Abstract
Objective
Persistent symptoms and poor quality of life (QoL) are common following anterior cruciate ligament reconstruction (ACLR). We aimed to determine the influence of a combined ACL injury (i.e., concomitant meniscectomy and/or arthroscopic chondral defect at the time of ACLR and/or secondary injury/surgery to ACLR knee) and MRI-defined cartilage defects, bone marrow lesions (BMLs) and meniscal lesions on patient-reported outcomes (PROs) 1- to 5-years post-ACLR.
Methods
80 participants (50 men) aged 32±14 years completed the Knee injury and OA Outcome Score (KOOS) and International Knee Documentation Committee (IKDC) questionnaire, and 3T MRI assessment at 1- and 5-years post-ACLR. Median PRO scores were compared between isolated and combined ACL injuries, and with published normative values. Multivariate regression evaluated the association between compartment-specific MRI cartilage, BMLs and meniscal lesions, and PROs at 1- and 5-years.
Results:
Individuals with a combined injury had significantly worse KOOS-Sport, and IKDC scores at 1-year, and worse KOOS-Pain, KOOS-Symptoms, KOOS-QoL, and IKDC scores at 5-years, compared to those with an isolated injury. Whilst no feature on MRI was associated with PROs cross-sectionally at 1-year, patellofemoral cartilage defects at 1-year were significantly associated with worse 5-year KOOS-Symptoms (β: −9.79; 95%CI:-16.67, −2.91), KOOS-Sport (β: −7.94; 95%CI:-15.27, −0.61), KOOS-QoL (β: −8.29; 95%CI:-15.28, −1.29) and IKDC (β: −4.79; 95%CI:-9.34, −0.24). Patellofemoral cartilage defects at 5-years were also significantly associated with worse 5-year KOOS-Symptoms (β: −6.86; 95%CI:-13.49, −0.24) and KOOS-QoL (β: −11.71; 95%CI:-19.08, −4.33).
Conclusion:
Combined injury, and patellofemoral cartilage defects on MRI are associated with poorer long-term outcomes. Clinicians should be vigilant to these individuals, who may benefit from targeted interventions to improve QoL and optimise symptoms.
Anterior cruciate ligament reconstruction (ACLR) is commonly performed following ACL injury in individuals seeking a return to pre-injury sports participation. Patient-reported symptoms, function and quality of life (QoL) typically improve during the first 6–12 months following ACLR, but appear to plateau beyond this point [1–4]. While 65% of young people return to pre-injury sports participation following ACLR [5], as many as 34% report unacceptable symptoms up to two years following surgery [6]. Persistent symptoms could induce negative lifestyle modifications (i.e. reduce physical activity, weight gain) [7], increasing burden on health-care systems in the longer term. Successfully identifying people with persistent symptoms early following ACLR may allow for development of targeted interventions.
A combined injury (i.e. ACL injury and meniscectomy and/or cartilage lesion assessed at time of ACLR) might increase the risk of worse symptoms and QoL in the short- to medium- (1–6 years) [1, 3] and long-term (15–20 years) [8]. However, some studies report no or minimal association between combined injuries and patient-reported outcomes (PROs) in the medium- to long-term [9–11]. Previous studies [2, 3, 8, 9] have utilised group-level data (i.e. determining if a significant group mean effect exists between isolated and combined ACLR groups). This may not be relevant to patients and clinicians, who are most interested in their own individual effect in relation to the treatment they have undergone. The group level approach does not describe the number of individuals who present with unacceptable outcomes, who may require and benefit from additional interventions. Identifying individuals with poor outcomes, and enhancing clinical interpretability of PROs may be improved by comparing scores from each ACLR individual (as opposed to group means) to scores from other ACLR individuals who report “acceptable” knee function.
Persistent symptoms following ACLR may be related to early deterioration of joint structure. Radiographic osteoarthritis (OA) occurs in 50–90% of knees 10–15 years after ACLR, but the relationship with PROs is unclear [12, 13]. In older populations with established knee OA, more specific imaging markers of disease observed on magnetic resonance imaging (MRI), such as bone marrow lesions (BMLs), inflammation and cartilage defects, are associated with clinical outcomes (i.e. pain) [14–17]. Whilst early structural pathology identified on MRI may be pre-existing, or occur with injury, OA features continue to deteriorate at an accelerated rate compared to primary OA between 1- and 5-years post-ACLR [18]. Yet, there is limited research on how these early OA features affect PROs. Tibiofemoral cartilage lesions and BMLs have little association with knee symptoms cross-sectionally at 2- [19] and 12-years post-ACLR [20]. An important omission in previous research is the patellofemoral joint, which is a potential contributor to knee symptoms following ACLR [21]. We recently identified that patellofemoral cartilage defects at 1-year post-ACLR were associated with worse PROs at 3-years [22]. Further cross-sectional and longitudinal evaluation of the relationship between MRI-OA features and PROs beyond 3-years is important, to determine if imaging features of OA affect patient reported pain, function or QoL.
The aims of the current study were to determine: i) the influence of a combined injury on PROs from 1- to 5-years post-ACLR, and compare these to known normative PRO scores (in non-injured and ACLR individuals); and ii) the association between patellofemoral and tibiofemoral cartilage defects, BMLs, meniscal lesions, and PROs, at 1- and 5-years post-ACLR.
METHODS
Study design and participants
All 112 consecutively recruited individuals who had completed PROs at 1-year post-ACLR as part of our previous evaluation [23] (median age at surgery; 27 (range 18–51) years) were eligible for the current prospective 5-year follow-up study. Baseline (1-year post-ACLR) eligibility criteria, ACLR technique, and changes in cartilage, bone marrow and meniscus between 1- and 5-years have been reported previously [18, 23]. Briefly, all individuals were operated on by one of two Melbourne-based orthopaedic surgeons with a single-bundle hamstring-autograft ACLR. Baseline exclusion criteria included knee injury/symptoms prior to ACL injury, >5 years between ACL injury and reconstruction, and any secondary injury/surgery (between surgery and 1-year post-ACLR). Secondary injury was defined as a new index or contralateral knee injury (ACL, meniscus, collateral ligament), or surgery. All participants were invited to participate at the 5-year post-ACLR follow-up, including 10 participants who sustained a secondary injury between 1- and 5-years, as this is a common occurrence and represents the wider ACLR population. Eighty-one (72%) participants completed the same PROs at the 5-year post-ACLR evaluation (Figure 1). Ethical approval was granted by La Trobe University Human Ethics Committee (HEC 15–100) and all participants signed informed consent.
Figure 1. Flowchart of participant recruitment into the study.
PROs = patient-reported outcomes; MRI = magnetic resonance imaging
~Clinical assessment was also performed on a subset of the cohort at 1- and 5-years. Body mass index from the clinical assessment was required for the regression analysis, resulting in n=6 not included in the analysis for 5-years MRI: 5-year PROs.
*Participant at 1-year was involved in the research team at 5-years
Demographic, injury and surgical factors
Participant age, sex, injury history, body mass index (BMI), previous and current activity level (defined as level 1=pivoting/jumping sports up to level 4 sedentary) [24] was obtained at 1- and 5-years. The combined injury group at 1-year consisted of individuals with ACL injury and concomitant meniscectomy or significant cartilage defect (i.e. Outerbridge grade ≥2) [25] at the time of ACLR (i.e. extracted from surgical notes). Those reporting to investigators a secondary injury/surgery to the index knee between the 1- and 5-year follow-up were added to the combined injury group at 5-years. Defining a combined injury by the presence of a concomitant injury at time of ACLR, and/or a secondary injury over time via this method is consistent with previous longitudinal cohort studies [8, 11]. Individuals without a combined injury were defined as having an “isolated” injury.
Patient-reported outcome measures
At 1- and 5-years, participants completed the Knee injury and OA Outcome Score (KOOS) and International Knee Documentation Committee (IKDC) subjective knee evaluation, with respect to their index knee condition during the previous week. The KOOS and IKDC are used extensively in people with ACL injuries, with established reliability and validity [26]. Four subscales of the KOOS were assessed: pain, symptoms, function in sport and recreation, and knee-related QoL. The KOOS activities of daily living subscale was excluded due to the ceiling effects observed in young active populations [27]. PROs were completed either in person (pen and paper) or via an online portal (Promptus, DS PRIMA, Melbourne, Australia) with matching instructions to the original paper version. The KOOS (ICC>0.96) [28] and IKDC (ICC=0.79) [29] have demonstrated test-retest reliability between paper and electronic formats.
Cartilage defects, BMLs, and meniscal lesions
MRI acquisition and interpretation
Of the 112 participants completing PROs at 1-year, 111 completed MRI assessment at 1-year, and 80 (71%) at 5-years (Figure 1) with identical MRI scanner and sequences as described previously [23]. Briefly, with a 3T system (Philips Achieva, The Netherlands), sequences consisted of a 3D proton-density weighted VISTA acquired at 0.35mm isotropically, short-tau inversion-recovery sequence, and an axial proton-density turbo spin-echo sequence. Cartilage defects, BMLs and meniscal lesions were scored using the MRI OA Knee Score (MOAKS) by a musculoskeletal radiologist (AG) with 19-years of experience, and established inter- and intra-rater reliability in semi-quantitative MRI assessment (kappa 0.61–0.80) [30]. The 1- and 5-year images were read paired (not blinded to time-points), but blind to clinical information. The MOAKS divides the knee into 14 articular sub-regions to score cartilage defects and BMLs. For the tibiofemoral compartment, cartilage defects and BMLs were graded in each of the 10 sub-regions (medial and lateral: central and posterior femur, anterior, central and posterior tibia). Four sub-regions were used to grade cartilage defects and BMLs in the patellofemoral compartment - the patella (medial and lateral) and trochlea (medial and lateral). Meniscal lesions were defined as medial or lateral, and divided into anterior, posterior and central sub-regions. Cartilage defects and BMLs were graded as present or absent in the tibiofemoral and patellofemoral compartments if any corresponding sub-regions for that compartment had a lesion ≥grade 1 in size (i.e., any lesion >0% in size relative to each sub-region surface area). Meniscal lesions were graded as present if in either tibiofemoral compartment sub-region there was i) a definite vertical, horizontal or complex tear (definite = an area of abnormal signal that extends to the meniscal articular surface); ii) partial or progressive maceration (loss of morphologic substance of the meniscus); or iii) at least grade 1 extrusion (i.e. >2mm) [30]. Details of MRI sequences and MOAKS appear in Supplementary File 1.
Statistical analyses
Combined and isolated injury group medians and interquartile range (IQR) for the KOOS and IKDC were calculated at 1- and 5-years, due to non-normally distributed data (assessed with Shapiro-Wilk tests). For the KOOS and IKDC, we visually compared and indicated if the ACLR median scores were at least a minimum detectable change (MDC) (i.e. ≥14 points) [26, 31] below the normative median [32–34]. Non-parametric analyses were used to account for the non-normal distribution of the KOOS and IKDC scores at 1- and 5-years. Mann-Whitney U tests compared PROs between the isolated and combined groups cross-sectionally at 1- and 5-years. The absolute change in PROs between 1- and 5-years was normally distributed and reported as mean (standard deviation), and parametric analyses (independent sample t-tests) compared the change in each group. In addition, each individual was classified as having an “acceptable” KOOS or IKDC score if it was greater than a pre-determined cut-off [6, 35]. The KOOS cut-offs were determined from the Norwegian Knee Ligament Registry (n=1197), using the lower 95% confidence interval (CI) score for each subscale (Pain: 88/100 Symptoms: 83/100 Sport: 73/100 QoL: 73/100) of individuals who perceived their knee function as acceptable 24-months post-ACLR [6]. The IKDC cut-off (75/100) was determined using the mean IKDC score (85/100) minus the standard deviation (SD=10) of individuals who perceived their knee function as acceptable 3.5 years post-ACLR [35]. Fisher’s exact test was used to compare the proportion of the isolated and combined groups defined as “acceptable.”
Multivariable linear regression was used to determine the cross-sectional relationship between the presence of cartilage lesions, BMLs, and meniscal lesions (dichotomous independent variables) in the patellofemoral and tibiofemoral compartment, and PROs (continuous KOOS and IKDC scores) at 1- and 5-years. Regression was adjusted for age at the time of surgery, sex, BMI at 1-year, and combined injury, due to their potential influence on PROs (Supplementary File 3). The relationship between cartilage lesions, BMLs, and meniscal lesions at 1-year with PROs at 5-years was also included, with additional adjustment for baseline PRO score. Stata for Windows V.14.2 was used for statistical analyses (StataCorp LLC, Texas, USA). P values <0.05 were considered statistically significant.
RESULTS
Demographic characteristics of the 81 participants included for PROs analysis at 1- and 5-years are presented in Table 1. There were no demographic, surgical or baseline MRI-related differences between those who did (n=81) and did not participate (n=30) in the follow-up assessment at 5-years (p≥0.05) (Supplementary File 4). This was except for medial meniscal lesions, which were more prevalent in the participating group at baseline. Forty (49%) and 46 (57%) of the 81 participants were classified as having a combined injury at 1- and 5-years respectively (i.e. six were added to the combined injury group at 5-years due to a secondary injury between 1- and 5-years). Between 1-year and 5-years, 10 participants had a secondary injury to the index knee (Table 1); however, four of these were already classified as a combined injury at 1-year.
Table 1.
Participant characteristics of combined and isolated injury groups at 1- and 5-years post-ACLR~
| 1 year (n=81)# | 5 years (n=81)# | |||
|---|---|---|---|---|
| Combined (n=40) ~ | Isolated (n=41) ~ | Combined (n=46) ~ | Isolated (n=35) ~ | |
| Age, median ± IQR years | 31±12* | 25±12 | 35±14* | 29±13 |
| Sex, no. (% male) | 26 (65) | 24 (59) | 31 (67) | 19 (54) |
| Body Mass Index^, median ± IQR kg/m2 | 26.9±5.4* | 24.8±3. | 27.5±5.1* | 24.7 ±4.2 |
| Pre-Injury Activity Level 1 sport◊, no. (%) | 28 (70) | 28 (68) | 34 (74) | 22 (63) |
| Anteroposterior laxity between-limb differenceϠ, median, ± IQR, millimeters | 1.1±2.7 | 1.9±2.1 | NA | NA |
| Time injury to surgery, median + IQR weeks | 19±32* | 12±9 | 17±26* | 12±9 |
| Meniscectomy at time of ACLR¥, no. (%) | 32 (80) | 0 (0)~ | 32 (40) | 0 (0)~ |
| Cartilage defect at time of ACLR¤, no. (%) | 16 (40) | 0 (0)~ | 16 (35) | 0 (0)~ |
| New knee Injuries (either limb), no. (%) | 0 (0)** | 0 (0)** | 13 (28) | 3 (9)~ |
| ACLR limb✪ | 0 (0)** | 0 (0)** | 10 (22) | 0 (0)~ |
| Contralateral limb★ | 0 (0)** | 0 (0)** | 3 (7) | 3 (9)~ |
| Returned to Level 1 sport◊, no. (%) | 9 (23) | 11 (27) | 11 (24) | 9 (26) |
Participants defined as a combined injury at 1- and 5-years if they had a significant cartilage defect/meniscectomy assessed at the time of ACLR.
Demographics for n=81 participating in PROs at 1- and 5-years (n=31 dropouts). Demographics for n=111 from 1-year assessment, are previously reported [23].
ACLR = anterior cruciate ligament reconstruction; IQR=interquartile range; NA, not assessed
BMI (body mass index), note: n=75 participating in BMI assessment at 5-years
Level 1 sport = jumping, cutting pivoting as per Sports Activity Classification based on Grindem et al., 2012 [24]
Assessed using the KT-1000 arthrometer (Mesmeric Corp., California, USA) at 30° of flexion with 30lb load [45]
Performed at the time of ACLR
Assessed arthroscopically at time of ACLR, cartilage defect defined as Outerbridge [25] grade ≥2 (i.e., at least a partial-thickness defect)
5-year new ACLR limb knee injuries/surgery n=10 (n= 3 ACLR revision, n=6 meniscectomy, n=1 lateral collateral ligament sprain)
5-year new contralateral limb knee injuries/surgery n=6 (combined: n=2 ACLR n=1 meniscectomy, isolated: n=1 ACLR, n=1 meniscectomy, n=1 lateral collateral sprain)
Statistically significant (p<0.05) difference between combined and isolated injury groups.
No new knee injuries were reported at 1-year as this was an exclusion criterion.
Patient-reported outcome measures
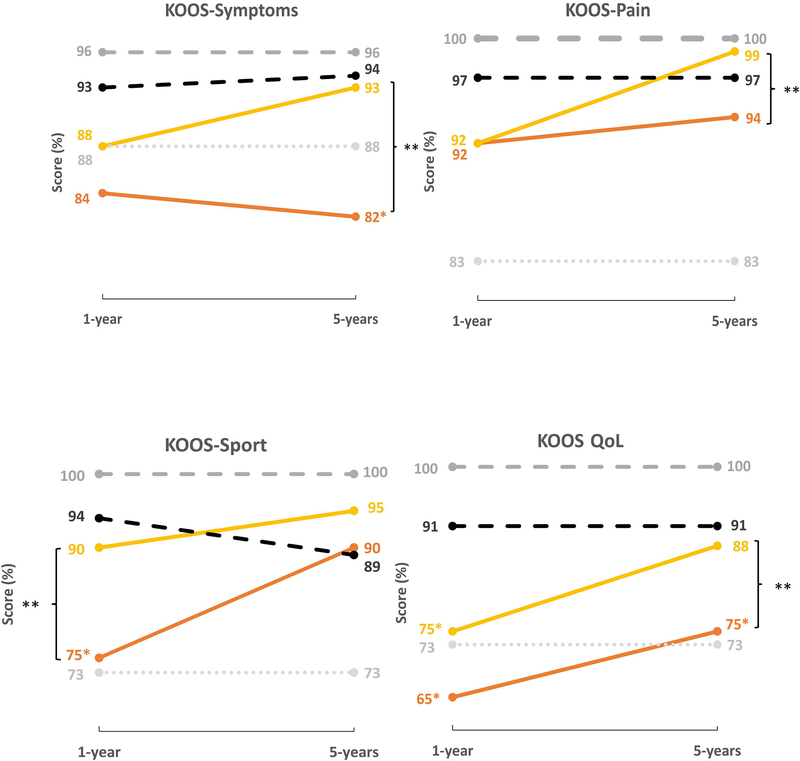
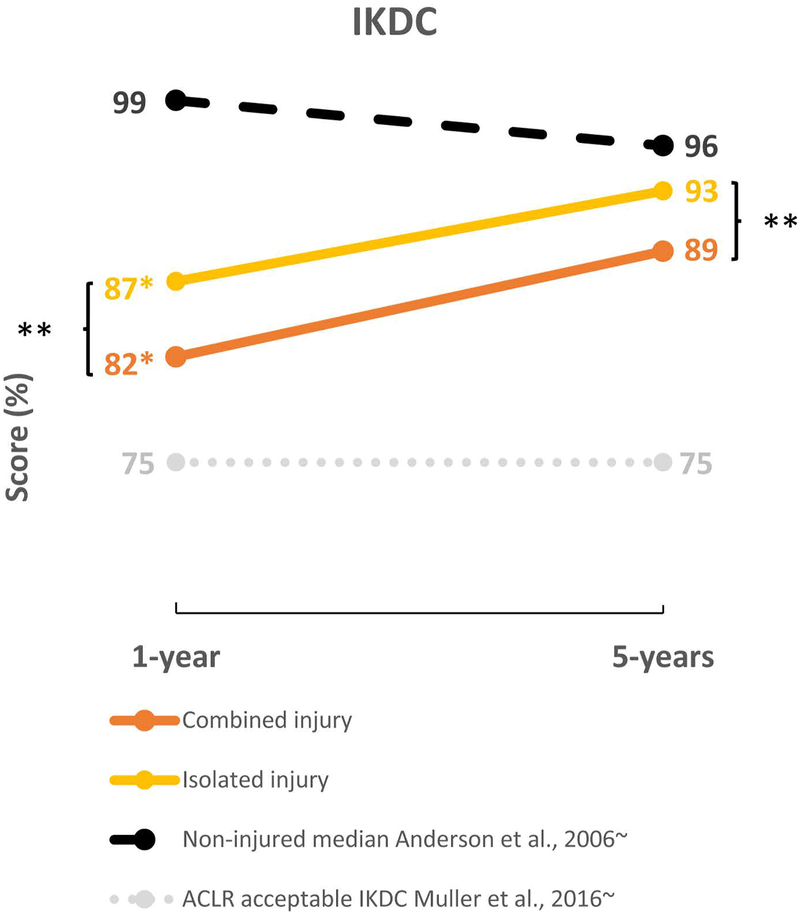
At 1-year post-ACLR, individuals in the combined injury group had significantly worse KOOS-Sport and IKDC scores (median difference (IQR): 15(4.6) and 5.0(3.5), respectively) (p<0.05). At 5-years all PROs (except KOOS-Sport) were significantly worse in the combined injury group. The median differences (IQR) were as follows; KOOS-Pain 5.0(2.5), KOOS-Symptoms 11.0(4.2), KOOS-QoL 13.0(4.6) and IKDC 4.0(3.2). KOOS and IKDC scores at 1- and 5-years for both groups are presented in Figure 2. The entire cohort (n=81) demonstrated significant (p<0.05) improvement (i.e. less knee symptoms, better function and QoL) between 1- and 5-years for all KOOS subscales (except KOOS-Symptoms) and IKDC. The mean change ±standard deviation for each subscale was; Pain: 2.8±9; Symptoms: 0.5±16.1; Sport: 6.0±18.2; QoL: 10.0±18.9 and IKDC 4.7±10.9. Improvement between 1- and 5-years did not differ between the combined and isolated groups (p≥0.05). At 5-years, the combined injury group median scores for KOOS-Symptoms and KOOS-QoL subscales were 14- and 25-points below age-matched normative values from non-injured young adults [34], which is greater than the recommended MDC (14–20 points) for individuals with an ACL injury [31]. Supplementary File 2 presents PROs for all groups at 1- and 5-years, and crude p-values for between-group analyses.
Figure 2.
A. Comparison between isolated and combined ALCR groups, non-injured and general population medians, and acceptable cut-off scores in ACLR individuals for the KOOS^
B. Comparison between isolated and combined ALCR groups, non-injured median values and acceptable cut-off scores in ACLR individuals for the IKDC^
^All values are presented as medians at 1-year and 5-years. Supplementary File 2 presents interquartile range values and scores for the entire group (n=81). At 1-year; n=40 combined, n=41 isolated. At 5-years; n=46 combined, n=35 isolated.
KOOS=Knee Osteoarthritis Outcome Score, IKDC=International Knee Documentation Committee knee evaluation
*Indicates median value at 1-year or 5-years is ≥minimal detectable change (MDC) [26, 31] below the general population (age-matched, non-injured) normative medians for the KOOS [32] and IKDC [34]
**Represents statistically significant difference (p<0.05) between combined and isolated injury groups at 1- or 5-years.
~ Weighted average median values for the KOOS and IKDC were calculated using respective healthy non-injured (no history of knee pain) data [32], general population (may have history of knee pain) age and sex-matched data [33, 34] and “acceptable” cut-off scores in ACLR individuals [6, 35].
The number of individuals above the “acceptable” cut-off for the KOOS subscales and the IKDC are presented in Table 2. A significantly lower percentage of combined injury individuals reported acceptable IKDC scores at 1-year, and KOOS-Symptoms, KOOS-Pain, KOOS-QoL, and IKDC scores at 5-years. These significant relationships persisted in the sensitivity analysis, which excluded the 10 participants with reinjury between 1- and 5-years (Supplementary File 5).
Table 2.
Number of participants with “acceptable” KOOS and IKDC scores~
| Number (%) Acceptable | Between-group differences^ | ||||
|---|---|---|---|---|---|
| Outcome Measure (acceptable cut-off score) | Group* | 1-year | 5-years | 1-year | 5-years |
| KOOS-Pain (88) | Whole group | 63 (78) | 66 (81) | 0.601 | 0.010 |
| Isolated | 33 (80) | 33 (94) | |||
| Combined | 30 (75) | 33 (72) | |||
| KOOS-Symptoms (83) | Whole group | 47 (58) | 47 (58) | 0.180 | 0.042 |
| Isolated | 27 (66) | 25 (71) | |||
| Combined | 20 (50) | 22 (48) | |||
| KOOS-Sport (73) | Whole group | 60 (75) | 69 (85) | 0.455 | 0.060 |
| Isolated | 32 (78) | 33 (94) | |||
| Combined | 28 (70) | 36 (78) | |||
| KOOS-QoL (73) | Whole group | 38 (47) | 55 (68) | 0.268 | 0.004 |
| Isolated | 22 (54) | 30 (86) | |||
| Combined | 16 (40) | 25 (54) | |||
| IKDC (75) | Whole group | 62 (77) | 71 (88) | 0.004 | 0.004 |
| Isolated | 37 (90) | 35 (100) | |||
| Combined | 25 (63) | 36 (78) | |||
Reported as the number of individuals (%) in the group with a raw score above “acceptable” cut-offs using previously published data in ACLR individuals for the KOOS [6] and IKDC [35].
KOOS=Knee injury and Osteoarthritis Outcome Score, IKDC=International Knee Documentation Committee knee evaluation.
Whole group at 1- and 5-years n=81. Participants were defined as a combined injury at 1- and 5-years if they had a concomitant injury (significant cartilage defects/meniscectomy assessed at the time of surgery). At 5-years individuals were added to the combined injury group if they had a new injury/surgery to the ACLR knee. All other participants were defined as having an isolated injury. At 1-year; n=40 combined, n=41 isolated. At 5-years; n=46 combined, n=35 isolated.
Fisher’s exact test was used to compare the proportions of the isolated and combined groups above the acceptable cut-off value. Values in bold represent p<0.05.
Association between cartilage defects, BMLs and meniscal lesions identified on MRI and PROs
There were no significant cross-sectional associations between cartilage defects, BMLs, or meniscal lesions, and KOOS or IKDC scores at 1-year. The presence of a patellofemoral cartilage defect at 1-year was significantly associated with worse KOOS-Symptoms (β: −9.79; 95%CI:-16.67, −2.91; p=0.006), KOOS-Sport (β: −7.94; 95%CI:-15.27, −0.61; p=0.034), KOOS-QoL (β: −8.29; 95%CI:-15.28, −1.29; p=0.021), and IKDC (β: −4.79; 95%CI:-9.34, −0.24; p=0.039) scores at 5-years (Table 3). The presence of a meniscal lesion at 1-year was significantly associated with worse KOOS-Symptoms at 5-years (β = −8.47, 95%CI:-16.54, −0.42; p=0.039). Similarly, at 5-years, the presence of a patellofemoral cartilage defect or meniscal tear was associated with worse PROs, and tibiofemoral BMLs were associated with better PROs (Table 3). Regression analysis was also performed without adjustment for age at time of surgery, sex, BMI at 1-year, and presence of combined injury. The unadjusted analysis resulted in larger effect sizes, and increased number of significant relationships (Supplementary File 6), suggesting these factors somewhat influence PROs following ACLR. Sensitivity analyses excluding 10 participants with reinjury between 1- and 5-years resulted in similar effect sizes (but wider confidence intervals), suggesting that the effect of reinjury on the relationship between lesions on MRI and PROs in this study was minimal (Supplementary File 5).
Table 3.
Multivariable linear regression analysis of MRI-OA features associated with PROs at 1- and 5-years post-ACLR~
| 1-year MRI-OA features^ (% with feature)# | 1-year PROs* | ||||
|---|---|---|---|---|---|
| KOOS-Symp | KOOS-Pain | KOOS-Sport | KOOS-QoL | IKDC | |
| PF Any Cartilage (45) | −0.87 (−6.35, 4.62) |
−0.37 (−4.18, 3.43) |
2.69 (−3.77, 9.14) |
5.34 (−2.20, 12.89) |
−0.03 (−4.47, 4.52) |
| PF Any BML (23) | −1.73 (−7.78, 4.31) |
−1.87 (−6.04, 2.30) |
−6.39 (−13.39, 0.61) |
−3.01 (−11.26, 5.24) |
−1.02 (−5.96, 3.92) |
| TF Any Cartilage (48) | 2.81 (−2.33, 7.94) |
1.25 (−2.32, 4.83) |
−0.93 (−7.02, 5.16) |
2.69 (−4.45, 9.85) |
2.52 (−1.68, 6.74) |
| TF Any BML (31) | 0.86 (−4.71, 6.44) |
1.03 (−2.81, 4.90) |
−0.26 (−6.81, 6.29) |
−0.17 (−7.79, 7.45) |
1.03 (−3.52, 5.58) |
| Meniscal lesion (72) | −1.61 (−5.96, 9.17) |
−1.06 (−6.66, 4.54) |
−2.92 (−12.61 6.77) |
1.42 (−9.74, 12.58) |
−3.29 (−10.07, 3.48) |
| 1-year MRI-OA features^ (% with feature)# | 5-year PROs** | ||||
| KOOS-Symp | KOOS-Pain | KOOS-Sport | KOOS-QoL | IKDC | |
| PF Any Cartilage (46) |
−9.79
(−16.67, −2.91) |
−2.88 (−6.62, 0.86) |
−7.94
(−15.27, −0.61) |
−8.29
(−15.28, −1.29) |
−4.79
(−9.34, −0.24) |
| PF Any BML (26) | −4.60 (−12.02, 2.81) |
−1.28 (−6.44, 2.36) |
−2.49 (−10.32, 5.34) |
1.82 (−5.63, 9.27) |
−1.62 (−6.39, 3.15) |
| TF Any Cartilage (47) | −5.32 (−11.84, 1.20) |
−1.26 (−4.73, 2.19) |
0.47 (−6.39, 7.34) |
1.95 (−4.67, 8.58) |
0.24 (−4.09, 4.58) |
| TF Any BML (30) | 0.12 (−6.89, 7.13) |
1.97 (−1.67, 5.62) |
3.46 (−3.79, 10.73) |
−0.94 (−7.97, 6.09) |
1.06 (−3.48, 5.61) |
| Meniscal lesion (79) |
−8.47
(−16.54, −0.42) |
−0.99 (−5.33, 3.34) |
−0.44 (−8.21, 9.10) |
−5.19 (−13.41, 3.04) |
−3.74 (−9.07, 1.58) |
| 5-year MRI-OA features^ (% with feature)# | 5-year PROs* | ||||
| KOOS-Symp | KOOS-Pain | KOOS-Sport | KOOS-QoL | IKDC | |
| PF Any Cartilage (58) |
−6.86
(−13.49, −0.24) |
−2.49 (−6.78, 1.79) |
−3.99 (−11.06, 3.07) |
−11.71
(−19.08, −4.33) |
−3.86 (−9.08, 1.36) |
| PF Any BML (22) | −1.19 (−8.77, 6.40) |
−0.74 (−5.96, 4.46) |
2.12 (−10.03, 5.79) |
−0.99 (−9.78, 7.80) |
−4.36 (−10.16, 1.44) |
| TF Any Cartilage (56) | −3.23 (−9.93, 3.45) |
−0.16 (−4.10, 4.42) |
1.53 (−5.48, 8.56) |
6.83 (−0.78, 14.45) |
4.23 (−0.89, 9.36) |
| TF Any BML (27) | 3.26 (−4.23, 10.76) |
4.19 (−0.47, 8.85) |
9.32
(1.79, 16.86) |
11.84
(3.60, 20.07) |
6.89
(1.28, 12.49) |
| Meniscal lesion (81) |
−9.12
(−17.41, −0.82) |
−1.81 (−7.23, 3.61) |
−1.66 (−10.62, 7.29) |
−3.74 (−13.64, 6.16) |
−4.10 (−10.69, 2.49) |
Values represent coefficient and 95% confidence interval. Values in bold represent p<0.05.
1-year MRI associations with 1-year PROs, n=111; for 1-year MRI association with 5-year PROs, n=80 (n=1 no MRI assessment at 1-year); for 5-year MRI associations with 5-year PROs, n=73 (n=2 no MRI at 5-years; n=5 no BMI (covariate) assessment at 5-years). Refer to Figure 1 for participant recruitment into current study.
MRI=magnetic resonance imaging; OA=osteoarthritis; PROs = patient-reported outcomes; KOOS=Knee injury and OA Outcome Score; IKDC= International Knee Documentation Committee knee evaluation; QoL=quality of life; PF= patellofemoral; TF=tibiofemoral; BML=bone marrow lesion;
Cartilage, BMLs and meniscal lesions were graded as present if ≥grade 1 in size as per the MRI OA Knee Score (MOAKS). Meniscal lesions include any type of tear, maceration or extrusion ≥grade 1 in either the medial or lateral tibiofemoral compartment.
Adjusted for age, sex, body mass index, presence of a combined injury. Unadjusted results are reported in Supplementary File 6.
Adjusted for age, sex, body mass index, presence of a combined injury and baseline KOOS and IKDC values. Unadjusted results are reported in Supplementary File 6.
DISCUSSION
Despite improvement in KOOS and IKDC scores between 1- and 5-years following ACLR, individuals with a combined injury (i.e., concomitant meniscectomy and/or arthroscopic chondral defect at the time of ACLR and/or secondary injury/surgery to ACL knee) had worse PROs at 5-years post-ACLR, compared to those with an isolated injury. At 5-years, a lower proportion of individuals with combined injury met previously reported “acceptable” PRO scores for ACLR individuals [6], and presented with worse PRO scores compared to healthy non-injured populations. In the second part of our analysis, MRI findings had minimal association with PROs at 1- and 5-years, except for patellofemoral cartilage defects at 1-year, which were associated with worse KOOS-Symptoms, KOOS-Sport, KOOS-QoL, and IKDC scores at 5-years. Patellofemoral cartilage defects on MRI at 1- and 5 years were generally associated with worse KOOS and IKDC scores at 5-years. The only other MRI findings to be associated with PROs were meniscal lesions at 1 and 5 years (worse KOOS-Symptoms at 5 years), and tibiofemoral BMLs at 5 years (better KOOS-Sport, KOOS-QOL and IKDC at 5 years).
At an entire group level, all PROs except KOOS-Symptoms improved from 1- to 5-years post-ACLR. Although improvements did not exceed known clinically meaningful change scores for the KOOS [36] or IKDC [37], all KOOS subscales and IKDC entire group median scores at 5-years were near normative values (within MDC score [26, 31]) when compared to the general population [33, 34]. Whilst group-level scores for most KOOS subscales and IKDC in the combined and isolated injury group at 5-years exceeded patient acceptable symptom state (PASS) cut-off values for ACLR populations [6, 35] (Figure 2), our novel analysis (Table 3) identified many individuals within the group did not achieve PASS values. Up to 42% (range: 0–42%; average: 22%) of all participants had not recovered to KOOS or IKDC PASS values at 5-years. Deficits were most evident for the KOOS-Symptom and KOOS-QoL subscales, in which 42% and 32% of participants (whole group) had not recovered to PASS values at 5-years, respectively. Entire group PRO scores in ACLR cohorts should be interpreted with caution, as they may depict successful outcomes, and do not necessarily represent the widespread disparity and considerably poor outcomes observed in some individuals.
Individuals with a combined injury demonstrate worse PROs at 1-year, and a greater deficit at 5-years, compared to those with an isolated ACLR and non-injured peers. KOOS-Symptoms and KOOS-QoL subscales were particularly impaired in those with a combined injury at 5-years, being 14- and 25-points below normative values [32], respectively. The proportion of people with acceptable scores on all of the KOOS subscales and IKDC improved from 1- to 5-years in the combined (1-year: 40–75%; average: 60%, 5-year: 48–78%; average 66%) and isolated groups (1-year: 54–90%; average 73%, 5-year: 71–100%; average 89%). This is consistent with previous reports that one-third of individuals have unacceptable symptoms 2-years post-ACLR [6, 10]. The combined injury group had a higher proportion of people not achieving PASS values for KOOS-Pain, -Symptoms and -QoL and IKDC scores at 5-years. Specifically, the KOOS-Symptoms and KOOS-QoL subscales in the combined injury group had the greatest proportion (52% and 46%, respectively) of individuals who had not recovered to PASS values. These results may assist clinical interpretation of PROs following ACLR. Clinicians can identify individuals with an acceptable outcome based on PASS scores [6], and provide education on realistic expectations of recovery for different patient groups. Clinicians should be cognisant approximately half of patients with a combined injury may not achieve an acceptable outcome for symptoms or QoL 5-years post-ACLR. Further research is needed to determine if targeted secondary prevention interventions can address current and potential future symptoms, functional and participation restrictions.
Our findings extend previous research reporting worse PROs in the presence of a combined injury in the short- (injury to 1-year) [1, 3] and long-term (15+ years) [8], confirming this relationship in the medium-term. Interventions targeting symptoms and QoL should be a high priority for individuals with a combined ACL-injury. This may include additional pre-operative education and potentially ongoing intervention beyond 1-year post-ACLR to enable achievement of similar outcomes to those with isolated injuries. The combined injury group was significantly older, and had a higher BMI at 1-year, therefore addressing potential negative lifestyle modifications, including physical inactivity [38] and weight gain [39] which could be associated with poorer QoL following ACLR [7, 22] may be important. Such interventions are beneficial in older adults with established knee OA [40, 41], but further high quality trials are required to determine efficacy in younger individuals with post-traumatic knee OA following ACLR.
Overall, we found minimal cross-sectional associations between tibiofemoral or patellofemoral cartilage defects, BMLs, meniscal lesions, and PROs between 1- and 5-years post-ACLR. These findings extend previous reports of no association between tibiofemoral radiographic OA with PROs in the longer-term [12, 13]. However, consistent with our 3-year follow-up PRO data [22], patellofemoral cartilage defects at 1-year were associated with worse KOOS-Symptoms, KOOS-Sport, KOOS-QoL, and IKDC scores at 5-years post-ACLR. Additionally, patellofemoral cartilage defects at 5-years were cross-sectionally associated with worse KOOS-Symptoms and KOOS-QoL. Whilst clinicians should consider the patellofemoral compartment as a potential source of symptoms and driver of poorer function following hamstring-autograft ACLR [21, 42], education to patients should express that MRI findings are often unrelated to symptoms.
We recently reported that one-third of individuals will have worsening BMLs between 1- and 5-years post-ACLR [18]. An interesting finding of this current analysis in the same cohort was that the presence of tibiofemoral BMLs were associated with better KOOS-Sport, KOOS-QoL, and IKDC at 5-years. This could indicate that BMLs reflect increased joint loading due to participation in sport, particularly in the presence of poor function [43]. The future symptomatic consequences of BMLs following ACLR are unknown, but in individuals at risk of OA (i.e. older, higher BMI), worsening BMLs predicted subsequent knee symptoms, progression of MRI-OA features, and radiographic OA 4–7 years later [17, 44]. Further research is required to understand the long term implications of BMLs on MRI in an ACLR population, and measure the response of individual joint features and PROs to potential interventions.
Our follow-up rate of the original 1-year cohort was 72%, which may introduce some selection bias. However, there were no differences in baseline participant or surgical characteristics between those participating and lost to follow-up (Supplementary File 4), and the current cohort had similar IKDC scores [1] and return to sport rates [5] to other larger ACLR cohorts at comparable follow-up time points. The combined injury group included 10 individuals who sustained a secondary injury between 1- and 5-years, which could influence results. Yet, sensitivity analyses excluding these 10 participants showed that the association between combined injury and PROs at 5 years, and relationship between cartilage, bone marrow and meniscal lesions and PROs at 5 years, were generally similar to the results from the whole cohort (Supplementary File 5). Slightly smaller effect sizes with wider confidence intervals were typically observed in this sensitivity analysis, likely due to the lower sample size and participants with a secondary injury reporting more symptoms at 5 years. Finally, regression findings should be interpreted cautiously, wide confidence intervals observed in the regression analysis were likely driven by a wide range in scores, and the multiple factors which may influence PROs.
In conclusion, individuals with a combined injury following ACLR may be an important subgroup requiring additional interventions, considering likely worse outcomes compared to their peers with an isolated ACLR. Individuals with patellofemoral cartilage defects may also require more targeted interventions due to the association with worse symptoms, function, and QoL at 5-years post-ACLR. Despite tibiofemoral BMLs being associated with fewer knee function and QoL impairments at 5 years, there seems to be a minimal relationship between other compartment-specific cartilage, BMLs, and meniscal lesions identified on MRI, and patient-reported symptoms, function, and QoL.
Supplementary Material
SIGNIFICANCE AND INNOVATIONS.
Individuals with a combined injury or patellofemoral cartilage defect on MRI had worse 5-year patient-reported outcomes and may benefit from additional education and targeted interventions.
This study assists clinical interpretability of patient-reported outcomes: approximately half of all patients with a combined injury at 5-years post-ACLR do not achieve acceptable symptoms or QoL.
Meniscal lesions were the only tibiofemoral feature on MRI associated with worse patient-reported outcomes. Tibiofemoral BMLs were associated with better patient-reported outcomes – the long-term significance of these should be explored further in ACL injured populations.
ACKNOWLEDGEMENTS
Brooke Patterson was the recipient of the Felice Rosemary-Lloyd Travel Scholarship, which assisted with travel and data analysis to visit co-author JS at the University of Delaware. We thank Imaging @Olympic Park for obtaining all MRIs and Mr. Hayden Morris and Mr. Timothy Whitehead (orthopaedic surgeons) for assisting recruitment into the project. The authors thank the participants, and Olympic Park Sports Medicine Centre for use of their facility for data collection.
FINANCIAL SUPPORT
Support for this study was provided by Arthritis Australia, La Trobe University Sport, Exercise and Rehabilitation Research Focus Area, the Queensland Orthopaedic Physiotherapy Network, the University of Melbourne (Research Collaboration grant), and the University of British Columbia Centre for Hip Health and Mobility (Society for Mobility and Health). Brooke Patterson is a recipient of a National Health and Medical Research Council (NHMRC) post-graduate scholarship. (No. 1114296). Adam Culvenor’s work is supported by a National Health and Medical Research Council (NHMRC) of Australia Early Career Fellowship (Neil Hamilton Fairley Clinical Fellowship No. 1121173). Joshua Stefanik’s (JS) work is supported by a NIH/NIGMS grant U54-GM104941. The sponsors were not involved in the design and conduct of this study, in the analysis and interpretation of the data, and in the preparation, review, or approval of the manuscript
Footnotes
Potential conflict of interest:
Ali Guermazi is a shareholder of Boston Imaging Core Lab (BICL), LLC, and a consultant to MerckSerono, Pfizer, GE Healthcare, Galapagos, Roche and TissueGene. No other authors declare a conflict of interest.
REFERENCES
- 1.Cox CL, Huston LJ, Dunn WR, Reinke EK, Nwosu SK, Parker RD, Wright RW, Kaeding CC, Marx RG, Amendola A et al. : Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med 2014, 42(5):1058–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spindler KP, Huston LJ, Wright RW, Kaeding CC, Marx RG, Amendola A, Parker RD, Andrish JT, Reinke EK, Harrell FE Jr. et al: The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med 2011, 39(2):348–359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ahlden M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J: The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med 2012, 40(10):2230–2235. [DOI] [PubMed] [Google Scholar]
- 4.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS: A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med 2010, 363(4):331–342. [DOI] [PubMed] [Google Scholar]
- 5.Ardern CL, Taylor NF, Feller JA, Webster KE: Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 2014, 48(21):1543–1552. [DOI] [PubMed] [Google Scholar]
- 6.Ingelsrud LH, Granan LP, Terwee CB, Engebretsen L, Roos EM: Proportion of Patients Reporting Acceptable Symptoms or Treatment Failure and Their Associated KOOS Values at 6 to 24 Months After Anterior Cruciate Ligament Reconstruction: A Study From the Norwegian Knee Ligament Registry. Am J Sports Med 2015. [DOI] [PubMed] [Google Scholar]
- 7.Filbay SR, Crossley KM, Ackerman IN: Activity preferences, lifestyle modifications and re-injury fears influence longer-term quality of life in people with knee symptoms following anterior cruciate ligament reconstruction: a qualitative study. J Physiother 2016, 62(2):103–110. [DOI] [PubMed] [Google Scholar]
- 8.Risberg MA, Oiestad BE, Gunderson R, Aune AK, Engebretsen L, Culvenor A, Holm I: Changes in Knee Osteoarthritis, Symptoms, and Function After Anterior Cruciate Ligament Reconstruction: A 20-Year Prospective Follow-up Study. Am J Sports Med 2016, 44(5):1215–1224. [DOI] [PubMed] [Google Scholar]
- 9.Rotterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Aroen A: Effect of meniscal and focal cartilage lesions on patient-reported outcome after anterior cruciate ligament reconstruction: a nationwide cohort study from Norway and Sweden of 8476 patients with 2-year follow-up. Am J Sports Med 2013, 41(3):535–543. [DOI] [PubMed] [Google Scholar]
- 10.Barenius B, Forssblad M, Engstrom B, Eriksson K: Functional recovery after anterior cruciate ligament reconstruction, a study of health-related quality of life based on the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc 2013, 21(4):914–927. [DOI] [PubMed] [Google Scholar]
- 11.Oiestad BE, Holm I, Aune AK, Gunderson R, Myklebust G, Engebretsen L, Fosdahl MA, Risberg MA: Knee function and prevalence of knee OA after ACLR: a prospective study with 10–15 years follow-up. Am J Sports Med 2010, 38(11):2201–2210. [DOI] [PubMed] [Google Scholar]
- 12.Lohmander LS, Ostenberg A, Englund M, Roos H: High prevalence of knee osteoarthritis, pain, and functional limitations in female soccer players twelve years after anterior cruciate ligament injury. Arthritis Rheum 2004, 50(10):3145–3152. [DOI] [PubMed] [Google Scholar]
- 13.Oiestad BE, Holm I, Engebretsen L, Risberg MA: The association between radiographic knee OA and knee symptoms, function and quality of life 10–15 years after ACLR. Br J Sports Med 2011, 45(7):583–588. [DOI] [PubMed] [Google Scholar]
- 14.Hunter DJ, Zhang W, Conaghan PG, Hirko K, Menashe L, Li L, Reichmann WM, Losina E: Systematic review of the concurrent and predictive validity of MRI biomarkers in OA. Osteoarthritis Cartilage 2011, 19(5):557–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang Y, Nevitt M, Niu J, Lewis C, Torner J, Guermazi A, Roemer F, McCulloch C, Felson DT: Fluctuation of knee pain and changes in bone marrow lesions, effusions, and synovitis on magnetic resonance imaging. Arthritis Rheum 2011, 63(3):691–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Felson DT, Chaisson CE, Hill CL, Totterman SM, Gale ME, Skinner KM, Kazis L, Gale DR: The association of bone marrow lesions with pain in knee osteoarthritis. Ann Intern Med 2001, 134(7):541–549. [DOI] [PubMed] [Google Scholar]
- 17.Felson DT, Niu J, Guermazi A, Roemer F, Aliabadi P, Clancy M, Torner J, Lewis CE, Nevitt MC: Correlation of the development of knee pain with enlarging bone marrow lesions on magnetic resonance imaging. Arthritis Rheum 2007, 56(9):2986–2992. [DOI] [PubMed] [Google Scholar]
- 18.Patterson BE, Culvenor AG, Barton CJ, Guermazi A, Stefanik JJ, Morris HG, Whitehead TS, Crossley KM: Worsening Knee Osteoarthritis Features on Magnetic Resonance Imaging 1 to 5 Years After Anterior Cruciate Ligament Reconstruction. Am J Sports Med 2018:363546518789685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Costa-Paz M, Muscolo DL, Ayerza M, Makino A, Aponte-Tinao L: Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy 2001, 17(5):445–449. [DOI] [PubMed] [Google Scholar]
- 20.Hanypsiak BT, Spindler KP, Rothrock CR, Calabrese GJ, Richmond B, Herrenbruck TM, Parker RD: Twelve-year follow-up on anterior cruciate ligament reconstruction: long-term outcomes of prospectively studied osseous and articular injuries. Am J Sports Med 2008, 36(4):671–677. [DOI] [PubMed] [Google Scholar]
- 21.Culvenor AG, Lai CC, Gabbe BJ, Makdissi M, Collins NJ, Vicenzino B, Morris HG, Crossley KM: Patellofemoral OA is prevalent and associated with worse symptoms and function after hamstring tendon autograft ACL reconstruction. Br J Sports Med 2014, 48(6):435–439. [DOI] [PubMed] [Google Scholar]
- 22.Culvenor AG, Collins NJ, Guermazi A, Cook JL, Vicenzino B, Whitehead TS, Morris HG, Crossley KM: Early Patellofemoral Osteoarthritis Features One Year After Anterior Cruciate Ligament Reconstruction: Symptoms and Quality of Life at Three Years. Arthritis Care Res (Hoboken) 2016, 68(6):784–792. [DOI] [PubMed] [Google Scholar]
- 23.Culvenor AG, Collins NJ, Guermazi A, Cook JL, Vicenzino B, Khan KM, Beck N, van Leeuwen J, Crossley KM: Early knee osteoarthritis is evident one year following anterior cruciate ligament reconstruction: a magnetic resonance imaging evaluation. Arthritis Rheumatol 2015, 67(4):946–955. [DOI] [PubMed] [Google Scholar]
- 24.Grindem H, Eitzen I, Snyder-Mackler L, Risberg MA: Online registration of monthly sports participation after anterior cruciate ligament injury: a reliability and validity study. Br J Sports Med 2014, 48(9):748–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Outerbridge RE: The etiology of chondromalacia patellae. J Bone Joint Surg Br 1961, 43-B:752–757. [DOI] [PubMed] [Google Scholar]
- 26.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM: Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res (Hoboken) 2011, 63 Suppl 11:S208–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS: Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. Br J Sports Med 2015, 49(10):700. [DOI] [PubMed] [Google Scholar]
- 28.Gudbergsen H, Bartels EM, Krusager P, Waehrens EE, Christensen R, Danneskiold-Samsoe B, Bliddal H: Test-retest of computerized health status questionnaires frequently used in the monitoring of knee osteoarthritis: a randomized crossover trial. BMC Musculoskelet Disord 2011, 12:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nguyen J, Marx R, Hidaka C, Wilson S, Lyman S: Validation of electronic administration of knee surveys among ACL-injured patients. Knee Surg Sports Traumatol Arthrosc 2017, 25(10):3116–3122. [DOI] [PubMed] [Google Scholar]
- 30.Hunter DJ, Guermazi A, Lo GH, Grainger AJ, Conaghan PG, Boudreau RM, Roemer FW: Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthritis Cartilage 2011, 19(8):990–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Collins NJ, Prinsen CA, Christensen R, Bartels EM, Terwee CB, Roos EM: Knee Injury and Osteoarthritis Outcome Score (KOOS): systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage 2016, 24(8):1317–1329. [DOI] [PubMed] [Google Scholar]
- 32.Cameron KL, Thompson BS, Peck KY, Owens BD, Marshall SW, Svoboda SJ: Normative values for the KOOS and WOMAC in a young athletic population: history of knee ligament injury is associated with lower scores. Am J Sports Med 2013, 41(3):582–589. [DOI] [PubMed] [Google Scholar]
- 33.Paradowski PT, Bergman S, Sunden-Lundius A, Lohmander LS, Roos EM: Knee complaints vary with age and gender in the adult population. Population-based reference data for the Knee injury and Osteoarthritis Outcome Score (KOOS). BMC Musculoskelet Disord 2006, 7:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ, International Knee Documentation C: The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med 2006, 34(1):128–135. [DOI] [PubMed] [Google Scholar]
- 35.Muller B, Yabroudi MA, Lynch A, Lai CL, van Dijk CN, Fu FH, Irrgang JJ: Defining Thresholds for the Patient Acceptable Symptom State for the IKDC Subjective Knee Form and KOOS for Patients Who Underwent ACL Reconstruction. Am J Sports Med 2016, 44(11):2820–2826. [DOI] [PubMed] [Google Scholar]
- 36.Roos EM, Lohmander LS: The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 2003, 1:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, Richmond JC, Shelborne KD: Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 2001, 29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 38.Daniel DM, Stone ML, Dobson BE, Fithian DC, Rossman DJ, Kaufman KR: Fate of the ACL-injured patient. A prospective outcome study. Am J Sports Med 1994, 22(5):632–644. [DOI] [PubMed] [Google Scholar]
- 39.Whittaker JL, Woodhouse LJ, Nettel-Aguirre A, Emery CA: Outcomes associated with early post-traumatic osteoarthritis and other negative health consequences 3–10 years following knee joint injury in youth sport. Osteoarthritis Cartilage 2015, 23(7):1122–1129. [DOI] [PubMed] [Google Scholar]
- 40.Skou ST, Pedersen BK, Abbott JH, Patterson B, Barton C: Physical Activity and Exercise Therapy Benefits More Than Just Symptoms and Impairments in People With Hip and Knee Osteoarthritis. J Orthop Sports Phys Ther 2018:1–36. [DOI] [PubMed] [Google Scholar]
- 41.Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL: Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev 2015, 1:CD004376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Culvenor AG, Crossley KM: Patellofemoral Osteoarthritis: Are We Missing an Important Source of Symptoms After Anterior Cruciate Ligament Reconstruction? J Orthop Sports Phys Ther 2016, 46(4):232–234. [DOI] [PubMed] [Google Scholar]
- 43.Culvenor AG, Patterson BE, Guermazi A, Morris HG, Whitehead TS, Crossley KM: Accelerated return to sport after ACL reconstruction and early knee osteoarthritis features at 1 year: an exploratory study. PM R 2017. [DOI] [PubMed] [Google Scholar]
- 44.Sharma L, Nevitt M, Hochberg M, Guermazi A, Roemer FW, Crema M, Eaton C, Jackson R, Kwoh K, Cauley J et al. : Clinical significance of worsening versus stable preradiographic MRI lesions in a cohort study of persons at higher risk for knee osteoarthritis. Ann Rheum Dis 2016, 75(9):1630–1636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Daniel DM, Malcom LL, Losse G, Stone ML, Sachs R, Burks R: Instrumented measurement of anterior laxity of the knee. J Bone Joint Surg Am 1985, 67(5):720–726. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.