Supplemental Digital Content is available in the text.
Key Words: fibromyalgia, health care resource, pharmacotherapy, sleep
Abstract
Objective:
This study aimed to determine whether comorbid insomnia is associated with increased use of fibromyalgia-related medications and health resources in fibromyalgia (FM) patients.
Materials and Methods:
We analyzed data retrieved from the Longitudinal Health Insurance Database 2010, which contains claims data of 1 million beneficiaries randomly selected from Taiwan’s National Health Insurance program. Patients treated for FM (n=17,920) on 2 separate visits between 2000 and 2001 were selected and subsequently divided into 2 groups: patients with and without comorbid insomnia (n=5466 and 12,454, respectively). Insomnia was identified through diagnosis on 2 separate visits after the index FM date. FM-related pharmacotherapies and ambulatory care visits were tracked from the index date to the end of 2013.
Results:
Insomnia was associated with increased likelihood of future use of antidepressants (adjusted odds ratio [OR]=3.84, P<0.001), gabapentin (adjusted OR=1.67, P<0.001), pregabalin (adjusted OR=1.79, P=0.046), muscle relaxants (adjusted OR=3.05, P<0.001), and opioids and tramadol (adjusted OR=1.59, P<0.001) among FM patients compared with FM patients without insomnia. In addition, a diagnosis of insomnia was associated with an increased frequency of visits to ambulatory care services for both FM (β=1.79; 95% confidence interval, 1.57-2.02; P<0.001) and other conditions (β=108.51; 95% confidence interval, 103.14-113.89; P<0.001).
Discussion:
This study demonstrates the substantial burden of comorbid insomnia in patients with FM.
Fibromyalgia (FM) is a complicated chronic pain syndrome that affects between 1.2% and 5.4% of the general population.1,2 The primary complaint of patients with FM is chronic widespread pain, which is often accompanied by other symptoms such as sleep disturbances, cognitive dysfunction, fatigue, and negative mood.2,3 Results of previous studies have shown that FM-related pain is associated with a substantial socioeconomic burden including greater health care costs and productivity loss from work.4 The usage rates of pain-related prescription medications5 and visits to physician6 in patients with FM were twice as many as those patients without any health care encounter for FM. Sleep symptoms are one of the most frequently subjective problems of FM patients. Most patients with FM report their sleep as poor or nonrestorative7 and feel unrefreshed upon awakening8 compared with healthy controls. Objective sleep quality as measured by polysomnography also supported that FM patients experienced shorter sleep duration, more time in light sleep, lower sleep efficiency, and longer duration of wakefulness during sleep than healthy individuals.9 Complex and multidimensional pathophysiological mechanisms underlie the effects of poor sleep on FM symptom severity (ie, myalgia, tenderness, and fatigue).10,11 Patients with FM with poor sleep quality were reported to show a higher degree of pain, poorer psychological status, more impaired body functions, and poorer quality of life than those with good sleep quality.7 A dose-dependent association between poor sleep and FM symptom severity has been found in an epidemiological study.12 Specifically, a reciprocal relationship is observed between sleep disturbance and pain.13 The hypothalamus-pituitary-adrenal-cortex axis dysregulation14 and central sensitization15 associated with FM may lead to increased pain sensitivity. Improved sleep quality can reduce pain in patients with FM revealed from results of clinical trials of pharmacotherapy.3,16,17 Despite that the linkage between pain and sleep alterations has been supported, however, scarce data are available on the extent to which disturbed sleep affects prescribed medications and health care resource utilization in the FM population.
Given that an increased use of medications and ambulatory care services might reflect increased burden of illness such as increased symptom severity and poor health status, we performed a population-based cohort study to test the following hypotheses: (1) patients with FM with comorbid insomnia are associated with an increased likelihood of being prescribed medications commonly used to treat FM than those without comorbid insomnia; and (2) patients with FM with comorbid insomnia are associated with an increased use of ambulatory care services for treating FM or other conditions during follow-up than those without comorbid insomnia.
MATERIALS AND METHODS
Data Source
We analyzed data retrieved from the Longitudinal Health Insurance Database 2010 (LHID2010) released by Taiwan’s National Health Research Institutes (NHRI). The LHID2010 includes medical claims data and registration files of 1 million enrollees randomly selected from the 2010 Registry for Beneficiaries (n=27.38 million) of the National Health Insurance (NHI) program. The NHI program, Taiwan’s single-payer universal health care system initiated in 1995 provides comprehensive coverage with low copayments and minimal restrictions on access to medical care, covering outpatient visits, inpatient care, prescription drugs, dialysis treatments, traditional Chinese medicine, and dental care. Currently, more than 99% of the Taiwanese population is covered by the NHI program. All insurance claims are scrutinized by reimbursement specialists and under strict audits through peer reviews to ensure accuracy of coding. The data set was encrypted by the NHRI to protect participant confidentiality. This study was exempted from a full review by the Institutional Review Board of Taipei Medical University, Taipei, Taiwan (protocol no. N201712080).
Patients
The International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes were used to identify the study cohort. To identify incident FM cases, patients newly diagnosed with FM on at least 2 separate occasions between 2000 and 2001 were identified using a principal diagnosis ICD-9-CM code of FM. Patients who were diagnosed with FM before 2000 were excluded (n=7697). Moreover, patients were excluded if they were aged above 100 or below 20 years (n=3362), were diagnosed with FM only once (n=11,697), were diagnosed with insomnia before the first FM diagnosis (n=2302), and if sex-related (n=4) or insurance premium-related (n=255) data were missing. The first FM diagnosis was considered the index date.
Insomnia after the index FM date was identified using a primary or secondary diagnosis of insomnia using the ICD-9-CM codes on 2 occasions between January 1, 2000, and December 31, 2012 were included in this study. Consequently, patients who were diagnosed with insomnia only once were excluded from the study (n=2141). Finally, 17,920 patients with FM were included for analyses and divided into 2 groups: patients with and without comorbid insomnia (n=5466 and 12,454, respectively).
Confounders
Potential confounders considered in the statistical analyses were age, sex, and personal income; insurance premium was used as a proxy for personal income. Comorbidities including conditions listed among the 17 diseases defining the Charlson Comorbidity Index (CCI)18 as well as depression and anxiety that were registered within 1 year before or on the index date were identified, and the CCI was calculated based on the 17 disease codes. Depression, anxiety, CCI, and hypnotics use were also considered as confounders in subsequent data analyses (the diagnostic codes were summarized in Appendix 1, Supplemental Digital Content 1, http://links.lww.com/CJP/A585).
Endpoints
FM-related medications such as antidepressants (tricyclic antidepressants [TCAs], selective serotonin reuptake inhibitors [SSRIs], and serotonin and norepinephrine reuptake inhibitors [SNRIs]), antiepileptic drugs (gabapentin and pregabalin), muscle relaxants, and opioids and tramadol were selected according to previous studies (the anatomic therapeutic chemical codes were summarized in Appendix 2, Supplemental digital Content 2, http://links.lww.com/CJP/A586).10,19 Moreover, the use of aforementioned were tracked from the index date to the end of 2013 so that individuals who had insomnia diagnosis between January 1, 2012 and December 31 could be followed for at least 1 year. The use of ambulatory care services for treating FM and other conditions was also tracked from the index date to the end of 2013.
Statistical Analyses
The odds ratio (OR) with associated confidence intervals (CIs) for insomnia status compared with noninsomnia status regarding prescriptions for antidepressants, gabapentin, pregabalin, muscle relaxants, and opioids were determined using multivariable logistic regression after adjustment for confounders and for the propensity score.20 The association between insomnia and ambulatory care visits tracked from the index date to 2013 was examined using multivariate generalized linear models after adjustment for the propensity score. The propensity score, which is the probability of group assignment conditional on, observed baseline covariates (ie, age, sex, insurance premium, depression, anxiety, the CCI, and hypnotics use) was calculated and adjusted in the statistical models to control for possible baseline imbalances between comparison groups.
We further stratified our analyses according to age group (≥50 vs.<50), sex (men vs. women), level of insurance premium (≥20,000 vs.<20,000 NTD), presence of depression (yes vs. no), presence of anxiety (yes vs. no), CCI score (≥1 vs. 0), and presence of hypnotics use (yes vs. no).
RESULTS
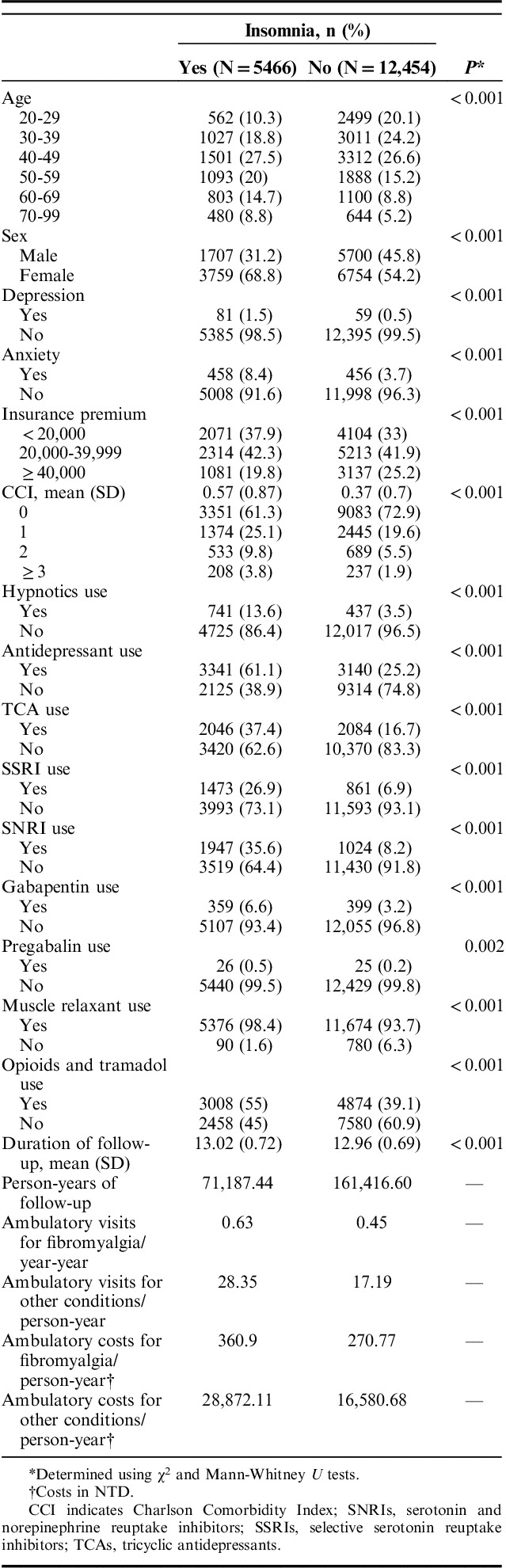
Table 1 shows the distribution of sample characteristics according to the insomnia status. The 2 groups significantly differed in all the analyzed confounders and usage rates of medications (all P<0.001). Ambulatory visits and costs per person-year for investigating or treating FM and for other conditions were both higher in patients with FM with comorbid insomnia than those without insomnia. It is noteworthy that most of the ambulatory visits were for treating conditions other than FM in both groups (Table 1). Among the visits for nonFM conditions, only a small portion was for treating insomnia in the group with comorbid insomnia. Appendix 3 (Supplemental Digital Content 3, http://links.lww.com/CJP/A587) shows the ambulatory visits and associated costs for insomnia.
TABLE 1.
Distribution of Sample Characteristics According to Insomnia in Patients With Fibromyalgia
The results of the association between insomnia status and FM-related medications are presented in Figure 1. Patients with FM with comorbid insomnia were associated with increased likelihood of being prescribed antidepressants (adjusted OR=3.84, P<0.001), gabapentin (adjusted OR=1.67, P<0.001), pregabalin (adjusted OR=1.79, P=0.043), muscle relaxants (adjusted OR=3.05, P<0.001), and opioids and tramadol (adjusted OR=1.59, P<0.001) during the follow-up period after adjustment for age, sex, depression, anxiety, hypnotics use, insurance premium, and the CCI compared with FM patients without insomnia. Specifically, patients with FM with comorbid insomnia were associated with increased likelihood of being prescribed TCAs (adjusted OR=2.37, P<0.001), SSRIs (adjusted OR=4.30, P<0.001), SNRIs (adjusted OR=5.40, P<0.001) after adjustment for confounders compared with FM patients without insomnia. We further stratified our analyses according to age group, sex, presence of depression, presence of anxiety, presence of hypnotics use, level of insurance premium, and the CCI score. The stratified analyses for the associations between insomnia and use of medications (Appendix 4, Supplemental Digital Content 4, http://links.lww.com/CJP/A588) were in general in line with the results from unstratified analyses. However, insomnia status was associated with an increased likelihood of pregabalin prescriptions for women (adjusted OR=2.34; 95% CI, 1.15-4.74; P=0.019), but not for men (P=0.980) after adjustment of confounders. It is also noted that the estimates for the association between insomnia and use of medications became less precise or even nonsignificant in the subgroups of FM patients with depression or anxiety but remain statistically significant in patients without depression or anxiety.
FIGURE 1.
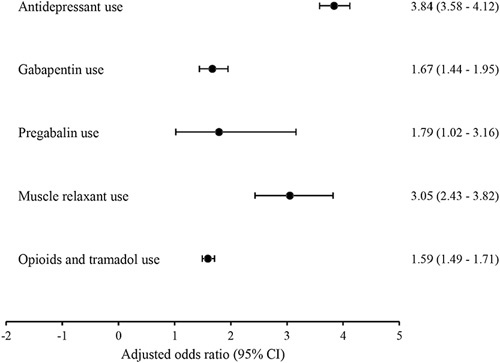
The association between insomnia status and fibromyalgia-related medications. The odds ratio and 95% confidence interval determined using multivariable logistic regression adjusting for age, sex, depression, anxiety, hypnotic use, insurance premium, and the Charlson Comorbidity Index.
After adjustment of the propensity score, patients with FM with comorbid insomnia were associated with increased likelihood of uses of antidepressants (adjusted OR=3.80, P<0.001), TCAs (adjusted OR=2.35, P<0.001), SSRIs (adjusted OR=4.20, P<0.001), SNRIs (adjusted OR=5.30, P<0.001), gabapentin (adjusted OR=1.68, P<0.001), pregabalin (adjusted OR=1.81, P=0.046), muscle relaxants (adjusted OR=3.04, P<0.001), and opioids and tramadol (adjusted OR=1.58, P<0.001), during the follow-up period.
Furthermore, a diagnosis of insomnia in patients with FM was associated with a higher number of ambulatory care visits (β=1.68; 95% CI, 1.47-1.90; P<0.001) and a higher cost of ambulatory visits (β=843.68; 95% CI, 711.51-975.85; P<0.001) for treating FM as well as a higher number of ambulatory visits (β=107.22; 95% CI, 102.02-112.42; P<0.001) and a higher cost (β=99,320.56; 95% CI, 92,771.61-105,869.52; P<0.001) for other conditions during the follow-up period after adjustment for age, sex, insurance premium, depression, anxiety, the CCI, and hypnotics use, as determined using generalized linear models. Similarly, patients with FM with comorbid insomnia were associated with a higher number of ambulatory care visits for treating FM (β=1.79; 95% CI, 1.57-2.02; P<0.001) and other conditions (β=108.51; 95% CI, 103.14-113.89; P<0.001) during the follow-up period after adjustment for the propensity score compared with FM patients without insomnia.
DISCUSSION
Scarce data are available on the burden of illness in patients with FM with comorbid insomnia. This study is the first to reveal that among a cohort of patients with FM, a diagnosis of insomnia was associated with an increased likelihood of the subsequent use of FM-related medications including antidepressants, anticonvulsants, muscle relaxants, opioids and tramadol. In particular, patients with FM with comorbid insomnia had 3 times the odds of being prescribed antidepressants compared with those without comorbid insomnia. Moreover, patients with FM with comorbid insomnia are not only associated with an increased future use and associated costs of ambulatory care services and for investigating or treating FM, but also subsequently used more ambulatory care services for treating other conditions. The significant associations between insomnia and increased uses of FM-related medications and frequency of visits to ambulatory care services in FM patients was found across different age groups, sex, levels of income, and levels of comorbidity burden.
Managing patients with FM remains challenging and often requires both pharmacological and nonpharmacological treatment. Basically a symptom-based pharmacological approach is adopted by most published guidelines. However, none of the available medications are effective against the whole spectrum of FM symptoms. Pregabalin, TCAs, SNRIs, muscle relaxants (ie, cyclobenzaprine) are the recommended choice of drugs for FM; other drugs with at least 1 positive clinical trial include some SSRIs, gabapentin, and tramadol, etc.21 It is noteworthy that the most frequent choice of drug for our FM cohort was a muscle relaxant followed by tramadol, SNRIs, and TCAs which in general conform to the pharmacotherapy guideline. Although aforementioned medications are used to reduce pain and sleep problems associated with FM, our results reveal that a diagnosis of insomnia was associated with more prescription medications and ambulatory care services even after controlling for hypnotics use. Moreover, female predominance in FM has been reported.22,23 Women are reported to use more health resources than men.24 We observed that the effects of insomnia on medical expenditures of patients with FM extend beyond the sex differences in health resource. This proof-of-concept study provided strong evidence to substantiate the impact of poor sleep on symptom burden in patients with FM. Disturbed sleep has been supported as a pathogenic stimulus of FM symptoms.11 Previous clinical trials have reported that the severity of pain of FM patients was reduced after their sleep problems were effectively improved.25,26 Thus, the effective management of sleep disturbances may be a critical option for managing patients with FM. Nonpharmacological treatments of insomnia such as cognitive-behavioral therapy have been shown to improve sleep quality in long-term painful health conditions.27 The illness burden of FM (ie, medications and health care utilization) may be decreased if insomnia can be effectively managed. Nonpharmacological sleep interventions should be integrated into the treatment regime of patients with FM to optimize the treatment outcomes of the disease.
We found in the current study that patients with FM with comorbid insomnia were more likely to be prescribed with antidepressants than those without comorbid insomnia even in the subgroup without depression. Compared with patients with FM without comorbid insomnia, those with comorbid insomnia had 4 times the odds of being prescribed either SSRI or SNRI after controlling for hypnotics use. We also found that comorbid insomnia increased the use of muscle relaxants and opioids in FM patients receiving hypnotics. Interestingly enough, in this study only 13.6% of FM patients with insomnia were being treated with a hypnotic, whereas 60% of them were being treated with an antidepressant, suggesting that physicians in Taiwan view poor sleep as a symptom of FM and prescribed medications according to the recommended pharmacotherapy for FM. Antidepressants have been widely used in treating sleep problems in patients with primary insomnia, chronic pain, depressive disorder, or other health problems.28 However, a meta-analysis study revealed inconclusive results regarding the effect of antidepressants on poor sleep in patients with FM.29 Moreover, a sizable number of patients discontinued treatment because of intolerable adverse effects of antidepressants or did not experience meaningful symptom reliefs.29 The observed increases in health resource utilization may suggest that insomnia was ineffectively treated in this population despite the fact that antidepressants were often prescribed to patients with FM with comorbid insomnia.
It is also important to note that only about 30% of patients with FM initiated a treatment with a prescription medication listed in the ACR guidelines, and many patients received less than the recommended dose revealed from a recent large-scale study.30 Discontinuation, switching, and addition of new pain medications were common in patients with FM within 1 year after first diagnosis.30 Compared with placebo treatments, licensed doses of ACR guidelines medications significantly produced greater improvements in sleep and greater number of responders (ie, ≥30% reduction in pain).31 The increased use of antidepressants in patients with comorbid insomnia in our study may reflect the insufficient exposure of medications or repeatedly changed medication profiles in this population.
Results of our study showed that the association between insomnia and use of medications was presented in the subgroups of FM patients without depression or anxiety but not in patients with depression or anxiety. Depression generally worsens somatic symptoms accompanied with FM including chronic pain or muscle tense.3 Thus, a diagnosis of insomnia may not be the key determinant of prescribing anticonvulsants, opioids and tramadol, and muscle relaxants in the subgroups of FM patients with depression. In contrast, we found that comorbid insomnia was associated with increased use of aforementioned medications in the subgroups of FM patients without depression, indicating that comorbid insomnia did have an impact on the manifestation of pain or muscle tense in patients with FM even without the presence of depression. Similarly, comorbid insomnia was associated with increased use of anticonvulsants, opioids and tramadol, and muscle relaxants in the subgroups of FM patients without anxiety. Of note, muscle tense is one of the core symptoms of anxiety. The comorbid insomnia may increase the severity of muscle tense related to both of FM and anxiety. Thus, comorbid insomnia may consequently increase the likelihood of prescription of muscle relaxants in the subgroups of FM patients with anxiety.
Numerous limitations must be considered when interpreting the present findings. First, FM and insomnia were diagnosed using claims data reported by clinics and hospitals. Physicians for many reasons could have overused the specific codes of FM and insomnia. In our study, only patients who received a primary diagnosis of FM on 2 separate medical encounters within 1 year were selected as the study cohort, which considerably reduced inaccurate patient inclusion in the study cohort. In terms of the exposure of interest, the presence of insomnia was limited to its primary or secondary diagnosis on 2 medical encounters after the index date. One may argue that sleep disturbance is universally seen in this population and the prevalence of insomnia symptoms may be underestimated. In addition, given that physicians might miss the diagnosis of insomnia if it is not a specific target of intervention, the incidence of insomnia in the FM population was probably underestimated in this study. Nonetheless, the rigorous method for identifying insomnia diagnosis is able to provide more solid evidence regard to the burden of FM in patients with sleep alterations. Second, although we only included patients with FM with newly diagnosed insomnia, we did not compare the use of prescription medications and ambulatory care services before and after the insomnia diagnosis. Therefore, causality cannot be determined. Third, there might remain residual confounding due to the fact that certain variables such as educational level, lifestyle factors, and nutritional factors (eg, vitamins D, B1, and B12), which were found to be correlated with sleep quality or widespread pain,10 were unavailable for analyses.
In addition, depression is common comorbidity among people with FM; however, only 1% of the FM patients had depressive disorders in the current study, which was lower than the rates reported by other studies.5,32 The reason why our finding is inconsistent with others’ might be that we used clinical diagnostic criteria whereas others used questionnaires such as the Hospital Anxiety and Depression Score or the Beck Depression Inventory to identify depression. The observed incidence of depression in our study was also lower than those reported by other studies in Taiwan, which the prevalence of depression ranged from 3.35% to 6.0%33–35 in FM patients and ranged from 1.05% to 2.27% in the general population.36 The reason might be that we did not include dysthymia (ICD-9-CM 300.4) (Appendix 1, Supplemental Digital Content 1, http://links.lww.com/CJP/A585) whereas those studies included dysthymia as a diagnostic code to identify depression. Also, about 41% of the patients included in the study were male. In clinical samples, there is often a stronger female preponderance.22,23 However, our finding is consistent with other studies in Taiwan, which reported that over 40% of the FM patients were male.33–35,37
Lastly, as we did not compare the pattern of health care utilization between patients with FM and the Taiwanese general population, whether the usage rates of medications and outpatient visits of the FM patients with or without insomnia were higher than the general population in Taiwan could not be determined. Nevertheless, the number of ambulatory visits in our FM cohort (>28 visits per person-year in the insomnia group and >17 visits per person-year in the noninsomnia group) was higher than that of the general population (average annual visits=14) reported by a previous study using the same database.38
Despite these limitations, our study had several strengths. The primary strength of our study was the use of claims data from a single-payer health care system, which enables conducting a large-scale, nation-wide investigation. A population-based study by using a claims database for examining the effects of insomnia on patients with FM not only considerably reduced selection bias but also enabled tracing the use of prescription medications commonly prescribed for patients with FM and of ambulatory care services over a follow-up period of at least 12 years. Furthermore, we employed covariate adjustment using the propensity score, which controlled for possible imbalances in the distribution of observed baseline covariates between patients with insomnia and patients without insomnia.
CONCLUSIONS
In conclusion, patients with FM with comorbid insomnia are more likely to receive prescription medications for FM and use more ambulatory care services than those without insomnia, demonstrating the significant burden of FM in patients with comorbid insomnia. Poor sleep may worsen symptom distress and pain intensity of the FM population, which may lead to an increase in the economic burden on the health care system.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.clinicalpain.com.
Footnotes
C.-J.H. and C.-L.H. contributed equally.
P.-S.T.: contributed to the conception of the idea, the study design, and to acquisition, analysis and interpretation of data; drafted and revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. C.-J.H and C.-L.H.: contributed to the conception of the idea, analysis and interpretation of results; drafted and revised the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy. Y.-C.F. and T.-Y.C.: were involved in the analysis and interpretation of data, drafting and revising the manuscript; gave final approval; and agreed to be accountable for all aspects of work ensuring integrity and accuracy.
Supported by grants from Taiwan Ministry of Science and Technology, Taipei, Taiwan (MOST #105-2314-B038-052-MY3 & MOST #107-2314-B038-023-MY3). The authors declare no conflict of interest.
REFERENCES
- 1.Jones GT, Atzeni F, Beasley M, et al. The prevalence of fibromyalgia in the general population: a comparison of the American College of Rheumatology 1990, 2010, and modified 2010 classification criteria. Arthritis Rheumatol. 2015;67:568–575. [DOI] [PubMed] [Google Scholar]
- 2.Walitt B, Nahin RL, Katz RS, et al. The prevalence and characteristics of fibromyalgia in the 2012 National Health Interview Survey. PLoS One. 2015;10:e0138024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clauw DJ. Fibromyalgia: a clinical review. JAMA. 2014;311:1547–1555. [DOI] [PubMed] [Google Scholar]
- 4.Lacasse A, Bourgault P, Choiniere M. Fibromyalgia-related costs and loss of productivity: a substantial societal burden. BMC Musculoskelet Disord. 2016;17:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berger A, Dukes E, Martin S, et al. Characteristics and healthcare costs of patients with fibromyalgia syndrome. Int J Clin Pract. 2007;61:1498–1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lachaine J, Beauchemin C, Landry PA. Clinical and economic characteristics of patients with fibromyalgia syndrome. Clin J Pain. 2010;26:284–290. [DOI] [PubMed] [Google Scholar]
- 7.Liedberg GM, Bjork M, Borsbo B. Self-reported nonrestorative sleep in fibromyalgia—relationship to impairments of body functions, personal function factors, and quality of life. J Pain Res. 2015;8:499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Munguia-Izquierdo D, Legaz-Arrese A. Determinants of sleep quality in middle-aged women with fibromyalgia syndrome. J Sleep Res. 2012;21:73–79. [DOI] [PubMed] [Google Scholar]
- 9.Wu YL, Chang LY, Lee HC, et al. Sleep disturbances in fibromyalgia: a meta-analysis of case-control studies. J Psychosom Res. 2017;96:89–97. [DOI] [PubMed] [Google Scholar]
- 10.Chinn S, Caldwell W, Gritsenko K. Fibromyalgia pathogenesis and treatment options update. Curr Pain Headache Rep. 2016;20:25. [DOI] [PubMed] [Google Scholar]
- 11.Choy EH. The role of sleep in pain and fibromyalgia. Nat Rev Rheumatol. 2015;11:513–520. [DOI] [PubMed] [Google Scholar]
- 12.Mork PJ, Nilsen TI. Sleep problems and risk of fibromyalgia: longitudinal data on an adult female population in Norway. Arthritis Rheum. 2012;64:281–284. [DOI] [PubMed] [Google Scholar]
- 13.Aili K, Nyman T, Svartengren M, et al. Sleep as a predictive factor for the onset and resolution of multi-site pain: a 5-year prospective study. Eur J Pain. 2015;19:341–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McLean SA, Williams DA, Harris RE, et al. Momentary relationship between cortisol secretion and symptoms in patients with fibromyalgia. Arthritis Rheum. 2005;52:3660–3669. [DOI] [PubMed] [Google Scholar]
- 15.Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(suppl):S2–S15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spaeth M, Rizzi M, Sarzi-Puttini P. Fibromyalgia and sleep. Best Pract Res Clin Rheumatol. 2011;25:227–239. [DOI] [PubMed] [Google Scholar]
- 17.Straube S, Derry S, Moore RA, et al. Pregabalin in fibromyalgia: meta-analysis of efficacy and safety from company clinical trial reports. Rheumatology (Oxford). 2010;49:706–715. [DOI] [PubMed] [Google Scholar]
- 18.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. [DOI] [PubMed] [Google Scholar]
- 19.Traynor LM, Thiessen CN, Traynor AP. Pharmacotherapy of fibromyalgia. Am J Health Syst Pharm. 2011;68:1307–1319. [DOI] [PubMed] [Google Scholar]
- 20.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46:399–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Calandre EP, Rico-Villademoros F, Slim M. An update on pharmacotherapy for the treatment of fibromyalgia. Expert Opin Pharmacother. 2015;16:1347–1368. [DOI] [PubMed] [Google Scholar]
- 22.Toda K. The prevalence of fibromyalgia in Japanese workers. Scand J Rheumatol. 2007;36:140–144. [DOI] [PubMed] [Google Scholar]
- 23.Vincent A, Lahr BD, Wolfe F, et al. Prevalence of fibromyalgia: a population-based study in Olmsted County, Minnesota, utilizing the Rochester Epidemiology Project. Arthritis Care Res (Hoboken). 2013;65:786–792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bertakis KD, Azari R, Helms LJ, et al. Gender differences in the utilization of health care services. J Fam Pract. 2000;49:147–152. [PubMed] [Google Scholar]
- 25.Davies KA, Macfarlane GJ, Nicholl BI, et al. Restorative sleep predicts the resolution of chronic widespread pain: results from the EPIFUND study. Rheumatology (Oxford). 2008;47:1809–1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lami MJ, Martinez MP, Sanchez AI, et al. Gender differences in patients with fibromyalgia undergoing cognitive-behavioral therapy for insomnia: preliminary data. Pain Pract. 2016;16:E23–E34. [DOI] [PubMed] [Google Scholar]
- 27.Tang NK, Lereya ST, Boulton H, et al. Nonpharmacological treatments of insomnia for long-term painful conditions: a systematic review and meta-analysis of patient-reported outcomes in randomized controlled trials. Sleep. 2015;38:1751–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shultz E, Malone DA., Jr A practical approach to prescribing antidepressants. Cleve Clin J Med. 2013;80:625–631. [DOI] [PubMed] [Google Scholar]
- 29.Hauser W, Wolfe F, Tolle T, et al. The role of antidepressants in the management of fibromyalgia syndrome: a systematic review and meta-analysis. CNS Drugs. 2012;26:297–307. [DOI] [PubMed] [Google Scholar]
- 30.Liu Y, Qian C, Yang M. Treatment patterns associated with ACR-recommended medications in the management of fibromyalgia in the United States. J Manag Care Spec Pharm. 2016;22:263–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Choy E, Marshall D, Gabriel ZL, et al. A systematic review and mixed treatment comparison of the efficacy of pharmacological treatments for fibromyalgia. Semin Arthritis Rheum. 2011;41:335–345. e336. [DOI] [PubMed] [Google Scholar]
- 32.Loge-Hagen JS, Saele A, Juhl C, et al. Prevalence of depressive disorder among patients with fibromyalgia: systematic review and meta-analysis. J Affect Disorders. 2019;245:1098–1105. [DOI] [PubMed] [Google Scholar]
- 33.Wang KA, Wang JC, Lin CL, et al. Association between fibromyalgia syndrome and peptic ulcer disease development. PLoS One. 2017;12:e0175370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Su CH, Chen JH, Lan JL, et al. Increased risk of coronary heart disease in patients with primary fibromyalgia and those with concomitant comorbidity—a Taiwanese population-based cohort study. PLoS One. 2015;10:e0137137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chang MH, Hsu JW, Huang KL, et al. Bidirectional association between depression and fibromyalgia syndrome: a nationwide longitudinal study. J Pain. 2015;16:895–902. [DOI] [PubMed] [Google Scholar]
- 36.Tu HP, Hsieh HM, Liu TL, et al. Prevalence of depressive disorder in persons with type 2 diabetes: a national population-based cohort study 2000-2010. Psychosomatics. 2017;58:151–163. [DOI] [PubMed] [Google Scholar]
- 37.Lan CC, Tseng CH, Chen JH, et al. Increased risk of a suicide event in patients with primary fibromyalgia and in fibromyalgia patients with concomitant comorbidities: a nationwide population-based cohort study. Medicine (Baltimore). 2016;95:e5187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chiang PH, Chang YC, Lin JD, et al. Healthcare utilization and expenditure analysis between individuals with intellectual disabilities and the general population in Taiwan: a population-based nationwide child and adolescent study. Res Dev Disabil. 2013;34:2485–2492. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.clinicalpain.com.


