Abstract
Background:
Black patients and older adults are less likely to receive minimally invasive hernia repair. These differences by race and age may be influenced by surgeon-specific utilization rate of minimally invasive repair. In this study, we explored the association between race, age, and surgeon utilization of minimally invasive surgery (MIS) with the likelihood of receiving MIS inguinal hernia repair.
Methods:
A retrospective cohort study was performed in patients undergoing elective primary inguinal hernia repair from 2012-2016, using data from the Michigan Surgical Quality Collaborative, a 72-hospital clinical registry. Surgeons were stratified by proportion of MIS performed. Using hierarchical logistic regression models, we investigated the association between receiving MIS repair and race, age, and surgeon MIS utilization rate.
Results:
Out of 4,667 patients, 1253 (27%) received MIS repair. Out of 190 surgeons, 81 (43%) performed only open repair. Controlling for surgeon MIS utilization, race was not associated with MIS receipt (OR 0.93, p=0.775), but older patients were less likely to receive MIS repair (OR 0.41, p<0.001).
Conclusions:
Race differences were explained by surgeon MIS utilization, implicating access to MIS-performing surgeon as a mediator. Conversely, age disparity was independent of MIS utilization, even after adjusting for comorbidities, indicating some degree of provider bias against performing MIS repair in older patients. Interventions to address disparities should include systematic efforts to improve access, as well as provider and patient education for older adults.
Keywords: inguinal hernia repair, laparoscopy, surgical technology, robotic inguinal hernia repair, minimally invasive surgery, surgical disparity
Introduction
Disparities in care for underrepresented minorities and older adults are well established, and minimally invasive surgery (MIS) is no exception. Black patients are less likely than white patients to undergo laparoscopic hysterectomy or colectomy, while older adults are less likely than younger patients to receive MIS for appendectomy and cholecystectomy.[1-5] These disparities are accentuated in inguinal hernia repair, where MIS adoption is already low. At present, only 20 – 25% of all inguinal hernias are repaired with minimally invasive surgery (MIS) in North America, compared to rates upwards of 40% in cholecystectomy, ventral hernia repair, foregut surgery, and colectomy.[6-8] In a previous population-based study of inguinal hernia repair, we found that older patients and black patients were less likely to receive MIS repair.[9] These differences are significant considering the advantages of MIS, including earlier return to work, decreased postoperative pain, and lower rates of chronic groin pain.[10-17]
While many studies describe disparities surgical care delivery, few explore possible mechanisms perpetuating healthcare inequity for underrepresented minorities and older adults. It is unclear whether disparities in MIS receipt persist due to issues with healthcare access versus surgeon bias (i.e., differences in care based on patient characteristics). For instance, in the case of inguinal hernia repair, considerable surgeon-level variation in MIS utilization may contribute to access inequities.[9] Conversely, if older adults or black patients are still less likely to receive MIS even if seen by a surgeon who performs MIS repair, this may represent bias, whether intentional or unconscious. A study investigating whether disparities persist after controlling for surgeon MIS utilization would help distinguish between access and bias.
In this context, we aimed to understand why disparities in MIS inguinal hernia repair exist by analyzing the relationship between demographic factors (age and race) and surgeon MIS utilization in the likelihood of receiving MIS repair. We hypothesized that, accounting for surgeon MIS utilization, disparities in MIS repair by age and race would be eliminated, indicating that these observed disparities resulted from differential access to MIS-performing surgeons.
Methods
Overview
This was a retrospective cohort study using data from the Michigan Surgical Quality Collaborative (MSQC), a payer-funded consortium of 72 hospitals. The MSQC maintains a robust clinical registry of patient characteristics, perioperative processes of care, and 30-day outcomes for general surgery, vascular surgery, and gynecology operations. Approximately 90% of eligible hospitals in Michigan participate, representing 50,000 cases a year. Trained nurses review patient charts and abstract clinical data. Cases are sampled according to a predetermined protocol to reduce selection bias, and these cases are weighted to represent the total cases in the population. Further details of data collection and follow-up are described in more detail in prior work.[18] As determined by the University of Michigan Institutional Review Board (IRB), MSQC data has patient identifiers removed, and this study was considered ‘Not Regulated.’[18, 19]
Study Population
We included adult patients who had an elective open or MIS inguinal hernia repair from January 1, 2012 to December 31, 2016 (CPT codes 49505, 49525, 49650). We excluded urgent and emergent cases, recurrent cases (CPT codes 49651, 49651) operations for strangulation or gangrene (CPT codes 49507, 49521), and bilateral repairs (defined as cases that had another inguinal hernia repair CPT code listed as a concurrent procedure). Since we aimed to investigate surgeon practice patterns, we then excluded patients from surgeons who performed fewer than 10 cases.
Surgeon Stratification by MIS Utilization
MIS utilization was defined for each surgeon as their proportion of MIS repairs over total repairs in their practice. For example, a surgeon who performed half of their repairs using MIS would have a 50% MIS utilization.
Outcome and Predictor Variables
The outcome of interest was the likelihood of receiving MIS repair. Predictors of interest included previously identified factors resulting in healthcare disparity: age (<45 years, 45 – 64 years, 65+ years) and race (white, black, other), as well as surgeon MIS utilization.[9] Other patient covariates included sex, insurance type (private, Medicare, Medicaid, self-pay, uninsured, and other), obesity (BMI >30 kg/m2), tobacco use within 1 year, history of alcohol abuse, functional status (independent, partially dependent, totally dependent), American Society of Anesthesiologists (ASA) classification, and comorbid conditions including diabetes, chronic obstructive pulmonary disease, hypertension, congestive heart failure, peripheral vascular disease, ascites, history of corticosteroid therapy, >10% body weight loss, and geographic region.
To define geographic regions in Michigan, we used the 2010 Hospital Referral Regions (HRRs) from the Dartmouth Atlas of Heath Care. [20] HRRs are geographic regions that represent where patients are referred for major cardiovascular surgical and neurosurgical procedures, using Medicare data. They reflect regional referral areas for tertiary healthcare and have been used to study healthcare utilization.
Analysis
We used a hierarchical logistic regression model of the likelihood of a patient receiving MIS repair, with predictor variables of race, age, surgeon MIS utilization, and the patient covariates listed above. As patients are clustered within surgeons, a hierarchical model allowed us to control for patient factors as well as surgeon-level clustering of patients. Our model included all patient and hospital covariates with a Pearson’s Chi-squared test result of p<0.10. All analyses were performed using StataSE version 14 (College Station, Texas).
Results
Characteristics of the Cohort
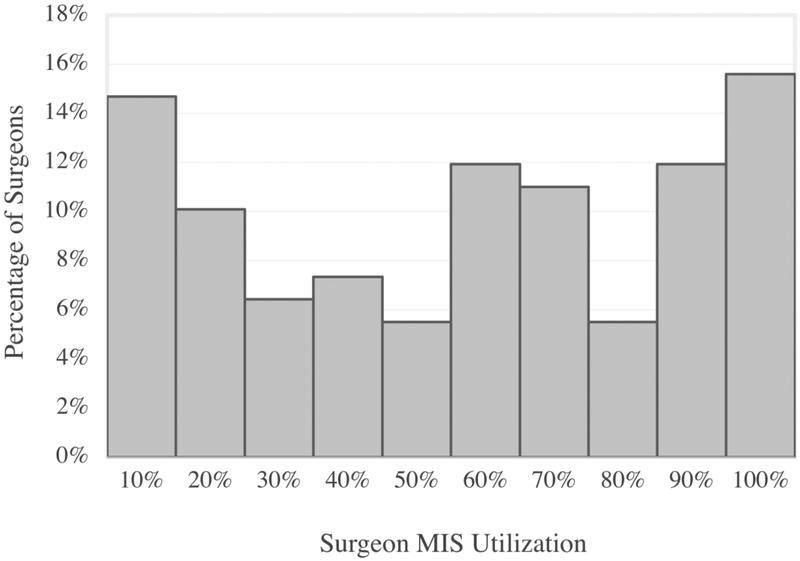
Between 2012 and 2016, a total of 4,667 primary, unilateral inguinal hernia repairs that met inclusion criteria were identified, representing 60% of eligible cases within the state. In total, patients from 71 hospitals and 190 surgeons were included in this analysis. Overall, 1253 (27%) of patients received an MIS repair. Demographic data stratified between open and MIS repair are shown in Table 1. The age distribution between the two groups was different, with a higher proportion of young (ages 18 – 44 and 45 – 64) patients receiving MIS repair. A higher proportion of white patients received MIS repair, and patients also differed with respect to COPD, hypertension, and ASA class. When surgeons were stratified by MIS utilization, we found that 81 (43%) surgeons performed only open inguinal hernia repair, with an MIS utilization of 0. The distribution of surgeons by MIS utilization is shown in Figure 1.
Table 1.
Patient Characteristics by open or MIS repair.
| Characteristics | Open N (%) |
MIS N (%) |
p-value |
|---|---|---|---|
| Cases, n | 3414 (73) | 1253 (27) | |
| Age | <0.001 | ||
| <= 44 | 661 (19) | 324 (26) | |
| 45 – 64 | 1484 (43) | 602 (48) | |
| >=65 | 1269 (37) | 327 (26) | |
| Gender | 0.41 | ||
| Male | 3090 (91) | 1144 (91) | |
| Female | 324 (9) | 109 (9) | |
| Race | 0.10 | ||
| White | 2979 (87) | 1096 (87) | |
| Black | 269 (8) | 80 (6) | |
| Insurance Type | <0.001 | ||
| Medicare | 332 (10) | 135 (11) | |
| Medicaid | 1092 (32) | 274 (22) | |
| Private | 1908 (56) | 791 (63) | |
| Other | 54 (2) | 34 (3) | |
| Self-pay | 4 (0.1) | 0 (0) | |
| Uninsured | 24 (0.7) | 19 (2) | |
| Region | <0.001 | ||
| Ann Arbor | 773 (23) | 269 (21) | |
| Detroit | 1101 (32) | 515 (41) | |
| Grand Rapids | 775 (23) | 264 (21) | |
| Lansing | 351 (10) | 57 (5) | |
| Saginaw | 295 (9) | 36 (3) | |
| Traverse City | 119 (4) | 1102 (9) | |
| Obesity | 0.25 | ||
| Obese | 653 (19) | 239 (19) | |
| Not Obese | 2759 (81) | 1011 (81) | |
| Unknown | 2 (0.06) | 3 (0.2) | |
| Tobacco Use | 783 (23) | 323 (26) | 0.04 |
| Alcohol Use | 123 (4) | 58 (5) | 0.11 |
| Functional Status: Not Independent | 20 (1) | 7 (1) | 0.95 |
| ASA Class: 3 - 4 | 997 (29) | 266 (21) | <0.001 |
| Diabetes | 313 (9) | 108 (9) | 0.56 |
| Chronic Obstructive Pulmonary Disease | 215 (6) | 40 (3) | <0.001 |
| Hypertension | 1440 (42) | 439 (35) | <0.001 |
| Congestive Heart Failure | 8 (0.2) | 1 (0.1) | 0.29 |
| Peripheral Vascular Disease | 58 (2) | 14 (1) | 0.15 |
| History of Corticosteroid Therapy | 49 (1) | 12 (1) | 0.20 |
| > 10% Body Weight Loss | 10 (0.3) | 1 (0.1) | 0.31 |
| Bleeding Disorder | 57 (2) | 19 (2) | 0.71 |
Figure 1.
Legend. Distribution of MIS utilization in surgeons who performed any MIS (109 surgeons).
Age and Race Disparities Adjusted for Surgeon MIS Utilization
Consistent with previous results, we found that black patients (OR 0.72, 95% CI 0.56 – 0.99, p=0.030) and patients aged 65 and older (OR 0.67, 95% CI 0.52 – 0.87, p=0.002) were less likely than white patients and patients aged 44 and younger to receive MIS repair on regression analysis controlling for clinical factors. However, when the model controlled for surgeon MIS utilization, the association between race and MIS receipt was no longer seen (OR 0.94, 95% CI 0.61 – 1.46, p=0.788) (Table 2). However, the decreased association of receiving MIS with older age remained (OR 0.41, 95% CI 0.28 – 0.61, p<0.001).
Table 2.
Hierarchical logistic regression model of the likelihood of receiving MIS hernia repair based on patient factors and surgeon MIS utilization.
| Odds Ratio of Receiving MIS Repair |
P-value | 95% Confidence Interval | ||
|---|---|---|---|---|
| Age (ref group: <=44) | ||||
| 45-64 | 0.92 | 0.53 | 0.70 | 1.21 |
| >=65 | 0.41 | <0.001 | 0.28 | 0.61 |
| Race (ref group: White) | ||||
| Black | 0.94 | 0.79 | 0.61 | 1.46 |
| % MIS utilization (ref group: 0-10% | ||||
| 11-20% | 18.85 | <0.001 | 11.31 | 31.43 |
| 21-30% | 34.87 | <0.001 | 20.11 | 60.46 |
| 31-40% | 64.56 | <0.001 | 38.88 | 107.21 |
| 41-50% | 91.72 | <0.001 | 57.05 | 147.46 |
| 51-61% | 163.61 | <0.001 | 101.22 | 264.46 |
| 61-70% | 243.28 | <0.001 | 147.64 | 400.86 |
| 71-80% | 362.77 | <0.001 | 189.08 | 696.04 |
| 81-90% | 833.13 | <0.001 | 475.03 | 1461.16 |
| 91-100% | 3475.71 | <0.001 | 1746.17 | 6918.31 |
| ASA Class 3-4 | 0.53 | <0.001 | 0.40 | 0.69 |
| COPD | 0.61 | 0.05 | 0.37 | 0.99 |
Surgeon % MIS utilization (as a continuous variable) was predictive of the likelihood of a patient receiving MIS. For every 10% increase in a surgeon’s MIS utilization, a patient’s likelihood of receiving MIS increased by 8% (95% CI 6.6% – 9.4%, p<0.001). Patients with ASA class 3 or 4 had lower rate of MIS repair compared to patients with lower ASA class (OR 0.53, 95% CI 0.40 – 0.69, p<0.001). Patients with COPD also had lower likelihood of receiving MIS (OR 0.61, 95% CI 0.37 – 0.99, p=0.045). There were no differences on multivariate analysis in MIS utilization with respect to gender, geographic region, obesity, or tobacco use.
Discussion
In this population-based study, we examined the relationship between patient demographics and surgeon practice to characterize disparities in receiving MIS inguinal hernia repair. The race disparity in MIS repair was no longer seen when controlling for surgeon MIS utilization. In other words, this difference in MIS receipt in black patients was mediated by between, rather than within-surgeon differences in MIS utilization. Surgeons likely do not offer MIS repair differently to black patients versus white patients; instead, the observed disparity may be related to access to surgeons who perform MIS. This finding is similar to a population-based study of mortality after emergency general surgery procedures, which found that higher mortality in black patients was related to decreased access to hospitals with good outcomes. [21] In contrast, older patients were still less likely than younger patients to receive MIS repair even after adjusting for surgeon MIS utilization, meaning that older patients who accessed high-MIS surgeons still experienced bias based on their age.
These findings indicate that surgeon bias, in addition to clinical indication, may play an important role in age disparity in MIS repair, especially as our study adjusted for comorbid conditions that could approximate frailty, including ASA class and functional status. Even surgeons who frequently use MIS may be more conservative based on a perception of an older patient’s overall frailty, and may offer open repair or regional anesthesia to patients thought to be at higher anesthetic or urinary retention risk.[22] However, a healthy older patient may stand to benefit greatly from the decreased postoperative pain and quicker return to activities after an MIS repair. Additionally, previous studies demonstrate that octogenarians have equivalent clinical outcomes after MIS repair compared to younger patients, and these may reassure surgeons debating whether to offer MIS repair to older patients.[23-25] Surgeon-facing interventions, such as education or implicit bias awareness training, or efforts to educate patients to discuss surgical options with their surgeons, may help increase MIS use for older patients who are good candidates.
Our study is the first to indicate that racial disparities in receiving MIS techniques for inguinal hernia repair may be mainly related to lack of access to surgeons that offer MIS. However, these findings do not implicate only systemic factors. Provider behavior, such as differences in regional referral patterns to MIS-performing surgeons, may also make MIS less available for black patients. In other areas of surgical care, racial disparities are well-documented, particularly for procedures or technologies that are under provider discretion.[26] For example, black men with prostate cancer are more likely than white men to undergo watchful waiting as opposed to receiving definitive therapy, even with advanced prostate cancer and after adjusting for household income and other sociodemographic factors.[27, 28] Black men also receive fewer incontinence procedures after prostatectomy than white patients despite having more incontinence.[29] In peripheral vascular disease, black patients are less likely to undergo revascularization attempts and more likely to have amputations.[30] This difference is partially due to differential access to specialist surgeons that perform revascularization, but persist even among black and white patients at the same hospitals, indicating differential treatment by the provider at the patient level.[31, 32] When these disparities are discovered, understanding this distinction between access or bias will guide the design of appropriate interventions that address the underlying mechanism.
This study has several limitations, the most important one being the inherent selection bias of observational studies. While this study finds associations between age, race, and likelihood of receiving MIS repair, these findings do not imply that these factors have a causal effect on the outcome. For example, the observed age disparity may be partially explained by characteristics that surgeons use to estimate a patient’s frailty but are not captured in our data. However, we were able to adjust for many comorbidities that are often used to assess preoperative fitness, including functional status, ASA class, BMI, history of weight loss, COPD, and other comorbid conditions. A further limitation was that our data did not capture other possible reasons for offering open repair, including scrotal hernia, need to continue anti-platelet medications, or prior surgery (particularly prostatectomy, which would be more common in older patients). Confounding by clinical presentation may be present, with older and black patients possibly presenting with more severe hernias necessitating open repair.[33, 34] Additionally, our dataset did not include data on hernia attributes, such as defect size or existing contamination. We also did not collect surgeon attributes such as fellowship training or years in practice. Finally, MSQC hospitals voluntarily participate and are committed to quality improvement, limiting the generalizability of this study. However, the majority of the hospitals are community hospitals and the cohort represents a statewide population.
Conclusions
This population-based study revealed that older and black patients are less likely to receive MIS inguinal hernia repair, but the differences by race may be explained by a lack of access to surgeons offering MIS. Conversely, disparity for older adults persists even after adjusting for surgeon MIS utilization, and surgeons may have intentional or unconscious bias towards older patients, perceiving them as less fit for MIS. Financial incentives that encourage surgeons to practice in regions with lower socioeconomic status may boost access to surgical techniques, including MIS, but improving health care access alone will likely not mitigate the demonstrated disparity in older adults. In addition to healthcare delivery reform that improves access to care for vulnerable populations, surgeons should also be encouraged to identify and challenge any preconceived bias about patient fitness and should consider MIS where clinically appropriate.
Acknowledgments
Financial support: Dr. Vu receives funding from the National Institutes of Health Ruth L. Kirschstein National Research Service Award (1F32DK115340-01A1). Dr. Telem receives funding for this work from the Agency for Healthcare Research and Quality (AHRQ) (K08HS025778).
Footnotes
Institution where work originated: Department of Surgery, University of Michigan, Ann Arbor, MI 48105, USA
Disclosures: Dr. Vu, Ms. Gunaseelan, Dr. Dimick, Dr. Englesbe, and Dr. Campbell have no conflicts of interest or financial ties to report. Dr. Telem receives consulting fees for Medtronic.
References
- 1.Lassiter RL, et al. , Racial disparities in the use of laparoscopic surgery to treat colonic diverticulitis Are not fully explained by socioeconomics or disease complexity. The American Journal of Surgery, 2017. 213(4): p. 673–677. [DOI] [PubMed] [Google Scholar]
- 2.Alnasser M, et al. , National disparities in laparoscopic colorectal procedures for colon cancer. Surg Endosc, 2014. 28(1): p. 49–57. [DOI] [PubMed] [Google Scholar]
- 3.Patel PR, et al. , Disparities in Utilization of Laparoscopic Hysterectomies: A Nationwide Analysis. Journal of minimally invasive gynecology, 2014. 21(2): p. 223–227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Varela JE and Nguyen NT, Disparities in access to basic laparoscopic surgery at U.S. academic medical centers. Surg Endosc, 2011. 25(4): p. 1209–14. [DOI] [PubMed] [Google Scholar]
- 5.Tucker JJ, et al. , Laparoscopic cholecystectomy is safe but underused in the elderly. Am Surg, 2011. 77(8): p. 1014–20. [DOI] [PubMed] [Google Scholar]
- 6.Smink DS, Paquette IM, and Finlayson SR, Utilization of laparoscopic and open inguinal hernia repair: a population-based analysis. J Laparoendosc Adv Surg Tech A, 2009. 19(6): p. 745–8. [DOI] [PubMed] [Google Scholar]
- 7.Zendejas B, et al. , Trends in the utilization of inguinal hernia repair techniques: a population-based study. The American Journal of Surgery, 2012. 203(3): p. 313–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trevisonno M, et al. , Current practices of laparoscopic inguinal hernia repair: a population-based analysis. Hernia, 2015. 19(5): p. 725–733. [DOI] [PubMed] [Google Scholar]
- 9.Vu JV, et al. , Surgeon utilization of minimally invasive techniques for inguinal hernia repair: a population-based study. Surg Endosc, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ielpo B, et al. , A prospective randomized study comparing laparoscopic transabdominal preperitoneal (TAPP) versus Lichtenstein repair for bilateral inguinal hernias. The American Journal of Surgery, 2017. [DOI] [PubMed] [Google Scholar]
- 11.Bignell M, et al. , Prospective randomized trial of laparoscopic (transabdominal preperitoneal-TAPP) versus open (mesh) repair for bilateral and recurrent inguinal hernia: incidence of chronic groin pain and impact on quality of life: results of 10 year follow-up. Hernia, 2012. 16(6): p. 635–40. [DOI] [PubMed] [Google Scholar]
- 12.Bowling K, et al. , Laparoscopic and open inguinal hernia repair: Patient reported outcomes in the elderly from a single centre - A prospective cohort study. Ann Med Surg (Lond), 2017. 22: p. 12–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eker HH, et al. , Randomized clinical trial of total extraperitoneal inguinal hernioplasty vs lichtenstein repair: A long-term follow-up study. Archives of Surgery, 2012. 147(3): p. 256–260. [DOI] [PubMed] [Google Scholar]
- 14.McCormack K, et al. , Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev, 2003(1): p. Cd001785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Abbas AE, et al. , Patient-perspective quality of life after laparoscopic and open hernia repair: a controlled randomized trial. Surgical Endoscopy, 2012. 26(9): p. 2465–2470. [DOI] [PubMed] [Google Scholar]
- 16.Wang WJ, et al. , Comparison of the effects of laparoscopic hernia repair and Lichtenstein tension-free hernia repair. J Laparoendosc Adv Surg Tech A, 2013. 23(4): p. 301–5. [DOI] [PubMed] [Google Scholar]
- 17.Westin L, et al. , Less Pain 1 Year After Total Extra-peritoneal Repair Compared With Lichtenstein Using Local Anesthesia: Data From a Randomized Controlled Clinical Trial. Ann Surg, 2016. 263(2): p. 240–3. [DOI] [PubMed] [Google Scholar]
- 18.Hendren S, et al. , Antibiotic choice is independently associated with risk of surgical site infection after colectomy: a population-based cohort study. Ann Surg, 2013. 257(3): p. 469–75. [DOI] [PubMed] [Google Scholar]
- 19.Waits SA, et al. , Developing an argument for bundled interventions to reduce surgical site infection in colorectal surgery. Surgery, 2014. 155(4): p. 602–6. [DOI] [PubMed] [Google Scholar]
- 20.The Center for the Evaluative Clinical Sciences, D.M.S., The Dartmouth atlas of health care. 1996: Chicago, Ill: : American Hospital Publishing, [1996] ©1996. [Google Scholar]
- 21.Hall EC, et al. , Racial/ethnic disparities in emergency general surgery: explained by hospital-level characteristics? The American Journal of Surgery, 2015. 209(4): p. 604–609. [DOI] [PubMed] [Google Scholar]
- 22.Patel JA, et al. , Risk factors for urinary retention after laparoscopic inguinal hernia repairs. Surg Endosc, 2015. 29(11): p. 3140–5. [DOI] [PubMed] [Google Scholar]
- 23.Hope WW, et al. , Comparing laparoscopic and open inguinal hernia repair in octogenarians. Hernia, 2013. 17(6): p. 719–22. [DOI] [PubMed] [Google Scholar]
- 24.Vigneswaran Y, et al. , Elderly and octogenarian cohort: Comparable outcomes with nonelderly cohort after open or laparoscopic inguinal hernia repairs. Surgery, 2015. 158(4): p. 1137–1144. [DOI] [PubMed] [Google Scholar]
- 25.Dallas KB, et al. , Laparoscopic versus open inguinal hernia repair in octogenarians: a follow-up study. Geriatr Gerontol Int, 2013. 13(2): p. 329–33. [DOI] [PubMed] [Google Scholar]
- 26.Haider AH, et al. , Racial Disparities in Surgical Care and Outcomes in the United States: A Comprehensive Review of Patient, Provider, and Systemic Factors. Journal of the American College of Surgeons, 2013. 216(3): p. 482–492.e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang EH, et al. , Disparities in Treatment of Patients With High-risk Prostate Cancer: Results From a Population-based Cohort. Urology, 2016. 95: p. 88–94. [DOI] [PubMed] [Google Scholar]
- 28.Ziehr DR, et al. , Income inequality and treatment of African American men with high-risk prostate cancer. Urol Oncol, 2015. 33(1): p. 18.e7–18.e13. [DOI] [PubMed] [Google Scholar]
- 29.Gupta S, et al. , Utilization of surgical procedures and racial disparity in the treatment of urinary incontinence after prostatectomy. Neurourol Urodyn, 2016. 35(6): p. 733–7. [DOI] [PubMed] [Google Scholar]
- 30.Holman KH, et al. , Racial disparities in the use of revascularization before leg amputation in Medicare patients. J Vasc Surg, 2011. 54(2): p. 420–6, 426.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dimick J, et al. , Black patients more likely than whites to undergo surgery at low-quality hospitals in segregated regions. Health Aff (Millwood), 2013. 32(6): p. 1046–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Regenbogen SE, et al. , Do differences in hospital and surgeon quality explain racial disparities in lower-extremity vascular amputations? Ann Surg, 2009. 250(3): p. 424–31. [DOI] [PubMed] [Google Scholar]
- 33.Beadles CA, Meagher AD, and Charles AG, Trends in emergent hernia repair in the united states. JAMA Surgery, 2015. 150(3): p. 194–200. [DOI] [PubMed] [Google Scholar]
- 34.Hernández-Irizarry R, et al. , Trends in emergent inguinal hernia surgery in Olmsted County, MN: a population-based study. Hernia, 2012. 16(4): p. 397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]