone (or to use SDM to potentially avoid a CT scan) is to save money for the healthcare system. I think the primary reason for me not to CT scan somebody is because it exposes them to radiation that they shouldn’t get. Having said that, I realize that my decisions of whether I put someone in the ICU or on the floor, whether I CT scan, is multiplied by everybody in the healthcare system, so those costs are huge overall, but I can say at a personal level at this point I’m not rationing my CT scans because I’m afraid that I’m gonna get a note that says I’ve scanned too many people.” (Female academic EP, explaining that her motivation for using SDM has to do with avoiding the potential harm of radiation, not decreasing CT scan use.)
“[regarding resource utilization] Not my first priority, and part of it is no one ever told you “good job” for doing any of those things [decreasing CT scans, admissions] [Interviewer: No one ever says good job on your resource utilization?] You know you get panned for not ordering the CT scan; you never get kudos for the other way around.” (Male community/academic EP, explaining that although he believes that SDM may improve resource utilization, resource utilization doesn’t motivate him to use SDM because there is no incentive to perform less testing, while missing a diagnosis has ramifications.)
Relative Importance of Research Findings and Policy on Physicians’ Motivation to Use SDM.
For this part of the interview, the Chest Pain Choice trial was used as a discussion point.2 The Chest Pain Choice trial was a randomized controlled trial of a decision support intervention to facilitate SDM regarding admission versus discharge for patients with chest pain who were thought to be low risk for acute coronary syndrome. The trial was described, and it was noted by the interviewer that admissions decreased and patient engagement and satisfaction increased. The participant was asked about the relative importance of those research outcomes in encouraging their use of SDM. Several physicians noted that improving resource utilization or patient satisfaction did encourage them to use SDM.
“It absolutely encourages me because it reinforces that what you’re spending your time doing and really kind of going out of your way [to do] in a busy shift [referring to SDM] is actually meaningful on multiple levels, right? Decreasing resource utilization, increasing patient satisfaction, all of those things are things that are becoming more and more important in healthcare today, and so, might as well do what you can.” (Female community EP)
At that point they were further asked via open-ended questions about what other research outcomes or policy changes would be important to them. Physicians were encouraged to endorse any outcome that was meaningful to them, and responses are listed in Table 5.
Table 5.
Responses to the Open-ended Question, “What Research Findings or Policy Changes Would Encourage Your Use of SDM?”*
| Research Finding or Policy | Number of Participants Endorsing (N = 15) |
|---|---|
| Decreased medicolegal risk | 5 |
| Improved resource utilization (such as decreased admissions) | 5 |
| Guidelines (would encourage use of SDM) | 5 |
| Participant expressed antiguideline sentiments | 3 |
| Increased patient satisfaction | 4 |
| Improved patient engagement/empowerment | 4 |
| Decreased or equivalent morbidity or mortality (e.g., missed MIs) | 4 |
| Decreased iatrogenic side effects of interventions | 1 |
| Improved patient flow or productivity | 2 |
| Research findings would not influence participant’s use of SDM | 1 |
MI = myocardial infarction; SDM = shared decision making.
Participants gave more than one answer each.
“So depending on the type of illness, number one should be mortality. Number two ... I would look at things like iatrogenic injuries because a lot of the extra tests do have potential risks.” (Male academic EP)
Several physicians mentioned that guidelines would be helpful or encourage them, but others noted that they were not interested in more guidelines.
“I really like hospital guidelines, especially if they’re done well where they don’t limit me, yet they give me kind of a something to stand on ... give me protection for what I think is right even though there is a small amount of risk involved in doing it.” (Male community/academic EP)
“There’s no guidelines that I really care about in this regard. I care about scientific studies and guidelines when it comes to the technical aspects of care, but for the social aspects of care, it’s completely irrelevant to me. And I’m sorry ‘cause that’s probably what this study is all about.” (Male community/academic EP)
Most notably, no single outcome was endorsed as important by even half the participants.
Themes Less Likely to Play a Role in Motivation
Based on our theoretical framework, a number of variables could have played a role in motivating physicians, but were not heavily endorsed as motivating by the participants. Examples include norms, skills, self-efficacy, patient characteristics, and physician personality characteristics. For example, while a few participants noted that SDM was more “part of the culture” in some settings they had worked in, none noted that their colleagues’ use of SDM influenced their own use (“Norms,” Figure 1). Similarly, almost all participants reported that they were “comfortable” doing SDM with their patients, but this did not seem to play a role in their motivation (“Skills,” Figure 1). While physicians did bring up patient characteristics that were barriers to SDM, only one patient characteristic—”patient asks about alternatives”—was noted by a participant to stimulate SDM. Finally, physicians noted personality characteristics in their colleagues that they associated with increased or decreased use of SDM, but rarely identified these characteristics in themselves as playing a role in their decision to engage in SDM.
DISCUSSION
This is the first study to qualitatively explore EPs’ attitudes and motivations regarding SDM. We noted that physicians often initiate SDM because of a conscious agenda, but that these agendas vary widely by clinical scenario. Physicians’ agendas included avoiding CT scans, sharing and mitigating uncertainty, avoiding admissions with questionable benefits, and avoiding aggressive end-of-life care. The subtext to these goals was often that the “standard of care” (or the pathway felt to have the least medicolegal risk) was in direct opposition to what the physician felt was best for that particular patient, so rather than unilaterally diverging from the standard of care, the physician used SDM to explain the situation and obtain input from the patient regarding their values, preferences, and often risk tolerance.
In some aspects, our results are aligned with the results of recent survey studies. Kanzaria et al.20 reported that most EPs felt that SDM may be a useful modality to decrease “unnecessary” testing. Our participants often noted that using SDM in scenarios that would lead to improved resource utilization or decreases in testing, but this was only occasionally the motivator for the conversation. Probst et al.15 asked physicians whether certain scenarios were appropriate for SDM, and the list generated has overlap with our participants’ usage patterns, shown in Table 2. However, in our study, a large minority of participants were not familiar with the term “shared decision making.” This has implications for the interpretation of previous surveys regarding the likelihood of social desirability influencing results, and it has implications for researchers and policy-makers looking to study or promote SDM.
Our study is the first study to examine the motivations for the use of SDM in the ED. We noted several themes that were important to EPs: SDM to avoid “standard” or algorithmic care when this care was not perceived as right for the patient; SDM to share or mitigate uncertainty; SDM to improve communication, patient satisfaction and engagement, and resource utilization; and SDM to guide the patient to the “best” option (“guided” SDM) while still allowing them input or dissent. Further study of the needs of the physician-as-stakeholder should investigate which research outcomes (i.e., morbidity, patient satisfaction, resource utilization) are most important in particular scenarios as well as quantify the relative importance of these outcomes in a larger and more representative population of practicing clinicians. Additionally, hospital-based interventions could target the areas that clinicians deem most important, for example, supporting SDM as standard of care in particular clinical scenarios.
The lack of consensus regarding the importance of any one possible research study outcome is notable and has ramifications for researchers and policy-makers. It is possible that even with larger studies there will not be consensus between clinicians regarding the importance of any one research outcome and that studies will need to have multiple outcomes to effectively encourage clinicians’ use of SDM in the ED. Because of this lack of consensus, individual efforts to promote or study SDM should involve EPs early, at the Evidence Prioritization stage of research, to further delineate these motivations in the context of any specific SDM scenario.19
In theory, physicians should partake in SDM out of respect for patient autonomy. In reality, physicians balance patient autonomy, stewardship of resources, and fear of uncertainty with every medical decision. The challenge of the next phase of SDM research will be to establish measurable outcomes that are meaningful to clinicians and patients while helping physicians navigate this balancing act.
STRENGTHS AND LIMITATIONS
One of the strengths of semistructured interviews is that participants are not given options, such as in a survey, that might bias their answers. In this respect, qualitative inquiry may result in both more honest responses and a wider breadth of responses than a survey. Additionally, although all the EPs included were practicing in the same region of the United States, we sampled physicians from a wide variety of practice settings and training backgrounds, further increasing the breadth of our responses.
Regarding limitations, qualitative inquiry is intended to be hypothesis generating, not hypothesis testing, hence no specific hypothesis was specified a priori. Also, it is possible that physicians outside our region would have answered these questions differently, leading to different themes and concepts. We did not include perceived barriers in this analysis, to more deeply examine the aforementioned themes. Finally, while our research team, including interviewers and coders, attempted to remain unbiased, preexisting assumptions as well as social desirability bias may have influenced data collection and interpretation. We are optimistic that via rigorous examination of the transcripts and fidelity to the emerging codes, we were able to recognize the effects of our own biases.
CONCLUSIONS
All physicians interviewed were able to give examples of when they use shared decision making and why, reflecting the acceptance of some degree of patient involvement in medical decision making in the ED. Sharing uncertainty and avoiding tests and interventions with minimal benefit or possible harm was noted to motivate many physicians, and while resource utilization and patient satisfaction were both felt to be benefits of SDM, neither played a large role in motivating a majority of physicians. Most participants were able to identify research outcomes that would be meaningful to them, but none of the eight outcomes mentioned were endorsed by even half of the cohort. The foundation gained from this inquiry can help researchers and policy-makers further involve physicians-as-stakeholders in the study and promotion of shared decision making.
Supplementary Material
Data Supplement S1. Semi-structured interview guide.
Data Supplement S2. Master codebook.
Acknowledgments
This study was funded by a grant from AHRQ: 1R03HS024311–01. Also, the project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health (NIH), award number UL1TR001064. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
The authors have no potential conflicts to disclose.
Supporting Information
The following supporting information is available in the online version of this paper:
References
- 1.Trikalinos TA, Wieland LS, Adam GP, Zgodic A, Ntzani EE. Decision Aids for Cancer Screening and Treatment. Comparative Effectiveness Review No. 145. AHRQ Publication No. 15-EHC002-EF. Rockville, MD: Agency for Healthcare Research and Quality, 2014. Dec. [PubMed] [Google Scholar]
- 2.Hess EP, Knoedler MA, Shah ND, et al. The chest pain choice decision aid: a randomized trial. Circ Cardiovasc Qual Outcomes 2012;5:251–9. [DOI] [PubMed] [Google Scholar]
- 3.Oshima Lee E, Emanuel EJ. Shared decision making to improve care and reduce costs. N Engl J Med 2013;368:6–8. [DOI] [PubMed] [Google Scholar]
- 4.Durand M-A, Carpenter L, Dolan H, et al. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PLoS One 2014;9:e94670–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davidson L Bending the Curve: Technical Documentation. The Lewin Group; 2008:1–108. Available at: http://www.lewin.com/content/dam/Lewin/Resources/Site_Sections/Publications/3888.pdf. Accessed Jan 15, 2015. [Google Scholar]
- 6.Wilson SR, Strub P, Buist AS, et al. Shared treatment decision making improves adherence and out-comes in poorly controlled asthma. Am J Respir Crit Care Med 2010;181:566–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Veroff D, Marr A, Wennberg DE. Enhanced support for shared decision making reduced costs of care for patients with preference-sensitive conditions. Health Aff (Millwood) 2013;32:285–93. [DOI] [PubMed] [Google Scholar]
- 8.Healthwise, Inc. Why Shared Decision Making? Available at: http://www.informedmedicaldecisions.org/what-is-shared-decision-making/. Accessed April 3, 2016.
- 9.Barry MJ, Edgman-Levitan S. Shared decision making-pinnacle of patient-centered care. N Engl J Med 2012;366:780–1. [DOI] [PubMed] [Google Scholar]
- 10.Elwyn G, Tilburt J, Montori V. The ethical imperative for shared decision-making. Eur J Person Centered Healthcare 2013;1:129–31. [Google Scholar]
- 11.Griffey RT, Shah MN. What we talk about when we talk about SDM. Acad Emerg Med 2016;23:493–4. [DOI] [PubMed] [Google Scholar]
- 12.Flynn D, Knoedler MA, Hess EP, et al. Engaging patients in health care decisions in the emergency department through shared decision-making: a systematic review. Acad Emerg Med 2012;19:959–67. [DOI] [PubMed] [Google Scholar]
- 13.Hess EP, Grudzen CR, Thomson R, Raja AS, Carpenter CR. Shared decision-making in the emergency department: respecting patient autonomy when seconds count. Acad Emerg Med 2015;22:856–64. [DOI] [PubMed] [Google Scholar]
- 14.Hess EP, Wyatt KD, Kharbanda AB, et al. Effectiveness of the head CT choice decision aid in parents of children with minor head trauma: study protocol for a multicenter randomized trial. 2014;15:253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Probst MA, Kanzaria HK, Frosch DL, et al. Perceived appropriateness of shared decision-making in the emergency department: a survey study. Acad Emerg Med 2016;23:375–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anderson RT, Montori VM, Shah ND, et al. Effectiveness of the Chest Pain Choice decision aid in emergency department patients with low-risk chest pain: study protocol for a multicenter randomized trial. 2014;15:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Deverka PA, Lavallee DC, Desai PJ, et al. Stakeholder participation in comparative effectiveness research: defining a framework for effective engagement. J Comp Eff Res 2012;1:181–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agency for Healthcare Research and Quality. Resources for Getting Involved and Involving Others. Module I: Text Version. Available at: http://effectivehealthcare.ahrq.gov/index.cfm/tools-and-resources/how-to-get-involved-in-the-effective-health-care-program/module-i/. Accessed April 3, 2016.
- 19.Concannon TW, Meissner P, Grunbaum JA, et al. A new taxonomy for stakeholder engagement in patient-centered outcomes research. J Gen Intern Med 2012;27:985–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kanzaria HK, Brook RH, Probst MA, Harris D, Berry SH, Hoffman JR. Emergency physician perceptions of shared decision-making. Acad Emerg Med 2015;22:399–405. [DOI] [PubMed] [Google Scholar]
- 21.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 2007;19:349–57. [DOI] [PubMed] [Google Scholar]
- 22.O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research. Acad Med 2014;89:1245–51. [DOI] [PubMed] [Google Scholar]
- 23.Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. Los Angeles, CA: Sage Publications, 2014. [Google Scholar]
- 24.National Cancer Institute. Theory at a Glance - A Guide for Health Promotion Practice (Second Edition). 2005, NIH Publication No. 05–3896; Available at: http://sbccimplementationkits.org/demandrmnch/ikitresources/theory-at-a-glance-a-guide-for-health-promotion-practice-second-edition/. Accessed Aug 26, 2014. [Google Scholar]
- 25.Pollard S, Bansback N, Bryan S. Physician attitudes toward shared decision making: a systematic review. Patient Educ Couns 2015:1–12. [DOI] [PubMed] [Google Scholar]
- 26.Zeuner R, Frosch DL, Kuzemchak MD, Politi MC. Physicians’ perceptions of shared decision-making behaviours: a qualitative study demonstrating the continued chasm between aspirations and clinical practice. Health Expect 2014;18:2465–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tiedje K, Shippee ND, Johnson AM, et al. ‘They leave at least believing they had a part in the discussion’: understanding decision aid use and patient-clinician decision-making through qualitative research. Patient Educ Couns 2013;93:86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stevenson FA. General practitioners’ views on shared decision making: a qualitative analysis. Patient Educ Couns 2003;50:291–3. [DOI] [PubMed] [Google Scholar]
- 29.Miles MB, Huberman AM, Saldana J. Qualitative Data Analysis: A Methods Sourcebook. (Edition 3). Los Angeles: Sage Publications, 2013. [Google Scholar]
- 30.Creswell JW. Qualitative Inquiry & Research Design: Choosing Among Five Approaches. Los Angeles, CA: Sage Publications, 2013:156–158. [Google Scholar]
- 31.Guest G, Bunce A, Johnson L. How many interviews are enough?: an experiment with data saturation and variability. Field Methods 2006;18:59. [Google Scholar]
- 32.Hsieh HF. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Supplement S1. Semi-structured interview guide.
Data Supplement S2. Master codebook.


