Supplemental Digital Content is available in the text.
Abstract
Background:
Ambient particulate matter (PM) and nitrogen oxide (NOx) air pollution may be diabetogenic.
Objective:
To examine longitudinal associations of short- and longer-term mean PM ≤10 μm (PM10), PM ≤2.5 μm (PM2.5), and NOx concentrations with five biomarkers of diabetes risk.
Methods:
We studied a stratified, random minority oversample of nondiabetic Women’s Health Initiative clinical trials participants with biomarkers and geocoded participant address-specific mean air pollution concentrations available at repeated visits (years = 1993–2004; n = 3,915; mean age = 62.7 years; 84% white). We log-transformed the biomarkers, then used multi-level, mixed-effects, longitudinal models weighted for sampling design/attrition and adjusted for sociodemographic, clinical, and meteorological covariates to estimate their associations with air pollutants.
Results:
Biomarkers exhibited null to suggestively negative associations with short- and longer-term PM10 and NOx concentrations, e.g., −3.1% (−6.1%, 0.1%), lower homeostatic model assessment of insulin resistance per 10 μg/m3 increase in 12-month PM10. A statistically significant interaction by impaired fasting glucose (IFG) at baseline in this analysis indicated potentially adverse effects only among women with versus without IFG, i.e., 1.4% (−3.5%, 6.5%) versus −4.6% (−7.9%, −1.1%), Pinteraction < 0.05. In contrast, longer-term PM2.5 concentrations were largely but not statistically significantly associated with higher biomarkers.
Conclusions:
Low-level short-term PM10 and NOx concentrations may have negligible adverse effects on biomarkers of diabetes risk. Although longer-term mean PM2.5 concentrations showed primarily null associations with these biomarkers, results suggestively indicated that PM2.5 exposure over the range of concentrations experienced in the United States may adversely affect biomarkers of diabetes risk at the population level, as may longer-term mean PM10 concentrations among women with IFG.
What this study adds
Examining longitudinal associations at lower exposures adds to the understanding of the relationship between air pollution, diabetes, and its related biomarkers. The study expands upon existing literature by focusing on a longitudinal population exposed to air pollution concentrations typically experienced in the United States and other countries with lower average air pollution exposure. Further, the focus on Women’s Health Initiative participants identified otherwise healthy women with impaired fasting glucose as a population potentially susceptible to the effects of air pollution on markers of diabetes risk.
Introduction
Diabetes mellitus, a metabolic disorder characterized by glucose dysregulation and insulin resistance, is a globally important cause of morbidity and mortality due to its high and increasing prevalence worldwide.1 In addition to traditional risk factors for diabetes (e.g., energy-rich diet, physical inactivity, and overweight/obesity), epidemiologic evidence suggests that longer-term mean ambient air pollution concentrations are associated with higher risk of incident diabetes,2–10 particularly among women.2 Endothelial dysfunction, visceral adipose inflammation, hepatic insulin resistance, and pulmonary oxidative stress have been implicated as plausible biological mechanisms by which air pollution may affect diabetogenesis.8–12
Recent epidemiologic studies also suggest that longer-term mean ambient particulate matter (PM) and nitrogen oxide (NOx) concentrations are associated with biomarkers of impaired glucose homeostasis and insulin resistance.13–23 Studies of shorter-term mean concentrations are sparse, but yield mostly consistent positive associations.17,23–29 Extant studies also indicate that prediabetes may exacerbate the adverse effects of air pollution on these biomarkers.13,29 However, current evidence examining short- and longer-term mean concentrations largely relies on cross-sectional studies13,15–21,26,27,29 with limited generalizability due to focus on adolescents,15,18,19 the elderly,14,24,28 or pregnant women.26
Accordingly, the present study aimed to determine whether short- and longer-term mean ambient PM and NOx concentrations are longitudinally associated with repeated, interval-scale measures of biomarkers of diabetes risk (fasting glucose, fasting insulin, homeostatic model assessment of insulin resistance [HOMA-IR], the ratio of triglycerides to high-density lipoprotein cholesterol [TG:HDL-C], and the triglyceride-glucose index [TyG]), including effect modification by impaired fasting glucose (IFG) status, in a well-characterized cohort of nondiabetic, postmenopausal women with and without IFG living in the 48 contiguous United States.
Methods
Study design and population
The methods of the Women’s Health Initiative clinical trials (WHI CT) have been detailed elsewhere.30 Briefly, the WHI CT were designed to evaluate the effects of hormone therapy (estrogen ± progesterone), calcium/vitamin D supplementation, and dietary modification (low-fat, high fruit, vegetable, and grain diet) on the risk of breast and colorectal cancer, cardiovascular disease, and bone fractures. Between 1993 and 1998, the trials enrolled 68,132 postmenopausal female volunteers aged 50–79 years from one of the 76 US examination centers (including satellite clinics, remote sites and their changes in location over time). These women were recruited using, e.g., residential mailing lists, media announcements, and participation in health screening programs or health maintenance organizations. The present study examines a center- and race-stratified ~6% random, minority oversample of WHI CT participants with repeated measures of fasting glucose, fasting insulin, and geocoded address coordinates. Participants (N = 4019) were eligible if they were free of diabetes at their screening visit and underwent phlebotomy at the screening visit or annual visits 1, 3, or 6 (1993–2004). Participants were included through annual visit 6 unless their WHI follow-up ended or they developed diabetes, as defined below (See Figure S1 of Supplemental Digital Content; http://links.lww.com/EDE/B555). Recruitment, consent, and data collection were overseen by institutional review boards at the WHI Clinical Coordinating Center in the Fred Hutchinson Cancer Research Center and the 40 WHI clinical centers. All participants provided written informed consent
Biomarkers of diabetes risk
Fasting (>9 hours) serum and EDTA-treated plasma collected at the screening and annual visits 1, 3, or 6 (1993–2004) were frozen at −70°C and shipped to Medical Research Laboratories (MRC, Highland Heights, KY). Serum glucose and plasma lipids were assayed on a Hitachi 747 analyzer, glucose by the hexokinase method and HDL-C via isolation using heparin-manganese chloride.31–33 Serum insulin was measured by radioimmunoassay or on an ES 300 analyzer (Boehringer Mannheim Diagnostics, Indianapolis, Indiana) in a stepwise sandwich enzyme-linked immunosorbent assay.34 Results of the two methods were comparable at insulin concentrations <60 µIU/ml. Moreover, intra-class correlation coefficients among 564 WHI participants with repeatedly measured analyte concentrations obtained 8–15 weeks apart were 0.71 (insulin, µIU/ml), 0.83 (glucose, mg/dl), 0.80 (triglycerides, mg/dl), and 0.89 (HDL-C, mg/dl).35 Three additional biomarkers of diabetes risk were estimated from these analytes. HOMA-IR was estimated as the product of insulin × glucose divided by 22.5,36 TG:HDL-C as a simple quotient,37 and TyG as the natural log-transformed product of (TG × glucose × 0.5).38 The American Diabetes Association definition was used to define IFG (glucose = 100–125 mg/dl) and diabetes (fasting glucose ≥126 mg/dl or nonfasting glucose ≥200, antidiabetic medication use, or self-reported history of previous physician diagnosis).39,40
Other participant characteristics
Clinical trial membership, randomly assigned treatment group, self-reported sociodemographic variables (age, race/ethnicity, education), and family history of diabetes were established at the screening visit. Using standardized instruments, relevant behaviors (current smoking; current alcohol use) were identified, use of oral or injectable anti-diabetic medications inventoried, and total energy expenditure (metabolic equivalent-hours/week) calculated based on the type, frequency, and duration of recreational physical activity at both the screening and annual visits. Anthropometrics (height, weight) also were measured at these visits and used to calculate body mass index (BMI; kg/m2). Between visits, incident comorbidities (such as myocardial infarction, congestive heart failure, cancer, and stroke) and use of anti-diabetic medications were identified by semiannual questionnaires and validated.41
Air pollution assessment
Participant addresses were collected at each visit, updated at least biannually (1993–2004), and geocoded.42,43 Two methods were then used to estimate exposure to ambient air pollutants because the study period included time before daily PM2.5 monitoring was initiated (1999). The first method involved spatially estimating a series of geocoded participant address-specific daily mean concentrations of ambient PM ≤ 10 μm in diameter (PM10, µg/m3) and NOx (ppb) using US Environmental Protection Agency Air Quality System (EPA AQS) monitored concentrations44 (see Figures S2–4 of Supplemental Digital Content; http://links.lww.com/EDE/B555 for monitor locations) and a semi-automated program.45–47 The program used a spherical model to perform national-scale, log-normal ordinary kriging with a weighted least squares method to estimate semi-variograms. This model has been previously cross-validated in WHI with prediction errors near 0 for PM10 and over 95% of average prediction errors within 2 µg/m3 of measured PM10.45 Because biomarkers of diabetes risk can acutely rise and fall but also tend to be chronically higher among individuals at risk of developing diabetes, we averaged estimated daily mean PM10 and NOx concentrations over the 2- to 7-day, and 365-day periods ending on the WHI visit dates (representing short- and long-term exposures). We compared associations of the 2- to 7-day means with the biomarkers of diabetes risk and assessed model fit using the Akaike Information Criterion values. Because models of the 2-day mean concentrations averaged over the day of and preceding the WHI visit produced the strongest associations and were best fitting, we focused on 2 days as the short-term averaging period in further analysis.
Comparably estimated daily mean concentrations of ambient PM ≤2.5 μm in diameter (PM2.5, µg/m3) were not available for the entire study period because US EPA AQS monitoring data for PM2.5 did not become widely available until 1999. Hence, we also used a second method to estimate ambient PM exposures at high spatial and temporal resolution.48 The second method involved spatiotemporally estimating a series of geocoded participant address-specific monthly mean concentrations of ambient PM2.5 and PM10 using the log-transformed ratio of PM2.5 to predicted PM10, geospatial predictors (elevation, urban land use, county population density, distance to nearest A1, A2, and A3 roads, point source emissions, meteorological variables), and generalized additive mixed models. We averaged the monthly mean concentrations over the 12-month periods ending on the WHI visit dates.48 Cross-validation of these models has been reported with R2 = 0.77 for PM2.5 and R2 = 0.58 for PM10. Exposure data for N = 95 participants living outside the contiguous United States could not be estimated with these models (Figure S1, Supplemental Digital Content; http://links.lww.com/EDE/B555).
Other contextual characteristics
Weather data from all National Climatic Data Center stations were used to estimate corresponding measures of geocoded address-specific mean temperature (°C), dew point (°C) and barometric pressure (kPa). US Census 2000 data were used to estimate address-specific neighborhood socioeconomic status (nSES) as a sum of six, z-transformed measures of wealth, income, education, and occupation.49
Statistical analyses
To facilitate inference to the entire WHI CT population, all analyses adjusted for unequal center- and race-specific sampling and for unequal visit- and comorbidity-specific participation. Adjustment involved weighting for the appropriately scaled, inverse product of the joint (sampling by participation) probabilities.50 All analyses also relied on outcome, exposure and covariate data previously subjected to flexible, multivariate imputation of infrequently missing values (maximum missing exposure was 12.8% for 365-day average PM10 and NOx at the screening visit and maximum missing outcome was 20.3% for HOMA-IR and TG:HDL-C at annual visit 6).51,52 The multiply imputed data were used to estimate exposure-outcome associations in weighted, longitudinal, multi-level, linear mixed-effects models, as follows:
where Yijk is a log-transformed biomarker at the ith visit (level 1) of the jth participant (level 2) in the kth center (level 3); β1-β4 are fixed effects; and b1–b2 and e are random effects. In this model, Pijk is the pollutant concentration, tijk is time since the screening visit, and Cijk is a vector of covariates including trial membership (hormone replacement therapy, calcium/vitamin D supplementation, or dietary modification), clinical trial treatment group, age (years), race/ethnicity, education (college graduate vs. not), nSES, current smoking, current alcohol use, recreational energy expenditure (metabolic equivalent-hours/week), BMI (kg/m2), family history of diabetes, season, day of the week, temperature (°C), dew point (°C), and barometric pressure (kPa). The terms b1k3 and b2k3 are the random intercept and slope for the pollutant concentration at level 3, b1jk2 and b2jk2 are the random intercept and slope for time at level 2, and eijk is the random error at level 1. Associations among nondiabetic participants with versus without IFG were estimated by including a pollutant × IFG interaction term in the former model. Sensitivity of estimation to handling of center as a fixed versus random effect also was examined. All analyses were conducted using the XTMIXED function in STATA 15 (STATA, College Station, Texas).
Results
Participants were largely born before World War II (n = 3,915; mean age at recruitment: 62.7 years), non-Hispanic white and high-school educated (Table 1). Examinations between 1993 and 2004 occurred in all seasons and most often on weekdays, with relatively few participants reporting a family history of diabetes, current smoking, abstaining from alcohol, or regular exercise. The mean BMI at screening was 28.7 kg/m2 (Table 2). Although IFG was prevalent (n = 1,013; weighted prevalence: 24.9%, 95% confidence interval [CI] = 23.1, 26.6%), mean fasting glucose (94.1 mg/dl) was within the normal range. Corresponding means of insulin, HOMA-IR, TG:HDL-C, and TyG were 10.9, 2.6, 2.9, and 8.7 µIU/ml, respectively, with little variation across visits (Table 2; Figure S5, Supplemental Digital Content; http://links.lww.com/EDE/B555). Participants contributed a mean (SD) follow-up time of 2,136 (469) days over a mean (SD) of 2.4 (1.1) visits.
Table 1.
Weighted demographic and behavioral characteristics at screening (1993–1998), WHI CT.
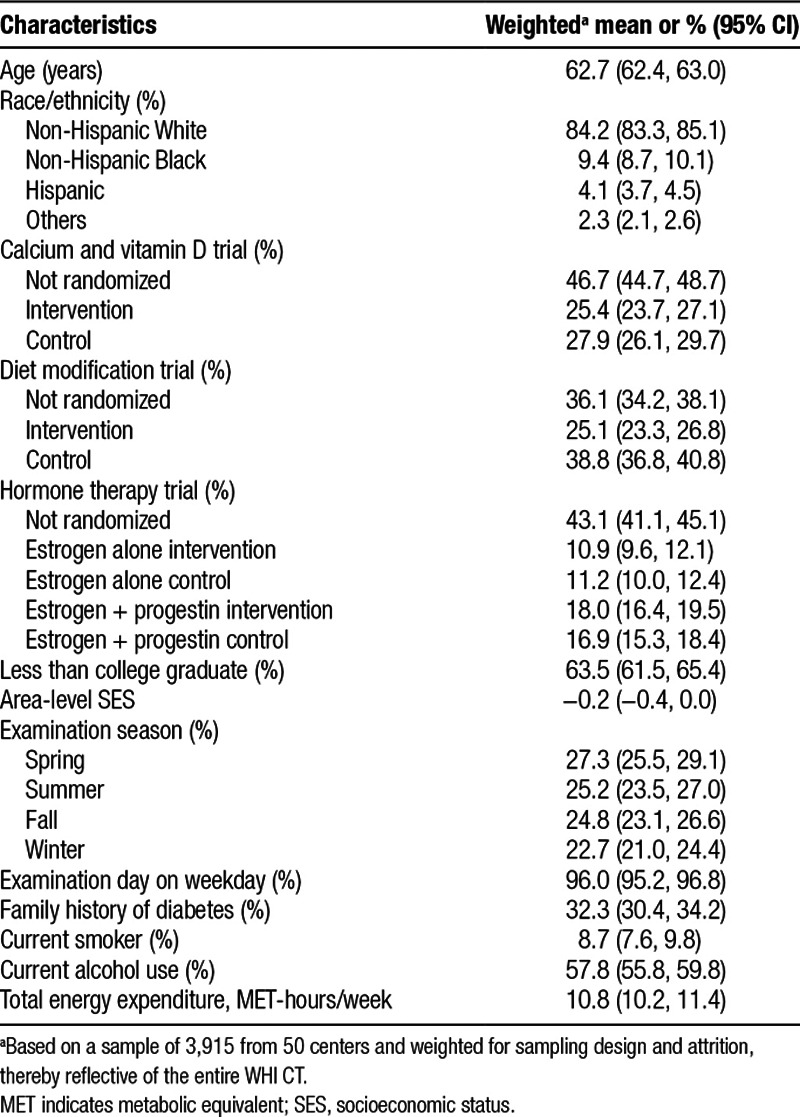
Table 2.
Weighted clinical and contextual characteristics at screening (1993–1998), WHI CT.
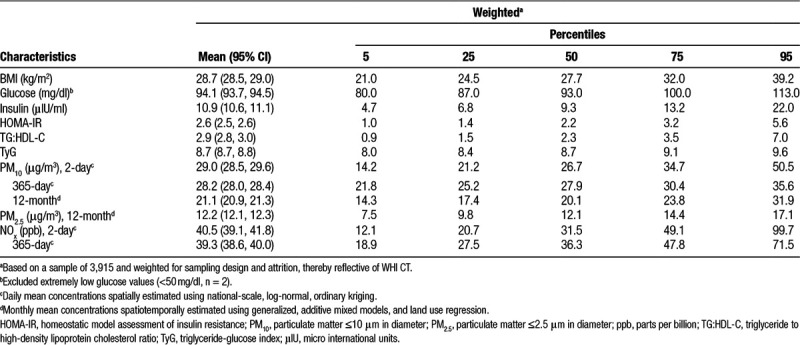
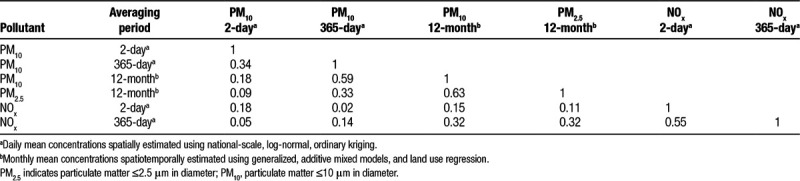
Participants, monitors, and exam sites were located throughout the contiguous United States, including representation in all 10 EPA regions (Figures S2–S4, Supplemental Digital Content; http://links.lww.com/EDE/B555). The median distance between geocoded participant addresses and nearest PM or NOx monitors was 7.4–15.0 km. Air pollutant concentrations and meteorological measures varied seasonally with PM10 and NOx means lower than and PM2.5 means slightly higher than US National Ambient Air Quality Standards in place at the time of examination53,54 (Table 2; Figure S5, Supplemental Digital Content; http://links.lww.com/EDE/B555). In general, correlation among pollutants was low. The highest Pearson correlations were observed for spatiotemporally estimated 12-month mean PM10 and PM2.5 concentrations (r = 0.63), spatiotemporally estimated 12-month and spatially estimated 365-day mean PM10 concentrations (r = 0.59), and spatially estimated 2- and 365-day mean NOx concentrations (r = 0.55) (Table 3).
Table 3.
Pearson correlations among air pollutant concentrations at screening (1993–1998), WHI CT.
We found little evidence to suggest that short-term mean PM10 and NOx concentrations were associated with biomarkers of diabetes risk. Indeed, the multi-variable adjusted models for the overall sample showed a null-to-suggestively negative association between biomarkers of diabetes risk and short-term mean pollutant concentrations (Table 4). For example, the percent changes (95% CI) in fasting glucose, fasting insulin, HOMA-IR, TG:HDL-C, and TyG per 10 µg/m3 increase in the 2-day mean PM10 concentration were −0.1% (−0.5, 0.2), −0.9% (−1.8, 0.0), −1.0% (−2.0, 0.0), 0.0% (−1.1, 1.2), and −0.1% (−1.0, 0.9), respectively. Corresponding percent changes per interquartile range (IQR) increase (28.4 ppb) in the 2-day mean NOx concentration were −0.2% (−0.7, 0.2), −0.4% (−1.4, 0.7), −0.6% (−2.1, 0.9), −0.2% (−1.4, 0.9), and −0.4% (−1.6, 0.8).
Table 4.
Percent change in biomarkers of diabetes risk (95% CI) per unit increase in air pollution concentration (1993–2004), WHI CT.
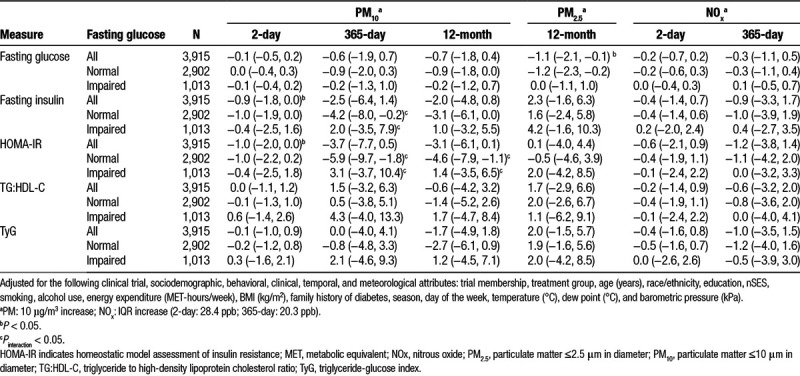
Similarly, there was little evidence to suggest that longer-term mean PM10 and NOx concentrations were associated with higher biomarkers of diabetes risk. For example, percent changes in fasting glucose, fasting insulin, HOMA-IR, TG:HDL-C, and TyG were −0.6% to −0.7%, −2.0 to −2.5%, −3.1 to −3.7%, −0.6 to 1.5%, and −1.7 to 0.0% per 10 µg/m3 increment in the 365-day and 12-month mean PM10 concentrations, respectively; and −0.3%, −0.9%, −1.2%, −0.6%, and −1.0% per IQR (20.3 ppb) increase in the 365-day mean NOx concentration with CIs that uniformly crossed the null. In contrast, longer-term mean PM2.5 concentrations were associated with positive, nonstatistically significant changes across some biomarkers of diabetes risk, including 2.3%, 1.7%, and 2.0% increases in fasting insulin, TG:HDL-C, and TyG per 10 µg/m3 increase in the 12-month mean PM2.5 concentration. Although these estimates were statistically null at α = 0.05, P-value functions for these analyses were shifted towards a positive association (Figure S6, Supplemental Digital Content; http://links.lww.com/EDE/B555). The exception was a −1.1% (−2.1, −0.1) change in fasting glucose per 10 µg/m3 increase in the 12-month PM2.5 concentration.
Interaction models demonstrated statistically significant heterogeneity of the effect of longer-term mean PM10 concentrations on fasting insulin and HOMA-IR among those with versus without IFG (P < 0.05). In these cases, percent changes were positive among participants with IFG and negative among those with normal fasting glucose, e.g., for HOMA-IR, 3.1% (−3.7%, 10.4%) versus −5.9% (−9.7%, −1.8%) per 10 µg/m3 increase in 365-day mean PM10 concentration. Although stratified point estimates for those with IFG were imprecise and non-significant at α = 0.05, they again favored a potentially adverse effect when considering the full P-value function. This pattern held for several other biomarkers of diabetes risk at nearly all pollutants, although without statistically significant interaction.
Unadjusted results can be found in Supplemental Table 2; http://links.lww.com/EDE/B555. Sequential addition of covariate groupings did not materially change estimates. Results were not materially different in sensitivity analyses treating WHI clinical center as a fixed rather than random effect (data not shown).
Discussion
In this large, longitudinal study of ambient air pollution in the United States, we found little evidence that low-levels of short- or longer-term mean ambient PM10 or NOx concentrations are significantly associated with adverse changes in biomarkers of diabetes risk. However, results were suggestive of a potential adverse effect of longer-term mean PM2.5 concentrations on these biomarkers, and women with IFG were identified as a group with potentially increased susceptibility to longer-term mean PM10 concentrations.
Because multiple metabolic pathways are involved in the onset of type 2 diabetes, this article focused on the effect of air pollution on several validated blood-based biomarkers of diabetes risk commonly used to identify high-risk populations while providing insight into diabetes risk and pathophysiology: fasting glucose, fasting insulin, HOMA-IR, TG/HDL-C, and TyG. The latter four biomarkers were previously developed because the various metabolic disturbances observed before diabetes onset can be difficult to assess in routine settings.55 Indeed, while fasting glucose is commonly used to identify hyperglycemia in the clinical context, fasting insulin reflects the secretion and action of the corresponding pancreatic hormone, and HOMA-IR, the TG/HDL-C ratio, and TyG are surrogate markers of insulin resistance and action. Both short- and long-term air pollution exposure may affect all of them because each biomarker can acutely rise and fall in response to stimuli, yet clusters at higher values on repeated measurement among individuals at risk of developing diabetes.
In contrast to previous longitudinal studies that found associations between increased short-term mean air pollutant concentrations, fasting blood glucose,24,25,28 and HOMA-IR,28 the present study found little evidence supportive of a positive association between 2-day mean PM10 concentrations and these biomarkers of diabetes risk. Rather, our results were suggestive of a negative association between short-term pollutant levels and these biomarkers, potentially reflecting an initially adaptive response to short-term mean air pollutant concentrations in which glucose homeostasis is reestablished and insulin sensitivity is improved. This finding aligns with the theory that short-term mean concentrations may induce endoplasmic reticulum stress, trigger the adaptive unfolded protein response in the liver, and restore glucose homeostasis, while longer-term mean concentrations and the resulting endoplasmic reticulum stress may lead to pancreatic beta cell apoptosis and exacerbated hyperglycemia.56–58 The latter possibility is consistent with the suggestive associations of longer-term mean air pollutant concentrations and biomarkers of diabetes risk observed herein among postmenopausal women with IFG.
Alternatively, differences in findings could be due to the populations under study, differences in the average air pollution exposure concentrations in the populations, or to differences in exposure averaging durations. For example, the lack of positive associations between short-term mean PM10 and NO2 concentrations and biomarkers of diabetes risk in the present study may reflect its focus on relatively healthy, postmenopausal women living in the United States. Indeed, two studies in which adverse associations were previously identified focused on Asian populations in which average fasting glucose concentrations were higher and diabetes was prevalent. This distinction is important because relatively healthy participants have greater homeostatic capacity to counteract hyperglycemic perturbations. Further, pollutant concentrations in these Asian populations exceeded those typically encountered in the United States. For example, the 2-day mean PM10 concentration was 29.0 μg/m3 herein versus 1- to 11-day means ranging from 42.6 to 106.9 μg/m3 in previous studies from China and Korea.25,28 Positive associations were also observed between PM, blood glucose, and hemoglobin A1c (HbA1c) among German participants.23 This study observed stronger associations between 2 and 4 months mean PM and HbA1c, a measure of glucose homeostasis over the preceding 2–3 months, but associations with blood glucose were strongest for PM2.5 averaged over 7–45 days. However, HbA1c and PM2.5 over such durations were unavailable for comparison herein.
We assessed whether IFG modified the association between air pollution and markers of diabetes risk and observed significantly different effects among those with versus without IFG. Susceptibility of individuals with IFG to adverse effects of air pollution has been reported in other studies. Notably, cross-sectional effects of annual PM10 and NOx concentration on HOMA-IR and insulin were strongest among prediabetic individuals in the German KORA study and appeared to drive associations in a combined nondiabetic, prediabetic, and diabetic population.13 Similarly, a cross-sectional study of over 130,000 Israeli patients in a Health Maintenance Organization found significantly stronger effects of 1- and 2-day NO2 concentration on serum glucose among those with versus without IFG.29 Taken together, this literature suggests that individuals with IFG may be vulnerable to the diabetogenic effects of air pollution and therefore positioned to benefit from more stringent regulatory protection.
Strengths and Limitations
The present study is limited by its focus on postmenopausal women participating in randomized clinical trials of interventions that may influence markers of diabetes risk. Although diabetes risk is greatest during young- to mid-adulthood, the study also focused on a population free of diabetes in mid- to older-adulthood, i.e., healthier than the general population. The study was also unable to examine short-term mean PM2.5 concentrations before 1999, relied on estimated ambient pollutant concentrations, and is limited by the lack of scientific knowledge on the most relevant exposure periods. Moreover, the two exposure estimation methods were limited by the availability of EPA AQS monitoring data, inability to account for differences in PM components across space, and in the case of the spatial model, failure to account for smaller-scale fluctuations in exposure captured by the spatiotemporal model inputs including, e.g., higher resolution roadway, point source emission, and population density data. Further, while the spatiotemporal model did include distance to various road types as a model input, there was no direct inclusion of noise exposure in the analyses. The study nevertheless accounted for potential selection bias, trial membership, treatment arm, and attrition when examining the effects of air pollution within its admittedly healthier, but otherwise multi-racial/ethnic, geographically diverse, and well-characterized population. In addition, the study ensured the accuracy of geocodes assigned to its participant addresses42,43,59 and validated the ambient concentrations spatiotemporally estimated at their address coordinates.45–48 Furthermore, the classical form of exposure measurement error associated with such concentrations is likely to bias estimates towards the null,60 potentially masking true associations between air pollutants and biomarkers of diabetes risk.
Conclusions
These findings suggest that low-level, short-term (2-day) mean PM10 and NOx concentrations may have negligible adverse effects on biomarkers of diabetes risk among nondiabetic postmenopausal women, potentially due to triggering of the body’s adaptive restoration of normal glucose homeostasis. Although longer-term (12-month) mean PM2.5 concentrations showed primarily null associations with biomarkers of diabetes risk, results suggestively indicated that PM2.5 exposure over the range of concentrations experienced in the United States may adversely affect biomarkers of diabetes risk at the population level, as may longer-term mean PM10 concentrations among women with IFG. Additional longitudinal studies among populations exposed to air pollution concentrations experienced in the United States are needed to further guide air quality standards, particularly those that examine effects among individuals with IFG.
ACKNOWLEDGMENTS
We thank the Women’s Health Initiative investigators, staff, and trial participants for their contributions.
Supplementary Material
Footnotes
Published online 17 July 2019
The authors declare that they have no conflicts of interest with regard to the content of this report.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.environepidem.com).
K.M.H. was supported by T32-ES007018 and R.G. by T32-HL-007055. The WHI programs are funded by the National Heart, Lung, and Blood Institute, National Institutes of Health, and US Department of Health and Human Services through contracts: HHSN268201600018C, HHSN268201600001C, HHSN268201600002C, HHSN268201600003C, and HHSN268201600004C. Air pollution data were generated with support from R01-ES017794. Other funding for this project was provided by grant R01-ES020871 from NIEHS and NIH. The content is the responsibility of the authors and does not necessarily represent the official views of the sponsoring institutions.
Process for obtaining data and code: WHI data can be accessed and used under existing policy and data use agreements available at www.whi.org.
References
- 1.Non-Communicable Disease Risk Factor Collaboration Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet 20163871513–1530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Eze IC, Hemkens LG, Bucher HC, et al. Association between ambient air pollution and diabetes mellitus in Europe and North America: systematic review and meta-analysis. Environ Health Perspect 2015123381–389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang B, Xu D, Jing Z, Liu D, Yan S, Wang Y. Effect of long-term exposure to air pollution on type 2 diabetes mellitus risk: a systemic review and meta-analysis of cohort studies. Eur J Endocrinol 2014171R173–R182 [DOI] [PubMed] [Google Scholar]
- 4.Balti EV, Echouffo-Tcheugui JB, Yako YY, Kengne AP. Air pollution and risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin Pract 2014106161–172 [DOI] [PubMed] [Google Scholar]
- 5.Hansen AB, Ravnskjær L, Loft S, et al. Long-term exposure to fine particulate matter and incidence of diabetes in the Danish Nurse Cohort. Environ Int 201691243–250 [DOI] [PubMed] [Google Scholar]
- 6.Weinmayr G, Hennig F, Fuks K, et al. ; Heinz Nixdorf Recall Investigator Group Long-term exposure to fine particulate matter and incidence of type 2 diabetes mellitus in a cohort study: effects of total and traffic-specific air pollution. Environ Health 20151453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park SK, Wang W. Ambient air pollution and type 2 diabetes: a systematic review of epidemiologic research. Curr Environ Health Rep 20141275–286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Esposito K, Petrizzo M, Maiorino MI, Bellastella G, Giugliano D. Particulate matter pollutants and risk of type 2 diabetes: a time for concern? Endocrine 20165132–37 [DOI] [PubMed] [Google Scholar]
- 9.Rao X, Montresor-Lopez J, Puett R, Rajagopalan S, Brook RD. Ambient air pollution: an emerging risk factor for diabetes mellitus. Curr Diab Rep 201515603. [DOI] [PubMed] [Google Scholar]
- 10.Thiering E, Heinrich J. Epidemiology of air pollution and diabetes. Trends Endocrinol Metab 201526384–394 [DOI] [PubMed] [Google Scholar]
- 11.Rajagopalan S, Brook RD. Air pollution and type 2 diabetes: mechanistic insights. Diabetes 2012613037–3045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haberzettl P, O’Toole TE, Bhatnagar A, Conklin DJ. Exposure to fine particulate air pollution causes vascular insulin resistance by inducing pulmonary oxidative stress. Environ Health Perspect 20161241830–1839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolf K, Popp A, Schneider A, et al. ; KORA-Study Group Association between long-term exposure to air pollution and biomarkers related to insulin resistance, subclinical inflammation, and adipokines. Diabetes 2016653314–3326 [DOI] [PubMed] [Google Scholar]
- 14.Wallwork RS, Colicino E, Zhong J, et al. Ambient fine particulate matter, outdoor temperature, and risk of metabolic syndrome. Am J Epidemiol 201718530–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thiering E, Markevych I, Brüske I, et al. Associations of residential long-term air pollution exposures and satellite-derived greenness with insulin resistance in German adolescents. Environ Health Perspect 20161241291–1298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu C, Yang C, Zhao Y, et al. Associations between long-term exposure to ambient particulate air pollution and type 2 diabetes prevalence, blood glucose and glycosylated hemoglobin levels in China. Environ Int 201692-93416–421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen Z, Salam MT, Toledo-Corral C, et al. Ambient air pollutants have adverse effects on insulin and glucose homeostasis in Mexican Americans. Diabetes Care 201639547–554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thiering E, Cyrys J, Kratzsch J, et al. Long-term exposure to traffic-related air pollution and insulin resistance in children: results from the GINIplus and LISAplus birth cohorts. Diabetologia 2013561696–1704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toledo-Corral CM, Alderete TL, Habre R, et al. Effects of air pollution exposure on glucose metabolism in Los Angeles minority children. Pediatr Obes 20161354–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eze IC, Schaffner E, Foraster M, et al. Long-term exposure to ambient air pollution and metabolic syndrome in adults. PLoS One 201510e0130337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tamayo T, Rathmann W, Krämer U, Sugiri D, Grabert M, Holl RW. Is particle pollution in outdoor air associated with metabolic control in type 2 diabetes? PLoS One 20149e91639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Honda T, Pun VC, Manjourides J, Suh H. Associations between long-term exposure to air pollution, glycosylated hemoglobin and diabetes. Int J Hyg Environ Health 20172201124–1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lucht SA, Hennig F, Matthiessen C, et al. Air pollution and glucose metabolism: an analysis in non-diabetic participants of the Heinz Nixdorf Recall Study. Environ Health Perspect 2018126047001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peng C, Bind MC, Colicino E, et al. Particulate air pollution and fasting blood glucose in nondiabetic individuals: associations and epigenetic mediation in the normative aging study, 2000–2011. Environ Health Perspect 20161241715–1721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen L, Zhou Y, Li S, et al. Air pollution and fasting blood glucose: a longitudinal study in China. Sci Total Environ 2016541750–755 [DOI] [PubMed] [Google Scholar]
- 26.Fleisch AF, Gold DR, Rifas-Shiman SL, et al. Air pollution exposure and abnormal glucose tolerance during pregnancy: the project Viva cohort. Environ Health Perspect 2014122378–383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chuang KJ, Yan YH, Cheng TJ. Effect of air pollution on blood pressure, blood lipids, and blood sugar: a population-based approach. J Occup Environ Med 201052258–262 [DOI] [PubMed] [Google Scholar]
- 28.Kim JH, Hong YC. GSTM1, GSTT1, and GSTP1 polymorphisms and associations between air pollutants and markers of insulin resistance in elderly Koreans. Environ Health Perspect 20121201378–1384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sade MY, Kloog I, Liberty IF, Katra I, Novack L, Novack V. Air pollution and serum glucose levels: a population-based study. Medicine (Baltimore) 201594e1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Anderson G, Cummings S, Freedman L, et al. Design of the Women’s Health Initiative clinical trial and observational study. Control Clin Trials 19981961–109 [DOI] [PubMed] [Google Scholar]
- 31.Schmidt F, Bergmeyer H. Methods of Enzymatic Analysis 1974Vol. 11962nd edNew York, NY: Academic Press [Google Scholar]
- 32.Peterson JI, Young DS. Evaluation of the hexokinase-glucose-6-phosphate dehydrogenase method of determination of glucose in urine. Anal Biochem 196823301–316 [DOI] [PubMed] [Google Scholar]
- 33.Warnick GR, Albers JJ. A comprehensive evaluation of the heparin-manganese precipitation procedure for estimating high density lipoprotein cholesterol. J Lipid Res 19781965–76 [PubMed] [Google Scholar]
- 34.Tietz N. Fundamentals of Clinical Chemistry 1987Vol. 5443rd edPhiladelphia, PA: Saunders [Google Scholar]
- 35.Langer RD, White E, Lewis CE, Kotchen JM, Hendrix SL, Trevisan M. The Women’s Health Initiative Observational Study: baseline characteristics of participants and reliability of baseline measures. Ann Epidemiol 200313suppl 9S107–S121 [DOI] [PubMed] [Google Scholar]
- 36.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 198528412–419 [DOI] [PubMed] [Google Scholar]
- 37.Giannini C, Santoro N, Caprio S, et al. The triglyceride-to-HDL cholesterol ratio: association with insulin resistance in obese youths of different ethnic backgrounds. Diabetes Care 2011341869–1874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord 20086299–304 [DOI] [PubMed] [Google Scholar]
- 39.Genuth S, Alberti KG, Bennett P, et al. ; Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003263160–3167 [DOI] [PubMed] [Google Scholar]
- 40.The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 200326suppl 1s5–s20 [DOI] [PubMed] [Google Scholar]
- 41.Curb JD, McTiernan A, Heckbert SR, et al. ; WHI Morbidity and Mortality Committee Outcomes ascertainment and adjudication methods in the Women’s Health Initiative. Ann Epidemiol 200313suppl 9S122–S128 [DOI] [PubMed] [Google Scholar]
- 42.Whitsel EA, Quibrera PM, Smith RL, et al. Accuracy of commercial geocoding: assessment and implications. Epidemiol Perspect Innov 200638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Whitsel EA, Rose KM, Wood JL, Henley AC, Liao D, Heiss G. Accuracy and repeatability of commercial geocoding. Am J Epidemiol 20041601023–1029 [DOI] [PubMed] [Google Scholar]
- 44.United States Environmental Protection Agency. Air Quality System (AQS). Available at: https://www.epa.gov/aqs. Accessed February 10, 2018.
- 45.Liao D, Peuquet DJ, Duan Y, et al. GIS approaches for the estimation of residential-level ambient PM concentrations. Environ Health Perspect 20061141374–1380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liao D, Peuquet DJ, Lin H-M, et al. National kriging exposure estimation: Liao et al. Respond. Environ Health Perspect 2007115A338–A339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liao D, Whitsel EA, Wellenius G, et al. Daily kriging to estimate large scale location specific PM10 – comparisons of measurement error options. Environ Health Perspect 20134269 [Google Scholar]
- 48.Yanosky JD, Paciorek CJ, Laden F, et al. Spatio-temporal modeling of particulate air pollution in the conterminous United States using geographic and meteorological predictors. Environ Health 20141363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med 200134599–106 [DOI] [PubMed] [Google Scholar]
- 50.Chen P, Chantala K; Guidelines for analyzing Add Health data Carolina Population Center, University of North Carolina at Chapel Hill. 20141–53Available at: https://www.cpc.unc.edu/projects/addhealth/documentation/guides/wt_guidelines_20161213.pdf
- 51.Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res 20112040–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stuart EA, Azur M, Frangakis C, Leaf P. Multiple imputation with large data sets: a case study of the Children’s Mental Health Initiative. Am J Epidemiol 20091691133–1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.United States Environmental Protection Agency. NAAQS Table. Available at: https://www.epa.gov/criteria-air-pollutants/naaqs-table. Accessed February 10, 2018.
- 54.United States Environmental Protection Agency. Table of Historical Particulate Matter (PM) National Ambient Air Quality Standards (NAAQS). Available at: https://www.epa.gov/pm-pollution/table-historical-particulate-matter-pm-national-ambient-air-quality-standards-naaqs. Accessed February 10, 2018.
- 55.Wilcox G. Insulin and insulin resistance. Clin Biochem Rev 20052619–39 [PMC free article] [PubMed] [Google Scholar]
- 56.Wang M, Kaufman RJ. Protein misfolding in the endoplasmic reticulum as a conduit to human disease. Nature 2016529326–335 [DOI] [PubMed] [Google Scholar]
- 57.Wang Q, Zhang H, Zhao B, Fei H. IL-1beta caused pancreatic beta-cells apoptosis is mediated in part by endoplasmic reticulum stress via the induction of endoplasmic reticulum Ca2+ release through the c-Jun N-terminal kinase pathway. Mol Cell Biochem 2009324183–190 [DOI] [PubMed] [Google Scholar]
- 58.Ozcan L, Tabas I. Role of endoplasmic reticulum stress in metabolic disease and other disorders. Annu Rev Med 201263317–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Whitsel E, Quibrera P, Smith R, et al. Accuracy of commercial geocoding in a Women’s Health Initiative ancillary study: the environmental epidemiology of arrhythmogenesis in WHI. Circulation 2005111E229:P216 [Google Scholar]
- 60.Holliday KM, Avery CL, Poole C, et al. Estimating personal exposures from ambient air pollution measures: using meta-analysis to assess measurement error. Epidemiology 20142535–43 [DOI] [PMC free article] [PubMed] [Google Scholar]


