Abstract
BACKGROUND
High sodium and low potassium consumption are risk factors for hypertension. The objectives of this study were to describe usual daily intake of sodium and potassium among US Hispanics/Latinos of diverse background groups and estimate the proportion meeting guidelines for dietary sodium and potassium intake.
METHODS
We studied 16,171 participants of the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), a diverse group of self-identified Hispanics/Latinos aged 18–74 years from 4 US communities. In 2008–2011, all HCHS/SOL participants underwent a standardized examination. Median usual daily intake of dietary sodium and potassium were derived from two 24-hour diet recalls; standard errors and 95% confidence intervals (CIs) were calculated using boot strap methods. Meeting 2015 US Department of Agriculture guidelines was defined as an intake of <2,300 mg/day of sodium and ≥4,700 mg/day of potassium.
RESULTS
Among US Hispanics/Latinos, median usual daily intake of sodium was 2,574 mg (95% CI: 2,547, 2,600) among women and 3,747 mg (95% CI: 3,697, 3,796) among men. Median usual daily intake of potassium was 2,069 mg (95% CI: 2,046, 2,092) among women and 2,649 mg (95% CI: 2,615, 2,683) among men. Overall, only 21.3% (95% CI: 20.2%, 22.4%) of the US Hispanic/Latino population met 2015 recommendations for sodium and 0.6% (95% CI: 0.4%, 0.8%) for potassium.
CONCLUSIONS
Among US Hispanics/Latinos intake of sodium is too high and potassium too low. Strategies to reduce sodium intake while simultaneously increasing intake of potassium in this US population are warranted.
Keywords: blood pressure, Hispanics, hypertension, Latinos, potassium, recommendations, sodium
High dietary sodium and low dietary potassium are known risk factors for hypertension,1 a major contributor to cardiovascular disease (CVD) and the leading cause of death in the United States.2 The relationship between higher sodium and higher blood pressure (BP) has long been established,3 prompting the US Department of Agriculture (USDA) to recommend limiting sodium intake to <2,300 mg/day.4,5 Likewise, USDA dietary guidelines call for optimizing potassium intake to ≥4,700 mg/day.4 Yet, intake of sodium for most Americans far exceeds recommendations, whereas intake of potassium falls short—it is estimated that in the United States, mean sodium intake is 3,608 mg/day, whereas median potassium intake is 2,155 mg/day.6 As such, only 25%6 and 1.4%7 of the US population meet current USDA targets for sodium and potassium, respectively. In response to this public health challenge, a myriad of initiatives have focused on reducing sodium intake on a population level.8 Thus, on-going surveillance of population-based sodium and potassium intake is necessary to assess the scope of the issue and identify subgroups that may benefit from additional intervention.
Among US Hispanics/Latinos, a fast growing segment of the US population,9 the intake of sodium and potassium has not been fully characterized. For example, although results from National Health and Nutrition Examination Survey (NHANES), have described sodium and potassium intake among Mexican Americans (median of 3,251 mg/day and 2,586 mg/day respectively)7 and shown intake to be comparable to that of non-Hispanic Whites,6 the US Hispanic/Latino population is heterogeneous9 with varying dietary patterns10 and CVD burden.11 In fact, in contrast to findings among Mexican Americans, results from 2 studies in New York City,12–14 including a population-based study,12 showed that Hispanic/Latinos, mostly of Caribbean background, had significantly higher sodium12,14 and lower potassium13 intake than non-Hispanic/Latino Whites. Further, results from 447 participants enrolled in the Study of Latinos: Nutrition and Physical Activity Assessment Study (SOLNAS), a substudy of the Hispanic Community Health Study/Study of Latinos (HCHS/SOL), suggest there may be variation in measures of sodium and potassium intake by Hispanic/Latino background.15 However, given the difficulties in recruiting large samples of Hispanics/Latinos from diverse backgrounds, to date, no prior study has fully characterized and directly compared sodium and potassium intakes in a large population-based study of diverse Hispanics/Latinos. Further, it remains unknown what proportion of US Hispanics/Latinos meet sodium and potassium intake guidelines.
Therefore, using data from the HCHS/SOL study which enrolled more than 16,000 diverse US Hispanics/Latinos across 4 sites, we aimed to estimate, usual intake of sodium, potassium, and molar sodium-to-potassium (Na-K) ratio and to determine whether intake differs by Hispanic/Latino background group. We also aimed to estimate the proportion of the US Hispanic/Latino population meeting recommendations for sodium and potassium.
METHODS
Study population
The HCHS/SOL is a population-based study of 16,415 Hispanic/Latino community dwelling adults ages 18–74 at baseline (in 2008–2011).16 Participants were recruited from communities surrounding four field sites: Bronx, New York; Chicago, Illinois, Miami-Dade, Florida; and San Diego, California. A 2-stage area probability sample of households was selected with stratification and over-sampling at each stage in order to obtain a diverse sample representative of the Hispanic/Latino population across the 4 sites.17 Once selected and recruited, participants underwent a standardized examination between 2008 and 2011. Participants were asked to bring in their current medications for review, to undergo a clinical examination, have fasting blood samples collected, and answer a questionnaire pertaining to their medical histories and health behaviors, including two 24-hour diet recalls. All participants provided informed consent and the study was approved by each study site, coordinating center and reading center institutional review boards. Detailed study methods have been described elsewhere.16,17
Dietary sodium and potassium
Dietary sodium and potassium intake were assessed with two 24-hour dietary recalls. The first recall was collected during the in-person HCHS/SOL clinic interview;10 the second recall was collected via phone within 3 months of the first assessment. Depending on language preference, interviews were conducted in English or Spanish by a trained research assistant. A food-amounts booklet was given to all participants to quantify portion sizes. Using Nutrition Data System for Research software which uses the multiple-pass method18 and was developed by Nutrition Coordinating Center at the University of Minnesota, values for sodium (mg/day), and potassium (mg/day) were derived. The Nutrition Data System for Research software includes over 18,000 foods, 8,000 brand name products, including Hispanic/Latino foods. Of the full HCHS/SOL sample of 16,415 participants, 16,171 (99.5%) had at least one recall and 93.7% had two 24-hour diet recalls.
Measurement of covariates
HCHS/SOL participants reported their age, sex, self-identified Hispanic/Latino background (Central American, Cuban, Dominican, Mexican, Puerto Rican, or South American), educational attainment (<high school (HS), HS or equivalent, or >HS), income (<$20,000, $20,000–<$50,000, or $50,000 or more), nativity (US born, or foreign born, including Puerto Rico), whether they currently smoke, and whether they take dietary supplements.
Height in meters and weight in kilograms measured at the study visit were used to calculate body mass index (BMI, in kg/m2). After a 5-minute rest period, 3 seated BP measurements were taken using an automatic sphygmomanometer (OMRON HEM-907 L). All 3 measurements were averaged. Hypertension was defined according to recommendations at the time the study was conducted, as systolic BP ≥ 140 mm Hg or diastolic BP ≥ 90 mm Hg, or documented use of anti-hypertension medication through scanned medications.19 Diabetes status was defined as fasting plasma glucose ≥126 mg/dl, a 2-hour postload glucose level ≥200 mg/dl, A1C level ≥6.5%, or documented use of hypoglycemic agents.20 Chronic kidney disease (CKD) was defined as having an estimated glomerular filtration rate <60 ml/minute/1.73 m2.21
Meeting recommendations
The study was conducted 2008–2011 and the USDA updated its guidelines for sodium intake in 2015. Therefore, we considered both 2010 and 2015 guidelines to reflect (i) guidelines at the time the study was conducted and (ii) current guidelines. Meeting the 2010 USDA recommendations for sodium was defined as <2,300 mg/day in the general population, and <1,500 mg/day for individuals with clinically relevant characteristics which include those: age 51+, black, with hypertension, diabetes, or CKD.22 Given that among US Hispanics/Latinos, race is often conflated with ethnicity23 and was not consistently reported in the HCHS/SOL, we did not consider race as a clinically relevant characteristic for the current analysis. Meeting the 2015 USDA recommendation for sodium was defined as <2,300 mg/day for all.4 For potassium intake, meeting USDA recommendations was defined as ≥4,700 mg/day.22 We also considered the World Health Organization (WHO) potassium recommendation, a less stringent criteria, which was defined as potassium intake of ≥3,510 mg/day.24 Finally, although the USDA does not have a recommendation for dietary Na-K ratio, we considered the WHO recommendation of molar Na-K ratio no greater than 1.25
Statistical analyses
Before characterizing intake of sodium and potassium in the population, we first described sociodemographic and clinically relevant characteristics overall and by sex. These analyses accounted for the complex survey design and were weighted by nonresponse adjusted, trimmed, and calibrated to US 2010 Census in the target area.
Next, to examine usual intake of sodium and potassium, we used methods and SAS macros (version 2.1) developed by the National Cancer Institute (NCI) to estimate the distribution of ubiquitously consumed nutrients (i.e., consumed everyday). This methodology, described elsewhere,26 fits a nonlinear mixed model with a Box-Cox transformation to accommodate the skewness of the nutrient intake, and accounts for the within- and between-person variance components to correct for the high intraindividual variation intrinsic to 24-hour recalls. Using parameters estimated and Monte Carlo simulation, 100 pseudo-persons for each individual were generated to estimate the nutrient distribution stratifying by sex and Hispanic/Latino background, education, income, nativity, smoking status, supplement use, BMI group, and by clinically relevant characteristics (age >50 years, with hypertension, diabetes, or CKD). Because HCHS/SOL has a complex survey design, we used 100 bootstrap samples to estimate standard errors and calculate 95% confidence intervals (CI) around the parameter estimates generated by the NCI models. Non-overlapping confidence intervals were used to indicate whether parameter estimates significantly differed. The NCI method has been validated,27 and found to be superior to reporting mean nutrient intake.
We also plotted kernel density distributions of usual daily intake of sodium, potassium, and Na-K ratio from the 100 pseudo estimates derived from the Monte Carlo simulation. Distributions were plotted by sex and Hispanic/Latino background group. Finally, the NCI method, described earlier, was also used to estimate the proportion meeting recommendations for sodium, potassium, and Na-K ratio by Hispanic/Latino background and other clinically relevant characteristics. All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC) and R software.
RESULTS
Mean age was 41 years old. The study population was heterogeneous in terms of Hispanic/Latino background with 8% Central American, 21% Cuban, 10% Dominican, 39% Mexican, 17% Puerto Rican, and 5% South American (Table 1). Overall, 32% had less than a HS education, 42% had an income <$20,000 per year, 77% were foreign-born, 21% were smokers, and 42% took dietary supplements. About 40% of adults had a BMI ≥ 30 kg/m2, 28% were older than 50 years of age, 22% had hypertension, 15% had diabetes, and 4% had CKD. A total of 40% had at least one of the following clinically relevant characteristics: age 51+, hypertension, diabetes, or CKD.
Table 1.
Characteristics of the study population overall and by sex, HCHS/SOL, 2008–2011
| Overall (N = 16,171) | Women (n = 9,707) | Men (n = 6,464) | ||||
|---|---|---|---|---|---|---|
| Mean or % | SE | Mean or % | SE | Mean or % | SE | |
| Sociodemographic characteristics | ||||||
| Mean Age (years) | 41.0 | 0.2 | 41.8 | 0.3 | 40.2 | 0.3 |
| Hispanic/Latino background, % | ||||||
| Central American | 7.7 | 0.6 | 7.7 | 0.6 | 7.7 | 0.7 |
| Cuban | 20.9 | 1.7 | 19.1 | 1.6 | 22.7 | 1.9 |
| Dominican | 10.4 | 0.7 | 12.0 | 0.9 | 8.6 | 0.8 |
| Mexican | 39.1 | 1.7 | 39.8 | 1.7 | 38.3 | 1.9 |
| Puerto Rican | 16.7 | 0.8 | 15.9 | 0.9 | 17.6 | 1.0 |
| South American | 5.2 | 0.3 | 5.4 | 0.4 | 5.0 | 0.4 |
| Education, % | ||||||
| <High school | 32.2 | 0.7 | 32.7 | 0.8 | 31.7 | 0.9 |
| High school or equivalent | 28.2 | 0.6 | 26.3 | 0.7 | 30.3 | 0.8 |
| >High school | 39.6 | 0.8 | 41.0 | 1.0 | 38.0 | 1.0 |
| Income, % | ||||||
| <$20,000 | 41.9 | 0.9 | 45.7 | 0.9 | 37.8 | 1.2 |
| $20,000–<$50,000 | 37.2 | 0.7 | 34.7 | 0.8 | 39.9 | 1.0 |
| ≥$50,000 | 11.7 | 0.8 | 8.8 | 0.6 | 15.0 | 1.1 |
| Foreign born, % | 77.3 | 0.8 | 79.2 | 0.8 | 75.2 | 1.1 |
| Behavioral factors | ||||||
| Current smoker, % | 21.2 | 0.6 | 16.4 | 0.7 | 26.6 | 0.8 |
| Takes dietary supplements, % | 41.9 | 0.9 | 45.3 | 0.8 | 38.1 | 1.0 |
| Body mass index (kg/m2), % | ||||||
| Normal: <25 | 23.1 | 0.5 | 23.6 | 0.8 | 22.6 | 0.7 |
| Overweight: 25–29.9 | 37.3 | 0.7 | 34.1 | 0.7 | 40.8 | 0.9 |
| Obese: ≥30 | 39.6 | 0.7 | 42.3 | 0.9 | 36.6 | 0.9 |
| Clinically relevant characteristics | ||||||
| Age 51+, % | 28.2 | 0.6 | 30.1 | 0.7 | 26.0 | 0.8 |
| Hypertension, % | 21.8 | 0.6 | 21.6 | 0.7 | 22.0 | 0.8 |
| Diabetes, % | 14.6 | 0.4 | 15.6 | 0.6 | 13.6 | 0.6 |
| Chronic Kidney Disease, % | 4.2 | 0.3 | 4.4 | 0.3 | 4.0 | 0.3 |
| Age 51+, HTN, Diabetes, or CKD, % | 39.6 | 0.7 | 40.5 | 0.8 | 38.7 | 1.0 |
Abbreviations: CKD, chronic kidney disease; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; HTN, hypertension; SE, standard error.
Among women (Table 2), median usual daily intake of sodium was 2,574 mg (95% CI: 2,547, 2,600). Compared with women of Mexican background (2,534 mg/day; 95% CI: 2,489, 2,580), median usual daily sodium intake was higher among women of Central American (3,144 mg/day; 95% CI: 3,083, 3,206) and South American (2,731 mg/day; 95% CI: 2,635, 2,826) backgrounds, lower among women of Dominican (2,195 mg/day; 95% CI: 2,119, 2,270) and Puerto Rican (2,307 mg/day; 95% CI: 2,221, 2,393) backgrounds, and similar among women of Cuban background (2,490 mg/day; 95% CI: 2,390, 2,590). Among women, median usual daily intake of sodium was lower among nonsmokers and individuals with higher BMI.
Table 2.
Usual daily intake of sodium and potassium among US Hispanic/Latino women, overall and across sample characteristics, HCHS/SOL 2008–2011
| Sodium (mg/day) | Potassium (mg/day) | Molar sodium-to-potassium ratio | |||||
|---|---|---|---|---|---|---|---|
| n | Median | (95% CI) | Median | (95% CI) | Median | (95% CI) | |
| Overall | 9,707 | 2,574 | (2,547, 2,600) | 2,069 | (2,046, 2,092) | 2.30 | (2.28, 2.33) |
| Hispanic/Latino background | |||||||
| Central American | 1,029 | 3,144a | (3,083, 3,206) | 2,216 | (2,153, 2,279) | 2.59a | (2.52, 2.66) |
| Cuban | 1,238 | 2,490 | (2,390, 2,590) | 1,956a | (1,889, 2,022) | 2.31a | (2.23, 2.38) |
| Dominican | 952 | 2,195a | (2,119, 2,270) | 1,943a | (1,871, 2,015) | 2.30a | (2.22, 2.39) |
| Mexican (ref) | 3,997 | 2,534 | (2,489, 2,580) | 2,185 | (2,144, 2,225) | 2.10 | (2.06, 2.14) |
| Puerto Rican | 1,562 | 2,307a | (2,221, 2,393) | 1,756a | (1,703, 1,808) | 2.47a | (2.39, 2.54) |
| South American | 631 | 2,731a | (2,635, 2,826) | 2,167 | (2,098, 2,236) | 2.29a | (2.20, 2.37) |
| Education | |||||||
| <HS | 3,712 | 2,415a | (2,367, 2,463) | 1,976a | (1,941, 2,012) | 2.30 | (2.25, 2.35) |
| HS or equivalent | 2,334 | 2,738a | (2,679, 2,797) | 2,074 | (2,033, 2,115) | 2.44a | (2.38, 2.50) |
| >HS (ref) | 3,632 | 2,609 | (2,560, 2,659) | 2,148 | (2,110, 2,186) | 2.23 | (2.19, 2.27) |
| Income | |||||||
| <$20,000 | 4,564 | 2,524 | (2,487, 2,562) | 2,045 | (2,015, 2,076) | 2.32 | (2.28, 2.36) |
| $20,000–<$50,000 | 3,408 | 2,638 | (2,587, 2,688) | 2,151 | (2,109, 2,194) | 2.25 | (2.20, 2.30) |
| ≥$50,000 (ref) | 752 | 2,642 | (2,536, 2,748) | 2,154 | (2,073, 2,234) | 2.21 | (2.12, 2.29) |
| Nativity | |||||||
| Foreign born | 8,103 | 2,523 | (2,493, 2,554) | 2,116a | (2,090, 2,142) | 2.21a | (2.18, 2.23) |
| US born (ref) | 1,587 | 2,779 | (2,708, 2,850) | 1,906 | (1,858, 1,954) | 2.69 | (2.63, 2.76) |
| Smoking status | |||||||
| Current smoker | 1,460 | 2,718a | (2,620, 2,816) | 2,001 | (1,945, 2,057) | 2.54a | (2.45, 2.62) |
| Nonsmoker (ref) | 8,232 | 2,554 | (2,524, 2,584) | 2,089a | (2,064, 2,114) | 2.27 | (2.24, 2.30) |
| Dietary supplement | |||||||
| Yes | 4,864 | 2,541 | (2,500, 2,581) | 2,195a | (2,164, 2,227) | 2.11a | (2.07, 2.14) |
| No (ref) | 4,843 | 2,603 | (2,564, 2,641) | 1,968 | (1,939, 1,997) | 2.48 | (2.44, 2.52) |
| BMI (kg/m2) | |||||||
| Normal (ref) | 1,918 | 2,758 | (2,692, 2,823) | 2,170 | (2,114, 2,226) | 2.36 | (2.30, 2.42) |
| Overweight | 3,346 | 2,502a | (2,458, 2,546) | 2,074a | (2,037, 2,111) | 2.23a | (2.18, 2.27) |
| Obese | 4,412 | 2,534a | (2,488, 2,579) | 2,012a | (1,978, 2,046) | 2.34 | (2.29, 2.38) |
The intraindividual coefficient of variation (a measure of within person variance) was 25.6% for sodium, 21.4% for potassium, and 24.2% for sodium-to-potassium ratio. The inter-individual coefficient of variation (a measure of between person variance) was 45.9% for sodium, 40.3% for potassium, and 45.0% for sodium-to-potassium ratio. Abbreviations: CI, confidence intervals; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; HS, high school; Ref, reference.
a95% confidence intervals do not overlap and usual nutrient intake is statistically significantly different compared with the reference category.
Among men (Table 3), median usual daily intake of sodium was 3,747 mg (95% CI: 3,697, 3,796). Compared with men of Mexican background (3,585 mg/day; 95% CI: 3,498, 3,671), median usual daily sodium intake was higher among men of Central American (4,437 mg/day; 95% CI: 4,340, 4,534) and South American (3,881 mg/day; 95% CI: 3,704, 4,058) backgrounds, lower among men of Dominican background (3,335 mg/day; 95% CI: 3,192, 3,478) and similar among men of Cuban (3,615 mg/day; 95% CI: 3,465, 3,765) and Puerto Rican (3,525 mg/day; 95% CI: 3,400, 3,650) backgrounds. Among men, median usual daily sodium intake was lower in individuals with less education, nonsmokers, and with higher BMI.
Table 3.
Usual daily intake of sodium and potassium among US Hispanic/Latino men, overall and across sample characteristics, HCHS/SOL 2008–2011
| Sodium (mg/day) | Potassium (mg/day) | Molar sodium-to-potassium ratio | |||||
|---|---|---|---|---|---|---|---|
| n | Median | (95% CI) | Median | (95% CI) | Median | (95% CI) | |
| Overall | 6,464 | 3,747 | (3,697, 3,796) | 2,649 | (2,615, 2,683) | 2.61 | (2.29, 2.93) |
| Hispanic/Latino background | |||||||
| Central American | 679 | 4,437a | (4,340, 4,534) | 2,858 | (2,799, 2,917) | 2.83a | (2.75, 2.90) |
| Cuban | 1,081 | 3,615 | (3,465, 3,765) | 2,530a | (2,428, 2,631) | 2.63a | (2.54, 2.73) |
| Dominican | 502 | 3,335a | (3,192, 3,478) | 2,481a | (2,356, 2,605) | 2.53 | (2.39, 2.66) |
| Mexican (ref) | 2,424 | 3,585 | (3,498, 3,671) | 2,751 | (2,692, 2,811) | 2.37 | (2.31, 2.43) |
| Puerto Rican | 1,110 | 3,525 | (3,400, 3,650) | 2,317a | (2,245, 2,388) | 2.86a | (2.78, 2.94) |
| South American | 434 | 3,881a | (3,704, 4,058) | 2,635 | (2,492, 2,779) | 2.80a | (2.67, 2.93) |
| Education | |||||||
| <HS | 2,402 | 3,482a | (3,403, 3,561) | 2,529a | (2,477, 2,580) | 2.56 | (2.51, 2.61) |
| HS or equivalent | 1,806 | 3,837 | (3,727, 3,947) | 2,599a | (2,536, 2,662) | 2.72a | (2.65, 2.78) |
| >HS (ref) | 2,246 | 3,913 | (3,840, 3,987) | 2,803 | (2,749, 2,857) | 2.58 | (2.53, 2.63) |
| Income | |||||||
| <$20,000 | 2,540 | 3,703 | (3,623, 3,783) | 2,598 | (2,545, 2,651) | 2.66a | (2.60, 2.71) |
| $20,000–<$50,000 | 2,674 | 3,798 | (3,729, 3,868) | 2,712 | (2,663, 2,760) | 2.57 | (2.52, 2.63) |
| ≥ $50,000 (ref) | 836 | 3,773 | (3,643, 3,903) | 2,745 | (2,647, 2,842) | 2.49 | (2.41, 2.56) |
| Nativity | |||||||
| Foreign born | 5,224 | 3,713 | (3,663, 3,762) | 2,694a | (2,660, 2,728) | 2.53a | (2.50, 2.57) |
| US born (ref) | 1,234 | 3,879 | (3,755, 4,003) | 2,528 | (2,446, 2,611) | 2.87 | (2.78, 2.95) |
| Smoking status | |||||||
| Current smoker | 1,651 | 4,013a | (3,877, 4,150) | 2,703 | (2,629, 2,777) | 2.73a | (2.67, 2.80) |
| Nonsmoker (ref) | 4,793 | 3,670 | (3,625, 3,714) | 2,636 | (2,598, 2,675) | 2.57 | (2.53, 2.61) |
| Dietary supplement | |||||||
| Yes | 2,563 | 3,704 | (3,617, 3,791) | 2,750a | (2,696, 2,803) | 2.45a | (2.40, 2.50) |
| No (ref) | 3,901 | 3,774 | (3,707, 3,842) | 2,589 | (2,545, 2,633) | 2.71 | (2.66, 2.76) |
| BMI (kg/m2) | |||||||
| Normal (ref) | 1,349 | 3,989 | (3,883, 4,095) | 2,670 | (2,601, 2,739) | 2.72 | (2.65, 2.79) |
| Overweight | 2,704 | 3,632 | (3,562, 3,702) | 2,679 | (2,622, 2,736) | 2.52a | (2.47, 2.57) |
| Obese | 2,392 | 3,746a | (3,655, 3,836) | 2,618 | (2,567, 2,669) | 2.65 | (2.60, 2.70) |
The intraindividual coefficient of variation (a measure of within person variance) was 25.5% for sodium, 22.4% for potassium, and 22.8% for sodium-to-potassium ratio. The inter-individual coefficient of variation (a measure of between person variance) was 46.5% for sodium, 41.0% for potassium, and 41.8% for sodium-to-potassium ratio. Abbreviations: CI, confidence intervals; HCHS/SOL, Hispanic Community Health Study/Study of Latinos; HS, high school; Ref, reference.
a95% confidence intervals do not overlap and usual nutrient intake is statistically significantly different compared with the reference category.
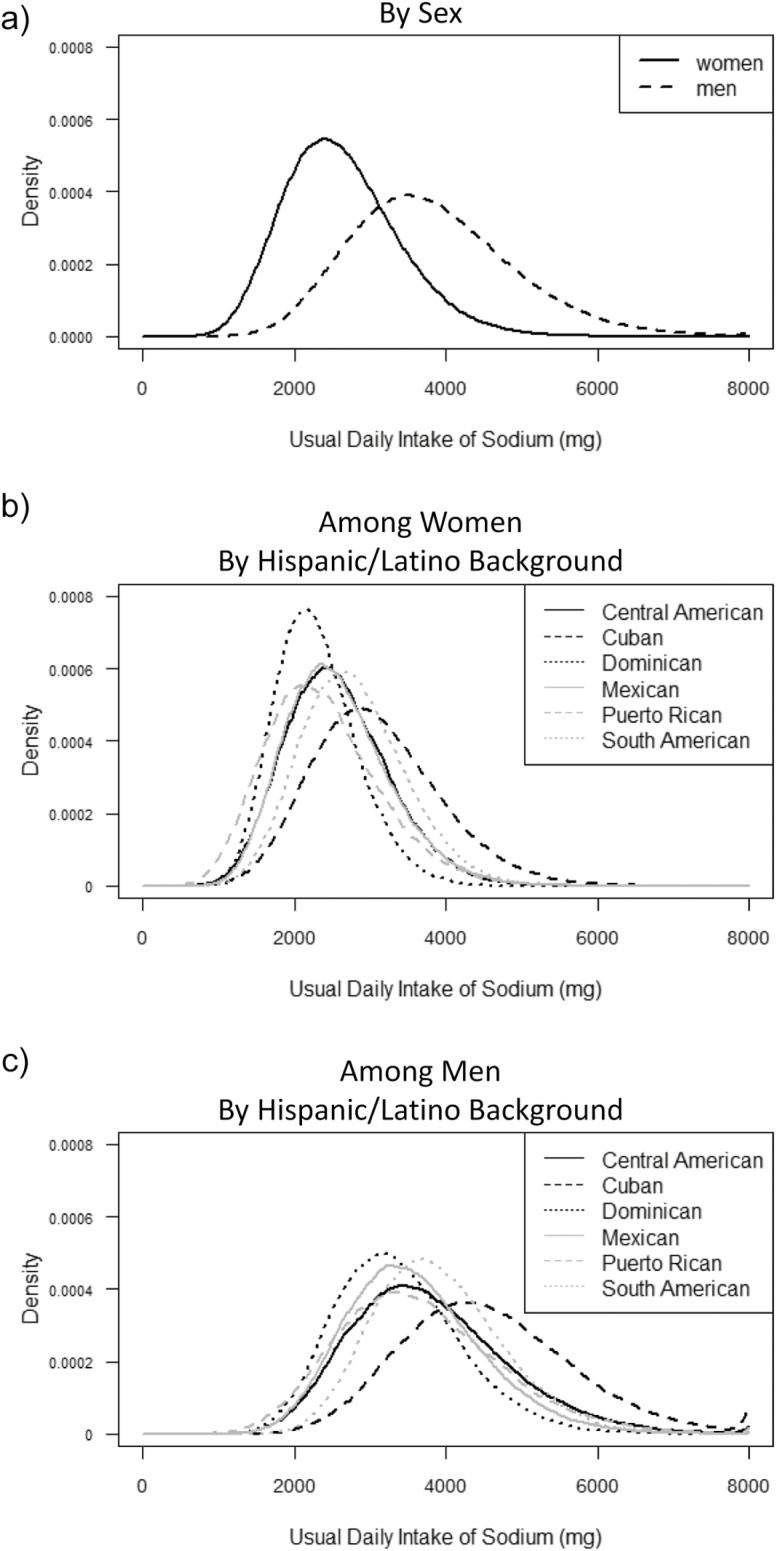
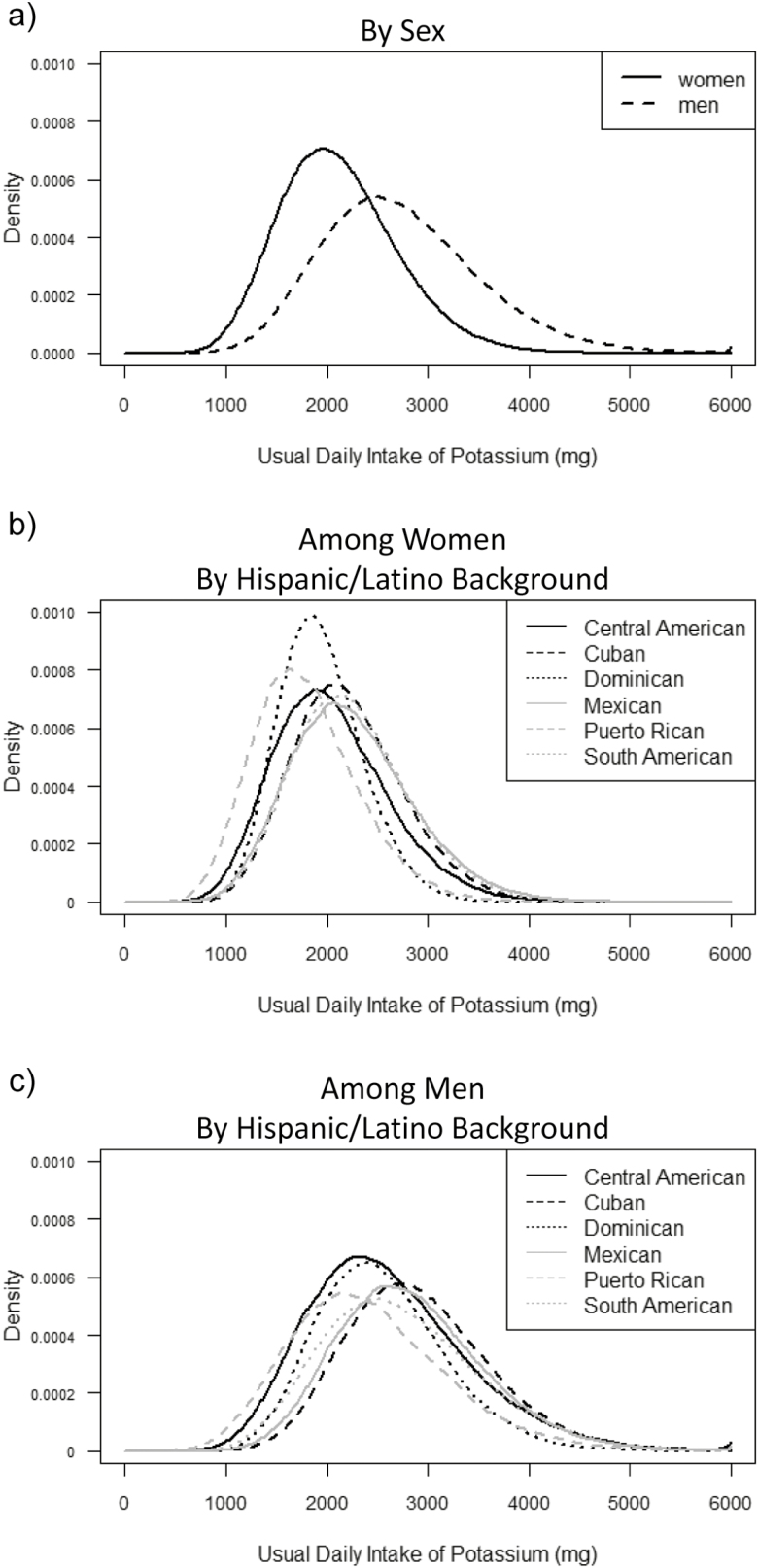
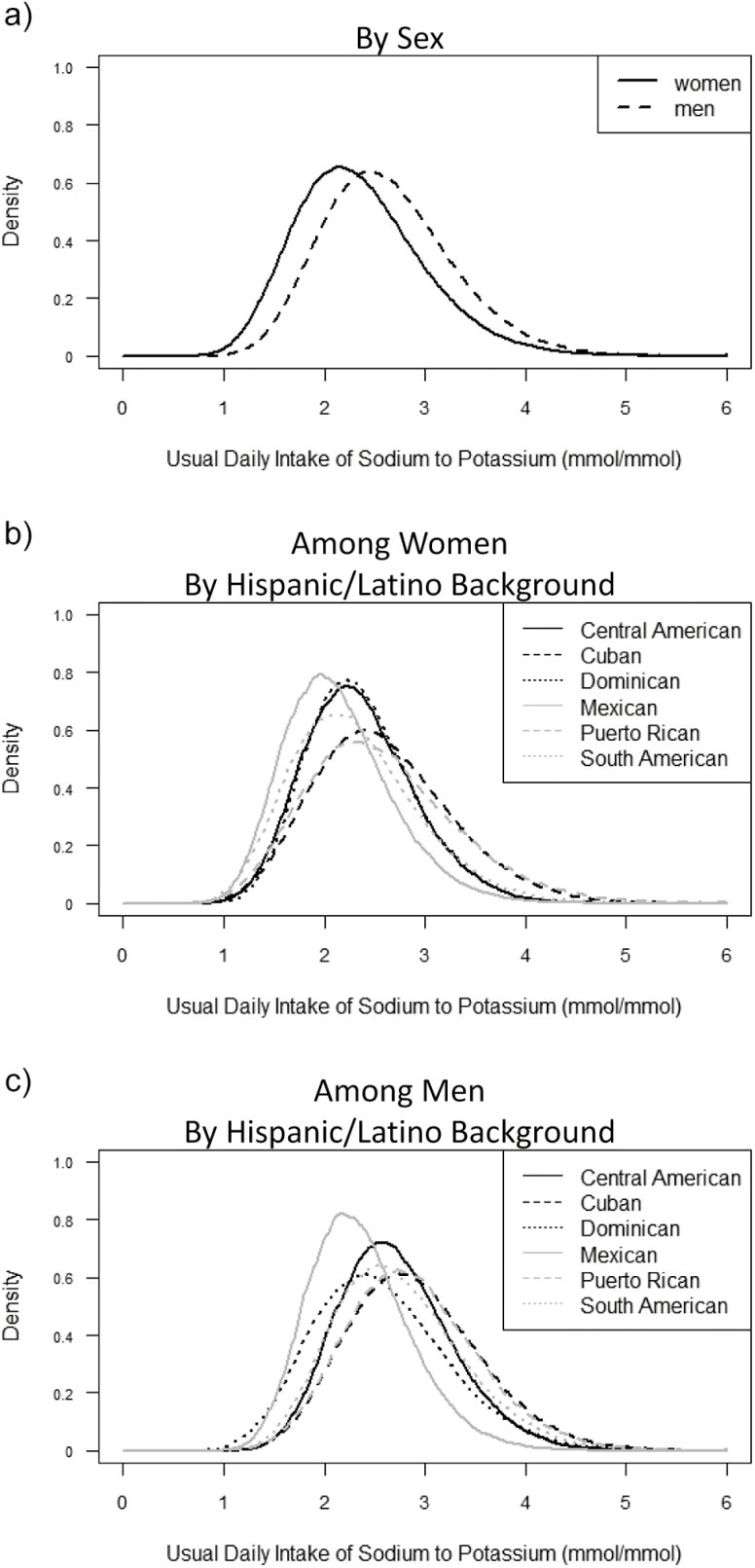
Kernel density distributions of usual intake of sodium, potassium, and sodium-to-potassium ratio by sex and Hispanic/Latino background group are plotted in Figures 1–3.
Figure 1.
The distribution of sodium is depicted by sex (a), by Hispanic/Latino background among women (b), and by Hispanic/Latino background among men (c).
Figure 2.
The distribution of potassium is depicted by sex (a), by Hispanic/Latino background among women (b), and by Hispanic/Latino background among men (c).
Figure 3.
The distribution of sodium to potassium ratio is depicted by sex (a), by Hispanic/Latino background among women (b), and by Hispanic/Latino background among men (c).
Median usual daily intake of potassium was 2,069 mg (95% CI: 2,046, 2,092) among women overall and it ranged from 1,756 mg/day (95% CI: 1,703, 1,808) among Puerto Rican women to 2,216 mg/day (95% CI: 2,153, 2,279) among Central American women (Table 2). Among men, median usual intake of potassium was 2,649 mg (95% CI: 2,615, 2,683) overall and it ranged from 2,317 mg/day (95% CI: 2,245, 2,388) among Puerto Rican men to 2,858 mg/day (95% CI: 2,799, 2,917) among Central American men (Table 3). Among both women and men, median usual daily intake of potassium was higher among individuals with more education, those foreign-born, and those who take supplements. Median usual daily intake of molar Na-K ratio was 2.30 (95% CI: 2.28, 2.33) among women and 2.61 (95% CI: 2.29, 2.93) among men. Among both women and men, Na-K ratio was highest among: Hispanic/Latinos of Central American and Puerto Rican backgrounds, those born in the United States, and those not taking supplements.
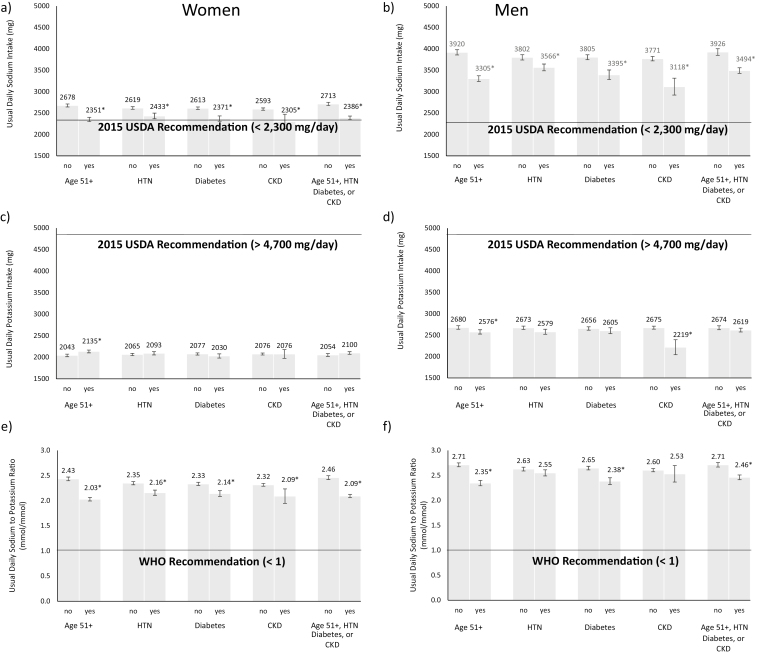
Median usual intake of sodium, potassium, and molar Na-K ratio also differed by clinically relevant characteristics (Figure 4). For example, among both women and men, median usual daily intake of sodium and Na-K ratio was lower among those with vs. without any clinically relevant characteristic (≥ 51 year or greater, hypertension, diabetes, or CKD).
Figure 4.
Usual daily sodium intake is depicted among women (a) and among men (b). Usual daily potassium intake is depicted among women (c) and among men (d). Usual daily sodium to potassium ratio is depicted among women (e) and among men (f).
Overall only 21.3% (95% CI: 20.2%, 22.4%) and 0.6% (95% CI: 0.4%, 0.8%) of the US Hispanic/Latino population met 2015 USDA recommendations for sodium and potassium, respectively. Only 8.3% (95% CI: 7.6, 8.9) met WHO recommendations for potassium and 0.3% (95% CI: 0.1%, 0.4%) met WHO recommendations for Na-K ratio (Table 4). Women were more likely than men to meet 2015 USDA recommendations for sodium (% <2,300 mg/day: 35.8% vs. 6.5%) but less likely than men to meet WHO recommendations for potassium intake (% >3,510 mg/day: 1.9% vs. 15.7%). Among both men and women, those with vs. without clinically relevant characteristics (age 51+, with hypertension, diabetes, or CKD) were also more likely to meet 2015 USDA recommendations for sodium (% <2,300 mg/day: 29.6% vs. 15.2%).
Table 4.
Proportion of US Hispanic/Latinos meeting recommendations for usual daily intake of sodium, potassium, and sodium-to-potassium ratio by relevant clinical characteristics, HCHS/SOL 2008–2011
| Sodium | Potassium | Sodium-to-potassium ratio | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| <1,500 mga | <2,300 mgb | >3,510 mgc | ≥4,700 mgd | <1 mmol/mmole | ||||||
| % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | |
| Overall (men and women) | 3.4 | (2.9, 4.0) | 21.3 | (20.2, 22.4) | 8.3 | (7.6, 8.9) | 0.6 | (0.5, 0.7) | 0.3 | (0.1, 0.4) |
| Age 51+, HTN, Diabetes, or CKD | ||||||||||
| No | 1.6 | (1.1, 2.1) | 15.2 | (13.7, 16.7) | 8.2 | (7.3, 9.2) | 0.6 | (0.4, 0.8) | 0.0 | (0.0, 0.1) |
| Yes | 7.0 | (5.8, 8.2) | 29.6 | (27.9, 31.3) | 8.0 | (7.2, 8.9) | 0.5 | (0.4, 0.7) | 0.9 | (0.5, 1.2) |
| Women | 5.3 | (4.2, 6.3) | 35.8 | (34.22, 37.4) | 1.9 | (1.4, 2.4) | 0.0 | (0.0, 0.0) | 0.4 | (0.2, 0.6) |
| Age 51+, HTN, Diabetes, or CKD | ||||||||||
| No | 1.7 | (0.8, 2.7) | 26.3 | (23.8, 28.8) | 1.6 | (0.9, 2.3) | 0.0 | (0.0, 0.1) | 0.1 | (0.0, 0.2) |
| Yes | 11.6 | (9.6, 13.7) | 45.9 | (43.8, 48.1) | 2.4 | (1.8, 3.0) | 0.1 | (0.0, 0.1) | 1.0 | (0.5, 1.5) |
| Men | 0.4 | (0.2, 0.7) | 6.5 | (5.0, 8.1) | 15.7 | (14.3, 17.2) | 1.5 | (1.0, 1.9) | 0.1 | (0.0, 0.2) |
| Age 51+, HTN, Diabetes, or CKD | ||||||||||
| No | 0.1 | (0.0, 0.2) | 3.4 | (2.0, 4.9) | 16.4 | (14.4, 18.4) | 1.6 | (0.9, 2.3) | 0.0 | (0.0, 0.0) |
| Yes | 1.3 | (0.4, 2.1) | 11.6 | (8.9, 14.3) | 14.7 | (13.0, 16.5) | 1.3 | (0.7, 1.8) | 0.4 | (0.0, 0.7) |
Abbreviations: CKD, chronic kidney disease; HCHS/SOL, Hispanic Community Health Survey/Study of Latinos; HTN, hypertension; USDA: US Department of Agriculture.
a2010 USDA recommendations: sodium <2,300 mg/day. Population subgroups who would benefit from additional reductions to <1,500 mg/day include: persons aged 51 or older, African Americans, or those who have hypertension, diabetes, or chronic kidney disease.
b2015 USDA recommendations: sodium <2,300 mg/day.
cWorld Health Organization recommendation for potassium ≥3,510 mg/day.
d2010 and 2015 USDA recommendation: potassium ≥4,700 mg/day.
eWorld Health Organization recommendation for sodium-to-potassium ratio: <1 (mmol/mmol) per day.
DISCUSSION
In the largest US population-based study of diverse Hispanic/Latinos, only 21% met 2015 USDA dietary guidelines of <2,300 mg/day of sodium. Usual daily intake of dietary sodium varied by Hispanic/Latino background, with highest intake among women and men of Central American backgrounds. Usual daily intake of potassium among US Hispanic/Latinos was also inadequate. Overall less than 1% met USDA guidelines of ≥4,700 mg/day and only 8% met the less stringent WHO guideline of ≥3,510 mg/day. Usual daily intake of potassium also varied by Hispanic/Latino background, though with less pronounced differences than sodium, and with lowest intake among women and men of Puerto Rican background. Finally, usual daily intake of Na-K was also inadequate in all Hispanic/Latino background groups, with less than 1% of the US Hispanic/Latino population meeting WHO recommendations of molar Na-K ratio <1, and highest intake among women and men of Central American and Puerto Rican background groups.
US Hispanic/Latinos are not a homogeneous group, some are US born and others come from different countries with diverse cultures and diets.9 Though sodium intake varied substantially by Hispanic/Latino background, usual sodium intake remained too high for all. Given the sheer ubiquity of sodium within the US food supply,28 this is of little surprise. It is estimated that 70% of sodium intake is derived from prepackaged, processed, and restaurant foods,28,29 offering individuals limited control in restricting their sodium intake. To effectively lower sodium intake, engaged individuals must be effective readers of nutrition facts labels and avoid prepared foods without nutrient information—such as most restaurant foods. This is a challenging task for even motivated individuals. For example, even among individuals with hypertension—a group in which sodium reduction is indicated—it has been shown that actively using the nutrition facts label is not associated with lower sodium intake.30 In fact, results from the current study show that sodium intake among US Hispanics/Latinos who may benefit from additional sodium restriction (such as those with hypertension or diabetes) was only modestly lower than individuals without any of these conditions. Along these lines, though individuals with vs. without such clinically recommended conditions are more likely to meet recommendations for sodium intake, less than 70% actually meet the less stringent 2015 USDA sodium guideline. Further, these individuals who are vulnerable to the BP raising effects of sodium, consume sodium at an average that is almost double the 2010 USDA guideline of <1,500 mg/day of sodium—a guideline that was in place at the time the data were collected and still reflects American Heart Association guidance.31 In light of a 2013 Institutes of Medicine report32 there has been much debate in recent years as to what threshold of sodium intake is sufficiently low. Further, the evidence regarding sodium and its association with CVD events has been mixed.33,34 Despite this, the BP elevating effect of a high sodium diet has been well established and sodium intake in the United States,7 particularly among US Hispanics/Latinos, is too high even according to less restrictive guidelines. Thus, sodium reduction is certainly warranted on a population level.
On the other hand, potassium—a nutrient which blunts the BP raising effect of sodium,1,35 is lacking in the US diet,7 and as the current study shows, potassium intake among US Hispanics/Latinos is inadequate. Potassium is most commonly found in fresh fruits and vegetables. But, unlike sodium, it is not added to processed foods by food manufacturers.36 Thus the variation in potassium intake among different Hispanic/Latino background groups is likely reflective of fruit and vegetable intake.13,37 In fact, in the HCHS/SOL, Puerto Ricans, a Hispanic/Latino background group with a high burden of CVD risk factors,11 had lower intake of fruits and vegetables compared with other US Hispanic/Latino background groups.10 Our data corroborate this, as men and women of Puerto Rican background by far had the lowest intake of potassium. Likewise, Na-K ratio, an indicator shown to be a valid measure of both fruit and vegetable consumption as well as dietary quality37 was highest (i.e., worst) among Puerto Ricans.
The lack of potassium in the US diet, in combination with large quantities of sodium supplementation in the US food system, has made the ratio of sodium-to-potassium unfavorable.36 Exacerbating this issue, research shows that diets low in Na-K ratio and in particular, dense in potassium, are associated with higher costs.38 In our study, there was a trend to both higher potassium and lower Na-K at higher income levels. Thus, improving Na-K ratio at a population level, by increasing potassium intake might prove particularly challenging among socioeconomically disadvantaged groups such as the US Hispanic/Latino population, 42% of which (in the current sample) have an annual household income less than $20,000 per year. These results underscore the need for changes in the US food system which enable individuals to improve overall dietary quality at an affordable cost, and without relying solely on individual-level behavioral changes.
Accurate measurement of nutrients, particularly sodium, is challenging39 and constitutes a major limitation of the current study. Although the NCI method used to derive usual intakes of sodium and potassium has been validated and found to be superior to 24-hour dietary recall means,27 a limitation of our study was that the NCI method was not validated against the gold-standard 24-hour urine collection for measurement of sodium and potassium in the HCHS/SOL sample. However, our results showing usual intake of sodium and potassium using the NCI method more closely mirrored means from 24-hour urine collections than means from 24-hour dietary recall, which were previously published in a small sample of HCHS/SOL participants.15 Further, results from the current study are consistent with dated, albeit comparable samples of US Hispanics from Hispanic HANES (conducted between 1982 and 1984) and show similar intakes of sodium among men and women of Mexican, Cuban, and Puerto Rican backgrounds (sampled from the same geographical regions of the HCHS/SOL study).40 in addition, sodium is highly correlated with energy intake and tends to be heavily underreported when assessed from 24-hour dietary recall.41 In fact, underreporting of energy and consequently sodium is more pronounced among those overweight or obese15—which represents the majority of the US Hispanic/Latino population.42 Consistent with such findings, in our sample, usual daily intake of sodium was actually lower among individuals of higher BMI—a counterintuitive finding, which likely reflects underreport of diet among these individuals. In fact, a previously published study using the same data, showed that the association between sodium and BMI was only positive after adjusting for sociodemographic and behavioral factors, including energy intake.43 Our current results are not adjusted for potential confounders associated with under or over report of dietary data. Therefore, we posit that current estimates reported should serve as approximations of usual daily intake of sodium and potassium, given typical variation in diet and challenges with accurately characterizing micronutrient content, especially using 24-hour dietary recall.
Though Hispanic/Latino background may certainly play a role in determining nutrient intake, we caution against over interpretation of our findings and emphasize that the current analysis seeks only to describe nutrient intake among US Hispanics/Latinos. Social determinants of health such as geographical location/neighborhood, income, education, acculturation experience, or skin color/discrimination experience can vary considerably across Hispanics/Latinos background groups,9 and may help explain observed variation in nutrient intake across Hispanic/Latino background groups. We also acknowledge that among certain groups, such as individuals with hypertension, sodium restriction is commonly reported30 thus self-reported diet may reflect eating behavior deemed more socially desirable and somewhat different from that typically consumed. Given the cross-sectional design of the study, we were not able to take into account any dietary changes which may have resulted from chronic conditions. Finally, our results are descriptive in nature, highlighting only median intakes of sodium and potassium without an assessment of whether intakes are associated with outcomes of interest, such as BP.
Despite these limitations, this is the first study of its kind to describe and directly compare estimates of sodium, potassium, and Na-K ratio in a large national study of diverse Hispanics/Latinos. As the US continues to deal with challenges related to a high prevalence of CVD and its risk factors, routine active surveillance of sodium and potassium intake is critical given their roles as important modifiable risk factors for hypertension. Further, though imperfect, our assessment of sodium and potassium, using the NCI method, accounted for within and between person variation in nutrient intake. The methodology used in this analysis is therefore comparable to results from the NHANES study7 and provides a robust first-look of usual intakes of sodium and potassium among the broader US Hispanic/Latino population.
In summary, among a diverse population of US Hispanics/Latinos, sodium intake varied considerably but was overall high, with only 21.3% meeting 2015 USDA guidelines of less than 2,300 mg/day. Potassium intake varied modestly by Hispanic/Latino background but was even more inadequate in the population as a whole, with only 0.6% meeting USDA recommendations of at least 4,700 mg/day. Likewise, Na-K ratio was also unfavorable, suggesting that dietary improvements among Hispanic/Latinos—a group burdened by high rates of CVD and CVD risk factors11,44 are necessary. Together these data support the need for broad population-based strategies aimed at optimizing the ratio of Na-K by simultaneously lowering sodium and increasing potassium intake.
ACKNOWLEDGMENTS
We thank Nicole Butera, MPH, and Pamela Shaw, PhD, for their help with the statistical methodology. The Study of Latinos: Nutrition & Physical Activity Assessment Study was supported by R01HL095856 from the National Heart, Lung, and Blood Institute. The Hispanic Community Health Study/Study of Latinos was carried out as a collaborative study supported by contracts from the National Heart, Lung, and Blood Institute (NHLBI) to the University of North Carolina (N01-HC65233), University of Miami (N01-HC65234), Albert Einstein College of Medicine (N01-HC65235), Northwestern University (N01-HC65236), and San Diego State University (N01-HC65237).
T.E. was supported by the American Heart Association post-doctoral fellowship (17POST32490000) and is currently supported by the University of Miami Clinical and Translational Science Institute, from the National Center for Advancing Translational Sciences and the National Institute on Minority Health and Health Disparities (KL2TR002737). D.B.H. was supported by a grant from the National Institutes of Health, National Heart, Lung, and Blood Institute (K01HL137557). A.Z.A.H. was supported by a grant from the National Institutes of Health, National Institute on Aging (K01AG047273).
DISCLOSURE
The authors declared no conflict of interest.
REFERENCES
- 1. Adrogué HJ, Madias NE. Sodium and potassium in the pathogenesis of hypertension. N Engl J Med 2007; 356:1966–1978. [DOI] [PubMed] [Google Scholar]
- 2. Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, Chiuve SE, Cushman M, Delling FN, Deo R, de Ferranti SD, Ferguson JF, Fornage M, Gillespie C, Isasi CR, Jiménez MC, Jordan LC, Judd SE, Lackland D, Lichtman JH, Lisabeth L, Liu S, Longenecker CT, Lutsey PL, Mackey JS, Matchar DB, Matsushita K, Mussolino ME, Nasir K, O’Flaherty M, Palaniappan LP, Pandey A, Pandey DK, Reeves MJ, Ritchey MD, Rodriguez CJ, Roth GA, Rosamond WD, Sampson UKA, Satou GM, Shah SH, Spartano NL, Tirschwell DL, Tsao CW, Voeks JH, Willey JZ, Wilkins JT, Wu JH, Alger HM, Wong SS, Muntner P; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics-2018 update: a report from the American heart association. Circulation 2018; 137:e67–e492. [DOI] [PubMed] [Google Scholar]
- 3. Sacks FM, Svetkey LP, Vollmer WM, Appel LJ, Bray GA, Harsha D, Obarzanek E, Conlin PR, Miller ER III, Simons-Morton DG, Karanja N, Lin PH; DASH-Sodium Collaborative Research Group . Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 2001; 344:3–10. [DOI] [PubMed] [Google Scholar]
- 4. US Department of Agriculture. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. U.S Government Printing Office: Washington, DC, 2015. [Google Scholar]
- 5. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997; 336:1117–1124. [DOI] [PubMed] [Google Scholar]
- 6. Cogswell ME, Loria CM, Terry AL, Zhao L, Wang CY, Chen TC, Wright JD, Pfeiffer CM, Merritt R, Moy CS, Appel LJ. Estimated 24-hour urinary sodium and potassium excretion in US adults. JAMA 2018; 319:1209–1220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cogswell ME, Zhang Z, Carriquiry AL, Gunn JP, Kuklina EV, Saydah SH, Yang Q, Moshfegh AJ. Sodium and potassium intakes among US adults: NHANES 2003-2008. Am J Clin Nutr 2012; 96:647–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cobb LK, Appel LJ, Anderson CA. Strategies to reduce dietary sodium intake. Curr Treat Options Cardiovasc Med 2012; 14:425–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rodriguez CJ, Allison M, Daviglus ML, Isasi CR, Keller C, Leira EC, Palaniappan L, Piña IL, Ramirez SM, Rodriguez B, Sims M; American Heart Association Council on Epidemiology and Prevention; American Heart Association Council on Clinical Cardiology; American Heart Association Council on Cardiovascular and Stroke Nursing . Status of cardiovascular disease and stroke in Hispanics/Latinos in the United States: a science advisory from the American Heart Association. Circulation 2014; 130:593–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Siega-Riz AM, Sotres-Alvarez D, Ayala GX, Ginsberg M, Himes JH, Liu K, Loria CM, Mossavar-Rahmani Y, Rock CL, Rodriguez B, Gellman MD, Van Horn L. Food-group and nutrient-density intakes by Hispanic and Latino backgrounds in the Hispanic Community Health Study/Study of Latinos. Am J Clin Nutr 2014; 99:1487–1498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Daviglus ML, Talavera GA, Avilés-Santa ML, Allison M, Cai J, Criqui MH, Gellman M, Giachello AL, Gouskova N, Kaplan RC, LaVange L, Penedo F, Perreira K, Pirzada A, Schneiderman N, Wassertheil-Smoller S, Sorlie PD, Stamler J. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. JAMA 2012; 308:1775–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Angell SY, Yi S, Eisenhower D, Kerker BD, Curtis CJ, Bartley K, Silver LD, Farley TA. Sodium intake in a cross-sectional, representative sample of New York City adults. Am J Public Health 2014; 104:2409–2416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Loftfield E, Yi S, Curtis CJ, Bartley K, Kansagra SM. Potassium and fruit and vegetable intakes in relation to social determinants and access to produce in New York City. Am J Clin Nutr 2013; 98:1282–1288. [DOI] [PubMed] [Google Scholar]
- 14. Gardener H, Rundek T, Wright CB, Elkind MS, Sacco RL. Dietary sodium and risk of stroke in the Northern Manhattan study. Stroke 2012; 43:1200–1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mossavar-Rahmani Y, Sotres-Alvarez D, Wong WW, Loria CM, Gellman MD, Van Horn L, Alderman MH, Beasley JM, Lora CM, Siega-Riz AM, Kaplan RC, Shaw PA. Applying recovery biomarkers to calibrate self-report measures of sodium and potassium in the hispanic community health study/study of latinos. J Hum Hypertens 2017; 31:860. [DOI] [PubMed] [Google Scholar]
- 16. Sorlie PD, Avilés-Santa LM, Wassertheil-Smoller S, Kaplan RC, Daviglus ML, Giachello AL, Schneiderman N, Raij L, Talavera G, Allison M, Lavange L, Chambless LE, Heiss G. Design and implementation of the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol 2010; 20:629–641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lavange LM, Kalsbeek WD, Sorlie PD, Avilés-Santa LM, Kaplan RC, Barnhart J, Liu K, Giachello A, Lee DJ, Ryan J, Criqui MH, Elder JP. Sample design and cohort selection in the Hispanic Community Health Study/Study of Latinos. Ann Epidemiol 2010; 20:642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nutrition Data System for Research (NDS-R) Version 2011. 1998–1999 Regents of the University of Minnesota: Minneapolis, MN. [Google Scholar]
- 19. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014; 311:507–520. [DOI] [PubMed] [Google Scholar]
- 20. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010; 33(Suppl 1):S62–S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis 2002; 39(2Suppl 1):S1–S266. [PubMed] [Google Scholar]
- 22. US Department of Agriculture. Dietary Guidelines for Americans. U.S Government Printing Office: Washington, DC, 2010. [Google Scholar]
- 23. Allen VC Jr, Lachance C, Rios-Ellis B, Kaphingst KA. Issues in the assessment of “Race” among Latinos: implications for research and policy. Hisp J Behav Sci 2011; 33:411–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. World Health Organization. Guideline: Potassium Intake for Adults and Children. World Health Organization (WHO): Geneva, 2012. [PubMed] [Google Scholar]
- 25. World Health Organization. Diet, Nutrition and the Prevention of Chronic Diseases. World Health Organization (WHO): Geneva, 2003. [PubMed] [Google Scholar]
- 26. National Cancer Institute. Usual Dietary Intakes: The NCI Method. National Institutes of Health. World Health Organization: Bethesda, MD, 2018. [Google Scholar]
- 27. Tooze JA, Kipnis V, Buckman DW, Carroll RJ, Freedman LS, Guenther PM, Krebs-Smith SM, Subar AF, Dodd KW. A mixed-effects model approach for estimating the distribution of usual intake of nutrients: the NCI method. Stat Med 2010; 29:2857–2868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Harnack LJm, Cogswell ME, Shikany JM, Garder CD, Gillespie C, Loria CM, Zhou X, Yuan K, Steffen LM. Sources of sodium in US adults from 3 geographic regions. Circulation. 2017; 135:1775–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. US Department of Agriculture. What We Eat in America: NHANES 2013–2014. Agricultural Research Service: Beltsville, MD. [Google Scholar]
- 30. Elfassy T, Yi S, Eisenhower D, Lederer A, Curtis CJ. Use of sodium information on the nutrition facts label in New York City adults with hypertension. J Acad Nutr Diet 2015; 115:278–283. [DOI] [PubMed] [Google Scholar]
- 31. Van Horn L, Carson JA, Appel LJ, Burke LE, Economos C, Karmally W, Lancaster K, Lichtenstein AH, Johnson RK, Thomas RJ, Vos M, Wylie-Rosett J, Kris-Etherton P; American Heart Association Nutrition Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular Disease in the Young; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Stroke Council . Recommended dietary pattern to achieve adherence to the American heart association/American college of cardiology (AHA/ACC) guidelines: a scientific statement from the American heart association. Circulation 2016; 134:e505–e529. [DOI] [PubMed] [Google Scholar]
- 32. Committee on the Consequences of Sodium Reduction in Populations; Food and Nutrition Board; Board on Population Health and Public Health Practice, Institute of Medicine. Sodium Intake in Populations: Assessment of Evidence. In Strom BL, Yaktine AL, Oria M (eds). National Academies Press (US): Washington, DC, 2013. [PubMed] [Google Scholar]
- 33. Stolarz-Skrzypek K, Kuznetsova T, Thijs L, Tikhonoff V, Seidlerová J, Richart T, Jin Y, Olszanecka A, Malyutina S, Casiglia E, Filipovský J, Kawecka-Jaszcz K, Nikitin Y, Staessen JA; European Project on Genes in Hypertension (EPOGH) Investigators . Fatal and nonfatal outcomes, incidence of hypertension, and blood pressure changes in relation to urinary sodium excretion. JAMA 2011; 305:1777–1785. [DOI] [PubMed] [Google Scholar]
- 34. Strazzullo P, D’Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta-analysis of prospective studies. BMJ 2009; 339:b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Castro H, Raij L. Potassium in hypertension and cardiovascular disease. Semin Nephrol 2013; 33:277–289. [DOI] [PubMed] [Google Scholar]
- 36. Cordain L, Eaton SB, Sebastian A, Mann N, Lindeberg S, Watkins BA, O’Keefe JH, Brand-Miller J. Origins and evolution of the Western diet: health implications for the 21st century. Am J Clin Nutr 2005; 81:341–354. [DOI] [PubMed] [Google Scholar]
- 37. Loftfield E, Yi S, Immerwahr S, Eisenhower D. Construct validity of a single-item, self-rated question of diet quality. J Nutr Educ Behav 2015; 47:181–187. [DOI] [PubMed] [Google Scholar]
- 38. Drewnowski A, Rehm CD, Maillot M, Monsivais P. The relation of potassium and sodium intakes to diet cost among U.S. adults. J Hum Hypertens 2015; 29:14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McLean RM. Measuring population sodium intake: a review of methods. Nutrients 2014; 6:4651–4662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kuczmarski M, Kuczmarski RJ, Najjar M. Food usage among Mexican-American, Cuban, and Puerto Rican adults: findings from the hispanic HANES. Nutrition Today 1995; 30(1):30–37. [Google Scholar]
- 41. Black AE. Critical evaluation of energy intake using the Goldberg cut-off for energy intake:basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes Relat Metab Disord 2000; 24:1119–1130. [DOI] [PubMed] [Google Scholar]
- 42. Freedman LS, Commins JM, Moler JE, Willett W, Tinker LF, Subar AF, Spiegelman D, Rhodes D, Potischman N, Neuhouser ML, Moshfegh AJ, Kipnis V, Arab L, Prentice RL. Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for potassium and sodium intake. Am J Epidemiol 2015; 181:473–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Elfassy T, Mossavar-Rahmani Y, Van Horn L, Gellman M, Sotres-Alvarez D, Schneiderman N, Daviglus M, Beasley JM, Llabre MM, Shaw PA, Prado G, Florez H, Zeki Al Hazzouri A. Associations of sodium and potassium with obesity measures among diverse US hispanic/latino adults: results from the hispanic community health study/study of latinos. Obesity (Silver Spring) 2018; 26:442–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Daviglus ML, Pirzada A, Talavera GA. Cardiovascular disease risk factors in the Hispanic/Latino population: lessons from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prog Cardiovasc Dis 2014; 57:230–236. [DOI] [PubMed] [Google Scholar]