Introduction
Asthma affects an estimated 7 million children (nearly 1 in 10) in the United States.1 Children (particularly African-Americans and Hispanics), are disproportionately affected by acute exacerbations, emergency department (ED) visits, and hospitalizations.1–4 Pediatric asthma accounts for over 600,000 ED visits, 150,000 hospitalizations, and $50 billion in healthcare costs annually.1,2,5
Previous studies have examined pediatric asthma’s epidemiology and best practices for treatment in the ED setting.3,6 Evidence-based guidelines for ED treatment have been promulgated, recommending administration of first-line short-acting inhaled beta-agonists (albuterol), inhaled ipratropium bromide, and systemic corticosteroids.7–9 Importantly, studies show that the benefits of systemic corticosteroids are time-sensitive, with earlier administration in the ED conferring decreases in hospital admission, ED length-of-stay (LOS), and relapse rates.10–12
Approximately 10% of all pediatric ED patients utilize emergency medical services (EMS) for prehospital management and transport.13,14 A national study of pediatric EMS encounters found that albuterol was the most frequently administered medication, yet did not offer further detail on pediatric EMS encounters for asthma or respiratory distress.15 No other current study has examined the epidemiology and treatment of pediatric asthma by EMS.16 To fill that gap, this study set out to describe the relevant demographic, clinical, and geographic characteristics of pediatric asthma patients treated by EMS in the state with the fourth-largest pediatric population to examine current EMS treatment practices.17
Materials & Methods
Study Design & Setting
This was a retrospective observational study of children treated and transported by EMS for an asthma exacerbation in the state of Florida from 2011–2016. Patients were identified from Florida’s EMS Tracking and Reporting System (EMSTARS) database, which contains EMS encounters from over 100 EMS agencies in a state with a population near 21 million, 20% of whom are under 18 years of age.18, 19 EMSTARS contains 74% of all 911 EMS encounters from 2011–2016.19 Both the University of Florida and Florida Department of Health Institutional Review Boards approved the study with waiver of informed consent.
Inclusion & Exclusion Criteria
Inclusion criteria were patients ages 2 to 18 years, transported by EMS to an ED, with a primary symptom of difficulty breathing, an EMS provider primary impression of respiratory distress, and who were administered inhaled albuterol by EMS at least once (to indicate an acute exacerbation). EMSTARS does not contain an asthma-specific diagnosis, therefore we chose to combine respiratory distress with administration of albuterol for the inclusion criteria. Patients were excluded if they were classified as a trauma/injury, seizure, pregnancy-related complication, or interfacility transport. Patients less than 2 years of age were excluded to avoid confounding with wheezing due to bronchiolitis. To test the albuterol administration inclusion criteria, we performed a sensitivity analysis examining characteristics of all EMSTARS patients ages 2–18 with an EMS provider primary impression of respiratory distress.
Data Variables
For vital signs, the first available recorded observation per vital sign was used (as many EMS treatment decisions are made based on the first assessed value).20 EMS scene time was calculated as the interval between EMS arrival on scene and when EMS left the scene. EMS transport time was calculated as the interval between EMS leaving the scene and arriving at the destination ED. A priori, the investigators considered any scene or transport times of negative, zero, or less than three minutes as potentially miscoded, and so time intervals less than three minutes were excluded from the analysis (<2% of values).
Patients were classified by severity (mild, moderate, severe, and critical) using the 2007 National Heart, Lung, and Blood Institute’s (NHLBI) Expert Panel Report-3’s recommended classification for asthma exacerbation severity.7 Not all components of the NHLBI’s scoring system were available in the EMSTARS database, therefore a modified version was created. In this modification, the variables “breathlessness,” “talks in,” “use of accessory muscles/suprasternal retractions,” and “wheeze” were substituted with EMSTARS’ “respiratory effort” (a graded scale with values: normal, increased, fatigued, and absent). Alertness, heart rate, respiratory rate, and oxygen saturation were used per the original scoring system with age-adjusted normal values for heart rate and respiratory rate.21 Pulsus paradoxus, peak expiratory flow, and arterial oxygen pressure are NHLBI score components, but are not usually measured by EMS and not available in EMSTARS, so those were removed from the modified version. Patients’ overall severity score comprised the highest value from each component of the modified classification (Table 1).
Table 1:
Modified-NHLBI Asthma Severity Classification*
| Mild | Moderate | Severe | Critical | |
|---|---|---|---|---|
| Level of Alertness | Alert | Verbal | Painful | Unresponsive |
| Respiratory Effort | Normal | Labored | Fatigued | Absent |
| Respiratory Rate (breaths per minute) |
||||
| 2-5 years | 10-29 | 30-40 | >40 | <10 |
| 6-11 years | 10-24 | 25-35 | >35 | <10 |
| 12-18 years | 10-19 | 20-30 | >30 | >10 |
| Pulse Rate (beats per minute) |
||||
| 2-5 years | 100-119 | 120-140 | >140 | <100 |
| 6-11 years | 60-109 | 110-130 | >130 | <60 |
| 12-18 years | 60-99 | 100-120 | >120 | <60 |
| Pulse Oximetry | > 95% | 90-95% | 80-89% | <80% |
Data Analysis
Demographic, clinical, and EMS characteristic variables were analyzed using descriptive statistics, including frequencies, percentages, mean, standard deviation, median, and interquartile ranges, as appropriate. Continuous variables were compared using unpaired t-test and Kruskal-Wallis tests, as appropriate. Categorical variables were compared using the Chi-Square test, or Fisher Exact Test when there were less than 10 observations (as a conservative approach).23 Whether variables were normally distributed was tested using the Shapiro-Wilk test, or the Kolmogorov-Smirnov test for sample sizes greater than 2,000.24 Missing data was excluded from the analysis given that EMSTARS comprises data from multiple heterogeneous EMS agencies, which precluded reliable interpretation of whether data was missing at random.
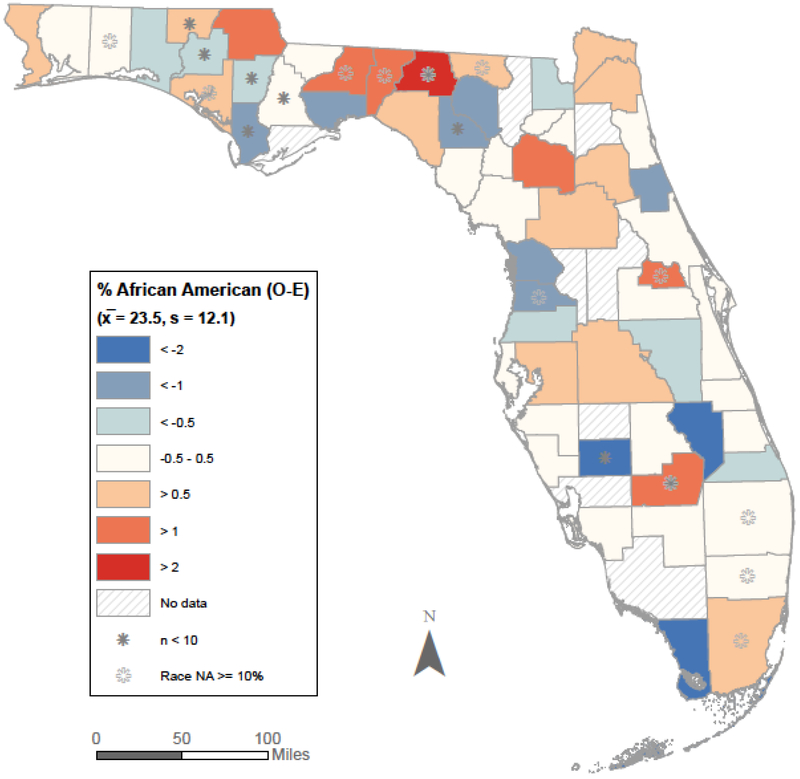
Given the known disparate impact of pediatric asthma on African-American children,3, 4 we chose to focus our geographic analysis on population-based disparities. Geospatial analysis classified patients by the county in which the responding EMS agency was based (as recorded in EMSTARS). Study population disparities were analyzed by calculating the difference between expected and observed frequencies of patient events by demographic variables such as race. Missing or unknown demographic variables were excluded from the analysis. Observed frequencies were taken from EMSTARS, and expected frequencies were based on the 2010 United States Census data on race and percentage of population under 18 years of age.22 Population disparities by county were then calculated using z-scores for the difference between observed and expected frequencies.
Since ED-based research and guidelines recommend early administration of systemic corticosteroids for pediatric asthma exacerbations,7–12 we analyzed characteristics for patients who did and did not receive systemic corticosteroids from EMS. First, univariate logistic regression was employed to screen all variables for their association with EMS systemic corticosteroid administration. Afterwards we performed a Bonferroni correction for multiple comparisons. A p value of < 0.20 was the threshold for candidate variables in the multivariable modeling process. A parsimonious multivariable logistic regression model was created using Akaike’s Information Criterion (AIC), area-under-the-curve (AUC), the Hosmer and Lemeshow Goodness-of-Fit test, and total number of variables as discrimination and calibration measures (Supplemental Digital Content 1). The final model’s significant predictors are presented with odds ratios (OR) and their corresponding 95% confidence intervals (CI). Statistical analysis was performed using SAS® version 9.4 (Cary, NC). Geospatial analysis was performed using ArcGIS Desktop 10.4.1 (Redlands, CA).
Results
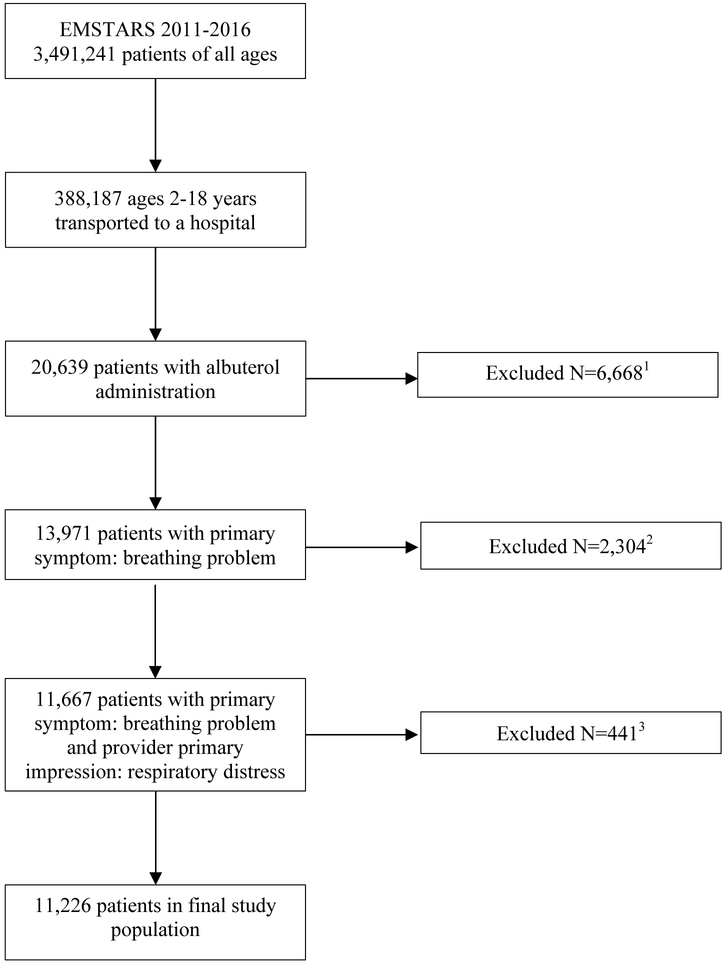
A total of 11,226 patients met the inclusion criteria from 2011–2016 (Figure 1). Demographic, clinical, and EMS characteristics are presented for the entire study population (Table 2). Notably, 49% of patients were African-American, and 60% were male. Most were treated by a Paramedic-level Emergency Medical Technician (EMT) (85%) and were transported from a home or residence (54%). Of note, parent or patient choice was the most frequent reason for choosing the destination facility (44%), as compared to the closest facility (41%). Using the modified-NHLBI severity classification, most patients scored moderate (43%), followed by severe (39%), mild (12.6%), then critical (3.2%). In addition to albuterol, 36.5% of patients received at least one administration of ipratropium bromide, 20.5% received supplemental oxygen, and <1% received magnesium sulfate. With regards to systemic corticosteroids, 1,036 (9.3%) received intravenous (IV) methylprednisolone and only 12 (<1%) of patients received dexamethasone (IV or oral). No other systemic corticosteroids (IV, intramuscular, or oral) were administered in the study sample. The three most frequent procedures performed were IV access in an extremity (12.4%), cardiac monitoring (11.3%), and electrocardiogram (9.7%). Less than one percent of patients required bag-valve mask ventilation, continuous positive airway pressure, or intubation. Missing data are varied greatly by variable (Table 2).
Figure 1: Study Inclusion and Exclusion Criteria.
1Excluded primary symptoms (N): Bleeding (25), change in responsiveness (199), choking (15), death (1), device/equipment problem (1), diarrhea (2), drainage/discharge (4), fever (177), malaise (94), mass/lesion (1), mental/psych (44), nausea/vomiting (4), not known or missing (5,556), pain (137), palpitations (1), rash/itching (201), swelling (80), transport only (43), weakness (46), wound (1)
2Excluded primary impressions: Behavioral / psychiatric disorder (28), diabetic symptoms (1), cardiac arrest (5), airway obstruction (90), vaginal hemorrhage (1), altered level of consciousness (21), syncope/fainting (5), seizure (14), hyperthermia (12), hypothermia (1), chest pain (30), abdominal pain (42), respiratory arrest (28), sexual assault/rape (1), traumatic injury (11) poisoning/drug ingestion (1), inhalational injury (7), stings/venomous bites (1), allergic reaction (493), fever (50), general malaise (97), heart-related illness (12), intentional drug use (1), not known or missing (1423), other non-traumatic pain (541), sepsis (4)
3Childbirth (3), seizure (38), interfacility transfer (160) or trauma (240) as indicated by other EMS procedure or classification codes
Table 2:
Characteristics of EMS pediatric asthma patients in Florida from 2011-2016 overall, and by those who did and did not receive systemic corticosteroids
| Total N=11,226 |
Missing N (%) |
Systemic Corticosteroids1 N=1,036 |
No Systemic Corticosteroids N=10,190 |
P Value* | |
|---|---|---|---|---|---|
| Patient Demographics, N (%) | |||||
| Age years (Median, IQR) | 9 (5-13) | 0 (0%) | 12.5 (8-16) | 8 (5-13) | <0.001* |
| Male Gender | 6726 (60%) | 2 (<1%) | 586 (56.5%) | 6140 (60%) | 0.02* |
| Race | 832 (7.4%) | 0.07 | |||
| African-American or Black | 5491 (49.0%) | 487 (47.0%) | 5004 (49.1%) | ||
| White | 3325 (30.0%) | 334 (32.2%) | 2991 (29.4%) | ||
| Other | 1377 (12.3%) | 177 (17.0%) | 2802 (27.5%) | ||
| Ethnicity | 1923 (17.1%) | 0.17 | |||
| Non-Hispanic or Latino | 7847 (70.0%) | 816 (78.8%) | 7031 (69.0%) | ||
| Hispanic or Latino | 1456 (13.0%) | 169 (16.3%) | 1287 (12.6%) | ||
| EMS Characteristics, N (%) | |||||
| EMS Encounter Year | 0 (0%) | 0.003* | |||
| 2011 | 1782 (15.8%) | 147 (8.0%) | 1635 (16.0%) | ||
| 2012 | 1944 (17.3%) | 185 (9.5%) | 1759 (17.3%) | ||
| 2013 | 2070 (18.4%) | 152 (7.3%) | 1918 (18.9%) | ||
| 2014 | 1981 (17.6%) | 205 (10.0%) | 1776 (17.4%) | ||
| 2015 | 1935 (17.2%) | 186 (9.6%) | 1749 (17.2%) | ||
| 2016 | 1514 (13.4%) | 161 (10.6%) | 1353 (13.3%) | ||
| EMS Level of Service | 0 (%) | <0.001* | |||
| EMT-Paramedic | 9555 (85%) | 938 (90.5%) | 8617 (84.6%) | ||
| EMT-Basic | 2 (<1%) | 0 (0%) | 2 (<1%) | ||
| Other2 | 1669 (14.9%) | 98 (<1%) | 1571 (15.4%) | ||
| Response Mode to Scene | 0 (0%) | 0.07 | |||
| Lights and Sirens | 10,445 (93.0%) | 966 (93.2%) | 9479 (93.0%) | ||
| No Lights and Sirens | 461 (4.1%) | 35 (<1%) | 426 (3.8%) | ||
| Other | 320 (2.9%) | 35 (<1%) | 285 (2.7%) | ||
| Scene Location Type | 578 (5.1%) | <0.001* | |||
| Home/Residence | 6096 (54.3%) | 591 (57.1%) | 5505 (54.0%) | ||
| Business | 993 (8.9%) | 132 (12.7%) | 861 (8.5%) | ||
| Health Care Facility | 936 (8.3%) | 83 (8.0%) | 853 (8.4%) | ||
| Public Building (School, etc.) | 919 (8.2%) | 61 (5.9%) | 858 (8.4%) | ||
| Other | 1704 (15.2%) | 143 (13.8%) | 1561 (15.3%) | ||
| Transport Mode from Scene | 0 (0%) | <0.001* | |||
| No Lights and Sirens | 5690 (50.7%) | 455 (44%) | 5235 (51.4%) | ||
| Lights and Sirens | 5281 (47.0%) | 555 (53.6%) | 4726 (46.4%) | ||
| Other | 255 (2.2%) | 26 (<1%) | 229 (2.2%) | ||
| Reason for Choosing Destination | 304 (2.7%) | <0.001* | |||
| Closest Facility | 4613 (41.0%) | 460 (44.4%) | 4153 (40.8%) | ||
| Parent/Patient Choice | 5005 (44.5%) | 474 (45.8%) | 4531 (44.5%) | ||
| Protocol | 679 (6.1%) | 59 (5.7%) | 620 (6.1%) | ||
| Specialty Resource Center | 382 (3.4%) | 27 (2.6%) | 355 (3.5%) | ||
| Other | 243 (2.2%) | 16 (1.5%) | 227 (2.2%) | ||
| Scene Time Minutes (Median, IQR) | 11.4 (9-15) | 124 (1.1%) | 13 (10-17) | 12 (8.2-15.6) | <0.001* |
| Transport Time Minutes (Median, IQR) | 13 (8.9-18.8) | 193 (1.7%) | 14 (10-19) | 12.7 (8.6-18.4) | <0.001* |
| Patient Clinical Characteristics | |||||
| Systolic Blood Pressure mmHg (Mean, SD) | 121.3 (19.1) | 1256 (11.2%) | 127.2 (17.5) | 120.7 (19.1) | <0.001* |
| Diastolic Blood Pressure mmHg (Mean, SD) | 76.4 (14.8) | 1484 (13.2%) | 78.8 (15.2) | 76.2 (14.7) | <0.001* |
| Heart Rate beats per minute (Mean, SD) | 120.5 (25.7) | 288 (2.6%) | 119.5 (25.4) | 120.6 (25.8) | 0.19 |
| Respiratory Rate breaths per minute (Mean, SD) | 27.3 (10.9) | 444 (4.0%) | 27.1 (9.8) | 27.3 (11.0) | 0.54 |
| Pulse Oximetry percentage (Median, IQR) | 98 (96-100) | 407 (3.6%) | 99 (96-100) | 98 (96-100) | 0.73 |
| Respiratory Effort, N (%) | 2254 (20.0%) | <0.001* | |||
| Normal | 5683 (50.6%) | 459 (44.3%) | 5224 (51.2%) | ||
| Labored | 3016 (26.9%) | 396 (38.2%) | 2620 (25.7%) | ||
| Fatigued | 258 (2.3%) | 37 (3.6%) | 231 (2.2%) | ||
| Absent | 15 (<1%) | 1 (<1%) | 14 (<1%) | ||
| Glasgow Coma Score (Median, IQR) | 15 (15-15) | 913 (8.1%) | 15 (15-15) | 15 (15-15) | 0.01* |
| Level of Alertness, N (%) | 1206 (10.7%) | <0.001* | |||
| Alert | 9791 (87.2%) | 900 (86.9%) | 8891 (87.3%) | ||
| Verbal | 87 (<1%) | 16 (1.5%) | 71 (<1%) | ||
| Painful | 46 (<1%) | 11 (1.0%) | 35 (<1%) | ||
| Unresponsive | 32 (<1%) | 5 (<1%) | 27 (<1%) | ||
| NHLBI Severity Score Classification3, N (%) | 246 (2.9%) | <0.001* | |||
| Mild | 1418 (12.6%) | 97 (9.4%) | 1321 (13.0%) | ||
| Moderate | 4828 (43.0%) | 397 (38.3%) | 4431 (43.5%) | ||
| Severe | 4377 (39.0%) | 485 (46.8%) | 3892 (38.2%) | ||
| Critical | 357 (3.2%) | 29 (2.8%) | 328 (3.2%) | ||
| Medications 4 , N (%) | |||||
| Number Albuterol per Patient (Mean, SD) | 1.24 (0.52) | 2106 (7.3%)5 | 1.5 (0.73) | 1.2 (0.48) | <0.001* |
| Methylprednisolone | 1036 (9.2%) | 1036 (100%) | 0 (0%) | - | |
| Ipratropium Bromide | 4095 (36.5%) | 618 (59.7%) | 3477 (31.0%) | <0.001* | |
| Oxygen | 5576 (49.7%) | 699 (67.5%) | 4877 (47.9%) | <0.001* | |
| Magnesium Sulfate | 168 (1.5%) | 99 (9.6%) | 69 (<1%) | <0.001* | |
| Normal Saline | 755 (6.7%) | 212 (20.5%) | 543 (5.3%) | <0.001* | |
| Epinephrine (1:1000) | 202 (1.8%) | 60 (5.8%) | 142 (1.4%) | <0.001* | |
| Procedures4, N (%) | |||||
| Venous Access-Extremity | 4035 (35.9%) | 7006 (19.3%)5 | 985 (95.1%) | 3050 (29.9%) | <0.001* |
| Cardiac Monitor | 3975 (35.4%) | 364 (35.1%) | 3611 (35.4%) | 0.85 | |
| Electrocardiogram | 3284 (29.3%) | 513 (49.5%) | 2771 (27.2%) | <0.001* | |
| Assessment-Adult | 2055 (18.3%) | 229 (22.1%) | 1826 (17.9%) | <0.001* | |
| Assessment-Pediatric | 2558 (22.8%) | 194 (18.7%) | 2364 (23.2%) | 0.001* | |
| Bag-Valve Mask Ventilation | 38 (<1%) | 5 (<1%) | 33 (<1%) | 0.39 | |
| CPAP | 29 (<1%) | 10 (<1%) | 19 (<1%) | <0.001* | |
| NPA | 92 (<1%) | 12 (1.2%) | 80 (<1%) | 0.20 | |
| OPA | 47 (<1%) | 0 (0%) | 47 (<1%) | 0.02* | |
| Intubation | 24 (<1%) | 2 (<1%) | 22 (<1%) | 0.89 | |
| Suction | 52 (<1%) | 3 (<1%) | 49 (<1%) | 0.63 | |
| Online Medical Direction | 104 (<1%) | 0 (0%) | 104 (1.0%) | 0.001* | |
| SQ or IM Injection | 24 (<1%) | 9 (<1%) | 15 (<1%) | <0.001* | |
| IO-Adult | 6 (<1%) | 1 (<1%) | 5 (<1%) | 0.44 | |
| IO-Pediatric | 4 (<1%) | 0 (0%) | 4 (<1%) | 0.52 | |
| CPR | 1 (<1%) | 0 (0%) | 1 (<1%) | 0.75 | |
P Values represent comparison between steroid and no steroid groups.
Indicates significance at p<0.05.
Categorical variables are represented by N (percentage).
Normally distributed continuous variables are described with mean and standard deviation (SD).
Non-normally distributed continuous variables are described with medians and interquartile ranges (IQR), from the 25th percentile to the 75th percentile.
Continuous variables are compared using Student’s T-Test (for normally distributed variables) and Kruskal-Wallis tests (for non-normally distributed variables).
Categorical variables are compared using Chi-Square test, or Fisher Exact tests if any observation was less than ten.
Methylprednisolone counted as systemic corticosteroid. As there were only 12 administrations of dexamethasone during the study period, dexamethasone was not included in the analysis. No other systemic corticosteroids were administered in the study population.
“Other” for EMS Level of Service includes nurses or physicians.
Score of mild, moderate, severe, or critical represent the highest ranking on the categories of modified 2007 National Heart, Lung, and Blood Institute’s (NHLBI) Expert Panel Report-3’s recommended system for classifying asthma exacerbation severity (Formal Evaluation of Asthma Exacerbation Severity in the Urgent or Emergent Care Setting – Table 1 & Reference 6).
N and percentage represent number of patients who were administered that medication or procedure.
N and percentage represent number of missing data for all medications or procedures administered (total N=29,020 for medications and N=36,267 for procedures).
CPAP = continuous positive airway pressure, CPR = cardiopulmonary resuscitation, EMS = Emergency medical services, EMSTARS = Emergency Medical Services Tracking and Reporting System, EMT = Emergency Medical Technician, IM = intramuscular, IO = intraosseous, SQ = subcutaneous, NPA = nasopharyngeal airway, OPA = oropharyngeal airway.
To test whether the albuterol inclusion requirement significantly altered results, a sensitivity analysis examined the number of patients aged 2–18 years with a provider primary impression of respiratory distress, but who did not receive albuterol from EMS. This produced 26,008 patient records, 22,500 (86.5%) of which were encounters attended to by EMT-paramedics, who are licensed to give albuterol for wheezing and/or asthma. Only 12 (<1%) of the 26,008 calls were attended to by EMT-Basic providers, who are not licensed to give albuterol or other medications for respiratory distress. The remaining patients were treated by intermediate-level EMTs or nurses. Therefore, it appears that in the vast majority of those excluded encounters the treating EMS providers did not believe the patient was suffering from an asthma exacerbation. As evidenced by Figure 1, for patients who did receive albuterol but were excluded, the primary symptoms and provider impressions were indicative of other processes besides asthma, such as trauma or allergic reactions.
County-based analysis of population disparities revealed a disparate impact on African-American pediatric patients with asthma. County level differences in proportion of African-Americans were normally distributed (W = 0.976, p value = 0.297, Shapiro-Wilk test). Several counties had frequencies of EMS encounters for that population much greater than expected based on population percentage (Figure 2). Of the 7 counties with z-scores greater than 1 standard deviation above the mean, 4 (including the county with the highest positive z-score) are classified as rural by the Florida Department of Health.22,25
Figure 2.
Legend: Distribution of Difference in Observed Versus Expected Percent of African-American EMSTARS Asthma Patients by County in Florida. Shading indicates numerical distribution of z scores.
We compared characteristics between patients who did and did not receive systemic corticosteroids (in the form of methylprednisolone only, as dexamethasone had few administrations). Patients who received systemic corticosteroids were older and had longer EMS scene and transport times (all p<0.0001) (Table 2). Also, systemic corticosteroid administration varied directly by respiratory effort (p<0.0001) and modified-NHLBI severity score (p<0.0001), and inversely by total Glasgow Coma Score (p=0.0104) and level of alertness (p<0.0001), all indicating a more severe clinical presentation. However, systemic corticosteroid administration did not vary by respiratory rate (p=0.54), heart rate (p=0.19), or pulse oximetry (p=0.73); nor did it vary by race (p=0.068) or ethnicity (p=0.17). Although 1,036 patients were documented as receiving systemic corticosteroids, IV access was only documented for 985 patients. A Bonferroni correction for multiple comparisons decreased the adjusted Type I error to 0.0012, which made gender, EMS encounter year, GCS, and oropharyngeal airway no longer significant.
The results of the multivariable logistic regression evaluating factors associated with EMS systemic corticosteroid administration demonstrated that the most significant predictors all related to medication administration (Table 3, Supplemental Digital Content 1). The strongest predictors were IV access (OR 33.3, 95% CI 24.4–45.6), administration of a subcutaneous or intramuscular injection (OR 3.6, 95% CI 1.3–10.3), and concomitant administration of other medications such as IV magnesium sulfate (OR 5.0, 95% CI 3.4–7.3) or inhaled ipratropium bromide (OR 2.4, 95% CI 2.0–2.8). Other significant predictors included labored respiratory effort (OR 1.6, 95% CI 1.4–1.9), and race other than African-American or white (OR 1.3, 95% CI 1.0–1.6). Patient or family choice of the destination facility was predictive of not receiving systemic corticosteroids (OR 0.7, 95% CI 0.6–0.9).
Table 3:
Multivariable logistic regression results: Significant predictor variables for EMS administration of systemic corticosteroids1,2
| Variable | Odds Ratio | 95% Confidence Limits | |
|---|---|---|---|
| Extremity Intravenous Access | 33.4 | 24.4 | 45.6 |
| Magnesium Sulfate administration | 5.0 | 3.4 | 7.3 |
| Subcutaneous or Intramuscular Injection | 3.6 | 1.3 | 10.3 |
| Ipratropium Bromide administration | 2.4 | 2.0 | 2.8 |
| Electrocardiogram | 1.9 | 1.6 | 2.2 |
| Oxygen administration | 1.8 | 1.5 | 2.2 |
| Labored Respiratory Effort | 1.6 | 1.4 | 1.9 |
| Adult Assessment | 1.5 | 1.3 | 1.9 |
| Normal Saline administration | 1.5 | 1.2 | 1.8 |
| Severe (per modified-NHLBI severity score) |
1.4 | 1.2 | 1.6 |
| Pediatric Assessment | 1.3 | 1.0 | 1.6 |
| Race other than Black or White | 1.3 | 1.0 | 1.6 |
| Patient Age (years)3 | 1.0 | 1.0 | 1.0 |
| Patient Choice of Destination Facility | 0.7 | 0.6 | 0.9 |
EMS = Emergency Medical Services, NHLBI = National Heart Lung and Blood Institute
Methylprednisolone counted as systemic corticosteroid. As there were only 12 administrations of dexamethasone over the study period, dexamethasone was not included in this analysis. No other systemic corticosteroids were administered in the study sample.
Hosmer-Lemeshow goodness-of-fit test = 0.3609, Model AUC = 0.895, AIC 4175.
Odds of steroid administration increased by increasing years of age, OR 1.023, 95% CI 1.005 – 1.041.
Discussion
This is the largest study to describe the epidemiology of EMS treatment of pediatric asthma. In this statewide study, we found disparate impacts on rural African-American children, as well as underutilization of evidence-based asthma treatments such as systemic corticosteroids and ipratropium bromide.
Nearly half of the study population was African-American (49%), which is much larger than the statewide African-American population (16.9%).18 However, this proportion is similar to other ED and population-based studies of disparities in asthma exacerbation frequency with respect to African-American patients.2,3,26 Although previous research has found evidence that African-Americans utilize EMS at a higher frequency, given that patients arriving via EMS are typically higher acuity, these findings underscore the disproportionate impact acute asthma exacerbations have on the African-American population.27,28
The typical epidemiologic description of the disparate impact of asthma on African-American populations describes urban, inner-city environments.29 However, this study’s geographic analysis reveals a geographic disparity of EMS asthma encounters involving African-Americans living in rural counties. The current rural health crisis of reduced service availability and its impact on emergency medical services is receiving increasing media and scholarly attention.30,31 However this study’s rural asthma EMS encounters may also reflect genetic, socioeconomic, or environmental factors in addition to the current rural healthcare crisis. Future studies should seek to define the etiology of these significant geographic disparities of asthma exacerbations affecting rural African-American children. Regardless of etiology, these findings underscore that the rural health crisis is affecting other racial groups in addition to white populations.31
With respect to asthma treatment, we found that systemic corticosteroids (in the form of methylprednisolone) are reserved for the small (<10%) percent of generally more severe patients. However, systemic corticosteroids are more liberally administered in the ED (usually via oral administration), as they confer benefits for mild, moderate, and severe asthma exacerbations.7,8,10–12 Furthermore, early administration of systemic corticosteroids in the ED has proven to reduce ED LOS and hospitalization rates.10–12 Therefore would even earlier EMS administration of systemic corticosteroids further improve patient outcomes? A study of one EMS agency that liberalized systemic corticosteroid use (in the form of oral dexamethasone) for all pediatric asthmatics found a decrease in ED LOS of nearly two hours, as well as a decrease in hospital admission rates from 30% to 21%.32 However, that same study also found very low overall rates of systemic corticosteroid administration, only increasing from 11% to 18% after the protocol change.32 Additionally, in this study approximately one-third of patients received ipratropium bromide, which also has proved to reduce hospitalizations when combined with albuterol in the pediatric ED setting.7,8,33,34 Therefore, it appears many EMS pediatric asthma patients miss the opportunity to receive medications prior to ED arrival that could markedly change their clinical outcomes. Those treatments may not be emphasized in the implementation of and education regarding pediatric EMS asthma protocols.
EMS medication use is typically governed by local agency protocols. In this study, although the percentage of patients who received systemic corticosteroids or ipratropium bromide varied by county, most counties did utilize both medications (data available upon request). In Florida, most counties are serviced by one EMS agency, although some more-populated urban counties contain more than one EMS agency.19 Given the greater than 50 individual EMS agencies in Florida, we were not able to ascertain each agency’s asthma or pediatric asthma protocol during the study period. However, given our results, it appears that either by protocol or practice, EMS providers infrequently (<1% of encounters in this study) administer oral systemic corticosteroids to pediatric asthma patients. The three most significant predictors of systemic corticosteroid use from the adjusted logistic regression were IV access, subcutaneous or intramuscular injection, and another IV medication (magnesium sulfate), perhaps indicating more severe patients who required IV access for other therapies. This suggests a barrier to more widespread EMS systemic corticosteroid administration may be pediatric IV placement. Indeed, previous studies have found low frequencies and increasing difficulties with EMS IV placement with younger ages, which may explain this study’s findings of increasing age conferring greater odds of receiving systemic corticosteroids.35,36 Other potential barriers to systemic corticosteroid administration previously identified in the ED literature include markers of severity, female sex, and longer duration of symptoms.37 Similarly, this study found that patients with labored breathing who scored severe on the modified-NHLBI severity scoring system were more likely to receive systemic corticosteroids.
In addition to clinical characteristics, this study found significantly longer EMS scene and transport times for patients who received systemic corticosteroids. Scene time increases may be a direct reflection of the time required for IV placement and medication administration. Transport time increases may reflect a decision by EMS providers to administer methylprednisolone based on longer transport times. Despite the scene time increase, EMS providers may be best-suited for efficient administration of systemic corticosteroids. A previous study of adult asthma patients compared the time from EMS provider arrival on scene to methylprednisolone administration, with the time from patient ED arrival to methylprednisolone administration.38 The average time from arrival to EMS administration was 15 minutes (SD 7 minutes), compared with 40 minutes (SD 22 minutes) for ED-treated patients.38 Since IV placement may be a larger barrier in children than adults, exploration of alternative routes of systemic corticosteroid delivery (such as oral prednisolone or oral or intramuscular dexamethasone) are needed to optimize pediatric asthma outcomes.
Limitations
This study is a retrospective study of one state and therefore its conclusions may not be generalizable to other areas of the United States. However, Florida is the state with the fourth-largest pediatric population and is one of the largest contributors to the National EMS Information Systems’ database.17, 19 As such, EMSTARS data contains a voluminous amount of EMS data worthy of examination. EMSTARS does not contain data from every EMS agency in Florida, which may be reflected in this study’s results, particularly the geographic analysis. However, the 100 agencies reporting to EMSTARS comprise 74% of all 911 EMS calls made during the study period.19 Although interfacility transports were intentionally excluded, there may such patients in the dataset not coded as such. Additionally, the EMSTARS dataset does not identify ground versus helicopter transports. Another limitation is that EMSTARS contains unique identifiers for each patient encounter, so we were unable to ascertain if any patients were repeat encounters.
EMSTARS does not include what medications patients may have received prior to EMS arrival, including oral systemic corticosteroids that may have been prescribed in case of an exacerbation. However, in our experience primary care providers rarely prescribe oral corticosteroids without an acute patient visit. EMSTARS does not contain hospital data, and so this study does not include patient outcomes. The modified NHLBI severity score used in this study has not been validated in the EMS setting, and although it represents a best estimate of severity, results should be interpreted in that context.
EMSTARS does not contain a data variable for ‘Past Medical History’, nor does it contain any free text narrative for each patient encounter. Therefore, we were unable to ascertain if any patients had a prior history of asthma to increase the accuracy of our inclusion and exclusion criteria. The inclusion criteria of receiving albuterol from EMS was specifically designed to include patients with acute asthma exacerbations. It may be possible that some EMS patients with asthma exacerbations did not receive albuterol, or that that some patients received albuterol who were not having an asthma exacerbation. However, the inclusion criteria’s sensitivity analysis revealed that the majority of all patients ages 2–18 with respiratory distress in EMSTARS were treated by EMT-paramedics. EMT-paramedics are highly trained in the indications for and administration of medications for respiratory conditions, including asthma. Therefore, we believe the albuterol inclusion criteria most likely selected for patients suffering from an asthma exacerbation and excluded those with respiratory distress due to other causes (e.g., pneumonia, croup). Additionally, requiring the primary symptom and provider primary impression to indicate respiratory distress filtered out wheezing potentially due to other causes other than asthma (e.g., trauma, allergic reaction) as evidenced by Figure 1. However it is possible that some of those excluded patients were indeed suffering from an asthma exacerbation.
Similar to other research utilizing large EMS datasets, EMSTARS variables contain missing data (as noted in Table 2). When large amounts of values are missing, this may bias the results or reduce their precision.39 The geospatial analysis was missing data for 8 out of Florida’s 59 counties. Many counties, especially in rural areas, had low numbers of patient encounters, (e.g., 9 counties with less than 10 records), and so results should be interpreted based on those small sample sizes. However, as compared with other previously published research, the majority of variables missing in this study was low.40
Conclusions
In this statewide study, the vast majority of pediatric asthma patients treated by EMS did not receive systemic corticosteroids or inhaled ipratropium bromide, two evidence-based ED treatments that reduces ED LOS and hospitalization rates. Thus, data from the present study demonstrate a need to educate EMS providers on the potential benefits of those medications and the need to update EMS protocols. This study also identifies disproportionate numbers of EMS encounters involving rural African-American children. Further work is required to discern the etiology of demographic and geographic disparities, as well as barriers and enablers to EMS administration of systemic corticosteroids. The results of this study suggest the need for a randomized controlled trial of EMS administered oral systemic corticosteroids.
Supplementary Material
Acknowledgements
The study investigators acknowledge Steve McCoy, Brenda Clotfelter, Karen Card, DrPH and Joshua Sturms from the Florida Department of Health’s Bureau of Emergency Medical Oversight for their assistance and data management. Also, the study investigators also wish to acknowledge Colleen Kalynych, Michelle Lott, and Justin Masud from the University of Florida – Jacksonville Department of Emergency Medicine, Division of Research, and Alexis Thomas and Paul Zwick, from the University of Florida GeoPlan Center, for their assistance with this study.
Funding Info: Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under University of Florida Clinical and Translational Science Awards KL2TR001429 and UL1TR001427. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Disclosures: All authors report no financial disclosures or conflicts of interest.
References
- 1.Moorman JE, Akinbami LJ, Bailey CM, et al. National Surveillance of Asthma: United States, 2001–2010. National Center for Health Statistics. Vital Health Stat. 2012;3(35). [PubMed] [Google Scholar]
- 2.Akimbami LJ, Schoendorf KC. Trends in childhood asthma: Prevalence, Health Care Utilization, and Mortality. Pediatrics. 2002;110(2):315–22. [DOI] [PubMed] [Google Scholar]
- 3.Boudreaux ED, Emond SD, Clark S, et al. Race/Ethnicity and asthma among children presenting to the emergency department: Differences in disease severity and management. Pediatrics. 2003;111:e615–21. [DOI] [PubMed] [Google Scholar]
- 4.Florida Department of Health , Division of Community Health Promotion, Bureau of Chronic Disease Prevention, Florida Asthma Program. Burden of Asthma in Florida, 2013. Available at: http://www.floridahealth.gov/diseases-and-conditions/asthma/data.html. Accessed July 26, 2018. [Google Scholar]
- 5.Loftus PA, Wise SK. Epidemiology and economic burden of asthma. Int Forum Allergy Rhinol. 2016;5(Suppl 1):S7–10. [DOI] [PubMed] [Google Scholar]
- 6.Tsai C, Sullivan AF, Gordon JA, et al. Quality of care for acute asthma in 63 US emergency departments. J Allergy Clin Immunol. 2009;123(2):354–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Camargo CA Jr., Rachelefsky G, Schatz M Managing asthma exacerbations in the emergency department: Summary of the National Asthma Education and Prevention Program Expert Panel Report 3 Guidelines for the management of asthma exacerbations. J Emerg Med. 2009;37(2S):S6–17. [DOI] [PubMed] [Google Scholar]
- 8.Jones BP, Fleming GM, Otillio JK, et al. Pediatric acute asthma exacerbations: Evaluation and management from emergency department to intensive care unit. J Asthma. 2016;53(6):607–617. [DOI] [PubMed] [Google Scholar]
- 9.CDC Guidelines: Workgroup on EMS Management of Asthma Exacerbations. A model protocol for Emergency Medical Services management of asthma exacerbations. Prehosp Emerg Care. 2006;10:418–429. [DOI] [PubMed] [Google Scholar]
- 10.Davis SR, Burke G, Hogan E, Smith SR. Corticosteroid timing and length of stay for children with asthma in the emergency department. J Asthma. 2012;49(8):862–867. [DOI] [PubMed] [Google Scholar]
- 11.Bhogal SK, McGillivray D, Bourbeau J, et al. Early administration of systemic corticosteroids reduces hospital admission rates for children with moderate and severe asthma exacerbation. Ann Emerg Med. 2012;60(1):84–91. [DOI] [PubMed] [Google Scholar]
- 12.Rowe BH, Spooner C, Ducharme FM, et al. Early emergency department treatment of acute asthma with systemic corticosteroids. Cochrane Database Syst Rev. 2001;(1):CD002178. [DOI] [PubMed] [Google Scholar]
- 13.Shah MN, Cushman JT, Davis CO, et al. The epidemiology of emergency medical services use by children: An analysis of the National Hospital Ambulatory Medical Care Survey. Prehosp Emerg Care. 2008;12(3):269–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bloom B, Jones IJ, Freeman G. Summary health statistics for U.S. children: National Health Interview Survey, 2012. National Center for Health Statistics. Vital Health Stat. 2013;10(258):1–81. [PubMed] [Google Scholar]
- 15.Lerner EB, Dayan PS, Brown K, et al. Characteristics of the pediatric patients treated by the Pediatric Emergency Care Applied Research Network’s affiliated EMS agencies. Prehosp Emerg Care. 2014;18:52–59. [DOI] [PubMed] [Google Scholar]
- 16.Delbridge T, Domeier R, Key CB. Prehospital asthma management. Prehosp Emerg Care. 2003;7(1):42–7. [DOI] [PubMed] [Google Scholar]
- 17.Howden LM, Meyer JA. Age and Sex Composition: 2010 Census Briefs. U.S. Census Bureau. 2011. Available at: https://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf. Accessed June 29, 2018. [Google Scholar]
- 18.United States Census Bureau. Quick Facts: Florida. Available at: https://www.census.gov/quickfacts/fact/table/fl/PST045217. Accessed June 30, 2018. [Google Scholar]
- 19.Florida’s Prehospital EMS Tracking and Reporting System (EMSTARS). “Basic Facts Document”. Available at: http://www.floridaemstars.com. Accessed July 28, 2018. [Google Scholar]
- 20.Gausche-Hill M, Eckstein M, Horeczko T, et al. Paramedics accurately apply the pediatric assessment triangle to drive management. Prehosp Emerg Care. 2014;18(4):520–30. [DOI] [PubMed] [Google Scholar]
- 21.de Caen AR, Berg MD, Chameides L, et al. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care (reprint). Pediatrics. 2015;136;S176. [DOI] [PubMed] [Google Scholar]
- 22.2010 Decennial Census of Population and Housing. United States Census Bureau. Available at: Florida Geographic Data Library (FGDL) ftp://ftp.fgdl.org/pub/state/cenblk2010_aug11.zip. Accessed August 2, 2018. [Google Scholar]
- 23.Kim H Statistical notes for clinical researchers: Chi-squared test and Fisher’s exact test. Restor Dent Endod. 2017;42(2):152–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Razali NM. Power comparisons of Shapiro-Wilk, Kolmogorov-Smirnov, Lilliefors and Anderson-Darling tests. Journal of Statistical Modeling and Analytics. 2011;2(1):21–33. [Google Scholar]
- 25.Florida’s Rural Counties. Florida Department of Health. Available at: http://www.floridahealth.gov/programs-and-services/community-health/rural-health/_documents/ruralcountiespdf.12.pdf. Accessed August 2, 2018. [Google Scholar]
- 26.Smith LA, Hatcher-Ross JL, Wertheimer R, Kahn RS. Rethinking race/ethnicity, income, and childhood asthma: Racial/Ethnic disparities concentrated among the very poor. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Knowlton A, Wier BW, Hughes BS, et al. Patient demographic and health factors associated with frequent use of emergency medical services in a midsized city. Acad Emerg Med. 2013;20:1101–1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meisel ZF, Pines JM, Polsky D, et al. Variations in ambulance use in the United States: The role of health insurance. Acad Emerg Med. 2011;18:1036–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Keet CA, McCormack MC, Pollack CE, et al. Neighborhood poverty, urban residence, race/ethnicity, and asthma: Rethinking the inner-city asthma epidemic. Journal of Allergy and Clinical Immunology. 2015;135(3):655–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Harrison S, Templeton K. Rural America’s Health Care Crisis. Published March 15, 2018. Available at: https://www.realclearhealth.com/articles/2018/03/15/rural_americas_health_care_crisis.html. Accessed June 30, 2018. [Google Scholar]
- 31.Erwin PC. Despair in the American heartland? A focus on rural health. AJPH. 2017;107(10):1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nassif A, Ostermayer DG, Hoang KB, et al. Implementation of a prehospital protocol change for asthmatic children. Prehosp Emerg Care. 2018;22(4):457–65. [DOI] [PubMed] [Google Scholar]
- 33.Schuh S, Johnson DW, Callahan S, et al. Efficacy of frequent nebulized ipratropium bromide added to frequent high-dose albuterol therapy in severe childhood asthma. J Pediatr. 1995;126:639–45. [DOI] [PubMed] [Google Scholar]
- 34.Qureshi F, Pestian J, Davis P, Zaritsky A. Effect of nebulized ipratropium on the hospitalization rates of children with asthma. N Engl J Med. 1998;339:1030–5. [DOI] [PubMed] [Google Scholar]
- 35.VanderKooy T, Spaur K, Brou L, et al. Utilization of intravenous catheters by prehospital providers during pediatric transports. Prehosp Emerg Care. 2018;22(1):50–7. [DOI] [PubMed] [Google Scholar]
- 36.Frisch A, Cammarata S, Mosesso VN Jr, Martin-Gill C. Multivariate analysis of successful intravenous line placement in the prehospital setting. Prehosp Emerg Care. 2013;17(1):46–50. [DOI] [PubMed] [Google Scholar]
- 37.Tsai C, Rowe BH, Sullivan AF, Camargo CA Jr. Factors associated with delayed use or nonuse of systemic corticosteroids in emergency department patients with acute asthma. Ann Allergy Asthma Immunol. 2009;103(4):318–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Knapp B, Wood C. The prehospital administration of intravenous methylprednisolone lowers hospital admission rates for moderate to severe asthma. Prehosp Emerg Care. 2003;7:423–6. [DOI] [PubMed] [Google Scholar]
- 39.Wayman JC. Multiple imputation for missing data: What is it and how can I use it? Presented at: Annual Meeting of the American Educational Research Association. 2003. Chicago, IL. [Google Scholar]
- 40.Newgard CD, Malveau S, Saudenmayer K, et al. Evaluating the use of existing data sources, probabilistic linkage, and multiple imputation to build population-based injury databases across phases of trauma care. Acad Emerg Med. 2012;19(4):469–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.