Abstract
Male partner involvement in prenatal care has been shown to improve outcomes for the entire family in low- and middle income countries. In Brazil, partners of pregnant women are encouraged to attend prenatal care for HIV testing. From November 2016 to July 2017, male partners of women delivering at Hospital Conceiçao were interviewed using computer-assisted telephone interviews regarding individual, relationship and system-wide facilitators and barriers to attending prenatal care. Of 403 men interviewed, 202 attended prenatal care and 201 did not. Individual factors that predicted prenatal care attendance included over-estimating the risk of mother to child transmission (AOR 2.13, 95% CI: 1.35–3.4), and endorsing that HIV-infected individuals can live satisfying lives (AOR 7.24, 95% CI: 1.9–47.5). Partnership factors associated with attendance included invitation by partner (AOR 5.6, 95% CI: 2.4–15.6). Systemic factors negatively associated with prenatal care attendance included a history of not being able to afford medical care (AOR 0.3, 95% CI: 0.15–0.6) and identifying work as a barrier to prenatal care attendance (AOR 0.19 95% CI: 0.11–0.31). Partners should be actively invited to prenatal care during flexible flexible hours. Once involved, almost all would accept HIV and sexually transmitted infection (STI) testing to protect partners and unborn infants during this vulnerable period.
Keywords: HIV/AIDS, partner testing, sexually transmitted infections, male partner involvement
Background
Impressive gains have been made in Latin America in increasing the number of people who know their HIV status and are on appropriate antiretroviral drugs. Brazil has been a key leader in HIV prevention in Latin America, but mother to child transmission MTCT) of HIV continues to be an area where preventative efforts can be optimized as vertical transmission rates hover around 11.4%.1 Porto Alegre is the capital of Rio Grande do Sul, a state in southern Brazil, and has the highest incidence rates of HIV in pregnant women in Brazil.2–4 It is estimated that 3–5% of women receiving prenatal care (PNC) and 5–10% of women without PNC in Rio Grande do Sul are HIV infected.5–9 At Hospital Conceiçao between 2006 and 2013, approximately 30% of HIV-infected women were newly diagnosed with HIV at the time of delivery. Acute maternal HIV seroconversion during pregnancy resulted in higher than expected rates of HIV MTCT with a 19% rate of vertical transmission rather than <2% in HIV-infected mothers previously diagnosed and placed on antiretroviral therapy.7,10,11 To address the problem of acute HIV acquisition during pregnancy, HIV testing of male partners during pregnancy was implemented at all the clinics associated with Hospital Conceiçao in 2011. Despite this intervention and the support of the Ministry of Health recommending male partner involvement in PNC,12 uptake of partner involvement continues to be low.
Engaging men in PNC and encouraging partner testing can allow health providers to offer interventions to decrease likelihood of HIV transmission during pregnancy and therefore reduce MTCT.13,14 Diagnosing and treating men for HIV infection and sexually transmitted infections (STIs) will also improve the health of men,15 and publications have shown that partner involvement has also been associated with improved health outcomes for the entire family, including the infant.16,17 Despite this known correlation, prior studies have shown low rates of HIV testing of male partners worldwide.15,18–20 Studies performed in Tanzania, South Africa, Ethiopia, and China have identified multiple barriers to male partner involvement including poor communication within couples,19–21 less stable relationship status,19,20,22 traditional gender roles,23,24 unfriendliness of clinics toward male partners19,21,23,24 scheduling conflicts due to work,21,23 and long wait times.19 However, there are few published studies examining barriers and facilitators in Latin America.
To further explore men’s perspectives on barriers and facilitators to HIV testing, we previously performed in-depth interviews with men visiting their newborn in the post-partum unit at this site.26 The current study further evaluates the themes that surfaced during the qualitative interviews in order to identify appropriate predictors associated with uptake of partner involvement.
Methods
Study setting and population
Hospital Conceiçao is a tertiary referral center in Porto Alegre, Brazil, the largest state in Rio Grande do Sul. It is a 1200-bed, publicly funded hospital serving as a major referral center for HIV-infected patients and mainly providing care from the lower socio-economic strata, where many cases of HIV and syphilis are reported.2,4 Approximately 7000 women per year receive PNC at its main campus or satellite clinics. As of 2011, all affiliated PNC clinics have been encouraged to offer HIV testing to male partners during women’s PNC visits. The Brazilian Ministry of Health further encouraged partner testing during PNC in a document published in 2016.25
Inclusion and exclusion criteria
All men 18 years of age and older whose HIV-negative female partner delivered a live-born infant at Hospital Conceiçao were included in the study pool and called at random within a month of their newborn’s delivery. Men who were unable to provide appropriate informed consent and men who were younger than 18 years of age were excluded.
Study design and recruitment
This was a case–control study design with cases comprising partners who attended PNC, and controls being those who did not attend PNC, matched in a 1:1 ratio. Women who had delivered a live-born infant in the last month were entered into a spreadsheet, randomized, called and informed of the study protocol. If women answered and agreed to participate, their male partners were then called and offered participation via a scripted interview. After verbal consent was obtained, men participated in a computer-assisted telephone interview (CATI), a modified ‘face to face’ format over the phone. Answers were directly entered into the survey instrument (Survey Monkey, San Mateo, California, US.). Interviews lasted on average 20 minutes. From 8 November 2016 until 1 July 2017, 202 men participating in PNC and 201 men who had refused participation in partner testing during PNC were recruited.
Interview questions focused on themes identified by men who participated in previous qualitative interviews, especially focusing on the individual, relationship and systems barriers that comprised our final theoretical model.26 Questions were piloted to 10 individuals and revised to appropriately reflect participants’ and interviewer’s feedback. Participants were asked questions regarding general demographics (age, race, education level), financial stability (income, employment, requests for outside assistance to meet needs), health-seeking behaviors, drug and alcohol use and abuse, relationship intimacy (modified from Relationship Closeness Inventory)27 including specific questions probing levels of jealousy (modified from Multidimensional Jealousy Scale),28 and perceived involvement as a father in their current and past children’s lives. There were also asked questions about their perception of HIV-related stigma,29 as well as their knowledge of HIV transmission during pregnancy. If they attended PNC, they were asked about whether their experience was positive with the medical providers and clinical staff. Finally, all participants were asked about barriers and facilitators to attendance in their partner’s PNC. Study protocol was approved by both UCLA and Hospital Conceiçao Institutional Review Boards.
Sample size and justification
With the sample size of 200 per group, we had an 80% power to detect differences in proportions for categorical variables (example: employment status) between the groups of 15% (assuming 50% in those who participated and 35% in those that did not) assuming a two-sided 0.05 level of significance and a Chi square test. For continuous variables (example: age, income), the sample size provided 80% power to detect effect sizes of 0.28 or above, assuming a two-sided 0.05 level of significance and a two-sample t-test. Further, this sample size was sufficient to include 10 variables in the multiple regression models using accepted standards suggesting 10–15 subjects per group per variable in the model.
Data collection and analysis
Descriptive statistics were performed for all data collected. Two-sample t-test and Pearson Chi squared statistics were used to analyze difference in continuous and categorical outcomes between those who participated in PNC and those who did not. To determine predictors associated with PNC attendance and successful receipt of HIV testing, univariate and multiple logistic regression was utilized. For adjusted models predicting PNC attendance, the first models adjusted for covariates grouped by individual, partnership or systematic factors (models 1–3), and the last model adjusted for all predictors with a p value <0.05. Covariates for the final model were selected if they appeared to be a confounder for at least one of the predictors. For covariates that were highly correlated (for instance, invited to PNC by partner or by anyone), only one covariate was selected in the final model. Analyses were conducted using the statistical package R (R version 3.0.1, The R Foundation for Statistical Computing, www.r-project.org, Vienna, Austria.).
Results
Four hundred and three men were interviewed during the study period. As seen in Figure 1, 366 (91%) of men were invited to PNC by either pregnant women or staff. Despite recommendations by Hospital Conceiçao health systems and the Brazilian Ministry of Health, 37 (9%) self-reported that they did not receive an invitation to attend. Of the 202 partners who attended PNC, 77 (38%) received HIV testing versus 4 (2%) of men who did not come to PNC. In general, most men felt welcomed and satisfied with their PNC experience.
Figure 1.
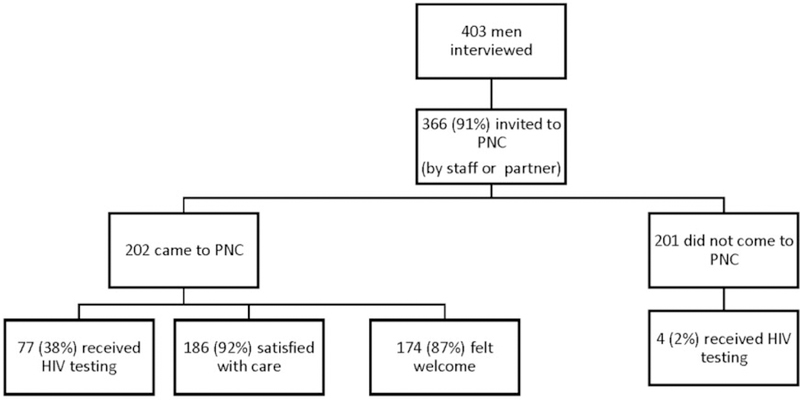
Flowchart of men who were invited to prenatal care, attended prenatal care and successfully received HIV testing. PNC: prenatal care.
Table 1 displays some of the demographic and behavioral characteristics of men interviewed. Of the men who participated, 235 (58.3%) self-identified as white, 64 (15.9%) as black, and 102 (25.3%) as mulatto/mixed. In regards to education, only 18 (4.5%) had completed high school. Despite the economic recession in Brazil, 371 (92%) stated they were employed; however, 71 (17.6%) stated they borrowed money from family in the last six months. There were no significant differences in race, education, or income between men who did and those who did not come to PNC. An investigation of differences in health utilization between the two groups showed that both groups rated their satisfaction with both their providers and Sistema Unico de Saude (SUS–Brazilian Health System) highly (4.2 out of 5 for individual’s specific obstetrical provider, 4 out of 5 for SUS). However, as seen in Table 1, men who did not come to PNC were more likely to state they had not sought medical care previously due to inability to afford care (p < 0.01).
Table 1.
Demographics and relationship characteristics of men who did and did not attend prenatal care.
| Total (% or SD) (N = 403) | Did not attend PNC (N = 201) | Attended PNC (N = 202) | p | |
|---|---|---|---|---|
| Mean age in years | 30.5 (SD 7.5) | 29.6 (SD 7.2) | 31.4 (SD 7.7) | 0.01 |
| Race | ||||
| White | 235 (58.3%) | 114 (56.7%) | 121 (59.9%) | 0.92 |
| Black | 64 (15.9%) | 34 (16.9%) | 30 (14.9%) | |
| Mulatto | 102 (25.3%) | 50 (24.9%) | 52 (25.7%) | |
| Financial stability | ||||
| Employed (yes) | 371 (92.1%) | 185 (92%) | 186 (92.1%) | 0.99 |
| Had to ask family for money in last six months (yes) | 71 (17.6%) | 35 (17.4%) | 36 (17.8%) | 0.91 |
| Not seeking MD because cannot afford (yes) | 70 (17.4%) | 47 (23.4%) | 23 (11.4%) | <0.01 |
| Alcohol use in last 12 months (yes) | 331 (82.1%) | 166 (82.6%) | 165 (81.7%) | 0.24 |
| Memory loss while drinking in last 12 months (yes) | 98 (24.3%) | 59 (29.4%) | 39 (19.3%) | 0.02 |
| Illicit drug use ever (yes) | 156 (38.7%) | 93 (46.3%) | 63 (31.2%) | <0.01 |
| Illicit drug use past month (yes) | 42 (10.4%) | 27 (13.4%) | 15 (7.4%) | 0.05 |
| Family request to cut down drug use (yes) | 13 (3.2%) | 11 (5.5%) | 2 (1%) | 0.01 |
| Jealousy | ||||
| I question my partner about telephone calls/textsa | 2.9 (SD 1.3) | 3.05 (SD 1.3) | 2.8 (SD 1.3) | 0.02 |
| Total Jealousy Score (max score 29) | 13.7 (SD 4.2) | 14.2 (SD 4.1) | 13.2 (SD 4.3) | 0.03 |
| Relationship Closeness Score (max score 16) | 14.6 (SD 2) | 14.5 (SD 2.1) | 14.6 (SD 1.9) | 0.42 |
| Pregnancy planned (yes) | 128 (31.8%) | 55 (27.4%) | 73 (36.1%) | 0.06 |
| Total Pregnancy Worry Score (max 15) | 10.3 (SD 2.8) | 10.4 (SD 2.8) | 10.2 (SD 2.9) | 0.58 |
| Stigma | ||||
| I would be ashamed if I was infected with HIV (agree) | 116 (28.8%) | 55 (27.4%) | 61 (30.2%) | 0.55 |
| I would allow my child to play with HIV-infected children (agree) | 360 (89.3%) | 179 (89.1%) | 181 (89.6%) | 0.74 |
| People with HIV can live long satisfying lives (agree) | 375 (93%) | 181 (90%) | 194 (96%) | 0.01 |
| Total HIV knowledge score (max score 6) | 4.31 (0.75) | 4.36 (0.78) | 4.26 (0.71) | 0.20 |
| Previously tested for HIV (yes) | 289 (71.7%) | 137 (68.2%) | 152 (75.2%) | 0.11 |
| Previously tested for other STIs (yes) | 286 (71%) | 135 (67.2%) | 151 (74.8%) | 0.09 |
| Invited to PNC by partner? (yes) | 365 (90.6%) | 169 (84.1%) | 196 (97%) | <0.01 |
| Accept HIV testing if offered (yes) | 378 (93.8%) | 182 (90.5%) | 196 (97%) | 0.01 |
| Accept STI testing if offered (yes) | 381 (94.5%) | 184 (91.5%) | 197 (97.5%) | 0.03 |
| Accept vaccinations if offered (yes) | 383 (95%) | 186 (92.5%) | 197 (97.5%) | 0.05 |
PNC: prenatal care, STI sexually transmitted infections. MD: medical doctor
Scale with 1 being never, 5 being all the time.
Investigating partnerships, 339 (84%) had been in a relationship with their partner longer than a year, and 340 (84.6%) stated that compared to other people’s relationships, they felt they were much closer with their current partner (data not shown). Many men admitted to a moderate amount of jealous behavior with an average jealousy score of 13.7 (maximum jealousy score 29); 250 (62%) of men stated that in the past week, they had felt jealous. Consistent with our qualitative interviews, significantly higher jealousy scores were seen in men who did not attend PNC, a potential reflection of distrust. Pregnancy was unplanned in roughly 275 (68.2%) of cases, with a lower frequency of planned pregnancies in men who did not attend PNC (n = 55, 27.4%) versus those who did attend (n = 73, 36.1%, p = 0.06). Nevertheless, 399 (99%) of men stated that as compared to other fathers they knew, they were more involved in their newborn infant’s life and nearly all were very excited about a new baby. As compared to men who did not attend PNC, men who attended PNC were more likely to accept HIV testing, STI testing, and immunizations if offered (Table 1).
We used different models to identify predictors associated with PNC attendance as seen in Table 2. Model 1 examined individual factors associated with PNC attendance, and found that overestimating the likelihood of MTCT doubled odds for PNC attendance (AOR 2.13, 95% CI: 1.35–3.4) as well as endorsing that HIV-infected individuals can have satisfying lives (AOR 7.24, 95% CI: 1.9–47.5). In Model 2, partnership factors associated with PNC attendance were evaluated and demonstrated that questioning partner about their telephone calls (aka jealousy) was associated with not attending PNC (AOR 0.82, 95% CI: 0.7–0.97), whereas being invited to PNC by partner was strongly associated with attendance (AOR 5.6, 95% CI: 2.4–15.6). Model 3 evaluated system factors associated with PNC attendance and showed that a history of avoiding medical care based on cost (AOR 0.3, 95% CI: 0.15–0.6) and identifying missing work as a barrier to PNC attendance (AOR 0.19, 95% CI: 0.11–0.31) were both negatively associated with uptake of PNC. Model 4 included all the indicators in one model and showed similar trends to models 1 through 3, but in this model, interest in making the partner happy was also significantly associated with PNC attendance (AOR 5.35, 95% CI: 1.3–27.9). As expected, the confidence intervals widened as we included more variables into each model, but the overall trends remained consistent.
Table 2.
Univariate and multivariate regression models evaluating predictors of male involvement of prenatal care (N = 403).
| Individual factors | n (%) | Odds ratio | 95% CI | Model 1 AOR | 95% CI | Model 4 AOR | 95% CI |
|---|---|---|---|---|---|---|---|
| Age | 1.03 | 1.01–1.06 | 1.01 | 0.98−1.05 | 1.01 | 0.98−1.05 | |
| Overestimating likelihood of HIV MTCT | 212 (52.74) | 1.83 | 1.20–2.7 | 2.13 | 1.35−3.4 | 2.17 | 1.24−3.8 |
| History of memory loss due to alcohol use | 98 (24.3) | 0.58 | 0.36–0.91 | 0.76 | 0.52−1.09 | 1.02 | 0.64−1.6 |
| Drug use | 156 (38.7) | 0.53 | 0.35–0.79 | 0.65 | 0.41−1.04 | 0.59 | 0.34−1.04 |
| Endorse that people with HIV can live long satisfying lives | 375 (93.52) | 2.91 | 1.25–7.6 | 7.24 | 1.9–47.5 | 6.61 | 1.4−52.6 |
| Barrier to PNC: Thinking prenatal care is for women | 74 (18.36) | 0.56 | 0.36–0.85 | 0.63 | 0.37–1.04 | 0.73 | 0.38−1.35 |
| Partnership factors | Odds ratio | 95% CI | Model 2 AOR | 95% CI | |||
| Having a planned pregnancy | 128 (31.8) | 1.50 | 0.99−2.3 | 1.3 | 0.84–2 | 1.02 | 0.55−1.87 |
| Questioning partner about telephone calls | 2.9 (SD 1.3) | 0.83 | 0.71−0.97 | 0.82 | 0.7–0.97 | 0.78 | 0.61−0.98 |
| Being invited to PNC by partner | 365 (90.6) | 6.19 | 2.7−16.7 | 5.6 | 2.4–15.6 | 31.42 | 7.45−199.2 |
| Identified making partner happy as a facilitator to PNC attendance | 382 (94.8) | 4.57 | 1.70−16.1 | 2.51 | 0.80–9.30 | 5.35 | 1.3−27.9 |
| Systemic factors | Odds ratio | 95% CI | Model 3 AOR | 95% CI | |||
| Endorsing avoidance of medical care due to cost | 70 (17.4) | 0.42 | 0.24−0.72 | 0.3 | 0.15–0.6 | 0.17 | 0.06−0.39 |
| Previously being tested for STIs | 286 (71.0) | 0.69 | 0.45−1.1 | 0.85 | 0.53−1.36 | 1.11 | 0.61−2.03 |
| Identifying missing work as a barrier to PNC attendance | 310 (76.9) | 0.21 | 0.13−0.33 | 0.19 | 0.11−0.31 | 0.07 | 0.03−0.15 |
Model 1: Adjusted for Individual factors associated with PNC attendance; Model 2: Adjusted for Partnership factors associated with PNC attendance; Model 3: Adjusted for Systemic factors associated with PNC attendance; Model 4: Adjusted for all factors in the table.
MTCT: mother to child transmission, PNC: prenatal care, STI: sexually transmitted infections.
Table 3 displays factors associated with successful completion of HIV testing during PNC. The most notable predictor of successful HIV testing in those who attended PNC was having been previously tested for HIV (AOR 5.12, 95% CI: 1.5–23.8).
Table 3.
Factors associated with successful testing for HIV if attended prenatal care (N = 202).
| Crude |
Adjusted |
||||||
|---|---|---|---|---|---|---|---|
| n (%) | OR | 95% CI | p | OR | 95% CI | p | |
| Race | |||||||
| White | 121 (59.9%) | ref | ref | ||||
| Non-white (black, mixed) | 81 (40.1%) | 0.98 | 0.5−1.8 | 0.95 | 1.40 | 0.65−3 | 0.39 |
| Previously tested for HIV | |||||||
| Yes | 152 (75.2%) | 14.28 | 4.9−60.5 | 0.00 | 5.12 | 1.5−23.8 | 0.02 |
| No | 50 (24.8%) | ref | ref | ||||
| Self-assessed risk for HIV | |||||||
| Impossible | 142 (70.3%) | ref | ref | ||||
| Improbable | 58 (28.7%) | 0.03 | 0.01−0.12 | 0.00 | 0.05 | 0.01−0.18 | 0.00 |
| Probable | 2 (1.0%) | 0.96 | 0.04−24.6 | 0.98 | 0.52 | 0.02−14.5 | 0.66 |
| Mean (sd) | OR | 95% CI | p | OR | 95% CI | p | |
| Age (years) | 31.4 (7.8) | 0.98 | 0.94−1 | 0.27 | 0.97 | 0.92−1 | 0.25 |
| Health concern for baby | 3.11 (1.05) | 0.92 | 0.7−1.2 | 0.56 | 1.00 | 0.7−1.4 | 0.99 |
| Satisfaction with medical provider | 4.24 (0.91) | 0.93 | 0.68−1.3 | 0.63 | 0.93 | 0.62−1.4 | 0.71 |
Figure 2 shows responses to questions about barriers and facilitators to PNC attendance. Of note, less than 5% of men reported distance, not feeling welcomed to PNC, fear of doctors, or fear of needles as important barriers to PNC attendance. Men who attended PNC were less likely to report missing work, thinking PNC is only for women, and thinking men’s attendance as important barriers as compared to men who did not attend PNC (p < 0.05). There was more heterogeneity of results when evaluating facilitators to attending PNC. Overall, 94.6% men stated that being able to see one’s baby on an ultrasound was ‘very important’. Men who attended PNC identified ‘making partner happy’ as an important facilitator, whereas men who did not attend PNC stated that getting an excuse from work and financial compensation were important facilitators at PNC attendance (p < 0.05).
Figure 2.
Barriers (top) and Facilitators (bottom) identified as very important (vertical stripes), somewhat important (dots) and not important (solid black) to male involvement in prenatal care.
*Significant differences in responses between those who did and did not attend prenatal care.
PNC: prenatal care; STI: sexually transmitted disease.
Discussion
Our study results indicate prominent individual, partnership, and systemic factors that affect successful uptake of PNC and HIV testing. As with our qualitative investigation26 as well as in other published reports,30,31 men stated they would be willing to receive HIV testing once participating in a PNC visit. Additionally, men in this cohort stated they would agree to receive STI testing, treatment, and immunizations during their PNC visit. Prior to our study, the Ministry of Health in Brazil created and distributed guidelines regarding the importance of partner involvement in PNC.25 Given that all providers are encouraged to invite and offer HIV rapid testing to partners of pregnant women, it is disappointing that less than 20% of men interviewed actually received HIV testing. Our results highlight important gaps in the male partner HIV testing cascade.
Our study underscores the importance of formally inviting men to PNC and excusing them from work to facilitate their attendance at PNC. The most commonly cited barrier continues to be ‘having to miss work’, and those who did not attend were more likely to cite ‘getting excused from work’ as an important facilitator. This is a common theme in other publications and possible solutions posited include weekend hours, early morning hours, fast-tracking men, and ‘father days’.32 Other options that have been successfully tried include home testing in Kenya and in Malawi.33,34
In all our analyses, men who had a history of not seeking medical care due to cost had lower odds of PNC attendance, likely because they were concerned about medical costs associated with PNC attendance. Considering that paternal PNC attendance is free of cost at SUS hospitals in Brazil, this belief potentially reflects transportation costs or costs incurred by the visit, the cost of medications, and the loss of daily wage because of missed work. Furthermore, men who denied that HIV-infected individuals could live satisfying lives were less likely to attend PNC for testing, which signals ongoing stigma associated with a diagnosis of HIV. When counseling partners, advancements in treatment options and prognosis for HIV-infected individuals should be emphasized, especially for serodiscordant couples, as fear of transmitting HIV to their partner was a main theme in our previous qualitative work.26
All interviewed men uniformly displayed great enthusiasm for fatherhood and the health of their infant, thus factors surrounding a man’s role as a father did not affect their decision to attend PNC as previously hypothesized. However, consistent with qualitative work in Brazil, we did see moderate levels of jealousy with evidence that jealous behavior (a marker of potential distrust) is negatively associated with PNC attendance. These results indicate that the most actionable factor associated with PNC attendance is to counsel pregnant women to provide a clear invitation for men to accompany them to antenatal care, as men who felt invited by their partner were 31 times more likely to attend PNC versus those who were not. Using a written invitation has been trialed in other countries with promising trends in South Africa,30 and Uganda,35 but in Tanzania, a randomized controlled trial did not reveal a difference between a written invitation and an oral invitation from the partner.31 Issuing both could be considered.
A study in South Africa found that over 90% of male partners identified HIV testing, syphilis testing, blood pressure screening, and fatherhood information as incentives to attend PNC.36 In contrast, in our Brazilian cohort, only 50% of men in our cohort identified these as very important facilitators, whereas more than 90% of men identified making their partner happy, helping their partner, and seeing their baby on an ultrasound as very important facilitators to PNC attendance. In future interventions to increase male partner involvement in PNC, invitations can be crafted to emphasize helping and/or pleasing pregnant partner as a part of the messaging.
Our study’s weakness is that we were not able to verify if men who stated they came to PNC actually did come and did or did not get HIV testing performed, as we did not collect any personal identifying information. Furthermore, since our interviews were by phone, we could not offer HIV testing to these men. Furthermore, our study is focused on women delivering in a hospital setting, which includes most women (>95%) in Porto Alegre but excludes those delivering via home-births. However, to our knowledge, our study is unique in providing a complete evaluation of individual, relationships, and systemic facilitators and barriers to male partner involvement in PNC in a large sample of men in Latin America. Factors investigated were derived from face-to-face qualitative interviews and personalized to this at-risk population. We used CATI to perform surveys to keep responses anonymous in order to better probe for socially unacceptable opinions. Although multiple studies have been performed in African countries evaluating predictors of male partner involvement in PNC, this study is one of the few studies evaluating these factors in South American men. There are some similarities in our results, including work as a barrier; however, men at our site appear to view PNC attendance as a way to please their partner and are less likely to see PNC as an opportunity to improve their own health or not attend because they perceive PNC as a ‘woman’s domain’.
Conclusion
In conclusion, officially inviting men to PNC and providing non-work hours for PNC attendance appear to be the most actionable indicators closely associated with successful male involvement in PNC. In future interventions, we will offer men testing for HIV as well as other STIs. In particular, congenital syphilis incidence rates continue to rise in Brazil and can be partially addressed by male partner testing and treatment. Male partner involvement in PNC is widely encouraged by the Brazilian Ministry of Health and can be the cornerstone of improving the health of the entire family. Our results can help inform the execution of this initiative in Brazil and Latin America.
Acknowledgements
We would like to acknowledge all the fathers who agreed to participate in these interviews for donating their time.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research in this article was supported by a grant from the NIH-NIAID 5K23AI118584-04.
Footnotes
Ethics approval and consent to participate
This study was approved by Institutional Review Boards of both UCLA (IRB#16–001762) and Hospital Conceiçao (CAAE: 46880615.1.0000.5530).
Consent for publication
All individuals involved in the study were consented verbally per our protocol prior to enrollment in this study. Interviewer read an information sheet/verbal consent to each participant in Portuguese. Once the participant consented, interviewer signed the consent form and gave a copy to participant. This procedure received IRB approval from both UCLA and Hospital Conceiçao, as a written consent with the participant’s name would be the only identifying information linking him to our study.
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.UNAIDS. UNAIDS Data 2018, www.unaids.org/en/resources/documents/2018/unaids-data-2018 (2018, accessed 25 February 2018).
- 2.Serafim AS, Moretti GP, Serafim GS, et al. Incidence of congenital syphilis in the South Region of Brazil. Rev Soc Bras Med Trop 2014; 47: 170–178. [DOI] [PubMed] [Google Scholar]
- 3.Secretaria de Vigilância em Saúde – departmento de DST AeHVBe. Boletim Epidemiológico de Sífilis 2015: p. 6.
- 4.Domingues RM, Szwarcwald CL, Souza PR Jr, et al. Prenatal testing and prevalence of HIV infection during pregnancy: data from the Birth in Brazil study, a national hospital-based study. BMC Infect Dis 2015; 15: 100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nielsen K, Santos VV, Bastos FI, et al. A pilot study using rapid HIV serologic testing during the peripartum period in Brazil Baltimore, MD: American Pediatric Society/Society for Pediatric Research (APS/SPR), 2001. [Google Scholar]
- 6.Saúde MD Secretaria de Vigilância em Saúde - Ministerio da Saúde. Boletim Epidemiológico HIV/ AIDS 2018 p 34 http://www.aids.gov.br/pt-br/pub/2018/boletim-epidemiologico-hivaids-2018 (2018, accessed April 2019).
- 7.Rocha T, Varella I, Raney J, et al. High rates of HIV seroconversion during pregnancy in Porto Alegre, Brazil. In: 9th world congress for the Society for the World Society of Pediatric Infectious Diseases (WSPID) Conference, Rio De Janeiro, Brazil 18–21 November 2015. [Google Scholar]
- 8.Veloso VG, Bastos FI, Portela MC, et al. HIV rapid testing as a key strategy for prevention of mother-to-child transmission in Brazil. Rev Saude Publica 2010; 44: 803–811. 2010/09/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Acosta LMW. Monitorando as metas do Comite da TV do HIC e SC de Porto Alegre. Secretaria Municipal de Saude de Porto Alegre—SMS, 2018.
- 10.Adachi K, Xu J, Yeganeh N, et al. Combined evaluation of sexually transmitted infections in HIV-infected pregnant women and infant HIV transmission. PLoS One 2018; 13: e0189851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nielsen-Saines K, Melo M, Varella I, Fonseca R, et al. Primary HIV-1 infection during pregnancy: high rate of HIV-1 MTCT in a cohort of patients in southern Brazil. Retrovirology 2008; (Suppl 1): O1. [Google Scholar]
- 12.Saúde M Guia do Pré-Natal do parceiro Para profissionais de saúde Rio De Janeiro, Brazil: Ministério da Saúde, 2016. [Google Scholar]
- 13.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med 2011; 365: 493–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral therapy for the prevention of HIV-1 transmission. N Engl J Med 2016; 375: 830–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Farquhar C, Kiarie J, Richardson B, et al. Antenatal couple counseling increases uptake of interventions to prevent HIV-1 transmission. J Acquir Immune Defic Syndr 2004; 37: 1620–1626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aluisio A, Richardson BA, Bosire R, et al. Male antenatal attendance and HIV testing are associated with decreased infant HIV infection and increased HIV-free survival. J Acquir Immune Defic Syndr 2011; 56: 76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ambia J and Mandala J. A systematic review of interventions to improve prevention of mother-to-child HIV transmission service delivery and promote retention. J Int AIDS Soc 2016; 19: 20309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moses SE, Tosswill J, Sudhanva M, et al. HIV-1 seroconversion during pregnancy resulting in vertical transmission. J Clin Virol 2008; 41: 152–153. [DOI] [PubMed] [Google Scholar]
- 19.Brittain K, Giddy J, Myer L, et al. Pregnant women’s experiences of male partner involvement in the context of prevention of mother-to-child transmission in Khayelitsha, South Africa. AIDS Care 2015; 27: 1020–1024. [DOI] [PubMed] [Google Scholar]
- 20.Ditekemena J, Matendo R, Koole O, et al. Male partner voluntary counselling and testing associated with the antenatal services in Kinshasa, Democratic Republic of Congo: a randomized controlled trial. Int J STD AIDS 2011; 22: 165–170. [DOI] [PubMed] [Google Scholar]
- 21.Reece M, Hollub A, Nangami M, et al. Assessing male spousal engagement with prevention of mother-to-child transmission (pMTCT) programs in western Kenya. AIDS Care 2010; 22: 743–750. [DOI] [PubMed] [Google Scholar]
- 22.Morfaw F, Mbuagbaw L, Thabane L, Rodrigues C, et al. Male involvement in prevention programs of mother to child transmission of HIV: a systemic review to identify barriers and facilitators. Syst Rev 2013; 2: 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Byamugisha R, Tumwine JK and Semiyaga N. Determinants of male involvement in the prevention of mother-to-child transmission of HIV programme in Eastern Uganda: a cross-sectional survey. Reprod Health 2010; 7: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nkuoh G, Meyer D, Tih P, et al. Barriers to men’s participation in antenatal and prevention of mother-to-child HIV transmission care in Cameroon, Africa. J Midwifery Womens Health 2010; 55: 363–369. [DOI] [PubMed] [Google Scholar]
- 25.Saúde M Guia do Pré-Natal do Parceiro para Profissionaisde Saúde Brasilia: DAPES, 2016. [Google Scholar]
- 26.Yeganeh N, Simon M, Mindry D, et al. Barriers and facilitators for men to attend prenatal care and obtain HIV voluntary counseling and testing in Brazil. PLoS One 2017; 12: e0175505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berscheid E, Snyder M and Omoto AM. The relationship closeness inventory: assessing the closeness of interpersonal relationships. J Personality Social Psychol 1989; 57: 792–807. [Google Scholar]
- 28.Pfeiffer S and Wong P. Multidimensional jealousy. J Soc Personal Relationships 1989; 6: 181–196. [Google Scholar]
- 29.USAID. Can we measure HIV/AIDS-related stigma and discrimination? Washington, D.C.: Development USAfl, 2006. [Google Scholar]
- 30.Mohlala BK, Boily MC and Gregson S. The forgotten half of the equation: randomized controlled trial of a male invitation to attend couple voluntary counselling and testing. AIDS 2011; 25: 1535–1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Theuring S, Jefferys LF, Nchimbi P, et al. Increasing partner attendance in antenatal care and HIV testing services: comparable outcomes using written versus verbal invitations in an urban facility-based controlled intervention trial in Mbeya, Tanzania. PLoS One 2016; 11: e0152734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ditekemena J, Koole O, Engmann C, et al. Determinants of male involvement in maternal and child health services in sub-Saharan Africa: a review. Reprod Health 2012; 9: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mark J, Kinuthia J, Roxby AC, et al. Uptake of homebased syphilis and human immunodeficiency virus testing among male partners of pregnant women in Western Kenya. Sex Transm Dis 2017; 44: 533–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Choko AT, Corbett EL, Stallard N, et al. HIV self-testing alone or with additional interventions, including financial incentives, and linkage to care or prevention among male partners of antenatal care clinic attendees in Malawi: an adaptive multi-arm, multi-stage cluster randomised trial. PLoS Med 2019; 16: e1002719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Byamugisha R, Astrom AN, Ndeezi G, et al. Male partner antenatal attendance and HIV testing in eastern Uganda: a randomized facility-based intervention trial. J Int AIDS Soc 2011; 14: 43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yende N, Van Rie A, West NS, et al. Acceptability and preferences among men and women for male involvement in antenatal care. J Pregnancy 2017; 2017: 4758017. [DOI] [PMC free article] [PubMed] [Google Scholar]



