Abstract
Introduction
New generation biologics, including interleukin (IL)-17 and IL-23 inhibitors, have delivered higher rates of skin clearance than older treatments in head-to-head studies. However, studies comparing these new biologics directly to one another are limited.
Objectives
To compare the short-term efficacy of available (or imminently available) biologic and non-biologic systemic therapies for treating patients with moderate-to-severe plaque psoriasis.
Methods
A systematic review was undertaken to identify randomised controlled trials evaluating biologic treatments, apremilast and dimethyl fumarate. MEDLINE, MEDLINE In-Process, Embase and the Cochrane Library were searched from the 1st January 2000 to 22nd November 2018. A Bayesian network meta-analysis (NMA) using a random-effects multinomial likelihood model with probit link and meta-regression to adjust for cross-trial variation in placebo responses compared the efficacy of interventions at inducing different levels of Psoriasis Area and Severity Index (PASI) response during the induction period. A range of sensitivity analyses was undertaken.
Results
Seventy-seven trials (34,816 patients) were included in the NMA. The base-case analysis showed that all active treatments were superior to placebo. IL-17 inhibitors, guselkumab and risankizumab were found to be more efficacious than tildrakizumab, ustekinumab, all TNF inhibitors and non-biologic systemic treatments at inducing all levels of PASI response. In addition, brodalumab, ixekizumab and risankizumab were significantly more efficacious than secukinumab; no significant difference was found in the comparison with guselkumab. The greatest benefit of brodalumab, ixekizumab, guselkumab, and risankizumab was seen for PASI 90 and PASI 100 response. Results were consistent across all analyses.
Conclusions
In the NMA brodalumab, ixekizumab, risankizumab and guselkumab showed the highest levels of short-term efficacy. There were differences in efficacy between treatments within the same class. Longer-term analyses are needed to understand differences between these drugs beyond induction in what is a life-long condition.
Introduction
Psoriasis is a chronic, immune‐mediated skin disease which affects approximately 100 million people worldwide [1]. It is estimated that in most developed countries between 1.5 and 5% of the population suffer from psoriasis, with the incidence highest in people in their twenties, thirties and sixties [2]. It affects men and women of all ages, although it is rare in children. The most common type is plaque psoriasis (psoriasis vulgaris), characterized by patches of erythema covered in plaques that can range in colour from silvery-white to yellow [3]. Approximately 20% of patients have moderate-to-severe disease [4, 5]. Psoriasis may affect patient’s self-esteem and lead to low quality of life, comparable to that of patients with heart disease or diabetes [6–10]. Many factors must be considered when selecting the best treatment for patients with plaque psoriasis.
Biologic therapies are generally licensed for treatment of patients eligible for systemic therapy; however, in practice they may be considered after other therapies have failed. For example, in the UK initial management of such patients may involve conventional systemic therapies such as methotrexate, cyclosporine, or acitretin [11]. Only patients with moderate-to-severe plaque psoriasis who do not respond to, or are intolerant of conventional systemic treatments are offered biologic systemic therapies, the phosphodiesterase 4 (PDE4) inhibitor apremilast or dimethyl fumarate (DMF) [4, 12–14]. In other countries, modern biologics may be prescribed earlier in the treatment pathway.
The first biologics used in psoriasis were anti-tumour necrosis factor (TNF) therapies, adalimumab, etanercept and infliximab [15]. Although their introduction transformed the treatment of the disease [16], in the majority of patients they do not provide complete skin clearance [17]. In addition, it is common for patients to discontinue anti-TNF treatment due to loss of response and adverse effects [18–20]. In 2009, the biologic therapy ustekinumab, which targets the interleukin (IL)-12/23 pathway, became available [21].
More recently, biologics targeting the IL-17 pathway have been introduced into clinical practice. The three approved IL-17 pathway inhibitors are secukinumab and ixekizumab, both IL-17A inhibitors, and brodalumab, which targets the IL-17-receptor A (IL-17RA) [22]. These treatments have been shown to be efficacious and safe and offer higher rates of complete or almost complete clearance compared to TNF inhibitors and ustekinumab [23–25]. Another class of systemic drugs potentially offering similarly high complete clearance rates target IL-23. These include guselkumab, tildrakizumab, and risankizumab [26–29]. Although data from clinical trials has shown these treatments to be more efficacious than anti-TNFs and ustekinumab [30–36], clinical trial data on their benefit compared to the more established IL-17 inhibitors is very limited [37, 38]. Rapid developments in the field of psoriasis treatments necessitate assessment of the efficacy of new drugs relative to older treatments and different drug classes.
The aim of this systematic review (SR) and network meta-analysis (NMA) was therefore, to compare the efficacy of IL-17 targeted drugs (brodalumab, ixekizumab, and secukinumab) to new IL-23 targeted treatments (guselkumab, risankizumab, and tildrakizumab), as well as other systemic biologic and non-biologic therapies using the latest evidence. Psoriasis Area and Severity Index (PASI) response was chosen as the measure of efficacy, as it captures both the severity and extent of psoriatic lesions. The PASI score is measured on a scale from 0 to 72 and response to treatment is often measured in terms of percentage decrease in the PASI score, with values of 50%, 75%, 90% and 100% usually reported in trials [39, 40].
Materials and methods
The SR was carried out in accordance with a protocol developed prior to commencement of the review (details reported in S1 Text).
Search strategy
Electronic databases (MEDLINE, MEDLINE In-Process, Embase and the Cochrane Library) were searched from the 1st January 2000 to 22nd November 2018 for articles published in English. Search terms included index and text terms for psoriasis, relevant interventions and study design. The full search strategies can be found in S1 Table. In addition, reference lists of included studies and any relevant systematic reviews or NMAs identified during title and abstract screening were scanned to identify further studies. Disease-specific and health economics and outcomes research conferences were also searched.
Study selection
All articles identified in the electronic searches were added to an EndNote database and duplicates removed. Titles, abstracts and potentially relevant full texts of articles were assessed for inclusion by one reviewer, with another reviewer performing a 50% check at both stages. Discrepancies were resolved by discussion or, if necessary, by a third reviewer.
Randomised controlled trials (RCTs) in adult patients with moderate-to-severe chronic plaque psoriasis were included in the review. Interventions of interest included licensed doses of IL-17 inhibitors (brodalumab, secukinumab and ixekizumab), IL-23 inhibitors (tildrakizumab, guselkumab and risankizumab), IL-12/23 inhibitor ustekinumab, anti-TNF therapies (infliximab, etanercept, certolizumab pegol and adalimumab), PDE4 inhibitor apremilast and fumaric acid ester (FAE) dimethyl fumarate (DMF). Comparators included all interventions of interest, as well as placebo and unlicensed doses of biological and non-biological therapies. Biosimilar versions of drugs were considered as part of the evidence base for the originator drug. The outcome of interest was the proportion of patients achieving 50, 75, 90 and 100% improvement in their PASI score at the end of the induction period. Only articles published in English were considered eligible. A full set of inclusion and exclusion criteria can be found in S2 Table.
Data extraction and quality assessment
Details of the study design, baseline patient characteristics, interventions, outcomes, timepoints and results were extracted by one reviewer and checked by another. Additional data from study investigators were not sought. The methodological quality of included studies was assessed by one independent reviewer and checked by another using the concise critical appraisal checklists in the National Institute for Health and Care Excellence (NICE) Single Technology Appraisal user guide [41].
Network meta-analysis of PASI response
A hierarchical Bayesian NMA was used to combine results of all relevant studies allowing for all data from direct and indirect comparisons to be synthesised into a single set of effect sizes. The methods followed the recommended best practice for evidence synthesis [42].
The outcome of interest was the proportion of patients achieving each level of PASI response (PASI 50, PASI 75, PASI 90 and PASI 100) at the end of the induction phase (between 10 and 16 weeks). Data were analysed using an ordered probit model designed to estimate probabilities of achieving each level of PASI response [42]. PASI 50 responses in placebo arms of the included studies were utilised to inform the baseline event rates [43]. PASI response was modelled as a discrete dependent variable that takes ordered multinomial outcomes (PASI 50, PASI 75, PASI 90 and PASI 100). Cross-trial variation in placebo response rates has been observed in psoriasis [44] and is an indicator of between-study heterogeneity, which can introduce bias to synthesised comparisons of treatment outcomes [45–47]. Randomised trials in moderate-to-severe psoriasis vary by design, eligibility criteria, time to primary endpoint and concomitant emollient use, all of which could contribute to differences in placebo responses and consequently to relative effect sizes. Adjusting for differences in the placebo arms may account for heterogeneity between trials and could improve the model fit [42, 48–50]. This approach has previously been used in other NMAs comparing the efficacy of biological treatments for moderate-to-severe psoriasis [38, 51] and has been recommended by NICE in recognition of the variability in placebo response across trials [52]. Analyses adjusting and not adjusting for cross-trial variation in placebo-arm responses were carried out using random-effects assumptions and assessed for their goodness of fit. In accordance with NMA guidelines [49], fit was informed by the statistical significance of the regression coefficient and whether there was a reduction in between-trial heterogeneity. The model with the best fit was used to draw conclusions. Inconsistency between the direct and indirect evidence was assessed using a random-effects unrelated mean effects model [53]. Full details of the model used are shown in S2 Text.
WinBUGS version 1.4 [54] was used to perform all statistical analyses, using non-informative priors. After an initial burn-in of at least 20,000 simulations, convergence was confirmed through visual inspection the Brook-Gelman-Rubin diagnostic and history plots. Sampled parameters were then estimated using 20,000 simulations on three chains. Results were calculated as the absolute probabilities of response for each treatment and as risk ratios (RRs) for every pairwise comparison at each level of PASI response. Point estimates reflecting the median value are presented, along with 95% credible intervals (95% CrI), reflecting the range of true effects with 95% probability. Sensitivity analyses were performed to test the impact of excluding trials reporting <5% biologic exposed patients, using a different timepoint (12 weeks rather than 16 weeks) for secukinumab, and excluding studies with fewer than 50 patients per arm. PASI data inputs are reported in S3 Table.
Results
Identification of trials
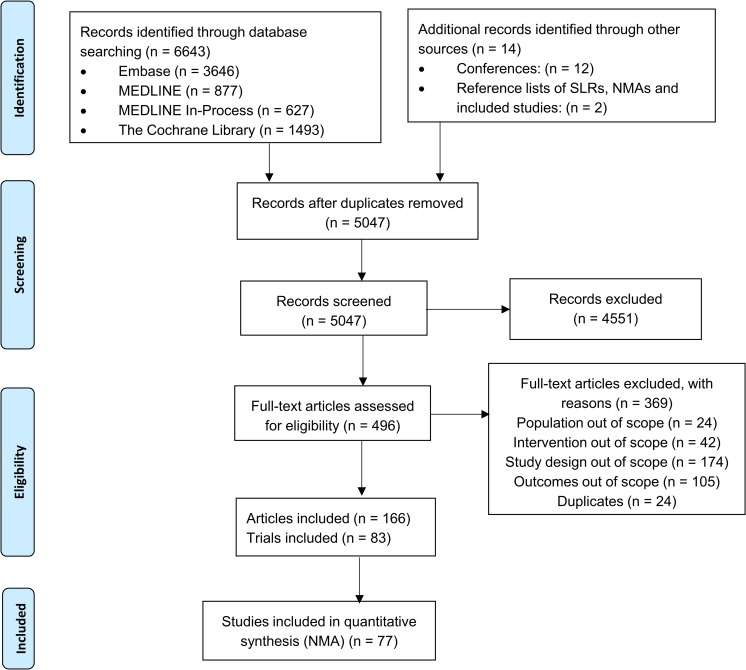
As shown in Fig 1, electronic database searches identified 6643 articles. A further fourteen were identified through searching conferences and reference lists of included studies, SRs and NMAs. After the removal of duplicates, 5047 titles and abstracts were screened, and subsequently 496 full texts were assessed for eligibility. Three-hundred and sixty-nine full text articles were excluded based on the population (n = 24), intervention (n = 42), study design (n = 174), outcomes (n = 105) and as duplicates (n = 24). References of excluded studies can be found in S4 Table. Eighty-three RCTs (reported in 127 articles) were included in the SR and 77 (including 34,816 patients) in the NMA. The trials not included in the NMA did not provide results at all [55–57] or in an appropriate format [58], or included a comparator that would not connect relevant interventions in the network [59, 60].
Fig 1. PRISMA flow diagram.
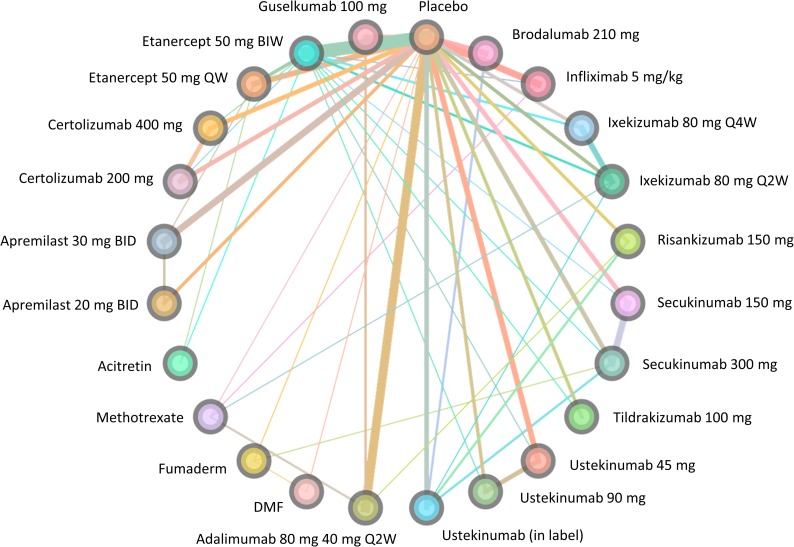
Fig 2 displays the evidence network for the analysis of the included trials. Data were available on all interventions of interest.
Fig 2. Network diagram for the base-case analysis.
Study and patient characteristics
The main details of trials included in the NMA are summarised in Table 1. Patient eligibility criteria in the included studies were largely consistent, with most requiring patients to have baseline BSA ≥ 10% and PASI score of ≥ 10 or ≥ 12. However, three trials [60–63] only required a minimum BSA of 5%.
Table 1. Characteristics of trials included in the NMA.
| Study | Study design | Interventions and comparator(s) (n) | Baseline characteristics | ||||||
|---|---|---|---|---|---|---|---|---|---|
| PASI outcomes reported | Primary endpoint (weeks) | Main inclusion criteria | Disease duration in years: mean (SD/ range*) | PsA (%) | Age in years: mean (SD/ range*) | Male (%) | % prior systemic therapy: conventional/ biologic | ||
| AMAGINE-1 [64] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 220) | 21 (12) | 29 | 47 (13) | 73 | 75/46 |
| Brodalumab 140 mg (n = 219) | 19 (13) | 27 | 46 (13) | 74 | 65/45 | ||||
| Brodalumab 210mg (n = 222) | 20 (13) | 26 | 46 (12) | 73 | 70/47 | ||||
| AMAGINE-2 [65] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 309) | 18 (12) | 17 | 44 (13) | 71 | 74/29 |
| Brodalumab 140 mg (n = 610) | 19 (12) | 21 | 45 (13) | 68 | 77/29 | ||||
| Brodalumab 210 mg (n = 612) | 19 (12) | 19 | 45 (13) | 69 | 77/29 | ||||
| Ustekinumab in-label (n = 300) | 19 (13) | 17 | 45 (13) | 68 | 75/28 | ||||
| AMAGINE-3 [65] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 315) | 18 (12) | 19 | 44 (13) | 66 | 65/24 |
| Brodalumab 140 mg (n = 629) | 17 (12) | 21 | 45 (13) | 70 | 70/25 | ||||
| Brodalumab 210 mg (n = 624) | 18 (12) | 20 | 45 (13) | 69 | 68/25 | ||||
| Ustekinumab in-label (n = 313) | 18 (12) | 20 | 45 (13) | 68 | 70/24 | ||||
| Nakagawa 2016 [66] | 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 38) | 17 (11) | 18 | 47 (11) | 71 | NR/8 |
| Brodalumab 140 mg (n = 37) | 15 (10) | 16 | 46 (13) | 81 | NR/8 | ||||
| Brodalumab 210 mg (n = 37) | 15 (11) | 14 | 46 (12) | 78 | NR/14 | ||||
| Papp 2012 [22] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 38) | 18 (12) | 18 | 42 (14) | 58 | 24/35 |
| Brodalumab 140 mg (n = 39) | 19 (10) | 28 | 44 (12) | 72 | 41/35 | ||||
| Brodalumab 210 mg (n = 40) | 17 (10) | 30 | 42 (12) | 62 | 40/35 | ||||
| UNCOVER-1 [67] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 431) | NR (NR) | NR | 46 (13) | 70 | 52/42 |
| Ixekizumab 80mg Q4W (n = 432) | NR (NR) | NR | 46 (13) | 67 | 49/39 | ||||
| Ixekizumab 80mg Q2W (n = 433) | NR (NR) | NR | 45 (12) | 67 | 57/40 | ||||
| UNCOVER-2 [68] | 75, 90, 100 | 12 | PASI ≥10, BSA ≥10% | Placebo (n = 168) | 19 (13) | NR | 45 (12) | 71 | 48/26 |
| Etanercept 50mg BIW (n = 358) | 19 (12) | NR | 45 (13) | 66 | 48/21 | ||||
| Ixekizumab 80mg Q4W (n = 347) | 19 (13) | NR | 45 (14) | 70 | 51/25 | ||||
| Ixekizumab 80mg Q2W (n = 351) | 18 (12) | NR | 45 (13) | 63 | 51/24 | ||||
| UNCOVER-3 [68] | 75, 90, 100 | 12 | PASI ≥10, BSA ≥10% | Placebo (n = 193) | 18 (13) | NR | 46 (12) | 71 | 43/17 |
| Etanercept 50mg BIW (n = 382) | 18 (12) | NR | 46 (14) | 70 | 48/16 | ||||
| Ixekizumab 80mg Q4W (n = 386) | 18 (12) | NR | 46 (13) | 67 | 47/15 | ||||
| Ixekizumab 80mg Q2W (n = 385) | 18 (12) | NR | 46 (13) | 66 | 44/15 | ||||
| IXORA-S [69, 70] | 75, 90, 100 | 12 | PASI ≥10, BSA ≥NR | Ixekizumab 80 mg Q2W (n = 136) | 18 (11) | NR | 43 (13) | 66 | 93/13 |
| Ustekinumab (45 mg if <100 kg; 90 mg if >100 kg) (n = 166) | 18 (12) | NR | 44 (13) | 68 | 92/15 | ||||
| Reich 2017 [71] | 75, 90, 100 | 12 | PASI ≥NR BSA ≥NR |
Ixekizumab 80 mg Q2W (n = 54) | NR (NR) | NR | NR (NR) | NR | 0/0 |
| Methotrexate (n = 54) | NR (NR) | NR | NR (NR) | NR | 0/0 | ||||
| IXORA-P [72] | 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Ixekizumab 80mg Q4W (n = 310) | 19 (12) | 19 | 47 (14) | 64 | 47/47 |
| Ixekizumab 80mg Q2W (n = 611) | 20 (13) | 16 | 49 (14) | 67 | 48/49 | ||||
| Khattri 2018 [73] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Ixekizumab 80mg Q4W (n = 6) | 22 (23) | NR | 55 (7) | 50 | NR/NR |
| Ixekizumab 80mg Q2W (n = 6) | 17 (13) | NR | 42 (13) | 83 | NR/NR | ||||
| FEATURE [74] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 59) | 20 (14) | NR | 47 (14) | 66 | 49/44 |
| Secukinumab 150mg (n = 59) | 20 (13) | NR | 46 (15) | 68 | 66/48 | ||||
| Secukinumab 300mg (n = 59) | 18 (12) | NR | 45 (13) | 64 | 34/39 | ||||
| ERASURE [75] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 248) | 17 (12) | 27 | 45 (13) | 69 | 44/29 |
| Secukinumab 150mg (n = 245) | 18 (12) | 19 | 45 (13) | 69 | 51/30 | ||||
| Secukinumab 300mg (n = 245) | 17 (11) | 23 | 45 (14) | 69 | 52/29 | ||||
| FIXTURE [75] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 326) | 17 (12) | 15 | 44 (13) | 73 | 61/11 |
| Etanercept 50mg BIW (n = 326) | 16 (12) | 14 | 44 (13) | 71 | 63/14 | ||||
| Secukinumab 150mg (n = 327) | 17 (12) | 15 | 45 (13) | 72 | 61/14 | ||||
| Secukinumab 300mg (n = 327) | 16 (12) | 15 | 45 (13) | 69 | 60/12 | ||||
| JUNCTURE [76] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 61) | 20 (12) | 20 | 44 (13) | 62 | 48/21 |
| Secukinumab 150mg (n = 61) | 21 (15) | 26 | 44 (14) | 67 | 51/25 | ||||
| Secukinumab 300mg (n = 60) | 21 (14) | 23 | 47 (14) | 77 | 50/25 | ||||
| SCULPTURE [77] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Secukinumab 150mg (n = 482) | 17 (13) | 22 | 45 (13) | 63 | NR/27 |
| Secukinumab 300mg (n = 484) | 17 (13) | 19 | 47 (13) | 69 | NR/29 | ||||
| CLEAR [78] | 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Secukinumab 300mg (n = 337) | 20 (13) | 21 | 45 (14) | 68 | 65/14 |
| Ustekinumab (45 mg if <100 kg; 90 mg if >100 kg) (n = 339) | 16 (11) | 16 | 45 (14) | 74 | 66/13 | ||||
| PRIME [79, 80] | 50, 75, 90, 100 | 24 | PASI ≥10, BSA ≥10% | Secukinumab 300mg (n = 105) | 16 (13) | 4 | 43 (14) | 62 | 0/0 |
| Fumaderm (n = 97) | 17 (13) | 8 | 47 (13) | 62 | 0/0 | ||||
| SIGNATURE [81] |
75, 90 | 16 | PASI ≥10, BSA NR | Secukinumab 150mg (n = 115) | NR (NR) | 41 | 45 (NR) | 55 | NR/100 |
| Secukinumab 300mg (n = 118) | NR (NR) | 40 | 47 (NR) | 57 | NR/100 | ||||
| CLARITY [82] | 75, 90, 100 | 16 | PASI ≥12, BSA ≥10% | Secukinumab (n = 550) | 17 (12) | NR | 45 (14) | 65 | NR/20 |
| Ustekinumab (n = 550) | 17 (13) | NR | 45 (14) | 68 | NR/24 | ||||
| VOYAGE 1 [30] | 75, 90, 100 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 174) | 18 (12) | 17 | 45 (13) | 68 | 53/20 |
| Adalimumab 80 mg 40 mg Q2W (n = 334) | 17 (11) | 19 | 43 (13) | 75 | 64/21 | ||||
| Guselkumab 100 mg (n = 329) | 18 (12) | 20 | 44 (13) | 73 | 64/22 | ||||
| VOYAGE 2 [31] | 75, 90, 100 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 248) | 18 (12) | 19 | 43 (12) | 70 | 60/22 |
| Adalimumab 80 mg 40 mg Q2W (n = 248) | 18 (12) | 18 | 43 (12) | 69 | 64/20 | ||||
| Guselkumab 100 mg (n = 496) | 18 (12) | 18 | 44 (12) | 70 | 67/20 | ||||
| Ohtsuki 2018 [83] | 50, 75, 90, 100 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 64) | 14 (10) | 16 | 48 (11) | 84 | 59/16 |
| Guselkumab 100 mg (n = 63) | 14 (9) | 16 | 48 (11) | 75 | 59/18 | ||||
| ORION [84] | 90, 100 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 16) |
NR (NR) | NR | NR (NR) | NR | NR/NR |
| Guselkumab 100 mg (n = 62) | NR (NR) | NR | NR (NR) | NR | NR/NR | ||||
| IMMhance [85, 86] | 90 | 16 | PASI NR, BSA NR | Placebo (n = 100) | NR (NR) | NR | NR (NR) | NR | NR/NR |
| Risankizumab 150mg (n = 407) | NR (NR) | NR | NR (NR) | NR | NR/NR | ||||
| IMMvent [32, 33] | 90, 100 | 16 | PASI ≥12, BSA ≥10% |
Adalimumab 80mg 40mg Q2W (n = 304) | NR (NR) | NR | NR (NR) | NR | NR/NR |
| Risankizumab 150mg (n = 301) | NR (NR) | NR | NR (NR) | NR | NR/NR | ||||
| UltiMMa-1 [35] |
75, 90, 100 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 102) | NR (NR) | 35 | 49 (14) | 77 | NR/39 |
| Risankizumab 150mg (n = 304) | NR (NR) | 28 | 48 (13) | 70 | NR/34 | ||||
| Ustekinumab (in-label dose) (n = 100) | NR (NR) | 23 | 47 (13) | 70 | NR/30 | ||||
| UltiMMa-2 [35, 36] |
75, 90, 100 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 98) | NR (NR) | 33 | 46 (13) | 68 | NR/43 |
| Risankizumab 150mg (n = 294) | NR (NR) | 25 | 46 (14) | 69 | NR/40 | ||||
| Ustekinumab (in-label dose) (n = 99) | NR (NR) | 27 | 49 (15) | 67 | NR/43 | ||||
| Papp 2015 [87] | 75, 90 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 46) | NR (NR) | 24 | 46 (12) | 83 | NR/28 |
| Tildrakizumab 100mg (n = 89) | NR (NR) | 17 | 46 (13) | 85 | NR/26 | ||||
| Tildrakizumab 200mg (n = 86) | NR (NR) | 17 | 43 (13) | 76 | NR/26 | ||||
| reSURFACE 1 [34] | 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 155) | NR (NR) | NR | 48 (14) | 65 | NR/23 |
| Tildrakizumab 100mg (n = 309) | NR (NR) | NR | 46 (13) | 67 | NR/23 | ||||
| Tildrakizumab 200 mg (n = 308) | NR (NR) | NR | 47 (13) | 73 | NR/23 | ||||
| reSURFACE2 [34] | 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 156) | NR (NR) | NR | 46 (12) | 72 | NR/13 |
| Etanercept 50 mg BIW (n = 313) | NR (NR) | NR | 46 (14) | 71 | NR/12 | ||||
| Tildrakizumab 100 mg (n = 307) | NR (NR) | NR | 45 (14) | 72 | NR/13 | ||||
| Tildrakizumab 200 mg (n = 314) | NR (NR) | NR | 45 (14) | 72 | NR/12 | ||||
| PEARL [88] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 60) | 14 (7) | 12 | 40 (10) | 88 | 72/15 |
| Ustekinumab 45mg (n = 61) | 12 (8) | 16 | 41 (13) | 82 | 71/21 | ||||
| PHOENIX-1 [89] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 255) | 20 (12) | 35 | 45 (11) | 72 | 56/50 |
| Ustekinumab 45mg (n = 255) | 20 (12) | 29 | 45 (13) | 69 | 55/53 | ||||
| Ustekinumab 90mg (n = 256) | 20 (11) | 37 | 46 (11) | 68 | 55/51 | ||||
| PHOENIX-2 [90] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 410) | 21 (12) | 26 | 47 (13) | 69 | 59/39 |
| Ustekinumab 45mg (n = 409) | 19 (12) | 26 | 45 (12) | 69 | 55/38 | ||||
| Ustekinumab 90mg (n = 411) | 20 (12) | 23 | 47 (12) | 67 | 55/37 | ||||
| LOTUS [91] | 50, 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 162) | 14 (9) | 9 | 39 (12) | 76 | 43/7 |
| Ustekinumab 45mg (n = 160) | 15 (9) | 9 | 40 (12) | 78 | 39/12 | ||||
| Igarashi 2012 [92] | 50, 75, 90 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 32) | 16 (11) | 3 | 49 (NR) | 84 | 66/0 |
| Ustekinumab 45mg (n = 64) | 16 (8) | 9 | 45 (NR) | 83 | 73/2 | ||||
| Ustekinumab 90mg (n = 62) | 17 (11) | 11 | 44 (NR) | 76 | 84/0 | ||||
| CHAMPION [93] | 50, 75, 90, 100 | 16 | PASI ≥10, BSA ≥10% | Placebo (n = 53) | 19 (9) | 21 | 41 (11) | 66 | NR/NR |
| Adalimumab 80 mg 40 mg Q2W (n = 108) | 18 (10) | 21 | 43 (13) | 65 | NR/NR | ||||
| Methotrexate (n = 110) | 19 (10) | 17 | 42 (12) | 66 | NR/NR | ||||
| Goldminz 2015 [94] | 75 | 16 | PASI NC, BSA NC | Adalimumab 80 mg 40 mg Q2W (n = 15) | 17 (NR) | 13 | 51 (NR) | 73 | 40/NR |
| Methotrexate (n = 15) | 22 (NR) | 20 | 50 (NR) | 87 | 27/NR | ||||
| Cai 2016 [95] | 75, 90, 100 | 12 | PASI ≥NR, BSA ≥NR | Placebo (n = 87) | 16 (10) | 12 | 44 (13) | 67 | 16/0 |
| Adalimumab 80 mg 40 mg Q2W (n = 338) | 15 (10) | 13 | 43 (12) | 75 | 29/0 | ||||
| REVEAL [96] | 75, 90, 100 | 16 | PASI ≥12, BSA ≥12% | Placebo (n = 398) | 18 (12) | 28 | 45 (13) | 65 | 22/13 |
| Adalimumab 80 mg 40 mg Q2W (n = 814) | 18 (12) | 28 | 44 (13) | 67 | 23/12 | ||||
| Asahina 2010 [97] | 50, 75, 90 | 16 | PASI ≥12, BSA ≥12% | Placebo (n = 46) | 16 (8) | NR | 44 (11) | 89 | 37/0 |
| Adalimumab 80 mg 40 mg Q2W (n = 43) | 14 (7) | NR | 44 (14) | 81 | 42/0 | ||||
| Gordon 2006 [61] | 75, 100 | 12 | PASI ≥NR, BSA ≥5% | Placebo (n = 52) | 19 (1–40) | 31 | 43 (20–70) | 65 | NR/0 |
| Adalimumab 80 mg 40 mg Q2W (n = 46) | 21 (1–58) | 33 | 46 (20–71) | 71 | NR/0 | ||||
| X-PLORE [98] | 75, 90, 100 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 42) | 18 (13) | 29 | 47 (NR) | 67 | 50/36 |
| Adalimumab 80 mg 40 mg Q2W (n = 43) | 19 (13) | 26 | 50 (NR) | 70 | 40/60 | ||||
| CIMPACT [99] | 75, 90 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 57) | 19 (13) | 21 | 47 (13) | 60 | NR/19 |
| Certolizumab 200mg (n = 165) | 20 (13) | 16 | 47 (14) | 69 | NR/27 | ||||
| Certolizumab 400mg (n = 167) | 18 (12) | 14 | 45 (12) | 64 | NR/29 | ||||
| Etanercept 50mg BIW (n = 170) | 17 (12) | 16 | 45 (14) | 75 | NR/30 | ||||
| CIMPASI-1 [100] | 75, 90, 100 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 51) | 19 (13) | 8 | 48 (13) | 69 | NR/29 |
| Certolizumab 200mg (n = 95) | 17 (12) | 11 | 45 (13) | 71 | NR/32 | ||||
| Certolizumab 400mg (n = 88) | 18 (13) | 17 | 44 (12) | 68 | NR/33 | ||||
| CIMPASI-2 [100] | 75, 90, 100 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 49) | 15 (12) | 18 | 43 (15) | 53 | NR/29 |
| Certolizumab 200mg (n = 91) | 19 (14) | 24 | 47 (13) | 64 | NR/35 | ||||
| Certolizumab 400mg (n = 87) | 19 (12) | 30 | 46 (14) | 49 | NR/35 | ||||
| Reich 2012 [101] | 50, 75, 90 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 59) | 20 (12) | NR | 43 (13) | 63 | NR/24 |
| Certolizumab 200mg (n = 59) | 21 (11) | NR | 43 (10) | 75 | NR/22 | ||||
| Certolizumab 400mg (n = 58) | 20 (10) | NR | 44 (12) | 72 | NR/24 | ||||
| Leonardi 2003 [102] | 50, 75, 90 | 16 | PASI ≥10, BSA ≥10% | Placebo (n = 166) | 18 (12) | NR | 46 (13) | 63 | NR/NR |
| Etanercept 25 mg BIW (n = 162) | 19 (12) | NR | 45 (13) | 67 | NR/NR | ||||
| Etanercept 50 mg BIW (n = 164) | 19 (12) | NR | 45 (10) | 65 | NR/NR | ||||
| Gottlieb 2003 [103] | 50, 75, 90 | 12 | PASI ≥NR, BSA ≥10% | Placebo (n = 55) | 20 (2) | 65 | 47 (18–77) | 67 | 36/NR |
| Etanercept 25 mg BIW (n = 57) | 23 (2) | 72 | 48.2 (25–72) | 58 | 39/NR | ||||
| Papp 2005 [104] | 50, 75, 90 | 12 | PASI ≥10, BSA ≥10% | Placebo (n = 193) | 18 (1–52) | 26 | 45 (11) | 64 | 39/0 |
| Etanercept 25mg BIW (n = 196) | 22 (1–65) | 28 | 45 (12) | 65 | 35/0 | ||||
| Etanercept 50mg BIW (n = 194) | 18 (1–61) | 26 | 45 (12) | 67 | 38/0 | ||||
| Van de Kerkhof 2008 [105] | 50, 75, 90 | 12 | PASI ≥10, BSA ≥10% | Placebo (n = 46) | 17 (8) | 11 | 44 (13) | 54 | 48/0 |
| Etanercept 50mg BIW (n = 96) | 19 (11) | 16 | 46 (13) | 62 | 49/0 | ||||
| Bagel 2012 [106] | 50, 75, 90 | 12 | PASI ≥10, BSA ≥10% | Placebo (n = 62) | 11 (1–49) | NR | 42 (8–70) | 58 | NR/7 |
| Etanercept 50mg BIW (n = 62) | 18 (1–45) | NR | 39 (18–71) | 53 | NR/7 | ||||
| Bachelez 2015 [107] | 50, 75, 90 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 107) | 17 (1–57) | 24 | 46 (21–81) | 66 | NR/11 |
| Etanercept 50mg BIW (n = 335) | 18 (1–62) | 21 | 42 (18–74) | 70 | NR/11 | ||||
| Tyring 2006 [108] | 50, 75, 90 | 12 | PASI ≥10, BSA ≥10% | Placebo (n = 309) | 20 (11) | 33 | 46 (12) | 70 | NR/NR |
| Etanercept 50mg BIW (n = 311) | 20 (12) | 35 | 46 (13) | 65 | NR/NR | ||||
| PRISTINE [109] | 50, 75, 90 | 12 | PASI ≥10, BSA ≥10% | Etanercept 50mg QW (n = 137) | 17 (11) | 29 | 44 (13) | 74 | NR/NR |
| Etanercept 50mg BIW (n = 136) | 18 (10) | 33 | 44 (13) | 65 | NR/NR | ||||
| M10-114 [110] | 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 68) | 19 (13) | 21 | 44 (14) | 69 | 28/15 |
| Etanercept 50mg BIW (n = 141) | 17 (13) | 23 | 43 (13) | 70 | 26/14 | ||||
| M10-315 [111] | 75, 90, 100 | 12 | PASI ≥12, BSA ≥10% | Placebo (n = 72) | 16 (12) | 21 | 45 (14) | 64 | 28/4 |
| Etanercept 50mg BIW (n = 139) | 15 (12) | 33 | 45 (15) | 61 | 32/8 | ||||
| PIECE [112] | 50, 75, 90, 100 | 12 | PASI ≥10, BSA ≥10% | Etanercept 50mg BIW (n = 23) | 18 (11) | 13 | 4 (13) | 57 | 100/22 |
| Infliximab 5mg/kg (n = 25) | 22 (13) | 8 | 46 (14) | 72 | 96/12 | ||||
| ACCEPT [113] | 75, 90 | 12 | PASI ≥12, BSA ≥10% | Etanercept 50mg BIW 45mg (n = 347) | 19 (12) | 27 | 46 (13) | 71 | 57/12 |
| Ustekinumab 45mg (n = 209) | 19 (12) | 30 | 45 (13) | 64 | 62/12 | ||||
| Ustekinumab 90mg (n = 347) | 19 (12) | 27 | 45 (12) | 67 | 52/10 | ||||
| Caproni 2009 [114] | 50, 75 | 12 | PASI ≥10, BSA ≥10% | Etanercept 50mg BIW (n = 30) | NR (NR) | NR | NR (28–67) | 43 | NR/NR |
| Acitretin (n = 30) | NR (NR) | NR | NR (31–65) | 37 | NR/NR | ||||
| Gisondi 2008 [115] | 50, 75 | 12 | PASI ≥NR, BSA ≥NR | Etanercept 25mg BIW (n = 22) | 24 (11) | NR | 55 (11) | 55 | NR/0 |
| Acitretin (n = 20) | 19 (16) | NR | 55 (11) | 60 | NR/0 | ||||
| Yang 2012 [116] | 75, 90, 100 | 10 | PASI ≥12, BSA ≥10% | Placebo (n = 45) | 16 (9) | NR | 40 (11) | 78 | NR/NR |
| Infliximab 5mg/kg (n = 84) | 16 (11) | NR | 39 (12) | 71 | NR/NR | ||||
| EXPRESS [117] | 50, 75, 90, 100 | 10 | PASI ≥12, BSA ≥10% | Placebo (n = 77) | 17 (11) | 29 | 44 (13) | 79 | 46/0 |
| Infliximab 5mg/kg (n = 301) | 19 (11) | 31 | 43 (12) | 69 | 42/0 | ||||
| Chaudhari 2001 [118] | 75 | 10 | PASI ≥NR, BSA ≥5% | Placebo (n = 11) | NR (NR) | NR | 45 (12) | NR | NR/0 |
| Infliximab 5mg/kg (n = 11) | NR (NR) | NR | 51 (14) | NR | NR/0 | ||||
| SPIRIT [119] | 50, 75, 90 | 10 | PASI ≥12, BSA ≥10% | Placebo (n = 51) | 16 (IQR: 6, 22) | 33 | 45 (IQR: 30, 52) | 61 | 82/31 |
| Infliximab 5mg/kg (n = 99) | 16 (IQR: 10, 25) | 29 | 44 (IQR: 34, 53) | 74 | 89/33 | ||||
| EXPRESS II [120] | 75, 90 | 10 | PASI ≥10, BSA ≥10% | Placebo (n = 208) | NR (NR) | 26 | 44 (13) | 69 | NR/13 |
| Infliximab 5mg/kg (n = 314) | NR (NR) | 28 | 45 (13) | 65 | NR/14 | ||||
| Torii 2010 [121] | 50, 75, 90 | 10 | PASI ≥12, BSA ≥10% | Placebo (n = 19) | 11 (6) | 37 | 43 (12) | 74 | 95/NR |
| Infliximab 5mg/kg (n = 35) | 14 (9) | 29 | 47 (13) | 63 | 94/NR | ||||
| RESTORE1 [122] | 50, 75, 90 | 16 | PASI ≥12, BSA ≥10% | Infliximab 5mg/kg (n = 653) | 19 (12) | NR | 44 (18–78) | 67 | 61/8 |
| Methotrexate (n = 215) | 17 (10) | NR | 42 (18–69) | 69 | 65/8 | ||||
| PSOR-005 [123] | 50, 75, 90, 100 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 88) | 20 (12) | 19 | 44 (14) | 60 | 44/NR |
| Apremilast 20 mg BID (n = 87) | 19 (12) | 18 | 45 (13) | 63 | 49/NR | ||||
| Apremilast 30 mg BID (n = 88) | 19 (12) | 24 | 44 (15) | 57 | 53/NR | ||||
| ESTEEM 1 [124] | 50, 75, 90 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 282) | 19 (12) | NR | 47 (13) | 69 | 36/28 |
| Apremilast 30 mg BID (n = 562) | 20 (13) | NR | 46 (13) | 67 | 38/29 | ||||
| ESTEEM 2 [125] | 50, 75, 90 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 137) | 19 (12) | NR | 46 (13) | 73 | 39/32 |
| Apremilast 30 mg BID (n = 274) | 18 (11) | NR | 45 (13) | 64 | 39/34 | ||||
| Papp 2013 [126] | 50, 75, 90 | 12 | BSA ≥10% | Placebo (n = 87) | NR (NR) | 13 | 44 (12) | 61 | NR/NR |
| Apremilast 20 mg BID (n = 85) | NR (NR) | 25 | 48 (12) | 58 | NR/NR | ||||
| Ohtsuki 2017 [127] | 50, 75, 90 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 84) | 12 (9) | NR | 48 (12) | 74 | 26/5 |
| Apremilast 20 mg BID (n = 85) | 13 (11) | NR | 52 (13) | 81 | 40/4 | ||||
| Apremilast 30 mg BID (n = 85) | 14 (9) | NR | 52 (13) | 84 | 31/2 | ||||
| LIBERATE [128, 129] | 50, 75, 90 | 16 | PASI ≥12, BSA ≥10% | Placebo (n = 84) | 17 (12) | NR | 43 (15) | 70 | 83/0 |
| Apremilast 30 mg BID (n = 83) | 20 (13) | NR | 46 (14) | 59 | 80/0 | ||||
| Etanercept 50 mg QW (n = 83) | 18 (12) | NR | 47 (14) | 59 | 70/0 | ||||
| UNVEIL [62, 63, 130] | 75 | 16 | PASI ≥NR, BSA ≥5% | Placebo (n = 73) | 14 (13) | NR | 51 (14) | 56 | 0/0 |
| Apremilast 30mg BID (n = 148) | 18 (14) | NR | 49 (15) | 50 | 0/0 | ||||
| BRIDGE [131] | 50, 75, 90 | 16 | PASI ≥10, BSA ≥10% | Placebo (n = 138) | NR (NR) | NR | 44 (14) | 68 | MTX: 10 CIC: 6; ACI: 7/TNF: 2 |
| Dimethyl Fumarate (n = 208) | NR (NR) | NR | 44 (15) | 62 | MTX: 7; CIC: 4; ACI: 3/TNF: 2.5; IL: 1 | ||||
| Fumaderm (n = 286) | NR (NR) | NR | 45 (14) | 65 | MTX: 14; CIC: 3; ACI: 5/TNF: 2; IL: 1 | ||||
n, number of patients; PASI, Psoriasis Area and Severity Index; BSA, body surface area; PsA, Psoriatic Arthritis; SD, standard deviation; BID, twice daily; BIW, twice weekly; QW, weekly; Q2W, every 2 weeks; Q4W, every 4 weeks; mg, milligrams; kg, kilograms; NR, not reported; NC, not considered; MTX, methotrexate; CIC, cyclosporin; ACI, acitretin; TNF, tumour necrosis factor; IL, interleukin
* range reported only if SD not available
Patient characteristics were broadly similar across studies. In the majority of RCTs mean baseline PASI scores ranged from 8 [62, 63, 115] to 32 [121]. In the included trials, patients’ mean age ranged from 40 [116] to 57 years [59] and the percentage of males was between 40% [114] and 85% [97]. Exposure to prior therapies varied across studies. Three RCTs included only systemic-naïve patients [62, 71, 79], while in the remaining studies the mean percentage of patients who had received prior conventional systemic therapy ranged from 23% [96] to 98% [112]. The proportion of patients who received prior phototherapy also varied considerably across trials and, where reported, percentages ranged between 16% [96] and 98% [132].
When studies reported previous exposure to biologic therapy, this ranged from 1% [92] to 100% [81] across trials. More recent studies [64, 65, 67, 74, 89, 90] included greater proportions of patients with previous exposure to biologic therapies, whereas, other studies required patients to be naïve to biologic therapies [61, 62, 71, 79, 93–95, 97, 104, 105, 115, 117, 118, 128].
Risk of bias
Overall, the risk of bias for most of the studies was judged to be low (details reported in S5 Table). Studies generally reported appropriate randomisation and allocation concealment. Patient characteristics appeared similar between treatment arms at baseline. Most of the studies were double-blind, however in some cases only investigator blinding was undertaken. Losses to follow-up appeared to be balanced between study arms, except for PRIME [79], where proportionally more patients were lost to follow-up in the FAE arm compared to secukinumab; Ohtsuki 2018 [83], where more patients dropped out of the placebo arm compared to guselkumab arms; and a phase II certolizumab trial [101, 133], where drop-outs from the placebo arm were much higher than from certolizumab arms. The risk of reporting bias was considered low in all studies. Most studies used an intention-to-treat or modified intention-to-treat approach, including all randomised patients. There was, however, variation in the method used to handle missing data: forty-one (53%) studies used non-responder imputation, 18 (23%) used last observation carried forward, four (5%) used multiple imputation methods, and the remaining fourteen (18%) did not report the method used.
Model fit
Goodness of fit was assessed for the model with placebo-adjustment compared to the model without adjustment. The estimated placebo arm adjustment coefficient was statistically significant (-0.676, 95% CrI: -0.824 to -0.507), indicating that the adjustment reduced unexplained heterogeneity and improved the model. In addition, the 95% CrI of the random effect, τ, was estimated to be from 60.4 to 271.9 in the adjusted model compared with 52.5 to 466.8 in the unadjusted model. The narrowing of the 95% CrI in the adjusted model demonstrates a reduction in the between-study heterogeneity being captured by the adjustment coefficient. No significant inconsistency was identified in the base-case or sensitivity analysis networks.
Efficacy relative to placebo
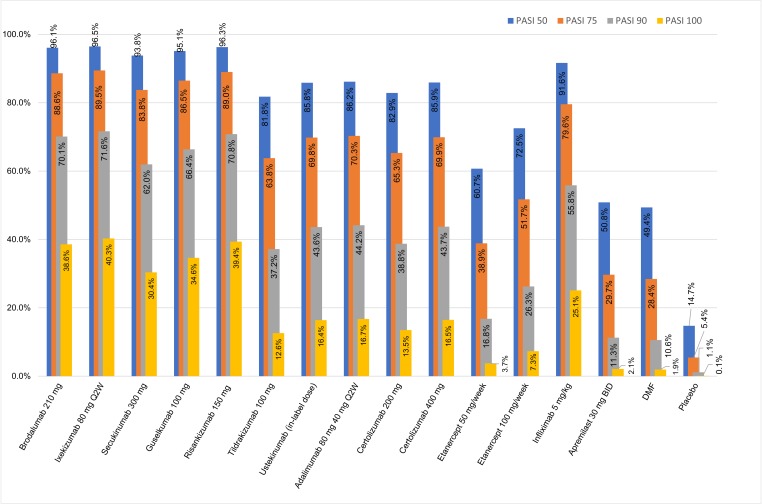
Fig 3 presents the probabilities of achieving each level of PASI response for each treatment. As shown in Table 2, the placebo-adjusted base-case analysis indicated all therapies to be superior to placebo. In comparison with placebo, licensed doses of ixekizumab, and brodalumab along with risankizumab and guselkumab have shown the greatest treatment effects at inducing all levels of PASI response. The effects of these treatments were particularly pronounced for PASI 100, for which the proportion achieving complete clearance was more than 350 times higher than with placebo. Compared with placebo, the number needed to treat (NNT) to achieve complete clearance was the lowest for ixekizumab (NNT = 3), risankizumab (NNT = 3), brodalumab (NNT = 3) and guselkumab (NNT = 3). Etanercept, apremilast and DMF were associated with the lowest probabilities of response and highest NNTs of 28, 50 and 55, respectively.
Fig 3. PASI response at end of induction—placebo-adjusted.
Table 2. Treatment effects at each level of PASI response for all interventions versus placebo at the end of induction.
Number needed to treat included for PASI 100 –placebo-adjusted base-case.
| Class | Treatment | Risk ratio versus placebo, median (95% CrI) | NNT for PASI 100 (95% CrI) | |||
|---|---|---|---|---|---|---|
| PASI 50 | PASI 75 | PASI 90 | PASI 100 | |||
| IL-17RA | Brodalumab 210mg | 6.52 (3.39 to 14.63) | 16.26 (7.07 to 42.54) | 62.34 (22.61 to 188.04) | 398.09 (124.07 to 1348.07) | 2.60 (1.71, 4.72) |
| IL-17A | Ixekizumab 80mg Q2W | 6.54 (3.39 to 14.75) | 16.42 (7.10 to 43.31) | 63.73 (22.91 to 194.67) | 415.97 (127.94 to 1436.99) | 2.49 (1.66, 4.43) |
| Secukinumab 300mg | 6.37 (3.36 to 13.91) | 15.36 (6.89 to 38.40) | 55.07 (21.08 to 155.69) | 313.68 (104.99 to 976.56) | 3.30 (2.02, 6.53) | |
| IL-23 | Guselkumab 100 mg | 6.45 (3.37 to 14.30) | 15.85 (6.99 to 40.62) | 58.89 (21.90 to 173.16) | 356.00 (114.80 to 1173.71) | 2.90 (1.83, 5.52) |
| Risankizumab 150 mg | 6.53 (3.39 to 14.68) | 16.32 (7.08 to 42.86) | 62.89 (22.72 to 191.53) | 405.52 (125.87 to 1392.95) | 2.55 (1.69, 4.62) | |
| Tildrakizumab 100 mg | 5.55 (3.15 to 10.77) | 11.67 (5.90 to 24.89) | 32.96 (15.02 to 76.80) | 129.52 (54.00 to 327.55) | 8.00 (3.81, 20.84) | |
| IL-12/23 | Ustekinumab (in-label dose) | 5.82 (3.23 to 11.73) | 12.80 (6.25 to 28.47) | 38.74 (16.84 to 94.52) | 168.83 (66.89 to 444.05) | 6.14 (3.17, 14.57) |
| Anti-TNF | Adalimumab 40mg Q2W | 5.84 (3.23 to 11.83) | 12.88 (6.27 to 28.87) | 39.22 (16.98 to 96.43) | 172.50 (67.93 to 456.20) | 6.01 (3.13, 14.09) |
| Certolizumab 200mg | 5.61 (3.17 to 11.02) | 11.96 (6.00 to 25.72) | 34.34 (15.43 to 80.91) | 138.72 (56.63 to 355.49) | 7.47 (3.61, 19.40) | |
| Certolizumab 400mg | 5.82 (3.23 to 11.74) | 12.80 (6.24 to 28.54) | 38.74 (16.76 to 95.33) | 169.03 (66.05 to 455.17) | 6.11 (3.11, 14.93) | |
| Etanercept 50 mg / week | 4.11 (2.66 to 6.76) | 7.10 (4.30 to 12.37) | 14.86 (8.45 to 27.43) | 38.52 (20.58 to 75.53) | 27.40 (10.16, 92.68) | |
| Etanercept 100 mg / week | 4.92 (2.96 to 8.83) | 9.50 (5.22 to 18.28) | 23.35 (11.87 to 47.69) | 75.41 (36.11 to 161.84) | 13.87 (6.00, 39.80) | |
| Infliximab 5mg/kg | 6.22 (3.32 to 13.23) | 14.58 (6.71 to 35.10) | 49.60 (19.72 to 133.53) | 258.53 (91.49 to 765.11) | 4.00 (2.31, 8.48) | |
| PDE4 | Apremilast 30mg BID | 3.44 (2.38 to 5.25) | 5.42 (3.54 to 8.70) | 9.96 (6.16 to 16.86) | 21.66 (12.65 to 39.09) | 49.66 (16.63, 187.54) |
| FAE | Dimethyl Fumarate | 3.32 (2.26 to 5.31) | 5.14 (3.22 to 8.96) | 9.27 (5.17 to 18.03) | 19.69 (9.46 to 43.84) | 54.68 (16.36, 238.67) |
A median risk ratio higher than 1 indicates that active treatments are more efficacious than placebo at inducing a given level of PASI response. For NNT the exact results of the NMA are provided here for accuracy, although for interpretation the results are rounded up to provide information on the number of patients who would need to be treated in order to observe an additional PASI 100 response.
BID, twice daily; CrI, credible interval; DMF, dimethyl fumarate; PASI, Psoriasis Area and Severity Index; Q2W, every 2 weeks; Q4W, every 4
Weeks; NNT, number needed to treat.
IL-17s versus IL-23s and IL-12/23
As shown in Fig 3, treatment with the IL-17RA brodalumab, the IL-17A ixekizumab and the IL-23s risankizumab and guselkumab produced similar proportions of patients achieving each level of PASI response, with any differences failing to reach statistical significance (PASI 75, 90 and 100 shown in Table 3). In the analysis risankizumab was significantly more efficacious than secukinumab, as were brodalumab and ixekizumab. Median point estimates suggest that guselkumab may be slightly more efficacious than secukinumab, but differences were not statistically significant. The NMA also showed all IL-17 targeted therapies, as well as guselkumab and risankizumab to be more efficacious than tildrakizumab, ustekinumab, adalimumab and certolizumab, which were all more efficacious than etanercept, apremilast and DMF. Risk ratios for each pairwise comparison at each level of PASI response are presented in S6 Table.
Table 3. Risk ratios for each pairwise comparison of IL-17As or IL-17RA vs IL-23 or IL-12/23 therapies at PASI 75, 90 and 100 from placebo-adjusted base-case analysis: median risk ratio (95% credible interval).
| Intervention vs. | Comparator | Median risk ratio (95% credible interval) | ||
|---|---|---|---|---|
| PASI 75 | PASI 90 | PASI 100 | ||
| Brodalumab | Ixekizumab | 0.99 (0.95, 1.03) | 0.98 (0.9, 1.06) | 0.96 (0.81, 1.12) |
| Secukinumab | 1.06 (1.02, 1.14) | 1.13 (1.04, 1.28) | 1.26 (1.08, 1.55) | |
| Guselkumab | 1.02 (0.98, 1.09) | 1.05 (0.96, 1.19) | 1.11 (0.93, 1.37) | |
| Risankizumab | 1 (0.95, 1.04) | 0.99 (0.9, 1.09) | 0.98 (0.82, 1.17) | |
| Tildrakizumab | 1.39 (1.18, 1.78) | 1.88 (1.45, 2.67) | 3.03 (2.08, 4.86) | |
| Ustekinumab (in label) | 1.27 (1.13, 1.52) | 1.6 (1.32, 2.07) | 2.35 (1.78, 3.29) | |
| Ixekizumab | Secukinumab | 1.07 (1.02, 1.15) | 1.15 (1.06, 1.32) | 1.32 (1.13, 1.63) |
| Guselkumab | 1.03 (0.99, 1.1) | 1.08 (0.99, 1.22) | 1.16 (0.97, 1.44) | |
| Risankizumab | 1.01 (0.97, 1.05) | 1.01 (0.93, 1.11) | 1.03 (0.86, 1.23) | |
| Tildrakizumab | 1.4 (1.18, 1.81) | 1.92 (1.47, 2.75) | 3.18 (2.16, 5.12) | |
| Ustekinumab (in label) | 1.28 (1.13, 1.55) | 1.64 (1.34, 2.15) | 2.45 (1.83, 3.51) | |
| Secukinumab | Guselkumab | 0.97 (0.91, 1.02) | 0.94 (0.83, 1.04) | 0.88 (0.72, 1.07) |
| Risankizumab | 0.94 (0.87, 0.98) | 0.88 (0.77, 0.96) | 0.78 (0.62, 0.93) | |
| Tildrakizumab | 1.31 (1.14, 1.62) | 1.66 (1.33, 2.24) | 2.39 (1.73, 3.6) | |
| Ustekinumab (in label) | 1.2 (1.09, 1.37) | 1.42 (1.22, 1.72) | 1.85 (1.49, 2.41) | |
| Guselkumab | Risankizumab | 0.97 (0.91, 1.01) | 0.94 (0.83, 1.03) | 0.88 (0.71, 1.05) |
| Tildrakizumab | 1.35 (1.16, 1.71) | 1.77 (1.39, 2.47) | 2.72 (1.89, 4.27) | |
| Ustekinumab (in label) | 1.24 (1.11, 1.46) | 1.51 (1.27, 1.93) | 2.1 (1.6, 2.94) | |
| Risankizumab | Tildrakizumab | 1.39 (1.18, 1.79) | 1.89 (1.45, 2.71) | 3.09 (2.1, 4.99 |
| Ustekinumab (in label) | 1.27 (1.13, 1.53) | 1.62 (1.33, 2.11) | 2.39 (1.79, 3.42) | |
| Tildrakizumab | Ustekinumab (in label) | 0.92 (0.8, 1.01) | 0.86 (0.69, 1.02) | 0.77 (0.56, 1.03) |
A median risk ratio higher than 1 indicates that the intervention is more efficacious than the comparator at inducing a given level of PASI response.
In terms of NNT compared to ustekinumab, five patients would need to be treated with brodalumab, ixekizumab or risankizumab, six with guselkumab and eight with secukinumab for one more patient to achieve complete clearance. Compared to secukinumab, eleven, twelve and thirteen patients would need to be treated with ixekizumab, risankizumab and brodalumab, respectively, in order to generate an additional PASI 100 responder.
Additional analyses
The analysis that did not adjust for cross-trial variation in placebo responses produced results similar to the placebo-adjusted analysis, though the model fit was poorer, indicating that the results are at risk of heterogeneity-induced bias. For completeness, details of this analysis can be found in S7 Table.
Thirty studies [32, 61, 62, 71, 73, 79, 84, 85, 92–95, 97, 102–105, 108, 109, 114–118, 121, 123, 126–128, 131], were excluded from the network in the sensitivity analysis which restricted trial inclusion to those that reported a minimum of 5% of patients with prior biologic exposure. Among these studies were all five studies [102–105, 109] evaluating the lower dose of etanercept (50 mg weekly) and the only study evaluating DMF [131]. For all other comparators, the results were similar to those of the placebo adjusted base-case. Details of this analysis can be found in S8 Table.
A sensitivity analysis was carried out to test the effect of using 12-week rather than 16-week outcomes from three secukinumab trials (CLEAR [78], SIGNATURE [81] and CLARITY [82]). To test for small study bias, a further sensitivity analysis was carried out excluding the eighteen trials with fewer than 50 patients per trial arm [73, 84, 85, 100, 134–147]. There were no major differences between the results of these sensitivity analyses and the base-case analysis.
Discussion
Our NMA evaluating PASI response among licensed treatments for moderate-to-severe plaque psoriasis included 77 RCTs and a total of 34,816 patients. Data were available on all interventions set out in the inclusion criteria. The base-case analysis showed that all active treatments were superior to placebo. A comparison of PASI response between the classes of drugs with the highest efficacy, IL-17, IL-23 and IL-12/23 targeted treatments, was also undertaken. This showed that IL-17 inhibitors (brodalumab, ixekizumab and secukinumab) were more efficacious than tildrakizumab and ustekinumab and not significantly different from guselkumab. Compared to risankizumab, there was no significant difference in our analysis for brodalumab and ixekizumab, however secukinumab was less efficacious. Comparisons within the IL-17 inhibitor class showed that ixekizumab and brodalumab were not significantly different from one another, but that both were more efficacious than secukinumab. When comparisons were made among the IL-23 inhibitors, risankizumab and guselkumab were both more efficacious than tildrakizumab, but were not significantly different from one another. The greatest benefits of IL-17 inhibitors and IL-23 inhibitors guselkumab and risankizumab were seen for PASI 90 and PASI 100 response.
Since 2017, numerous NMAs have been published comparing the efficacy of various treatments in moderate to severe plaque type psoriasis [23, 24, 38, 148–153], and some have been critically appraised in the literature [154]. This largely reflects the dynamic development of the field, both in terms of treatment availability and new clinical trials being carried out. However, none of the currently published NMAs includes all currently licensed treatments in this patient population. In addition to NMAs, several pairwise meta-analyses have been undertaken comparing the efficacy of treatments in moderate-to-severe plaque psoriasis [155–157]. However, pairwise meta-analyses can only provide limited information and do not allow for a formal comparison of all available treatments. Valid relative efficacy comparisons between multiple treatments can only be made in an NMA [158, 159].
To our knowledge, this NMA provides the most recent and comprehensive comparison of available treatments for chronic plaque psoriasis. Specifically, it is the first to include the recently published clinical trial data for risankizumab and certolizumab pegol. Though many of the most recent clinical trials in moderate-to-severe psoriasis include a head-to-head comparison of targeted therapies, there are still many comparisons that have not been observed. In their absence, the network meta-analytic approach gives the most reliable estimate of comparative efficacy [159].
This NMA was based on a systematic review of RCTs evaluating licensed treatment doses. We followed a protocol designed for the systematic review; however, this was not registered online. English-language publications were searched, which has the potential to introduce bias [160, 161]; however, we believe this was unlikely to have had a substantial impact on our findings. A recent systematic review [23] that did not apply language restrictions identified no additional studies that would have been relevant to our NMA.
Although we were interested in evaluating licensed treatments, we included trials with any intervention or dose as the comparator. Although other recent NMAs chose to restrict inclusion to licensed doses only [25], we believe that such a broad approach allowed the construction of an extensive network of evidence and ensured that all relevant evidence was included and uncertainty in efficacy estimates was reduced [158].
As we set out to provide the best efficacy estimates to inform clinical practice, our analysis was dose-specific. Some recent NMAs have analysed a broad range of treatments, however the conclusions that can be drawn from these may be limited by their design. In particular, some of these analysis pool together both licensed and unlicensed doses of treatments [23, 24]. Although this has the advantage of including all the available information, interpretation of results may be challenging, and may lead to underestimation of the efficacy of treatments available to patients if evidence for subtherapeutic doses is included. Therefore, we analysed different doses separately to provide information we believe to be most relevant to clinical practice. Other recent NMAs [148, 149] have analysed a narrower range of treatments which makes a comprehensive assessment of the available treatments for plaque psoriasis impossible and conclusions limited in their relevance.
We evaluated all treatments at the end of their licensed induction period, which varies by drug [29, 162–172]. As a result, and similarly to a number of other NMAs [25, 38, 173], we combined data from different timepoints (10–16 weeks). Although this may have introduced some heterogeneity, it allowed the inclusion of all relevant information. In the recent Cochrane review and NMA [23], only trials with follow up between 12 and 16 weeks were included. Though this may have reduced the between-study heterogeneity, it resulted in the exclusion of all the pivotal studies comparing infliximab to placebo [116–121].
As our NMA only included data up to 16 weeks obtained from clinical trials, it does not provide an estimate of long-term effectiveness in a trial or real-world clinical setting. Psoriasis is a chronic condition, therefore a better understanding of the comparative effectiveness of biological drugs beyond induction would be beneficial. The randomised evidence is however limited, although some trials have reported 52-week results [30, 35, 36, 65, 69, 75, 174, 175] and researchers have synthesised some of these data [176]. Existence of such data will facilitate future evaluation of these treatments using an NMA approach.
A further limitation of the analysis was the inclusion of only PASI response rates. Although these are the most commonly used efficacy outcomes in psoriasis clinical trials, they do not provide a complete understanding of patient wellbeing. Statistical analysis of health-related quality of life (HRQoL) and safety data may also be helpful in clinical decision making. One of the most recent evaluations of HRQoL and tolerability in psoriasis suggested that IL-17 and IL-23 inhibitors provide the most benefit in terms of quality of life, while the occurrence of serious adverse events is not significantly more frequent than in patients treated with placebo [23, 24].
In psoriasis, placebo response rates have been observed to vary considerably between trials [44], reflecting differences in study design and patient characteristics. In line with these observations, we have identified variation in factors such as patient age, baseline PASI scores, or prior exposure to systemic therapy. To account for the potential heterogeneity introduced by these differences, our analysis presented the results of two statistical models: one that adjusted for variation in placebo-arm response and one that did not. Consistent with three previous NMAs [25, 38, 51], the estimated placebo arm adjustment coefficient was statistically significant, indicating that the adjustment reduced unexplained heterogeneity and improved the model. Cameron et al. explored several covariates in meta-regression analyses, including placebo-response adjustment, prior biologic use, body weight, disease duration, age, race and baseline outcome scores. In their analysis of PASI responses, the authors also found the placebo-adjusted model to have the best fit and argued that it likely accounted for multiple effect modifiers simultaneously.
Our results are broadly similar to those of other recently published NMAs [23–25, 38] in showing that all active treatments are superior to placebo and that IL-17 (in particular brodalumab and ixekizumab) and IL-23 inhibitors (in particular guselkumab and risankizumab) are the most efficacious in inducing PASI response. All analyses show that achieving complete and near complete clearance is more likely with these new treatments. We can also compare our results to those of the ECLIPSE study which has recently been reported in Johnson & Johnson press material [37]. Both our analysis and the current reports for ECLIPSE suggest there is no significant difference between secukinumab and guselkumab at the end of a 12-week induction period. Future work should focus on incorporating this new head-to-head comparison once it is published.
We believe our NMA adds to the current body of evidence, evaluating the efficacy of licensed doses of all treatments that are or will soon be available to patients. This NMA is the first to include risankizumab, and the recently licensed certolizumab pegol in its licensed dose. As our searches have been carried out recently, we have also included a number of recent trials that were not previously included in any NMA [72, 73, 79, 81–84].
With PASI 90 and PASI 100 becoming attainable treatment goals, consensus is growing that dermatologists should expect more highly effective therapies for their psoriasis patients [177, 178], especially as these have been shown to translate to improved HRQoL [179, 180].
Conclusions
The results of the NMA indicated that brodalumab, ixekizumab, risankizumab and guselkumab showed the highest levels of efficacy. It is not possible to make conclusions at drug class level, as there are differences between treatments within the same class, some significant. In our analysis the IL-17RA inhibitor brodalumab and IL-17A inhibitor ixekizumab as well as the IL-23 targeted risankizumab were found to be significantly more efficacious than secukinumab. The NMA showed that across all levels of PASI response, all IL-17 targeted therapies, risankizumab and guselkumab outperformed tildrakizumab and ustekinumab as well as anti-TNFs such as adalimumab, certolizumab pegol and etanercept. These effects were particularly pronounced for PASI 90 and PASI 100. Our results are broadly consistent with previously published NMAs.
Supporting information
(DOCX)
(DOCX)
(XLSX)
(DOCX)
(XLSX)
(XLSX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This study was funded by Leo Pharma A/S, https://www.leo-pharma.com. The funders had a role in study design, interpretation of results, decision to publish and preparation of the manuscript.
References
- 1.Girolomoni G, Strohal R, Puig L, Bachelez H, Barker J, Boehncke WH, et al. The role of IL‐23 and the IL‐23/T(H)17 immune axis in the pathogenesis and treatment of psoriasis. Journal of the European Academy of Dermatology and Venereology. 2017;31(10):1616–26. 10.1111/jdv.14433 PMC5697699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parisi R, Symmons DPM, Griffiths CEM, Ashcroft DM. Global Epidemiology of Psoriasis: A Systematic Review of Incidence and Prevalence. Journal of Investigative Dermatology. 2013;133(2):377–85. 10.1038/jid.2012.339 [DOI] [PubMed] [Google Scholar]
- 3.Dogra S, Mahajan R. Psoriasis: Epidemiology, clinical features, co-morbidities, and clinical scoring. Indian dermatol. 2016;7(6):471–80. 10.4103/2229-5178.193906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Menter A, Gottlieb A, Feldman SR, Van Voorhees AS, Leonardi CL, Gordon KB, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis. Journal of the American Academy of Dermatology. 2008;58(5):826–50. 10.1016/j.jaad.2008.02.039 [DOI] [PubMed] [Google Scholar]
- 5.Goff K, Karimkhani C, Boyers L, Weinstock M, Lott J, Hay R, et al. The global burden of psoriatic skin disease. British Journal of Dermatology. 2015;172(6):1665–8. 10.1111/bjd.13715 [DOI] [PubMed] [Google Scholar]
- 6.Langley R, Krueger G, Griffiths C. Psoriasis: epidemiology, clinical features, and quality of life. Annals of the Rheumatic Diseases. 2005;64(Suppl 2):ii18–ii23. 10.1136/ard.2004.033217 PMC1766861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiss SC, Kimball AB, Liewehr DJ, Blauvelt A, Turner ML, Emanuel EJ. Quantifying the harmful effect of psoriasis on health-related quality of life. Journal of the American Academy of Dermatology. 2002;47(4):512–8. 10.1067/mjd.2002.122755 [DOI] [PubMed] [Google Scholar]
- 8.Obradors M, Blanch C, Comellas M, Figueras M, Lizan L. Health-related quality of life in patients with psoriasis: a systematic review of the European literature. Quality of Life Research. 2016;25(11):2739–54. 10.1007/s11136-016-1321-7 [DOI] [PubMed] [Google Scholar]
- 9.Rapp SR, Feldman SR, Exum ML, Fleischer AB, Jr., Reboussin DM. Psoriasis causes as much disability as other major medical diseases. Journal of the American Academy of Dermatology. 1999;41(3):401–7. 10.1016/S0190-9622(99)70112-X [DOI] [PubMed] [Google Scholar]
- 10.de Korte J, Mombers FMC, Bos JD, Sprangers MAG. Quality of Life in Patients with Psoriasis: A Systematic Literature Review. Journal of Investigative Dermatology Symposium Proceedings. 2004;9(2):140–7. 10.1046/j.1087-0024.2003.09110.x. [DOI] [PubMed] [Google Scholar]
- 11.NICE. Psoriasis: assessment and management. Clinical Guideline CG153. 2017 update. National Institute of Health and Care Excellence. 2018 [22 June 2018]. Available from: https://www.nice.org.uk/guidance/cg153. [PubMed]
- 12.NICE. NICE Pathways: Systemic biological therapy for psoriasis 2018 [25 June 2018]. Available from: https://pathways.nice.org.uk/pathways/psoriasis#content=view-node%3Anodes-adalimumab&path=view%3A/pathways/psoriasis/systemic-biological-therapy-for-psoriasis.xml.
- 13.Smith CH, Jabbar‐Lopez ZK, Yiu ZZ, Bale T, Burden AD, Coates LC, et al. British Association of Dermatologists guidelines for biologic therapy for psoriasis 2017. British Journal of Dermatology. 2017;177(3):628–36. 10.1111/bjd.15665 [DOI] [PubMed] [Google Scholar]
- 14.Skilarence 2018 [04 February 2019]. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/skilarence.
- 15.Winterfield LS, Menter A, Gordon K, Gottlieb A. Psoriasis treatment: current and emerging directed therapies. Annals of the Rheumatic Diseases. 2005;64(suppl 2):ii87–ii90. 10.1136/ard.2004.032276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gaspari AA, Tyring S. New and emerging biologic therapies for moderate‐to‐severe plaque psoriasis: mechanistic rationales and recent clinical data for IL‐17 and IL‐23 inhibitors. Dermatologic therapy. 2015;28(4):179–93. 10.1111/dth.12251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Malakouti M, Jacob SE, Anderson NJ. Treatment challenges in the management of moderate-to-severe plaque psoriasis–role of secukinumab. Clinical, cosmetic and investigational dermatology. 2016;9:347 10.2147/CCID.S81160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carrascosa JM, Doorn MBA, Lahfa M, Nestle FO, Jullien D, Prinz JC. Clinical relevance of immunogenicity of biologics in psoriasis: Implications for treatment strategies. Journal of the European Academy of Dermatology and Venereology. 2014;28(11):1424–30. 10.1111/jdv.12549 [DOI] [PubMed] [Google Scholar]
- 19.Warren RB, Smith CH, Yiu ZZN, Ashcroft DM, Barker JNWN, Burden AD, et al. Differential Drug Survival of Biologic Therapies for the Treatment of Psoriasis: A Prospective Observational Cohort Study from the British Association of Dermatologists Biologic Interventions Register (BADBIR). Journal of Investigative Dermatology. 2015;135(11):2632–40. 10.1038/jid.2015.208 [DOI] [PubMed] [Google Scholar]
- 20.Gniadecki R, Bang B, Bryld LE, Iversen L, Lasthein S, Skov L. Comparison of long‐term drug survival and safety of biologic agents in patients with psoriasis vulgaris. British Journal of Dermatology. 2015;172(1):244–52. 10.1111/bjd.13343 [DOI] [PubMed] [Google Scholar]
- 21.Benson JM, Peritt D, Scallon BJ, Heavner GA, Shealy DJ, Giles-Komar JM, et al. Discovery and mechanism of ustekinumab: a human monoclonal antibody targeting interleukin-12 and interleukin-23 for treatment of immune-mediated disorders. mAbs. 2011;3(6):535–45. Epub 11/01. 10.4161/mabs.3.6.17815 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Papp KA, Leonardi C, Menter A, Ortonne JP, Krueger JG, Kricorian G, et al. Brodalumab, an anti-interleukin-17-receptor antibody for psoriasis. N Engl J Med. 2012;366(13):1181–9. 10.1056/NEJMoa1109017 . [DOI] [PubMed] [Google Scholar]
- 23.Sbidian E, Chaimani A, Garcia-Doval I, Do G, Hua C, Mazaud C, et al. Systemic pharmacological treatments for chronic plaque psoriasis: A network meta-analysis. Cochrane Database of Systematic Reviews. 2017;2017 (12) (no pagination)(CD011535). 10.1002/14651858.CD011535.pub2. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jabbar-Lopez ZK, Yiu ZZN, Ward V, Exton LS, Mohd Mustapa MF, Samarasekera E, et al. Quantitative Evaluation of Biologic Therapy Options for Psoriasis: A Systematic Review and Network Meta-Analysis. Journal of Investigative Dermatology. 2017;137(8):1646–54. 10.1016/j.jid.2017.04.009 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Loos AM, Liu S, Segel C, Ollendorf DA, Pearson SD, Linder JA. Comparative effectiveness of targeted immunomodulators for the treatment of moderate-to-severe plaque psoriasis: A systematic review and network meta-analysis. Journal of the American Academy of Dermatology. 2018;79(1):135–44.e7. 10.1016/j.jaad.2018.02.027 [DOI] [PubMed] [Google Scholar]
- 26.ICER. Targeted Immunomodulators for the Treatment of Moderate-to-Severe Plaque Psoriasis: Effectiveness and Value. Condition update.: Institute for Clinical and Economic Review; 2018 [17 June 2018]. Available from: https://icer-review.org/wp-content/uploads/2017/11/ICER_Psoriasis_Update_Evidence_Report_061218.pdf.
- 27.EMA. Tremfya: European Medicines Agency; 2017 [25 June 2018]. Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/004271/human_med_002183.jsp&mid=WC0b01ac058001d124.
- 28.EMA. Applications for new human medicines under evaluation by the Committee for Medicinal Products for Human Use. December 2018: European Medicines Agency; 2018 [19 December 2018]. Available from: https://www.ema.europa.eu/documents/report/applications-new-human-medicines-under-evaluation-chmp-december-2018_en.pdf.
- 29.EMA. Ilumetri: European Medicines Agency; 2018 [19.12.2018]. Available from: https://www.ema.europa.eu/documents/overview/ilumetri-epar-medicine-overview_en.pdf.
- 30.Blauvelt A, Papp K, Griffiths C, Randazzo B, Wasfi Y, Shen Y, et al. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the continuous treatment of patients with moderate to severe psoriasis: results from the phase III, double-blinded, placebo- and active comparator-controlled VOYAGE 1 trial. Journal of the american academy of dermatology. 2017;76(3):405–17. 10.1016/j.jaad.2016.11.041 CN-01341398; PubMed Central PMCID: PMCincluded. [DOI] [PubMed] [Google Scholar]
- 31.Reich K, Armstrong A, Foley P, Song M, Wasfi Y, Randazzo B, et al. Efficacy and safety of guselkumab, an anti-interleukin-23 monoclonal antibody, compared with adalimumab for the treatment of patients with moderate to severe psoriasis with randomized withdrawal and retreatment: results from the phase III, double-blind, placebo- and active comparator-controlled VOYAGE 2 trial. Journal of the american academy of dermatology. 2017;76(3):418–31. 10.1016/j.jaad.2016.11.042 CN-01341399; PubMed Central PMCID: PMC [DOI] [PubMed] [Google Scholar]
- 32.Risankizumab Meets All Primary Endpoints Reporting Positive Results in Fourth Pivotal Phase 3 Psoriasis Study [Internet]. Abbvie; 2017; DECEMBER 4, 2017 [cited 11.04.2018]; [6]. Available from: https://news.abbvie.com/news/press-releases/risankizumab-meets-all-primary-endpoints-reporting-positive-results-in-fourth-pivotal-phase-3-psoriasis-study.htm
- 33.Risankizumab Meets All Co-Primary and Ranked Secondary Endpoints, Achieving Significantly Greater Efficacy Versus Standard Biologic Therapies in Three Pivotal Phase 3 Psoriasis Studies [Internet]. Abbvie; 2017 [cited 11.04.2018]. Available from: https://news.abbvie.com/news/press-releases/risankizumab-meets-all-co-primary-and-ranked-secondary-endpoints-achieving-significantly-greater-efficacy-versus-standard-biologic-therapies-in-three-pivotal-phase-3-psoriasis-studies.htm
- 34.Reich K, Papp KA, Blauvelt A, Tyring SK, Sinclair R, Thaci D, et al. Tildrakizumab versus placebo or etanercept for chronic plaque psoriasis (reSURFACE 1 and reSURFACE 2): results from two randomised controlled, phase 3 trials.[Erratum appears in Lancet. 2017 Jul 15;390(10091):230; PMID: 28721878]. Lancet. 2017;390(10091):276–88. 10.1016/S0140-6736(17)31279-5 ; PubMed Central PMCID: PMC [DOI] [PubMed] [Google Scholar]
- 35.Gordon KB, Strober B, Lebwohl M, Augustin M, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab: Results from two double-blind, placebo-and ustekinumab-controlled, phase 3 trials in moderate-to-severe plaque psoriasis. Acta Dermato-Venereologica. 2018;98 (Supplement 219):28–9. 10.2340/00015555-2978. . [DOI] [PubMed] [Google Scholar]
- 36.Gordon KB, Strober B, Lebwohl M, Augustin M, Blauvelt A, Poulin Y, et al. Efficacy and safety of risankizumab in moderate-to-severe plaque psoriasis (UltIMMa-1 and UltIMMa-2): results from two double-blind, randomised, placebo-controlled and ustekinumab-controlled phase 3 trials. The Lancet. 2018;392(10148):650–61. 10.1016/S0140-6736(18)31713-6. ; PubMed Central PMCID: PMCYes. [DOI] [PubMed] [Google Scholar]
- 37.New Phase 3 data demonstrate superiority of TREMFYA® (guselkumab) vs Cosentyx® (secukinumab) in delivering PASI 90 responses in the treatment of moderate to severe plaque psoriasis at week 48 [Internet]. 2018 [cited 17/01/2019]. Available from: https://www.jnj.com/new-phase-3-data-demonstrate-superiority-of-tremfya-guselkumab-vs-cosentyx-secukinumab-in-delivering-pasi-90-responses-in-the-treatment-of-moderate-to-severe-plaque-psoriasis-at-week-48
- 38.Cameron C, Druchok C, Hutton B, McElligott S, Nair S, Schubert A, et al. Guselkumab for the Treatment of Moderate-to-Severe Plaque Psoriasis During Induction Phase: A Systematic Review and Network Meta-Analysis. Journal of Psoriasis and Psoriatic Arthritis. 2018;0(0):2475530318818816. 10.1177/2475530318818816 [DOI] [Google Scholar]
- 39.Shikiar R, Bresnahan BW, Stone SP, Thompson C, Koo J, Revicki DA. Validity and reliability of patient reported outcomes used in Psoriasis: results from two randomized clinical trials. Health and Quality of Life Outcomes. 2003;1(1):53 10.1186/1477-7525-1-53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Feldman SR, Krueger GG. Psoriasis assessment tools in clinical trials. Annals of the Rheumatic Diseases. 2005;64(suppl 2):ii65–ii8. 10.1136/ard.2004.031237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.National Institute for Health and Care Excellence. Guide to the methods of technology appraisal 2013. London: National Institute for Health and Care Excellence, 2013. [PubMed]
- 42.Dias S, Sutton AJ, Ades AE, Welton NJ. Evidence synthesis for decision making 2: a generalized linear modeling framework for pairwise and network meta-analysis of randomized controlled trials. Med Decis Making. 2013;33(5):607–17. 10.1177/0272989X12458724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dias S, Welton NJ, Sutton AJ, Ades AE. Evidence synthesis for decision making 5: the baseline natural history model. Med Decis Making. 2013;33(5):657–70. 10.1177/0272989X13485155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lamel SA, Myer KA, Younes N, Zhou JA, Maibach H, Maibach HI. Placebo response in relation to clinical trial design: a systematic review and meta-analysis of randomized controlled trials for determining biologic efficacy in psoriasis treatment. Arch Dermatol Res. 2012;304(9):707–17. 10.1007/s00403-012-1266-9 . [DOI] [PubMed] [Google Scholar]
- 45.Sharp SJ, Thompson SG. Analysing the relationship between treatment effect and underlying risk in meta-analysis: comparison and development of approaches. Stat Med. 2000;19(23):3251–74. . [DOI] [PubMed] [Google Scholar]
- 46.Sharp SJ, Thompson SG, Altman DG. The relation between treatment benefit and underlying risk in meta-analysis. BMJ. 1996;313(7059):735–8. 10.1136/bmj.313.7059.735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thompson SG, Smith TC, Sharp SJ. Investigating underlying risk as a source of heterogeneity in meta-analysis. Stat Med. 1997;16(23):2741–58. . [DOI] [PubMed] [Google Scholar]
- 48.Achana FA, Cooper NJ, Dias S, Lu G, Rice SJ, Kendrick D, et al. Extending methods for investigating the relationship between treatment effect and baseline risk from pairwise meta-analysis to network meta-analysis. Stat Med. 2013;32(5):752–71. 10.1002/sim.5539 . [DOI] [PubMed] [Google Scholar]
- 49.Dias S, Sutton AJ, Welton NJ, Ades AE. Evidence synthesis for decision making 3: heterogeneity—subgroups, meta-regression, bias, and bias-adjustment. Med Decis Making. 2013;33(5):618–40. 10.1177/0272989X13485157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cameron C, Hutton B, Druchok C, McElligott S, Nair S, Schubert A, et al. Importance of assessing and adjusting for cross-study heterogeneity in network meta-analysis: a case study of psoriasis. Journal of Comparative Effectiveness Research. 2018;7(11):1037–51. 10.2217/cer-2018-0065 . [DOI] [PubMed] [Google Scholar]
- 51.Signorovitch JE, Betts KA, Yan YS, LeReun C, Sundaram M, Wu EQ, et al. Comparative efficacy of biological treatments for moderate-to-severe psoriasis: a network meta-analysis adjusting for cross-trial differences in reference arm response. Br J Dermatol. 2015;172(2):504–12. 10.1111/bjd.13437 . [DOI] [PubMed] [Google Scholar]
- 52.NICE. Final appraisal determination–Brodalumab for treating moderate to severe plaque psoriasis: NATIONAL INSTITUTE FOR HEALTH AND CARE EXCELLENCE; 2018 [19.12.2018]. Available from: https://www.nice.org.uk/guidance/ta511/documents/final-appraisal-determination-document.
- 53.Dias S, Welton NJ, Sutton AJ, Caldwell DM, Lu G, Ades A. Evidence synthesis for decision making 4: inconsistency in networks of evidence based on randomized controlled trials. Medical Decision Making. 2013;33(5):641–56. 10.1177/0272989X12455847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lunn DJ, Thomas A, Best N, Spiegelhalter D. WinBUGS-a Bayesian modelling framework: concepts, structure, and extensibility. Statistics and computing. 2000;10(4):325–37. [Google Scholar]
- 55.Gelfand JM, Joshi A, Shin D, Dey A, Torrigian D, Rader D, et al. A trial to determine the effect of psoriasis treatment (adalimumab, phototherapy, and placebo) on cardiometabolic disease: The vascular inflammation in psoriasis (VIP) trial. Journal of Investigative Dermatology. 2018;138 (5 Supplement 1):S67 . [Google Scholar]
- 56.Gelfand JM, Takeshita J, Dey A, Shin D, Noe M, Fuxench ZC, et al. A Phase IV, randomised, double-blind, placebo-controlled crossover study of the effects of ustekinumab on vascular inflammation in psoriasis (the VIP-U trial). Journal of Investigative Medicine. 2018;66 (3):697 10.1136/jim-2018-000730.1. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Busard CI, Menting SP, van Bezooijen JS, van den Reek JM, Hutten BA, Prens EP, et al. Optimizing adalimumab treatment in psoriasis with concomitant methotrexate (OPTIMAP): study protocol for a pragmatic, single-blinded, investigator-initiated randomized controlled trial.[Erratum appears in Trials. 2017 Mar 7;18(1):113; PMID: 28270175]. Trials2017. p. 52 10.1186/s13063-017-1777-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ikonomidis I, Papadavid E, Makavos G, Andreadou I, Varoudi M, Gravanis K, et al. Lowering Interleukin-12 Activity Improves Myocardial and Vascular Function Compared With Tumor Necrosis Factor-a Antagonism or Cyclosporine in Psoriasis. Circulation Cardiovascular imaging. 2017;10(9). 10.1161/CIRCIMAGING.117.006283 . [DOI] [PubMed] [Google Scholar]
- 59.Bissonnette R, Tardif JC, Harel F, Pressacco J, Bolduc C, Guertin MC. Effects of the tumor necrosis factor-alpha antagonist adalimumab on arterial inflammation assessed by positron emission tomography in patients with psoriasis: results of a randomized controlled trial. Circ Cardiovasc Imaging. 2013;6(1):83–90. 10.1161/CIRCIMAGING.112.975730 . [DOI] [PubMed] [Google Scholar]
- 60.Callis DK, Bagel J, Bukhalo M, Mercado CI, Choi S, Zhao F, et al. Phase 3, open-label, randomized study of the pharmacokinetics, efficacy and safety of ixekizumab following subcutaneous administration using a prefilled syringe or an autoinjector in patients with moderate-to-severe plaque psoriasis (UNCOVER-A). Journal of the european academy of dermatology and venereology: JEADV. 2017;31(1):107–13. 10.1111/jdv.13768 CN-01368719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gordon KB, Langley RG, Leonardi C, Toth D, Menter MA, Kang S, et al. Clinical response to adalimumab treatment in patients with moderate to severe psoriasis: double-blind, randomized controlled trial and open-label extension study. J Am Acad Dermatol. 2006;55(4):598–606. 10.1016/j.jaad.2006.05.027 . [DOI] [PubMed] [Google Scholar]
- 62.Stein Gold L, Bagel J, Lebwohl M, Jackson JM, Chen R, Goncalves J, et al. Efficacy and Safety of Apremilast in Systemic- and Biologic-Naive Patients With Moderate Plaque Psoriasis: 52-Week Results of UNVEIL. Journal of drugs in dermatology: JDD. 2018;17(2):221–8. . [PubMed] [Google Scholar]
- 63.Strober B, Bagel J, Lebwohl M, Stein Gold L, Jackson JM, Chen R, et al. Efficacy and Safety of Apremilast in Patients With Moderate Plaque Psoriasis With Lower BSA: Week 16 Results from the UNVEIL Study. J Drugs Dermatol. 2017;16(8):801–8. . [PubMed] [Google Scholar]
- 64.Papp KA, Reich K., Paul C., Blauvelt A., Baran W., Bolduc C., Toth D., Langley R.G., Cather J., Gottlieb A.B.,Thaci D., Krueger J.G., Russell C.B., Milmont C.E., Li J., Klekotka P.A., Kricorian G., Nirula A. A prospective phase III, randomized, double-blind, placebo-controlled study of brodalumab in patients with moderate-to-severe plaque psoriasis. British Journal of Dermatology. 2016;175:273–86. 10.1111/bjd.14493 [DOI] [PubMed] [Google Scholar]
- 65.Lebwohl M, Strober B, Menter A, Gordon K, Weglowska J, Puig L, et al. Phase 3 Studies Comparing Brodalumab with Ustekinumab in Psoriasis. The New England journal of medicine. 2015;373(14):1318–28. 10.1056/NEJMoa1503824 . [DOI] [PubMed] [Google Scholar]
- 66.Nakagawa H, Niiro H, Ootaki K. Brodalumab, a human anti-interleukin-17-receptor antibody in the treatment of Japanese patients with moderate-to-severe plaque psoriasis: Efficacy and safety results from a phase II randomized controlled study. Journal of Dermatological Science. 2016;81(1):44–52. 10.1016/j.jdermsci.2015.10.009 . [DOI] [PubMed] [Google Scholar]
- 67.Gordon KB, Blauvelt A, Papp KA, Langley RG, Luger T, Ohtsuki M, et al. Phase 3 Trials of Ixekizumab in Moderate-to-Severe Plaque Psoriasis. N Engl J Med. 2016;375(4):345–56. 10.1056/NEJMoa1512711 . [DOI] [PubMed] [Google Scholar]
- 68.Griffiths CE, Reich K, Lebwohl M, van de Kerkhof P, Paul C, Menter A, et al. Comparison of ixekizumab with etanercept or placebo in moderate-to-severe psoriasis (UNCOVER-2 and UNCOVER-3): results from two phase 3 randomised trials. Lancet. 2015;386(9993):541–51. 10.1016/S0140-6736(15)60125-8 . [DOI] [PubMed] [Google Scholar]
- 69.Reich K, Pinter A, Lacour JP, Ferrandiz C, Micali G, French LE, et al. Comparison of ixekizumab with ustekinumab in moderate-to-severe psoriasis: 24-week results from IXORA-S, a phase III study. British Journal of Dermatology. 2017;177(4):1014–23. 10.1111/bjd.15666 . [DOI] [PubMed] [Google Scholar]
- 70.Burkhardt N, Reich K, Lomaga M, Henneges C, Dossenbach M, Wilhelm S, et al. Efficacy and safety of ixekizumab (IXE) compared to ustekinumab (UST) in patients with moderate-tosevere plaque psoriasis: A randomised head-to-head trial. Australasian Journal of Dermatology. 2017;58:43 10.1111/ajd.12652. . [DOI] [Google Scholar]
- 71.Reich K, Pinter A, Leutz A, Henneges C, Schneider E, Schacht A, et al. A randomized, open-label comparison of ixekizumab vs. methotrexate in patients with moderate-to-severe plaque-type psoriasis naive to systemic therapy: Interim analysis of week 12 findings. British Journal of Dermatology. 2017;177 (Supplement 1):61 10.1111/bjd.15426. . [DOI] [Google Scholar]
- 72.Langley RG, Papp K, Gooderham M, Zhang L, Mallinckrodt C, Agada N, et al. Efficacy and safety of continuous every-2-week dosing of ixekizumab over 52 weeks in patients with moderate-to-severe plaque psoriasis in a randomized phase III trial (IXORA-P). British Journal of Dermatology. 2018;178(6):1315–23. 10.1111/bjd.16426 . [DOI] [PubMed] [Google Scholar]
- 73.Khattri S, Goldblum O, Solotkin K, Amir Y, Min MS, Ridenour T, et al. Early onset of clinical improvement with Ixekizumab in a Randomized, open-label study of patients with moderate-to-severe plaque psoriasis. Journal of Clinical and Aesthetic Dermatology. 2018;11(5):33–7. . [PMC free article] [PubMed] [Google Scholar]
- 74.Blauvelt A, Prinz JC, Gottlieb AB, Kingo K, Sofen H, Ruer-Mulard M, et al. Secukinumab administration by pre-filled syringe: efficacy, safety and usability results from a randomized controlled trial in psoriasis (FEATURE). Br J Dermatol. 2015;172(2):484–93. 10.1111/bjd.13348 . [DOI] [PubMed] [Google Scholar]
- 75.Langley RG, Elewski BE, Lebwohl M, Reich K, Griffiths CE, Papp K, et al. Secukinumab in plaque psoriasis—results of two phase 3 trials. N Engl J Med. 2014;371(4):326–38. 10.1056/NEJMoa1314258 . [DOI] [PubMed] [Google Scholar]
- 76.Paul C, Lacour J.P., Tedremets L., Kreutzer K., Jazayeri S., Adams S., Guindon C., You R., Papavassilis C. Efficacy, safety and usability of secukinumab administration by autoinjector/pen in psoriasis: a randomized, controlled trial (JUNCTURE). Journal of European Academy of Dermatology and Venereology. 2015:1082–90. 10.1111/jdv.12751 [DOI] [PubMed] [Google Scholar]
- 77.Mrowietz U, Leonardi CL, Girolomoni G, Toth D, Morita A, Balki SA, et al. Secukinumab retreatment-as-needed versus fixed-interval maintenance regimen for moderate to severe plaque psoriasis: A randomized, double-blind, noninferiority trial (SCULPTURE). J Am Acad Dermatol. 2015;73(1):27–36 e1. 10.1016/j.jaad.2015.04.011 . [DOI] [PubMed] [Google Scholar]
- 78.Thaci D, Blauvelt A, Reich K, Tsai TF, Vanaclocha F, Kingo K, et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate to severe plaque psoriasis: CLEAR, a randomized controlled trial. J Am Acad Dermatol. 2015;73(3):400–9. 10.1016/j.jaad.2015.05.013 . [DOI] [PubMed] [Google Scholar]
- 79.Sticherling M, Mrowietz U, Augustin M, Thaci D, Melzer N, Hentschke C, et al. Secukinumab is superior to fumaric acid esters in treating patients with moderate-to-severe plaque psoriasis who are naive to systemic treatments: results from the randomized controlled PRIME trial. British Journal of Dermatology. 2017;177(4):1024–32. 10.1111/bjd.15707 ; PubMed Central PMCID: PMCincluded. [DOI] [PubMed] [Google Scholar]
- 80.Reich K, Sieder C, Bachhuber T, Melzer N, Sticherling M. PASI 2 corresponds to PASI 90, irrespective of baseline severity: A post-hoc analysis of the PRIME-study. Journal of Investigative Dermatology. 2017;137 (10 Supplement 2):S194 10.1016/j.jid.2017.07.105. . [DOI] [Google Scholar]
- 81.Warren RB, Barker JN, Burden AD, Finlay AY, Hatchard C, Jeffery P, et al. Secukinumab has demonstrated efficacy and safety in hard-to-treat anti-TNFα failure patients from the UK and Republic of Ireland: Results of the SIGNATURE study. Annual Meeting of the American Academy of Dermatology; San-Diego, California2018.
- 82.Bagel J, Nia J, Hashim P, Patekar M, De Vera A, Hugot S, et al. Secukinumab is superior to ustekinumab in clearing skin of patients with moderate-tosevere plaque psoriasis: CLARITY, a randomized, controlled, Phase IIIb trial. Journal of Clinical and Aesthetic Dermatology. 2018;11 (5 Supplement 1):S27–S8. . [Google Scholar]
- 83.Ohtsuki M, Kubo H, Morishima H, Goto R, Zheng R, Nakagawa H. Guselkumab, an anti-interleukin-23 monoclonal antibody, for the treatment of moderate to severe plaque-type psoriasis in Japanese patients: Efficacy and safety results from a phase 3, randomized, double-blind, placebo-controlled study. J Dermatol. 2018;45(9):1053–62. 10.1111/1346-8138.14504 ; PubMed Central PMCID: PMCYes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ferris L, Ott E, Jiang G, Chih-Ho Hong H, Baran W. Efficacy and safety of guselkumab administered with a novel self-injection device for the treatment of moderate-to-severe psoriasis: Results from the phase iii orion self-dose study through week 16. Acta Dermato-Venereologica. 2018;98 (Supplement 219):29 10.2340/00015555-2978. ; PubMed Central PMCID: PMCYes. [DOI] [Google Scholar]
- 85.Blauvelt A, Papp KA, Gooderham M, Langley RG, Leonardi C, Lacour JP, et al. Efficacy and safety of risankizumab, an interleukin-23 inhibitor, in patients with moderate-to-severe chronic plaque psoriasis: 16-week results from the phase III IMMhance trial. British Journal of Dermatology. 2017;177 (5):e248 10.1111/bjd.16059. ; PubMed Central PMCID: PMCincluded. [DOI] [Google Scholar]
- 86.Blauvelt A, Papp KA, Gooderham M, Langley RG, Leonardi C, Lacour JP, et al. Risankizumab efficacy/safety in moderate-to-severe plaque psoriasis: 16-week results from immhance. Acta Dermato-Venereologica. 2018;98 (Supplement 219):30 10.2340/00015555-2978. ; PubMed Central PMCID: PMCYes. [DOI] [Google Scholar]
- 87.Papp K, Thaci D, Reich K, Riedl E, Langley RG, Krueger JG, et al. Tildrakizumab (MK-3222), an anti-interleukin-23p19 monoclonal antibody, improves psoriasis in a phase IIb randomized placebo-controlled trial.[Erratum appears in Br J Dermatol. 2016 Jun;174(6):1426; PMID: 27317290]. British Journal of Dermatology. 2015;173(4):930–9. 10.1111/bjd.13932 . [DOI] [PubMed] [Google Scholar]
- 88.Tsai TF, Ho JC, Song M, Szapary P, Guzzo C, Shen YK, et al. Efficacy and safety of ustekinumab for the treatment of moderate-to-severe psoriasis: a phase III, randomized, placebo-controlled trial in Taiwanese and Korean patients (PEARL). J Dermatol Sci. 2011;63(3):154–63. 10.1016/j.jdermsci.2011.05.005 . [DOI] [PubMed] [Google Scholar]
- 89.Leonardi CL, Kimball AB, Papp KA, Yeilding N, Guzzo C, Wang Y, et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 76-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 1). Lancet. 2008;371(9625):1665–74. 10.1016/S0140-6736(08)60725-4 . [DOI] [PubMed] [Google Scholar]
- 90.Papp KA, Langley RG, Lebwohl M, Krueger GG, Szapary P, Yeilding N, et al. Efficacy and safety of ustekinumab, a human interleukin-12/23 monoclonal antibody, in patients with psoriasis: 52-week results from a randomised, double-blind, placebo-controlled trial (PHOENIX 2). Lancet. 2008;371(9625):1675–84. 10.1016/S0140-6736(08)60726-6 . [DOI] [PubMed] [Google Scholar]
- 91.Zhu X, Zheng M, Song M, Shen YK, Chan D, Szapary PO, et al. Efficacy and safety of ustekinumab in Chinese patients with moderate to severe plaque-type psoriasis: results from a phase 3 clinical trial (LOTUS). J Drugs Dermatol. 2013;12(2):166–74. . [PubMed] [Google Scholar]
- 92.Igarashi A, Kato T, Kato M, Song M, Nakagawa H, Japanese Ustekinumab Study G. Efficacy and safety of ustekinumab in Japanese patients with moderate-to-severe plaque-type psoriasis: long-term results from a phase 2/3 clinical trial. J Dermatol. 2012;39(3):242–52. 10.1111/j.1346-8138.2011.01347.x . [DOI] [PubMed] [Google Scholar]
- 93.Saurat JH, Stingl G, Dubertret L, Papp K, Langley RG, Ortonne JP, et al. Efficacy and safety results from the randomized controlled comparative study of adalimumab vs. methotrexate vs. placebo in patients with psoriasis (CHAMPION). Br J Dermatol. 2008;158(3):558–66. 10.1111/j.1365-2133.2007.08315.x . [DOI] [PubMed] [Google Scholar]
- 94.Goldminz AM, Suarez-Farinas M, Wang AC, Dumont N, Krueger JG, Gottlieb AB. CCL20 and IL22 Messenger RNA Expression After Adalimumab vs Methotrexate Treatment of Psoriasis: A Randomized Clinical Trial. JAMA dermatology. 2015;151(8):837–46. 10.1001/jamadermatol.2015.0452 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Cai L, Gu J, Zheng J, Zheng M, Wang G, Xi L, et al. Efficacy and safety of adalimumab in Chinese patients with moderate-to-severe plaque psoriasis: results from a phase 3, randomized, placebo-controlled, double-blind study. Journal of the european academy of dermatology and venereology: JEADV. 2017;31(1):89–95. 10.1111/jdv.13746 CN-01368717; PubMed Central PMCID: PMCincluded. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Menter A, Tyring SK, Gordon K, Kimball AB, Leonardi CL, Langley RG, et al. Adalimumab therapy for moderate to severe psoriasis: A randomized, controlled phase III trial. J Am Acad Dermatol. 2008;58(1):106–15. 10.1016/j.jaad.2007.09.010 . [DOI] [PubMed] [Google Scholar]
- 97.Asahina A, Nakagawa H, Etoh T, Ohtsuki M, Adalimumab MSG. Adalimumab in Japanese patients with moderate to severe chronic plaque psoriasis: efficacy and safety results from a Phase II/III randomized controlled study. J Dermatol. 2010;37(4):299–310. 10.1111/j.1346-8138.2009.00748.x . [DOI] [PubMed] [Google Scholar]
- 98.Gordon KB, Duffin KC, Bissonnette R, Prinz JC, Wasfi Y, Li S, et al. A Phase 2 Trial of Guselkumab versus Adalimumab for Plaque Psoriasis. New England Journal of Medicine. 2015;373(2):136–44. 10.1056/NEJMoa1501646 . [DOI] [PubMed] [Google Scholar]
- 99.Lebwohl M, Blauvelt A, Paul C, Sofen H, Weglowska J, Piguet V, et al. Certolizumab pegol for the treatment of chronic plaque psoriasis: Results through 48 weeks of a phase 3, multicenter, randomized, double-blind, etanercept- and placebo-controlled study (CIMPACT). Journal of the American Academy of Dermatology. 2018;79(2):266–76.e5. 10.1016/j.jaad.2018.04.013 ; PubMed Central PMCID: PMCYes. [DOI] [PubMed] [Google Scholar]
- 100.Gottlieb AB, Blauvelt A, Thaci D, Leonardi CL, Poulin Y, Drew J, et al. Certolizumab pegol for the treatment of chronic plaque psoriasis: Results through 48 weeks from 2 phase 3, multicenter, randomized, double-blinded, placebo-controlled studies (CIMPASI-1 and CIMPASI-2). Journal of the American Academy of Dermatology. 2018;79(2):302–14.e6. 10.1016/j.jaad.2018.04.012 ; PubMed Central PMCID: PMCYes. [DOI] [PubMed] [Google Scholar]
- 101.Reich K, Ortonne JP, Gottlieb AB, Terpstra IJ, Coteur G, Tasset C, et al. Successful treatment of moderate to severe plaque psoriasis with the PEGylated Fab certolizumab pegol: Results of a phase II randomized, placebo-controlled trial with a re-treatment extension. British Journal of Dermatology. 2012;167(1):180–90. 10.1111/j.1365-2133.2012.10941.x ; PubMed Central PMCID: PMCYes. [DOI] [PubMed] [Google Scholar]
- 102.Leonardi CL, Powers JL, Matheson RT, Goffe BS, Zitnik R, Wang A, et al. Etanercept as monotherapy in patients with psoriasis. N Engl J Med. 2003;349(21):2014–22. 10.1056/NEJMoa030409 . [DOI] [PubMed] [Google Scholar]
- 103.Gottlieb AB, Matheson RT, Lowe N, Krueger GG, Kang S, Goffe BS, et al. A randomized trial of etanercept as monotherapy for psoriasis. Archives of dermatology. 2003;139(12):1627–32; discussion 32. 10.1001/archderm.139.12.1627 . [DOI] [PubMed] [Google Scholar]
- 104.Papp KA, Tyring S, Lahfa M, Prinz J, Griffiths CE, Nakanishi AM, et al. A global phase III randomized controlled trial of etanercept in psoriasis: safety, efficacy, and effect of dose reduction. Br J Dermatol. 2005;152(6):1304–12. 10.1111/j.1365-2133.2005.06688.x . [DOI] [PubMed] [Google Scholar]
- 105.Van de Kerkhof PCM, Segaert S., Lahfa M., Luger T.A., Karolyi Z.,§ Kaszuba A., Leigheb G., Camacho F.M., Forsea D., Zang C., Boussuge M.P., Paolozzi L. and Wajdula J. Once weekly administration of etanercept 50 mg is efficacious and well tolerated in patients with moderate-to-severe plaque psoriasis: a randomized controlled trial with open-label extension. British Journal of Dermatology. 2008;(159):1177–85. [DOI] [PubMed] [Google Scholar]
- 106.Bagel J, Lynde C, Tyring S, Kricorian G, Shi Y, Klekotka P. Moderate to severe plaque psoriasis with scalp involvement: a randomized, double-blind, placebo-controlled study of etanercept. J Am Acad Dermatol. 2012;67(1):86–92. 10.1016/j.jaad.2011.07.034 . [DOI] [PubMed] [Google Scholar]
- 107.Bachelez H, van de Kerkhof PC, Strohal R, Kubanov A, Valenzuela F, Lee JH, et al. Tofacitinib versus etanercept or placebo in moderate-to-severe chronic plaque psoriasis: a phase 3 randomised non-inferiority trial. Lancet. 2015;386(9993):552–61. 10.1016/S0140-6736(14)62113-9 . [DOI] [PubMed] [Google Scholar]
- 108.Tyring S, Gottlieb A, Papp K, Gordon K, Leonardi C, Wang A, et al. Etanercept and clinical outcomes, fatigue, and depression in psoriasis: double-blind placebo-controlled randomised phase III trial. Lancet. 2006;367(9504):29–35. 10.1016/S0140-6736(05)67763-X . [DOI] [PubMed] [Google Scholar]
- 109.Strohal R, Puig L, Chouela E, Tsai TF, Melin J, Freundlich B, et al. The efficacy and safety of etanercept when used with as-needed adjunctive topical therapy in a randomised, double-blind study in subjects with moderate-to-severe psoriasis (the PRISTINE trial). J Dermatolog Treat. 2013;24(3):169–78. 10.3109/09546634.2012.658015 . [DOI] [PubMed] [Google Scholar]
- 110.Gottlieb AB, Leonardi C., Kerdel F., Mehlis S., Olds M. and Williams D.A. Efficacy and safety of briakinumab vs. etanercept and placebo in patients with moderate to severe chronic plaque psoriasis. British Journal of Dermatology. 2011;165:652–60. 10.1111/j.1365-2133.2011.10418.x [DOI] [PubMed] [Google Scholar]
- 111.Strober BE, Crowley JJ, Yamauchi PS, Olds M, Williams DA. Efficacy and safety results from a phase III, randomized controlled trial comparing the safety and efficacy of briakinumab with etanercept and placebo in patients with moderate to severe chronic plaque psoriasis. Br J Dermatol. 2011;165(3):661–8. 10.1111/j.1365-2133.2011.10419.x . [DOI] [PubMed] [Google Scholar]
- 112.de Vries AC, Thio HB, de Kort WJ, Opmeer BC, van der Stok HM, de Jong EM, et al. A prospective randomised controlled trial comparing infliximab and etanercept in patients with moderate to severe chronic plaque type psoriasis Psoriasis Infliximab versus Etanercept Comparison Evaluation, the PIECE study. Br J Dermatol. 2016. 10.1111/bjd.14867 . [DOI] [PubMed] [Google Scholar]
- 113.Griffiths CE, Strober BE, van de Kerkhof P, Ho V, Fidelus-Gort R, Yeilding N, et al. Comparison of ustekinumab and etanercept for moderate-to-severe psoriasis. N Engl J Med. 2010;362(2):118–28. 10.1056/NEJMoa0810652 . [DOI] [PubMed] [Google Scholar]
- 114.Caproni M, Antiga E, Melani L, Volpi W, Del Bianco E, Fabbri P. Serum levels of IL-17 and IL-22 are reduced by etanercept, but not by acitretin, in patients with psoriasis: a randomized-controlled trial. Journal of clinical immunology. 2009;29(2):210–4. 10.1007/s10875-008-9233-0 . [DOI] [PubMed] [Google Scholar]
- 115.Gisondi P, Del Giglio M, Cotena C, Girolomoni G. Combining etanercept and acitretin in the therapy of chronic plaque psoriasis: a 24-week, randomized, controlled, investigator-blinded pilot trial. Br J Dermatol. 2008;158(6):1345–9. 10.1111/j.1365-2133.2008.08564.x . [DOI] [PubMed] [Google Scholar]
- 116.Yang HZ, Wang K, Jin HZ, Gao TW, Xiao SX, Xu JH, et al. Infliximab monotherapy for Chinese patients with moderate to severe plaque psoriasis: a randomized, double-blind, placebo-controlled multicenter trial. Chinese medical journal. 2012;125(11):1845–51. . [PubMed] [Google Scholar]
- 117.Reich K, Nestle FO, Papp K, Ortonne JP, Evans R, Guzzo C, et al. Infliximab induction and maintenance therapy for moderate-to-severe psoriasis: a phase III, multicentre, double-blind trial. Lancet. 2005;366(9494):1367–74. 10.1016/S0140-6736(05)67566-6 . [DOI] [PubMed] [Google Scholar]
- 118.Chaudhari U, Romano P, Mulcahy LD, Dooley LT, Baker DG, Gottlieb AB. Efficacy and safety of infliximab monotherapy for plaque-type psoriasis: a randomised trial. Lancet. 2001;357(9271):1842–7. 10.1016/s0140-6736(00)04954-0 . [DOI] [PubMed] [Google Scholar]
- 119.Gottlieb AB MD, PhD, Evans Robert, PharmD., Li Shu MS., Dooley Lisa T. DrPH., Guzzo Cynthia A.MD., Baker DanielMD., Bala aPhD., Marano Colleen W.PhD., Menter AlanMD. Infliximab induction therapy for patients with severe plaque-type psoriasis: A randomized, double-blind, placebo-controlled trial. Journal American Academy of Dermatology. 2004;51(4):534–42. 10.1016/j.jaad.2004.02.021 [DOI] [PubMed] [Google Scholar]
- 120.Menter A, Feldman SR, Weinstein GD, Papp K, Evans R, Guzzo C, et al. A randomized comparison of continuous vs. intermittent infliximab maintenance regimens over 1 year in the treatment of moderate-to-severe plaque psoriasis. J Am Acad Dermatol. 2007;56(1):31 e1–15. 10.1016/j.jaad.2006.07.017 . [DOI] [PubMed] [Google Scholar]
- 121.Torii H, Nakagawa H, Japanese Infliximab Study i. Infliximab monotherapy in Japanese patients with moderate-to-severe plaque psoriasis and psoriatic arthritis. A randomized, double-blind, placebo-controlled multicenter trial. J Dermatol Sci. 2010;59(1):40–9. 10.1016/j.jdermsci.2010.04.014 . [DOI] [PubMed] [Google Scholar]
- 122.Barker J, Hoffmann M, Wozel G, Ortonne JP, Zheng H, van Hoogstraten H, et al. Efficacy and safety of infliximab vs. methotrexate in patients with moderate-to-severe plaque psoriasis: results of an open-label, active-controlled, randomized trial (RESTORE1). Br J Dermatol. 2011;165(5):1109–17. 10.1111/j.1365-2133.2011.10615.x . [DOI] [PubMed] [Google Scholar]
- 123.Papp K, Cather JC, Rosoph L, Sofen H, Langley RG, Matheson RT, et al. Efficacy of apremilast in the treatment of moderate to severe psoriasis: a randomised controlled trial. Lancet. 2012;380(9843):738–46. 10.1016/S0140-6736(12)60642-4 . [DOI] [PubMed] [Google Scholar]
- 124.Papp K, Reich K, Leonardi CL, Kircik L, Chimenti S, Langley RG, et al. Apremilast, an oral phosphodiesterase 4 (PDE4) inhibitor, in patients with moderate to severe plaque psoriasis: Results of a phase III, randomized, controlled trial (Efficacy and Safety Trial Evaluating the Effects of Apremilast in Psoriasis [ESTEEM] 1). J Am Acad Dermatol. 2015;73(1):37–49. 10.1016/j.jaad.2015.03.049 . [DOI] [PubMed] [Google Scholar]
- 125.Paul C, Cather J, Gooderham M, Poulin Y, Mrowietz U, Ferrandiz C, et al. Efficacy and safety of apremilast, an oral phosphodiesterase 4 inhibitor, in patients with moderate-to-severe plaque psoriasis over 52 weeks: a phase III, randomized controlled trial (ESTEEM 2). Br J Dermatol. 2015;173(6):1387–99. 10.1111/bjd.14164 . [DOI] [PubMed] [Google Scholar]
- 126.Papp KA, Kaufmann R, Thaci D, Hu C, Sutherland D, Rohane P. Efficacy and safety of apremilast in subjects with moderate to severe plaque psoriasis: results from a phase II, multicenter, randomized, double-blind, placebo-controlled, parallel-group, dose-comparison study. J Eur Acad Dermatol Venereol. 2013;27(3):e376–83. 10.1111/j.1468-3083.2012.04716.x . [DOI] [PubMed] [Google Scholar]
- 127.Ohtsuki M, Okubo Y, Komine M, Imafuku S, Day R, Chen P, et al. Apremilast, an oral phosphodiesterase 4 inhibitor, in the treatment of Japanese patients with moderate to severe plaque psoriasis: efficacy, safety and tolerability results from a phase 2b randomized controlled trial. J Dermatol. 2017;(no pagination). 10.1111/1346-8138.13829 CN-01365837; PubMed Central PMCID: PMC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Reich K, Gooderham M, Green L, Bewley A, Zhang Z, Khanskaya I, et al. The efficacy and safety of apremilast, etanercept and placebo in patients with moderate-to-severe plaque psoriasis: 52-week results from a phase IIIb, randomized, placebo-controlled trial (LIBERATE). Journal of the european academy of dermatology and venereology: JEADV. 2017;31(3):507–17. 10.1111/jdv.14015 CN-01413768; PubMed Central PMCID: PMC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Reich K, Soung J, Gooderham M, Zhang Z, Nograles K, Goodfield M. Sustained efficacy of apremilast in patients with moderate to severe psoriasis who continued on apremilast or switched from etanercept treatment: 52-week results from the LIBERATE study. Journal of the American Academy of Dermatology. 2016;1):AB276 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Lebwohl M, Mark Jackson J, Bagel J, Levi E, Weaver J, Gold LS, et al. Examining disease severity and symptom improvement with patient and physician assessments: Results from a phase iv analysis of apremilast in patients with moderate plaque psoriasis. Acta Dermato-Venereologica. 2018;98 (Supplement 219):14 10.2340/00015555-2978. ; PubMed Central PMCID: PMCYes. [DOI] [PubMed] [Google Scholar]
- 131.Mrowietz U, Szepietowski J, Loewe R, Kerkhof P, Lamarca R, Ocker W, et al. Efficacy and safety of LAS41008 (dimethyl fumarate) in adults with moderate-to-severe chronic plaque psoriasis: a randomized, double-blind, Fumaderm®—and placebo-controlled trial (BRIDGE). British journal of dermatology. 2017;176(3):615–23. 10.1111/bjd.14947 CN-01413968; PubMed Central PMCID: PMC [DOI] [PubMed] [Google Scholar]
- 132.de Vries AC, Thio HB, de Kort WJ, Opmeer BC, van der Stok HM, de Jong EM, et al. A prospective randomized controlled trial comparing infliximab and etanercept in patients with moderate-to-severe chronic plaque-type psoriasis: the Psoriasis Infliximab vs. Etanercept Comparison Evaluation (PIECE) study. British Journal of Dermatology. 2017;176(3):624–33. 10.1111/bjd.14867 . [DOI] [PubMed] [Google Scholar]
- 133.Ortonnne JP, Tasset C, Reich K, Sterry W. Safety and efficacy of subcutaneous certolizumab pegol, a new anti-TNFa monoclonal antibody, in patients with moderate-to-severe chronic plaque psoriasis: preliminary results from a double-blind, placebo-controlled trial Abstract P21. American Academy of Dermatology 65th Annual Meeting February 2–6, 2007. Journal of the american academy of dermatology. 2007;56(2):Ab6. CN-00615995. [Google Scholar]
- 134.Zhu Y, Marini JC, Wasfi Y, Randazzo B, Shen YK, Li S, et al. Antibodies to guselkumab are not associated with reduction in clinical response or development of injection-site reactions in patients with moderateto- severe plaque psoriasis. British Journal of Dermatology. 2017;177 (5):e274 10.1111/bjd.16059. . [DOI] [Google Scholar]
- 135.Reich K, Papp K, Armstrong AW, Wasfi Y, Jiang G, Shen YK, et al. Safety of guselkumab in patients with plaque psoriasis through 2 years: A pooled analysis from VOYAGE 1 VOYAGE 2. British Journal of Dermatology. 2017;177 (5):e297 10.1111/bjd.16059. . [DOI] [PubMed] [Google Scholar]
- 136.Foley P, Song M, Shen YK, You Y, Wasfi Y, Griffiths CEM. Guselkumab treatment provided higher frequency of complete skin clearance compared with adalimumab treatment among patients with moderate-to-severe plaque psoriasis. British Journal of Dermatology. 2017;177 (5):e273–e4. 10.1111/bjd.16059. . [DOI] [Google Scholar]
- 137.Mason KJ, Barker JNWN, Smith CH, Hampton PJ, Lunt M, McElhone K, et al. A real-world comparison of effectiveness and safety outcomes between clinical trial-eligible and -ineligible patients in the British Association of Dermatologists Biologic Interventions Register (BADBIR). British Journal of Dermatology. 2017;177 (5):e273 10.1111/bjd.16059. . [DOI] [Google Scholar]
- 138.Paul C, Van De Kerkhof P, Dutronc Y, Henneges C, Dossenbach M, Hollister K, et al. 52-Week results from IXORA-S: A randomized head-to-head trial of ixekizumab and ustekinumab in patients with moderate-to-severe plaque psoriasis. British Journal of Dermatology. 2017;177 (5):e293 10.1111/bjd.16059. . [DOI] [PubMed] [Google Scholar]
- 139.Yiu Z, Smith C, Ashcroft D, Lunt M, Walton S, Murphy R, et al. Infliximab is associated with an increased risk of serious infection in patients with psoriasis: Results from the British Association of Dermatologists Biologic Interventions Register (BADBIR). British Journal of Dermatology. 2017;177 (5):e289–e90. 10.1111/bjd.16059. . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Bissonnette R, Luger T, Thaci D, Toth D, Lacombe A, Xia S, et al. Secukinumab demonstrates high sustained efficacy and a favourable safety profile through 5 years of treatment in moderate-to-severe psoriasis. British Journal of Dermatology. 2017;177 (5):e289 10.1111/bjd.16059. ; PubMed Central PMCID: PMCincluded. [DOI] [Google Scholar]
- 141.Frieder J, Kivelevitch D, Fiore CT, Saad S, Menter A. The impact of biologic agents on health-related quality of life outcomes in patients with psoriasis. Expert Review of Clinical Immunology. 2018;14(1):1–19. 10.1080/1744666X.2018.1401468 . [DOI] [PubMed] [Google Scholar]
- 142.Martinez-Vinson C, Courbette O, Aupiais C, Viala J, Hugot JP. Infliximab induced psoriasis in a cohort of children with inflammatory bowel disease: aaaa 12 years follow-up study. Journal of Pediatric Gastroenterology and Nutrition. 2017;65 (Supplement 1):S53–S4. 10.1097/MPG.0000000000001744. . [DOI] [PubMed] [Google Scholar]
- 143.Braun J, Baraliakos X, Deodhar A, Baeten D, Sieper J, Emery P, et al. Effect of secukinumab on clinical and radiographic outcomes in ankylosing spondylitis: 2-year results from the randomised phase III MEASURE 1 study. Annals of the Rheumatic Diseases. 2017;76(6):1070–7. 10.1136/annrheumdis-2016-209730 . [DOI] [PubMed] [Google Scholar]
- 144.Papp K, Bachelez H, Costanzo A, Foley P, Gooderham M, Kaur P, et al. Clinical similarity of the biosimilar ABP 501 compared with adalimumab after single transition: Long-term results from a randomized controlled, double-blind, 52-week, phase III trial in patients with moderate-to-severe plaque psoriasis. British Journal of Dermatology. 2017. 10.1111/bjd.15857. . [DOI] [PubMed] [Google Scholar]
- 145.Duarte A, Mebrahtu T, Goncalves PS, Harden M, Murphy R, Palmer S, et al. Adalimumab, etanercept and ustekinumab for treating plaque psoriasis in children and young people: Systematic review and economic evaluation. Health Technology Assessment. 2017;21(64):1–243. 10.3310/hta21640 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Guenther L, Warren RB, Cather JC, Sofen H, Poulin Y, Lebwohl M, et al. Impact of ixekizumab treatment on skin-related personal relationship difficulties in moderate-to-severe psoriasis patients: 12-week results from two Phase 3 trials. Journal of the European Academy of Dermatology and Venereology. 2017;31(11):1867–75. 10.1111/jdv.14377 . [DOI] [PubMed] [Google Scholar]
- 147.Mease PJ, McInnes IB, Reich K. Consistent safety and tolerability of secukinumab over long-term exposure in patients with active psoriatic arthritis and moderate to severe plaque psoriasis: Updated pooled safety analyses. Rheumatology (United Kingdom). 2017;56 (Supplement 2):ii78–ii9. 10.1093/rheumatology/kex062. . [DOI] [Google Scholar]
- 148.Geng W, Zhao J, Fu J, Zhang H, Qiao S. Efficacy of several biological therapies for treating moderate to severe psoriasis: A network meta‑analysis. Experimental and therapeutic medicine. 2018;16(6):5085–95. 10.3892/etm.2018.6859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Loos AM, Liu S, Segel C, Ollendorf D, Pearson SD, Linder JA. Comparative effectiveness of targeted immunomodulators for the treatment of moderate-to-severe plaque psoriasis: A systematic review and network meta-analysis. Value in Health. 2017;20 (5):A210 . [DOI] [PubMed] [Google Scholar]
- 150.Lv J, Zhou D, Wang Y, Zhao J, Chen Z, Zhang J, et al. Quantitative evaluation to efficacy and safety of therapies for psoriasis: A network meta-analysis. Molecular Pain. 2018;14:1744806918762205 10.1177/1744806918762205 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Sawyer L, Fotheringham I, Wright E, Yasmeen N, Gibbons C, Holmen Møller A. The comparative efficacy of brodalumab in patients with moderate-to-severe psoriasis: a systematic literature review and network meta-analysis. Journal of Dermatological Treatment. 2018:1–12. 10.1080/09546634.2018.1427205 [DOI] [PubMed] [Google Scholar]
- 152.Bewley AP, Shear NH, Calzavara-Pinton PG, Hansen JB, Nyeland ME, Signorovitch J. Calcipotriol plus betamethasone dipropionate aerosol foam vs. apremilast, methotrexate, acitretin or fumaric acid esters for the treatment of plaque psoriasis: a matching-adjusted indirect comparison. Journal of the European Academy of Dermatology and Venereology. 2019;0(0). 10.1111/jdv.15369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Hendrix N, Ollendorf DA, Chapman RH, Loos A, Liu S, Kumar V, et al. Cost-Effectiveness of Targeted Pharmacotherapy for Moderate to Severe Plaque Psoriasis. Journal of Managed Care & Specialty Pharmacy. 2018;24(12):1210–7. 10.18553/jmcp.2018.24.12.1210 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Ellis AG, Flohr C, Drucker AM. Network meta-analyses of systemic treatments for psoriasis: a critical appraisal. British Journal of Dermatology. 2019;180(2):282–8. 10.1111/bjd.17335 [DOI] [PubMed] [Google Scholar]
- 155.Tausend W, Downing C, Tyring S. Systematic review of interleukin-12, interleukin-17, and interleukin-23 pathway inhibitors for the treatment of moderate-to-severe chronic plaque psoriasis: Ustekinumab, briakinumab, tildrakizumab, guselkumab, secukinumab, ixekizumab, and brodalumab. Journal of Cutaneous Medicine and Surgery. 2014;18(3):156–69. 10.2310/7750.2013.13125 ; PubMed Central PMCID: PMCincluded. [DOI] [PubMed] [Google Scholar]
- 156.Bilal J, Berlinberg A, Bhattacharjee S, Trost J, Riaz IB, Kurtzman DJB. A systematic review and meta-analysis of the efficacy and safety of the interleukin (IL)-12/23 and IL-17 inhibitors ustekinumab, secukinumab, ixekizumab, brodalumab, guselkumab and tildrakizumab for the treatment of moderate to severe plaque psoriasis. Journal of Dermatological Treatment. 2018;29(6):569–78. 10.1080/09546634.2017.1422591 [DOI] [PubMed] [Google Scholar]
- 157.Cui L, Chen R, Subedi S, Yu Q, Gong Y, Chen Z, et al. Efficacy and safety of biologics targeting IL-17 and IL-23 in the treatment of moderate-to-severe plaque psoriasis: A systematic review and meta-analysis of randomized controlled trials. International Immunopharmacology. 2018;62:46–58. 10.1016/j.intimp.2018.06.020 [DOI] [PubMed] [Google Scholar]
- 158.Cipriani A, Higgins JT, Geddes JR, Salanti G. Conceptual and technical challenges in network meta-analysis. Annals of Internal Medicine. 2013;159(2):130–7. 10.7326/0003-4819-159-2-201307160-00008 [DOI] [PubMed] [Google Scholar]
- 159.Mills EJ, Thorlund K, Ioannidis JPA. Demystifying trial networks and network meta-analysis. BMJ: British Medical Journal. 2013;346 10.1136/bmj.f2914 [DOI] [PubMed] [Google Scholar]
- 160.Higgins J GS. Cochrane handbook for systematic reviews of interventions Version 5.1. 0. The Cochrane Collaboration 2011 [5 July 2018]. Available from: www.handbook.cochrane.org.
- 161.CRD. CRD’s guidance for undertaking reviews in health care Centre for Reviews and Dissemination. University of York; 2009.
- 162.EMA. Kyntheum. Summary of Product Characteristics.: European Medicines Agency; 2017 [5 July 2018]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003959/WC500232913.pdf.
- 163.EMA. Otezla. Summary of Product Characteristics.: European Medicines Agency; 2017 [5 July 2018]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003746/WC500182627.pdf.
- 164.EMA. Enbrel. Summary of Product Characteristics.: European Medicines Agency; 2018 [5 July 2018]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000262/WC500027361.pdf.
- 165.EMA. Tremfya. Summary of Product Characteristics. 2017 [5 July 2018]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/004271/WC500239623.pdf.
- 166.EMA. Remicade. Summary of Product Characteristics.: European Medicines Agency; 1999 [5 July 2018]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000240/WC500050888.pdf.
- 167.EMA. Taltz. Summary of Product Characteristics.: European Medicines Agency; 2008 [5 July 2018]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003943/WC500205804.pdf.
- 168.EMA. Cosentyx. Summary of Product Characteristics.: European Medicines Agency; 2018 [5 July 2018]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/003729/WC500183129.pdf.
- 169.EMA. Stelara. Summary of Product Characteristics.: European Medicines Agency; 2018 [5 July 2018]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/000958/WC500058513.pdf.
- 170.EMA. Skilarence. Summary of Product Characteristics.: European Medicines Agency; 2017 [5 July 2018]. Available from: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002157/WC500231107.pdf.
- 171.EMA. Humira (adalimumab): European Medicines Agency; 2019 [11 January 2019]. Available from: https://www.ema.europa.eu/en/medicines/human/EPAR/humira#product-information-section.
- 172.EMA. Cimzia. Opinion.: European Medicines Agency; 2018 [5 July 2018]. Available from: http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/001037/smops/Positive/human_smop_001292.jsp&mid=WC0b01ac058001d127.
- 173.Gómez-García F, Epstein D, Isla-Tejera B, Lorente A, Vélez García-Nieto A, Ruano J. Short-term efficacy and safety of new biological agents targeting the interleukin-23–T helper 17 pathway for moderate-to-severe plaque psoriasis: a systematic review and network meta-analysis. British Journal of Dermatology. 2017;176(3):594–603. 10.1111/bjd.14814 [DOI] [PubMed] [Google Scholar]
- 174.Blauvelt A, Reich K, Tsai T, Tyring S, Vanaclocha F, Kingo K, et al. Secukinumab is superior to ustekinumab in clearing skin of subjects with moderate-to-severe plaque psoriasis up to 1 year: results from the CLEAR study. Journal of the american academy of dermatology. 2017;76(1):60–9.e9. 10.1016/j.jaad.2016.08.008 CN-01368612; PubMed Central PMCID: PMCincluded. [DOI] [PubMed] [Google Scholar]
- 175.Paul C, Griffiths CEM, van de Kerkhof PCM, Puig L, Dutronc Y, Henneges C, et al. Ixekizumab provides superior efficacy compared with ustekinumab over 52 weeks of treatment: Results from IXORA-S, a phase 3 study. Journal of the American Academy of Dermatology. 2019;80(1):70–9.e3. 10.1016/j.jaad.2018.06.039 [DOI] [PubMed] [Google Scholar]
- 176.Sawyer L, Fotheringham I, Cornic L, Yasmeen N, Jemec G, Levin L, et al. Assessing the longer-term efficacy of biologic therapies and apremilast for patients with moderate-to-severe psoriasis: A systematic review and network meta-analysis. Value in Health. 2017;20 (9):A801 10.1016/j.jval.2017.08.2380. . [DOI] [Google Scholar]
- 177.Manalo IF, Gilbert KE, Wu JJ. Time to Raise the Bar to Psoriasis Area Severity Index 90 and 100. J Drugs Dermatol. 2015;14(10):1086–8. [PubMed] [Google Scholar]
- 178.Puig L. PASI 90 response: the new standard in therapeutic efficacy for psoriasis. Journal of the European Academy of Dermatology and Venereology. 2015;29(4):645–8. 10.1111/jdv.12817 [DOI] [PubMed] [Google Scholar]
- 179.Puig L, Thom H, Mollon P, Tian H, Ramakrishna GS. Clear or almost clear skin improves the quality of life in patients with moderate-to-severe psoriasis: a systematic review and meta-analysis. Journal of the European Academy of Dermatology and Venereology. 2017;31(2):213–20. 10.1111/jdv.14007 [DOI] [PubMed] [Google Scholar]
- 180.Elewski B, Puig L, Mordin M, Gilloteau I, Sherif B, Fox T, et al. Psoriasis patients with psoriasis Area and Severity Index (PASI) 90 response achieve greater health-related quality-of-life improvements than those with PASI 75–89 response: results from two phase 3 studies of secukinumab. Journal of dermatological treatment. 2017;28(6):492–9. 10.1080/09546634.2017.1294727 CN-01443627. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(XLSX)
(DOCX)
(XLSX)
(XLSX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.