Abstract
A general assumption that deployment is the primary catalyst for psychological and social difficulties may contribute to under-recognition and under-treatment of problems among never-deployed service members (i.e., having no history of ever being deployed). We aimed to determine if ever-deployed (i.e., having a history of at least one deployment) and never-deployed United States Army Reserve and National Guard (USAR/NG) soldiers differed in mental health, substance use, and resiliency factors, and to determine the relative influence of deployment status and each of these factors on poor psychosocial outcomes. We analyzed a subset of data from Operation:SAFETY (N = 404), an ongoing study examining the health and well-being of USAR/NG soldiers. Bivariate analyses demonstrated that soldiers did not significantly differ across a range of measures on the basis of deployment status (ps > 0.05). In fact, Factor Analyses and Discriminant Function Analysis revealed that deployment status was the least salient factor to psychosocial problems among the measured variables and that the observed variables could not accurately discriminate between ever-deployed and never-deployed soldiers, F(8, 374) = 1.34, p > 0.05. Measures of mental health and substance use were more salient to psychosocial problems (ps < 0.05). Measures of resiliency loaded negatively onto psychosocial problems (ps < 0.05), indicating that they contribute to better well-being. Targeting screening and intervention efforts only on soldiers who have been deployed will miss opportunities to intervene on an equally affected group. Resiliency factors should be considered as intervention targets.
Military populations are at risk for psychological and social issues, including alcohol and drug abuse (Bray, Brown, & Williams, 2013; Eisen et al., 2004; Green, Beckham, Youssef, & Elbogen, 2014; Hoopsick, Fillo, Vest, Homish, & Homish, 2017; Jacobson et al., 2008; Milliken, Auchterlonie, & Hoge, 2007; J. L. Thomas et al., 2010), mental health problems (Eisen et al., 2004; Milliken et al., 2007; J. L. Thomas et al., 2010), and relationship conflict (Gibbons, Barnett, & Hickling, 2012; Heavey, Homish, Goodell, & Homish, 2017; Milliken et al., 2007). The interdependent relationships among mental and emotional wellbeing and the social environment have been well-studied in psychological research and are the focus of evidence-based psychosocial assessments and interventions (Institute of Medicine, 2015). Yet, to what extent deployment status contributes to psychosocial difficulties among military personnel has not been well-described. This dearth of research likely contributes to the general notion that whether or not a service member has deployed is the key determinant of military psychosocial problems.
Problems Among Service Members Who Have Been Deployed
There is robust evidence (Bray & Hourani, 2007; Hassija, Jakupcak, Maguen, & Shipherd, 2012; Hoopsick, Vest, Homish, & Homish, 2018; Jacobson et al., 2008; Larson, Mohr, Jeffery, Adams, & Williams, 2016; Milliken et al., 2007; Renshaw, Rodrigues, & Jones, 2009; Seal et al., 2011; M. M. Thomas, Harpaz-Rotem, Tsai, Southwick, & Pietrzak, 2017; Vest, Heavey, Homish, & Homish, 2017; Vest, Homish, Hoopsick, & Homish, 2018; Vogt et al., 2011) demonstrating the effects of combat deployment on a range of psychological problems in various military populations. Among military service members that have been deployed, combat exposure is a well-established risk factor for problematic alcohol and other substance use (Hassija et al., 2012; Hoopsick, Vest, et al., 2018; Jacobson et al., 2008; Larson et al., 2016; Milliken et al., 2007; Seal et al., 2011; Vest et al., 2018; Wright, Foran, Wood, Eckford, & McGurk, 2012) Similarly, combat exposure has been associated with aggression (Heavey et al., 2017; Milliken et al., 2007; Vest et al., 2017), anxiety (M. M. Thomas et al., 2017; Vest et al., 2017), depression (Hassija et al., 2012; Renshaw et al., 2009; Vest et al., 2017), and posttraumatic stress disorder (PTSD) (Hassija et al., 2012; Milliken et al., 2007; Renshaw et al., 2009; M. M. Thomas et al., 2017; Vest et al., 2017; Vogt et al., 2011). However, some resiliency factors have been shown to positively contribute to the psychological well-being of military populations by buffering the effects of combat. For example, psychological hardiness (i.e. the dispositional resiliency of an individual in approaching and interpreting experiences) is protective of problems with alcohol (Bartone et al., 2015; Bartone, Hystad, Eid, & Brevik, 2012; Green et al., 2014) and symptoms of war-related stress, including depression and anxiety (Bartone, 1999). Greater marital functioning (i.e., marital satisfaction and adjustment of partners to each other) has also been shown to be a resiliency factor for these issues (Vest et al., 2017; Vest et al., 2018).
Despite similar roles and combat experiences, Reserve/Guard service members have a greater risk of substance use and mental health symptomatology than active duty service members (Cohen, Fink, Sampson, & Galea, 2015; Griffith, 2010; Hotopf et al., 2006; Jacobson et al., 2008; Milliken et al., 2007; Rundell, 2006; Vasterling et al., 2010) and represent an understudied, but high-risk group. For example, research has demonstrated a greater risk for post-deployment PTSD (Hoge, Auchterlonie, & Milliken, 2006; Hotopf et al., 2006; J. L. Thomas et al., 2010), aggression (J. L. Thomas et al., 2010), and alcohol misuse (Cohen et al., 2015; Griffith, 2010; Jacobson et al., 2008; Milliken et al., 2007; J. L. Thomas et al., 2010) among Reserve/Guard service members compared to active duty service members. This increased risk among Reserve/Guard service members may be due to having less unit support as compared to active duty service members who spend more time with their unit (Griffith, 2010, 2015). Civilian employment and financial stressors might also contribute to differences between Reserve/Guard service members and active duty services members; Reserve/Guard soldiers must rely on income from civilian employment supplemented by their military service (Griffith, 2011). Further, one study suggests that nearly 1 in 5 Reserve/Guard families has experienced financial difficulties due to a deployment and 1 in 10 experienced job loss (Riviere, Kendall-Robbins, McGurk, Castro, & Hoge, 2011). Combat can have detrimental effects on the psychological and social well-being of service members who have been deployed, particularly among Reserve/Guard service members. However, few studies have compared these factors between never-deployed and ever-deployed service members or described to what extent deployment status contributes to these problems.
Problems Among Service Members Who Have Never Been Deployed
Although the effects of combat exposure are important to consider in the overall health and wellbeing of military populations, it is possible that a lack of research comparing service members who have and have not been deployed may contribute to an under-recognition and under-treatment of mental health and substance use problems among service members who have not experienced deployment. While 49% of Reserve/Guard service members were deployed in 2017 (Defense Manpower Data Center, 2017), a significant proportion of Reserve/Guard service members do not deploy. Not deploying may have detrimental effects on the emotional well-being of these service members; previous research (Hoopsick, Homish, Bartone, & Homish, in press) demonstrated that never-deployed Reserve/Guard soldiers experience negative emotions related to having never been deployed, such as feelings of guilt, decreased value, decreased connectedness, and decreased camaraderie. Other research suggests that service members with more severe mental health symptomology are less likely to be deployed (Ireland, Kress, & Frost, 2012; Wilson et al., 2009), and this “healthy warrior effect” may leave never-deployed Reserve/Guard soldiers an even more susceptible subgroup within an already high-risk population.
Limited evidence (Fink et al., 2016; Hoopsick et al., in press; Hoopsick, Homish, Vest, & Homish, 2018; Jacobson et al., 2008; Kang et al., 2015; Russell et al., 2015; Trautmann et al., 2014; Wells et al., 2010; Worthen et al., 2015) suggests that psychological problems, including mental illness and substance use, are prevalent among never-deployed service members. Findings from the Millennium Cohort Study showed that the percentage of new-onset depression among never-deployed service members was higher than that of those who were deployed but not exposed to combat (3.9% vs. 2.3% among male service members and 7.7% vs. 5.1% among female service members) (Wells et al., 2010). In a study of 1.3 million veterans, those who never deployed had a higher risk of suicide than those who had previously been deployed (Kang et al., 2015). Research also suggests that suicidal ideation may be higher among soldiers who have been deployed, but that suicidal ideation was associated with PTSD among both never-deployed and ever-deployed soldiers (Vanderploeg et al., 2015). Population data show that the prevalence of lifetime non-deployment-related PTSD (5.4%) is similar to that of deployment-related PTSD (5.5%) among Reserve service members (Russell et al., 2015). Further, prior research demonstrated no difference in the prevalence of substance use or substance use disorders between recently deployed and never-deployed service members (Trautmann et al., 2014). Other research has demonstrated that civilian-related trauma may be more relevant to psychological problems in military populations than deployment-related trauma (Worthen et al., 2014, 2015). Taken together, this suggests that deployment may not be the only factor in the psychological problems among military populations.
Prior research has not compared a wide range of risk and protective factors among never- and ever-deployed Reserve/Guard service members, who both appear to be at increased risk for substance use and mental health symptomatology compared to active duty service members (Griffith, 2010; Renshaw, 2010; Riviere et al., 2011; J. L. Thomas et al., 2010). Moreover, to our knowledge, no studies have demonstrated the comparative salience of deployment status relative to other determinants in the prediction of psychosocial health and wellness in military personnel. Current intervention efforts focused only on the effects of combat deployment may miss opportunities to intervene on other more salient factors. Given the emerging evidence suggesting that never-deployed soldiers may also have poor outcomes, it is critical to gain a better understanding of what contributes to psychosocial issues among these soldiers to develop more targeted intervention efforts. This study examined what factors are the most salient to the formation of psychosocial problems among a sample of USAR/NG soldiers, which may help to inform intervention efforts aimed at reducing psychosocial military sequelae among USAR/NG soldiers as a whole.
The Current Study
The current study examined a subset of the 1-year follow-up data from Operation:SAFETY, an ongoing survey-based study that examines the health and well-being of USAR/NG soldiers and their partners. Using a sample of never- and ever-deployed USAR/NG soldiers, we sought to answer the following research questions: (1) do mental health problems, substance use, and resiliency factors differ on the basis of deployment status among USAR/NG soldiers?; (2) do observed variables representing mental health symptomatology (i.e., anger, anxiety, depression, PTSD), substance use (i.e., hazardous drinking and drug use), deployment status, and resiliency factors (i.e., psychological hardiness and marital satisfaction) form a unidimensional latent construct (i.e., psychosocial problems) and if so, what is the order of salience of these variables to psychosocial problems?; and (3) what is the discriminatory power of the aforementioned variables to differentiate between varying levels of psychosocial problems among USAR/NG soldiers?
Materials and Methods
Recruitment
We recruited USAR/NG soldiers and their partners from 47 units across New York, United States between the summer of 2014 and the fall of 2015 for the Operation:SAFETY study. The military occupational specialties of these units were diverse and included combat, medical, logistics, and support roles. Participation involved the completion of three online surveys (baseline with two yearly follow-ups), covering a variety of general health topics. In order to be eligible for the study, all of the following inclusion criteria must have been met: (1) the couple is married or living as if married; (2) one member of the couple dyad is a current Army Reserve soldier or National Guard soldier; (3) the soldier is between the ages of 18 and 45; (4) both partners are able to speak and understand English; (5) both partners are willing and able to participate; and (6) both partners have had at least one alcoholic beverage in the past year. A total of 731 soldiers and partners were eligible for inclusion in [BLINDED – STUDY NAME]. Of those, 572 (78%) agreed to participate and 83% of these couples (N = 472, 65% of those eligible) completed some part of the survey. Surveys were included only if both partners completed follow-up (N = 418). We conducted sensitivity analyses and found that couples where a civilian partner screened for the study (n = 11) were less likely to enroll (p < 0.001) than couples where a soldier screened for the study.
Participants
The current study, a substudy of Operation:SAFETY, examined cross-sectional 1-year follow-up data from soldiers who completed the first and second waves of the ongoing study (N = 404). Participants were predominantly Non-Hispanic European American (79.5%), had at least some college education (87.9%), and were an enlisted rank (83.9%); see Table 1. Tests of two proportions revealed that when compared to never-deployed soldiers (n = 160), soldiers who had previously been deployed were more likely to be male (88.9% vs. 73.8%, p < 0.001) and have an annual household income ≥ $60,000 (66.1% vs. 41.03%, p < 0.001). T-tests also showed that soldiers who had previously been deployed tended to be older, t(401) = −8.3, p < 0.001 (M = 34.4, SD = 5.8 vs. M = 29.4, SD = 5.9) and have served more years in the military, t(402) = −12.7, p < 0.001 (M = 12.2, SD = 5.6 vs. M = 5.7, SD = 4.2) than never-deployed soldiers.
Table 1.
Characteristics of US Army Reserve and National Guard Soldiers
| Never-Deployed (n = 160) | Ever-Deployed (n = 244) | Significance Testa | |
|---|---|---|---|
| % (n) or mean (±SD) | % (n) or mean (±SD) | p-values | |
| Sex | |||
| Male | 73.8% (118) | 88.9% (217) | |
| Female | 26.3% (42) | 11.1% (27) | < 0.001 |
| Age | 29.4 (±5.9) | 34.4 (±5.8) | < 0.001 |
| Race/Ethnicity | |||
| Non-Hispanic European American | 77.7% (122) | 83.3% (199) | |
| Non-Hispanic African American | 7.6% (12) | 4.6% (11) | |
| Hispanic | 8.3% (13) | 8.4% (20) | |
| Other | 6.4% (10) | 3.8% (9) | 0.360 |
| Years of Service | 5.7 (±4.2) | 12.2 (±5.6) | < 0.001 |
| Education | |||
| <HS – HS Grad | 12.5% (20) | 11.9% (29) | |
| Some College | 51.9% (83) | 56.6% (138) | |
| College + | 35.6% (57) | 31.6% (77) | 0.657 |
| Total Family Income | |||
| ≤ $19,999 | 8.3% (13) | 0.9% (2) | |
| $20,000 -- $59,999 | 50.6% (79) | 33.1% (78) | |
| $60,000 -- $99,999 | 29.5% (46) | 41.1% (97) | |
| ≥ $100,000 | 11.5% (18) | 25.0% (59) | < 0.001 |
| Relationship Status | |||
| Married or Cohabitating | 93.8% (150) | 95.9% (234) | |
| Separated or Divorced | 6.3% (10) | 4.1% (10) | 0.330 |
| Rank | |||
| Enlisted | 84.3% (134) | 84.4% (205) | |
| Officer | 15.7% (25) | 15.6% (38) | 0.982 |
| AUDIT Score | 3.8 (±3.4) | 4.5 (±3.8) | 0.074 |
| Current Drug Use | |||
| Yes | 6.9% (11) | 7.0% (17) | |
| No | 93.1% (149) | 93.0% (226) | 0.963 |
| PROMIS Anger Score | 17.0 (±6.2) | 17.9 (±6.8) | 0.217 |
| Anxiety Score | 4.0 (±5.4) | 4.8 (±6.1) | 0.190 |
| PHQ-8 Score | 2.9 (±4.0) | 3.5 (±4.4) | 0.206 |
| PCL-5 Score | 7.4 (±12.2) | 10.7 (±13.2) | 0.012 |
| Dispositional Resiliency Scale Score | 31.3 (±5.8) | 31.2 (±5.6) | 0.885 |
| MAT Score | 113.7 (±26.3) | 109.1 (±30.0) | 0.121 |
T-tests for differences in means, chi-square tests for differences in distributions
Procedures
Surveys were administered and encrypted with the HIPAA-compliant survey programming software, StudyTrax™. Participants had the option to complete their consent and survey at the the University at Buffalo Center for Health Research or to complete the same consent and survey online using unique login information. Baseline surveys took approximately 2 ½ hours to complete and follow-ups lasted 90 minutes. Soldiers and partners each received a $60 check for baseline and a $70 check for each of the follow-ups.
Measures
Hazardous Drinking.
We assessed hazardous drinking with the Alcohol Use Disorders Identification Test (AUDIT) (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993). The AUDIT consists of 10 items rated on a 4-point scale from “Never” to “Daily or almost daily,” with total scores ranging from 0 – 40. Items include questions such as “Have you or someone else been injured because of your drinking?” and “How often during the last year have you had a feeling of guilt or remorse after drinking?” Invariance testing has shown that the psychometric properties of the AUDIT are equivalent across sex and assessment settings (Moehring et al., 2018). This measure has been shown to have high internal consistency across a range of populations and settings, α = 0.75 – 0.94 (Allen, Litten, Fertig, & Babor, 1997) and had good internal consistency reliability for our sample, α = 0.76. Hazardous drinking was entered as a count variable in all analyses.
Drug Use.
We used the NIDA Modified ASSIST 2.0 (Alcohol, Smoking, and Substance Involvement Screening Test) to assess current drug use (i.e. past 3 months). The ASSIST was previously vigorously tested with three phases to examine and ensure reliability and validity across settings and cultures (WHO Assist Working Group, 2002). Research has shown that the ASSIST has concurrent validity with other validated measures of substance use and dependence, r = 0.59 – 0.88, p < 0.05 (Humeniuk et al., 2008). The ASSIST captures both lifetime and current use, but we focused on current use with the question “In the past three months, how often have you used [substance]?” for illicit drugs and nonmedical use of prescription drugs. The test-retest reliability for consistency of reporting drug use in the last three months has been shown to be high with the ASSIST, Kappa = 0.66 – 0.95 (WHO Assist Working Group, 2002). Any current drug use was dichotomized (yes/no) and included as a binary variable in all analyses.
Anger.
We assessed anger with the Adult Anger Short Form from the Emotional Distress Scale of the Patient Reported Outcomes Measurement Information System (PROMIS) (Pilkonis et al., 2011). This 8-item measure assesses the frequency with which the respondent experienced various states of anger in the past 7 days. Items include statements such as “I was irritated more than people knew” and “I felt angrier than I thought I should.” Each item was scored 1 – 5 on a Likert scale with responses ranging from “Never” to “Always.” Scores can range from 8 – 40, with higher scores indicating greater anger. Examination of the ecological validity of this measure demonstrate that 7-day recall of anger using the PROMIS was well-correlated with daily ratings of anger, r = 0.73 – 0.83, p < 0.001 (Stone, Broderick, Junghaenel, Schneider, & Schwartz, 2016). This measure had high internal consistency reliability in our sample (α = 0.94). PROMIS anger score was considered as a count variable in all analyses.
Anxiety.
To strengthen the potential application of our findings to clinical practice, we assessed anxiety with 10 items based upon the “emerging measures” from DSM-5 (Craske et al., 2013). The items examine the past 7 days on a Likert scale scored 0 – 4 ranging from “Never” to “All of the time.” Example items include “Felt moments of sudden terror, fear or fright” and “Felt anxious, worried, or nervous.” Scores range from 0 – 40, with higher scores indicating a greater severity of anxiety. Preliminary evidence demonstrates that these measures have high internal consistency, unidimensionality, and convergent and discriminant validity (Lebeau et al., 2012). The internal consistency reliability for the Severity Measure for Generalized Anxiety Disorder was high in our sample (α = 0.92). We entered anxiety score as a count variable in all analyses.
Depression.
We assessed depression using the 8-item Patient Health Questionnaire (PHQ-8) (Kroenke et al., 2009), a modified version of the 9-item Patient Health Questionnaire (PHQ-9) (Kroenke, Spitzer, & Williams, 2001). The PHQ-8 assesses the frequency with which the respondent has been affected by depressed states over the last 2 weeks, such as “Feeling down, depressed, or hopeless” and “Feeling bad about yourself.” The PHQ-8 differs from the PHQ-9 in that it does not include an item assessing suicidal/self-injurious thoughts. Due to the nature of a web-based assessment, immediate intervention could not be ensured for participants at risk for immediate self-harm. However, the PHQ-8 has been shown to be a valid and reliable measure of current depression for use in the general population (Kroenke et al., 2009). Items are scored 0 – 3 on a Likert scale ranging from “Not at all” to “Nearly every day.” Scores range from 0 – 24, with higher scores indicating a greater severity of depression. The PHQ-8 had high internal consistency reliability in our sample, α = 0.89.We entered depression score as a count variable in all analyses.
Posttraumatic Stress.
We assessed posttraumatic stress using the 20-item Posttraumatic Stress Disorder Checklist (PCL-5) (Bovin et al., 2016) that evaluates the 20 DSM-5 symptoms of PTSD across the symptom clusters. Respondents are asked to indicate how much they are bothered by each PTSD symptom over the last month. Example items include “Repeated, disturbing, and unwanted memories of the stressful experience” and “Having strong negative feelings such as fear, horror, anger, guilt, or shame.” Items are scored 0 – 4 on a Likert scale ranging from “Not at all” to “Extremely.” We used the total symptom severity scoring method and scores range from 0 – 80, with higher scores indicating a greater PTSD symptoms. The PCL-5 has been shown to be valid in reliable among military populations (Bovin et al., 2016; Wortmann et al., 2016). The internal consistency reliability for the PCL-5 was high in our sample, α = 0.96. We entered total PCL-5 score as a count variable in all analyses.
Psychological Hardiness.
We assessed psychological hardiness at baseline with the 15-item Dispositional Resiliency Scale (DRS-15) (Bartone, 1999, 2007). This measure includes subscales for commitment, control, and challenge, with responses ranging from “Not true at all” to “Completely true.” Example items include: “Most of my life gets spent doing things that are meaningful” (commitment), “By working hard you can nearly always achieve your goals” (control), and “I enjoy the challenge when I have to do more than one thing at a time” (challenge). The DRS-15 has been shown to have high reliability, Kappa = 0.78 (Bartone, 2007) In our sample, the measure had good internal consistency reliability (α = 0.81). For all analyses, we entered psychological hardiness score as a count variable.
Marital Satisfaction.
We assessed relationship functioning with the Marital Adjustment Test (MAT) (Locke & Wallace, 1959). This 15-item instrument measures overall marital satisfaction and adjustment of husbands and wives to each other and total scores range from 2 – 158. Prior research has shown that the MAT has good internal consistency, α = 0.88 (Funk & Rogge, 2007), which was also true in the current sampleα = 0.79. We used marital satisfaction score as count variable in all analyses.
Deployment Status.
At each wave, participants were asked if they had ever been deployed. Based on the participant response at the 1-year follow-up, we dichotomized deployment status (yes/no) and included as a binary variable in all analyses.
Analytic Approach
We performed all analyses using Stata version 15.0 software (Stata Corporation, College Station, TX). First, we calculated descriptive statistics and used bivariate analyses to test for differences between never-deployed and ever-deployed soldiers. We calculated Pearson correlations to describe the relationships between each of the following observed variables: hazardous drinking, drug use, anger, anxiety, depression, PTSD, psychological hardiness, marital satisfaction, and deployment status. Rhos and p-values are reported. We used an exploratory factor analysis to confirm unidimensionality of a formative latent construct comprised of all nine observed variables. Next, we used a confirmatory factor analysis to verify the structural relationships between the observed variables and the formative latent construct. The model was examined for fit and adjusted as indicated. Standardized factor loadings (λ) and p-values are reported in a path diagram. Lastly, we used Discriminant Function Analysis to determine the extent to which deployment status (never-deployed vs. ever-deployed) can be discriminated by variables representing mental health symptomatology (i.e., anger, anxiety, depression, PTSD), substance use (i.e., hazardous drinking and drug use), and resiliency factors (i.e., psychological hardiness and marital satisfaction). Deployment status was used as the grouping variable and the remaining observed variables were considered as the discriminating or predictor variables. The overall model F-test and classification results are reported.
Results
Examination of Observed Variables on the Basis of Deployment Status
One in seven (14.4%) soldiers met the threshold for hazardous drinking, with an overall mean AUDIT score of 4.2 (SD = 3.6)Current drug use had an overall prevalence of 7.0%. The mean anger score was 17.5 (SD = 6.6), which is higher than the general population mean (Pilkonis et al., 2011)Among the sample, 72.0% reported symptoms consistent with mild or worse anxiety (59.2% mild, 8.4% moderate, 4.2% severe, 0.3% extreme) and 26.2% reported symptoms consistent with mild or worse depression (16.8% mild, 5.9% moderate, 2.7% moderately severe, 0.7% severe). Additionally, 7.7% of the sample met DSM-5 criteria for PTSD. Additional details, including tests for differences in observed variables on the basis of deployment status are presented in Table 1. Correlations among observed variables and selected demographic variables (i.e., sex, age, years of service, family income) are shown in Table 2.
Table 2.
Correlations among Observed Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Hazardous Drinking | 1.00 | ||||||||||||
| 2. Drug Use | 0.21*** | 1.00 | |||||||||||
| 3. Anger | 0.21*** | 0.18*** | 1.00 | ||||||||||
| 4. Anxiety | 0.26*** | 0.21*** | 0.59*** | 1.00 | |||||||||
| 5. Depression | 0.19*** | 0.17*** | 0.57*** | 0.70*** | 1.00 | ||||||||
| 6. PTSD | 0.25*** | 0.22*** | 0.59*** | 0.83*** | 0.76*** | 1.00 | |||||||
| 7. Psychological Hardiness | −0.15** | −0.18*** | −0.44*** | −0.37*** | −0.42*** | −0.35*** | 1.00 | ||||||
| 8. Marital Satisfaction | −0.17** | −0.07 | −0.40*** | −0.18*** | −0.28*** | −0.27*** | 0.28*** | 1.00 | |||||
| 9. Deployment Status | 0.09 | 0.00 | 0.06 | 0.07* | 0.06 | 0.12* | −0.01 | −0.08 | 1.00 | ||||
| 10. Sex | −0.14** | 0.01 | 0.12* | 0.11* | 0.07 | 0.03 | −0.02 | 0.01 | −0.20*** | 1.00 | |||
| 11. Age | −0.02 | −0.05 | −0.06 | −0.01 | −0.02 | 0.06 | 0.03 | 0.01 | 0.38*** | −0.12* | 1.00 | ||
| 12. Years of Service | 0.01 | 0.00 | 0.11* | 0.11* | 0.10 | 0.19*** | −0.04 | −0.02 | 0.54*** | −0.14** | 0.77*** | 1.00 | |
| 13. Family Income | 0.03 | −0.05 | −0.08 | −0.07 | −0.10 | −0.02 | 0.08 | 0.05 | 0.28*** | −0.10 | 0.40*** | 0.35*** | 1.00 |
p < 0.05
p < 0.01
p < 0.001
Identification of Latent Construct and Saliency of Observed Variables
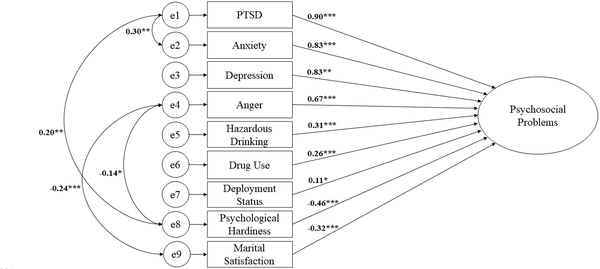
One unique factor emerged from the exploratory factor analysis (eigenvalue = 3.18), which explained 97.6% of the variance in the total scores of the observed variables. In a confirmatory factor analysis, all nine indicator variables significantly loaded onto this single formative latent construct (ps < 0.05), but with varying strength and directionality. Model fit statistics and covariance among error terms indicated that the model could be improved. After adding paths between the error terms for psychological hardiness to anger, marital satisfaction to anger, and psychological hardiness to PTSD, model fit statistics improved (Table 3). In our final model, all observed variables significantly loaded onto a single formative latent construct (Figure 1), which we refer to as “psychosocial problems.” Standardized factor loadings allowed us to rank the variables in order of direction and salience. Measures of mental health and substance use positively loaded onto psychosocial problems: PTSD (λ = 0.90, p < 0.001), anxiety (λ = 0.83, p < 0.001), depression (λ = 0.83, p < 0.01), anger (λ = 0.67, p < 0.001), hazardous drinking (λ = 0.31, p < 0.001), drug use (λ = 0.26, p < 0.001). Deployment status positively loaded onto psychosocial problems, but had the least salience to this latent construct (λ = 0.11, p < 0.05). Measures of resilience negatively loaded onto psychosocial problems: psychological hardiness (λ = −0.46 p < 0.001), marital satisfaction (λ = −0.32, p < 0.001).
Table 3.
Fit Statistics for Confirmatory Factor Analyses
| RMSEA | AIC | BIC | CFI | TLI | SRMR | CD | |
|---|---|---|---|---|---|---|---|
| Model 1 | 0.095 | 17788.709 | 17895.306 | 0.922 | 0.896 | 0.058 | 0.925 |
| Model 2 | 0.061 | 17733.531 | 17855.920 | 0.972 | 0.956 | 0.041 | 0.900 |
Model 1 = Model from Exploratory Factor Analysis
Model 2 = Residual covariance allowed between Marital Satisfaction and Anger, Psychological Hardiness and Anger, and Psychological Hardiness and PTSD
RMSEA = Root Mean Squared Error of Approximation; AIC = Akaike’s Information Criterion; BIC= Bayesian Information Criterion; CFI = Comparative Fit Index; TLI = Tucker -Lewis Index; SRMR = Standardized Root Mean Squared Residual; CD = Coefficient of Determination
Figure 1.
Confirmatory Factor Analysis. This figure displays the standardized factor loadings of each of the observed variables onto the latent construct in order of strength and direction of loading. * p < .05. ** p < .01. *** p < .001.
Power of Observed Variables to Discriminate Between Never- and Ever-Deployed Soldiers
Results from the Discriminant Function Analysis demonstrate that deployment status was not well predicted by observed variables representing mental health symptomatology (i.e., anger, anxiety, depression, PTSD), substance use (i.e., hazardous drinking and drug use), and resiliency factors (i.e., psychological hardiness and marital satisfaction). The overall model F-test was not significant, F(8, 374) = 1.34, p > 0.05. Further, classification results demonstrate poor sensitivity (49.4%) and specificity (72.7%) of the observed variables to correctly predict deployment status (Table 4). The positive predictive value shows that only 73.7% of soldiers who were classified by the Discriminant Function Analysis as having been deployed had actually experienced deployment. Further, the negative predictive value shows that only 48.0% of soldiers who were classified as having never been deployed had never actually experienced deployment.
Table 4.
Classification Results of Discriminant Function Analysis
| Predicted Group
Membership |
||
|---|---|---|
| Original | Never-deployed, % (n) | Ever-deployed, % (n) |
| Never-deployed | 72.7% (109) | 27.3% (41) |
| Ever-deployed | 50.6% (118) | 49.4% (115) |
Discussion
We examined the components of psychosocial problems among never- and ever-deployed USAR/NG soldiers. Interestingly, we found that deployment status was the least salient determinant of psychosocial problems among the observed variables. Previous research has shown that combat exposure had significant effects on psychosocial well-being among service members (Bray & Hourani, 2007; Hassija et al., 2012; Hoopsick, Vest, et al., 2018; Jacobson et al., 2008; Larson et al., 2016; Milliken et al., 2007; Renshaw et al., 2009; Seal et al., 2011; M. M. Thomas et al., 2017; Vest et al., 2017; Vest et al., 2018; Vogt et al., 2011). However, emerging evidence has suggested that never-deployed service members are also at risk for psychosocial issues (Fink et al., 2016; Hoopsick et al., in press; Hoopsick, Homish, et al., 2018; Jacobson et al., 2008; Kang et al., 2015; Russell et al., 2015; Trautmann et al., 2014; Wells et al., 2010; Worthen et al., 2015). The current study expands upon this idea by demonstrating that soldiers who have never been deployed and soldiers who have been deployed are more alike than different across a range of psychosocial factors. Thus, though the severity of combat exposure is important to consider among service members who have been deployed (Bray & Hourani, 2007; Hassija et al., 2012; Hoopsick, Vest, et al., 2018; Jacobson et al., 2008; Larson et al., 2016; Milliken et al., 2007; Renshaw et al., 2009; Seal et al., 2011; M. M. Thomas et al., 2017; Vest et al., 2017; Vogt et al., 2011), deployment status in and of itself is a poor indicator of psychosocial problems among military personnel. To our knowledge, no other studies have demonstrated that deployment status is a poor determinant of psychosocial problems, particularly among USAR/NG soldiers – a high risk group.
Findings from other studies support the notion that deployment is less relevant to psychosocial problems than other factors. For example, research by Worthen and colleagues (Worthen et al., 2014, 2015) demonstrated similar PTSD and anger severity among trauma-exposed service members who had deployed and service members who had never deployed. Further, this study also demonstrated that civilian-related trauma was associated with anger, but deployment-related trauma was not, suggesting that there are significant factors beyond deployment status that are more relevant to military psychosocial well-being (Worthen et al., 2014, 2015). Likewise, additional research among USAR/NG soldiers demonstrated that civilian trauma, but not deployment, was associated with an increased risk of PTSD and depression (Fink et al., 2016).
Our findings demonstrated that PTSD, anxiety, depression, and anger were the most salient factors to psychosocial problems among USAR/NG soldiers. Mental health symptoms are prevalent among both those that have been deployed (Hassija et al., 2012; Heavey et al., 2017; Milliken et al., 2007; Renshaw et al., 2009; M. M. Thomas et al., 2017; Vest et al., 2017; Vogt et al., 2011) and those that have not (Kang et al., 2015; Russell et al., 2015; Trautmann et al., 2014; Vanderploeg et al., 2015; Wells et al., 2010). Some research has shown that service members with worse mental health are less likely to be deployed (Wilson et al., 2009). However, not deploying is also thought to have negative effects on the mental health of never-deployed USAR/NG soldiers (Hoopsick et al., in press; Hoopsick, Homish, et al., 2018). Regardless of what contributes to poor mental health among never-deployed soldiers, our findings showed that mental health factors were the most salient to psychosocial problems among USAR/NG soldiers as a whole.
Next in order of salience to psychosocial problems were hazardous drinking and drug use. Although active duty and Reserve/Guard service members hold similar roles and have similar combat experiences, research has shown that Reserve/Guard service members have a greater risk of alcohol misuse (Cohen et al., 2015; Jacobson et al., 2008). These differences may be due in part to reduced unit support because of limited time spent with units (Griffith, 2010, 2015), as well as civilian employment (Griffith, 2011) and family financial stressors (Riviere et al., 2011). Limited evidence has shown that the prevalence of substance use and substance use disorders did not differ between recently deployed and never-deployed service members (Trautmann et al., 2014). Consistent with this finding, our research demonstrated that substance use contributed to psychosocial problems among both ever- and never-deployed USAR/NG soldiers.
We also found that psychological hardiness and marital satisfaction negatively loaded onto our latent construct. This suggested that these factors were salient to promoting resiliency against psychosocial problems. Research has shown that psychological hardiness protects against problems with alcohol (Bartone et al., 2015; Bartone et al., 2012; Green et al., 2014) and mental health (Bartone, 1999). Similarly, good marital functioning has also been shown to be a resiliency factor among USAR/NG soldiers (Vest et al., 2017; Vest et al., 2018). Consistent with these findings, our research demonstrated that these resiliency factors positively contributed to the psychosocial well-being. These factors represent potential points of intervention.
Methodological Considerations and Clinical Implications
Our findings have implications for the effective care of service members. Given the general assumption that deployment status is the critical determinant of psychosocial problems, more salient factors may be less likely to be addressed through intervention efforts. Further, Reserve/Guard soldiers who have never been deployed do not meet eligibility criteria for health benefits under the U.S. Department of Veterans Affairs upon separation from the military (Veterans Benefits Administration, 2012). Given that these never-deployed service members would need to seek care outside of the military, it is important to note that less than half of community mental health providers regularly screen for both military status and psychosocial stressors related to military life (Tanielian et al., 2014). Moreover, curricula to advance this competence tends to emphasize only the effects of combat deployment (Elliott & Patterson, 2017). Our findings demonstrate that mental health and substance use are much more salient to psychosocial problems than deployment status, and that ever- and never-deployed USAR/NG soldiers are both at risk for difficulties with mental health and substance use. Additionally, psychological hardiness and marital satisfaction represent strength-based approaches for interventions to promote psychosocial well-being among USAR/NG soldiers as a whole.
This study possessed several notable strengths. The use of Factor Analyses and Discriminant Function Analysis allowed us to demonstrate that there were a range of factors more salient to psychosocial problems among USAR/NG soldiers than deployment status, which has long been the focus of military-centered assessments and interventions. The inclusion of psychological hardiness and marital satisfaction also allowed us to examine for factors that promote psychosocial well-being. This research made a significant contribution to our understanding of two understudied, but high-risk populations: USAR/NG and never-deployed service members. Additionally, through the collection of data on sensitive topics such as mental health, substance use, and marital satisfaction via confidential surveys using validated tools, we were able to accurately estimate and compare the prevalence of psychosocial problems between never-deployed and ever-deployed soldiers.
The findings of this study can be interpreted within the context of its limitations. First, as with any survey-based study, there is a potential for response bias. However, given the wide range of responses collected using validated tools and the use of a confidential survey, social desirability is unlikely. Second, all data in this report are cross-sectional, so the temporal relationships between deployment and changes in psychosocial problems were not examined. Nonetheless, applications of structural equation modeling using a cross-sectional design are common in the field of psychology (MacCallum & Austin, 2000). An additional limitation is that all participants were either married or living as married at study enrollment, which may limit generalizability. However, data show that the majority of U.S. service members are married (Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy, 2015). Generalizability may also be limited by the inclusion of only service members from New York. Further, it is not known if these findings can be generalized to reservists from other branches of the military. However, our overall sample is consistent with the demographic and military characteristics (i.e., rank enlisted vs. officer) of Reserve and Guard soldiers nationally (Office of the Deputy Assistant Secretary of Defense, 2016). Lastly, we did not examine for differences between never-deployed soldiers who were in units that did not deploy and never-deployed soldiers who did not deploy when their unit deployed. Additional research is needed to further explore these nuances and to examine the role of deployment status in the development of psychosocial issues among other military populations.
Findings from this study demonstrated that many factors were significant to the development of psychosocial problems. However, deployment status had the least relevance. Given that a substantial proportion of Reserve/Guard soldiers may never deploy (“Counts of Active Duty and Reserve Service Members and APF Civilians Location Country Report,” 2016) and that non-deployment results in negative emotions related to having never been deployed (Hoopsick et al., in press; Hoopsick, Homish, et al., 2018), our findings underscore the need for systematic screening for mental illness and substance use in military populations, regardless of deployment status. Furthermore, psychological hardiness and marital satisfaction may be protective against psychosocial problems for both never- and ever-deployed soldiers. Intervention efforts targeted only for soldiers who have been deployed will miss opportunities to intervene on never-deployed soldiers who represent on an equally affected and high-risk group.
Funding and Disclosure:
Research reported in this manuscript was supported by the National Institute on Drug Abuse award number R01DA034072 to Gregory G. Homish and by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR001412 to the University at Buffalo. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The authors have no conflicts of interest to declare.
REFERENCES
- Allen JP, Litten RZ, Fertig JB, & Babor T (1997). A review of research on the Alcohol Use Disorders Identification Test (AUDIT). Alcohol Clin Exp Res, 21(4), 613–619. [PubMed] [Google Scholar]
- Bartone PT (1999). Hardiness protects against war-related stress in Army Reserve forces. Consulting Psychology Journal: Practice and Research, 51(2), 72. [Google Scholar]
- Bartone PT (2007). Test-retest reliability of the dispositional resilience scale-15, a brief hardiness scale. Psychol Rep, 101(3 Pt 1), 943–944. doi: 10.2466/pr0.101.3.943-944 [DOI] [PubMed] [Google Scholar]
- Bartone PT, Eid J, Hystad SW, Jocoy K, Laberg JC, & Johnsen BH (2015). Psychological Hardiness and Avoidance Coping Are Related to Risky Alcohol Use in Returning Combat Veterans. Military Behavioral Health, 3(4), 274–282. [Google Scholar]
- Bartone PT, Hystad SW, Eid J, & Brevik JI (2012). Psychological hardiness and coping style as risk/resilience factors for alcohol abuse. Mil Med, 177(5), 517–524. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric Properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in Veterans. Psychol Assess, 28(11), 1379–1391. doi: 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Bray RM, Brown JM, & Williams J (2013). Trends in binge and heavy drinking, alcohol-related problems, and combat exposure in the U.S. military. Substance Use & Misuse, 48(10), 799–810. doi: 10.3109/10826084.2013.796990 [DOI] [PubMed] [Google Scholar]
- Bray RM, & Hourani LL (2007). Substance use trends among active duty military personnel: findings from the United States Department of Defense Health Related Behavior Surveys, 1980–2005. Addiction, 102(7), 1092–1101. doi: 10.1111/j.1360-0443.2007.01841.x [DOI] [PubMed] [Google Scholar]
- Cohen GH, Fink DS, Sampson L, & Galea S (2015). Mental health among reserve component military service members and veterans. Epidemiol Rev, 37, 7–22. doi: 10.1093/epirev/mxu007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Counts of Active Duty and Reserve Service Members and APF Civilians Location Country Report. (2016). Retrieved from https://www.dmdc.osd.mil/appj/dwp/rest/download?fileName=DMDC_Website_Location_Report_1612.xlsx&groupName=milRegionCountry
- Craske M, Wittchen U, Bogels S, Stein M, Andrews G, & Lebeu R (2013). Severity Measure for Generalized Anxiety Disorder - Adult. In American Psychiatric Association (Ed.), Diagnostic and Stastical Manual V (5th ed. ed.). Arlington, VA: American Psychiatric Publishing. [Google Scholar]
- Defense Manpower Data Center. (2017). Counts of Active Duty and Reserve Service Members and APF Civilians. Retrieved from https://www.dmdc.osd.mil/appj/dwp/rest/download?fileName=DMDC_Website_Location_Report_1612.xlsx&groupName=milRegionCountry
- Eisen SA, Griffith KH, Xian H, Scherrer JF, Fischer ID, Chantarujikapong S, . . . Tsuang MT (2004). Lifetime and 12-month prevalence of psychiatric disorders in 8,169 male Vietnam War era veterans. Mil Med, 169(11), 896–902. [DOI] [PubMed] [Google Scholar]
- Elliott B, & Patterson B (2017). Joining Forces: The Status of Military and Veteran Health Care in Nursing Curricula. J Prof Nurs, 33(2), 145–152. doi: 10.1016/j.profnurs.2016.06.006 [DOI] [PubMed] [Google Scholar]
- Fink DS, Cohen GH, Sampson LA, Gifford RK, Fullerton CS, Ursano RJ, & Galea S (2016). Incidence of and risk for post-traumatic stress disorder and depression in a representative sample of US Reserve and National Guard. Ann Epidemiol. doi: 10.1016/j.annepidem.2016.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk JL, & Rogge RD (2007). Testing the ruler with item response theory: increasing precision of measurement for relationship satisfaction with the Couples Satisfaction Index. J Fam Psychol, 21(4), 572–583. doi: 10.1037/0893-3200.21.4.572 [DOI] [PubMed] [Google Scholar]
- Gibbons SW, Barnett SD, & Hickling EJ (2012). Family stress and posttraumatic stress: the impact of military operations on military health care providers. Arch Psychiatr Nurs, 26(4), e31–39. doi: 10.1016/j.apnu.2012.04.001 [DOI] [PubMed] [Google Scholar]
- Green KT, Beckham JC, Youssef N, & Elbogen EB (2014). Alcohol misuse and psychological resilience among U.S. Iraq and Afghanistan era veterans. Addictive Behaviors, 39(2), 406–413. doi: 10.1016/j.addbeh.2013.08.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith J (2010). Citizens Coping as Soldiers: A Review of Deployment Stress Symptoms Among Reservists. Military Psychology, 22(2), 176–206. doi: 10.1080/08995601003638967 [DOI] [Google Scholar]
- Griffith J (2011). Decades of transition for the US reserves: Changing demands on reserve identity and mental well-being. International Review of Psychiatry, 23(2), 181–191. doi:Doi 10.3109/09540261.2010.541904 [DOI] [PubMed] [Google Scholar]
- Griffith J (2015). Homecoming of soldiers who are citizens: Re-employment and financial status of returning Army National Guard soldiers from Operations Iraqi Freedom (OIF) and Enduring Freedom (OEF). Work-a Journal of Prevention Assessment & Rehabilitation, 50(1), 85–96. doi: 10.3233/wor-131794 [DOI] [PubMed] [Google Scholar]
- Hassija CM, Jakupcak M, Maguen S, & Shipherd JC (2012). The influence of combat and interpersonal trauma on PTSD, depression, and alcohol misuse in U.S. Gulf War and OEF/OIF women veterans. Journal of Traumatic Stress, 25(2), 216–219. doi: 10.1002/jts.21686 [DOI] [PubMed] [Google Scholar]
- Heavey SC, Homish DL, Goodell EA, & Homish GG (2017). U.S. reserve soldiers’ combat exposure and intimate partner violence: Not more common but it is more violent. Stress Health, 33(5), 617–623. doi: 10.1002/smi.2748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge CW, Auchterlonie JL, & Milliken CS (2006). Mental Health Problems, Use of Mental Health Services, and Attrition From Military Service After Returning From Deployment to Iraq or Afghanistan. JAMA, 295(9), 1023–1032. doi: 10.1001/jama.295.9.1023 [DOI] [PubMed] [Google Scholar]
- Hoopsick RA, Fillo J, Vest BM, Homish DL, & Homish GG (2017). Substance use and dependence among current reserve and former military members: Cross-sectional findings from the National Survey on Drug Use and Health, 2010–2014. J Addict Dis, 36(4), 243–251. doi: 10.1080/10550887.2017.1366735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoopsick RA, Homish DL, Bartone PT, & Homish GG (in press). Developing a measure to assess emotions associated with never being deployed. Military Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoopsick RA, Homish DL, Vest BM, & Homish GG (2018). Alcohol use among never-deployed U.S. Army Reserve and National Guard soldiers: The effects of non-deployment emotions and sex. Alcoholism: Clinical & Experimental Research, 42(12), 2413–2422. doi: 10.1111/acer.13901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoopsick RA, Vest BM, Homish DL, & Homish GG (2018). Combat exposure, emotional and physical role limitations, and substance use among male United States Army Reserve and National Guard soldiers. Quality of life research, 27(1), 137–147. doi: 10.1007/s11136-017-1706-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hotopf M, Hull L, T Fear N, Browne T, Horn O, Iversen A, . . . Wessely S (2006). The health of UK military personnel who deployed to the 2003 Iraq war: a cohort study. Lancet, 367(9524), 1731–1741. doi: 10.1016/s0140-6736(06)68662-5 [DOI] [PubMed] [Google Scholar]
- Humeniuk R, Ali R, Babor TF, Farrell M, Formigoni ML, Jittiwutikarn J, . . . Simon S (2008). Validation of the Alcohol, Smoking And Substance Involvement Screening Test (ASSIST). Addiction, 103(6), 1039–1047. doi: 10.1111/j.1360-0443.2007.02114.x [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. (2015). Psychosocial Interventions for Mental and Substance Use Disorders: A Framework for Establishing Evidence-Based Standards. Retrieved from Washington, D.C.: [PubMed] [Google Scholar]
- Ireland RR, Kress AM, & Frost LZ (2012). Association between mental health conditions diagnosed during initial eligibility for military health care benefits and subsequent deployment, attrition, and death by suicide among active duty service members. Mil Med, 177(10), 1149–1156. [DOI] [PubMed] [Google Scholar]
- Jacobson IG, Ryan MA, Hooper TI, Smith TC, Amoroso PJ, Boyko EJ, . . . Bell NS (2008). Alcohol use and alcohol-related problems before and after military combat deployment. JAMA: Journal of the American Medical Association, 300(6), 663–675. doi: 10.1001/jama.300.6.663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang HK, Bullman TA, Smolenski DJ, Skopp NA, Gahm GA, & Reger MA (2015). Suicide risk among 1.3 million veterans who were on active duty during the Iraq and Afghanistan wars. Annals of Epidemiology, 25(2), 96–100. doi: 10.1016/j.annepidem.2014.11.020 [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer R, & Williams JW (2001). The PHQ-9. Journal of General Internal Medicine, 16(9), 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, & Mokdad AH (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. doi: 10.1016/j.jad.2008.06.026 [DOI] [PubMed] [Google Scholar]
- Larson MJ, Mohr BA, Jeffery DD, Adams RS, & Williams TV (2016). Predictors of Positive Illicit Drug Tests After OEF/OIF Deployment Among Army Enlisted Service Members. Mil Med, 181(4), 334–342. doi: 10.7205/milmed-d-15-00110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebeau RT, Glenn DE, Hanover LN, Beesdo-Baum K, Wittchen HU, & Craske MG (2012). A dimensional approach to measuring anxiety for DSM-5. Int J Methods Psychiatr Res, 21(4), 258–272. doi: 10.1002/mpr.1369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Locke HJ, & Wallace KM (1959). Short marital-adjustment and prediction tests: Their reliability and validity. Marriage and family living, 21(3), 251–255. [Google Scholar]
- MacCallum RC, & Austin JT (2000). Applications of structural equation modeling in psychological research. Annu Rev Psychol, 51, 201–226. doi: 10.1146/annurev.psych.51.1.201 [DOI] [PubMed] [Google Scholar]
- Milliken CS, Auchterlonie JL, & Hoge CW (2007). Longitudinal Assessment of Mental Health Problems Among Active and Reserve Component Soldiers Returning From the Iraq War. JAMA: Journal of the American Medical Association, 298(18), 2141–2148. doi: 10.1001/jama.298.18.2141 [DOI] [PubMed] [Google Scholar]
- Moehring A, Krause K, Guertler D, Bischof G, Hapke U, Freyer-Adam J, . . . Meyer C (2018). Measurement invariance of the alcohol use disorders identification test: Establishing its factor structure in different settings and across gender. Drug Alcohol Depend, 189, 55–61. doi: 10.1016/j.drugalcdep.2018.05.002 [DOI] [PubMed] [Google Scholar]
- Office of the Deputy Assistant Secretary of Defense. (2016). 2016 Demographics Profile of the Military Community. Department of Defense. [Google Scholar]
- Office of the Deputy Assistant Secretary of Defense for Military Community and Family Policy. (2015). 2015 Demographics Profile of the Military Community. Department of Defense; Retrieved from http://download.militaryonesource.mil/12038/MOS/Reports/2015-Demographics-Report.pdf. [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, & Cella D (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment, 18(3), 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renshaw KD (2010). Deployment experiences and postdeployment PTSD symptoms in National Guard/Reserve service members serving in operations Enduring Freedom and Iraqi Freedom. Journal of Traumatic Stress, 23(6), 815–818. doi: 10.1002/jts.20575 [DOI] [PubMed] [Google Scholar]
- Renshaw KD, Rodrigues CS, & Jones DH (2009). Combat exposure, psychological symptoms, and marital satisfaction in National Guard soldiers who served in Operation Iraqi Freedom from 2005 to 2006. Anxiety Stress and Coping, 22(1), 101–115. doi: 10.1080/10615800802354000 [DOI] [PubMed] [Google Scholar]
- Riviere LA, Kendall-Robbins A, McGurk D, Castro CA, & Hoge CW (2011). Coming home may hurt: risk factors for mental ill health in US reservists after deployment in Iraq. British Journal of Psychiatry, 198(2), 136–142. doi:DOI 10.1192/bjp.bp.110.084863 [DOI] [PubMed] [Google Scholar]
- Rundell JR (2006). Demographics of and diagnoses in Operation Enduring Freedom and Operation Iraqi Freedom personnel who were psychiatrically evacuated from the theater of operations. Gen Hosp Psychiatry, 28(4), 352–356. doi: 10.1016/j.genhosppsych.2006.04.006 [DOI] [PubMed] [Google Scholar]
- Russell DW, Cohen GH, Gifford R, Fullerton CS, Ursano RJ, & Galea S (2015). Mental health among a nationally representative sample of United States Military Reserve Component Personnel. Soc Psychiatry Psychiatr Epidemiol, 50(4), 639–651. doi: 10.1007/s00127-014-0981-2 [DOI] [PubMed] [Google Scholar]
- Saunders J, Aasland O, Babor T, de la Fuente J, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption-II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, & Ren L (2011). Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug & Alcohol Dependence, 116(1–3), 93–101. [DOI] [PubMed] [Google Scholar]
- Stone AA, Broderick JE, Junghaenel DU, Schneider S, & Schwartz JE (2016). PROMIS fatigue, pain intensity, pain interference, pain behavior, physical function, depression, anxiety, and anger scales demonstrate ecological validity. J Clin Epidemiol, 74, 194–206. doi: 10.1016/j.jclinepi.2015.08.029 [DOI] [PubMed] [Google Scholar]
- Tanielian T, Farris C, Batka C, Farmer C, Robinson E, Engel C, . . . LH J (2014). Ready to Serve: Community-Based Provider Capacity to Deliver Culturally Competent, Quality Mental Health Care to Veterans and Their Families. Retrieved from Santa Monica, CA: https://www.rand.org/pubs/research_reports/RR806.html [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, & Hoge CW (2010). Prevalence of Mental Health Problems and Functional Impairment Among Active Component and National Guard Soldiers 3 and 12 Months Following Combat in Iraq. Archives of General Psychiatry, 67(6), 614–623. [DOI] [PubMed] [Google Scholar]
- Thomas MM, Harpaz-Rotem I, Tsai J, Southwick SM, & Pietrzak RH (2017). Mental and Physical Health Conditions in US Combat Veterans: Results From the National Health and Resilience in Veterans Study. Prim Care Companion CNS Disord, 19(3). doi: 10.4088/PCC.17m02118 [DOI] [PubMed] [Google Scholar]
- Trautmann S, Schonfeld S, Behrendt S, Hofler M, Zimmermann P, & Wittchen HU (2014). Substance use and substance use disorders in recently deployed and never deployed soldiers. Drug Alcohol Depend, 134, 128–135. doi: 10.1016/j.drugalcdep.2013.09.024 [DOI] [PubMed] [Google Scholar]
- Vanderploeg RD, Nazem S, Brenner LA, Belanger HG, Donnell AJ, & Scott SG (2015). Suicidal Ideation among Florida National Guard Members: Combat Deployment and Non-Deployment Risk and Protective Factors. Arch Suicide Res, 19(4), 453–471. doi: 10.1080/13811118.2014.957454 [DOI] [PubMed] [Google Scholar]
- Vasterling JJ, Proctor SP, Friedman MJ, Hoge CW, Heeren T, King LA, & King DW (2010). PTSD symptom increases in Iraq-deployed soldiers: comparison with nondeployed soldiers and associations with baseline symptoms, deployment experiences, and postdeployment stress. Journal of Traumatic Stress, 23(1), 41–51. doi: 10.1002/jts.20487 [DOI] [PubMed] [Google Scholar]
- Vest BM, Heavey SC, Homish DL, & Homish GG (2017). Marital Satisfaction, Family Support, and Pre-Deployment Resiliency Factors Related to Mental Health Outcomes for Reserve and National Guard Soldiers. Military Behavioral Health, 5(4), 313–323. doi: 10.1080/21635781.2017.1343694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vest BM, Homish DL, Hoopsick RA, & Homish GG (2018). What drives the relationship between combat and alcohol problems in soldiers? The roles of perception and marriage. Soc Psychiatry Psychiatr Epidemiol, 53(4), 413–420. doi: 10.1007/s00127-017-1477-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veterans Benefits Administration. (2012). Summary of VA benefits for National Guard and reserve members and veterans. U.S. Department of Veterans Affairs; Retrieved from http://www.benefits.va.gov/benefits/benefits-summary/summaryofvanationalguardandreserve.pdf. [Google Scholar]
- Vogt D, Smith B, Elwy R, Martin J, Schultz M, Drainoni M-L, & Eisen S (2011). Predeployment, deployment, and postdeployment risk factors for posttraumatic stress symptomatology in female and male OEF/OIF veterans. Journal of Abnormal Psychology, 120(4), 819–831. doi: 10.1037/a0024457 [DOI] [PubMed] [Google Scholar]
- Wells TS, LeardMann CA, Fortuna SO, Smith B, Smith TC, Ryan MA, . . . Blazer D (2010). A prospective study of depression following combat deployment in support of the wars in Iraq and Afghanistan. Am J Public Health, 100(1), 90–99. doi: 10.2105/ajph.2008.155432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO Assist Working Group. (2002). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction, 97(9), 1183–1194. doi: 10.1046/j.1360-0443.2002.00185.x [DOI] [PubMed] [Google Scholar]
- Wilson J, Jones M, Fear NT, Hull L, Hotopf M, Wessely S, & Rona RJ (2009). Is previous psychological health associated with the likelihood of Iraq War deployment? An investigation of the “healthy warrior effect”. Am J Epidemiol, 169(11), 1362–1369. doi: 10.1093/aje/kwp044 [DOI] [PubMed] [Google Scholar]
- Worthen M, Rathod SD, Cohen G, Sampson L, Ursano R, Gifford R, . . . Ahern J (2014). Anger problems and posttraumatic stress disorder in male and female National Guard and Reserve Service members. Journal of Psychiatric Research, 55, 52–58. doi: 10.1016/j.jpsychires.2014.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worthen M, Rathod SD, Cohen G, Sampson L, Ursano R, Gifford R, . . . Ahern J (2015). Anger and Posttraumatic Stress Disorder Symptom Severity in a Trauma-Exposed Military Population: Differences by Trauma Context and Gender. Journal of Traumatic Stress, 28(6), 539–546. doi: 10.1002/jts.22050 [DOI] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, . . . Litz BT (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess, 28(11), 1392–1403. doi: 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]
- Wright KM, Foran HM, Wood MD, Eckford RD, & McGurk D (2012). Alcohol problems, aggression, and other externalizing behaviors after return from deployment: understanding the role of combat exposure, internalizing symptoms, and social environment. Journal of Clinical Psychology, 68(7), 782–800. doi: 10.1002/jclp.21864 [DOI] [PubMed] [Google Scholar]