Supplemental Digital Content is available in the text.
Keywords: Adolescent; Anxiety disorders; Conduct disorder; Depressive disorder, Major; Mental health; Noise; Substance-related disorders; United States Environmental Protection Agency
Abstract
Background:
Environmental noise has been linked to negative health outcomes, like poor sleep, poor mental health, and cardiovascular disease, and likely accounts for more than 1 million disability-adjusted life years annually in Western Europe. Adolescence may be a particularly sensitive period for noise exposure due to an increased need for sleep, failure to meet sleep guidelines, and increased risk for first onset of some mental health disorders. However, the potential health effects of living in high-noise environments have not been studied in US adolescents, rarely in European adolescents, and mental health outcomes studied have not corresponded to diagnoses from the Diagnostic and Statistical Manual of Mental Disorders (DSM).
Methods:
Using a US-based nationally representative survey of urban adolescents (N = 4,508), we estimated associations of day-night average sound levels exceeding the US Environmental Protection Agency’s 55 decibel limit with sleep outcomes and lifetime mental health DSM diagnoses. We implemented doubly robust targeted minimum loss-based estimation coupled with propensity score matching to account for numerous potential adolescent, household, and environmental confounders.
Results:
Living in a high- versus low-noise Census block group was associated with later bedtimes on weeknights (0.48 hours, 95% confidence interval [CI] = –0.15, 1.12) and weekend nights (0.65 hours, 95% CI = 0.37, 0.93), but not with total hours slept. Associations between living in a high- versus low-noise Census block group and mental disorders were mixed, with wide CIs, and not robust to sensitivity analyses.
Conclusions:
We find evidence for an association between residence in a high-noise area and later bedtimes among urban adolescents but no consistent evidence of such an association with mental health disorders.
What this study adds
This is the first US study to examine a relation between environmental noise and adolescent health. We identified communities where day-night average sound levels exceeded the US Environmental Protection Agency’s limit of 55 decibels (which we call high-noise). We then estimated associations between noise and sleep and mental health diagnoses from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) among a nationally representative sample of US urban adolescents. We used machine learning and doubly robust estimation to control for numerous potentially confounding variables at the community, family, and individual levels. We found that residence in a high-noise communities was associated with later bedtimes but not with mental health.
Introduction
Environmental noise—unwanted or extraneous sound from sources like traffic and airports—has been linked to negative health outcomes including sleep disturbances, poor mental health, and cardiovascular disease.1 Among adults, a pooled analysis of polysomnographic and self-reported awakenings studies found consistent evidence that nighttime noise caused cortical awakenings and sleep disturbances.2 Nighttime noise may also affect sleep duration, efficiency, and insomnia.2,3 These sleep disturbances may harm mental health,4,5 but depression and anxiety may also arise independently from sustained central autonomic arousal due to chronic noise exposure.6,7 Considering these negative health effects together, exposure to high environmental noise levels is estimated to result in the loss of at least 1 million disability-adjusted life years annually in Western Europe.8
Adolescents may be particularly sensitive to negative health effects from environmental noise due to their increased need for sleep9 coupled with failure to meet sleep guidelines,10 and risk of mental disorder onset during this developmental period.11 However, despite adolescence being a potentially developmentally vulnerable period, there is little research on the health effects of noise exposure in this subgroup.12,13 In terms of sleep outcomes, three studies among children and early adolescents reported associations between noise and reduced sleep quality14 and greater sleep problems.15,16 In terms of mental health outcomes, studies among children and adolescents generally found no association between noise and depression and anxiety scales,13,17 but generally did find associations between noise and inattention and hyperactivity.15,16,18–20 However, none of these studies examined mental health outcomes that corresponded with diagnostic criteria. Sympathetic nervous system activation, noise annoyance, social cohesion, and physical activity have been proposed as mediators and/or moderators of the possible relation between noise exposure and mental health.21,22
If a relation exists between environmental noise and adolescent sleep and mental health, there are reasons to believe it would be strongest in urban areas. First, the prevalence and incidence of mental disorders such as schizophrenia23 and depression and anxiety24,25 tend to be greater in urban areas. Short sleep duration is also more common among adults living in more urban locations.26 Exposure to environmental noise varies spatially in type and magnitude and is greater in urban areas.27 Finally, previous research demonstrated that the strength of association between adolescent depression and anxiety and another contextual variable—neighborhood deprivation—varied by level of urbanicity, with the strongest relation in urban areas.28
Our objectives were two-fold. First, we identified US communities that exceed the US Environmental Protection Agency’s (EPA) day-night average sound level (Ldn) of <55 decibels (dB)29 using a high-resolution nationwide noise model. These recommended levels are likely exceeded in many communities,30 but no recent estimates of noise exceedances in the US exist. Second, we tested the policy-relevant hypothesis that living in communities where environmental noise exceeds the US EPA threshold is associated with worse sleep and higher prevalence of mental health disorders corresponding to the DSM-IV in a nationally representative sample of US urban adolescents.
Methods
We examined this research question in an urban subsample of the National Comorbidity Survey Replication Adolescent Supplement (NCS-A), a nationally representative survey of adolescents living in the contiguous US conducted 2001–2004 (N = 4,508 urban adolescents). Details of the sampling design and procedures have been published previously.31–33 Briefly, household and school samples of 13–18 year-olds participated in face-to-face interviews, with an overall response rate of 75.6%. Parents provided written informed consent (except for emancipated minors) and adolescents provided assent. Study procedures were approved by the human subjects committees of Harvard Medical School and the University of Michigan. This analysis, utilizing de-identified data, was determined nonhuman subjects research by the University of California, Berkeley, and University of California, Davis.
Outcomes
We examined several sleep and mental health outcomes. Sleep patterns included the following: (1) typical hours slept per weeknight; (2) per weekend night; (3) typical bedtime on a weeknight; and (4) weekend night, based on adolescent response to open-ended questions. Mental disorders included the following: (1) lifetime anxiety or depressive disorder (major depressive disorder, dysthymia, or any anxiety disorder) based on adolescent interview in accordance with prior recommendations34; (2) lifetime behavioral disorder (conduct disorder or oppositional defiant disorder) based on adolescent or caregiver interviews combined at the symptom level, among those with caregiver interviews; (3) lifetime attention-deficit/hyperactivity disorder (ADHD) with impairment based on caregiver interviews; and (4) lifetime substance use disorder based on adolescent interview. Disorders were categorized using adolescent and/or caregiver endorsement of symptoms, as specified above, as has been done previously,35 using a modified version of the World Health Organization Composite International Diagnostic Interview (CIDI) Version 3.0, administered by trained interviewers. The resulting disorder categorizations correspond to DSM-IV diagnoses according to a blinded clinical reappraisal substudy.36 Caregiver reports of adolescent behavioral symptoms were ascertained by a self-administered questionnaire completed by caregivers of 2,645 (59%) urban adolescents (as well as 2,242 suburban and 1,596 rural adolescents).
Sample
We examined associations among adolescents living in urban centers for our primary analysis (N = 4,508), and include adolescents living in urban fringe areas (N = 3,304) and nonurban areas (N = 2,311) in the Supplement. Urban areas were defined as central counties within standard metropolitan statistical areas (MSAs) and having populations ≥ 100,000. Urban fringe and nonurban areas, which we consider in the Supplement, were defined as noncentral counties within MSAs or those < 100,000 and as small-large towns outside of MSAs or rural areas.
Environmental and sociodemographic measures
Our exposure of interest was ambient outdoor noise over the US EPA threshold of 55 dB. Ambient outdoor noise was defined by Ldn, the sound level averaged over the year and A-weighted to mimic the sensitivity of the human auditory system.1 Ldn is calculated within a 24-hour period with 10 dB added to levels between the hours of 10 pm and 7 am. The additional 10 dB upweights nighttime noise, reflecting increased sensitivity to noise at night. The metrics were projected to a 270 m × 270 m grid across the contiguous US from geospatial sound models, models derived from over 1.5 million hours of acoustical data (sampled 2000–2014) and dozens of geospatial features accounting for both natural and anthropogenic sources.27,37 Ldn was averaged within each US Census block group. For the primary analyses, noise was dichotomized as high (≥55 dB) versus low (<55 dB). The sensitivity analyses described below used alternative exposure definitions.
We included numerous potentially confounding variables in our models, including aspects of the environment: air pollution (modeled block group level nitrogen dioxide [NO2] in 2000),38 satellite-based greenness (block group level normalized difference vegetative index [NDVI] in 2000),39 average high temperature (county-level in 2000),40 population density, and neighborhood socioeconomic status (block group level in 2000, measured as a 6-item index from the US Census that includes median household income, median housing value, occupation types, education levels, and sources of wealth)41; adolescent characteristics: sex, age, race/ethnicity (black, white, Hispanic/Latino, other), English as primary language, citizenship status, immigrant generation, region of the country (Northeast, Midwest, South, West), religion (protestant, catholic, other religion, no religion), whether the adolescent lived her/his whole life with his/her mother and/or father, student status; and family characteristics: family income (log-transformed), maternal age at birth of the adolescent, maternal education, parental marital status, and family conflict tactics (presence of psychological aggression, moderate forms of physical assault, and severe forms of physical assault separately for adolescent-parent dyad and parent-parent dyad, as have been included in previous NCS-A analyses relating contextual exposures to mental health).28,42
Statistical approach
We first imputed missing values using multiple imputation by chained equations, which assumes the data are missing at random conditional on the variables in the imputation model,43 producing 30 imputed datasets. Out of the 36 variables used for the analysis, 19 variables were missing between 0.03% and 43% of observations. Parent marital status and maternal level of education had highest levels of missingness at 43% and 30%, respectively. The remaining variables had less than 4% missing. An analysis that ignores the missingness assumes that the data are missing completely at random—that is, missingness is independent of both observed and unobserved variables.44 This is a strong and typically unrealistic assumption.44 Addressing missingness through multiple imputation instead assumes that the data are missing at random—that is, missingness can depend on observed variables that are included in the missingness model.44 We included all variables used in our analysis in all missingness models, which is necessary for congeniality,45 as well as many additional variables at the individual, family, and Census block group levels for a total of 122 variables and 40 additional second order interactions that improved model fit. We assessed the quality of the imputation by comparing densities of the imputed and observed values, as recommended.43 We completed analysis on each dataset and then pooled the results using combining rules of Rubin46.
We then used full matching on the propensity score47 for living in a high-noise area, including exact matching on sex and matching within narrow calipers on family income and neighborhood socioeconomic status, given the importance of these factors in adolescent mental health.35,48 Web Figure 1; http://links.lww.com/EE/A50 shows the resulting propensity score and covariate balance across the two exposure groups. The resulting frequency weights from the matching procedure were multiplied by the NCS-A sampling weights for analysis. We used a doubly robust substitution estimator, targeted minimum loss-based estimation,49 which incorporates the previously estimated propensity scores and includes for the aforementioned covariates in the outcome model, to estimate the adjusted association of exposure to high noise levels with each outcome. Confidence intervals (CIs) were further adjusted to account for multiple testing using a false discovery rate of 5%.50 Additional details of our approach are available in the Web Appendix 1; http://links.lww.com/EE/A50.
R Version 3.3.1 was used and code to replicate these analyses is provided: https://github.com/kararudolph/code-for-papers/blob/master/NCSAnoisepaper.R.
Sensitivity analyses
We assessed the sensitivity of our results to extrapolations beyond the support of the data by limiting our analysis to the subsample of urban adolescents (N = 1,880) with counterparts in the opposite exposure group with similar propensities to live in high-noise areas (Web Appendix 2, Web Figure 2; http://links.lww.com/EE/A50).51–53 However, because such restriction results in no longer being able to interpret the results as applying to the nationally representative sample of urban US adolescents, we use the unrestricted sample for the primary analysis.
We also repeated our analyses using three alternative exposure definitions. First, we repeated our analyses using a continuous measure of noise. Second, we dichotomized noise at the US Federal Aviation Administrations Ldn threshold of 65 dB.54 Third, we used a data-driven approach to dichotomize community noise as high or low by using hierarchical clustering of several measures of block group level noise (Web Appendix 3; http://links.lww.com/EE/A50).55
Results
Geospatial sound model projections in the period 2000–2014 revealed elevated noise levels in many US communities, particularly in those with dense populations and transportation networks (Figure 1). The 4,508 urban-dwelling adolescent NCS-A participants lived in 2,751 block groups with an average Ldn of 57.2 dB (SD = 4.6). Nearly 91% of participants lived in communities where Ldn exceeded 55 dB (i.e., high-noise). Non-Hispanic Black and Hispanic/Latino participants more often lived in high-noise communities (Table 1). In contrast, 75% of urban fringe adolescents and 18% of nonurban adolescents lived in communities where Ldn exceeded 55 dB (Web Table 1; http://links.lww.com/EE/A50). Overall, we estimated that nearly 71% of US adolescents (n = 29,698,782) lived in block groups where Ldn exceeded the US EPA limit of 55 dB. Percentages varied by state, from 0% in Montana and Wyoming to over 95% in Illinois (Figure 2).
Figure 1.
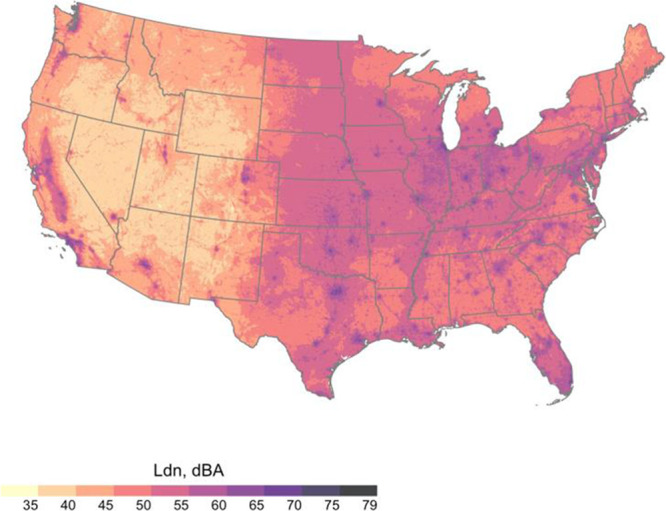
Ldn in dB across the continental United States, 2000–2014. Values estimated from a geospatial sound model.
Table 1.
Demographic and community characteristics by noise level: NCS-A, United States, 2001–2004
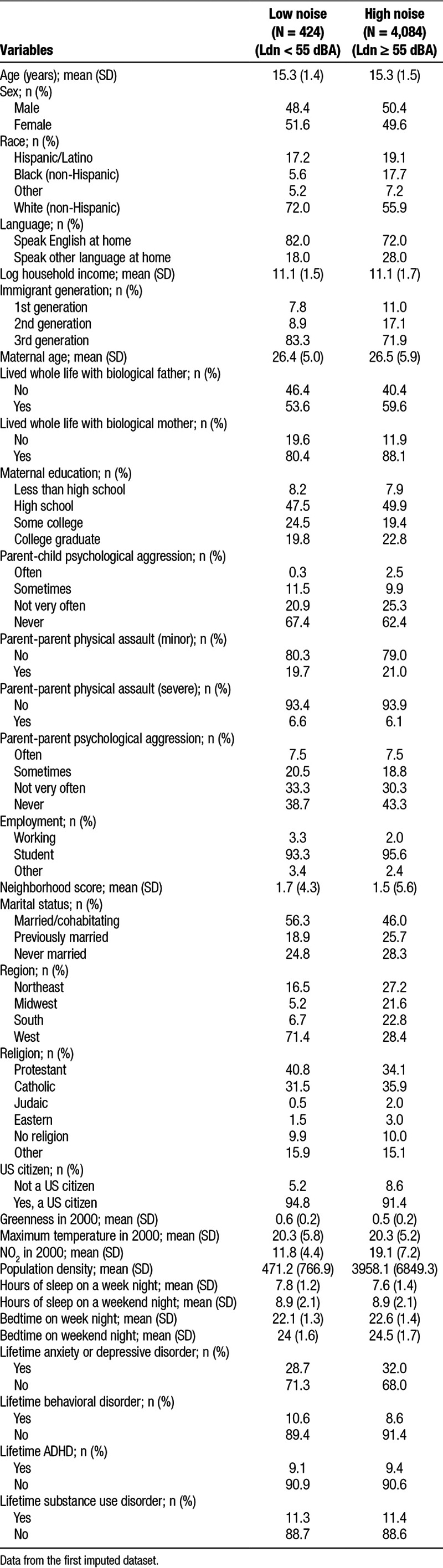
Figure 2.
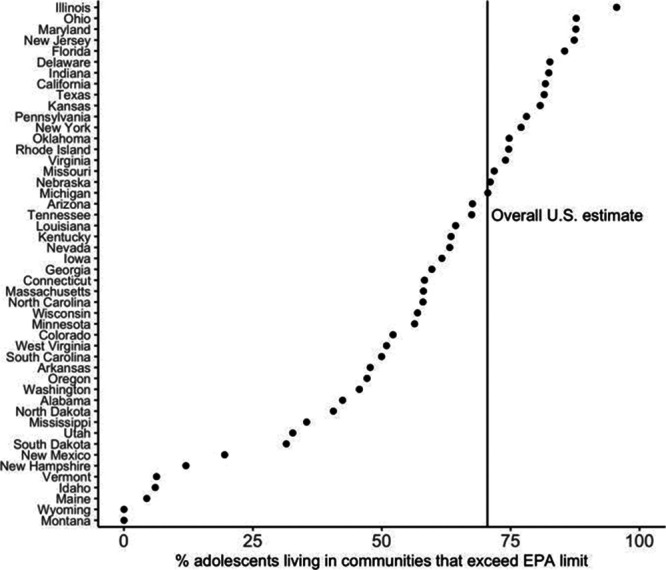
State-specific estimates of the percentage of adolescents living in block groups where average day-night noise exceeded 55 dB, 2000–2014. Data on adolescents were downloaded from the 2010 US Census.
Table 2 shows associations between living in a high- versus low-noise Census block group and sleep and mental health outcomes among urban adolescents, conditioning on numerous adolescent, household, and environmental covariates. Several of these covariates were potentially strong confounders: we observed moderate correlation between our exposure measure and NDVI (ρ = –0.50) and fairly strong correlation with NO2 (ρ = 0.75). High noise exposure above the US EPA threshold was associated with bedtimes that were about 30–40 minutes later on both weeknights and weekend nights (0.48 hours, 95% CI = –0.26, 1.23 and 0.65 hours, 95% CI = 0.32, 0.98, respectively), but not with total hours slept (–0.07, 95% CI = –0.83, 0.69 and 0.06, 95% CI = –0.55, 0.68, respectively, Table 2). These results were robust to sensitivity analyses in which we restricted to the area of support (Web Table 3; http://links.lww.com/EE/A50), treated noise as a continuous exposure (Web Table 4; http://links.lww.com/EE/A50), and used a data-drive noise dichotomization (Web Table 6; http://links.lww.com/EE/A50).
Table 2.
Associations between residence in an high- versus low-noise community and sleep and mental health among adolescents in the NCS-A, United States, 2001–2004 (N = 4,508)
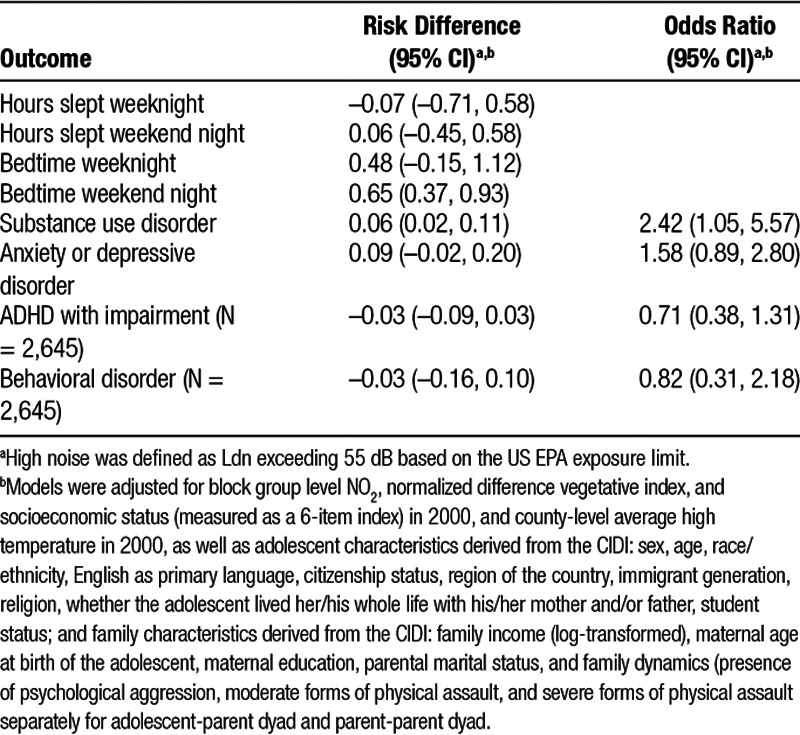
In contrast to the robust results for later bedtimes, associations between high noise exposure and mental disorders among urban adolescents were mixed with wide CIs and less robust to sensitivity analyses. Living in a high- versus low-noise Census block group was associated with increased odds of anxiety or depressive disorder (Odds Ratio (OR): 1.58, 95% CI = 0.89, 2.80) and substance use disorder (2.42, 95% CI = 1.05, 5.57) but with reduced odds of behavioral disorders (0.82, 95% CI = 0.31, 2.18) and severe ADHD (0.71, 95% CI = 0.38, 1.31) (Table 2). Point estimates for anxiety or depressive disorder and substance use disorder were in similar directions using a higher threshold for noise dichotomization (Web Table 5; http://links.lww.com/EE/A50), using a data-driven noise dichotomization (Web Table 6; http://links.lww.com/EE/A50), and were similar for substance use disorder restricting to the area of support (Web Table 3; http://links.lww.com/EE/A50). However, CIs were generally too wide to be informative in these sensitivity analyses.
We repeated our primary analysis among adolescents in urban fringe and nonurban areas. Web Table 1; http://links.lww.com/EE/A50 gives descriptive statistics for adolescents living in these areas. Web Table 2; http://links.lww.com/EE/A50 shows that among these subgroups, all associations were null with wide CIs.
Discussion
In a cross-sectional analysis of a nationally representative sample of US urban adolescents, we found that living in a community where average day-night noise exceeded the US EPA safety guideline of 55 dB was associated with approximately 30–40 minute later bedtimes. Associations with DSM-IV mental disorders were mixed, generally with wide CIs, and not robust across sensitivity analyses. Although we found that air pollution was highly correlated with noise, it could not explain the observed association between high noise levels and later bedtimes, consistent with prior studies.56–58 Our results were also not explained by area-level socioeconomic status, residential greenness,59 or compositional factors at the adolescent and household level. Recent European evidence suggests that noise harms human mental health and sleep,1 but, to our knowledge, this study represents the first analysis of noise and adolescent sleep and mental health in the United States. Further, by applying the nationwide noise model based on data collected 2000–2014 to 2010 US Census data, we estimated that over 70% of US adolescents lived in communities where day-night noise levels exceeded the US EPA exposure limit.
Early60,61 and more recent62,63 US studies have focused on transportation noise at schools, generally finding lower reading scores, cognition, and attention among students in louder learning environments. Most recent child and adolescent studies took place in Europe and reported positive associations between noise and cognitive impairment.13,58,64 Further studies among children and early adolescents have supported a relation between noise and hyperactivity/inattention symptoms15,16,18–20,65 and ADHD symptomology measured by DSM-IV criteria (although not diagnoses).57 The few studies that assessed the association between elevated noise and child/adolescent sleep found increased parent-reported sleep problems3,14–16 but not reduced sleep quality measured by wrist actigraphy.14 Almost no studies have included mid-late adolescents,22,66 as we did herein.
Noise activates the sympathetic nervous system, even during sleep,1,2 which can fragment sleep and reduce total sleep time. We found that adolescents living in high-noise areas had later bedtimes on both weeknights and weekend nights. We saw no difference in sleep duration, implying that high-noise exposure may shift sleep phase. Later bedtimes among adolescents have been associated with adverse mental health outcomes, substance use, and poorer academic performance.67–71 Similarly, negative health outcomes have been reported in association with greater differences in bedtime between weeknights and weekend nights.71–74 Health problems can result from sleep deprivation and circadian misalignment from later bedtimes.75
Although we found some evidence for a relation between high noise in urban areas and increased odds of substance use disorder and anxiety or depressive disorders, these results were not robust across sensitivity analyses. Prior studies have made similar conclusions, with a recent review describing evidence of the relation between noise and mental health in children as “heterogeneous and limited.”76 Several studies have reported associations between noise pollution and hyperactivity and inattention in children, including in a longitudinal context.77 However, we found no evidence for a relation between high-noise and odds of behavioral disorder and severe ADHD—even the directionality of point estimates differed across sensitivity analyses.
Contrasting our primary analytic results (Table 2) with the sensitivity analysis restricting to the area of support (Web Table 3 and Web Figure 2; http://links.lww.com/EE/A50) is instructive for interpreting these findings. Restricting to the area of support reduced the sample size by about 60% (from 4,508 urban adolescents to 1,880), indicating that residing in high-noise areas may be subject to significant structural confounding.78 For most urban adolescents, their levels of exposure to air pollution, greenspace, neighborhood disadvantage, etc., nearly perfectly predict whether or not they are exposed to noise levels greater than 55dB. Thus, by restricting to the area of support, we not only greatly reduced sample size and power, but we also effectively changed the estimated effect from the average treatment effect among urban adolescents to an effect that is less interpretable in that it applies to a subset of urban adolescents who have counterparts with similar propensity scores in the opposite exposure group. Point estimates differed between these two analyses, with those for ADHD and anxiety or depressive disorder demonstrating the largest differences, suggesting that that the relation between noise exposure and these disorders may be modified by important factors that differed between the representative sample and the subsample.
Contrasting our primary analytic results with the sensitivity analysis restricting to the area of support also demonstrated the extent of the challenge of estimating health effects of noise given the degree of structural confounding. We took several approaches to address confounding, including adjusting for numerous individual level, family level, and environmental covariates by full matching on the propensity score coupled with a doubly robust substitution estimator, as has been recommended previously.79 However, unobserved confounding likely remains.
The unexpected point estimates indicating reduced odds of ADHD and behavioral disorders in areas with high noise levels may reflect bias due to unobserved confounding, including measurement error. Prior work has found that the sensitivity and specificity of CIDI ADHD diagnoses may vary by characteristics such as race/ethnicity.80 ADHD and other behavioral disorder diagnoses stemming from caregiver or teacher reports also inherently include a degree of subjectivity and reliance on comparing the child/adolescent to his/her peers.81,82
Prior research suggests that noise sensitivity—internal states that increase the likelihood of noise annoyance83—may modify the relation between noise and health. In adults, noise sensitivity has predicted onset of depressive and psychological symptoms.84 In adolescents, higher morning saliva cortisol levels were correlated with high noise annoyance and living in high-noise areas.85 We lacked a measure of noise sensitivity or annoyance, and so could not assess its effect. Children, however, seem to report less annoyance than adults under the same noise conditions.86,87 Relatedly, psychological noise appraisal may also modify the relation between noise and health.88 Individuals may perceive noisy neighborhoods as lower quality. This in turn may constrain psychological restoration,89 limit physical activity,90,91 and reduce social contact.92
Strengths and limitations
To our knowledge, only one prior study evaluated associations between noise and health nationwide in the United States93 and was among adults. Ours is the first to examine health effects among adolescents in the United States and one of the few to examine sleep and mental health outcomes among adolescents. We employed a well-documented, nationally representative sample of adolescents with information on both sleep patterns and DSM-IV mental health diagnoses. Many prior studies focused solely on aircraft17,20,21,58,66,94 or traffic-related noise.3,14–16,18,22 We implemented a nationwide sound model that incorporated diverse geospatial data to comprehensively account for the total burden of noise from anthropogenic sources.37 Another contribution was our analytic strategy. We employed propensity score matching coupled with a doubly robust estimator to improve control for potential confounding variables and a flexible modeling strategy. We categorized communities as high- and low-noise based on the policy- and health-relevant US EPA exposure limit.29 This has the advantages of being policy-relevant, making the stable unit treatment value assumption (SUTVA) more plausible,95 and facilitated our robust analytic strategy. However, it asks a research question about that particular US EPA threshold instead of estimating a more general relation between exposure to noise and adolescent sleep and mental health. Examination of other reasonable thresholds and a continuous relation with level of noise was the goal of several sensitivity analyses (Web Tables 3–6; http://links.lww.com/EE/A50). Comparing the results from the main analysis to these sensitivity analyses provides some evidence that there may be a general relation between increasing noise levels and later bedtimes but not for the other sleep outcomes or for mental health outcomes.
This study also had limitations. One central issue was mismeasurement/misclassification of the exposure. Measurement error was due to (at least) (1) model uncertainty; (2) aggregation uncertainty; and (3) misalignment of data years. In terms of model uncertainty, noise was predicted at 270 m resolutions from a model, the model-based prediction error is an area for future work. Aggregation uncertainty results from (1) having noise predictions in at 270 m resolution instead of a personal measurement of noise exposure (thereby ignoring locations beyond the residential block group where adolescents may have spent time or any noise abatement strategies employed in the home) and (2) from further aggregating the 270 m noise prediction to the block group level, resulting in standard errors of the sample mean. We have standard error estimates from the latter portion of aggregation error, from which we estimate 3% misclassification of the binary noise exposure using multiple overimputation.96 In addition, the noise model was built using data collected 2000–2014 to health data collected 2001–2004; the misalignment of years used also introduces some error, the form and extent of which are unknown.
In addition to measurement error, the type, quality, and annoyance of noise exposure were unmeasured (e.g., specific sources of noise like road or air traffic) but likely important factors in characterizing and identifying specific noise exposures that are important for adolescent sleep and mental health. The predictions from the noise model ignore such characteristics, potentially violating SUTVA.95 Although dichotomizing noise exposure at the US EPA limit makes SUTVA more plausible, the binary measure can nonetheless be meaningfully different for different subgroups in the NCS-A (e.g., due to different sources of noise). We stratified on level of urbanicity to minimize this issue, although we used crude urbanicity categorizations.
The study was cross-sectional, preventing us from establishing a temporal relation between exposure and outcome. It was also observational, likely resulting in residual confounding, as discussed above. Sleep patterns were measured by adolescent report; future studies may wish to use objective measures such as actigraphy to measure sleep patterns. Caregiver reports of adolescent behavioral symptoms were not available for all adolescents, which may have impacted our findings. Finally, studies have shown that the relation between noise and health may differ by sex,3 socioeconomic status,4,97 or baseline health status,98 but we lacked the sample size to assess relation by subgroup. Future studies should prioritize longitudinal designs, improved exposure assessment, and objective sleep measures, as well as assessment of whether certain subgroups of adolescents are more susceptible to the potential adverse effects of environmental noise.
Conclusions
Nationwide, nearly 30 million adolescents lived in communities where Ldn exceeded the US EPA exposure limit in 2010. In a nationally representative sample of urban adolescents, we found that exceeding this limit was associated with later bedtimes. Interventions aimed at reducing exposure to environmental noise among adolescents may positively impact their sleep. Public health strategies to reduce noise exposure include direct regulation of sources of noise as well alterations to the built environment.30
Conflicts of interest statement
The authors declare that they have no conflicts of interest with regard to the content of this report.
Supplementary Material
Footnotes
Published online 25 June 2019
Supported by grant R00DA042127 from the National Institute on Drug Abuse (K.E.R.), grant K99ES027023 from the National Institute of Environmental Health Sciences (J.A.C.), grant R00CA201542 from the National Cancer Institute (P.J.), and by the Intramural Research Program of the National Institute of Mental Health (ZIAMH002808).
Computing code and data: Computing code to replicate results is posted here: https://github.com/kararudolph/code-for-papers/blob/master/NCSAnoisepaper.R Those interested can apply to access the restricted National Comorbidity Survey Replication Adolescent Supplement data here: https://www.icpsr.umich.edu/icpsrweb/HMCA/studies/28581.
Supplemental digital content is available through direct URL citations in the HTML and PDF versions of this article (www.epidem.com).
References
- 1.Basner M, Babisch W, Davis A, et al. Auditory and non-auditory effects of noise on health. Lancet 20143831325–1332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Basner M, McGuire S. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and effects on sleep. Int J Environ Res Public Health 201815519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weyde KV, Krog NH, Oftedal B, et al. Nocturnal road traffic noise exposure and children’s sleep duration and sleep problems. Int J Environ Res Public Health 201714491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Orban E, McDonald K, Sutcliffe R, et al. Residential road traffic noise and high depressive symptoms after five years of follow-up: results from the Heinz Nixdorf recall study. Environ Health Perspect 2016124578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sygna K, Aasvang GM, Aamodt G, Oftedal B, Krog NH. Road traffic noise, sleep and mental health. Environ Res 201413117–24 [DOI] [PubMed] [Google Scholar]
- 6.Hardoy MC, Carta MG, Marci AR, et al. Exposure to aircraft noise and risk of psychiatric disorders: the Elmas survey–aircraft noise and psychiatric disorders. Soc Psychiatry Psychiatr Epidemiol 20054024–26 [DOI] [PubMed] [Google Scholar]
- 7.van Kamp I, Davies H. Environmental noise and mental health: five year review and future directions. In: Proceedings of the 9th International Congress on Noise as a Public Health ProblemJuly 21–25,2008Mashantucket, Connecticut [Google Scholar]
- 8.Fritschi L, Brown AL, Kim R, Schwela DH, Kephalopoulos S. Burden of Disease From Environmental Noise 2011Copenhagen, Denmark: World Health Organization [Google Scholar]
- 9.Paruthi S, Brooks LJ, D’Ambrosio C, et al. Recommended amount of sleep for pediatric populations: a consensus statement of the American Academy of Sleep Medicine. J Clin Sleep Med 201612785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olds T, Blunden S, Petkov J, Forchino F. The relationships between sex, age, geography and time in bed in adolescents: a meta-analysis of data from 23 countries. Sleep Med Rev 201014371–378 [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 200562593–602 [DOI] [PubMed] [Google Scholar]
- 12.Muzet A. Environmental noise, sleep and health. Sleep Med Rev 200711135–142 [DOI] [PubMed] [Google Scholar]
- 13.Stansfeld S, Clark C. Health effects of noise exposure in children. Curr Environ Health Rep 20152171–178 [DOI] [PubMed] [Google Scholar]
- 14.Öhrström E, Hadzibajramovic E, Holmes M, Svensson H. Effects of road traffic noise on sleep: studies on children and adults. J Environ Psychol 200626116–126 [Google Scholar]
- 15.Tiesler CM, Birk M, Thiering E, et al. Exposure to road traffic noise and children’s behavioural problems and sleep disturbance: results from the GINIplus and LISAplus studies. Environ Res 20131231–8 [DOI] [PubMed] [Google Scholar]
- 16.Skrzypek M, Kowalska M, Czech EM, Niewiadomska E, Zejda JE. Impact of road traffic noise on sleep disturbances and attention disorders amongst school children living in Upper Silesian Industrial Zone, Poland. Int J Occup Med Environ Health 201730511. [DOI] [PubMed] [Google Scholar]
- 17.Haines MM, Stansfeld SA, Job RF, Berglund B, Head J. Chronic aircraft noise exposure, stress responses, mental health and cognitive performance in school children. Psychol Med 200131265–277 [DOI] [PubMed] [Google Scholar]
- 18.Weyde KV, Krog NH, Oftedal B, et al. Road traffic noise and children’s inattention. Environ Health 201716127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Crombie R, Clark C, Stansfeld SA. Environmental noise exposure, early biological risk and mental health in nine to ten year old children: a cross-sectional field study. Environ Health 20111039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stansfeld SA, Clark C, Cameron RM, et al. Aircraft and road traffic noise exposure and children’s mental health. J Environ Psychol 200929203–207 [Google Scholar]
- 21.Evans GW, Bullinger M, Hygge S. Chronic noise exposure and physiological response: a prospective study of children living under environmental stress. Psychol Sci 1998975–77 [Google Scholar]
- 22.Dzhambov A, Tilov B, Markevych I, Dimitrova D. Residential road traffic noise and general mental health in youth: the role of noise annoyance, neighborhood restorative quality, physical activity, and social cohesion as potential mediators. Environ Int 20171091–9 [DOI] [PubMed] [Google Scholar]
- 23.March D, Hatch SL, Morgan C, et al. Psychosis and place. Epidemiol Rev 20083084–100 [DOI] [PubMed] [Google Scholar]
- 24.Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr Scand 201012184–93 [DOI] [PubMed] [Google Scholar]
- 25.Vassos E, Agerbo E, Mors O, Pedersen CB. Urban–rural differences in incidence rates of psychiatric disorders in Denmark. Br J Psychiatry 2016208435–440 [DOI] [PubMed] [Google Scholar]
- 26.Hale L, Do DP. Racial differences in self-reports of sleep duration in a population-based study. Sleep 2007301096–1103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Casey JA, Morello-Frosch R, Mennitt DJ, Fristrup K, Ogburn EL, James P. Race/ethnicity, socioeconomic status, residential segregation, and spatial variation in noise exposure in the contiguous United States. Environ Health Perspect 2017125077017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rudolph KE, Stuart EA, Glass TA, Merikangas KR. Neighborhood disadvantage in context: the influence of urbanicity on the association between neighborhood disadvantage and adolescent emotional disorders. Soc Psychiatry Psychiatr Epidemiol 201449467–475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.US Environmental Protection Agency Office of Noise Abatement and Control. Information on Levels of Environmental Noise Requisite to Protect Public Health and Welfare With an Adequate Margin of Safety. Volume 74, for sale by the Supt. of Docs., US Govt. Print. Off. 1974 Available at: https://nepis.epa.gov/Exe/ZyNET.exe/2000L3LN.TXT?ZyActionD=ZyDocument&Client=EPA&Index=Prior+to+1976&Docs=&Query=&Time=&EndTime=&SearchMethod=1&TocRestrict=n&Toc=&TocEntry=&QField=&QFieldYear=&QFieldMonth=&QFieldDay=&IntQFieldOp=0&ExtQFieldOp=0&XmlQuery=&File=D%3A%5Czyfiles%5CIndex%20Data%5C70thru75%5CTxt%5C00000001%5C2000L3LN.txt&User=ANONYMOUS&Password=anonymous&SortMethod=h%7C-&MaximumDocuments=1&FuzzyDegree=0&ImageQuality=r75g8/r75g8/x150y150g16/i425&Display=hpfr&DefSeekPage=x&SearchBack=ZyActionL&Back=ZyActionS&BackDesc=Results%20page&MaximumPages=1&ZyEntry=1&SeekPage=x&ZyPURL. Accessed 7 June, 2019.
- 30.Hammer MS, Swinburn TK, Neitzel RL. Environmental noise pollution in the United States: developing an effective public health response. Environ Health Perspect 2014122115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Merikangas KR, Avenevoli S, Costello EJ, Koretz D, Kessler RC. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): I. Background and measures. J Am Acad Child Adolesc Psychiatry 200948367–379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kessler RC, Avenevoli S, Costello EJ, et al. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): II. Overview and design. J Am Acad Child Adolesc Psychiatry 200948380–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kessler RC, Avenevoli S, Costello EJ, et al. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A). Int J Methods Psychiatr Res 20091869–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Angold A, Weissman MM, John K, et al. Parent and child reports of depressive symptoms in children at low and high risk of depression. J Child Psychol Psychiatry 198728901–915 [DOI] [PubMed] [Google Scholar]
- 35.Merikangas KR, He JP, Burstein M, et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 201049980–989 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kessler RC, Avenevoli S, Green J, et al. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): III. Concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J Am Acad Child Adolesc Psychiatry 200948386–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mennitt DJ, Fristrup KM. Influence factors and spatiotemporal patterns of environmental sound levels in the contiguous United States. Noise Control Eng J 201664342–353 [Google Scholar]
- 38.Novotny EV, Bechle MJ, Millet DB, Marshall JD. National satellite-based land-use regression: NO2 in the United States. Environ Sci Technol 2011454407–4414 [DOI] [PubMed] [Google Scholar]
- 39.James P, Banay RF, Hart JE, Laden F. A review of the health benefits of greenness. Curr Epidemiol Rep 20152131–142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Disease Control Centers, Prevention. North America Land Data Assimilation System (NLDAS) Daily Air Temperatures and Heat Index 2017. Available at: https://catalog.data.gov/dataset/cdc-wonder-daily-air-temperatures-and-heat-index Accessed February 9, 2017.
- 41.Diez-Roux AV, Kiefe CI, Jacobs DR, Jr, et al. Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Ann Epidemiol 200111395–405 [DOI] [PubMed] [Google Scholar]
- 42.Rudolph KE, Wand GS, Stuart EA, et al. The association between cortisol and neighborhood disadvantage in a US population-based sample of adolescents. Health Place 20142568–77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.van Buuren S, Groothuis-Oudshoorn K. mice: multivariate imputation by chained equations in R. J Stat Softw 201145 [Google Scholar]
- 44.Stuart EA, Azur M, Frangakis C, Leaf P. Multiple imputation with large data sets: a case study of the Children’s Mental Health Initiative. Am J Epidemiol 20091691133–1139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Meng X-L. Multiple-imputation inferences with uncongenial sources of input. Stat Sci 19949538–558 [Google Scholar]
- 46.Rubin DB. Multiple Imputation for Nonresponse in Surveys, Volume 81 2004New York, NY: John Wiley & Sons [Google Scholar]
- 47.Stuart EA, Green KM. Using full matching to estimate causal effects in nonexperimental studies: examining the relationship between adolescent marijuana use and adult outcomes. Dev Psychol 200844395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Reiss F. Socioeconomic inequalities and mental health problems in children and adolescents: a systematic review. Soc Sci Med 20139024–31 [DOI] [PubMed] [Google Scholar]
- 49.van der Laan MJ, Rubin D. Targeted maximum likelihood learning. Int J Biostat 20062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Methodol 199557289–300 [Google Scholar]
- 51.Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci 2010251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stürmer T, Rothman KJ, Avorn J, Glynn RJ. Treatment effects in the presence of unmeasured confounding: dealing with observations in the tails of the propensity score distribution—a simulation study. Am J Epidemiol 2010172843–854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Petersen ML, Porter KE, Gruber S, Wang Y, van der Laan MJ. Diagnosing and responding to violations in the positivity assumption. Stat Methods Med Res 20122131–54 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schmidt CW. Noise that annoys: regulating unwanted sound. Environ Health Perspect 2005113A42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Johnson SC. Hierarchical clustering schemes. Psychometrika 196732241–254 [DOI] [PubMed] [Google Scholar]
- 56.Tzivian L, Dlugaj M, Winkler A, et al. Long-term air pollution and traffic noise exposures and mild cognitive impairment in older adults: a cross-sectional analysis of the Heinz Nixdorf recall study. Environ Health Perspect 20161241361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Forns J, Dadvand P, Foraster M, et al. Traffic-related air pollution, noise at school, and behavioral problems in Barcelona schoolchildren: a cross-sectional study. Environ Health Perspect 2016124529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Clark C, Crombie R, Head J, van Kamp I, van Kempen E, Stansfeld SA. Does traffic-related air pollution explain associations of aircraft and road traffic noise exposure on children’s health and cognition? A secondary analysis of the United Kingdom sample from the RANCH project. Am J Epidemiol 2012176327–337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dzhambov A, Hartig T, Markevych I, Tilov B, Dimitrova D. Urban residential greenspace and mental health in youth: different approaches to testing multiple pathways yield different conclusions. Environ Res 201816047–59 [DOI] [PubMed] [Google Scholar]
- 60.Bronzaft AL, McCarthy DP. The effect of elevated train noise on reading ability. Environ Behav 19757517–528 [Google Scholar]
- 61.Cohen S, Evans GW, Krantz DS, Stokols D. Physiological, motivational, and cognitive effects of aircraft noise on children: moving from the laboratory to the field. Am Psychol 198035231. [DOI] [PubMed] [Google Scholar]
- 62.Evans GW, Maxwell L. Chronic noise exposure and reading deficits: the mediating effects of language acquisition. Environ Behav 199729638–656 [Google Scholar]
- 63.Sharp B, Connor TL, McLaughlin D, Clark C, Stansfeld SA, Hervey J. Assessing aircraft noise conditions affecting student learning 2014Washington, DC: Transportation Research Board of the National Academies [Google Scholar]
- 64.Clark C, Paunovic K. WHO environmental noise guidelines for the European region: a systematic review on environmental noise and cognition. Int J Environ Res Public Health 201815285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dreger S, Meyer N, Fromme H, Bolte G; Study Group of the GME cohort Environmental noise and incident mental health problems: a prospective cohort study among school children in Germany. Environ Res 201514349–54 [DOI] [PubMed] [Google Scholar]
- 66.Clark C, Head J, Stansfeld SA. Longitudinal effects of aircraft noise exposure on children’s health and cognition: a six-year follow-up of the UK RANCH cohort. J Environ Psychol 2013351–9 [Google Scholar]
- 67.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev 199869875–887 [PubMed] [Google Scholar]
- 68.Sivertsen B, Harvey AG, Lundervold AJ, Hysing M. Sleep problems and depression in adolescence: results from a large population-based study of Norwegian adolescents aged 16–18 years. Eur Child Adolesc Psychiatry 201423681–689 [DOI] [PubMed] [Google Scholar]
- 69.Asarnow LD, McGlinchey E, Harvey AG. The effects of bedtime and sleep duration on academic and emotional outcomes in a nationally representative sample of adolescents. J Adolesc Health 201454350–356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hasler BP, Franzen PL, de Zambotti M, et al. Eveningness and later sleep timing are associated with greater risk for alcohol and marijuana use in adolescence: initial findings from the National Consortium on Alcohol and Neurodevelopment in Adolescence study. Alcohol Clin Exp Res 2017411154–1165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Zhang J, Paksarian D, Lamers F, Hickie IB, He J, Merikangas KR. Sleep patterns and mental health correlates in US adolescents. J Pediatr 2017182137–143 [DOI] [PubMed] [Google Scholar]
- 72.Pasch KE, Laska MN, Lytle LA, Moe SG. Adolescent sleep, risk behaviors, and depressive symptoms: are they linked? Am J Health Behav 201034237–248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lee YJ, Cho SJ, Cho IH, Kim SJ. Insufficient sleep and suicidality in adolescents. Sleep 201235455–460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sivertsen B, Skogen JC, Jakobsen R, Hysing M. Sleep and use of alcohol and drug in adolescence. A large population-based study of Norwegian adolescents aged 16 to 19 years. Drug Alcohol Depend 2015149180–186 [DOI] [PubMed] [Google Scholar]
- 75.Roenneberg T, Merrow M. The circadian clock and human health. Curr Biol 201626R432–R443 [DOI] [PubMed] [Google Scholar]
- 76.Zare Sakhvidi F, Zare Sakhvidi MJ, Mehrparvar AH, Dzhambov AM. Environmental noise exposure and neurodevelopmental and mental health problems in children: a systematic review. Curr Environ Health Rep 20185365–374 [DOI] [PubMed] [Google Scholar]
- 77.Hjortebjerg D, Andersen AM, Christensen JS, et al. Exposure to road traffic noise and behavioral problems in 7-year-old children: a cohort study. Environ Health Perspect 2015124228–234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Oakes JM. Commentary: advancing neighbourhood-effects research–selection, inferential support, and structural confounding. Int J Epidemiol 200635643–647 [DOI] [PubMed] [Google Scholar]
- 79.Colson KE, Rudolph KE, Zimmerman SC, et al. Optimizing matching and analysis combinations for estimating causal effects. Sci Rep 2016623222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Green JG, Gruber MJ, Kessler RC, et al. Diagnostic validity across racial and ethnic groups in the assessment of adolescent DSM-IV disorders. Int J Methods Psychiatr Res 201221311–320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Evans WN, Morrill MS, Parente ST. Measuring inappropriate medical diagnosis and treatment in survey data: the case of ADHD among school-age children. J Health Econ 201029657–673 [DOI] [PubMed] [Google Scholar]
- 82.Layton TJ, Barnett ML, Hicks TR, Jena AB. Attention deficit–hyperactivity disorder and month of school enrollment. N Engl J Med 20183792122–2130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Job RF. Noise sensitivity as a factor influencing human reaction to noise. Noise Health 1999157–68 [PubMed] [Google Scholar]
- 84.Stansfeld SA, Shipley M. Noise sensitivity and future risk of illness and mortality. Sci Total Environ 2015520114–119 [DOI] [PubMed] [Google Scholar]
- 85.Wallas A, Eriksson C, Gruzieva O, et al. Road traffic noise and determinants of saliva cortisol levels among adolescents. Int J Hyg Environ Health 2018221276–282 [DOI] [PubMed] [Google Scholar]
- 86.van Kempen EE, van Kamp I, Stellato RK, et al. Children’s annoyance reactions to aircraft and road traffic noise. J Acoust Soc Am 2009125895–904 [DOI] [PubMed] [Google Scholar]
- 87.Babisch W, Schulz C, Seiwert M, Conrad A. Noise annoyance as reported by 8-to 14-year-old children. Environ and Behav 20124468–86 [Google Scholar]
- 88.Stansfeld SA, Matheson MP. Noise pollution: non-auditory effects on health. Br Med Bull 200368243–257 [DOI] [PubMed] [Google Scholar]
- 89.von Lindern E, Hartig T, Lercher P. Traffic-related exposures, constrained restoration, and health in the residential context. Health Place 20163992–100 [DOI] [PubMed] [Google Scholar]
- 90.Foraster M, Künzli N, Aguilera I, et al. High blood pressure and long-term exposure to indoor noise and air pollution from road traffic. Environ Health Perspect 20141221193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Roswall N, Ammitzbøll G, Christensen JS, et al. Residential exposure to traffic noise and leisure-time sports–a population-based study. Int J Hyg Environ Health 20172201006–1013 [DOI] [PubMed] [Google Scholar]
- 92.Honold J, Wippert P-M, van der Meer E. Urban health resources: physical and social constitutes of neighborhood social capital. Procedia Soc Behav Sci 2014131491–496 [Google Scholar]
- 93.Correia AW, Peters JL, Levy JI, Melly S, Dominici F. Residential exposure to aircraft noise and hospital admissions for cardiovascular diseases: multi-airport retrospective study. BMJ 2013347f5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Stansfeld SA, Berglund B, Clark C, et al. Aircraft and road traffic noise and children’s cognition and health: a cross-national study. Lancet 20053651942–1949 [DOI] [PubMed] [Google Scholar]
- 95.Rubin DB. Comment: which ifs have causal answers. J Am Stat Assoc 198681961–962 [Google Scholar]
- 96.Blackwell M, Honaker J, King G. A unified approach to measurement error and missing data: overview and applications. Sociol Methods Res 201746303–341 [Google Scholar]
- 97.Riedel N, Fuks K, Hoffmann B, et al. Insomnia and urban neighbourhood contexts–are associations modified by individual social characteristics and change of residence? Results from a population-based study using residential histories. BMC Public Health 201212810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lercher P, Evans GW, Meis M, Kofler WW. Ambient neighbourhood noise and children’s mental health. Occup Environ Med 200259380–386 [DOI] [PMC free article] [PubMed] [Google Scholar]


