Abstract
It was recently suggested that the Metabolic Syndrome should be renamed to “Circadian Syndrome”. In this context, we explored the effects of living under standard laboratory conditions, where light is the only cycling variable (relevant to human modern life), in a diurnal mammal, on the relationships between affective-like pathology, type 2 diabetes mellitus (T2DM), and cardiac hypertrophy. After 20 weeks, some of the animals spontaneously developed T2DM, depressive and anxiety-like behavior and cardiac hypertrophy. There were significant correlations between levels of anxiety-like behavior and glucose tolerance, and between heart/total body weight ratio and glucose tolerance. Our data suggest a relationship between the development of T2DM, emotional and cardiac pathology as seen in diurnal humans. Furthermore, our data show a possible relationship between reduced daily cycling cues in the laboratory and what has been regularly termed “Metabolic Syndrome” and recently proposed by us to be renamed to “Circadian Syndrome”.
Subject terms: Animal physiology, Metabolic syndrome
Introduction
The comorbid relationship between depression, cardiovascular diseases (CVD) and type 2 diabetes mellitus (T2DM) is repeatedly described in the literature1–7. Whereas the underlying mechanisms connecting CVD and T2DM are somewhat understood3,8, the relationship between these two very common chronic diseases with depression is well-documented clinically but not yet understood at the mechanistic level1,9–15.
Yet, depression16–18, CVD19–24 and T2DM25,26 have been strongly linked with circadian rhythm disturbances. Moreover, it was recently suggested that circadian disruption might be an important underlying and uniting etiological factor for the key cardio-metabolic components of the Metabolic Syndrome and its associated comorbidities: sleep disturbances, depression, steatohepatitis and cognitive dysfunction. We have suggested that this combination of the Metabolic Syndrome and the comorbidities warrants that it should be renamed the “Circadian Syndrome”15.
The fat sand rat (Psammomys obesus) is a large burrow-dwelling gerbil (160 ± 30 g) that inhabits wadi beds, saline and saline-marsh plains in the deserts of North Africa, from Mauritania to Egypt, Sudan and Israel27. Studies from the 1960’s discovered that when sand rats are held under laboratory conditions and fed standard rodent food they quickly develop diabetes28,29. As a result, it has become a frequently used animal model to explore the underlying biology of T2DM30–34.
Sand rats in nature are strictly diurnal, spending extended periods in foraging on salt bushes35. When brought into laboratory conditions, they demonstrate an unstable, nocturnal phase preference, with low amplitude and, in some cases, no rhythm at all36,37. A switch from clear diurnality in nature to a mixed diurnal/nocturnal pattern in the laboratory is not uncommon and has been described for the golden spiny mouse (Acomys russatus)38, Nile grass rat (Arvicanthis niloticus)39, degu (Octodon degu)40, tuco-tuco (Ctenomys aff. knighti)41 and Mongolian gerbil (Meriones unguiculatus)42. No such responses have been reported in nocturnal rodents36, albeit mice with targeted mutation in the Per2 clock gene were shown to have less robust circadian rhythms when placed in a semi-natural environment43.
We recently demonstrated that relatively mild interference with circadian rhythms in the sand rat can accelerate the development of T2DM, obesity and cardiac hypertrophy37, and suggested that the possible underlying mechanism of this process is related to changes that accompany the switch from the mammalian ancestral nocturnal activity to the current diurnal one37,44. Interference with the sand rat circadian rhythms can also lead to the development of a depressive- and anxiety-like behavioral phenotype45–47 that is ameliorated by antidepressant treatment48, increased physical activity (voluntary wheel running)49 and bright white or blue light treatment50–52. Interestingly, similar circadian interventions in nocturnal mice did not result in depressive-like phenotypes53.
All things considered, data have shown that (1) when transferred into laboratory conditions most, but not all, sand rats develop T2DM. (2) Relatively small circadian manipulation induce a depression/anxiety-like phenotype in the sand rats. (3) Small manipulation of circadian rhythms in the sand rat accelerate the development of T2DM and cardiac hypertrophy. Based on these data we hypothesized that circadian disruption could be the underlying common denominator for the development of T2DM, obesity, CVD and depression and for the comorbidity between these four pathological states as a part of the newly termed “Circadian Syndrome”15.
To further explore this hypothesis, the current study examined correlations between the development of diabetes and depression/anxiety-like phenotype in sand rats maintained in laboratory settings under 12:12 LD conditions and fed standard rodent food.
Results
Development of T2DM
From 60 sand rats, 15 died during the 20-week period of eating standard rodent food. At the time of the glucose tolerance test, 13 out of the remaining 45 animals had glucose levels above 110 mg/dl and were considered diabetic and 32 had glucose levels lower than 110 mg/dl and were considered non-diabetic. Of the non-diabetic animals, we randomly selected 13 individuals for the experiment for further analyses to match the sample size of the diabetic group.
Behavioral tests
To obtain an overall analysis of the difference between diabetic and non-diabetic animals in the behavioral tests we analyzed in one matrix one measure from each test: Sink 2 in the FST and time in the open arms in the EPM54. The analysis indicated a significant difference between the groups [ANOVA: F(2,22) = 4.5, p = 0.023]. We then analyzed separately the data for each test.
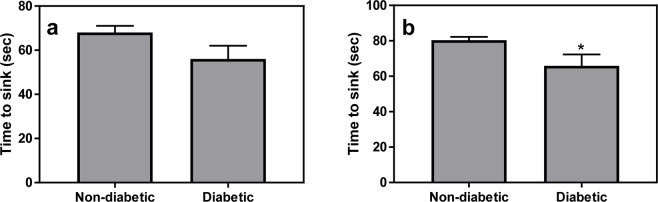
Forced swim test
repeated measures ANOVA across Sink 1 and Sink 2 showed a significant “Sink” effect [F(1,23) = 63, p < 0.001, a near significant Diabetes effect [F(1,23) = 3.8, p = 0.063] and no interaction [F1,23) = 0.96, p = 0.34]. Following the significant “Sink” effect, we separately analyzed the Sink 1 and Sink 2 data. Data show a trend for difference for Sink 1 [Fig. 1a, t(23) = 1.7, p = 0.1] and a significant difference between diabetic and non-diabetic sand rats for Sink 2 [Fig. 1b, t(23) = 2.1, p = 0.047]. However, we found no correlation between sink time in the FST and glucose levels in the glucose tolerance test (data not shown, r = 0.26, p = 0.2).
Figure 1.
In the modified FST, diabetic fat sand rats exhibited a trend for lower time to Sink 1 (a) and a significantly lower time to sink 2 (b) compared with the non-diabetic animals. *Signifies p < 0.05 between the groups. N = 12 for non-diabetic group and 13 for diabetic group.
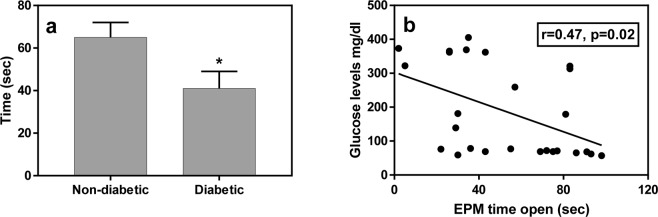
Elevated plus maze
analysis of “time in open arms” indicated a significantly lower time in the open arms in the diabetic compared with non-diabetic animals [Fig. 2a; t (24) = 2.32, p = 0.03; effect size – Cohen’s d = 0.91]. A similar trend that did not reach statistical significance was demonstrated for the open/closed arms time ratio [t (24) = 2.01, p = 0.06]. Additionally, we found a significant correlation between the time in open arms and glucose levels in the glucose tolerance test for all animals combined (Fig. 2b; r = 0.47, p = 0.02).
Figure 2.
Diabetic fat sand rats spent less time in the open arms of the EPM than the non-diabetic animals (a, N = 13/group). The response in the EPM shows correlation with glucose levels in the GTT (b, N = 26). *Signifies p < 0.05 for the difference between the groups.
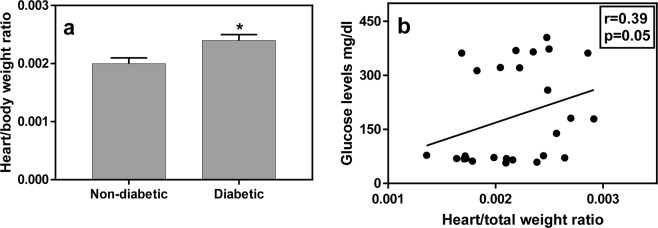
Weight and heart weight
Heart weights were larger in the diabetic groups [t (24) = 3.7, p = 0.001; effect size – Cohen’s d = 1.41] and similar results were demonstrated in the measure of heart/total body weight ratio [Fig. 3a; t (24) = 2.7, p = 0.013; effect size – Cohen’s d = 1.0]. No difference was detected in total body weight between non-diabetic and diabetic animals [t (24) = 1.0, p = 0.35]. Similar to the finding for the EPM, there was also a significant correlation between heart/total body weight ratio and glucose levels for all animals combined (Fig. 3b; r = 0.39, p = 0.05).
Figure 3.
Diabetic animals exhibited a higher heart/total body weight ratio than the non-diabetic ones (a, N = 13/group). There was a significant correlation between the heart/total body weight ratio and glucose levels in the GTT (b, N = 26). *Signifies p < 0.05 for the difference between the groups.
Discussion
Studies from the 1960’s onwards show that when sand rats are brought into laboratory conditions and fed standard laboratory food, most, but not all, develop T2DM28,29. In the past, it was believed by most that this was due to the change in their diet in the laboratory28,29,55. It comes as a surprise that recent data show that when held outdoors in laboratory cages and fed standard rodent food sand rats do not develop T2DM, and that small circadian manipulation can result in depressive- and anxiety-like phenotype47 and in accelerated development of T2DM, obesity and cardiac hypertrophy37. With that in mind, the current study was designed to explore possible relationship between living under standard laboratory conditions, where light is the only cycling variable (relevant to human modern life), and the development of T2DM, CVD and depressive/anxiety-like phenotype in a diurnal mammal - the fat sand rat.
Indeed, the results replicate previous findings showing that HsdHu diabetes-prone sand rats develop T2DM under laboratory conditions. In the present experiment, approximately 50% of animals developed T2DM, whereas some of the previous studies reported higher rates at around 70%32,56,57. Interestingly, the animals developing T2DM show more depressive- and anxiety-like behavior compared with sand rats that did not develop diabetes. Moreover, animals that develop diabetes show cardiac hypertrophy. Together, the findings suggest a relationship between the development of diabetes, emotional pathology and cardiac pathology as seen in T2DM in human subjects1,9–15. Furthermore, that data raise a possible relationship between reduced daily cycling cues under laboratory conditions and what has regularly been termed the Metabolic Syndrome15,58–61, recently suggested to be termed the “Circadian Syndrome”15.
In humans, even small desynchronization between the internal clock and external light/dark cycle has been demonstrated to be linked to decreased metabolic efficiency and disrupted cardiac function62 as well as influence insulin secretion and metabolism, contributing to the development of insulin resistance63. Evidence shows that disturbed circadian rhythms could be implicated in key features of the Metabolic Syndrome as well as in sleep disturbances, depression, steatohepatitis and cognitive dysfunction forming the “Circadian Syndrome”15. The current and previous findings in the sand rats64 highlight disrupted or reduced circadian rhythms as a potential common denominator of these pathologies and suggest that the diurnal fat sand rat could be an advantageous animal model to further explore these relationships.
Sand rats in their natural environment do not develop T2DM, CVD, obesity or depressive-like behavior, but when exposed to small circadian interference pathologies appear37,47. Whereas in previous studies we used short photoperiod conditions as a circadian stressor, the current study explored the effects of standard laboratory conditions alone with no additional interventions. The rational for using laboratory conditions was twofold: (1) It is well-documented that sand rats kept in laboratory conditions lose or decrease their diurnal rhythms65,66. (2) It has been reported that many sand rats maintained in laboratory conditions develop T2DM28,55,57,67. In the laboratory the only cycling environmental condition is light, while under natural conditions a wealth of factors, both a-biotic (temperature, humidity, radiation) and biotic (competitors, predators, conspecifics) show a daily rhythm that may promote daytime activity65. This was also shown in laboratory conditions with mice where experimental food scarcity resulted in a switch to diurnal patterns and changes in energy balance68. Moreover, our standard laboratory light illuminance is around 800 lux, and wavelength is with a constant range of 420–780 nm52, while the range of natural light illuminance in Israel (the most northern range of sand rats) is between 7,500 and 80,000 lux (depending on season and cloud overcast)69 and light wavelength range between 300–2400 nm70. It is possible that the laboratory conditions are not sufficient for synchronizing the circadian system and promoting diurnal activity pattern65.
Laboratory conditions are similar in many ways to the modern Western lifestyle and living conditions: controlled ambient temperature and constant food availability71, low physical activity, no interspecific interactions, extensive use of artificial light during the night (“light pollution”) and low light exposure during the day72–74. Consequently, circadian rhythm disturbances were offered to be important contributors to the modern-day epidemics of T2DM, CVD and obesity19,23,63,72,75–81 through what we have recently suggested to be termed the “Circadian Syndrome“15. Recognizing the link between modern lifestyle and circadian disruption, risk and etiology of T2DM, CVD, obesity and depression that form the “Circadian Syndrome”, may have key implications for non-pharmacological prevention and therapeutic strategies to manage the contemporary and escalating non-communicable disease epidemic.
Methods
Animals
Sixty HsdHu diabetes-prone male fat sand rats (Psammomys obesus, 6–7 months old, from our colony at Tel Aviv University Zoological Research Garden) were used as subjects. As previously done37, animals were individually housed in standard plastic cages (42 cm × 26 cm × 15 cm) positioned in temperature-controlled rooms (25 °C) 12 hr/12 hr light/dark cycle with lights on at 08:00 and off at 20:00. Light intensity was 800 lux. Animals were provided ad-lib tap water and standard rodent food (product 19510; Koffolk, Petach-Tikva, Israel). All experimental procedures followed the NIH guidelines for the care and use of laboratory animals and were approved by the Institutional Animal Care and Use Committee (IACUC) of Tel Aviv University (permit number L15055).
Procedure
Following former work from our laboratory37, animals were maintained in the colony conditions for 20 weeks before the start of any manipulation or testing. On week 20, Animals were weighed, blood glucose levels were measured, and oral glucose tolerance tests were performed. Behavioral tests for anxiety- and depressive- like behavior were conducted on week 21. On week 22, the sand rats were euthanized, the chest cavity was rapidly opened, the heart removed and weighed, and the heart weight/body weight ratio calculated.
Glucose tolerance test (GTT)
Glucose tolerance tests were performed in animals fasted for 4 hours. Tests were performed at ZT 2 (ZT = Zeitgaber Time; ZT 0 = the time of lights-on) by administering 2 g glucose/kg body weight using gastric gavages (a syringe attached to a 20-gauge × 1.5 feeding needle), inserted through the mouth into the stomach37. When blood glucose values exceeded 110 mg/dl animals were considered as hyperglycemic32. We selected this relatively strict cutoff criterion suggested by Marquié and colleagues32 to allow as many animals as possible in the study. Based on the results the sand rats were divided into two groups – diabetic and healthy.
Behavioral tests
On week 21 animals were evaluated in two standard behavioral tests of depression- and anxiety-like behaviors. The tests were performed in sequence, the Elevated Plus Maze (EPM) and the Forced Swim Test (FST).
Elevated Plus-Maze (EPM)
As explained in multiple previous work (e.g.82), the test presents the rodent with a conflict between its tendency to remain in a safe enclosed area and the need to explore new environments83. For the present study, we followed our standard procedure84,85. The maze was constructed from black aluminum and had two open arms (50 cm long and 10 cm wide) and two closed arms (same dimensions with 15 cm high walls). The plus maze was elevated 50 cm above the floor and light levels at the open arms were 200 lux. The test started an hour after light onset in the rooms (09:00) and animals were tested only during the next 3.5 hours. Order of testing was random within group with alternation between diabetic and non-diabetic animals. Sand rats were individually placed in the center of the maze and their behavior digitally recorded for a 5 min session. Recordings were used for later manual scoring of behaviors. At the end of the session, animals were returned to their cages and the maze was wiped clean with 70% ethanol before the start of the next session. Scoring included the time and the number of entries into each arm and was done by an investigator blind to treatment84.
Forced swim test
The FST is a commonly used test for the evaluation of depression-like behavior and assessment of antidepressants effects. As described in our previous papers84,85, the FST was used with several methodological alterations in sand rats [for review see47]. In the present study, we followed the established sand rats’ protocol as previously described37,45,46. Each animal was subjected to the FST twice over two consecutive days with the second exposure serving as the test session. Testing started an hour after the onset of lights and ended within the light period in the colony rooms. Each animal was placed individually into a white opaque cylinder, 30 cm in diameter and 45 cm high, filled with water (22–23 °C) to a depth of 25 cm. The test was digitally recorded from above for later manual scoring of behavior. As noted in previous work with sand rats, their ability to float is lower compared with rats or mice. Therefore, the standard measure of floating time in the FST was replaced with the measure of “time to sink” where a sink event is defined by the animal going entirely under water for approximately 2 seconds. Accordingly, right after the second sink, animals were taken out of the water by the experimenter and placed in their home cage and the test was terminated. Water in the cylinder was replaced after each test. Recordings were used to score the time of sink events by an experimenter blind to treatments.
Heart weight
As previously described37, on week 22, the sand rats were euthanized, the chest cavity was rapidly opened, the heart removed and rinsed in two washes of ice-cold saline. Major blood vessels and connective tissue were removed, the heart blotted dry, weighed, and the heart weight/body weight ratio calculated.
Statistical analysis
Statistical analysis was performed using STATISTICA 13.0 software (Dell, Tulsa, OK). Analysis of variance was utilized to explore statistical significance between diabetic (blood glucose levels that exceed 110 mg/dl) and non-diabetic animals. Initially we analyzed in one matrix one measure from each test, Sink 2 in the FST and time in the open arms in the EPM54. Following the overall analysis, we separately analyzed the results of the FST with a repeated measures ANOVA (with diabetic/not diabetic as main factor and Sink 1 and Sink 2 as repeated measure factor). One animal from the non-diabetic group was excluded as an outlier (more than 2XSTD away from the mean). The results from the EPM and heart weight ratio were analyzed with student’s t-test. Homogeneity of variance was analyzed using Levene’s test. Effect sizes were computed using Cohen’s d online calculator (https://www.uccs.edu/lbecker/) Correlations were performed using Pearson’s correlation test.
Acknowledgements
This research was supported by the Israel Science Foundation (grant No. 866/17).
Author Contributions
C.B., H.E., P.Z., G.A. and N.K.S. conceived and designed the study. C.B., O.B., V.V.D. A.G., performed the study, C.B., H.E. and N.K.S. analyzed the data. C.B., H.E., P.Z., N.K.S. wrote the manuscript.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Holt, R.I., de Groot, M. & Golden, S.H. Diabetes and depression. Curr Diab Rep. 14, 491, 410.1007/s11892-11014-10491-11893 (2014). [DOI] [PMC free article] [PubMed]
- 2.Park, M., Katon, W.J. & Wolf, F.M. Depression and risk of mortality in individuals with diabetes: a meta-analysis and systematic review. Gen Hosp Psychiatry. 35, 217–225, 210.1016/j.genhosppsych.2013.1001.1006 Epub 2013 Feb 1013 (2013). [DOI] [PMC free article] [PubMed]
- 3.Petrie JR, Guzik TJ, Touyz RM. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Canadian Journal of Cardiology. 2018;34:575–584. doi: 10.1016/j.cjca.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gluckman PD, Hanson MA, Buklijas T, Low FM, Beedle AS. Epigenetic mechanisms that underpin metabolic and cardiovascular diseases. Nature Reviews Endocrinology. 2009;5:401. doi: 10.1038/nrendo.2009.102. [DOI] [PubMed] [Google Scholar]
- 5.Prasai MJ, George JT, Scott EM. Molecular clocks, type 2 diabetes and cardiovascular disease. Diabetes and Vascular Disease Research. 2008;5:89–95. doi: 10.3132/dvdr.2008.015. [DOI] [PubMed] [Google Scholar]
- 6.Sowers JR, Epstein M, Frohlich ED. Diabetes, hypertension, and cardiovascular disease: an update. Hypertension. 2001;37:1053–1059. doi: 10.1161/01.HYP.37.4.1053. [DOI] [PubMed] [Google Scholar]
- 7.Zimmet, P., Boyko, E. J., Collier, G. R. & De Courten, M. Etiology of the Metabolic Syndrome: Potential role of insulin resistance, leptin resistance, and other players. In The Metabolic Syndrome X: Convergence of Insulin Resistance, Glucose Intolerance, Hypertension, Obesity, and Dyslipidemias-Searching for the Underlying Defects 25–44 (1999). [DOI] [PubMed]
- 8.Cheung BM, Li C. Diabetes and hypertension: is there a common metabolic pathway? Current atherosclerosis reports. 2012;14:160–166. doi: 10.1007/s11883-012-0227-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes - A meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 10.Egede LE, Nietert PJ, Zheng D. Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care. 2005;28:1339–1345. doi: 10.2337/diacare.28.6.1339. [DOI] [PubMed] [Google Scholar]
- 11.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002 Mar. 2002;25(3):464–70. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 12.Renn BN, Feliciano L, Segal DL. The bidirectional relationship of depression and diabetes: a systematic review. Clinical psychology review. 2011;31:1239–1246. doi: 10.1016/j.cpr.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 13.Li, Z., Li, Y., Chen, L., Chen, P. & Hu, Y. Prevalence of depression in patients with hypertension: a systematic review and meta-analysis. Medicine94 (2015). [DOI] [PMC free article] [PubMed]
- 14.Graham N, Smith DJ. Comorbidity of depression and anxiety disorders in patients with hypertension. Journal of hypertension. 2016;34:397–398. doi: 10.1097/HJH.0000000000000850. [DOI] [PubMed] [Google Scholar]
- 15.Zimmet, P. et al. The Circadian Syndrome: is the metabolic syndrome and much more! Journal of Internal Medicine, 286, 181–191 (2019). [DOI] [PMC free article] [PubMed]
- 16.Robillard, R. et al. Circadian rhythms and psychiatric profiles in young adults with unipolar depressive disorders. Transl Psychiatry. 8, 213, 210.1038/s41398-41018-40255-y (2018). [DOI] [PMC free article] [PubMed]
- 17.Wirz-Justice A. Biological rhythm disturbances in mood disorders. Int Clin Psychopharmacol. 2006;21:S11–15. doi: 10.1097/1001.yic.0000195660.0000137267.cf. [DOI] [PubMed] [Google Scholar]
- 18.Edgar, N. & McClung, C. A. Major depressive disorder: a loss of circadian synchrony? Bioessays. 35, 940–944, 910.1002/bies.201300086. Epub 201302013 Sep 201300083 (2013). [DOI] [PMC free article] [PubMed]
- 19.Crnko, S., Du Pré, B. C., Sluijter, J. P. G. & Van Laake, L. W. Circadian rhythms and the molecular clock in cardiovascular biology and disease. Nature Reviews Cardiology (2019). [DOI] [PubMed]
- 20.Van Laake LW, Luscher TF, Young ME. The circadian clock in cardiovascular regulation and disease: Lessons from the Nobel Prize in Physiology or Medicine 2017. European Heart Journal. 2018;39:2326–2329. doi: 10.1093/eurheartj/ehx775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thosar SS, Butler MP, Shea SA. Role of the circadian system in cardiovascular disease. Journal of Clinical Investigation. 2018;128:2157–2167. doi: 10.1172/JCI80590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Durgan DJ, Young ME. The Cardiomyocyte Circadian Clock Emerging Roles in Health and Disease. Circulation Research. 2010;106:647–658. doi: 10.1161/CIRCRESAHA.109.209957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ruger M, Scheer F. Effects of circadian disruption on the cardiometabolic system. Reviews in Endocrine & Metabolic Disorders. 2009;10:245–260. doi: 10.1007/s11154-009-9122-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shaw E, Tofler GH. Circadian rhythm and cardiovascular disease. Current Atherosclerosis Reports. 2009;11:289–295. doi: 10.1007/s11883-009-0044-4. [DOI] [PubMed] [Google Scholar]
- 25.Javeed, N. & Matveyenko, A.V. Circadian Etiology of Type 2 Diabetes Mellitus. Physiology (Bethesda). 33, 138–150, 110.1152/physiol.00003.02018 (2018). [DOI] [PMC free article] [PubMed]
- 26.Poggiogalle, E., Jamshed, H. & Peterson, C.M. Circadian regulation of glucose, lipid, and energy metabolism in humans. Metabolism. 84: 11-27, 10.1016/j.metabol.2017.1011.1017 Epub 2018 Jan 1019 (2018). [DOI] [PMC free article] [PubMed]
- 27.Mendelssohn, H. & Yom-Tov, Y. Fauna Palestina: Mammalia of Israel (Israel Academy of Science and Humanities, Jerusalem, 1999).
- 28.Schmidt-Nielsen K, Haines HB, Hackel DB. Diabetes mellitus in the sand rat induced by standard laboratory diets. Science. 1964;143:689–690. doi: 10.1126/science.143.3607.689. [DOI] [PubMed] [Google Scholar]
- 29.Haines H, Hackel DB, Schmidt-Nielsen K. Experimental diabetes mellitus induced by diet in the sand rat. Am J Physiol. 1965;208:297–300. doi: 10.1152/ajplegacy.1965.1208.1152.1297. [DOI] [PubMed] [Google Scholar]
- 30.Kalderon B, Gutman A, Levy E, Shafrir E, Adler JH. Characterization of stages in development of obesity-diabetes syndrome in sand rat (Psammomys obesus) Diabetes. 1986;35:717–724. doi: 10.2337/diab.35.6.717. [DOI] [PubMed] [Google Scholar]
- 31.Kaiser, N., Cerasi, E. & Leibowitz, G. Diet-induced diabetes in the sand rat (Psammomys obesus). In Animal Models in Diabetes Research 89–102 (Springer 2012). [DOI] [PubMed]
- 32.Marquie G, Duhault J, Jacotot B. Diabetes mellitus in sand rats (Psammomys obesus). Metabolic pattern during development of the diabetic syndrome. Diabetes. 1984;33:438–443. doi: 10.2337/diab.33.5.438. [DOI] [PubMed] [Google Scholar]
- 33.Shafrir E, Gutman A. Psammomys obesus of the Jerusalem colony: a model for nutritionally induced, non-insulin-dependent diabetes. J Basic Clin Physiol Pharmacol. 1993;4:83–99. doi: 10.1515/JBCPP.1993.4.1-2.83. [DOI] [PubMed] [Google Scholar]
- 34.Walder KR, Fahey RP, Morton GJ, Zimmet PZ, Collier GR. Characterization of obesity phenotypes in Psammomys obesus (Israeli sand rats) Journal of Diabetes Research. 2000;1:177–184. doi: 10.1155/EDR.2000.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Haim A, Alma A, Neuman A. Body mass is a thermoregulatory adaptation of diurnal rodents to the desert environment. Journal of Thermal Biology. 2006;31:168–171. doi: 10.1016/j.jtherbio.2005.11.016. [DOI] [Google Scholar]
- 36.Barak, O. & Kronfeld-Schor, N. Activity rhythms and masking response in the diurnal fat sand rat under laboratory conditions. Chronobiol Int. 30, 1123–1134, 1110.3109/07420528.07422013.07805337 Epub 07422013 Aug 07420528 (2013). [DOI] [PubMed]
- 37.Bilu C, et al. Diurnality, Type 2 Diabetes, and Depressive-Like Behavior. J Biol Rhythms. 2019;34:69–83. doi: 10.1177/0748730418819373. [DOI] [PubMed] [Google Scholar]
- 38.Cohen R, Kronfeld-Schor N. Individual variability and photic entrainment of circadian rhythms in golden spiny mice. Physiology & Behavior. 2006;87:563–574. doi: 10.1016/j.physbeh.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 39.Blanchong JA, McElhinny TL, Mahoney MM, Smale L. Nocturnal and diurnal rhythms in the unstriped Nile rat, Arvicanthis niloticus. J Biol Rhythms. 1999;14:364–377. doi: 10.1177/074873099129000777. [DOI] [PubMed] [Google Scholar]
- 40.Hagenauer MH, Lee TM. Circadian organization of the diurnal Caviomorph rodent, Octodon degus. Biol. Rhythm Res. 2008;39:269–289. doi: 10.1080/09291010701683425. [DOI] [Google Scholar]
- 41.Tomotani Barbara M., Flores Danilo E. F. L., Tachinardi Patrícia, Paliza José D., Oda Gisele A., Valentinuzzi Verônica S. Field and Laboratory Studies Provide Insights into the Meaning of Day-Time Activity in a Subterranean Rodent (Ctenomys aff. knighti), the Tuco-Tuco. PLoS ONE. 2012;7(5):e37918. doi: 10.1371/journal.pone.0037918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Umezu T, Kuribara H, Tadokoro S. Characteristics of circadian rhythm of wheel-running activity and drinking behavior in Mongolian gerbils. Yakubutsu Seishin Kodo. 1989;9:369–373. [PubMed] [Google Scholar]
- 43.Daan Serge, Spoelstra Kamiel, Albrecht Urs, Schmutz Isabelle, Daan Moritz, Daan Berte, Rienks Froukje, Poletaeva Inga, Dell'Omo Giacomo, Vyssotski Alexei, Lipp Hans-Peter. Lab Mice in the Field: Unorthodox Daily Activity and Effects of a Dysfunctional Circadian Clock Allele. Journal of Biological Rhythms. 2011;26(2):118–129. doi: 10.1177/0748730410397645. [DOI] [PubMed] [Google Scholar]
- 44.Kronfeld-Schor N, Dayan T. Activity patterns of rodents: the physiological ecology of biological rhythms. Biol. Rhythm Res. 2008;39:193–211. doi: 10.1080/09291010701683268. [DOI] [Google Scholar]
- 45.Einat H, Kronfeld-Schor N, Eilam D. Sand rats see the light: Short photoperiod induces a depression-like response in a diurnal rodent. Behav Brain Res. 2006;173:153–157. doi: 10.1016/j.bbr.2006.06.006. [DOI] [PubMed] [Google Scholar]
- 46.Ashkenazy T, Einat H, Kronfeld-Schor N. We are in the dark here: induction of depression- and anxiety-like behaviours in the diurnal fat sand rat, by short daylight or melatonin injections. Int J Neuropsychopharmacol. 2009;12:83–93. doi: 10.1017/S1461145708009115. [DOI] [PubMed] [Google Scholar]
- 47.Bilu C, Einat H, Kronfeld-Schor N. Utilization of Diurnal Rodents in the Research of Depression. Drug Dev Res. 2016;77:336–345. doi: 10.1002/ddr.21346. [DOI] [PubMed] [Google Scholar]
- 48.Krivisky K, Ashkenazy T, Kronfeld-Schor N, Einat H. Antidepressants reverse short-photoperiod-induced, forced swim test depression-like behavior in the diurnal fat sand rat: further support for the utilization of diurnal rodents for modeling affective disorders. Neuropsychobiology. 2011;63:191–196. doi: 10.1159/000321805. [DOI] [PubMed] [Google Scholar]
- 49.Tal-Krivisky K, Kronfeld-Schor N, Einat H. Voluntary exercise enhances activity rhythms and ameliorates anxiety-and depression-like behaviors in the sand rat model of circadian rhythm-related mood changes. Physiology & Behavior. 2015;151:441–447. doi: 10.1016/j.physbeh.2015.08.002. [DOI] [PubMed] [Google Scholar]
- 50.Ashkenazy T, Einat H, Kronfeld-Schor N. Effects of bright light treatment on depression- and anxiety-like behaviors of diurnal rodents maintained on a short daylight schedule. Behav Brain Res. 2009;201:343–346. doi: 10.1016/j.bbr.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 51.Krivisky, K., Einat, H. & Kronfeld-Schor, N. Effects of morning compared with evening bright light administration to ameliorate short-photoperiod induced depression- and anxiety-like behaviors in a diurnal rodent model. J Neural Transm. 119, 1241-1248. Epub 2012 Mar 1213 (2012). [DOI] [PubMed]
- 52.Bilu C, et al. Red white and blue – bright light effects in a diurnal rodent model for seasonal affective disorder. Chronobiol Int. 2019;36:919–926. doi: 10.1080/07420528.2019.1595638. [DOI] [PubMed] [Google Scholar]
- 53.Flaisher-Grinberg S, Gampetro DR, Kronfeld-Schor N, Einat H. Inconsistent effects of photoperiod manipulations in tests for affective-like changes in mice: implications for the selection of appropriate model animals. Behav Pharmacol. 2011;22:23–30. doi: 10.1097/FBP.0b013e3283425012. [DOI] [PubMed] [Google Scholar]
- 54.Stukalin Y, Einat H. Analyzing test batteries in animal models of psychopathology with multivariate analysis of variance (MANOVA): One possible approach to increase external validity. Pharmacol Biochem Behav. 2017;28:30408–30402. doi: 10.1016/j.pbb.2017.11.003. [DOI] [PubMed] [Google Scholar]
- 55.Kalman, R., Ziv, E., Lazarovici, G. & Shafrir, E. Chapter 54 - Sand Rat. In The Laboratory Rabbit, Guinea Pig, Hamster, and Other Rodents 1171–1190 (Academic Press, Boston, 2012).
- 56.Kanety, H., Moshe, S., Shafrir, E., Lunenfeld, B. & Karasik, A. Hyperinsulinemia induces a reversible impairment in insulin receptor function leading to diabetes in the sand rat model of non-insulin-dependent diabetes mellitus. Proceedings of the National Academy of Sciences91, 1853–1857 (1994). [DOI] [PMC free article] [PubMed]
- 57.Kaiser, N., Cerasi, E. & Leibowitz, G. Diet-induced diabetes in the sand rat (Psammomys obesus). Animal Models in Diabetes Research, 89–102 (2012). [DOI] [PubMed]
- 58.Staels B. When the Clock stops ticking, metabolic syndrome explodes. Nature medicine. 2006;12:54. doi: 10.1038/nm0106-54. [DOI] [PubMed] [Google Scholar]
- 59.McIntyre RS, et al. Should depressive syndromes be reclassified as “metabolic syndrome type II”? Annals of Clinical Psychiatry. 2007;19:257–264. doi: 10.1080/10401230701653377. [DOI] [PubMed] [Google Scholar]
- 60.Yaffe K. Metabolic syndrome and cognitive disorders: is the sum greater than its parts? Alzheimer Disease & Associated Disorders. 2007;21:167–171. doi: 10.1097/WAD.0b013e318065bfd6. [DOI] [PubMed] [Google Scholar]
- 61.Gramaglia, C. et al. Increased Risk of Metabolic Syndrome in Antidepressants Users: A Mini Review. Frontiers in Psychiatry9 (2018). [DOI] [PMC free article] [PubMed]
- 62.West, A.C. et al. Misalignment with the external light environment drives metabolic and cardiac dysfunction. Nat Commun. 8, 417, 410.1038/s41467-41017-00462-41462 (2017). [DOI] [PMC free article] [PubMed]
- 63.Stenvers DJ, Scheer F, Schrauwen P, la Fleur SE, Kalsbeek A. Circadian clocks and insulin resistance. Nat Rev Endocrinol. 2019;15:75–89. doi: 10.1038/s41574-41018-40122-41571. [DOI] [PubMed] [Google Scholar]
- 64.Chaudhary R, Walder KR, Hagemeyer CE, Kanwar JR. Psammomys obesus: a Natural Diet-Controlled Model for Diabetes and Cardiovascular Diseases. Current atherosclerosis reports. 2018;20:46. doi: 10.1007/s11883-018-0746-6. [DOI] [PubMed] [Google Scholar]
- 65.Barak O, Kronfeld-Schor N. Activity rhythms and Masking response in the diurnal Fat Sand Rat under laboratory conditions. Chronobiology International. 2013;30:828–836. doi: 10.3109/07420528.2013.805337. [DOI] [PubMed] [Google Scholar]
- 66.Touati H, et al. Diet-induced insulin resistance state disturbs brain clock processes and alters tuning of clock outputs in the Sand rat, Psammomys obesus. Brain Research. 2018;1679:116–124. doi: 10.1016/j.brainres.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 67.Barnett M, Collier GR, Zimmet P, Odea K. The effect of restricting energy-intake on diabetes in Psammomys-obesus. International Journal of Obesity. 1994;18:789–794. [PubMed] [Google Scholar]
- 68.van der Vinne V, Gorter JA, Riede SJ, Hut RA. Diurnality as an energy-saving strategy: energetic consequences of temporal niche switching in small mammals. J Exp Biol. 2015;218:2585–2593. doi: 10.1242/jeb.119354. [DOI] [PubMed] [Google Scholar]
- 69.Neeman, E. Natural light in buildings - principles and planning directions. (Ministry of Energy, Israel 1999).
- 70.Bird RE, Hulstrom RL, Lewis L. Terrestrial solar spectral data sets. Solar energy. 1983;30:563–573. doi: 10.1016/0038-092X(83)90068-3. [DOI] [Google Scholar]
- 71.Stevenson, T.J. et al. Disrupted seasonal biology impacts health, food security and ecosystems. Proceedings of the Royal Society of London B: Biological Sciences282 (2015). [DOI] [PMC free article] [PubMed]
- 72.Dominoni, D. M., Borniger, J. C. & Nelson, R. J. Light at night, clocks and health: from humans to wild organisms. Biology Letters12 (2016). [DOI] [PMC free article] [PubMed]
- 73.Ouyang, J. Q., Davies, S. & Dominoni, D. Hormonally mediated effects of artificial light at night on behavior and fitness: linking endocrine mechanisms with function. Journal of Experimental Biology221 (2018). [DOI] [PMC free article] [PubMed]
- 74.Versteeg RI, et al. Nutrition in the spotlight: metabolic effects of environmental light. Proceedings of the Nutrition Society. 2016;75:451–463. doi: 10.1017/S0029665116000707. [DOI] [PubMed] [Google Scholar]
- 75.Qian J, Caputo R, Morris CJ, Wang W, Scheer FA. Circadian misaligment increases the desire for food intake in chronic shif workers. Sleep. 2018;41:A17–A17. doi: 10.1093/sleep/zsy061.040. [DOI] [Google Scholar]
- 76.Qian JY, Scheer F. Circadian System and Glucose Metabolism: Implications for Physiology and Disease. Trends in Endocrinology and Metabolism. 2016;27:282–293. doi: 10.1016/j.tem.2016.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Li M-D, Li C-M, Wang Z. The role of circadian clocks in metabolic disease. The Yale journal of biology and medicine. 2012;85:387. [PMC free article] [PubMed] [Google Scholar]
- 78.Kalsbeek A, et al. Circadian disruption and SCN control of energy metabolism. Febs Letters. 2011;585:1412–1426. doi: 10.1016/j.febslet.2011.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Panda, S. The arrival of circadian medicine. Nature ReviewsEndocrinology, 1 (2019). [DOI] [PubMed]
- 80.Noordam, R. et al. Associations of outdoor temperature, bright sunlight and cardiometabolic traits in two European population-based cohorts. The Journal of clinical endocrinology and metabolism (2019). [DOI] [PMC free article] [PubMed]
- 81.Zimmet PZ, Magliano DJ, Herman WH, Shaw JE. Diabetes: a 21st century challenge. The lancet Diabetes & endocrinology. 2014;2:56–64. doi: 10.1016/S2213-8587(13)70112-8. [DOI] [PubMed] [Google Scholar]
- 82.Pellow S, Chopin P, File SE, Briley M. Validation of open:closed arm entries in an elevated plus-maze as a measure of anxiety in the rat. J Neurosci Methods. 1985;14:149–167. doi: 10.1016/0165-0270(85)90031-7. [DOI] [PubMed] [Google Scholar]
- 83.Belzung C, Griebel G. Measuring normal and pathological anxiety-like behaviour in mice: a review. Behav Brain Res. 2001;125:141–149. doi: 10.1016/S0166-4328(01)00291-1. [DOI] [PubMed] [Google Scholar]
- 84.Bilu C, Kronfeld-Schor N. Effects of circadian phase and melatonin injection on anxiety-like behavior in nocturnal and diurnal rodents. Chronobiol Int. 2013;30:828–836. doi: 10.3109/07420528.2013.773439. [DOI] [PubMed] [Google Scholar]
- 85.Bilu C, et al. Red white and blue - bright light effects in a diurnal rodent model for seasonal affective disorder. Chronobiol Int. 2019;15:1–8. doi: 10.1080/07420528.2019.1595638. [DOI] [PubMed] [Google Scholar]