Abstract
Racial/ethnic minority populations underutilize mental health services, even in the presence of psychiatric disorder, and differences in perceived need may contribute to these disparities. Using the Collaborative Psychiatric Epidemiology Surveys, we assessed how the intersections of race/ethnicity, gender, and socioeconomic status affect perceived need. We analyzed a nationally representative sample of U.S. adults (18 years or older; N=14,906), including non-Latino whites, Asian Americans, Latinos, African Americans, and Afro-Caribbeans. Logistic regressions were estimated for the total sample, a clinical need subsample (meets lifetime diagnostic criteria), and a no disorder subsample. Perceived need varies by gender and nativity, but these patterns are conditional on race/ethnicity. Men are less likely than women to have a perceived need but only among non-Latino whites and African Americans. Foreign-born immigrants have lower perceived need than U.S.-born persons, only among Asian Americans. Intersectional approaches to understanding perceived need may help uncover social processes that lead to disparities in mental health care.
Introduction
Consistent variation in mental health services utilization across social strata can be indicative of mental health care disparities when these differences are due to access barriers and persist net of need for services. The limited use of services among racial/ethnic minority groups relative to non-Latino whites is of critical concern because these disparities remain even after adjusting for mental health need and other dimensions of social status (e.g., Abe-Kim, Takeuchi, Hong et al. 2007, Alegría, Canino, Ríos et al. 2002, Alegría, Chatterji, Wells et al. 2008, Jackson, Neighbors, Torres et al. 2007, Neighbors, Caldwell, Williams et al. 2007). Existing research on mental health care disparities examines the role of policies, provider practices, and differential access, often overlooking attitudes and perceptions about mental illness and its treatment. The presence of a psychiatric disorder, a commonly used but imperfect indicator of need for services (Druss, Wang, Sampson et al. 2007, Mechanic 2003, Tuithof, Have, Brink et al. 2016), is a major influence on help-seeking behaviors (Alegría, Mulvaney-Day, Woo et al. 2007, Jang, Yoon, Chiriboga et al. 2015, Wang, Lane, Olfson et al. 2005). Nevertheless, many persons with psychiatric disorders, including serious mental illness, do not self-label as having a disorder, much less one that requires treatment (Kessler, Berglund, Bruce et al. 2001, Mojtabai, Olfson, Sampson et al. 2011). Perceiving a need for mental health care, an element of the self-labeling process, is a pivotal precursor to voluntary help-seeking (Mojtabai, Olfson and Mechanic 2002, Mojtabai et al. 2011, Narendorf and Palmer 2016) and is thought to contribute to racial/ethnic disparities in mental health care utilization (Nadeem, Lange and Miranda 2009), but little is known about the social distribution of perceived need, especially between and within racial/ethnic groups. The current study examines perceived need as a type of self-labeling and the extent to which it varies across lines of social demarcation, focusing on the intersections of race/ethnicity with two other status characteristics with strong links to both mental health and treatment—gender and socioeconomic status (SES).
Perceived Need for Mental Health Care
We conceptualize perceived need for mental health care as a person’s awareness that something is wrong, that what is wrong relates to his or her mental health, and that professional assistance is necessary to overcome it. This perception figures prominently in sociological theories about help-seeking. The widely used Behavioral Model of Health Services Use, for example, posits three main influences on help-seeking behavior: predisposing characteristics, enabling factors, and need, which includes not only actual (biological/clinical) need but also perceived need (Andersen and Davidson 2007). Correspondingly, perceived need is a key element of mental illness career models (Aneshensel 2013, Karp 1996), self-labeling theory (Thoits 1985, Thoits 2005), and the network-episode model, which describes the impact of social support systems and treatment systems on how individuals view their mental health and whether they see themselves as requiring help (Pescosolido, Boyer and Medina 2013).
Perceived need is conceptualized here as an element of self-labeling theory (Thoits 1985, Thoits 2005), which seeks to explain how individuals perceive and label their mental health problems. This theory posits that individuals experiencing significant emotional distress are likely to recognize that their psychological problems require professional treatment; this self-labeling process then motivates individuals to voluntarily seek help or treatment, although not all do so, and in some cases “voluntary” treatment may not be entirely voluntary (Thoits 2011, Thoits 2005). As summarized by Moses (2009), Thoits (1985) asserts that three criteria are necessary for self-labeling to occur: (1) The individual is assumed to be a well-socialized actor who shares the cultural perspectives of others and understands normative expectations; (2) norms about acceptable behaviors are clear, known, and can be applied to oneself or others; and (3) the individual is motivated to conform to social expectations. As such, self-labeling requires the individual to have “knowledge of and acceptance of basic psychological dynamics that underlie the etiology of mental disorder” (p. 105) and sufficient material resources to recognize and seek care (Thoits 2005). Therefore, these criteria suggest that variation in cultural orientations, adherence to dominant social norms, and location in the social system may generate variation in self-labeling across racial/ethnic groups, especially in relation to non-Latino whites.
The awareness that something is wrong and requires treatment often begins with the attribution of inchoate feelings of distress to proximal events and circumstances (e.g., job loss), which subsequently becomes identified as an internal dysfunction when the situation changes but the distress persists (Karp 1996). Thoits (2011) cites the person’s self-awareness of emotional reactions to stressful situations as “inappropriately intense, recurrent, or prolonged” (p. 4). In sociological terms, this realization signifies onset of illness because it is the perception of the condition as distinct from any underlying biological malfunction (Aneshensel 2013).
However, Thoits (2005) notes that differential self-labeling across social status groups may exist because socially and economically advantaged groups (e.g., non-Latino whites, high SES) will find it “easier” to self-label than others as a result of better mental health literacy and possession of sufficient resources to seek care. For instance, self-labeling is more prevalent among high SES than low SES adults, resulting in relatively high rates of voluntary service use (Thoits 2005) and relatively low probabilities of deflecting a mental illness identity or label (Thoits 2016). Moses (2009) demonstrates that self-labeling is a difficult process for youth, even for those who are in treatment: Only some used psychiatric terms to label their problems, while others applied different labels or none at all. Among these youthful patients, self-labeling was associated with being white relative to being a member of a racial/ethnic minority group. However, generalizability is limited because the study used a convenience sample of youth in treatment.
Even though diagnostic status is often equated with need, these states often do not align well with people’s self-assessments overall (Pescosolido et al. 2013), but especially among racial/ethnic minority groups (Jang, Park, Kang et al. 2014). Instead, there is considerable slippage between the presence of an underlying disorder and the perception that one needs help (Kessler et al. 2001, Moses 2009), particularly among Black and Hispanic adults relative to non-Hispanic Whites (Jang et al. 2014). Racial/ethnic minority populations also face a constellation of life stressors that may have unique influences on mental illness and how it is perceived, especially whether treatment is needed. For instance, exposure to everyday discrimination and residential segregation may predispose members of racial/ethnic minority groups to attribute symptoms of psychological distress to these experiences and situations and not to an underlying mental disorder. Some African Americans and Latinos, especially those with low incomes, interpret symptoms as normal responses to stressful life situations (Cabassa, Hansen, Palinkas et al. 2008, Hines-Martin, Malone, Kim et al. 2003). In the case of Asian Americans and Latinos, there also is a tendency to report somatic complaints in the face of psychiatric disorders (Cabassa et al. 2008, Yang and Benson 2016), which may impede the realization of need for services and delay the consideration of mental health in the health care context.
Race/Ethnicity and Perceived Need
Some studies report that racial/ethnic minority groups are less likely than non-Latino whites to perceive a need for help (Kimerling and Baumrind 2005, Nadeem et al. 2009, Narendorf and Palmer 2016), but others report the opposite (Falck, Wang, Carlson et al. 2007) or find no differences (Ault-Brutus and Alegría 2016, Mackenzie, Pagura and Sareen 2010, Mojtabai et al. 2002, Mojtabai et al. 2011). These discrepant findings may be due in part to methodological factors, such as sampling (e.g., select samples such as older adults) and implicit omission of some subpopulations (e.g., recent immigrants via English-only interviews). In addition, some studies examine differences for the population overall, controlling for psychiatric disorder, while other studies are limited to persons with disorders. Moreover, existing research on perceived need has almost exclusively focused on between group differences (Edlund, Unützer and Curran 2006, Mojtabai et al. 2002, Nadeem et al. 2009), overlooking potential heterogeneity within racial/ethnic groups. A more comprehensive examination of between-and within-group variation in perceived need with a sample representative of the population and its diversity is essential to the development of social explanations for these differences.
While past research on race/ethnicity and perceived need is inconclusive, we expect racial/ethnic differences to exist for several reasons. First, although perceptions about the causes of mental illness are generally similar across groups (Schnittker 2013), compared to non-Latino whites, a greater proportion of other racial/ethnic groups believe mental illness is caused by social stressors (Alvidrez 1999, Hines-Martin et al. 2003, Jimenez, Bartels, Cardenas et al. 2012). Second, racial/ethnic groups may respond differently to the presence of a disorder. For example, there are notable differences in help-seeking by race/ethnicity. African Americans and Afro-Caribbeans prefer to seek out informal supports to a greater extent than non-Latino whites (Jimenez et al. 2012, Taylor, Woodward, Chatters et al. 2011, Woodward, Chatters, Taylor et al. 2010). African Americans are more likely than Caucasians to believe mental health problems will improve on their own (Anglin, Alberti, Link et al. 2008) and also are less likely to believe pharmacological treatments are acceptable or helpful (Cooper, Gonzales, Gallo et al. 2003, Givens, Houston, Voorhees et al. 2007). In comparison to non-Latino whites, Asian Americans are less willing to get help from anyone (Jimenez et al., 2012), and if services are sought, counseling services are preferred over medications (Givens et al. 2007). In contrast, some Latinos in primary care are more likely than non-Latino whites to endorse a preference for medications (Jimenez et al. 2012). Yet Givens and colleagues (2007) also note that in comparison to medications, counseling is a preferred method of treatment among Latinos with depression. Lastly, attitudes do not necessarily translate into help-seeking behaviors, mirroring documented discrepancies in the application of expressed attitudes to oneself (Pescosolido et al. 2013). In particular, racial/ethnic minority groups consistently underuse mental health services (Cook, Zuvekas, Carson et al. 2014) despite having more positive attitudes towards mental health care (Anglin et al. 2008, Schnittker, Pescosolido and Croghan 2005) and beliefs that some forms of treatment are beneficial to improving mental health (Givens et al. 2007, Schnittker et al. 2005)—with the notable exception of psychiatric medications for some groups (Jimenez et al. 2012, Kasckow, Ingram, Brown et al. 2011, Mojtabai 2009).
Perceived need may also depend on other conjoined characteristics of race/ethnicity, such as nativity, English language proficiency (ELP), and ethnic subgroup identity (e.g., Mexican, Chinese). Although Asian Americans and Latinos constitute more than 70% of the U.S. immigrant population, there is considerable migration from Europe (Zong and Batalova 2015) and nearly one in ten of all U.S. immigrants are Black, most of whom are from Caribbean nations (Anderson 2015). White immigrant groups, in particular, may have better general health literacy than other groups (Sentell and Braun 2012), and therefore be more likely to engage in treatment-seeking behaviors than other racial/ethnic immigrant groups. Immigrants and those with poor ELP also tend to use mental health services infrequently, but existing studies mostly have been limited to Asian Americans and Latinos (Abe-Kim et al. 2007, Alegría et al. 2007, Bauer, Chen and Alegría 2010). Likewise, foreign-born nativity is negatively associated with perceived need (Sareen, Cox, Afifi et al. 2005), but its impact among non-Latino whites and African Americans has been largely ignored in existing research. ELP and ethnic subgroup variation in perceived need patterns are inconclusive (Bauer, Chen and Alegría 2012, Nguyen 2011).
Variation by Gender and SES
Research on race/ethnicity and perceived need tends to emphasize between group variation while controlling for other status characteristics (Ault-Brutus and Alegría 2016, Nadeem et al. 2009), including gender and SES. People simultaneously belong to multiple social groups (Mays and Ghavami 2017), however, and the amalgamation of these statuses may impact perceived mental illness and need for treatment. Existing research has not taken into consideration how intersections of race/ethnicity with other social status categories may impact perceived need. Studies have typically assumed that multiple statuses are independent of each other, an assumption implicit in the “main effects” models used in these studies. As a result, current approaches to understanding perceived need leave unanswered questions about combinations of statuses, for instance, whether one disadvantaged status (race/ethnicity) magnifies the impact of a second one (SES), which instead requires the estimation of “conditional” or “interaction effects” models.
The possibility that individuals can be affected by multiple disadvantaged statuses has a long history that is recounted by Nguyen and colleagues (2013) for the concept of “double jeopardy” as articulated and applied to elderly black women, who are especially disadvantaged due to being black and older, followed by the development of the concepts of “triple jeopardy” and “quadruple jeopardy.” Rosenfield (2012) points to the relatively good mental health of African American women as evidence that the mental health risks associated with multiple disadvantaged statuses do not simply summate over these statuses (as implied by the main effects model and the concept of double jeopardy), but instead combine in seemingly paradoxical ways, which she attributes to self-schemas that privilege the self or others. Thus, approaches that take into account combinations of race/ethnicity, gender, and SES may be especially useful for understanding the social distribution of perceived need given that conditional relationships of this type have been documented for perceptions and attitudes about mental health care in general (Gonzalez, Alegría and Prihoda 2005, Gonzalez, Alegría, Prihoda et al. 2011, Ojeda and Bergstresser 2008)). Furthermore, the examination of these intersections may help unmask complex relationships among multiple statuses for self-labeling in particular (Hankivsky and Grace 2015, Mays and Ghavami 2017).
Socioeconomic factors such as income and education—which are associated with positive attitudes towards treatment (Mojtabai 2009), better problem recognition (Thoits 2016), and more frequent help-seeking (Cook et al. 2014)—may intersect with race/ethnicity to affect perceived need. non-Latino whites and high SES persons are more knowledgeable about mental illnesses, on average—that is, have better mental health literacy—than some racial/ethnic minority groups and low SES persons, respectively (Alvidrez 1999, Gonzalez et al. 2005, Jimenez et al. 2012). Better mental health literacy is thought to then affect how individuals identify and respond to their mental health problems, which may “advantage” certain groups like non-Latino whites in recognizing and responding to a need for treatment. Hence, the benefits of economic and educational resources for the identification of need for treatment and its response may not extend to racial/ethnic minority populations in the same ways that it benefits non-Latino whites. For example, SES is not as strongly linked to mental health literacy among African Americans and Asian Americans as Whites (Lin and Cheung 1999, Thompson, Baxile and Akbar 2004). Given these patterns, we expect SES to be positively associated with perceptions of need, overall, but more strongly among non-Latino whites than other racial/ethnic groups.
Similarly, it is by no means certain that gendered expectations about emotional expressiveness and help-seeking are universal across racial/ethnic groups. In general, women surpass men in perceived need (Mojtabai et al. 2002, Mojtabai et al. 2011), willingness to use mental health services (Gonzalez et al. 2011), and utilization of these services (Ojeda and McGuire 2006, Wang et al. 2005), but the magnitude of these differences varies by race/ethnicity. Compared to men, traditional gender role socialization may lead women to be more expressive of feelings and to engage in more help-seeking behaviors in general (Gonzalez et al. 2005), but some differences may be greater among non-Latino whites than other groups (Gonzalez et al. 2005, Gonzalez et al. 2011). Similar coping strategies among African American men and women may contribute to more similar attitudes toward mental health, more so than among non-Latino whites (Rosenfield and Mouzon 2013). Additionally, adherence to Western masculine norms (e.g., emotional self-reliance, dominance) may foster negative attitudes towards mental health services and erode willingness to seek these services, particularly among Asian American men (Berger, Addis, Green et al. 2013, Vogel, Heimerdinger-Edwards, Hammer et al. 2011). Yet, this tendency may be offset by higher than average levels of education among non-Latino whites and Asian Americans because education is associated with more egalitarian concepts of gender (Rosenfield and Mouzon 2013). Although existing research suggests women are more likely than men to perceive a need for treatment, we posit that this gender difference is more pronounced among non-Latino whites than other racial/ethnic groups.
The current study expands our understanding of self-labeling by examining how the intersections of race/ethnicity with gender and SES differentially influence perceptions of need for mental health care. We expect to find overall lower odds of perceived need among racial/ethnic minority groups, low SES groups, males, and immigrants compared to non-Latino whites, high SES groups, females, and U.S.-born citizens, respectively. However, we hypothesize that the combination of these status characteristics will produce the following conditional effects: (a) High SES will be associated with high odds of perceived need for mental health care only among non-Latino whites; and (b) men will be less likely than women to perceive a need among non-Latino whites, but not other groups. We also examine conjoined aspects of race/ethnicity and expect that foreign-born immigrants will have less perceived need than U.S.-born persons—and that this effect will be most prominent among Asian Americans and Latinos than other groups. Within these groups, we also anticipate heterogeneity by ELP and ethnic subgroups.
Methods
Data are from the Collaborative Psychiatric Epidemiology Surveys, a national household probability sample of U.S. adults (18 years or older) comprised of three epidemiological studies: the National Comorbidity Survey-Replication (NCS-R; Kessler and Merikangas 2004), the National Survey of American Life (NSAL; Jackson, Torres, Caldwell et al. 2004), and the National Latino and Asian American Study (NLAAS; Alegría, Takeuchi, Canino et al. 2004). Respondents were interviewed face-to-face using a computer-assisted structured questionnaire; a few were interviewed by telephone. Trained lay interviewers collected information about mental disorders, impairments associated with these disorders, and treatment. NSAL and NCS-R interviews were conducted in English and NLAAS interviews were conducted in English, Spanish, Mandarin, Cantonese, Tagalog, and Vietnamese. Data collection occurred between February 2001 and November 2003.
Sample
The NLAAS sampled Latinos and Asian Americas (n=4,649; 73.2% response rate), the NSAL sampled African Americans, Afro-Caribbeans, and non-Latino whites (n=6,082, 70.9% response rate) and the NCS-R sampled all racial/ethnic groups (n=9,282; 70.9% response rate). The NCS-R was completed in two parts: Part 1 included the core mental health and services measures; Part 2 included additional psychosocial and demographic questions. Part 2 was completed by all respondents meeting diagnostic criteria for a lifetime mental disorder and a probability subsample of other respondents. The current study uses all NLAAS and NSAL participants and the Part 2 NCS-R participants (n=5,692). When weighted, the three datasets collectively constitute a single sample that is nationally representative of the non-institutionalized adult population (18+) of the United States (n=16,423; for details see Heeringa et al., 2004).
The total sample is analyzed to assess the overall association between status characteristics and perceived need in the general population, controlling for current clinical need for treatment—defined as meeting research diagnostic criteria for a 12-month mood, anxiety and/or substance use disorder (SUD). The sample is then subdivided into: a clinical need subsample of respondents who meet lifetime diagnostic criteria for any psychiatric disorder; and, a no disorder subsample who do not meet these criteria because a sizeable proportion of persons who use mental health services do not have a diagnosable disorder (Druss et al. 2007).
Measures
Perceived Need.
For this study, self-labeling is operationalized as perceived need for mental health care, which is a positive response to the question: “Was there ever a time during the past 12-months when you felt that you might need to see a professional because of problems with your emotions or nerves or your use of alcohol or drugs?” NSAL and NCS-R respondents who used mental health services in the past year skipped this question and were asked instead whether treatment was voluntary or due to coercion or pressure from others. Similar to previous studies using the National Comorbidity Survey or the NCS-R (Katz, Kessler, Frank et al. 1997, Mojtabai et al. 2002), perceived need for these respondents was coded positive if their use was voluntary and negative if their use was coerced or pressured.
Social Status Characteristics.
Race/ethnicity is coded: non-Latino white—the omitted reference group, Asian American (Chinese, Filipino, Vietnamese, and all other Asian origins), Latino (Puerto Rican, Cuban, Mexican, and all other Latino origins—including Afro-Caribbeans of Hispanic descent), non-Latino Afro-Caribbean, or African American. “Other race/ethnicity” is excluded due to the small sample size (n=162) and the considerable diversity of the category. SES is operationalized as years of education in four categories (less than 12 years—reference group; 12 years; 13–15 years; and 16 or more years) and as an income-to-poverty ratio (hereafter income/poverty) calculated by dividing household income by the 2001 federal poverty threshold. Nativity is coded as foreign-born=1, U.S.-born=0. Aspects of ethnicity measured only in the Latino and Asian American subsamples are: ethnic subgroup (as previously listed) and ELP, which was explicitly measured in the NLAAS, but assumed for NCS-R Latino and Asian American respondents because proficiency is implied by English-only interviews. For stratified analyses, nativity and ELP were combined because of sample size limitations: U.S.-born—reference group, foreign-born with fair/poor ELP, and foreign-born with excellent/good ELP.
Clinical Need Indicators.
Clinical need consists of three dichotomous variables for 12-month research diagnosis of any mood disorder (major depression and dysthymia), anxiety disorder (generalized anxiety, agoraphobia, social phobia, panic attack, and panic disorder), or SUD (alcohol and/or drug abuse/dependence). Disorders were assessed using the World Mental Health Survey Initiative version of the Composite International Diagnostic Interview (CIDI; Kessler and Üstün 2004). Diagnostic criteria are from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychiatric Association 2000). Need for care is also indexed with two measures of mental health crises: lifetime history of psychiatric hospitalizations (ever hospitalized=1, else=0) and lifetime suicidality (ever had suicidal ideation, plan, or attempt=1; else=0). In addition, self-rated mental health, an indicator of subjective need, was measured by asking, “How would you rate your overall mental health?” (1=“Excellent” to 5=“Poor”).
Need was additionally measured as nonspecific psychological distress during the past 30 days using the Kessler 6 (Kessler, Barker, Colpe et al. 2003)—a six-item measure with each symptom (e.g., how often did you feel so depressed nothing could cheer your up) rated from 0 “None of the time” to 4 “All of the time” (range 0–24). Functional impairment is assessed with four items from the World Health Organization’s Disability Assessment Scale (WHODAS; WHO 2001; e.g., the number of days in the past month respondent was unable to work or carry out normal activities because of problems with their physical or mental health). Items were aggregated to create a standardized role impairment score (range 0–100). A count of lifetime chronic physical conditions was used to take somatization into account—heart problems, hypertension, asthma, chronic lung disease, diabetes, stomach ulcers, and cancer (range 0 to 7).
Control Variables.
Insurance status was operationalized as two dichotomous variables: private insurance (i.e., employer-sponsored or privately purchased) and public insurance (i.e., Medicaid, Medicare, or other public insurance plans). Medical care from a usual place or person is coded as 1=yes, 0=no. There are three sociodemographic controls: age (18–29 years—omitted reference, 30–44 years, 45–59 years, and 60 or more years), employment status (employed—omitted reference, unemployed, and not in labor force), and marital status (married/cohabiting—omitted reference, previously married [divorced or widowed], and never married).
Statistical Analysis
Multivariable analyses were conducted using logistic regressions. The first set of analyses is for the total sample and for its two subsamples defined by lifetime diagnosis status: the clinical need and no disorder subsamples. We start by modeling the main effects of race/ethnicity, gender, SES, and nativity on perceived need. Intersections of race/ethnicity with other status characteristics were then examined by estimating conditional effects models that included two-way product interaction terms of: race/ethnicity with gender, race/ethnicity with SES, and race/ethnicity with nativity. Interactions were tested using adjusted Wald tests. Average marginal effects in predicted probabilities of statistically significant interactions are presented to aid interpretation (Norton, Wang and Ai 2003). For the post-estimation tests, we compare all racial/ethnic groups to one another, set covariates to their means, and adjust for multiple comparisons.
The second set of analyses is limited to the clinical need subsample and is stratified by race/ethnicity. Stratified analyses are presented irrespective of the significance of interaction terms in the previous analysis to ascertain whether there are pervasive differences across groups for multiple variables that go beyond a specific interaction. Part A of the stratified analysis tests factors that are shared in common across racial/ethnic groups. For each group, the main effects model was tested against the same model with the addition of a SES by gender interaction (education by gender and income/poverty by gender). Part B tests the addition of ELP and ethnic subgroups for Latinos and Asian Americans (not shown, null findings). Stratified models were modified to address smaller sample sizes: age was continuous; education was dichotomized (less than or high school equivalent=0, more than high school=1); insurance and employment status were dropped due to non-significance; and, the Afro-Caribbean subsample was dropped.
About one-quarter of respondents are missing on self-rated mental health because of a design feature of the NCS-R. We imputed this variable with ordinal logistic regression; ten datasets were imputed using the STATA SE 14 multiple imputation chained procedures (StataCorp 2015). Respondents missing on other variables were excluded (8.3% missing). Rubin’s rules were used to combine results across imputed datasets (Rubin 1987).
All analyses used sample design variables and weights developed by Heeringa and colleagues (2004) to correct for stratification, clustering, unequal selection probabilities, and nonresponse. STATA SE 14 survey procedures were used to calculate estimate all statistical models (StataCorp 2015). Standard errors were calculated using Taylor Series approximation.
Results
Sample Characteristics
Table 1 presents the distribution of variables for the total sample, the clinical need subsample as defined by lifetime history of any mood, anxiety, or SUD, and the no disorder subsample. Overall, somewhat more respondents were female than male (52.4% vs. 47.6%, respectively), non-Latino whites predominated (70.0%), a majority had at least some college education (51.1%) and incomes averaged four times above the poverty line. Respondents, on average, were middle-aged. The overwhelming majority had health insurance (86.2%) and a usual source of care (87.3%). The sociodemographic profiles of the two subsamples approximate those of the total sample except the clinical need sample has a disproportionately high representation of non-Latino whites (76.5%) and females (54.7%) and a disproportionally low representation of foreign-born persons (8.6%).
Table 1.
Sample Characteristics: CPESa, 2001 – 2003
| Total Sample (n = 14,906)b |
Clinical Need Subsample (n = 6,863)c |
No Disorder Subsample (n = 8,043)d |
||
|---|---|---|---|---|
| Unweighted | Weighted | Weighted | Weighted | |
|
n |
Mean (SE) or % |
Mean (SE) or % |
Mean (SE) or % |
|
| Age | 14,906 | 44.87 (.44) | 42.50 (.37) | 46.89 (.64) |
| Male | 6,175 | 47.6% | 45.3% | 49.5% |
| Race/Ethnicity | ||||
| Asian American | 2,170 | 4.9% | 2.6% | 6.8% |
| Latino | 3,237 | 13.2% | 10.7% | 15.3% |
| Afro-Caribbean | 1,421 | 0.7% | 0.6% | 0.9% |
| African American | 4,025 | 11.2% | 9.6% | 12.6% |
| Non-Latino White | 4,053 | 70.0% | 76.5% | 64.4% |
| Years of Education | ||||
| Less than 12 years | 3,231 | 18.2% | 16.8% | 19.4% |
| 12 years | 4,313 | 30.7% | 30.5% | 30.9% |
| 13–15 years | 3,925 | 27.3% | 28.2% | 26.5% |
| 16 or more years | 3,437 | 23.8% | 24.5% | 23.2% |
| Income-to-poverty ratio | 14,906 | 4.42 (.09) | 4.41 (.11) | 4.42 (.10) |
| Foreign-Born | 4,821 | 13.6% | 8.6% | 17.8% |
| Disorder History | ||||
| No Lifetime Disorder | 8,043 | 54.1% | ||
| Any 12-Month Disorder | 3,617 | 22.7% | 49.4% | |
| Any Lifetime Disorder Only | 3,246 | 31.4% | 50.6% | |
| 12-Month Mood Disorder | 1,416 | 8.4% | 18.2% | |
| 12-Month Anxiety Disorder | 2,861 | 17.9% | 39.0% | |
| 12-Month Substance Use Disorder | 480 | 3.6% | 7.7% | |
| Lifetime Hospitalization | 1,252 | 7.7% | 14.9% | 1.7% |
| Lifetime Suicidality | 2,248 | 14.7% | 25.8% | 5.3% |
| Role Impairment (WHODAS) | 14,906 | 10.33 (.35) | 14.74 (.48) | 6.59 (.48) |
| Psychological Distress (K6) | 14,906 | 3.69 (.09) | 5.38 (.10) | 2.24 (.08) |
| Self-Rated Mental Healthe | 14,906 | 2.15 (.03) | 2.35 (.03) | 1.97 (.04) |
| Uninsured | 2,714 | 13.8% | 15.0% | 12.8% |
| Usual Source of Care | 12,573 | 87.3% | 87.7% | 87.0% |
| Perceived Need | 2,734 | 18.6% | 33.3% | 6.0% |
CPES = Collaborative Psychiatric Epidemiology Surveys
Total CPES sample includes all NLAAS, NSAL, and Part 2 NCS-R participants
Respondents who meet lifetime diagnostic criteria for any mood, anxiety, or substance use disorder
Respondents who do not meet lifetime diagnostic criteria for any disorder
Self-rated mental health, 1=Excellent to 5=Poor
The two subsamples have distinctly different mental health profiles, as expected based on the criterion for selection into these subsamples. For the clinical need subsample, approximately half meet diagnostic criteria for any past-year disorder: two in five for anxiety disorders, one in five for mood disorders, and one in ten for SUDs. There also is a sizeable concentration of psychiatric hospitalizations and suicidality in this subsample. Few persons in the no disorder subsample report these mental health-related crises. Individuals in the no disorder subsample also report better self-rated mental health, on average, than persons in the clinical need subsample.
About one in three persons with a clinical need report a perceived need for care. Among those with a perceived need, 17.6% have no history of disorder, which attests to the importance of identifying the determinants of perceived need in this group.
Social Status and Perceived Need: Total Sample
Table 2 presents the main and conditional effects (interaction effects) models for the total sample. For the main effects model, Asian Americans and African Americans have significantly lower odds than non-Latino whites of perceiving a need for care, other factors held constant, but not Latinos and Afro-Caribbeans (Model IA). Post-estimation tests additionally reveal that relative to Latinos, Asian Americans (OR = 0.47, p < .001), Afro-Caribbeans (OR = 0.45, p = .04), and African Americans (OR = 0.53, p < .001) have lower odds of realizing a need (not shown in Table 2). Men have lower odds than women of perceiving they need help, other factors held constant. Persons with high incomes and high education versus low levels of education are more likely to perceive a need. Nativity is not statistically significant, net of other factors. Thus, there is evidence of differential self-labeling across race/ethnicity, gender, and SES, insofar as these variables are statistically significant net of need and other covariates.
Table 2.
Logistic Regressions of Perceived Need for Mental Health Care on Social Status, Demographic Characteristics, and Need: Weighted Sample, (OR [95% CI])
| I. Total Sample (n = 14,906) |
II. No Disorder Subsample (n = 8,043) |
III. Clinical Need Subsample (n = 6,863) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| A. Main Effects Model | B. Interaction Effects Model |
A. Main Effects Model | A. Main Effects Model | B. Interaction Effects Model |
||||||
| Social Status Characteristics | ||||||||||
| Race/Ethnicity | ||||||||||
| Non-Latino White | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Asian American | .51*** | [0.36, 0.73] | 0.72 | [0.47, 1.09] | 0.78 | [0.39, 1.58] | 0.47*** | [0.30, 0.74] | 0.93 | [0.59, 1.45] |
| Latino | 1.09 | [0.83, 1.41] | 0.96 | [0.72, 1.28] | 1.27 | [0.71, 2.25] | 1.07 | [0.81, 1.43] | 1.12 | [0.86, 1.45] |
| Afro-Caribbean | 0.49 | [0.22, 1.07] | 0.43* | [0.21, 0.86] | 1.02 | [0.40, 2.60] | 0.39* | [0.18, 0.84] | 0.45 | [0.12, 1.69] |
| African American | 0.58*** | [0.45, 0.74] | 0.54*** | [0.42, 0.71] | 0.66 | [0.39, 1.13] | 0.58*** | [0.45, 0.75] | 0.59*** | [0.46, 0.77] |
| Male | 0.60*** | [0.53, 0.67] | 0.55*** | [0.47, 0.64] | 0.61*** | [0.45, 0.81] | 0.61*** | [0.53, 0.70] | 0.61*** | [0.53, 0.70] |
| Years of Education | ||||||||||
| Less than 12 years | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 12 years | 0.93 | [0.70, 1.24] | 0.92 | [0.69, 1.23] | 0.71 | [0.42, 1.19] | 1.04 | [0.75, 1.43] | 1.03 | [0.75, 1.42] |
| 13–15 years | 1.20 | [0.89, 1.62] | 1.18 | [0.88, 1.60] | 0.92 | [0.58, 1.48] | 1.35 | [0.91, 1.98] | 1.34 | [0.91, 1.96] |
| 16+ years | 1.76*** | [1.27, 2.44] | 1.75*** | [1.26, 2.41] | 1.41 | [0.87, 2.31] | 1.92*** | [1.30, 2.84] | 1.90*** | [1.29, 2.80] |
| Income-to-Poverty Ratio | 1.03* | [1.01, 1.06] | 1.03* | [1.01, 1.06] | 1.03 | [0.98, 1.07] | 1.03 | [0.99, 1.06] | 1.03 | [0.99, 1.06] |
| Foreign-born Nativity | 0.84 | [0.65, 1.10] | 1.15 | [0.64, 2.04] | 0.69 | [0.40, 1.19] | 1.01 | [0.72, 1.40] | 1.52 | [0.80, 3.04] |
| Clinical Need Indicators | ||||||||||
| 12-Month Mood Disorder | 2.55*** | [2.10, 3.09] | 2.55*** | [2.10, 3.10] | 2.23*** | [1.83, 2.72] | 2.25*** | [1.84, 2.74] | ||
| 12-Month Anxiety Disorder | 2.61*** | [2.22, 3.06] | 2.60*** | [2.22, 3.05] | 1.90*** | [1.61, 2.26] | 1.90*** | [1.60, 2.25] | ||
| 12-Month SUD | 1.97** | [1.25, 3.10] | 1.97** | [1.25, 3.09] | 1.68** | [1.14, 2.47] | 1.67** | [1.14, 2.46] | ||
| Lifetime Hospitalization | 1.51** | [1.16, 1.97] | 1.51** | [1.16, 1.97] | 1.51 | [0.81, 2.80] | 1.35* | [1.04, 1.74] | 1.35* | [1.05, 1.75] |
| Lifetime Suicidality | 1.67*** | [1.44, 1.92] | 1.67*** | [1.43, 1.92] | 2.11*** | [1.35, 3.30] | 1.43*** | [1.26, 1.63] | 1.43*** | [1.25, 1.62] |
| Role Impairment Score | 1.00* | [1.00, 1.01] | 1.00* | [1.00, 1.01] | 1.01** | [1.00, 1.02] | 1.00 | [0.99, 1.00] | 1.00 | [0.99, 1.00] |
| Psychological Distress | 1.12*** | [1.10, 1.15] | 1.13*** | [1.11, 1.15] | 1.14*** | [1.09, 1.20] | 1.11*** | [1.08, 1.14] | 1.11*** | [1.09, 1.14] |
| Self-Rated Mental Healtha | 1.42*** | [1.24, 1.63] | 1.43*** | [1.24, 1.64] | 1.52** | [1.15, 2.02] | 1.39*** | [1.21, 1.59] | 1.39*** | [1.21, 1.59] |
| No. of Chronic Conditions | 1.19** | [1.06, 1.34] | 1.19** | [1.06, 1.34] | 1.23* | [1.00, 1.52] | 1.15* | [1.02, 1.30] | 1.15* | [1.01, 1.30] |
| Controls | ||||||||||
| Insurance Status | ||||||||||
| Uninsured | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Privately Insured | 1.08 | [0.89, 1.30] | 1.07 | [0.89, 1.29] | 1.25 | [0.78, 2.01] | 1.04 | [0.78, 1.39] | 1.05 | [0.78, 1.39] |
| Publicly Insured | 1.14 | [0.90, 1.43] | 1.14 | [0.91, 1.44] | 1.34 | [0.73, 2.46] | 1.14 | [0.90, 1.44] | 1.14 | [0.90, 1.44] |
| Usual source of care | 1.39* | [1.07, 1.82] | 1.40* | [1.07, 1.83] | 1.78* | [1.02, 3.08] | 1.31 | [0.97, 1.76] | 1.32 | [0.98, 1.78] |
| Age | ||||||||||
| 18–29 years old | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| 30–44 years old | 0.98 | [0.79, 1.20] | 0.98 | [0.80, 1.21] | 0.96 | [0.59, 1.59] | 0.94 | [0.69, 1.26] | 0.94 | [0.69, 1.27] |
| 45–59 years old | 0.74*** | [0.62, 0.88] | 0.74** | [0.62, 0.89] | 0.75 | [0.44, 1.26] | 0.71* | [0.53, 0.94] | 0.71* | [0.54, 0.94] |
| 60 years old and over | 0.28*** | [0.18, 0.43] | 0.28*** | [0.18, 0.42] | 0.17** | [0.05, 0.52] | 0.38*** | [0.26, 0.56] | 0.38*** | [0.26, 0.56] |
| Marital Status | ||||||||||
| Married/Cohabiting | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Previously married | 1.37** | [1.08, 1.74] | 1.36** | [1.08, 1.72] | 1.27 | [0.71, 2.27] | 1.37** | [1.08, 1.73] | 1.36** | [1.08, 1.72] |
| Never married | 1.08 | [0.88, 1.32] | 1.07 | [0.87, 1.31] | 1.31 | [0.76, 2.27] | 0.99 | [0.80, 1.24] | 0.99 | [0.80, 1.23] |
| Employment Status | ||||||||||
| Employed | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | |||||
| Unemployed | 1.03 | [0.77, 1.37] | 1.03 | [0.77, 1.37] | 1.23 | [0.68, 2.23] | 1.01 | [0.72, 1.42] | 1.01 | [0.72, 1.42] |
| Not in labor force | 1.07 | [0.90, 1.28] | 1.08 | [0.91, 1.30] | 1.15 | [0.76, 1.76] | 1.11 | [0.89, 1.39] | 1.11 | [0.89, 1.40] |
| Interaction Terms | ||||||||||
| Gender by Race/Ethnicity | ||||||||||
| Non-Latino White, Male | 1.00 | |||||||||
| Asian, Male | 1.53* | [1.00, 2.35] | ||||||||
| Latino, Male | 1.46* | [1.09, 1.97] | ||||||||
| Afro-Caribbean, Male | 1.38 | [0.26, 7.48] | ||||||||
| African American, Male | 1.23 | [0.91, 1.65] | ||||||||
| Nativity by Race/Ethnicity | ||||||||||
| Non-Latino White, Foreign | 1.00 | 1.00 | ||||||||
| Asian American, Foreign | 0.36** | [0.18, 0.71] | 0.23*** | [0.10, 0.52] | ||||||
| Latino, Foreign | 0.69 | [0.35, 1.36] | 0.62 | [0.28, 1.33] | ||||||
| Afro-Caribbean, Foreign | 0.76 | [0.22, 2.54] | 0.52 | [0.12, 2.29] | ||||||
| African American, Foreign | 0.60 | [0.15, 2.48] | 0.24 | [0.05, 1.06] | ||||||
| Test of Gender by Race/Ethnicity | p = .05 | |||||||||
| Test of Foreign-Born by Race/Ethnicity | p = .02 | p = .002 | ||||||||
NOTE:
p ≤ .05,
p ≤ .01,
p ≤ .001; OR = odds ratio; CI = Confidence interval
Self-rated mental health scores range from 1 = Excellent to 5 = Poor
The presence of mental health problems is the dominant influence on whether individuals think they need professional help (Model IA, Table 2). Meeting 12-month diagnostic criteria is strongly associated with perceived need, somewhat more so for mood and anxiety disorders than SUDs. Lifetime suicidality, psychiatric hospitalizations, role impairments, psychological distress, and poor subjective mental health ratings are also associated with relatively high odds of perceived need. Other significant contributors to having a perceived need include having poor physical health and a usual source of care. The significant coefficient for being previously married (relative to currently married/cohabiting) may represent an impact of life problems as distinct from mental health problems per se. People who are late midlife and older have lower odds than young adults, especially those who are 60 years of age and older.
The main effects model presented assumes that the correlates of perceived need have independent effects across all racial/ethnic groups, which means the parameter estimates are constrained by default to be equivalent across groups, an assumption that may not be warranted because these groups have distinct social and economic profiles. For this sample, women represent a larger proportion of African Americans (56.1%) than other groups (not shown). The mode for education is less than high school for Latinos (42.6%), high school for African Americans (37.4%) and Afro-Caribbeans (30.4%), and college graduate or more for Asian Americans (42.9%); over half of non-Latino whites (55.9%) received at least some college education. In contrast, 10.2% of Latinos, 21.8% of Afro-Caribbeans, and 14.1% of African Americans completed college or pursued graduate education. Income/poverty ratios are 1.8 and 2.1 times those of African Americans for non-Latino whites and Asian Americans, respectively. Foreign-born immigrants are a majority for Asian Americans (77.2%), Afro-Caribbeans (66.6%), and Latinos (51.5%) but only 2.4% of African Americans and 3.2% of non-Latino whites.
We examined statistical interaction terms that enable the impact of social and economic status characteristics on perceived need to vary by race/ethnicity. Most of the two-way interactions are not statistically significant, with the exception of race/ethnicity with gender and with nativity (Model IB, Table 2). To interpret the race/ethnicity by gender interaction terms, differences in predicted probabilities of perceived need were calculated and are plotted for men and women across racial/ethnic groups; all other covariates were set at their mean values (see Figure 1a). Generally, men are less likely than women to believe they need treatment, but this difference is statistically significant only among non-Latino whites (p <.001) and not among other groups. Although Figure 1a suggests similar predicted probabilities of perceived need between African American men and women (given the overlapping confidence intervals [CIs]), the logistic model results indicate that this gender difference is statistically significant for this group (p < .01). This inconsistency may arise because predicted probabilities are sensitive to the values set for the covariates, while the odds ratios are not. We give priority to the results of the logistic model for this reason and because the predicted probabilities are derived from this statistical model. The gender difference is also significant among the African American clinical need subsample in the stratified analysis (see Table 3). In this instance, the coefficient for gender is estimated with all other independent variables estimated separately among African Americans with a clinical need; by contrast, Model IB (Table 1) estimates the gender effect holding the effects of all other independent variables (except nativity) constant across racial ethnic groups. Females have significantly higher levels of perceived need than males among African Americans with clinical need. Therefore, we conclude that there are gender differences among African Americans overall and for the clinical need subsample. In multiple comparison tests (not shown), no other differences between racial/ethnic groups were observed. Correspondingly, racial/ethnic group differences in perceived need in the total sample are somewhat greater among women than men.
Figure 1a and 1b.
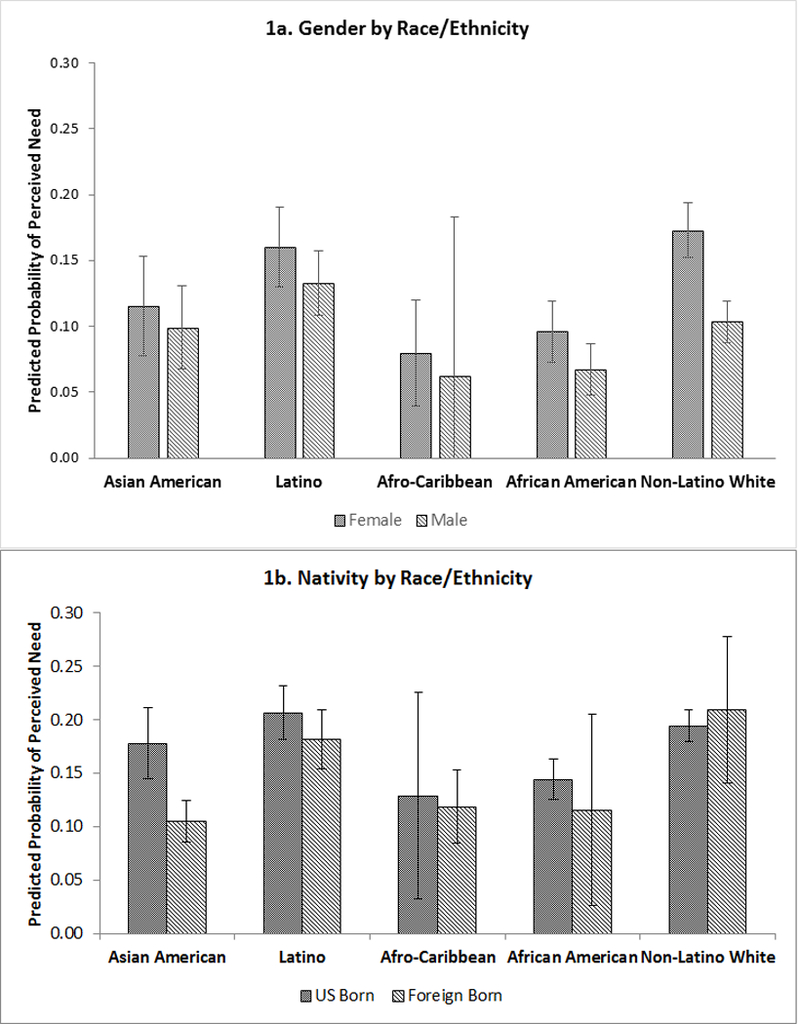
Predicted Probabilities of Perceiving a Need for Mental Health Care across (1a) Gender and Race/Ethnicity and (1b) Nativity and Race/Ethnicity: Total CPES Sample
Table 3.
Logistic Regressions of Perceived Need for Mental Health Care on Social Status, Demographic Characteristics, and Need: Clinical Need Subsample (OR [95% CI])
| Asian American (n = 538) |
Latino (n = 1,359) |
African American (n = 1,745) |
Non-Latino White (n = 2,789) |
|||||
|---|---|---|---|---|---|---|---|---|
| Social Status Characteristics | ||||||||
| Male | 0.75 | [0.35, 1.63] | 0.75 | [0.54, 1.05] | 0.68* | [0.50, 0.92] | 0.57*** | [0.49, 0.68] |
| Education | ||||||||
| 12 years or less | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 13 years or more | 1.55 | [0.73, 3.32] | 1.21 | [0.88, 1.68] | 1.99*** | [1.52, 2.60] | 1.54** | [1.14, 2.07] |
| Income-to-Poverty Ratio | 1.04 | [0.99, 1.09] | 1.03 | [0.98, 1.08] | 0.98 | [0.94, 1.04] | 1.04* | [1.00, 1.07] |
| Foreign-born Nativity | 0.40** | [0.20, 0.78] | 0.88 | [0.63, 1.23] | 0.43 | [0.24, 1.26] | 1.60 | [0.81, 3.19] |
| Clinical Need Indicators | ||||||||
| 12-Month Mood Disorderc | 4.43*** | [2.25, 8.73] | 2.20*** | [1.54, 3.15] | 2.69*** | [1.83, 3.95] | 2.21*** | [1.70, 2.86] |
| 12-Month Anxiety Disorderc | 2.25** | [1.25, 4.06] | 2.70*** | [1.67, 4.37] | 2.39*** | [1.68, 3.39] | 1.74*** | [1.40, 2.17] |
| 12-Month SUDc | 2.96 | [0.51, 17.28] | 2.19 | [0.74, 6.48] | 1.96* | [1.02, 3.76] | 1.46 | [0.91, 2.35] |
| Lifetime Hospitalization | 5.15*** | [1.94, 13.65] | 2.22*** | [1.42, 3.48] | 1.25 | [0.80, 1.94] | 1.23 | [0.88, 1.73] |
| Lifetime Suicidality | 1.81 | [0.99, 3.31] | 1.49* | [1.08, 2.05] | 1.79*** | [1.28, 2.49] | 1.38*** | [1.17, 1.63] |
| Role Impairment Score | 1.01* | [1.00, 1.02] | 1.00 | [0.99, 1.00] | 1.00 | [0.99, 1.01] | 1.00 | [0.99, 1.01] |
| Psychological Distress | 0.99 | [0.90, 1.10] | 1.10*** | [1.06, 1.15] | 1.06** | [1.02, 1.10] | 1.12*** | [1.09, 1.16] |
| Self-Rated Mental Health | 1.48* | [1.05, 2.07] | 1.42*** | [1.21, 1.67] | 1.29** | [1.09, 1.54] | 1.38** | [1.15, 1.66] |
| No. of Chronic Conditions | 1.00 | [0.75, 1.33] | 1.19 | [0.98, 1.45] | 1.13 | [0.98, 1.30] | 1.16 | [0.98, 1.38] |
| Controls | ||||||||
| Usual source of care | 2.57* | [1.17, 5.63] | 1.24 | [0.80, 1.90] | 1.36 | [0.86, 2.14] | 1.34 | [0.94, 1.92] |
| Age | 1.00 | [0.98, 1.03] | 0.99* | [0.97, 0.99] | 0.99 | [0.98, 1.01] | 0.98*** | [0.97, 0.99] |
| Marital Status | ||||||||
| Married/Cohabiting | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Previously Married | 0.75 | [0.26, 2.20] | 0.94 | [0.54, 1.64] | 0.91 | [0.68, 1.22] | 1.52** | [1.14, 2.03] |
| Never Married | 1.31 | [0.56, 3.10] | 0.62 | [0.34, 1.13] | 0.67* | [0.46, 0.98] | 0.98 | [0.74, 1.30] |
NOTE:
p ≤ .05,
p ≤ .01,
p ≤ .001; OR = odds ratio; CI = Confidence interval
Figure 1b plots the predicted probabilities of perceiving a need for mental health care by nativity and by race/ethnicity: foreign-born Asian Americans are less likely to perceive a need than U.S.-born Asian Americans, and this nativity difference is statistically significant (p < .001). Additionally, this nativity difference is largest among Asian Americans when compared to non-Latino whites; however, this difference disappears when adjusted for multiple comparisons (not shown) and no other group differences were observed. In sum, the significant interactions in the total sample suggest that gender and nativity differences in self-labeling are conditional on race/ethnicity.
Social Status and Perceived Need: No Disorder Subsample
Persons who do not meet criteria for a lifetime diagnosis are significantly less likely to see themselves as needing professional help than persons who meet these criteria (6.0% vs. 33.3%, Table 1). Social status characteristics have a limited impact on self-labeling in the no disorder subsample (Model IIA, Table 2). Only one status characteristic is statistically significant in this subsample. Males have lower odds of perceived need than females, other factors held constant. Furthermore, there are no significant interactions among status characteristics (not shown).
Suicidality, role impairments, and nonspecific psychological distress are significantly associated with larger odds of perceived need; lifetime psychiatric hospitalization is not, which may be due to its extremely low occurrence (1.7%). Self-rated mental health and physical health status as assessed by the number of chronic conditions, also are significant in the expected direction. Similar to the total sample, age differences are found—those in the oldest age group have lower odds than those in the youngest group, and having a usual source of care is associated with relatively high odds of seeing oneself as needing mental health care.
Social Status and Perceived Need: Clinical Need Subsample
Model IIIA in Table 2 presents the main effects for the subsample who meets research diagnostic criteria for any lifetime mood, anxiety, and/or SUD. With the exception of Latinos, racial/ethnic minority groups have lower odds of perceiving a need for care than non-Latino whites, other variables held constant. In post-estimation tests of other contrasts (not shown in Table 2), we also find that Asian Americans (OR = 0.44, p < .001), Afro-Caribbeans (OR = 0.37, p < .01), and African Americans (OR = 0.54, p < .001) have significantly lower odds of perceived need than Latinos. No other group comparisons are statistically significant. Men have significantly lower odds than women. Other things being equal, SES has a limited impact, with the only significant difference being the higher odds among people with at least a college education compared to less than a high school education. Foreign-born nativity is not significant.
All indicators of clinical need for services are significantly associated with greater odds of perceived need for professional help, with the exception of role impairments (Model IIIA, Table 2). Compared to those with no past-year disorder, the odds of seeing oneself as needing care are roughly two times as great for persons with a mood, anxiety, or substance use disorder. Other things being equal, these odds are also greater among those who are positive for lifetime psychiatric hospitalizations and suicidality than among those who are negative on these variables. Psychological distress, poor self-rated mental health, and chronic conditions are associated with greater odds of perceiving a need. The odds of seeing oneself as needing help are lower among persons who are late middle age and older, compared to young adults. Previously married persons have greater odds than married persons.
Turning to the conditional model, only one statistically significant interaction term is found of the four tested: race/ethnicity with nativity (Model IIIB, Table 2). Figure 2 plots the predicted probabilities of perceiving a need for mental health care across nativity and race/ethnicity for the clinical need subsample. Similar to the total sample, the probability of perceived need is significantly lower among foreign-born than U.S.-born Asian Americans (p < .001). This nativity effect is statistically significant only among Asian Americans. The nativity difference among this group is also largest when compared to non-Latino whites. There are no significant nativity differences for other racial/ethnic groups.
Figure 2.
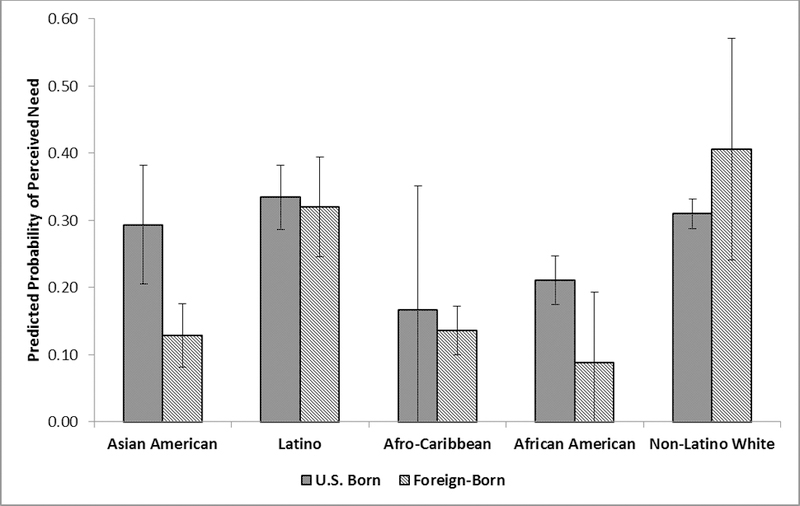
Predicted Probabilities of Perceiving a Need for Mental Health Care across Nativity and Race/Ethnicity: Clinical Need Subsample
Variation in Perceived Need within Racial/Ethnic Groups
The first set of stratified analyses assessing within-group heterogeneity in perceived need examines factors that are relevant to all racial/ethnic groups with a clinical need (Table 3). Social status characteristics have some impact on perceived need within all groups, net of other factors. Males are significantly less likely than women to believe they need mental health services among African Americans and non-Latino whites, but gender is not significant among Asian Americans or Latinos. Likewise, high education is associated with higher odds of perceived need for African Americans and non-Latino whites only. Lastly, foreign-born nativity is significantly associated with lower odds among Asian Americans only.
We also examined potential interactions between gender and SES within each group; all but one were statistically nonsignificant. Among African Americans with a clinical need, a statistically significant interaction between gender and income/poverty was found (not shown). Further investigation revealed that the effect of income/poverty on perceived need was positive but statistically nonsignificant among African American women and negative but only marginally significant among African American men (p = .054).
For the most part, diagnostic status indicators (with the exception of past-year SUD in most stratified models), psychological distress, and self-rated mental health are strong and fairly consistent correlates of perceived need within groups. Lifetime hospitalization is associated with higher odds of perceived need for Asian Americans and Latinos, but not for African Americans or non-Latino whites. Suicidality is associated with high odds among all groups except Asian Americans, whereas role impairments are associated with higher odds of perceived need among Asian Americans only. With respect to other covariates, older Latinos and non-Latino whites are less likely to perceive a need for care than younger persons. Usual care has a particularly large impact among Asian Americans. Lastly, compared to married/cohabiting adults, non-Latino whites who are previously married are more likely to self-label as having a need for care, while single African Americans are less likely to perceive a need.
The second set of stratified models of Asian Americans and Latinos examined characteristics assessed only for these groups—ELP and ethnic subgroup identity (not shown). Ethnic subgroup variation in perceived need was not found within either the Asian American or the Latino groups, net of other variables in the model. Compared to U.S.-born Asian Americans, foreign-born Asian Americans overall, irrespective of ELP, are less likely to perceive a need for mental health treatment. Foreign-born nativity and ELP are not significant for Latinos.
Discussion
The current study examines how the intersections of race/ethnicity with gender and SES are associated with self-labeling, defined as perceiving that one needs treatment for mental health-related problems. Perceived need commands our attention because it plays a pivotal role in voluntary help-seeking and may contribute to mental health care disparities. A key determinant of perceived need is clinical need, indexed in this study as psychiatric disorder, nonspecific psychological distress, and social role impairments. Variation in perceived need by social status characteristics that persist net of these indicators points to potential disparities that may be passed along to the use of services, particularly among persons with psychiatric disorders. Therefore, it is imperative to have an accurate accounting of the associations between these status characteristics and perceived need.
We hypothesized that race/ethnicity combines with gender, SES, and with the related characteristic of nativity to influence perceived need. Specifically, we expected the following conditional effects: (a) high SES groups to have greater perceived need than low SES groups but only among non-Latino whites; (b) men to be less likely than women to believe a need for care, but only among non-Latino whites; and (c) foreign-born nativity to have a negative effect on perceived need among Asian American and Latino groups but not among other groups. Our findings provide some support for these conditional effects in the form of statistically significant interactions: two for the full sample—between race/ethnicity and gender and between race/ethnicity and nativity; and, one for the clinical need subsample between race/ethnicity and nativity. The impact of higher education and income on perceived need is not conditional on race/ethnicity for the total sample or the two subsamples, an unanticipated result (however, we note that an income by gender interaction was found in the African American clinical need subsample). The alternative, that each status has the same impact on perceived need irrespective of a person’s other status characteristics, operationalized as the main effects model, is preferred for the no psychiatric disorder subsample. In other words, there was no evidence of conditional effects in self-labeling for the no disorder subsample. Finally, quite a few interactions were tested and only four were statistically significant, which means that the findings overall tilt in favor of independent effects of social status characteristics on self-labeling rather than conditional effects.
Self-labeling theory posits that socially and economically disadvantaged persons are less likely than advantaged persons to apply mental illness-related labels to themselves and to engage in voluntary help-seeking. The results from the main effects models provide some support for this assertion in the total sample and clinical need subsample (with the caveat that the corresponding conditional model is the preferred model). Net of clinical need and controls, the odds of having a perceived need are lower among racial/ethnic minority groups relative to non-Latino whites, with the exception of Latinos, and among those with the lowest level of education relative to the highest. Higher education may facilitate the recognition of mental health problems by improving mental health literacy.
Furthermore, self-labeling theory implies that the person who is most likely to self-label is a well socialized actor who is experiencing abnormal states and who endorses dominant cultural perspectives toward mental health and treatment, which in contemporary American society favors the medical model of mental illness. From this perspective, the low perceived need among Asian Americans, Afro-Caribbeans (clinical need subsample only), and African Americans may stem from cultural differences in beliefs about mental illness and its etiology as well as variations in culturally-acceptable ways to respond to mental illness. The similarity in perceived need between Latinos and non-Latino whites may result from comparable or more favorable attitudes toward help-seeking and mental health services observed among these groups (Gonzalez et al. 2005, Mojtabai 2007).
In contrast, the observed gender difference contradicts this theory because women, who on average are socially and economically disadvantaged relative to men, are more likely than men to think they need care. The most likely influence for the gender exception is the continued existence of traditional gender role prohibitions against the expression of emotions and help seeking by males. Based on the main effects models, we conclude that social disadvantage is not the sole factor at work in self-labeling as it pertains to perceived need for services; some other factors appear to have the capacity to offset at least some specific manifestations of disadvantage.
However, the conditional model is preferred over the main effects model for the total sample and the clinical need subsample because differences in perceived need by gender and nativity are contingent on race/ethnicity, as indicated by the significant interactions among these variables. The first interaction applies to the total sample: overall, men have significantly lower odds than women of thinking they need help, but the magnitude of this difference varies by race/ethnicity and is only statistically significant among non-Latino whites and African Americans. We expected to find significant gender differences in non-Latino whites, but the significant difference among African Americans was unforeseen. Although masculine norms are associated with less positive attitudes towards mental health treatments, this effect seems to be particularly strong among African American men compared to European American men (Vogel et al. 2011), which may contribute to the observed low perceived need among African American men. Additionally, non-Latino white men are less likely to self-label than other women, particularly non-Latino white and Latina women, perhaps as a way to avoid stigma because they may think they have more to “lose” by adopting a mental illness label, thereby jeopardizing their dominant social status (Ojeda and Bergstresser 2008). The similarity between men and women among Asian Americans and Latinos may result from cultural norms about keeping personal and family troubles private, which may discourage both men and women from even thinking about turning toward professionals for help. This interpretation is consistent with research showing that men have significantly more negative attitudes toward mental health services than women among non-Latino whites but not Latinos (Gonzalez et al. 2005).
The second interaction applies to both the total sample and clinical need subsample: Differences in perceived need by nativity are greater among Asian Americans than other groups, in part consistent with our hypotheses; the lack of a nativity effect among Latinos was not expected. Foreign-born Asian Americans are less likely to perceive a need for mental health care than U.S.-born Asian Americans, and this difference is unexpectedly not affected by English language proficiency as evidenced in the stratified analysis. This nativity effect is consistent with reports of low utilization of mental health services among immigrant Asian Americans (Abe-Kim et al. 2007). Poorer self-labeling among Asian American immigrants compared to their U.S.-born counterparts may reflect poorer health literacy and more stringent cultural norms against disclosing private information to outsiders within immigrant subpopulations (Leong and Lau 2001). Aside from Latinos, the lack of an effect of nativity for the other groups may be a function of low rates of immigration as evidenced by the wide confidence intervals. Lastly, we did not find support for our hypothesis that other conjoined aspects of ethnicity (ELP, ethnic subgroup identity) would impact perceived need for Latinos and Asian Americans.
For the sample as a whole, our results suggest that perceiving a need for mental health care is a complex function of different dimensions of social stratification that transcend the relationships specified by self-labeling theory. Social groups that have historically experienced cumulative social and economic disadvantage theoretically should be at highest risk of not self-labeling. We observe these differences in the main effects of race/ethnicity and SES. However, the preferred conditional effects model tells a different story: social disadvantage does not always translate to poor self-labeling given paradoxical patterns in perceived need across gender and race/ethnicity. Despite their advantaged position in society, non-Latino white men have a low predicted probability of perceived need whereas these probabilities are high among non-Latino white women and among Latinos irrespective of gender. Social and economic disadvantage do not appear to be sufficient alone to account for these patterns; instead, variation in gender roles across racial/ethnic groups appear to be implicated. The idea that one disadvantaged status magnifies the impact of another disadvantaged status is not supported insofar as there were no statistically significant synergistic interactions.
Heterogeneity in the impact of SES, principally education, is seen in the within racial/ethnic groups stratified analyses for the clinical need subsample. Education is significantly associated with perceived need, but only among African Americans and non-Latino whites. Higher education is thought to convey greater knowledge about mental illnesses and their treatment, knowledge that may become relevant to perceived need primarily when people experience firsthand signs and symptoms that are recognizable as psychiatric disorders. An interaction between gender and income/poverty also was observed within the African American clinical need subsample (not shown), with income/poverty having a marginally significant negative effect on perceived need for men and not women, contrary to self-labeling theory. The high proportion of immigrant Asian Americans and Latinos may account for the absence of an education effect in these groups if strong cultural influences among immigrants offset the impact of education and income among non-immigrants.
Among persons with no disorders, only one status characteristic is associated with perceived need: men have lower odds than women, taking into consideration other status and demographic characteristics, indicators of clinical need (other than diagnosable disorder), and enabling factors (health insurance and usual source of care). Of the relevant indicators of clinical need included in this model, all are significantly associated with perceived need except lifetime psychiatric hospitalization, which is quite rare in this subsample and may have limited power. That perceived need is associated with clinical factors indicates that perceptions are grounded in genuine experiences of mental health problems, which resurrects a long-standing debate in sociology over the reification of diagnosis (Mirowsky and Ross 1989). In an ideal world, perceived need should be independent of social status when actual need is taken into account; therefore, the results for the no disorder subsample approach an absence of health disparities.
Several limitations merit mention. First, some variables could not be evaluated because they were not measured, including the impact of stigma on perceived need, which may be a source of omitted variable bias. Likewise, discrimination can negatively affect mental health treatment among racial/ethnic minority groups (Mays et al., 2017), but its impact on perceived need could not be assessed for the total sample due to extensive data missing by design. Provisional analysis suggests that discrimination is associated with perceived need only among African Americans and not Latinos or Asian Americans. Future research should more thoroughly examine this association, including discrimination experienced within the health care system. These assessments should be conducted for the entire population and not exclude non-Latino whites because all groups contain people who are at risk for discrimination on some traits, and because discrimination based on mental illness and treatment is relevant to all racial/ethnic groups.
Second, the NCS-R and NSAL did not measure perceived need directly for all respondents, but instead inferred it for respondents who used mental health services in the past 12-months and then reported that the use was voluntary; these persons skipped out of the perceived need question. This procedure is logical, but it is based on a rational choice model, whereas the process leading to treatment is often haphazard. People who “muddle through” are unsure about whether treatment was entirely voluntary or not (Pescosolido, Gardner and Lubell 1998); thus, reports of “voluntary” treatment may nevertheless reflect subtle coercion or pressure by others but the dataset does not contain measures to discern these subtleties. Yet again, the direct assessments of perceived need also are subjective assessments, mitigating this concern somewhat. That having been said, perceived need has been measured this way in several published studies using the National Comorbidity Survey and the NCS-R (Katz et al. 1997, Mojtabai et al. 2002), which supports this approach. Nevertheless, future studies should assess perceived need for all respondents prior to assessing treatment.
Third, perceived need was measured for any formal mental health provider, but racial/ethnic differences in this perception may be more disparate for some types of providers (e.g., medications) than others (e.g., medical doctors). We recommend that future research in this area directly assess perceived need for specific providers.
Lastly, clinical need was defined for three classes of mental disorders that were assessed across the three CPES datasets, meaning that there is misclassification for people who met criteria for other disorders. For example, the NLAAS did not assess bipolar disorder, unlike the NCS-R and NSAL. Consequently, mood disorders do not include bipolar disorder. Likewise, psychotic disorders were either not assessed in specific surveys or generated substantial missing data. For these reasons, the association between disorder status and perceived need may be biased. However, in sensitivity analyses of respondents with data about psychotic symptoms, there was no significant association with perceived need.
These limitations notwithstanding, the current study has a number of notable strengths, including the large probability sample that permits generalization to the U.S. adult population. The use of multiple languages means that the sample more fully represents the Asian American and Latino populations than other similar studies. The large and diverse sample also enables the examination of intersections among statuses and within-group heterogeneity, which is overlooked in existing research on perceived need. Finally, our use of perceived need as an indicator of self-labeling expands previous studies that have equated self-labeling with accounts of voluntary help-seeking (Thoits 2005) or with perceptions of illness identity (Moses 2009, Thoits 2016). The concept of perceived need aligns with self-labeling processes because it represents a pivotal antecedent that drives voluntary help-seeking—that is, the recognition that a problem requires professional intervention.
The findings from our study have theoretical implications towards the expansion of self-labeling theory. We utilized an intersectional approach to understand the social distribution of perceived need and found that intersections of race/ethnicity with other social status characteristics, particularly gender and nativity, matter to self-labeling. Incorporating an intersectionality framework into Self-Labeling Theory may better help inform our understanding of the mechanisms and social processes that lead to differential self-labeling among socially and economically disadvantaged groups. This framework asserts that the intersection of different social statuses reflects interlocking structural systems of power, privilege, and disadvantage and creates unique life experiences (e.g., discrimination, social stereotypes, etc.) that impact outcomes (Crenshaw 1989, Crenshaw 1991, Ghavami, Katsiaficas and Rogers 2016, Mays and Ghavami 2017). The application of this framework would emphasize how major social statuses and context come together to create experiences that are “more than the sum of statuses” (Crenshaw 1989, Crenshaw 1991, Mays and Ghavami 2017).
For example, racial/ethnic minority groups with high SES may not self-label as readily as high SES, non-Latino whites because of bias and discrimination within formal systems of care, which not only produces perceptions of distrust in these systems (Dovidio, Penner, Albrecht et al. 2008) but also disrupts treatment (Mays, Jones, Delany-Brumsey et al. 2017). Bauer (2014) warns, however, that imposing an intersectional approach that solely intersects social identities or positions is insufficient and recommends that these approaches also consider the examination of underlying intersectional social processes (e.g., racism, classism). Thus, adapting an intersectionality framework to self-labeling theory would not only be important for understanding self-labeling patterns across social strata, but would also reveal how various statuses and social processes associated with self-labeling may lead to disparities in mental health care utilization.
The application of an intersectionality framework to self-labeling theory raises methodological considerations. The current study examines intersections with cross-product interactions, revealing whether the effect of SES on perceived need, for example, varies significantly across racial/ethnic groups—that is, whether the impact of one status differs across another. Other approaches may focus on assessing whether self-labeling varies at different intersections by combining highly correlated social status categories into a single variable and then comparing combined groups (Hankivsky and Grace 2015). For example, merging race/ethnicity and SES as one variable would allow the comparison of perceived need between high SES non-Latino whites to low SES non-Latino whites, low SES and high SES Asian Americans, etc. This approach implies a “dissection of individuals into their stratified component identities, positions, or experiences” (pg. 15; Bauer 2014). While our study uses the former approach (i.e., examined interactions), it is the first study, to our knowledge, to provide evidence of conditional patterns in self-labeling across race/ethnicity, gender, and nativity. We recommend that future studies on self-labeling to utilize alternative statistical specifications to examine how intersections of social statuses influence differential self-labeling.
Our findings suggest practical steps to improving mental health care utilization in the U.S. As expected, worse mental health—as indexed by the presence of a recent psychiatric disorder, psychiatric hospitalizations, and so forth—consistently increase the odds of reporting a need for services across social statuses and subsamples. These findings indicate that actual need for services is the primary contributor to perceived need and is shared in common across diverse groups. Therefore, improving people’s knowledge of the signs and symptoms of psychiatric disorders may facilitate more accurate self-labeling and assessments of need for treatment. Furthermore, treatment of physical health conditions may function as a gateway to mental health service use insofar as chronic conditions and having a usual source of care are associated with seeing oneself as needing help for mental problems. It seems likely that persons routinely gain knowledge about mental disorders and their treatment at these sites, perhaps by consulting their physicians or other health professionals about problems they experience. Therefore, primary care settings may be important locations for programmatic efforts to improve people’s ability to recognize mental health problems and to consider treatment as needed.
Self-labeling processes are essential for the voluntary use of mental health services among persons with psychiatric problems. The current study provides some support to the idea that combination of multiple social status characteristics—including race/ethnicity with gender, nativity, and SES—may create barriers for specific groups for the recognition of mental health problems and realization that treatment is needed. Intervention efforts that target racial/ethnic groups with low rates of perceived need, will need to address the unique experiences of immigrants, low SES groups, and men in order to reduce disparities in mental health services utilization. More importantly, identifying the statuses and mechanisms that lead to differential self-labeling is essential to explaining why disparities in mental health care utilization exist.
Acknowledgements:
This work was supported by: the National Institutes of Health (NIH)/National Center for Advancing Translational Science (NCATS) UCLA Clinical and Translation Science Institute (CTSI) grant (TL1 TR000121), a National Institute of Mental Health (NIMH) T32 postdoctoral grant (5-T32-MH 13043), and a NIH National Institute of Minority and Minority Health Disparities Grant (MD 006923). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health and National Institute of Mental Health.
Contributor Information
Alice P. Villatoro, Columbia University.
Vickie M. Mays, University of California, Los Angeles.
Ninez A. Ponce, University of California, Los Angeles.
Carol S. Aneshensel, University of California, Los Angeles.
References
- Abe-Kim Jennifer, Takeuchi David T., Hong Seunghye, Zane Nolan, Sue Stanley, Spencer Michael S., Appel Hoa, Nicdao Ethel and Margarita Alegría. 2007. “Use of Mental Health-Related Services among Immigrant and Us-Born Asian Americans: Results from the National Latino and Asian American Study.” American Journal of Public Health 97(1):91–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría Margarita, Canino Glorisa, Ruth Ríos Mildred Vera, José Calderón Dana Rusch and Ortega Alexander N.. 2002. “Inequalities in Use of Specialty Mental Health Services among Latinos, African Americans, and Non-Latino Whites.” Psychiatric Services 53(12):1547–55. [DOI] [PubMed] [Google Scholar]
- Alegría Margarita, Takeuchi David, Canino Glorisa, Duan Naihua, Shrout Patrick, Meng Xiao-Ling, Vega William, Zane Nolan, Vila Doryliz, Woo Meghan, Vera Mildred, Guarnaccia Peter, Sergio Aguilar-Gaxiola Stanley Sue, Escobar Javier, Lin Keh-Ming and Gong Fong. 2004. “Considering Context, Place and Culture: The National Latino and Asian American Study.” International Journal of Methods in Psychiatric Research 13(4):208–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría Margarita, Mulvaney-Day Norah, Woo Meghan, Torres Maria, Gao Shan and Oddo Vanessa. 2007. “Correlates of Past Year Mental Health Services Use among Latinos: Results from the National Latino and Asian American Study.” American Journal of Public Health 97(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría Margarita, Chatterji Pinka, Wells Kenneth, Cao Zhun, Chen Chih-nan, Takeuchi David, Jackson James and Meng Xiao-Li. 2008. “Disparity in Depression Treatment among Racial and Ethnic Minority Populations in the United States.” Psychiatric Services 59:1264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvidrez Jennifer. 1999. “Ethnic Variation in Mental Health Attitudes and Service Use among Low-Income African American, Latina, and European American Young Women.” Community Mental Health Journal 35(6). [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association, ed. 2000. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: Author. [Google Scholar]
- Andersen Ronald M. and Davidson Pamela L.. 2007. “Improving Access to Care in America: Individual and Contextual Indicators” Pp. 3–32 in Changing the U.S. Health Care System: Key Issues in Health Services Policy and Management, edited by Andersen RM, Rice TH and Kominski GF. San Francisco, CA: Jossey-Bass. [Google Scholar]
- Anderson Monica. 2015. “A Rising Share of the U.S. Black Population Is Foreign Born; 9 Percent Are Immigrants; and While More Are from the Caribbean, Africans Drive Recent Growth.” Vol. Washington, D.C.: Pew Research Center. [Google Scholar]
- Aneshensel Carol S. 2013. “Mental Illness as a Career: Sociological Perspectives” in Handbook of the Sociology of Mental Health, edited by Aneshensel CS, Phelan JC and Bierman A. College Station, TX: Springer. [Google Scholar]
- Anglin Diedre M., Alberti Philip M., Link Bruce G. and Phelan Jo C.. 2008. “Racial Differences in Beliefs About the Effectiveness and Necessity of Mental Health Treatment.” Am J Community Psychol 42:17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ault-Brutus Andre and Alegría Margarita. 2016. “Racial/Ethnic Differences in Perceived Need for Mental Health Care and Disparities in Use of Care among Those with Perceived Need in 1990–1992 and 2001–2003.” Ethnicity & Health:1–16. [DOI] [PubMed] [Google Scholar]
- Bauer Amy M., Chen Chih-Nan and Margarita Alegría. 2010. “English Language Proficiency and Mental Health Service Use among Latino and Asian Americans with Mental Disorders.” Medical Care 48(12):1097–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer Amy M., Chen Chih-Nan and Margarita Alegría. 2012. “Association of Physical Symptoms with Perceived Need for and Use of Mental Health Services among Latino and Asian Americans.” Social Science & Medicine 75:1128–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer Greta R. 2014. “Incorporating Intersectionality Theory into Population Health Research Methodology: Challenges and the Potential to Advance Health Equity.” Social Science & Medicine 110:10–17. [DOI] [PubMed] [Google Scholar]
- Berger Joshua L., Addis Michael E., Green Jonathan D., Mackowiak Christopher and Goldberg Victoria. 2013. “Men’s Reactions to Mental Health Labels, Forms of Help-Seeking, and Sources of Help-Seeking Advice.” Psychology of Men & Masculinity 14(4):433–43. [Google Scholar]
- Cabassa Leopoldo J., Hansen Marissa C., Palinkas Lawrence A. and Ell Kathleen. 2008. “Azúcar Y Nervios: Explanatory Models and Treatment Experiences of Hispanics with Diabetes and Depression.” Social Science & Medicine 66(12):2413–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook Benjamin Lê, Zuvekas Samuel H., Carson Nicholas, Geoffrey Ferris Wayne, Andrew Vesperand McGuire Thomas G.. 2014. “Assessing Racial/Ethnic Disparities in Treatment across Episodes of Mental Health Care.” Health Services Research 49(1):206–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper Lisa A., Gonzales Junius J., Gallo Joseph J., Rost Kathryn M., Meredith Lisa S., Rubenstein Lisa V., Wang Nae-Yuh and Ford Daniel E.. 2003. “The Acceptability of Treatment for Depression among African American, Hispanic, and White Primary Care Patients.” Medical Care 41(4):479–89. [DOI] [PubMed] [Google Scholar]
- Crenshaw Kimberlé. 1989. “Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics.” University of Chicago Legal Forum:139– 67. [Google Scholar]
- Crenshaw Kimberlé. 1991. “Mapping the Margins: Intersectionality, Identity Politics, and Violence against Women of Color.” Stanford Law Review 43(6):1241–99. [Google Scholar]
- Dovidio John F., Penner Louis A., Albrecht Terrance L., Norton Wynne E., Gaertner Samuel L. and Shelton J. Nicole. 2008. “Disparities and Distrust: The Implications of Psychological Processes for Understanding Racial Disparities in Health and Health Care.” Social Science & Medicine 67:478–86. [DOI] [PubMed] [Google Scholar]
- Druss Benjamin G., Wang Philip S., Sampson Nancy A., Olfson Mark, Pincus Harold A., Wells Kenneth B. and Kessler Ronald C.. 2007. “Understanding Mental Health Treatment in Persons without Mental Diagnoses.” Arch Gen Psychiatry 64(10):1196–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edlund Mark J., Jürgen Unützer and Curran Geoffrey M.. 2006. “Perceived Need for Alcohol, Drug, and Mental Health Treatment.” Soc Psychiatry Psychiatr Epidemiol 41:480–87. [DOI] [PubMed] [Google Scholar]
- Falck Russel S., Wang Jichuan, Carlson Robert G., Krishnan Laura L., Leukfeld Carl and Booth Brenda M.. 2007. “Perceived Need for Substance Abuse Treatment among Illicit Stimulant Drug Users in Rural Areas of Ohio, Arkansas, and Kentucky.” Drug and Alcohol Dependence 91:107–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghavami Negin, Katsiaficas Dalal and Leoandra Onnie Rogers. 2016. “Toward an Intersectional Approach in Developmental Science: The Role of Race, Gender, Sexual Orientation, and Immigrant Status.” Advances in Child Development and Behavior 50:31–73. [DOI] [PubMed] [Google Scholar]
- Givens Jane L., Houston Thomas K., Van Voorhees Benjamin W., Ford Daniel E. and Cooper Lisa A.. 2007. “Ethnicity and Preferences for Depression Treatment.” Psychiatry and Primary Care 29:182–91. [DOI] [PubMed] [Google Scholar]
- Gonzalez Jodi M., Alegría Margarita and Prihoda Thomas J.. 2005. “How Do Attitudes toward Mental Health Treatment Vary by Age, Gender, and Ethnicity/Race in Young Adults?”. Journal of Community Psychology 33(5):611–29. [Google Scholar]
- Gonzalez Jodi M., Alegría Margarita, Prihoda Thomas J., Copeland Laural A. and Zeber John E.. 2011. “How the Relationship of Attitudes toward Mental Health Treatment and Service Use Differs by Age, Gender, Ethnicity/Race and Education.” Soc Psychiat Epidemiology 46:45–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankivsky Olena and Grace Daniel. 2015. “Understanding and Emphasizing Difference and Intersectionality in Multimethod and Mixed Methods Research.” in The Oxford Handbook of Multimethod and Mixed Methods Research Inquiry. [Google Scholar]
- Heeringa Steven G., Wagner James, Torres Myriam, Duan Naihua, Adams Terry and Berglund Patricia. 2004. “Sample Designs and Sampling Methods for the Collaborative Psychiatric Epidemiology Studies (Cpes).” International Journal of Methods in Psychiatric Research 13(4):221–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines-Martin Vicki, Malone Mary, Kim Sanggil and Ada Brown-Piper. 2003. “Barriers to Mental Health Care Access in an African American Population.” Issues in Mental Health Nursing 24:237–56. [DOI] [PubMed] [Google Scholar]
- Jackson James S., Torres Myriam, Caldwell Cleopatra H., Neighbors Harold W., Nesse Randolph M., Taylor Robert Joseph, Trierweiler Steven J. and Williams Davide R.. 2004. “The National Survey of American Life: A Study of Racial, Ethnic and Cultural Influences on Mental Disorders and Mental Health.” International Journal of Methods in Psychiatric Research 13(4):196–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson James S., Neighbors Harold W., Torres Myriam, Martin Lisa A., Williams David R. and Baser Paymond. 2007. “Use of Mental Health Services and Subjective Satisfaction with Treatment among Black Caribbean Immigrants: Results from the National Survey of American Life.” American Journal of Public Health 97(1):60–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang Yuri, Park Nan Sook, Kang Suk-Youngand Chiriboga David A.. 2014. “Racial/Ethnic Differences in the Association between Symptoms of Depression and Self-Rated Mental Health among Older Adults.” Community Mental Health Journal 50:325–30. [DOI] [PubMed] [Google Scholar]
- Jang Yuri, Yoon Hyunwoo, Chiriboga David A., Molinari Victor and Powers Daniel A.. 2015. “Bridging the Gap between Common Mental Disorders and Service Use: The Role of Self-Rated Mental Health among African Americans.” Am J Geriatr Psychiatry 23(7):658–65. [DOI] [PubMed] [Google Scholar]
- Jimenez Daniel E., Bartels Stephen J., Cardenas Veronica, Dhaliwal Sanam S. and Alegría Margarita. 2012. “Cultural Beliefs and Mental Health Treatment Preferences of Ethnically Diverse Older Adult Consumers in Primary Care.” Am J Geriatr Psychiatry 20:533–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karp David A. 1996. Speaking of Sadness. Oxford: Oxford University Press. [Google Scholar]
- Kasckow John, Ingram Erin, Brown Charlotte, Tew James D., Conner Kyaien O., Morse Jennifer Q., Haas Gretchen L., Reynolds Charles F. and Oslin David W.. 2011. “Differences in Treatment Attitudes between Depressed African American and Caucasian Veterans in Primary Care.” Psychiatric Services 62(4):426–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz Steven J., Kessler Ronald C., Frank Richard G., Leaf Philip, Lin Elizabeth and Edlund Mark. 1997. “The Use of Outpatient Mental Health Services in the United States and Ontario: The Impact of Mental Morbidity and Perceived Need for Care.” American Journal of Public Health 87(7):1136–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand S-LT, Manderscheid RW, Walters EE and Zaslavsky AM. 2003. “Screening for Serious Mental Illness in the General Population.” Archives of General Psychiatry 60(2):184–89. [DOI] [PubMed] [Google Scholar]
- Kessler Ronald C., Berglund Patricia A., Bruce Martha L., Koch J. Randy, Laska Eugene M., Leaf Philip J., Manderscheid Ronald W., Rosenheck Robert A., Walters Ellen E. and Wang Philip S.. 2001. “The Prevalence and Correlates of Untreated Serious Mental Illness.” Health Services Research 36(6):987–1007. [PMC free article] [PubMed] [Google Scholar]
- Kessler Ronald C. and Merikangas Kathleen R.. 2004. “The National Comorbidity Survey Replication (Ncs-R): Background and Aims.” International Journal of Methods in Psychiatric Research 13(2):60–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler Ronald C. and Üstün T. Bedirhan. 2004. “The World Mental Health (Wmh) Survey Initiative Version of the World Health Organization (Who) Composite International Diagnostic Interview (Cidi).” International Journal of Methods in Psychiatric Research 13(2):93–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimerling Rachel and Baumrind Nikki. 2005. “Access to Specialty Mental Health Services among Women in California.” Psychiatric Services 56:729–34.15939951 [Google Scholar]
- Leong Frederick T. L. and Lau Anna S. L.. 2001. “Barriers to Providing Effective Mental Health Services to Asian Americans.” Mental Health Services Research 3(4):201–14. [DOI] [PubMed] [Google Scholar]
- Lin Keh-Ming and Cheung Freda. 1999. “Mental Health Issues for Asian Americans.” Psychiatric Services 50:774–80. [DOI] [PubMed] [Google Scholar]
- Mackenzie Corey S., Pagura Jina and Sareen Jitender. 2010. “Correlates of Perceived Need for and Use of Mental Health Services by Older Adults in the Collaborative Psychiatric Epidemiology Surveys.” American Journal of Geriatric Psychiatry 18(12):1103–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays Vickie M. and Ghavami N. 2017. “History, Aspirations, and Transformations of Intersectionality: Focusing on Gender” in American Psychological Association Handbook of the Psychology of Women, Vol. 1, edited by Travis C and White J. [Google Scholar]
- Mays Vickie M., Jones Audrey L., Ayesha Delany-Brumsey Courtney Coles and Cochran Susan. 2017. “Perceived Discrimination in Health Care and Mental Health/Substance Abuse Treatment among Blacks, Latinos, and Whites.” Medical Care 55(2):173–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechanic David. 2003. “Is the Prevalence of Mental Disorders a Good Measure of the Need for Services?”. Health Affairs 22(5):8–20. [DOI] [PubMed] [Google Scholar]
- Mirowsky John and Ross Catherine E.. 1989. “Psychiatric Diagnosis as Reified Measurement.” Journal of Health and Social Behavior 30(1):11–25. [PubMed] [Google Scholar]
- Mojtabai Ramin, Olfson Mark and Mechanic David. 2002. “Perceived Need and Help-Seeking in Adults with Mood, Anxiety, or Substance Use Disorders.” Arch Gen Psychiatry 59:77–84. [DOI] [PubMed] [Google Scholar]
- Mojtabai Ramin. 2007. “Americans’ Attitudes Towards Mental Health Treatment Seeking: 1990–2003.” Psychiatric Services 58:642–51. [DOI] [PubMed] [Google Scholar]
- Mojtabai Ramin. 2009. “Americans’ Attitudes toward Psychiatric Medications: 1998–2006.” Psychiatric Services 60(8):1015–23. [DOI] [PubMed] [Google Scholar]
- Mojtabai Ramin, Olfson Mark, Sampson Nancy A., Jin Robert, Druss Benjamin, Wang Philip S., Wells Kenneth B., Pincus Harold A. and Kessler Ronald C.. 2011. “Barriers to Mental Health Treatment: Results from the National Comorbidity Survey Replication.” Psychological Medicine 41:1751–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moses Tally. 2009. “Self-Labeling and Its Effects among Adolescents Diagnosed with Mental Disorders.” Social Science & Medicine 68:570–78. [DOI] [PubMed] [Google Scholar]
- Nadeem Erum, Lange Jane M. and Miranda Jeanne. 2009. “Perceived Need for Care among Low-Income Immigrant and U.S.-Born Black and Latina Women with Depression.” Journal of Women’s Health 18(3):369–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narendorf Sarah Carter and Palmer Ashley. 2016. “Perception of Need and Receipt of Mental Health Treatment: A Three-Group Comparison of Young Adults with Psychological Distress.” Psychiatric Services 67:924–27. [DOI] [PubMed] [Google Scholar]
- Neighbors Harold W., Caldwell Cleopatra, Williams David R., Nesse Randolph, Taylor Robert Joseph, Bullard Kai McKeever, Torres Myriam and Jackson James S.. 2007. “Race, Ethnicity, and the Use of Services for Mental Disorders: Results from the National Survey of American Life.” Arch Gen Psychiatry 64:485–94. [DOI] [PubMed] [Google Scholar]
- Nguyen Ann W., Taylor Robert Joseph, Peterson Tina and Chatters Linda M.. 2013. “Health, Disability, Psychological Well-Being, and Depressive Symptoms among Older African American Women.” Women, Gender, and Families of Color 1(2):105–23. [Google Scholar]
- Nguyen Duy. 2011. “Acculturation and Perceived Mental Health Need among Older Asian Immigrants.” Journal of Behavioral Health Services & Research 38(4):526–32. [DOI] [PubMed] [Google Scholar]
- Norton Edward C., Wang Hua and Ai Chunrong. 2003. “Computing Interaction Effects and Standard Errors in Logit and Probit Models.” The Stata Journal 4(2):154–67. [Google Scholar]
- Ojeda Victoria D. and McGuire Thomas G.. 2006. “Gender and Racial/Ethnic Differences in Use of Outpatient Mental Health and Substance Use Services by Depressed Adults.” Psychiatric Quarterly 77:211–22. [DOI] [PubMed] [Google Scholar]
- Ojeda Victoria D. and Bergstresser Sara M.. 2008. “Gender, Race-Ethnicity, and Psychosocial Barriers to Mental Health Care: An Examination of Perceptions and Attitudes among Adults Reporting Unmet Need.” Journal of Health and Social Behavior 49(3):317–34. [DOI] [PubMed] [Google Scholar]
- Pescosolido Bernice A., Gardner Carol Brooksand Lubell Keri M.. 1998. “How People Get into Mental Health Services: Stories of Choice, Coercion and “Muddling Throught” from “First Timers”.” Social Science and Medicine 46(2):275–86. [DOI] [PubMed] [Google Scholar]
- Pescosolido Bernice A., Boyer Carol A. and Medina Tait R.. 2013. “The Social Dynamics of Responding to Mental Health Problems” Pp. 505–24 in Handbook of the Sociology of Mental Health, edited by Aneshensel CS, Bierman A and Phelan JC: Springer. [Google Scholar]
- Rosenfield Sarah. 2012. “Triple Jeopardy? Mental Health at the Intersection of Gender, Race, and Class.” Social Science & Medicine 74:1791–801. [DOI] [PubMed] [Google Scholar]
- Rosenfield Sarah and Mouzon Dawne. 2013. “Gender and Mental Health” Pp. 277–96 in Handbook of the Sociology of Mental Health, edited by Aneshensel CS, Bierman A and Phelan JC. College Station, TX: Springer. [Google Scholar]
- Rubin Donald. 1987. Multiple Imputation for Non-Respondents in Surveys. New York: Wiley & Sons. [Google Scholar]
- Sareen Jitender, Cox Brian J., Afifi Tracie O., Clara Ian and Yu Bo Nancy. 2005. “Perceived Need for Mental Health Treatment in a Nationally Representative Canadian Sample.” Canadian Journal of Psychiatry 50:643–51. [DOI] [PubMed] [Google Scholar]
- Schnittker Jason, Pescosolido Bernice A. and Croghan Thomas A.. 2005. “Are African Americans Really Less Willing to Use Health Care?”. Social Problems 52(2):255–71. [Google Scholar]
- Schnittker Jason. 2013. “Public Beliefs About Mental Illness” Pp. 75–93 in Handbook of the Sociology of Mental Health, edited by Aneshensel CS, Bierman A and Phelan JC: Springer. [Google Scholar]
- Sentell Tetine and Braun Kathryn. 2012. “Low Health Literacy, Limited English Proficiency, and Health Status in Asians, Latinos, and Other Racial/Ethnic Groups in California.” Journal of Health Communication 17:82–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. 2015. “Stata Statistical Software: Release 14.” College Station, TX: StataCorp LP. [Google Scholar]
- Taylor, Joseph Robert, Woodward Amanda Toler, Chatters Linda M., Mattis Jacqueline S. and Jackson James S.. 2011. “Seeking Help from Clergy among Black Caribbeans in the United States.” Race and Social Problems 3(4):241–51. [Google Scholar]
- Thoits Peggy. 2011. “Perceived Social Support and the Voluntary, Mixed, or Pressured Use of Mental Health Services.” Society and Mental Health 1(1):4–19. [Google Scholar]
- Thoits Peggy A. 1985. “Self-Labeling Processes in Mental Illness: The Role of Emotional Deviance.” American Journal of Sociology 91(2):221–49. [Google Scholar]
- Thoits Peggy A. 2005. “Differential Labeling of Mental Illness by Social Status: A New Look at an Old Problem.” Journal of Health and Social Behavior 46:102–19. [DOI] [PubMed] [Google Scholar]
- Thoits Peggy A. 2016. ““I’m Not Mentally Ill”: Identity Deflection as a Form of Stigma Resistance.” Journal of Health and Social Behavior 57(2):135–51. [DOI] [PubMed] [Google Scholar]
- Thompson Vetta L. Sanders, Baxile Anita and Akbar Maysa. 2004. “African Americans’ Perceptions of Psychotherapy and Psychotherapists.” Professional Psychology: Research and Practice 35(1):19–26. [Google Scholar]
- Tuithof M, ten Have M, van den Brink W, Vollebergh W and de Graaf R. 2016. “Treatment Seeking for Alcohol Use Disorders: Treatment Gap or Adequate Self-Selection?”. European Addiction Research 22(5):277–85. [DOI] [PubMed] [Google Scholar]
- Vogel David L., Heimerdinger-Edwards Sarah R., Hammer Joseph H.and Hubbard Asale. 2011. ““Boys Don’t Cry”: Examination of the Links between Endorsement of Masculine Norms, Self-Stigma, and Help-Seeking Attitudes for Men from Diverse Backgrounds.” Journal of Counseling Psychology 58(3):368–82. [DOI] [PubMed] [Google Scholar]
- Wang Philip S., Lane Michael, Olfson Mark, Pincus Harold A., Wells Kenneth B. and Kessler Ronald C.. 2005. “Twelve-Month Use of Mental Health Services in the United States: Results from the National Comorbidity Survey Replication.” Arch Gen Psychiatry 62:629–40. [DOI] [PubMed] [Google Scholar]
- WHO. 2001. “World Health Organization Disability Assessment Schedule Ii.” Vol. Geneva, Switzerland: World Health Organization. [Google Scholar]
- Woodward Amanda T., Chatters Linda M., Taylor Robert Joseph, Neighbors Harold W.and Jackson James S.. 2010. “Differences in Professional and Informal Help Seeking among Older African Americans, Black Caribbeans, and Non-Hispanic Whites.” Journal of the Society for Social Work and Research 1(3):124–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Lawrence H. and Benson J. 2016. “The Role of Culture in Population Mental Health: Prevalence of Mental Disorders among Asian and Asian American Populations” in The Oxford Handbook of Cultural Neuroscience, edited by Chiao JY, Li S-C, Seligman R and Turner R: Oxford University Press. [Google Scholar]
- Zong Jie and Batalova Jeanne. 2015, “Frequently Requested Statistics on Immigrants and Immigration in the United States”: Migration Policy Institute. Retrieved September 9, 2015 (http://www.migrationpolicy.org/article/frequently-requested-statistics-immigrants-and-immigration-united-states-Demographic,%20Educational,%20and%20Linguistic). [Google Scholar]


