Abstract
The field of autoimmune epilepsy has evolved substantially in the last few decades with discovery of several neural autoantibodies and improved mechanistic understanding of these immune-mediated syndromes. A considerable proportion of patients with epilepsy of unknown etiology have been demonstrated to have an autoimmune cause. The majority of the patients with autoimmune epilepsy usually present with new-onset refractory seizures along with subacute progressive cognitive decline and behavioral or psychiatric dysfunction. Neural specific antibodies commonly associated with autoimmune epilepsy include leucine-rich glioma-inactivated protein 1 (LGI1), N-methyl-d-aspartate receptor (NMDA-R), and glutamic acid decarboxylase 65 (GAD65) IgG. Diagnosis of these cases depends on the identification of the clinical syndrome and ancillary studies including autoantibody evaluation. Predictive models (Antibody Prevalence in Epilepsy and Encephalopathy [APE2] and Response to Immunotherapy in Epilepsy and Encephalopathy [RITE2] scores) based on clinical features and initial neurological assessment may be utilized for selection of cases for autoimmune epilepsy evaluation and management. In this article, we will review the recent advances in autoimmune epilepsy and provide diagnostic and therapeutic algorithms for epilepsies with suspected autoimmune etiology.
Key Words: Autoimmune limbic encephalitis, Diagnosis, Epilepsy, Immunotherapy
Introduction
Epilepsy affects approximately 0.5% to 1.0% of the world’s population [1]. The etiology of a significant proportion of cases remains unknown [2]. Lately, the role of autoimmunity in epilepsy has been highlighted by multiple studies [3, 4]. In the latest 2017 epilepsy classification, the International League Against Epilepsy (ILAE) has recognized autoimmune epilepsy as a distinct entity [5].
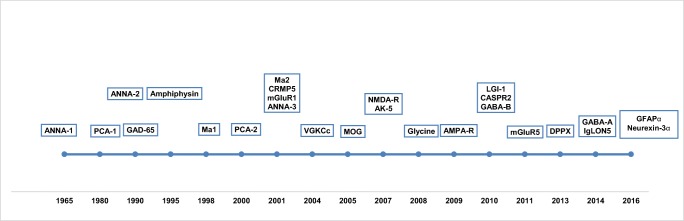
The link between epilepsy and neuroinflammation for syndromes such as Rasmussen’s encephalitis [6] has been speculated for decades. Furthermore, in the 1960s, initial cases of paraneoplastic limbic encephalitis associated with epilepsy were described [7]. Over the last few decades, multiple neural autoantibodies targeting cell surface or intracellular antigens associated with epilepsy and/or encephalopathy have been discovered (Fig. 1) [8]. Many more biomarkers with specific clinical and/or oncological associations are likely to be discovered over the coming years [9, 10]. These biomarker discoveries are likely to be accelerated with optimization of phage immunoprecipitation sequencing (PhIP-Seq), immunoprecipitation mass spectrometry, and protein microarray techniques [10–12].
Fig. 1.
Timeline of neural specific antibody discovery
Identification of immune-mediated epilepsy is critical as early initiation of immunotherapy has been associated with favorable clinical outcome [13]. Diagnosis of autoimmune epilepsy, in majority of the cases, is based on their clinical characteristics, magnetic resonance imaging (MRI) results, and cerebrospinal fluid (CSF) analysis. At times, immunotherapy trial is utilized for dual purpose of diagnosis and management, especially, in seronegative cases.
In this review article, we provide an overview of autoimmune epilepsy with emphasis on the recent advances regarding pathophysiology, imaging studies, and therapeutic interventions. We provide a diagnostic and therapeutic algorithm for epilepsies with suspected autoimmune etiology.
Epidemiology
The true incidence of autoimmune epilepsy remains unknown. There are no population-based studies providing age- and sex-adjusted incidence and prevalence of autoimmune epilepsy.
A recent population-based study from Olmsted county, MN, estimated the incidence and prevalence of autoimmune encephalitis to be 0.8/100,000 person-years and 13.7/100,000 people, respectively [14]. Interestingly, there was a significant increase in the incidence of autoimmune encephalitis in the last decade, with increased recognition of neural specific antibodies contributing to the diagnosis of definite autoimmune encephalitis [15]. However, only a subset of cases in this study had epilepsy as a part of their autoimmune syndrome. Additionally, case selection was based on proposed autoimmune encephalitis diagnostic criteria [16], and patients with epilepsy cases without cognitive impairment were excluded.
A hospital-based prospective study reported that 20% of adult patients with epilepsy of unknown etiology were seropositive for neural specific antibodies associated with autoimmune epilepsy or encephalopathy [4, 17]. However, there was clear difference in specificities of neural specific antibodies detected in patients with new-onset and chronic epilepsy. Leucine-rich glioma-inactivated protein 1 (LGI1) and N-methyl-d-aspartate receptor (NMDA-R) immunoglobulin G (IgG) were detected in new-onset epilepsies, whereas chronic epilepsies had a higher proportion of glutamic acid decarboxylase 65 (GAD65) IgG. Another UK-based retrospective study also estimated frequency of neural specific antibodies to be 15% among patients without a genetic, structural, or metabolic etiology for epilepsy [18]. Epilepsies of unknown etiology are estimated to constitute one-third of all epilepsies among adults [19]. Therefore, the rate of autoimmune epilepsies based on these studies can be inferred to be around 5 to 7% of all epilepsies, at least in adults. The frequency of autoantibodies in pediatric epilepsy is more unclear. Studies from Europe and Australia have reported the presence of autoantibodies in about 10% of pediatric patients with new-onset epilepsy [20, 21].
Pathophysiology
Discovery of neural specific antibodies has played a significant role in understanding the etiopathogenesis of autoimmune epilepsy. In some instances, the immunological trigger is an underlying occult tumor [22]. Tumor cells express onconeural antigen which then leads to a misdirected immune response contributing to neuronal dysfunction. Some of these antibody responses are tumor specific, e.g., antineuronal nuclear antibody type 1 (ANNA-1) IgG and small cell lung carcinoma, Ma-2 IgG, and testicular germ cell cancer (Table 1).
Table 1.
Clinical features of neural specific autoantibody–associated syndromes
| Antibody | Neurological presentations | Epilepsy association (3+, 2+, 1+) | Epilepsy presentations | Brain MRI | Specific cancer type (proportion of patients with cancer) |
|---|---|---|---|---|---|
| LGI1 | FBDS, piloerection seizures, PDS, limbic encephalitis, hyponatremia | 3+ | FBDS, unilateral piloerection, paroxysmal dizzy spells | Medial temporal FLAIR hyperintensity, T1 basal ganglia hyperintensity (FBDS cases) | Thymoma (10–15%) |
| GABA-B | SE, limbic encephalitis | 3+ | Crescendo seizures, SE is frequent. | Medial temporal FLAIR hyperintensity | Small cell lung cancer (50–60%) |
| GABA-A | SE, autoimmune encephalitis | 3+ | Crescendo seizures and status epilepticus | Multifocal cortical and subcortical hyperintensity | Thymoma (10–30%) |
| NMDA-R | Oral dyskinesia, catatonia, neuropsychiatric dysfunction, autonomic dysfunction, refractory epilepsy | 3+ | Crescendo seizures, status epilepticus, and encephalopathy (EEG: extreme delta-brush) | Normal or nonspecific cortical and/or subcortical changes | Ovarian teratoma (20–30%) |
| GAD65 | SPS, hyperekplexia, brainstem encephalitis (especially African–Americans) | 2+ | Multifocal epilepsy, drug-resistant epilepsy, rarely SE | Multifocal cortical and subcortical hyperintensity or brainstem hyperintensity | Lung carcinoma (small cell or nonsmall cell), Thymoma (< 10%) |
| AMPA-R | Limbic encephalitis | 2+ | SE has been reported | Cortical atrophy, deep gray nuclei FLAIR hyperintensity | Thymoma, small cell lung cancer, breast adenocarcinoma (50–70%) |
| mGluR5 | Encephalopathy, mood changes, movement disorder and seizures | 2+ | Seizures are common, SE in children | Normal in 50%, limbic/cortical FLAIR changes | Hodgkin lymphoma (50–70%) |
| ANNA-1/Hu | Limbic encephalitis, sensory neuronopathy, autonomic dysfunction | 2+ | Temporal and/or extratemporal seizures, rarely SE | Normal or medial temporal FLAIR hyperintensity | Small cell lung cancer, neuroendocrine tumors (> 70%) |
| Ma-1/Ma-2 | Limbic encephalitis, brainstem encephalitis | 2+ | Focal unaware seizure or bilateral tonic–clonic | Brainstem FLAIR hyperintensity or medial temporal FLAIR hyperintensity | Testicular germ cell tumor†, small cell lung cancer‡ (50–70%) |
| Amphiphysin | SPS, PERM, transverse myelitis | 2+ | Limbic encephalitis and seizures can occur in up to 30% of patients. | Normal or nonspecific cortical and/or subcortical changes | Small cell lung cancer, breast cancer (50–70%) |
| ANNA-2/Ri | Stridor, laryngospasm, jaw dystonia, opsoclonus myoclonus | 1+ | Seizures are rare | brainstem FLAIR hyperintensity and/or atrophy | Small cell lung cancer, breast cancer (> 70%) |
| CASPR-2 | Neuromyotonia, Morvan’s syndrome, limbic encephalitis, refractory epilepsy, sleep disorder | 1+ | Nonspecific | Normal or medial temporal FLAIR hyperintensity | Thymoma (10–20%) |
| Glycine | SPS, PERM | 1+ | Rarely associated with seizures | Normal or nonspecific cortical and/or subcortical changes | Thymoma (< 5%) |
| DPPX | Diarrhea, hyperekplexia, ambiguous sleep, parasomnias, PERM, | 1+ | Rarely associated with seizures | Normal or nonspecific cortical and/or subcortical changes | Lymphoma (< 10%) |
| GFAPα | Meningo-encephalomyelitis, tremor, ataxia, autonomic dysfunction | 1+ | Rarely associated with seizures | Peri-radial/patchy enhancement or diffuse subcortical hyperintensity | Ovarian teratoma (20%) |
| CRMP-5 | Choreoathetosis, optic neuritis, retinitis, limbic encephalitis, ataxia, transverse myelitis, polyradiculoneuropathy | 1+ | Rarely associated with seizures (focal aware and focal unaware) | Normal or medial temporal FLAIR hyperintensity | Small cell lung cancer, thymoma (50–70%) |
| Neurexin-3α | Prodrome of fever, headache and gastrointestinal symptoms followed by development of encephalopathy and seizures | 1+ | Limited data available | Normal | None |
| MOG | ADEM, ON, TM | 1+ | Focal seizures with secondary generalization and status epilepticus | Multifocal demyelination, involvement of corpus callosum, deep gray nuclei | None |
| AK5 | Limbic encephalitis | Rare | Limited data available. 1 patient reported to have seizure 6 months after disease onset | Bilateral medial temporal FLAIR hyperintensity | None |
| IgLON5 | Parasomnias, REM, and NREM dysfunction, brainstem dysfunction, hyperexcitability disorder | Rare | Rarely associated with nocturnal frontal lobe epilepsy | Normal or nonspecific cortical and/or subcortical changes | None |
ADEM = acute disseminated encephalomyelitis; AMPA-R = amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid; ANNA-1 = antineuronal nuclear antibody type 1; ANNA-2 = antineuronal nuclear antibody type 2; AK5 = adenylate kinase 5; CBA = cell-based assay; CASPR-2 = contactin-associated protein-like 2; CRMP-5 = collapsin response mediator protein-5; DPPX = dipeptidyl-peptidase-like protein 6; EMG = electromyography; FLAIR = fluid-attenuated inversion recovery; GABA-A = γ-aminobutyric acid type A; GABA-B = γ-aminobutyric acid type B; GAD65 = glutamic acid decarboxylase 65; GFAP = glial fibrillary acidic protein; LGI1 = leucine-rich glioma-inactivated protein 1; MOG = myelin oligodendrocyte glycoprotein; NMDA-R = N-methyl-d-aspartate receptor; ON = optic neuritis; PERM = progressive encephalomyelitis with rigidity and myoclonus; PDS = Paroxysmal dizzy spells, REM = rapid eye movement; SPS = stiff person syndrome; TM = transverse myelitis; WB = Western blot
*Coexisting LGI1 and CASPR-2 antibodies
†Ma-2 antibodies
‡Ma-1 antibodies with or without Ma-2 antibodies
Infection is another potential trigger for autoimmune neurological syndrome [23]. Different mechanisms including molecular mimicry, epitope spreading, and bystander activation have been postulated. Structural and/or amino acid sequence similarity between pathogen and self-antigen leading to a cross-reactive immune response is the basis for molecular mimicry. Secondly, cellular damage by an infection may lead to release of putative autoantigen, triggering an autoimmune response. Thirdly, the infection may lead to activation of autoreactive lymphocytes and antigen-presenting cells leading to an immune response against self-antigens. An example of infectious trigger leading to autoimmunity is the association of herpes simplex virus encephalitis and NMDA-R encephalitis [24].
Autoantigen can be divided based on their cellular localization into cell surface or intracellular epitopes. Some cell surface antibodies have a direct pathogenic role. Both LGI1 and NMDA-R antibodies are two such examples which target extracellular epitopes. LGI1 IgG has been postulated to cause pathogenic effect by ion channel deficiency. LGI1 IgG leads to disruption of LGI1–ADAM22 interaction which reduces synaptic α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor function, subsequently disrupting calcium influx [25, 26]. On the other hand, NMDA-R IgG binds to a region of the GluN1 subunit of NMDA-R. This disrupts the interaction between NMDAR and ephrin type B2 receptor, and initiates internalization of NMDA-R contributing to neuronal dysfunction [27]. The process of internalization is reversible, and good recovery has been demonstrated with removal of NMDA-R IgG [28].
Antibodies against intracellular autoantigens such as anti-Hu or anti-Yo are surrogate biomarkers; neuronal injury is attributed to CD8+ cytotoxic T-cell response. These antibodies and neurotoxic T cells may share the same autoantigen specificity, e.g., Ant-Yo (CDR2) paraneoplastic syndrome [29].
Clinical Presentation
Patients with autoimmune epilepsy usually present with new onset of refractory seizures with one or more coexisting features of autoimmune encephalitis including subacute progressive cognitive decline, psychiatric symptoms, viral prodrome, autonomic dysfunction, inflammatory CSF, oncological association, or brain MRI changes consistent with autoimmune encephalitis [11]. The optimal selection of patients based on their clinical characteristics for neural specific antibody evaluation is critical.
Prediction of neural autoantibody specificities based on clinical characteristics can be difficult due to overlapping features, one of the exceptions being a faciobrachial dystonic seizure which is pathognomic for LGI1 IgG. Therefore, both serum and CSF should be tested to avoid false negative and false positive test results. Specifically, NMDA-R IgG and glial fibrillary acidic protein IgG testing is more sensitive and specific in the CSF [28, 30]. Furthermore, detection of GAD65 IgG in the CSF (even in low titers) is supportive of neurological autoimmunity but low serum GAD65 IgG titers can be nonspecific [31, 32]. Whereas, CSF is less sensitive than serum in detection of LGI1 or contactin-associated protein-like 2 (CASPR-2) IgG.
In this regard, a predicative model (Antibody Prevalence in Epilepsy and Encephalopathy [APE2] score) based on clinical features and initial neurological assessment can be utilized (Table 2) [3, 4, 17, 33]. Furthermore, a scoring system to predict favorable response to initial immunotherapy (Response to Immunotherapy in Epilepsy and Encephalopathy [RITE2] score) may also be used for management of these patients. (Table 2) [17]. For prediction of neural specific antibody seropositivity, an APE2 score ≥ 4 in patients with epilepsy of unknown etiology was demonstrated to have a sensitivity and specificity of 98% and 85% respectively. An APE2 score ≥ 7 had specificity of 100% for an autoimmune etiology of epilepsy. For patient receiving first-line immunotherapy, RITE2 score ≥ 7 has a sensitivity and specificity of 88% and 84% respectively [3].
Table 2.
Components of the APE2 score (1A) and RITE2 score (1B). RITE2 score included all the components of APE2 score and 2 additional variables: initiation of immunotherapy within 6 months of symptom onset and plasma membrane–specific autoantibody detected (1B). The assigned APE2 and RITE2 scores are the sum of values for all components
| 1A: Antibody Prevalence in Epilepsy and Encephalopathy (APE2) score | Value | 1B: Response to Immunotherapy in Epilepsy and Encephalopathy (RITE2) score | Value |
|---|---|---|---|
| New-onset, rapidly progressive mental status changes that developed over 1–6 weeks or new-onset seizure activity (within 1 year of evaluation) | (+1) | New-onset, rapidly progressive mental status changes that developed over 1–6 weeks or new-onset seizure activity (within 1 year of evaluation) | (+1) |
| Neuropsychiatric changes: agitation, aggressiveness, emotional lability | (+1) | Neuropsychiatric changes: agitation, aggressiveness, emotional labiality | (+1) |
| Autonomic dysfunction (sustained atrial tachycardia or bradycardia, orthostatic hypotension, hyperhidrosis, persistently labile blood pressure, ventricular tachycardia, cardiac asystole or gastrointestinal dysmotility)* | (+1) | Autonomic dysfunction (sustained atrial tachycardia or bradycardia, orthostatic hypotension, hyperhidrosis, persistently labile blood pressure, ventricular tachycardia, cardiac asystole or gastrointestinal dysmotility)* | (+1) |
| Viral prodrome (rhinorrhea, sore throat, low-grade fever) to be scored in the absence of underlying systemic malignancy within 5 years of neurological symptom onset | (+2) | Viral prodrome (rhinorrhea, sore throat, low-grade fever) only to be scored in the absence of underlying malignancy within 5 years of neurological symptom onset | (+2) |
| Faciobrachial dystonic seizures | (+3) | Faciobrachial dystonic seizures | (+3) |
| Facial dyskinesias, to be scored in the absence of faciobrachial dystonic seizures | (+2) | Facial dyskinesias, to be scored in the absence of faciobrachial dystonic seizures | (+2) |
| Seizure refractory to at least to two antiseizure medications | (+2) | Seizure refractory to at least to two antiseizure medications | (+2) |
| CSF findings consistent with inflammation† (elevated CSF protein > 50 mg/dL and/or lymphocytic pleocytosis > 5 cells/mcL, if the total number of CSF RBC is < 1000 cells/mcL) | (+2) | CSF findings consistent with inflammation† (elevated CSF protein > 50 mg/dL and/or lymphocytic pleocytosis > 5 cells/mcL, if the total number of CSF RBC is < 1000 cells/mcL) | (+2) |
| Brain MRI suggesting encephalitis (T2/FLAIR hyperintensity restricted to one or both medial temporal lobes, or multifocal in gray matter, white matter, or both compatible with demyelination or inflammation) | (+2) | Brain MRI suggesting encephalitis (T2/FLAIR hyperintensity restricted to one or both medial temporal lobes, or multifocal in gray matter, white matter, or both compatible with demyelination or inflammation) | (+2) |
| Systemic cancer diagnosed within 5 years of neurological symptom onset (excluding cutaneous squamous cell carcinoma, basal cell carcinoma, brain tumor, cancer with brain metastasis) | (+2) | Systemic cancer diagnosed within 5 years of neurological symptom onset (excluding cutaneous squamous cell carcinoma, basal cell carcinoma, brain tumor, cancer with brain metastasis) | (+2) |
| Total (max, 18) | Immunotherapy initiated within 6 months of symptom onset | (+2) | |
| Neural plasma membrane autoantibody detected (NMDA-R, GABAAR, GABABR, AMPA-R, DPPX, mGluR1, mGluR5, LGI1, CASPR-2, neurexin-3α, MOG) | (+2) | ||
| Total (max, 22) |
ANNA-1 = antineuronal nuclear antibody 1; ANNA-2 = antineuronal nuclear antibody 2; ANNA-3 = antineuronal nuclear antibody 3; AMPA-R = amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid; CASPR-2 = contactin-associated protein 2; DPPX = dipeptidyl-peptidase-like protein 6; FLAIR = fluid-attenuated inversion recovery; GABAAR = γ-aminobutyric acid A receptor; GABABR = γ-aminobutyric acid B receptor; GFAPα = glial fibrillary acidic protein; LGI1 = leucine-rich glioma-inactivated protein 1; MOG = myelin oligodendrocyte glycoprotein; mGluR1 = metabotropic glutamate receptor 1; mGluR5 = metabotropic glutamate receptor 5; NMDA-R = N-methyl-d-aspartate receptor
*Scored only if no history of autonomic dysfunction prior to onset of suspected autoimmune syndrome and the autonomic dysfunction not attributable to medications, hypovolemia, plasmapheresis, or infection
†Patients scored zero if brain MRI or CSF analysis not performed
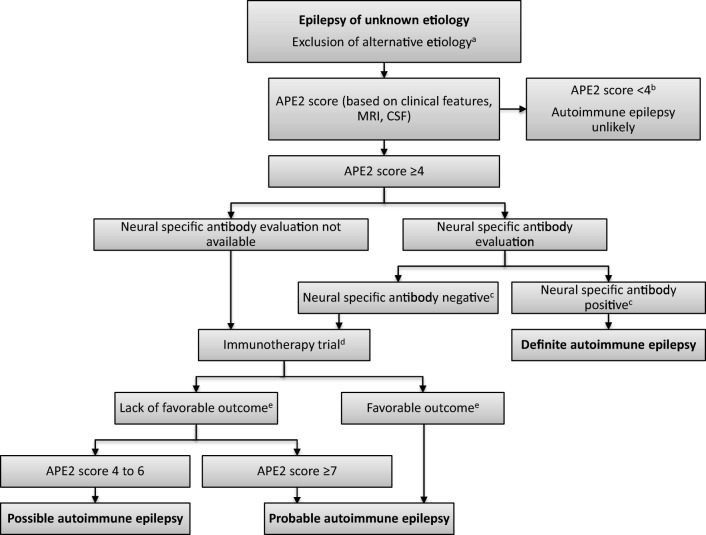
Using APE2 score, neural specific antibody serum status, and trial of immunotherapy, a diagnostic criterion for autoimmune epilepsy has been proposed [3]. Patients have been classified into either “definite autoimmune epilepsy,” “probable autoimmune epilepsy,” or “possible autoimmune epilepsy” (Fig. 2). All patients with epilepsy of unknown etiology and APE2 score ≥ 4 should undergo autoantibody evaluation. If the neural specific antibodies clinically validated to be associated with autoimmune epilepsy are positive, these cases meet the criteria for “definite autoimmune epilepsy.” For patients with epilepsy of unknown etiology despite thorough workup and negative autoantibody evaluation who have an APE2 score ≥ 4, a diagnostic trial of immunotherapy (as described later) should be considered. A favorable response to immunotherapy trial (defined as > 50% reduction in seizure frequency after immunotherapy) or an APE2 score ≥ 7 irrespective of immunotherapy trial outcome (due to higher specificity for autoimmune etiology) supports the diagnosis of “probable autoimmune epilepsy.”
Fig. 2.
Proposed autoimmune epilepsy diagnostic criteria stratifying patients based on APE2 score and immunotherapy trial into “definite,” “possible,” or “probable” autoimmune epilepsy. APE2 = Antibody Prevalence in Epilepsy and Encephalopathy; CSF = cerebrospinal fluid; MRI = magnetic resonance imaging. Superscript letter “a” indicates reasonable exclusion of alternative etiology (genetic, infectious encephalitis, neoplasm, neurodegenerative process, metabolic or toxic encephalopathy). Superscript letter “b” indicates rare patients with leucine-rich glioma-inactivated protein 1 antibody and mild presentation was found to have APE2 score < 4. Superscript letter “c” indicates neural specific antibodies clinically validated to have an association with autoimmune epilepsy (AMPA-R = amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor, amphiphysin; AK5 = adenylate kinase 5; ANNA-1 = antineuronal nuclear antibody 1; ANNA-2 = antineuronal nuclear antibody 2; ANNA-3 = antineuronal nuclear antibody 3; DPPX = dipeptidyl-peptidase-like protein 6; CASPR-2 = contactin-associated protein 2; CRMP-5 = collapsin response mediator protein-5; GAD65 = glutamic acid decarboxylase 65 (serum > 20 nmol/L or CSF detected); GABABR = γ-aminobutyric acid B receptor; GABAAR = γ-aminobutyric acid A receptor; GFAPα = glial fibrillary acidic protein (CSF detected), IgLON5; LGI1 = leucine-rich glioma-inactivated protein 1, Ma-1/Ma-2; MOG = myelin oligodendrocyte glycoprotein; mGluR5 = metabotropic glutamate receptor 5, Neurexin-3α; NMDA-R = N-methyl-d-aspartate receptor (preferably CSF detected), PCA2 = Purkinje cell antibody type 2, PCA Tr) evaluated and confirmed by latest and validated techniques. Superscript letter “d” indicates standardized immunotherapy trials should be considered. 12-week IVMP trial: 1 g, intravenously once per day for 3 consecutive days, then once weekly for 5 weeks, followed by once every 2 weeks for 6 weeks, for total 12 weeks’ therapy; 6-week IVMP trial: 1 g, intravenously once per day for 3 consecutive days, then once weekly for 5 weeks; 12-week IVIG trial: 0.4 g/kg daily for 3 days followed by 0.4 g/kg every week for 6 weeks and then every 2 weeks for 6 weeks; 6-week IVIG trial: 0.4 g/kg daily for 3 days followed by 0.4 g/kg every week for 6 weeks. Superscript letter “d” indicates > 50% reduction in seizure frequency
Cell Surface Epitopes
N-Methyl-d-Aspartate Receptor IgG
N-methyl-d-aspartate receptor (NMDA-R) encephalitis typically affects young women with a reported median age of 22 years (range, 2 months–85 years) [34]. Clinical presentation usually begins with a prodrome of a headache or fever, followed by psychiatric manifestations including delusions, hallucinations, mania-like episodes, alternating episodes of extreme agitation, and catatonia. Patients then progress to develop seizures, encephalopathy, oral dyskinesia, choreoathetosis, and autonomic dysfunction [35]. Seizures in NMDA-R encephalitis are usually focal nonmotor seizures that might progress to refractory status epilepticus [36]. If untreated, patients will progress to a comatose state [35].
In about half of the patients, a trigger can be identified. The two main triggers are the presence of ovarian teratoma [37] and a history of herpes simplex virus (HSV) encephalitis [24]. Approximately two-thirds of adult women between ages 18 and 45 years with NMDA-R encephalitis have been reported to have ovarian teratoma [35]. However, presence of this tumor is extremely rare in children younger than 12 years or older adults (≥ 45 years) [8, 35, 38]. Furthermore, prospective evaluation of HSV encephalitis patients showed that 17% of these cases developed NMDA-R encephalitis during follow-up. Three additional patients in this cohort were positive for NMDA-R IgG without any clinical features of autoimmune encephalitis on follow-up evaluation [24].
Recent human leukocyte antigen (HLA) studies in NMDA-R encephalitis demonstrated a weak association of patients with adult-onset patients with major histocompatibility complex (MHC) I allele B*07:02 [39].
Leucine-Rich Glioma-Inactivated Protein 1 IgG
LGI1 IgG is typically associated with seizures and memory deficits usually among older patients (> 40 years). However, a few pediatric cases have also been described [40]. One characteristic phenotype described among the adult patients is faciobrachial dystonic seizures (FBDS). These are brief focal dystonic motor seizures occuring multiple times a day. They have a characteristic stereotypic contraction of the face, arm, and leg [41]. Another, characteristic seizure semiology is unilateral piloerection episodes. More recently, paroxysmal dizzy spells have also described in a subset of patients [42]. These “dizzy spells” or “out of body experiences” may precede encephalopathy by 2 to 12 months.
HLA analysis of LGI1 encephalitis has shown strong association with a 27 single-nucleotide polymorphisms (SNPs) in the HLA-II region and MHC class II haplotypes DRB1*07:01, DQA1*02:01, and DQB1*02:02 [39].
A minority (~ 2%) of patients with voltage-gated potassium channel–complex (VGKCc) antibodies have coexisting CASPR-2 IgG. Peripheral nervous system involvement is more common (neuromyotonia, myokymia, or dysautonomia) among these patients. However, a considerable proportion of patients, especially older patients, may have coexisting epilepsy or encephalitis. VGKCc IgG in the absence of LGI1 and/or CASPR-2 IgG seropositivity may not be a specific biomarker of autoimmunity [43, 44].
α-Amino-3-hydroxy-5-methyl-4-isoxazolepropionic Acid IgG
AMPA receptor antibodies are directed against GluR1 and GluR2 subunits causing downregulation of the receptor and decrease its synaptic clustering. The median age of onset is around 60 years [35]. AMPA receptor encephalitis typically presents with classic limbic encephalitis symptoms (anterograde memory deficits, retrograde amnesia, mood changes, and temporal lobe seizures). Recent studies have supported direct antibody-mediated pathogenicity [45, 46]. Two-thirds of the patients have underlying malignancy, mainly small cell lung cancer and thymoma [47]. Few patients can have a refractory course despite aggressive immunotherapy and go on to develop diffuse cortical atrophy [45, 46, 48].
γ-Aminobutyric Acid Type B IgG
γ-Aminobutyric acid type B (GABA-B) receptors are linked to G protein–gated potassium channels. GABA-B receptor encephalitis usually presents as refractory nonconvulsive status epilepticus [35]. The majority of patients are older adult males (median age, 61 years) [8]. In 50 to 60% of cases, an underlying malignancy is detected, most commonly small cell lung carcinoma.
GABA-A Receptor IgG
Fulminant encephalitis and refractory seizures or status epilepticus have been associated with GABA-A receptor encephalitis. These patients have characteristic multifocal asynchronous cortical and subcortical T2/fluid-attenuated inversion recovery (FLAIR) hyperintensities [36]. The age of symptom onset tends to be younger (median age, 40 years) than that of cases with GABA-B encephalitis [8].
Dipeptidyl-Peptidase-Like Protein 6 IgG
Dipeptidyl-peptidase-like protein 6 (DPPX) is a cell surface auxiliary subunit of the Kv4.2 potassium channel family. Patients with DPPX antibody–associated encephalitis can also have seizures as part of the syndrome. The characteristic clinical manifestations include gastrointestinal dysmotility, weight loss, cognitive dysfunction, delirium, hyperekplexia, myoclonus, parasomnias, and occasionally progressive encephalomyelitis with rigidity and myoclonus (PERM) [35, 49].
Metabotropic Glutamate Receptor 5 IgG
In 1982, Ian Carr described a neuropsychiatric syndrome of bizarre behavior, depression, memory loss, and hallucinations in his 15.5-year-old daughter. She was diagnosed with Hodgkin’s lymphoma and underwent treatment, leading to significant neurological recovery. He named it “Ophelia syndrome” after a character from Shakespeare’s play “Hamlet” [50]. Dr. Carr speculated a humorally mediated paraneoplastic mechanism “perhaps a circulating neurotransmitter-like molecule secreted by the tumor.” In 2011, metabotropic glutamate receptor 5 (mGlur5) IgGs were found in two patients with clinical manifestations consistent with Ophelia syndrome (subacute onset of encephalopathy, mood changes, seizures, and Hodgkin’s lymphoma) [51]. In a recent series of 11 mGlur5 IgG–seropositive patients, 5 were found to have Hodgkin’s lymphoma and 1 small cell lung cancer [52]. Neuropsychiatric dysfunction, movement disorder, sleep disorder, and seizures were the common clinical manifestations. Five of the 11 cases had limbic system involvement on brain MRI, and 4 had changes in the extralimbic region. In 2 patients, status epilepticus was reported as the presenting clinical feature.
Intracellular Epitopes
Glutamic Acid Decarboxylase (65 kd) IgG
GAD65 antibodies (serum titers > 20 nmol/L or detection in CSF) are associated with various autoimmune neurological diseases including autoimmune epilepsy, stiff person syndrome, cerebellar ataxia, limbic encephalitis, and PERM [53, 54]. Women are more frequently affected than men, and the median age of symptom onset is 30 years (range, 5–80 years) [36]. In a study of 112 patients with unexplained adult-onset focal epilepsy, 5.4% were found to have high titers of GAD65 antibodies (> 1000 U/mL) [55]. Usually, patients with GAD65 antibodies (serum titers > 20 nmol/L or detection in CSF) are associated with a treatment–refractory course [54, 55]. The refractory nature of the disease is postulated to be secondary to cell-mediated cytotoxicity rather than a direct antibody-mediated pathogenesis.
Antineuronal Nuclear Antibody Type 1 (a.k.a. anti-Hu) IgG
Patients with ANNA-1 IgG antibodies present with various central and peripheral nervous system manifestations. ANNA-1 IgG seropositivity has a strong association with small cell cancer (81%). HuD-specific T cells are postulated to play a major role in pathogenicity of the paraneoplastic syndrome [56]. Sensory neuronopathy and autonomic dysfunction, especially gastroparesis, are hallmarks of ANNA-1 autoimmunity [15]. However, a few patients (10–17%) also present with limbic encephalitis and/or refractory seizures. Seizures can be temporal or extratemporal in onset [57].
ANNA-2 (a.k.a. anti-Ri) IgG
Seizures and limbic encephalitis have been reported among patients with ANNA-2 IgG (a.k.a. anti-Ri). However, a typical clinical manifestation is brainstem or cerebellar syndrome including ataxia, nystagmus, opsoclonus–myoclonus, jaw-opening dystonia, and laryngospasms [58].
Ma-2 or PNMA Family Member 2 IgG
Ma-2 IgG patients usually have a limbic encephalitis or brainstem encephalitis phenotype. A retrospective study of Ma-2 IgG–seropositive patients reported bilateral tonic–clonic or focal unaware seizures in 12 out of 27 (44%) patients [59]. Majority of Ma-2 IgG patients have either testicular germ cell tumor (especially young men) or small cell lung cancer (older patients with coexisting Ma-1 IgG) [60]. Favorable clinical outcomes have been associated with the absence of coexisting Ma-1 antibody, male gender, younger age (< 45 years), and presence of testicular tumor with complete response to treatment.
Collapsin Response Mediator Protein-5 IgG
Collapsin response mediator protein-5 (CRMP-5) IgG is a paraneoplastic biomarker of small cell lung cancer or thymoma [61]. Patients with CRMP-5 IgG usually manifest with various neurologic signs including limbic encephalitis, chorea, cranial neuropathy, cerebellar ataxia, myelopathy, and polyradiculoneuropathy [36, 62, 63]. Focal aware and unaware seizures have also been reported among CRMP-5-seropositive patients. Management of underlying malignancy and early initiation of immunotherapy is critical for better clinical outcome [64].
Other Presumed Immune-Mediated Epilepsies
Rasmussen’s Encephalitis
Rasmussen’s encephalitis is a rare chronic neurological disorder suspected to have an immune-mediated pathogenesis. It is characterized by drug-resistant focal motor epilepsy (epilepsia partialis continua), cognitive decline, hemiplegia, and unilateral hemispheric brain atrophy [7]. The majority of the cases have onset during childhood. Three different disease stages have been described. The first phase is the “prodromal stage” characterized by relatively low seizure frequency and usually no hemiparesis. The second phase is the “acute stage” which is characterized by frequent intractable seizures and progressive neurological deterioration (hemiparesis, hemianopia, cognitive deterioration, and aphasia if dominant hemisphere) and radiological evidence of brain atrophy. The third phase is the “residual stage” during which seizure frequency decreases, and the patient develops permanent and stable neurological deficits [65].
CSF analysis among these patients may be normal or may demonstrate lymphocytic pleocytosis and elevated CSF protein. Electroencephalogram (EEG) findings are usually characterized by emerging persistent delta activity over the affected hemisphere with contralateral normal background rhythm [66]. With disease progression, the contralateral side also develops inter-ictal epileptiform discharges. Focal ictal rhythmic discharges migrating from the affected cortical hemisphere with clinical events have been described. However, no disease-specific electrographic signature has been associated with syndrome. Brain MRI demonstrates unilateral cortical and/or subcortical regions T2/FLAIR hyperintensity and atrophy. The MRI changes are most prominent in the perisylvian area. Fluorodeoxyglucose positron emission tomography (FDG-PET) scan usually demonstrates hypermetabolism on the affected hemisphere [7, 65]. Variable responses to immunotherapy have been reported in several case reports. A randomized trial of tacrolimus or intravenous immune globulin (IVIG) showed slowing down of tissue and function loss with either therapies, and prevented development of intractable epilepsy [67]. At present, hemispherectomy continues to be the preferred approach in severely disabled immunotherapy refractory patients for seizure control and arresting the neurological decline [68].
New-Onset Refractory Status Epilepticus
Diagnosis of new-onset refractory status epilepticus (NORSE) should be considered, when a previously healthy individual develops refractory de novo seizures and status epilepticus with no readily identifiable etiology. NORSE can affect patients of all ages. A retrospective study exploring NORSE in the adult population has shown a significant percentage of these patients to have immune-mediated etiologies, primarily antibody-mediated encephalitis [69]. Various treatments have been tried, including antiseizure medications, achieving burst suppression with anesthetics, and dietary therapy with modest and variable effects [70]. Immunotherapy has been associated with favorable outcomes (5–33%) in a few cases [70].
Ancillary Studies in Autoimmune Epilepsy
Electroencephalogram
EEG plays a vital role in diagnosis and management of autoimmune epilepsy and encephalitis. Long-term monitoring is utilized among patients with subclinical or clinical status epilepticus [71]. Additionally, EEG can also be utilized to evaluate response to immunotherapy and anti-epileptic drugs in some instances.
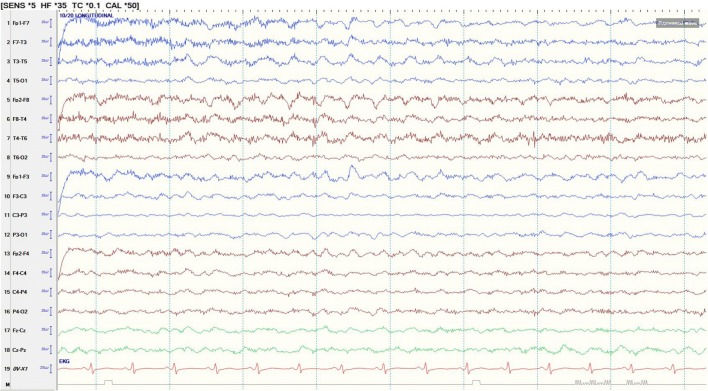
EEG findings in autoimmune encephalitis are variable and may be nonspecific. Extreme delta brush (EDB) has been described as characteristic finding in NMDA encephalitis patients [72]. This EEG pattern consists of rhythmic delta activity at 1 to 3 Hz with superimposed burst of rhythmic beta activity at 20 to 30 Hz riding on each delta wave. EDB has been reported in approximately 30% of NMDA encephalitis patients (Fig. 3). Although, recent studies have described the presence of EDB with other metabolic and structural causes of encephalopathy as well [73].
Fig. 3.
Extreme delta brush in a patient with NMDA-R encephalitis. Anterior–posterior bipolar montage. Sensitivity, 5 μV; high pass filter, 35 Hz
In a small series of LGI1 encephalitis patients, multiple frequent seizure semiologies or subclinical seizures associated with temporal and frontal discharges were reported [74]. Multifocal inter-ictal epileptiform discharges and inter-ictal slow-wave activity were observed in 25% and 69% patients, respectively. Ictal EEG during FBDS is usually obscured by prominent muscle artifact [74]. However, rhythmic delta activity over the contralateral frontotemporal region followed by diffuse EEG attenuation can occasionally be seen [74].
Imaging
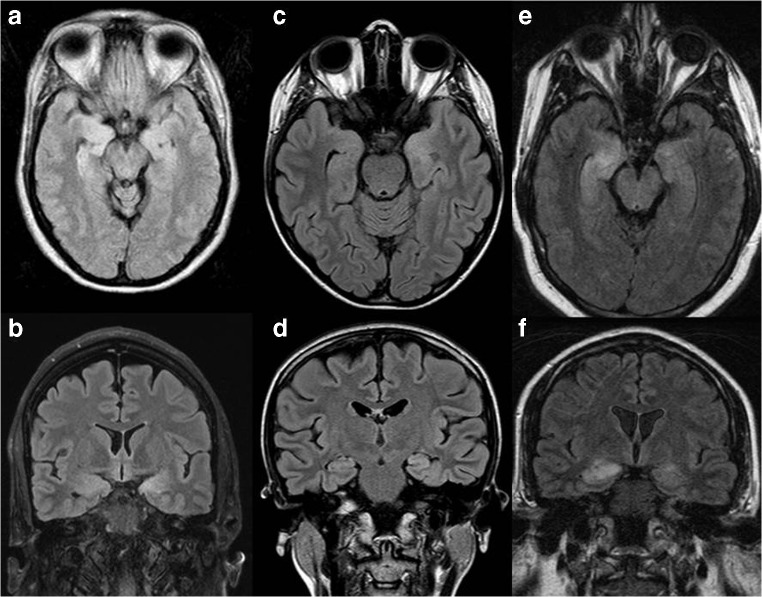
Brain MRI is usually included as part of the initial diagnostic workup for new-onset epilepsy or encephalitis. Radiological features which can be suggestive of autoimmune encephalitis include T2/FLAIR hyperintensity restricted to one or both medial temporal lobes (Fig. 4A–D), or multifocal T2/FLAIR hyperintensities in the gray matter, white matter, or both compatible with demyelination or inflammation (Fig. 4E, F) [75]. However, MRI may be normal especially early in the course of the disease [76, 77]. Brain MRI also provides valuable information regarding differential diagnosis of new-onset epilepsy like brain tumors, brain abscess, neurosarcoidosis, and other inflammatory and infectious etiologies. Volumetric MRI analysis has demonstrated dynamic amygdala enlargement may be an early radiological biomarker of autoimmune epilepsy in the subset of patients [78].
Fig. 4.
(A–E) Patient 1 with LGI1 IgG limbic encephalitis. Brain MRI (FLAIR sequence) demonstrating bilateral medial temporal hyperintensities on axial (A) and sagittal (B) sections. Patient 2 with ANNA-1 IgG limbic encephalitis. Brain MRI (FLAIR sequence) demonstrating bilateral medial temporal hyperintensities on axial (C) and sagittal (D) sections. Patient 3 with Ma-2 IgG limbic encephalitis. Brain MRI (FLAIR sequence) demonstrating bilateral medial temporal (right greater than left) hyperintensities on axial (E) and sagittal (F) sections. ANNA-1 = antineuronal nuclear antibody-1; FLAIR = fluid-attenuated inversion recovery; LGI1 = leucine-rich glioma-inactivated protein 1
Beside brain MRI, abnormalities in functional MRI [79], diffusion tensor imaging (DTI) [79], FDG-PET/CT [80, 81], and single-photon emission computed tomography (SPECT) [82] have been described in patients with autoimmune epilepsy and can provide valuable diagnostic and, at times, prognostic values. Several studies have reported a higher sensitivity of FDG-PET compared with MRI, especially early in the disease course [83].
Early in the disease course of NMDA-R encephalitis, the brain MRI may be normal or have nonspecific changes [34, 84]. However, resting-state functional MRI shows disrupted hippocampal functional connectivity. Moreover, DTI has demonstrated widespread white matter damage that correlated with disease severity [79]. FDG-PET/CT shows decreased occipital lobe metabolism, which is a unique finding in some of these patients [81]. Resolution of lateral and medial occipital hypometabolism may correlate with clinical improvement.
In LGI1 encephalitis, brain MRI findings vary depending on the stage of the disease and the progression [85]. In the early phase of the disease, brain MRI is typically normal although basal ganglia abnormalities including increased FLAIR signal, restricted diffusion, and contrast enhancement have been reported [85]. Patients with FBDS may develop T1 hyperintensity in the region of the basal ganglia [86]. As the disease progress, unilateral or bilateral T2/FLAIR hyperintensities of the medial temporal lobes and basal ganglia are observed. Long-term follow-up MRI may demonstrate hippocampal atrophy, at times consistent with mesial temporal sclerosis [84]. Basal ganglia hypermetabolism on FDG-PET/CT is another early and specific imaging finding which may aid in the diagnosis of LGI1 encephalitis [87].
Majority of the patients with autoimmune epilepsy associated with GAD65 antibody have disproportionate parenchymal (cerebral and cerebellar) atrophy for age and abnormal cortical/subcortical T2 hyperintensities on brain MRI. A minority of patients (26%) have hippocampal abnormalities (including T2 hyperintensities and enlargement of amygdala/hippocampus) [88].
Patients with GABA-A receptor encephalitis have a unique pattern of multifocal cortical and subcortical FLAIR hyperintensity [89]. Most of these cortical and subcortical abnormalities are not associated with gadolinium enhancement.
Medial temporal lobe involvement has been reported in multiple antibody specificities including LGI1 IgG, AMPA-R [90], GABA-B receptor IgG [91], ANNA-1 IgG [57], Ma-2 IgG [59], mGluR5 [52], and adenylate kinase 5 [92]. Majority of these cases do not have associated gadolinium enhancement except for Ma-2 IgG–associated limbic encephalitis [59].
Cancer Screening
CT of the chest, abdomen, and pelvis with contrast is recommended as the initial evaluation for cancer association. Scrotal ultrasounds should be performed in all males, when an autoimmune or paraneoplastic etiology is suspected. In women, mammograms are the gold standard for evaluation of breast cancer. Transvaginal sonography and pelvic MRI are recommended for ovarian teratoma or adenocarcinoma screening. If initial radiological evaluations did not reveal any malignancies and clinical suspicion for paraneoplastic neurological syndrome is high or the patient has neural specific antibody with strong oncological association (Table 1), PET-CT should be pursued [16, 93]. If the patient’s evaluation reveals a neoplasm other than the one predicted by the onconeural antibody present, further cancer evaluation should be performed as more than 1 cancer can coexist [93].
Treatment
Treatment of patients with autoimmune epilepsy is comprised of immunotherapy, removal of an immunologic trigger such as a tumor (when applicable), and symptomatic therapy including antiseizure medications. Multiple studies have demonstrated favorable effects of early initiation of immunotherapy on seizure frequency and cognition [13, 17, 94, 95]. However, randomized control trials evaluating efficacy immunotherapy in autoimmune epilepsy are lacking. Current immunotherapy recommendations are based on case series and clinical experience [34, 96].
Immunotherapeutic agents are classically divided into first-line (acute phase) and second-line therapies (maintenance phase) (Table 3). First-line therapies include high-dose intravenous methylprednisolone (IVMP), intravenous immune globulin (IVIG), or plasma exchange (PLEX). Second-line agents such as rituximab, cyclophosphamide, mycophenolate, azathioprine, bortezomib, or tocilizumab are used in refractory cases or as a maintenance therapy to prevent relapses.
Table 3.
Review of dosing, mechanism of action, adverse effects, and monitoring of various immunomodulatory agents
| Immunomodulatory agent | Route of administration | Dosing/regimen | Mechanism of action | Adverse effects | Monitoring and prophylaxis |
|---|---|---|---|---|---|
| Corticosteroids | IV or PO |
Initial dose: IV methylprednisolone (1 g per day for 3–5 days) 6 week trial: 1 g per day for 3 days followed by once weekly for 5 weeks 12 week trial: 1 g per day for 3 days followed by once weekly for 5 weeks, followed by once every 2 weeks for 6 weeks. Oral Maintenance: 60–80 mg prednisone daily, duration of taper variable |
-Acts on nuclear glucocorticoids receptors to reduce cytokine and chemokine production -Reduces migration of leukocytes to the target tissue |
Insomnia, psychiatric dysfunction, hyperglycemia, electrolyte imbalances, fluid retention, hypertension, peptic ulcer, Cushing syndrome, cataracts, infections, osteoporosis and avascular necrosis. Addisonian crisis on rapid withdrawal of corticosteroids |
-Blood pressure, serum electrolytes, and glucose monitoring - PJP ppx: TMP/SMX - osteoporosis ppx: vitamin D + calcium - GI ppx: PPI or H2 blocker |
| Plasmapheresis | IV | 1 exchange every other day for 10–14 days | -Extracorporeal blood filtration designed to remove large molecular weight molecules, including immunoglobulins, immune complex, and complements | Hypotension, electrolyte imbalance, perioral paresthesia (hypocalcemia), coagulopathy, central line infection, hemorrhage, thrombosis and pneumothorax | PT, INR, PTT, Fibrinogen |
| IVIG | IV |
Initial dose 2 g/kg daily divided over 2–5 days 6 week trial: 0.4 g/kg IVIG daily for 3 days followed by 0.4 g/kg every week for 6 weeks 12 week trial: 0.4 g/kg IVIG daily for 3 days followed by 0.4 g/kg every week for 6 weeks, then every 2 weeks for 6 weeks |
Remains unclear Interaction with antigen-binding fragment on the antibodies and/or crystalizable fragment on the antibodies or the antigen-presenting cells |
Headache, aseptic meningitis, acute renal failure, thrombotic/thromboembolic events anaphylaxis due to IgA deficiency | Electrolytes, renal function |
| Rituximab | IV | 1000 mg followed by 2nd dose in 2 weeks, or 375 mg/m2 weekly for 4 weeks | B cell depletion by antibody dependent cellular cytotoxicity, complement dependent cytotoxicity and apoptosis | Allergic reaction, opportunistic infection, reactivation of tuberculosis infection or hepatitis B infection, PML | Hepatitis B antibodies, quatiferon test (for latent tuberculosis), pregnancy test, Liver function test |
| Cyclophosphamide | IV or PO |
IV: 500–800 mg/m2 or 1000 mg. PO: 1–2 mg/kg/day (renal adjustment necessary) |
Alkylating agent which interferes with DNA synthesis | Gastrointestinal (nausea, vomiting), hair loss, mucositis, hemorrhagic cystitis, infertility and myelosuppression |
CBC, liver function test, creatinine CBC at 8–14 days post-infusion, increased hydration recommended |
| Mycophenolate | PO | Initially 500 mg twice daily, target 1000–1500 mg twice daily | Inhibition of inosine monophosphate dehydrogenase mediated guanosine nucleotide synthesis | Gastrointestinal (nausea, vomiting, diarrhea), hypertension, peripheral edema, infections, myelosuppression, lymphoma |
CBC, creatinine, urine pregnancy test CBC once per week for 1 month, then once every 2 weeks for 2 months then once every 1–3 months for the duration of therapy |
| Azathioprine | PO | Initially 1.5 mg/kg/day, target 2–3 mg/kg/ day (guided by 5-point MCV increase from baseline) | Converted to cytotoxic 6-thioguanine nucleotides which leads to incorporation as a false base into DNA inducing lymphocyte apoptosis |
Gastrointestinal symptoms (nausea, vomiting, diarrhea), hypersensitivity reactions, hair loss, cytopenia, hepatotoxicity, lymphoma, and infections |
CBC, liver function test, creatinine, TPMT and urine pregnancy. CBC should be checked once per week for 1 month, then once every 2 weeks for 2 months, then once every 1–3 months for the duration of therapy |
| Bortezomib | SC | 1–6 cycles, each cycle consists of 4 injections (1.3 mg/m2) | Proteasome inhibitor, decreasing levels of plasma cells. | Bone marrow suppression, GI side effects, peripheral neuropathy, opportunistic infections. | CBC, liver function and electrolytes. |
| Tocilizumab | IV | 4–8 mg/kg per dose, weekly for 2 weeks. Monthly 8 mg/kg if needed | IL-6 receptor monoclonal antibody | Bone marrow suppression, serious infections including pneumonia and sepsis | CBC, liver function test and electrolytes, lipid panel, quanteferon gold |
IV = intravenous; PO = per oral; PLEX = plasmapheresis; IVIG = intravenous immunoglobulin; PT = prothrombin time; INR = International Normalized Ratio; PTT = partial thromboplastin time; CBC = complete blood count; TPMT = thiopurine S-methyltransferase; TMP = trimethoprim; SMX = sulfamethoxazole; PPI = proton pump inhibitor; ppx = prophylaxis
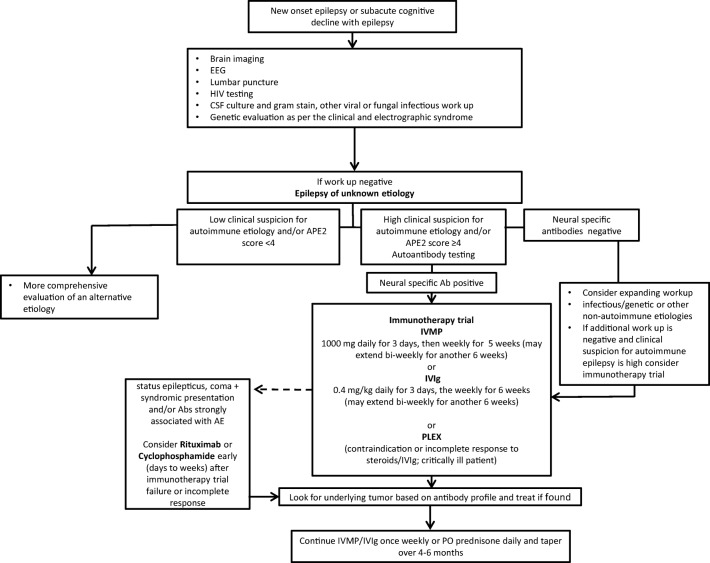
Treatment of autoimmune epilepsy should be based on the severity of the clinical course (Fig. 5). In patients with rapid progression and refractory course, more aggressive immunotherapy is needed including a combination of both first- and second-line therapies. Conversely, some patients with autoimmune epilepsy have a more benign course and their epilepsy can be controlled with antiepileptic drugs and short course of immunotherapy. In all cases, cancer surveillance as discussed above should be pursued. Treatment of the underlying cancer is pivotal for the successful treatment of autoimmune epilepsy.
Fig. 5.
Management algorithm for autoimmune epilepsy. Ab = antibody; APE2 = Antibody Prevalence in Epilepsy and Encephalopathy; CSF = cerebrospinal fluid; IVIG = intravenous immunoglobulin; IVMP = intravenous methyl prednisolone; PLEX = plasmapheresis
Acute Phase Treatment
Preferred first-line treatments for autoimmune epilepsy include high-dose intravenous corticosteroid therapy, PLEX, and IVIG. In some scenarios, such as refractory nonconvulsive status epilepticus, an initial course of IVMP at 1 g per day for 5 days combined with or followed by PLEX (5–7 cycles; 1 exchange every other day spread over 10–14 days) or IVIG (0.4 g/kg per day for 5 consecutive days) may also be utilized. In cases in which both PLEX and IVIG are utilized, PLEX should precede IVIG therapy, to avoid removal of the immune globulins from the circulation.
In outpatient settings, we utilize 6- to 12-week immunotherapy trials. The IVMP trial includes 1 g per day for 3 days followed by once weekly for 5 weeks (6-week IVMP trial), followed by once every 2 weeks for 6 weeks (12-week IVMP trial). If the patient has contraindications for IVMP or cannot tolerate high-dose corticosteroids due to side effects, a 6- to 12-week course of IVIG may be considered. This includes 0.4 g/kg IVIG daily for 3 days followed by 0.4 g/kg every week for 6 weeks (6-week IVIG trial), then every 2 weeks for 6 weeks (12-week IVIG trial).
A treatment response can be ascertained using a seizure diary to assess seizure frequency and/or change in semiology and neurological examination including screening mental status examination after completion of immunotherapy trial. The quality of life in epilepsy (QOLIE-31) can be utilized as well. EEG, brain MRI with gadolinium, brain PET, and formal cognitive tests are additional parameters that can be monitored. Seizures in autoimmune epilepsy may show early improvement within 4 to 6 weeks of initiating immunotherapy. Conversely, cognitive impairment and amnesia, if present, recover more slowly.
Maintenance Phase
The main goals of the maintenance phase treatment are to prevent disease progression and relapses, while avoiding medication adverse effects. In most instances, chronic immunotherapy decisions are based on response to the acute immunotherapy regimen and the specific autoantibodies identified. In cases which continue to have a refractory course despite aggressive initial immunotherapy and optimal anti-epileptic regimen, second-line immunosuppressive agents are initiated early in the disease course. Rituximab, cyclophosphamide, mycophenolate, and azathioprine are commonly utilized agents. In some instances, chronic IVIG or plasmapheresis, once every 2 to 3 weeks, is also utilized as a maintenance therapy. If mycophenolate or azathioprine is initiated, an overlapping 2- to 3-month course of corticosteroids should be considered, due to their delayed therapeutic effect.
Understanding the potential immune mechanism of the disease can also help in deciding second-line immunotherapeutic strategy. In general, classic paraneoplastic antibodies with intracellular antigens, such as anti-Hu IgG, are primarily considered to have T-cell-mediated syndromes leading to preference of broad-spectrum immunosuppressive agents such as cyclophosphamide and mycophenolate. However, some of the antibodies against neural cell surface antigens are directly pathogenic, such as NMDA-R IgG; therefore, B-cell-targeted therapies reducing antibody production are preferred. Careful evaluation of adverse effects of these agents, with frequent labs (specific to immunotherapy agent utilized), is extremely important.
Bortezomib and tocilizumab have emerged as novel second-line immunotherapeutics for management of refractory cases of autoimmune epilepsy and encephalitis. Bortezomib is a proteasome inhibitor used in the treatment of multiple myeloma and off-label use in SLE. Bortezomib decreases both the short-lived and long-lived plasma cells which ultimately leads to decreased production of circulating antibodies [97]. Bortezomib has been utilized for management of severe refractory NMDA-R encephalitis with limited success [97]. Tocilizumab is a humanized anti-interleukin (IL)-6 receptor monoclonal antibody, which blocks IL-6-mediated signal transduction [98]. Tocilizumab has been used in several autoimmune conditions including SLE, rheumatoid arthritis, and giant cell arteritis [98, 99]. A recent retrospective observational study reported favorable outcome with the administration of tocilizumab in 7 adult patients with NORSE who remained refractory to first-line immunotherapy and/or rituximab [100]. In another study of 20 patients without autoimmune encephalitis, use of tocilizumab was associated with favorable clinical response at the last follow-up [101].
Studies assessing duration of maintenance immunotherapy are limited. Although, a trial of immunotherapy withdrawal may be considered after 2 years of treatment if patient has not had any relapses.
Antiepileptic Drugs
Even though seizures in autoimmune epilepsy are characteristically resistant to antiepileptic drugs (AEDs) alone, they continue to play an important role in symptomatic management. In all autoimmune epilepsy patients, AEDs should be used along with immunotherapy treatment. There are no randomized clinical trial data to support one AED over another. Levetiracetam is commonly employed for management of seizures given the favorable side effect profile and minimal drug to drug interaction. However psychiatric dysfunction due to adverse effects of levetiracetam may be difficult to differentiate from syndromic manifestation of limbic encephalitis [102].
A recent retrospective study evaluating AEDs in autoimmune epilepsy demonstrated seizure freedom rates were considerably higher with use of sodium channel–blocking AEDs (carbamazepine, phenytoin, oxcarbazepine, and lacosamide) compared with levetiracetam [103]. The reason for better efficacy of sodium channel–blocking AEDs remains unclear. Interestingly, both carbamazepine and oxcarbazepine have been shown to reduce levels of IL-1 and IL-2 in healthy subjects [104]. Medications such as carbamazepine and phenytoin have enzyme induction properties which can alter the pharmacokinetics of immunosuppressive therapies. Therefore, newer sodium channel–blocking AEDs with more favorable pharmacokinetic profiles (such as oxcarbazepine and lacosamide) could be preferred in management of autoimmune epilepsy.
Epilepsy Surgery
Epilepsy surgery has been tried in select cases of autoimmune epilepsy [105, 106]. However, among these patients, outcomes seem to be worse when compared with other etiologies of drug-resistant epilepsy.
Outcome and Prognosis
Most patients with autoimmune epilepsy and encephalitis are responsive to either first- or second-line therapies. However, a subset of patients remains refractory to multiple immunotherapies. Certain laboratory and imaging features can predict a more severe course. In patients with LGI1 encephalitis, higher CSF LGI1 IgG4 subclass–specific titer and index correlated with worse outcome [107]. In NMDA-R encephalitis, the presence of extreme delta brush was associated with a prolonged course [72].
Among NMDA-R encephalitis patients, a 5-point grading system, antiNMDA-R Encephalitis One-Year Functional Status (NEOS) score, predicts neurologic function at 1 year. The factors included in the NEOS score were intensive care unit admission, treatment delay more than 4 weeks, lack of clinical improvement within 4 weeks, abnormal MRI and CSF white blood cell count more than 20 cells/mcL. A high NEOS score was associated with probability of poor functional status at 1 year [108].
Follow-up
Patients with autoimmune epilepsy should be followed up regularly, preferably by an epileptologist in conjunction with a neuroimmunologist. On long-term follow-up, some patients continue to have chronic drug-resistant epilepsy despite aggressive immunotherapy and anti-epileptic drugs. Discerning whether epilepsy is secondary to irreversible cortical damage or due to a persistent inflammatory process can be difficult. In such instances, ancillary tests including brain MRI with gadolinium contrast, repeat CSF analysis, and brain PET can be helpful in guiding treatment decisions. Serum and/or CSF neural specific antibody titers usually have a poor predictive relationship with treatment response or clinical relapse. However, one retrospective study has shown utility of CSF NMDA-R IgG titers detected with brain immunohistochemistry in predicting disease relapse [75].
With better insight into the mechanisms of antibody-mediated and autoantigen-specific T-cell-mediated autoimmune epilepsy syndromes, utilization of AEDs and immunotherapy is likely to be further optimized. In the future, we anticipate well-designed randomized controlled trials will help in evidence-based selection of the most efficacious treatments (agents, drug doses, and treatment duration) for autoimmune epilepsy management.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ong MS, et al. Population-level evidence for an autoimmune etiology of epilepsy. JAMA Neurol. 2014;71(5):569–74. doi: 10.1001/jamaneurol.2014.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brodie MJ, et al. The 2017 ILAE classification of seizure types and the epilepsies: what do people with epilepsy and their caregivers need to know? Epileptic Disord. 2018;20(2):77–87. doi: 10.1684/epd.2018.0957. [DOI] [PubMed] [Google Scholar]
- 3.Dubey D, Pittock SJ, McKeon A. Antibody Prevalence in Epilepsy and Encephalopathy score: Increased specificity and applicability. Epilepsia. 2019;60(2):367–369. doi: 10.1111/epi.14649. [DOI] [PubMed] [Google Scholar]
- 4.Dubey D, et al. Neurological Autoantibody Prevalence in Epilepsy of Unknown Etiology. JAMA Neurol. 2017;74(4):397–402. doi: 10.1001/jamaneurol.2016.5429. [DOI] [PubMed] [Google Scholar]
- 5.Scheffer IE, et al. ILAE classification of the epilepsies: Position paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58(4):512–521. doi: 10.1111/epi.13709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Granata T, Andermann F. Rasmussen encephalitis. Handb Clin Neurol. 2013;111:511–9. doi: 10.1016/B978-0-444-52891-9.00054-3. [DOI] [PubMed] [Google Scholar]
- 7.Britton J. Autoimmune epilepsy. Handb Clin Neurol. 2016;133:219–45. doi: 10.1016/B978-0-444-63432-0.00013-X. [DOI] [PubMed] [Google Scholar]
- 8.Dalmau J, Graus F. Antibody-Mediated Encephalitis. N Engl J Med. 2018;378(9):840–851. doi: 10.1056/NEJMra1708712. [DOI] [PubMed] [Google Scholar]
- 9.Larman HB, et al. Autoantigen discovery with a synthetic human peptidome. Nat Biotechnol. 2011;29(6):535–41. doi: 10.1038/nbt.1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Scharf M, et al. A Spectrum of Neural Autoantigens, Newly Identified by Histo-Immunoprecipitation, Mass Spectrometry, and Recombinant Cell-Based Indirect Immunofluorescence. Front Immunol. 2018;9:1447. doi: 10.3389/fimmu.2018.01447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schubert RD, Wilson MR. A tale of two approaches: how metagenomics and proteomics are shaping the future of encephalitis diagnostics. Curr Opin Neurol. 2015;28(3):283–7. doi: 10.1097/WCO.0000000000000198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun H, Chen GY, Yao SQ. Recent advances in microarray technologies for proteomics. Chem Biol. 2013;20(5):685–99. doi: 10.1016/j.chembiol.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 13.Toledano M, et al. Utility of an immunotherapy trial in evaluating patients with presumed autoimmune epilepsy. Neurology. 2014;82(18):1578–86. doi: 10.1212/WNL.0000000000000383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dubey D, et al. Autoimmune encephalitis epidemiology and a comparison to infectious encephalitis. Ann Neurol. 2018;83(1):166–177. doi: 10.1002/ana.25131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dubey D, Toledano M, McKeon A. Clinical presentation of autoimmune and viral encephalitides. Curr Opin Crit Care. 2018;24(2):80–90. doi: 10.1097/MCC.0000000000000483. [DOI] [PubMed] [Google Scholar]
- 16.Graus F, et al. Recommended diagnostic criteria for paraneoplastic neurological syndromes. J Neurol Neurosurg Psychiatry. 2004;75(8):1135–40. doi: 10.1136/jnnp.2003.034447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dubey D, et al. Predictive models in the diagnosis and treatment of autoimmune epilepsy. Epilepsia. 2017;58(7):1181–1189. doi: 10.1111/epi.13797. [DOI] [PubMed] [Google Scholar]
- 18.Brenner T, et al. Prevalence of neurologic autoantibodies in cohorts of patients with new and established epilepsy. Epilepsia. 2013;54(6):1028–35. doi: 10.1111/epi.12127. [DOI] [PubMed] [Google Scholar]
- 19.Abramovici S, Bagic A. Epidemiology of epilepsy. Handb Clin Neurol. 2016;138:159–71. doi: 10.1016/B978-0-12-802973-2.00010-0. [DOI] [PubMed] [Google Scholar]
- 20.Wright S, et al. Neuronal antibodies in pediatric epilepsy: Clinical features and long-term outcomes of a historical cohort not treated with immunotherapy. Epilepsia. 2016;57(5):823–31. doi: 10.1111/epi.13356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suleiman J, et al. Autoantibodies to neuronal antigens in children with new-onset seizures classified according to the revised ILAE organization of seizures and epilepsies. Epilepsia. 2013;54(12):2091–100. doi: 10.1111/epi.12405. [DOI] [PubMed] [Google Scholar]
- 22.Bauer J, et al. Innate and adaptive immunity in human epilepsies. Epilepsia. 2017;58(Suppl 3):57–68. doi: 10.1111/epi.13784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fujinami RS, et al. Molecular mimicry, bystander activation, or viral persistence: infections and autoimmune disease. Clin Microbiol Rev. 2006;19(1):80–94. doi: 10.1128/CMR.19.1.80-94.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Armangue T, et al. Frequency, symptoms, risk factors, and outcomes of autoimmune encephalitis after herpes simplex encephalitis: a prospective observational study and retrospective analysis. Lancet Neurol. 2018;17(9):760–772. doi: 10.1016/S1474-4422(18)30244-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ohkawa T, et al. Autoantibodies to epilepsy-related LGI1 in limbic encephalitis neutralize LGI1-ADAM22 interaction and reduce synaptic AMPA receptors. J Neurosci. 2013;33(46):18161–74. doi: 10.1523/JNEUROSCI.3506-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Aysit-Altuncu N, et al. Effect of LGI1 antibody-positive IgG on hippocampal neuron survival: a preliminary study. Neuroreport. 2018;29(11):932–938. doi: 10.1097/WNR.0000000000001055. [DOI] [PubMed] [Google Scholar]
- 27.Hughes EG, et al. Cellular and synaptic mechanisms of anti-NMDA receptor encephalitis. J Neurosci. 2010;30(17):5866–75. doi: 10.1523/JNEUROSCI.0167-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gresa-Arribas N, et al. Antibody titres at diagnosis and during follow-up of anti-NMDA receptor encephalitis: a retrospective study. Lancet Neurol. 2014;13(2):167–77. doi: 10.1016/S1474-4422(13)70282-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Albert ML, et al. Tumor-specific killer cells in paraneoplastic cerebellar degeneration. Nat Med. 1998;4(11):1321–4. doi: 10.1038/3315. [DOI] [PubMed] [Google Scholar]
- 30.Flanagan, E. P., et al., (2017), Glial fibrillary acidic protein immunoglobulin G as biomarker of autoimmune astrocytopathy: Analysis of 102 patients. Ann Neurol., 81:298–309. [DOI] [PubMed]
- 31.Liimatainen S, et al. Clinical significance of glutamic acid decarboxylase antibodies in patients with epilepsy. Epilepsia. 2010;51(5):760–7. doi: 10.1111/j.1528-1167.2009.02325.x. [DOI] [PubMed] [Google Scholar]
- 32.Daif A, et al. Antiglutamic acid decarboxylase 65 (GAD65) antibody-associated epilepsy. Epilepsy Behav. 2018;80:331–336. doi: 10.1016/j.yebeh.2018.01.021. [DOI] [PubMed] [Google Scholar]
- 33.Dubey D, et al. Predictors of neural-specific autoantibodies and immunotherapy response in patients with cognitive dysfunction. J Neuroimmunol. 2018;323:62–72. doi: 10.1016/j.jneuroim.2018.07.009. [DOI] [PubMed] [Google Scholar]
- 34.Titulaer MJ, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 2013;12(2):157–65. doi: 10.1016/S1474-4422(12)70310-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dalmau J, Geis C, Graus F. Autoantibodies to Synaptic Receptors and Neuronal Cell Surface Proteins in Autoimmune Diseases of the Central Nervous System. Physiol Rev. 2017;97(2):839–887. doi: 10.1152/physrev.00010.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quek AML, O’Toole O. Autoimmune Epilepsy: The Evolving Science of Neural Autoimmunity and Its Impact on Epilepsy Management. Semin Neurol. 2018;38(3):290–302. doi: 10.1055/s-0038-1660860. [DOI] [PubMed] [Google Scholar]
- 37.Dalmau J, et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann Neurol. 2007;61(1):25–36. doi: 10.1002/ana.21050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Titulaer MJ, et al. Late-onset anti-NMDA receptor encephalitis. Neurology. 2013;81(12):1058–63. doi: 10.1212/WNL.0b013e3182a4a49c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mueller SH, et al. Genetic predisposition in anti-LGI1 and anti-NMDA receptor encephalitis. Ann Neurol. 2018;83(4):863–869. doi: 10.1002/ana.25216. [DOI] [PubMed] [Google Scholar]
- 40.Sebastian Lopez-Chiriboga A, et al. LGI1 and CASPR2 Neurological Autoimmunity in Children. Ann Neurol. 2018;84(3):473–480. doi: 10.1002/ana.25310. [DOI] [PubMed] [Google Scholar]
- 41.Irani SR, et al. Faciobrachial dystonic seizures precede Lgi1 antibody limbic encephalitis. Ann Neurol. 2011;69(5):892–900. doi: 10.1002/ana.22307. [DOI] [PubMed] [Google Scholar]
- 42.Gadoth A, et al. Expanded phenotypes and outcomes among 256 LGI1/CASPR2-IgG-positive patients. Ann Neurol. 2017;82(1):79–92. doi: 10.1002/ana.24979. [DOI] [PubMed] [Google Scholar]
- 43.Lilleker JB, et al. The relevance of VGKC positivity in the absence of LGI1 and Caspr2 antibodies. Neurology. 2016;87(17):1848–1849. doi: 10.1212/WNL.0000000000003300. [DOI] [PubMed] [Google Scholar]
- 44.van Sonderen A, et al. The relevance of VGKC positivity in the absence of LGI1 and Caspr2 antibodies. Neurology. 2016;86(18):1692–9. doi: 10.1212/WNL.0000000000002637. [DOI] [PubMed] [Google Scholar]
- 45.Lai M, et al. AMPA receptor antibodies in limbic encephalitis alter synaptic receptor location. Ann Neurol. 2009;65(4):424–34. doi: 10.1002/ana.21589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Haselmann H, et al. Human Autoantibodies against the AMPA Receptor Subunit GluA2 Induce Receptor Reorganization and Memory Dysfunction. Neuron. 2018;100(1):91–105.e9. doi: 10.1016/j.neuron.2018.07.048. [DOI] [PubMed] [Google Scholar]
- 47.Hoftberger R, et al. Encephalitis and AMPA receptor antibodies: Novel findings in a case series of 22 patients. Neurology. 2015;84(24):2403–12. doi: 10.1212/WNL.0000000000001682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Joubert B, et al. Clinical Spectrum of Encephalitis Associated With Antibodies Against the alpha-Amino-3-Hydroxy-5-Methyl-4-Isoxazolepropionic Acid Receptor: Case Series and Review of the Literature. JAMA Neurol. 2015;72(10):1163–9. doi: 10.1001/jamaneurol.2015.1715. [DOI] [PubMed] [Google Scholar]
- 49.Boronat A, et al. Encephalitis and antibodies to dipeptidyl-peptidase-like protein-6, a subunit of Kv4.2 potassium channels. Ann Neurol. 2013;73(1):120–8. doi: 10.1002/ana.23756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Carr I. The Ophelia syndrome: memory loss in Hodgkin’s disease. Lancet. 1982;1(8276):844–5. doi: 10.1016/s0140-6736(82)91887-6. [DOI] [PubMed] [Google Scholar]
- 51.Lancaster E, et al. Antibodies to metabotropic glutamate receptor 5 in the Ophelia syndrome. Neurology. 2011;77(18):1698–701. doi: 10.1212/WNL.0b013e3182364a44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Spatola M, et al. Encephalitis with mGluR5 antibodies: Symptoms and antibody effects. Neurology. 2018;90(22):e1964–e1972. doi: 10.1212/WNL.0000000000005614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pittock SJ, et al. Glutamic acid decarboxylase autoimmunity with brainstem, extrapyramidal, and spinal cord dysfunction. Mayo Clin Proc. 2006;81(9):1207–14. doi: 10.4065/81.9.1207. [DOI] [PubMed] [Google Scholar]
- 54.Peltola J, et al. Autoantibodies to glutamic acid decarboxylase in patients with therapy-resistant epilepsy. Neurology. 2000;55(1):46–50. doi: 10.1212/wnl.55.1.46. [DOI] [PubMed] [Google Scholar]
- 55.Lilleker JB, Biswas V, Mohanraj R. Glutamic acid decarboxylase (GAD) antibodies in epilepsy: diagnostic yield and therapeutic implications. Seizure. 2014;23(8):598–602. doi: 10.1016/j.seizure.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 56.Roberts WK, et al. Patients with lung cancer and paraneoplastic Hu syndrome harbor HuD-specific type 2 CD8+ T cells. J Clin Invest. 2009;119(7):2042–51. doi: 10.1172/JCI36131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rudzinski LA, et al. Extratemporal EEG and MRI findings in ANNA-1 (anti-Hu) encephalitis. Epilepsy Res. 2011;95(3):255–62. doi: 10.1016/j.eplepsyres.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 58.Pittock SJ, Lucchinetti CF, Lennon VA. Anti-neuronal nuclear autoantibody type 2: paraneoplastic accompaniments. Ann Neurol. 2003;53(5):580–7. doi: 10.1002/ana.10518. [DOI] [PubMed] [Google Scholar]
- 59.Dalmau J, et al. Clinical analysis of anti-Ma2-associated encephalitis. Brain. 2004;127(Pt 8):1831–44. doi: 10.1093/brain/awh203. [DOI] [PubMed] [Google Scholar]
- 60.Voltz R, et al. A serologic marker of paraneoplastic limbic and brain-stem encephalitis in patients with testicular cancer. N Engl J Med. 1999;340(23):1788–95. doi: 10.1056/NEJM199906103402303. [DOI] [PubMed] [Google Scholar]
- 61.Yu Z, et al. CRMP-5 neuronal autoantibody: marker of lung cancer and thymoma-related autoimmunity. Ann Neurol. 2001;49(2):146–54. [PubMed] [Google Scholar]
- 62.Dubey D, et al. Autoimmune CRMP5 neuropathy phenotype and outcome defined from 105 cases. Neurology. 2018;90(2):e103–e110. doi: 10.1212/WNL.0000000000004803. [DOI] [PubMed] [Google Scholar]
- 63.Vernino S, et al. Paraneoplastic chorea associated with CRMP-5 neuronal antibody and lung carcinoma. Ann Neurol. 2002;51(5):625–30. doi: 10.1002/ana.10178. [DOI] [PubMed] [Google Scholar]
- 64.Quek AM, et al. Autoimmune epilepsy: clinical characteristics and response to immunotherapy. Arch Neurol. 2012;69(5):582–93. doi: 10.1001/archneurol.2011.2985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bien CG, et al. Pathogenesis, diagnosis and treatment of Rasmussen encephalitis: a European consensus statement. Brain. 2005;128(Pt 3):454–71. doi: 10.1093/brain/awh415. [DOI] [PubMed] [Google Scholar]
- 66.Longaretti F, et al. Evolution of the EEG in children with Rasmussen’s syndrome. Epilepsia. 2012;53(9):1539–45. doi: 10.1111/j.1528-1167.2012.03565.x. [DOI] [PubMed] [Google Scholar]
- 67.Bien CG, et al. Rasmussen encephalitis: incidence and course under randomized therapy with tacrolimus or intravenous immunoglobulins. Epilepsia. 2013;54(3):543–50. doi: 10.1111/epi.12042. [DOI] [PubMed] [Google Scholar]
- 68.Vining EP, et al. Why would you remove half a brain? The outcome of 58 children after hemispherectomy-the Johns Hopkins experience: 1968 to 1996. Pediatrics. 1997;100(2 Pt 1):163–71. doi: 10.1542/peds.100.2.163. [DOI] [PubMed] [Google Scholar]
- 69.Gaspard N, et al. New-onset refractory status epilepticus: Etiology, clinical features, and outcome. Neurology. 2015;85(18):1604–13. doi: 10.1212/WNL.0000000000001940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gaspard N, et al. New-onset refractory status epilepticus (NORSE) and febrile infection-related epilepsy syndrome (FIRES): State of the art and perspectives. Epilepsia. 2018;59(4):745–752. doi: 10.1111/epi.14022. [DOI] [PubMed] [Google Scholar]
- 71.Kaplan PW, Sutter R. Electroencephalography of autoimmune limbic encephalopathy. J Clin Neurophysiol. 2013;30(5):490–504. doi: 10.1097/WNP.0b013e3182a73d47. [DOI] [PubMed] [Google Scholar]
- 72.Schmitt SE, et al. Extreme delta brush: a unique EEG pattern in adults with anti-NMDA receptor encephalitis. Neurology. 2012;79(11):1094–100. doi: 10.1212/WNL.0b013e3182698cd8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Baykan B, et al. Delta Brush Pattern Is Not Unique to NMDAR Encephalitis: Evaluation of Two Independent Long-Term EEG Cohorts. Clin EEG Neurosci. 2018;49(4):278–284. doi: 10.1177/1550059417693168. [DOI] [PubMed] [Google Scholar]
- 74.Aurangzeb S, et al. LGI1-antibody encephalitis is characterised by frequent, multifocal clinical and subclinical seizures. Seizure. 2017;50:14–17. doi: 10.1016/j.seizure.2017.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Graus F, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol. 2016;15(4):391–404. doi: 10.1016/S1474-4422(15)00401-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Escudero D, et al. Antibody-associated CNS syndromes without signs of inflammation in the elderly. Neurology. 2017;89(14):1471–1475. doi: 10.1212/WNL.0000000000004541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Dubey D, et al. The spectrum of autoimmune encephalopathies. J Neuroimmunol. 2015;287:93–7. doi: 10.1016/j.jneuroim.2015.08.014. [DOI] [PubMed] [Google Scholar]
- 78.Malter MP, et al. Suspected new-onset autoimmune temporal lobe epilepsy with amygdala enlargement. Epilepsia. 2016;57(9):1485–94. doi: 10.1111/epi.13471. [DOI] [PubMed] [Google Scholar]
- 79.Finke C, et al. Functional and structural brain changes in anti-N-methyl-D-aspartate receptor encephalitis. Ann Neurol. 2013;74(2):284–96. doi: 10.1002/ana.23932. [DOI] [PubMed] [Google Scholar]
- 80.Solnes LB, et al. Diagnostic Value of (18)F-FDG PET/CT Versus MRI in the Setting of Antibody-Specific Autoimmune Encephalitis. J Nucl Med. 2017;58(8):1307–1313. doi: 10.2967/jnumed.116.184333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Probasco JC, et al. Decreased occipital lobe metabolism by FDG-PET/CT: An anti-NMDA receptor encephalitis biomarker. Neurol Neuroimmunol Neuroinflamm. 2018;5(1):e413. doi: 10.1212/NXI.0000000000000413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ohta K, et al. Perfusion IMP-SPECT shows reversible abnormalities in GABA(B) receptor antibody associated encephalitis with normal MRI. Brain Behav. 2011;1(2):70–2. doi: 10.1002/brb3.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Guerin J, et al. Autoimmune epilepsy: findings on MRI and FDG-PET. Br J Radiol. 2019;92(1093):20170869. doi: 10.1259/bjr.20170869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Heine J, et al. Imaging of autoimmune encephalitis--Relevance for clinical practice and hippocampal function. Neuroscience. 2015;309:68–83. doi: 10.1016/j.neuroscience.2015.05.037. [DOI] [PubMed] [Google Scholar]
- 85.Irani SR, Vincent A. Voltage-gated potassium channel-complex autoimmunity and associated clinical syndromes. Handb Clin Neurol. 2016;133:185–97. doi: 10.1016/B978-0-444-63432-0.00011-6. [DOI] [PubMed] [Google Scholar]
- 86.Flanagan EP, et al. Basal ganglia T1 hyperintensity in LGI1-autoantibody faciobrachial dystonic seizures. Neurol Neuroimmunol Neuroinflamm. 2015;2(6):e161. doi: 10.1212/NXI.0000000000000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Shin YW, et al. VGKC-complex/LGI1-antibody encephalitis: clinical manifestations and response to immunotherapy. J Neuroimmunol. 2013;265(1–2):75–81. doi: 10.1016/j.jneuroim.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 88.Fredriksen JR, et al. MRI findings in glutamic acid decarboxylase associated autoimmune epilepsy. Neuroradiology. 2018;60(3):239–245. doi: 10.1007/s00234-018-1976-6. [DOI] [PubMed] [Google Scholar]
- 89.Spatola M, et al. Investigations in GABAA receptor antibody-associated encephalitis. Neurology. 2017;88(11):1012–1020. doi: 10.1212/WNL.0000000000003713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Dogan Onugoren M, et al. Limbic encephalitis due to GABAB and AMPA receptor antibodies: a case series. J Neurol Neurosurg Psychiatry. 2015;86(9):965–72. doi: 10.1136/jnnp-2014-308814. [DOI] [PubMed] [Google Scholar]
- 91.Hoftberger R, et al. Encephalitis and GABAB receptor antibodies: novel findings in a new case series of 20 patients. Neurology. 2013;81(17):1500–6. doi: 10.1212/WNL.0b013e3182a9585f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Do LD, et al. Characteristics in limbic encephalitis with anti-adenylate kinase 5 autoantibodies. Neurology. 2017;88(6):514–524. doi: 10.1212/WNL.0000000000003586. [DOI] [PubMed] [Google Scholar]
- 93.Pittock SJ, Palace J. Paraneoplastic and idiopathic autoimmune neurologic disorders: approach to diagnosis and treatment. Handb Clin Neurol. 2016;133:165–83. doi: 10.1016/B978-0-444-63432-0.00010-4. [DOI] [PubMed] [Google Scholar]
- 94.Irani SR, et al. Faciobrachial dystonic seizures: the influence of immunotherapy on seizure control and prevention of cognitive impairment in a broadening phenotype. Brain. 2013;136(Pt 10):3151–62. doi: 10.1093/brain/awt212. [DOI] [PubMed] [Google Scholar]
- 95.Byun JI, et al. Effect of Immunotherapy on Seizure Outcome in Patients with Autoimmune Encephalitis: A Prospective Observational Registry Study. PLoS One. 2016;11(1):e0146455. doi: 10.1371/journal.pone.0146455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Thompson J, et al. The importance of early immunotherapy in patients with faciobrachial dystonic seizures. Brain. 2018;141(2):348–356. doi: 10.1093/brain/awx323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Scheibe F, et al. Bortezomib for treatment of therapy-refractory anti-NMDA receptor encephalitis. Neurology. 2017;88(4):366–370. doi: 10.1212/WNL.0000000000003536. [DOI] [PubMed] [Google Scholar]
- 98.Kishimoto T. IL-6: from its discovery to clinical applications. Int Immunol. 2010;22(5):347–52. doi: 10.1093/intimm/dxq030. [DOI] [PubMed] [Google Scholar]
- 99.Abbott BP, et al. GW170104: Observation of a 50-Solar-Mass Binary Black Hole Coalescence at Redshift 0.2. Phys Rev Lett. 2017;118(22):221101. doi: 10.1103/PhysRevLett.118.221101. [DOI] [PubMed] [Google Scholar]
- 100.Jun JS, et al. Tocilizumab treatment for new onset refractory status epilepticus. Ann Neurol. 2018;84(6):940–945. doi: 10.1002/ana.25374. [DOI] [PubMed] [Google Scholar]
- 101.Lee WJ, et al. Tocilizumab in Autoimmune Encephalitis Refractory to Rituximab: An Institutional Cohort Study. Neurotherapeutics. 2016;13(4):824–832. doi: 10.1007/s13311-016-0442-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Abou-Khalil BW. Antiepileptic Drugs. Continuum (Minneap Minn) 2016;22(1 Epilepsy):132–56. doi: 10.1212/CON.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 103.Feyissa AM, Lopez Chiriboga AS, Britton JW. Antiepileptic drug therapy in patients with autoimmune epilepsy. Neurol Neuroimmunol Neuroinflamm. 2017;4(4):e353. doi: 10.1212/NXI.0000000000000353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Beghi E, Shorvon S. Antiepileptic drugs and the immune system. Epilepsia. 2011;52(Suppl 3):40–4. doi: 10.1111/j.1528-1167.2011.03035.x. [DOI] [PubMed] [Google Scholar]
- 105.Carreno M, et al. Epilepsy surgery in drug resistant temporal lobe epilepsy associated with neuronal antibodies. Epilepsy Res. 2017;129:101–105. doi: 10.1016/j.eplepsyres.2016.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Malter MP, et al. Treatment of immune-mediated temporal lobe epilepsy with GAD antibodies. Seizure. 2015;30:57–63. doi: 10.1016/j.seizure.2015.05.017. [DOI] [PubMed] [Google Scholar]
- 107.Gadoth A, et al. Elevated LGI1-IgG CSF index predicts worse neurological outcome. Ann Clin Transl Neurol. 2018;5(5):646–650. doi: 10.1002/acn3.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Balu R, et al. A score that predicts 1-year functional status in patients with anti-NMDA receptor encephalitis. Neurology. 2019;92(3):e244–e252. doi: 10.1212/WNL.0000000000006783. [DOI] [PMC free article] [PubMed] [Google Scholar]