Abstract
The objective of our study was to determine whether treatment with baclofen is neurologically safe with respect to exposure during recovery from spinal cord injury. We performed a secondary longitudinal analysis of a cohort of adult patients with traumatic acute spinal cord injury. Cumulative baclofen dose was computed over the first 4 weeks following injury from concomitant medication information from a completed clinical trial. The main outcome measure was neurologic status, which was assessed over 52 weeks with “marked recovery” defined as the conversion to higher sensory and motor function. To complete the drug safety profile, drug toxicity was assessed with assays from standard blood work. Multivariable Cox regression was used to compute hazard ratios (HRs) and 95% confidence intervals (CIs). Of the cohort (n = 651), 18% (n = 115) received baclofen within 4 weeks post injury. Baclofen use was associated with higher rates of marked neurologic recovery, even after adjustment for injury severity (HR = 2.1, 95% CI 1.5–3.0 for high dose vs none). Baclofen exposure was not associated with liver or renal side effects. The use of other medications indicated for spasticity was not associated with neurological outcomes. Overall, this longitudinal analysis provides level 3 evidence on the neurologic safety of baclofen and potential beneficial effects on recovery in the early days after acute traumatic spinal cord injury. The usefulness of concomitant medication files from completed clinical trials is highlighted. We also highlight the importance of incorporating logical patient questions and neurological outcomes into research addressing drug safety.
Keywords: spinal cord injury, baclofen, anti-spasticity, drug safety, patient-oriented research
Introduction
Traumatic spinal cord injury is caused by sudden mechanical trauma to the spinal cord, resulting in mild to severe paralysis and reduced sensation [1]. The lifelong deficits accompanying injury can have a devastating impact on the individual, caregivers, and society, reducing quality of life and massively burdening health care systems [2, 3]. At present, there are no acute pharmacological interventions to enhance the extent of neurologic recovery beyond that which occurs spontaneously.
In addition to paralysis and sensory loss, acute spinal cord injury is accompanied by various other neurological complications. Among the most frequent and debilitating are involuntary extensor or flexor muscle spasms [4, 5]. These often develop in the initial days to weeks after spinal shock due to injury and are commonly managed pharmacologically by enhancing central nervous system inhibition with baclofen, a GABA-B agonist [4, 5].
Despite decades of clinical application and widespread use for spasticity, the safety of administering baclofen in the acute phases of injury has never been examined. This is surprising considering that baclofen is centrally acting and its administration overlaps with recovery of neurological function [6, 7]. Moreover, there are anecdotal reports of deleterious effects of baclofen in both humans and animal models [8, 9]. Concerns regarding the neurologic safety of baclofen have even led to precautions against the use of anti-spasticity medications in the “recovery phase” of stroke and multiple sclerosis [10]. One guideline reports that “it is best to consider that the GABAergic agents may have a harmful effect on the body during the recovery phase” [10]. These precautions are, at present, not based on clinical evidence.
Moreover, patients and their caregivers have urgent questions with regard to factors that potentially interfere with their recovery. These questions extend to the use of medications [11]. At present, care providers cannot provide an informed, evidence-based response regarding the use of baclofen in the acute phase of spinal cord injury. These legitimate patient concerns warrant that the safety of baclofen with respect to neurologic recovery be established. The primary objective of our study was therefore to determine whether acutely administered baclofen is safe in the context of neurologic recovery following spinal cord injury.
Methods
Study Design, Data Source, and Cohort Definition
A secondary analysis was performed of the completed United States Food and Drug Administration (FDA)-sponsored Sygen spinal cord injury clinical trial. The Sygen trial was a randomized, prospective, phase III, placebo-controlled, multi-center study testing the efficacy of GM-1 ganglioside therapy in acute, traumatic spinal cord injury [13, 14]. Full design, recruitment, and enrollment details have been published previously [14]. For inclusion in Sygen, patients were required to have at least one lower extremity with a substantial motor deficit. Patients with spinal cord transection or penetration were excluded, as were patients with a cauda equina, brachial or lumbosacral plexus, or peripheral nerve injury. Multiple trauma cases were included as long as they were not so severe as to preclude neurologic evaluation. It is notable that this requirement of participating in a detailed neurologic exam excluded major head trauma cases and also intubated chest trauma cases. For the purpose of this study, we applied further inclusion/exclusion criteria. Namely, to be included in our analysis, subjects in Sygen needed complete sensory and motor scores from the International Standards for the Neurological Classification of Spinal Cord Injury (ISNCSCI) at baseline (within 72 h after injury) and one follow-up ISNCSCI and/or Benzel grade between 4 and 52 weeks post injury. These measures are described in more detail below.
The Sygen trial, which followed patients over the first year following injury, was clinically active from 1992 to 1998 and showed no differences between treatment and placebo. The negative finding of the Sygen study is considered Class I Medical Evidence by the spinal cord injury Committee of the American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS) [15, 16]. Subsequent analyses of the Sygen data have been performed to characterize the trajectory and extent of spontaneous recovery from acute spinal cord injury [17–19].
Exposures (Independent Variables)
The original Sygen trial rigorously tracked the use of medications delivered alongside the study medication (i.e., GM-1). For each concomitant drug administered during the trial, the dosage, reason for administration, and the timing of administration were recorded. The cumulative dose, the sum of all medication exposures over the first month (4 weeks or approx. 30 days), was treated as a continuous variable and also categorized as “not exposed,” “low dose” (> 0 and < 50th percentile), and “high dose” (≥ 50th percentile) according to the distribution of total doses. Note that, although patients were randomized to GM-1 ganglioside therapy, individuals were not randomized to concomitant medication administration.
Outcome Variables (Dependent Variables)
The primary outcome was “marked recovery.” This binary outcome was based on both Benzel grades and American Spinal Injury Association Impairment Scale (AIS) grades according to the 2011 ISNCSCI [20]. AIS grades reflect injury completeness (AIS A/B are motor complete and AIS C/D are motor incomplete). Benzel grades are used to assess ambulation (scale of 1 to 7: for example, grade 5 = limited walking [motor function allows walking with assistance or unassisted, but significant problems secondary to lack of endurance or fear of falling limit patient mobility, must be able to ambulate at least 25 ft]; grade 6 = unlimited walking [ambulatory without assistance and without significant limitations other than slightly dyscoordinated gait, must be able to ambulate at least 150 ft without a helper]). For patients with AIS-A and AIS-B injuries at baseline, “marked recovery” was defined by a conversion to (at a minimum) AIS-C and AIS-D, respectively (i.e., regaining sensory and motor function caudal to the level of injury). To achieve “marked recovery,” AIS-C and AIS-D patients were required to recover limited or unlimited walking function, respectively, according to the Benzel grades.
Secondary neurological outcomes included sensory and motor scores as determined by the ISNCSCI. In brief, motor scores are based on preserved muscle strength, which is evaluated on a 0 to 5 scale (0, complete paralysis; 5, full strength) in 5 upper and 5 lower limb key muscles (right and left, for a total of 100). Sensory scores were determined on a 3-point scale (0, none; 1, abnormal; 2, normal) separately for light touch and pinprick in 28 dermatomes (right and left, total of 112).
Other secondary safety outcomes included liver and renal enzyme assays from standard blood work. We categorized “detrimental outcomes” for blood chemistry as levels lower than standard cutoff for albumin (3.5 g/dL) and higher than standard cutoffs for alkaline phosphatase (147 U/L), alanine aminotransferase (56 U/L), aspartate aminotransferase (40 U/L), inorganic phosphorus (4.5 mg/dL), urea nitrogen (20 mg/dL), total bilirubin (1.2 mg/dL), and blood creatinine (1.2 mg/dL for males, 1.1 mg/dL for females) [21–27].
Statistical Analyses
For the primary outcome (marked recovery), hazard ratios (HRs) and corresponding 95% confidence intervals (CIs) were derived from multivariable Cox proportional hazards regression, stratified by AIS grade. Potential confounders included sex, age at injury, baseline lower extremity motor score (within 72 h post injury), and injury level (cervical vs thoracic). GM-1 administration was also considered as a potential confounder, though the original clinical trial showed no significant effects on marked recovery [13]. For the secondary outcomes (lower extremity motor scores, sensory scores, and blood chemistry values), Pearson correlation coefficients and 95% confidence intervals were computed, and their absolute values were classified as “weak” (0–0.39), “moderate”(0.4 to 0.59), “strong” (0.6–0.79), or “very strong” (0.8 to 1.0) [12]. R Statistical Software (Version 2.15.3) was used for all analyses.
Ethics Approval
Approval for this study (secondary analysis) was received by an institutional ethical standards committee on human experimentation at the University of British Columbia. The original Sygen clinical trial (results published elsewhere [13, 14]) also received ethical approval but was conducted before clinical trials were required to be registered. The data received from the original clinical trial were de-identified.
Results
Patient Characteristics and Summary Statistics
Based on the inclusion criteria, 651 patients were included in the analysis (mean age at injury, 33 years; 80% male); 77% were injured at the cervical level, 74% had a motor complete injury according to ISNCSCI, and 18% received baclofen within 30 days post injury. The median cumulative dose for baclofen was 220 mg (median daily dose was 30 mg; Fig. 1). Baclofen was administered orally in all patients. Cohort characteristics by cumulative baclofen exposure status are provided in Table 1.
Fig. 1.
Baclofen usage after spinal cord injury. (A) Patterns of baclofen use within first 30 days after injury; each row represents a unique patient; white spaces indicate no baclofen use during that period. (B) Histogram of total baclofen dosages in first 30 days after injury. (C) Histogram of timing of administration of first baclofen use within the first 30 days after injury
Table 1.
Cohort characteristics by baclofen status
| Characteristic | Entire cohort | No baclofen | Low-dose baclofen (total cumulative dose < 220 mg) | High-dose baclofen (total cumulative dose ≥ 220 mg) |
|---|---|---|---|---|
| Total count | 651 | 536 | 56 | 59 |
| Sex | ||||
| Females | 131 (20.1) | 104 (19.4) | 12 (21.4) | 15 (25.4) |
| Males | 520 (79.9) | 432 (80.6) | 44 (78.6) | 44 (74.6) |
| Age at injury [years] | 32.5 (13.4) | 32.4 (13.5) | 32.5 (12.8) | 34.0 (13.4) |
| Injury completeness | ||||
| AIS A | 412 (63.3) | 360 (67.2) | 30 (53.6) | 22 (37.3) |
| AIS B | 71 (10.9) | 56 (10.4) | 7 (12.5) | 8 (13.6) |
| AIS C | 139 (21.4) | 94 (17.5) | 17 (30.4) | 28 (47.5) |
| AIS D | 29 (4.5) | 26 (4.9) | 2 (3.6) | 1 (1.7) |
| Injury level | ||||
| Cervical | 499 (76.7) | 404 (75.4) | 44 (78.6) | 51 (86.4) |
| Thoracic | 152 (23.3) | 132 (24.6) | 12 (21.4) | 8 (13.6) |
| LEMS at 52 weeks | 12.9 (19.4) | 11.3 (18.6) | 12.2 (19.5) | 26.6 (20.3) |
| Change in LEMS motor score (4–52 weeks) | 6.0 (10.7) | 5.4 (10.4) | 6.3 (11.1) | 10.9 (11.4) |
| Light touch score at 52 weeks | 58.1 (32.7) | 56.3 (32.1) | 56.2 (31.4) | 75.3 (34.3) |
| Change in light touch score (4–52 weeks) | 7.5 (17.7) | 7.6 (17.8) | 7.9 (16.1) | 6.7 (18.2) |
| Pinprick score at 52 weeks | 51.2 (31.6) | 49.2 (30.7) | 51.3 (31.6) | 68.7 (34.4) |
| Change in pinprick score (4–52 weeks) | 7.2 (16.9) | 6.5 (16.2) | 8.1 (16.5) | 12.2 (21.9) |
| Albumin levels at 4 weeks [g/dL] | 3.5 (0.5) | 3.5 (0.5) | 3.5 (0.4) | 3.7 (0.4) |
| Albumin levels at 52 weeks [g/dL] | 4.2 (0.4) | 4.2 (0.4) | 4.3 (0.3) | 4.3 (0.4) |
| Alkaline phosphatase levels at 4 weeks [U/L] | 146.9 (80.9) | 151.0 (83.6) | 138.5 (71.3) | 116.9 (54.1) |
| Alkaline phosphatase levels at 52 weeks, [U/L] | 122.8 (74.1) | 126.7 (79.9) | 117.2 (44.4) | 97.8 (34.6) |
| Total bilirubin levels at 4 weeks [mg/dL] | 0.5 (0.3) | 0.5 (0.3) | 0.5 (0.2) | 0.5 (0.2) |
| Total bilirubin levels at 52 weeks [mg/dL] | 0.6 (0.9) | 0.6 (1.0) | 0.6 (0.3) | 0.6 (0.4) |
| Aspartate aminotransferase levels at 4 weeks [U/L] | 37.1 (26.5) | 38.0 (27.7) | 37.3 (22.1) | 28.0 (15.6) |
| Aspartate aminotransferase levels at 52 weeks [U/L] | 22.6 (11.1) | 22.6 (11.5) | 22.1 (9.8) | 22.4 (9.0) |
| Alanine aminotransferase levels at 4 weeks [U/L] | 74.8 (76.4) | 77.5 (80.8) | 70.1 (49.9) | 54.7 (47.8) |
| Alanine aminotransferase levels at 52 weeks [U/L] | 27.4 (24.7) | 27.7 (25.4) | 27.4 (24.9) | 25.3 (17.8) |
| Creatinine levels at 4 weeks [mg/dL] | 0.8 (0.3) | 0.8 (0.3) | 0.8 (0.3) | 0.8 (0.3) |
| Creatinine levels at 52 weeks [mg/dL] | 0.9 (0.3) | 0.8 (0.3) | 0.8 (0.2) | 0.9 (0.2) |
| Urea nitrogen levels at 4 weeks [mg/dL] | 14.7 (8.2) | 14.9 (8.4) | 13.8 (8.9) | 13.6 (4.3) |
| Urea nitrogen levels at 52 weeks [mg/dL] | 12.8 (7.1) | 13.0 (7.7) | 11.9 (4.1) | 12.2 (4.1) |
| Inorganic phosphorus levels at 4 weeks [mg/dL] | 4.5 (0.9) | 4.5 (0.9) | 4.6 (0.8) | 4.6 (0.7) |
| Inorganic phosphorus levels at 52 weeks [mg/dL] | 3.9 (1.3) | 4.0 (1.5) | 3.8 (0.4) | 3.7 (0.4) |
Continuous variables presented as mean (standard deviation); categorical variables presented as count (percentage)
Baclofen and Marked Recovery
There was no detrimental effect of baclofen exposure on marked recovery. In fact, high-dose baclofen was associated with a significantly higher rate of marked recovery in individuals with AIS A and C/D grades (Table 2, Fig. 2). The higher rates of recovery persisted after adjustment for age, sex, injury level, baseline LEMS, baseline AIS grade, and GM-1 administration. Thus, baclofen was not only safe with respect to neurologic recovery, but in higher doses was associated with improved neurological outcomes.
Table 2.
Hazard ratios for marked recovery (stratified by injury completeness)
| Baclofen cumulative dose | Crude HR [95% CI] | Adjusted HR-1 [95% CI] | Adjusted HR-2 [95% CI] | Adjusted HR-3 [95% CI] |
| Overall (all AIS grades combined) | (n = 651) | (n = 651) | (n = 630) | (n = 651) |
| None | Reference | Reference | Reference | Reference |
| Low | 1.1 [0.7, 1.8] | 0.9 [0.6, 1.5] | 0.7 [0.4, 1.2] | 0.9 [0.6, 1.5] |
| High | 3.4 [2.4, 4.8] | 2.1 [1.5, 3.0] | 2.1 [1.4, 3.0] | 2.1 [1.5, 3.0] |
| Crude HR [95% CI] | Adjusted HR-4 [95% CI] | Adjusted HR-5 [95% CI] | Adjusted HR-6 [95% CI] | |
| AIS A | (n = 412) | (n = 412) | (n = 402) | (n = 412) |
| None | Reference | Reference | Reference | Reference |
| Low | 0.4 [0.1, 1.8] | 0.4 [0.1, 1.8] | 0.4 [0.1, 1.8] | 0.4 [0.1, 1.8] |
| High | 4.8 [2.5, 9.2] | 4.6 [2.4, 8.9] | 4.5 [2.2, 9.2] | 4.7 [2.5, 9.1] |
| AIS B | (n = 71) | (n = 71) | (n = 71) | (n = 71) |
| None | Reference | Reference | Reference | Reference |
| Low | 0.3 [0.03, 1.9] | 0.2 [0.03, 1.8] | 0.3 [0.03, 1.9] | 0.2 [0.03, 1.8] |
| High | 1.8 [0.7, 4.6] | 1.9 [0.7, 5.0] | 1.8 [0.7, 4.6] | 1.6 [0.6, 4.4] |
| AIS C/D | (n = 168) | (n = 168) | (n = 157) | (n = 168) |
| None | Reference | Reference | Reference | Reference |
| Low | 1.3 [0.8, 2.2] | 1.3 [0.8, 2.2] | 1.0 [0.5, 1.8] | 1.3 [0.8, 2.2] |
| High | 1.5 [1.0, 2.4] | 1.6 [1.01, 2.5] | 1.9 [1.2, 2.9] | 1.5 [1.0, 2.4] |
High dose = cumulative exposure of ≥ 220 mg within 30 days post injury; low dose = cumulative exposure of < 220 mg within 30 days post injury. HR-1 adjusted for age, sex, injury level, baseline AIS grade; HR-2 adjusted for baseline lower extremity motor score, baseline AIS grade; HR-3 adjusted for GM-1 administration, baseline AIS grade; HR-4 adjusted for age, sex, injury level; HR-5 adjusted for baseline lower extremity motor score; HR-6 adjusted for GM-1 administration. AIS = American Spinal Injury Association (ASIA) Impairment Scale; significant values (P < 0.05) are italicized. Square brackets indicate 95% confidence intervals; round brackets indicate sample sizes; sample sizes vary slightly for adjusted hazard ratio due to missing data for lower extremity motor score
Fig. 2.
Survival curves for marked recovery. AIS = American Spinal Injury Association (ASIA) Impairment Scale. Survival curves were derived from Cox Proportional Hazards regression models. High dose = cumulative exposure of ≥ 220 mg within 30 days post injury; low dose = cumulative exposure of < 220 mg within 30 days post injury
Baclofen and Sensory Outcomes: Pinprick
Table 3 shows the relationship between cumulative baclofen exposure during the first month following injury and pinprick scores. Cumulative baclofen exposure was generally not significantly associated with: pinprick sensory scores at 4 weeks or 52 weeks or the change in pinprick sensory scores from 4 weeks until 52 weeks. The only exception was in sensorimotor complete injuries (AIS-A), where there was a weak positive correlation between cumulative baclofen exposure and pinprick scores.
Table 3.
Correlation between cumulative baclofen exposure and sensorimotor outcomes
| Measure | Outcome | N | Correlation coefficient [95% CI] | P value |
|---|---|---|---|---|
| AIS A | ||||
| Pinprick score | 4 weeks | 393 | 0.15 [0.05, 0.25] | 0.002 |
| 52 weeks | 365 | 0.16 [0.059, 0.26] | 0.002 | |
| Change from 4 weeks to 52 weeks | 353 | 0.05 [− 0.05, 0.15] | 0.35 | |
| Light touch score | 4 weeks | 393 | 0.13 [0.04, 0.23] | 0.008 |
| 52 weeks | 366 | 0.11 [0.008, 0.21] | 0.03 | |
| Change from 4 weeks to 52 weeks | 354 | 0.004 [− 0.0996, 0.11] | 0.93 | |
| LEMS | 4 weeks | 388 | 0.4 [0.31, 0.48] | < 0.001 |
| 52 weeks | 360 | 0.24 [0.14, 0.34] | < 0.001 | |
| Change from 4 weeks to 52 weeks | 346 | 0.11 [0.005, 0.21] | 0.04 | |
| AIS B | ||||
| Pinprick score | 4 weeks | 65 | − 0.11 [− 0.34, 0.13] | 0.37 |
| 52 weeks | 59 | 0.048 [− 0.21, 0.30] | 0.71 | |
| Change from 4 weeks to 52 weeks | 57 | 0.2 [− 0.055, 0.44] | 0.12 | |
| Light touch score | 4 weeks | 65 | − 0.12 [− 0.35, 0.13] | 0.34 |
| 52 weeks | 59 | 0.083 [− 0.17, 0.33] | 0.53 | |
| Change from 4 weeks to 52 weeks | 57 | 0.21 [− 0.04, 0.45] | 0.10 | |
| LEMS | 4 weeks | 63 | 0.18 [− 0.07, 0.41] | 0.15 |
| 52 weeks | 57 | 0.20 [− 0.05, 0.44] | 0.12 | |
| Change from 4 weeks to 52 weeks | 53 | 0.10 [− 0.17, 0.36] | 0.45 | |
| AIS C/D | ||||
| Pinprick score | 4 weeks | 157 | − 0.044 [− 0.20, 0.11] | 0.58 |
| 52 weeks | 142 | − 0.055 [− 0.22, 0.11] | 0.51 | |
| Change from 4 weeks to 52 weeks | 136 | 0.024 [− 0.14, 0.19] | 0.78 | |
| Light touch score | 4 weeks | 157 | 0.06 [− 0.093, 0.22] | 0.42 |
| 52 weeks | 142 | − 0.028 [− 0.19, 0.14] | 0.74 | |
| Change from 4 weeks to 52 weeks | 136 | − 0.09 [− 0.25, 0.078] | 0.29 | |
| LEMS | 4 weeks | 149 | 0.001 [− 0.16, 0.16] | 0.99 |
| 52 weeks | 138 | − 0.008 [− 0.17, 0.16] | 0.92 | |
| Change from 4 weeks to 52 weeks | 124 | − 0.0072 [− 0.18, 0.17] | 0.94 | |
Significant values (P < 0.05) are italicized
LEMS = lower extremity motor score, AIS = American Spinal Injury Association (ASIA) Impairment Scale
Baclofen and Sensory Outcomes: Light Touch
Table 3 shows the relationship between cumulative baclofen exposure during the first month following injury and light touch scores. Cumulative baclofen exposure was generally not significantly associated with light tough sensory scores at 4 weeks or 52 weeks or the change in light tough sensory scores from 4 weeks until 52 weeks. The only exception was in sensorimotor complete injuries (AIS-A), where there was a weak positive correlation between cumulative baclofen exposure and light tough scores.
Baclofen and Motor Outcomes
Table 3 shows the relationship between cumulative baclofen exposure during the first month following injury and lower extremity motor scores. Cumulative baclofen exposure was generally not significantly associated with lower extremity motor scores at 4 weeks or 52 weeks or the change in lower extremity motor score from 4 weeks until 52 weeks. The only exception was in sensorimotor complete injuries (AIS-A), where there was a weak positive correlation between cumulative baclofen exposure and motor outcome.
Baclofen and Liver/Renal Enzymes
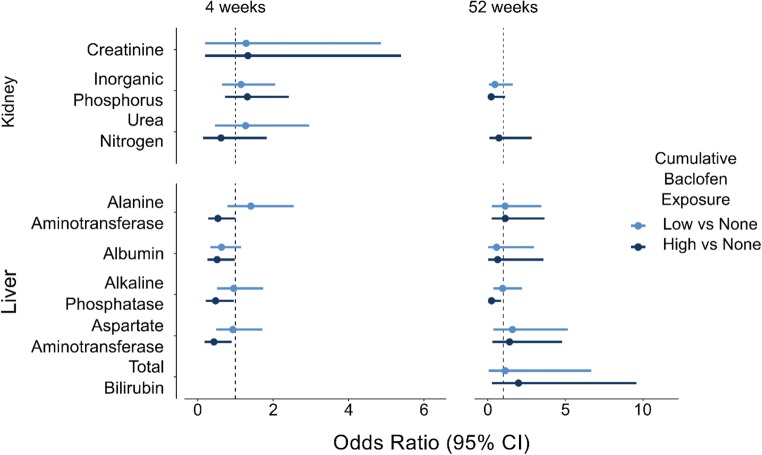
Cumulative baclofen exposure was not significantly associated with increased odds of detrimental liver and renal outcomes at 4 or 52 weeks post injury (Fig. 3).
Fig. 3.
Relationship between baclofen and renal and hepatotoxicity. Odds ratios and 95% confidence intervals for detrimental outcome (high or low value, depending on the assay). Reference category for odds ratio: no baclofen. There were no odds ratios produced for total bilirubin at 4 weeks and creatinine at 52 weeks because the cell counts were too small to produce a reliable estimate
Missing Data
The demographics of those included in Sygen but excluded from our cohort did not significantly differ in age (33 years), sex (84% male), or injury level (70% were injured at the cervical level; P > 0.05).
Other Anti-spasticity Medications
Among the cohort, other medications indicated for spasticity within the first 30 days post injury included the following: diazepam, methobarbamol, belladonna alkaloids/opium, carbamazepine, carisoprodol, chlorzoxazone, clonazepam, clonoidine, cyclobenzaprine, desipramine, atropine and diphenoxylate, gabapentin, glycopyrrolate, ibuprofen, ketorolac, lorazepam, methocarbamol, acetaminophen and methocarbamol, midazolam, and oxybutynin. Cumulative exposure (over the first 30 days) to these medications indicated for muscle spasms, but excluding baclofen, was not associated with marked recovery (crude HR 1.12 [0.58, 1.36]; P > 0.05).
Discussion
In a large sample of individuals with acute spinal cord injury, we found no evidence that baclofen limits neurologic recovery during the transition from acute to chronic injury. Based on these observations, we provide level 3 evidence that the administration of baclofen within the first month post injury at therapeutic doses for the management of spasticity and involuntary muscle spasms is safe. Our findings also demonstrate no adverse effects on liver or kidney function. From this knowledge, informed medical decisions can be made regarding acute spinal cord injury care.
In the absence of acute interventions to enhance neurologic recovery, it is imperative to understand the degree to which pharmacological management of complications arising from damaging the spinal cord (e.g., spasticity) has long-term effects. Prior studies have demonstrated mixed results with respect to the use of anti-spasticity agents on motor and functional outcomes after spinal cord injury [28]. Three small studies (n = 27, n = 18, n = 12) found that baclofen produced minor functional improvements in individuals with chronic (> 1 year) spinal cord injury [29–31]. The benefits of baclofen were presumably related to the relief of severe involuntary muscle spasms, which facilitated better performance of activities of daily living. A more recent study of individuals with acute and chronic injuries (n = 1259, 2–275 days post injury) reported that anti-spasticity medications (including baclofen) had no effect on muscle strength between admission and discharge [32]. Limitations of this previous study are that anti-spasticity medications were grouped together and timing (or dosing) of administration was not considered.
The strength of our study is that detailed baclofen administration information, including timing and dose, was incorporated into the analysis. We focused specifically on baclofen administered in the first 30 days post injury, which was done to determine the effect of exposure during the “window of opportunity” for neurologic repair and recovery. Indicating drug safety, none of the neurological outcomes, nor observations from the analysis of hematological data (i.e., secondary safety outcome), indicated a detrimental effect.
In startling contrast, baclofen exposure was consistently associated with improved neurological outcomes. This was observed as a significant effect in individuals with AIS A and C/D injuries (note that AIS B showed a similar trend), and independent of level of injury (cervical/thoracic). There are a number of potential explanations for a beneficial effect. First, baclofen could be relieving involuntary flexor and extensor muscle spasms, which facilitate the recovery of muscle strength. This, however, does not explain improvements in pinprick and light touch scores, which were necessary for marked recovery to occur in individuals with AIS A.
Second, the 1-month cumulative dosage of baclofen could indicate a subgroup of sensorimotor complete individuals with “spastic paralysis” early after injury. By this, acute baclofen administration may have no causal effect on recovery, but rather is a marker for more incomplete injury among individuals with AIS A injuries. This, in turn, may have led to greater neurological recovery. In such a case, greater recovery associated with the administration of baclofen is a type of indication bias [33]. However, we found that other medications indicated for spasticity were not associated with neurological outcomes, which provides more support for baclofen (vs spasticity itself) as the causal factor. Nevertheless, recognizing early spasticity could serve to improve prognosis of a cohort of patients (i.e., AIS A) in which current prediction is extremely difficult.
Finally, baclofen could also pharmacologically modify central nervous system activity underlying spinal cord injury repair. GABA-B receptors play an integral role in the neuro-protection and preservation of white matter during anoxic injury by decreasing glutaminergic activity and reducing synaptic hyperactivity [34, 35]. Baclofen has also been suggested to improve myelination in peripheral nerves [36–39]. This is purportedly mediated through an interaction with GABA-B receptors on glial cells and supported by evidence that GABA-B-deficient mice exhibit morphological and molecular changes in peripheral myelin [36–39]. Further basic science research is needed to address the biological plausibility (i.e., a pillar of causality) of enhancing neurologic recovery after spinal cord injury by manipulating GABA-B function.
Our study also highlights a potential application of concomitant medication files in drug safety studies. Most monitored clinical trials track concomitant medications, generally due to safety concerns of drug interactions. Despite advances in methodology for summarizing concomitant medication information [40], these data are largely ignored. However, as we have shown, concomitant medication files can provide important exposure data for drugs other than the study drug of interest.
Spinal cord injury is a unique condition in which a considerable number of concomitant medications are likely to be administered during an acute clinical trial. These include cardiovascular medications and antibiotics, as well as a variety of anticonvulsants, antidepressants, and anxiolytics. For medications that interact in the central nervous system or systems associated with neurological recovery (e.g., cardiovascular), there is an urgent need to establish drug safety and inform acute care management practices. The potential for some of these medications (e.g., gabapentinoids) to enhance neurological recovery has also recently been examined [41, 42].
The primary limitation of the proposed study is that the Sygen data represents a historical clinical trial, first initiated in the 1992 and completed in 1997. Sygen data has been used in previous studies to describe the longitudinal progression of spinal cord injury, and these recovery profiles (in both the placebo group and the treatment group) are similar to those from more contemporary data sources [19]. However, some acute management practices have changed since this trial concluded. Most notable is the discontinuation of methylprednisolone as a standard of care. Since methylprednisolone was administered to all subjects in Sygen, we could not account for differential exposure between high, low, and no baclofen groups. Recent and comprehensive analysis of methylprednisolone, however, indicates no effects on neurologic outcomes [43]. Moreover, methylprednisolone would only be a confound if also associated with baclofen exposure/spasticity, for which there is no evidence. Interestingly, clinical practice guidelines for spasticity management with baclofen have not changed since Sygen [44–47]. A recent study in acute spinal cord injury found a similar likelihood of anti-spasmodic administration in the first month post injury [48], with oral baclofen the most commonly administered [48]. Thus, we are confident our results generalize to the wider (and contemporary) spinal cord injury population. In addition, Sygen represents the largest acute trial in the field of spinal cord injury to date [13], further adding to the generalizability of our study. Another common limitation of observational study design is confounding and misclassification of exposures and outcomes. We attempted to account for confounding in our multivariable analysis, and our medication exposures were captured in-hospital by study investigators (and according to FDA guidelines), adding to the validity of drug records. Also, as the data were collected as part of a clinical trial, the issue of missing data is reduced in comparison with other observational studies within spinal cord injury where subject drop-out is more common [19]. Although lacking randomization, previous research has found that the results of well-designed observational studies (i.e., a detailed assessment of confounding) provide similar results as clinical trials [49–52]. Thus, the outcome of our analysis should be taken as a valid indication of baclofen safety.
Conclusions
This analysis provides evidence on the safety of baclofen in the early days after acute traumatic spinal cord injury with the recommended doses for symptomatic muscle spasms. In addition to standard safety endpoints, neurological outcomes should also be considered a unique aspect of drug safety profiles for commonly used centrally acting medications. This study also highlights the use of concomitant medication files (from completed clinical trials) and incorporating patient concerns in drug safety studies.
Acknowledgments
Dr. Cragg is supported by the Society in Science—Branco Weiss Postdoctoral Fellowship and the Michael Smith Foundation for Health Research (MSFHR). Dr. Kramer is supported by a Scholar Award from the MSFHR and Rick Hansen Institute, as well as the Canadian Institutes of Health Research, ERA-NET NEURON, Wings for Life, and the International Foundation for Research in Paraplegia (IRP). Dr. Jutzeler is supported by the IRP and is a Craig H. Nielsen Foundation postdoctoral fellow. Ms. Warner is supported by the University of British Columbia Four Year Fellowship.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author Contributions
JJC was responsible for the design and conceptualization of the study, data analyses, and drafting the manuscript. BT was responsible for data cleaning, data analyses, and drafting the manuscript. CRJ, FMW, and NC were responsible for interpretation of data and revising the manuscript for intellectual content. FG was responsible for primary data collection, interpretation of data, and revising the manuscript for intellectual content. JLK was responsible for study concept/design, interpretation of data, and revising the manuscript for intellectual content.
Compliance with Ethical Standards
Approval for this study (secondary analysis) was received by an institutional ethical standards committee on human experimentation at the University of British Columbia.
Disclosures
All authors report no disclosures.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jacquelyn J. Cragg and Bobo Tong contributed equally to this work.
References
- 1.Tator CH. Update on the Pathophysiology and Pathology of Acute Spinal Cord Injury. Brain Pathol. 1995;5:407–413. doi: 10.1111/j.1750-3639.1995.tb00619.x. [DOI] [PubMed] [Google Scholar]
- 2.Krueger H, Noonan VK, Trenaman LM, et al. The economic burden of traumatic spinal cord injury in Canada. Chronic Dis Inj Can. 2013;33:113–122. [PubMed] [Google Scholar]
- 3.Noonan VK, Fingas M, Farry A, et al. Incidence and Prevalence of Spinal Cord Injury in Canada: A National Perspective. Neuroepidemiology. 2012;38:219–226. doi: 10.1159/000336014. [DOI] [PubMed] [Google Scholar]
- 4.Elbasiouny SM, Moroz D, Bakr MM, Mushahwar VK. Management of Spasticity After Spinal Cord Injury: Current Techniques and Future Directions. Neurorehabil Neural Repair. 2010;24:23–33. doi: 10.1177/1545968309343213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adams M, Hicks A. Spasticity after spinal cord injury. Spinal Cord. 2005;43:577–586. doi: 10.1038/sj.sc.3101757. [DOI] [PubMed] [Google Scholar]
- 6.Kwon BK, Tetzlaff W, Grauer JN, et al. Pathophysiology and pharmacologic treatment of acute spinal cord injury. Spine J. 2004;4:451–64. doi: 10.1016/j.spinee.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 7.Tator CH, Fehlings MG. Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg. 1991;75:15–26. doi: 10.3171/jns.1991.75.1.0015. [DOI] [PubMed] [Google Scholar]
- 8.Belegu V, Oudega M, Gary DS, McDonald JW. Restoring Function After Spinal Cord Injury: Promoting Spontaneous Regeneration with Stem Cells and Activity-Based Therapies. Neurosurg. Clin. N. Am. 2007;18:143–168. doi: 10.1016/j.nec.2006.10.012. [DOI] [PubMed] [Google Scholar]
- 9.McDonald JW, Sadowsky CL, Stampas A. The changing field of rehabilitation: Optimizing spontaneous regeneration and functional recovery. Handb Clin Neurol. 2012;109:317–336. doi: 10.1016/B978-0-444-52137-8.00020-6. [DOI] [PubMed] [Google Scholar]
- 10.Yelnik AP, Simon O, Bensmail D, et al. Drug treatments for spasticity. Ann Phys Rehabil Med. 2009;52:746–756. doi: 10.1016/j.rehab.2009.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Dr. Wise Young - Baclofen Question. http://sci.rutgers.edu/forum/showthread.php?133388-Dr-Wise-Young-Baclofen-Question. Accessed 6 Apr 2018
- 12.11. Correlation and regression | The BMJ. https://www.bmj.com/about-bmj/resources-readers/publications/statistics-square-one/11-correlation-and-regression. Accessed 6 Apr 2018
- 13.Geisler FH, Coleman WP, Grieco G, et al. The Sygen multicenter acute spinal cord injury study. Spine (Phila Pa 1976) 2001;26:S87–98. doi: 10.1097/00007632-200112151-00015. [DOI] [PubMed] [Google Scholar]
- 14.Geisler FH, Coleman WP, Grieco G, et al. Recruitment and early treatment in a multicenter study of acute spinal cord injury. Spine (Phila Pa 1976) 2001;26:S58–67. doi: 10.1097/00007632-200112151-00013. [DOI] [PubMed] [Google Scholar]
- 15.Hadley MN, Walters BC. Introduction to the Guidelines for the Management of Acute Cervical Spine and Spinal Cord Injuries. Neurosurgery. 2013;72:5–16. doi: 10.1227/NEU.0b013e3182773549. [DOI] [PubMed] [Google Scholar]
- 16.Hadley MN, Walters BC, Grabb PA, et al. Guidelines for the management of acute cervical spine and spinal cord injuries. Clin. Neurosurg. 2002;49:407–498. [PubMed] [Google Scholar]
- 17.Geisler FH, Coleman WP, Grieco G, et al. Measurements and recovery patterns in a multicenter study of acute spinal cord injury. Spine (Phila Pa 1976) 2001;26:S68–86. doi: 10.1097/00007632-200112151-00014. [DOI] [PubMed] [Google Scholar]
- 18.Fawcett JW, Curt A, Steeves JD, et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord. 2007;45:190–205. doi: 10.1038/sj.sc.3102007. [DOI] [PubMed] [Google Scholar]
- 19.Steeves JD, Kramer JK, Fawcett JW, et al. Extent of spontaneous motor recovery after traumatic cervical sensorimotor complete spinal cord injury. Spinal Cord. 2011;49:257–65. doi: 10.1038/sc.2010.99. [DOI] [PubMed] [Google Scholar]
- 20.Kirshblum SC, Burns SP, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury (revised 2011) J Spinal Cord Med. 2011;34:535–46. doi: 10.1179/204577211X13207446293695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Albumin: Reference Range, Interpretation, Collection and Panels. https://emedicine.medscape.com/article/2054430-overview. Accessed 6 Apr 2018
- 22.ALP - blood test. http://arh.adam.com/content.aspx?productId=101&pid=1&gid=003470. Accessed 6 Apr 2018
- 23.Hepatitis C, Liver Enzyme Levels | Hepatitis Central. http://www.hepatitiscentral.com/hcv/labs/liverenzymes/. Accessed 6 Apr 2018
- 24.Hyperphosphatemia (High Phosphate) - Managing Side Effects - Chemocare. http://chemocare.com/chemotherapy/side-effects/hyperphosphatemia-high-phosphate.aspx. Accessed 6 Apr 2018
- 25.Blood urea nitrogen (BUN) test - About - Mayo Clinic. https://www.mayoclinic.org/tests-procedures/blood-urea-nitrogen/about/pac-20384821. Accessed 6 Apr 2018
- 26.Bilirubin blood test Information | Mount Sinai - New York. http://www.mountsinai.org/health-library/tests/bilirubin-blood-test. Accessed 6 Apr 2018
- 27.What Is a Creatinine Blood Test? Symptoms, Low & High Ranges. https://www.medicinenet.com/creatinine_blood_test/article.htm. Accessed 6 Apr 2018
- 28.Domingo A, Al-Yahya AA, Asiri Y, et al. A Systematic Review of the Effects of Pharmacological Agents on Walking Function in People with Spinal Cord Injury. J Neurotrauma. 2012;29:865–879. doi: 10.1089/neu.2011.2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dario A, Scamoni C, Bono G, et al. Functional improvement in patients with severe spinal spasticity treated with chronic intrathecal baclofen infusion. Funct Neurol. 2001;16:311–5. [PubMed] [Google Scholar]
- 30.Azouvi P, Mane M, Thiebaut JB, et al. Intrathecal baclofen administration for control of severe spinal spasticity: Functional improvement and long-term follow-up. Arch Phys Med Rehabil. 1996;77:35–39. doi: 10.1016/S0003-9993(96)90217-8. [DOI] [PubMed] [Google Scholar]
- 31.Norman KE, Pepin A, Barbeau H. Effects of drugs on walking after spinal cord injury. Spinal Cord. 1998;36:699–715. doi: 10.1038/sj.sc.3100674. [DOI] [PubMed] [Google Scholar]
- 32.Theriault ER, Huang V, Whiteneck G, et al. Antispasmodic medications may be associated with reduced recovery during inpatient rehabilitation after traumatic spinal cord injury. J Spinal Cord Med. 2016;00:1–9. doi: 10.1080/10790268.2016.1245010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Psaty BM, Siscovick DS. Minimizing Bias Due to Confounding by Indication in Comparative Effectiveness Research. JAMA. 2010;304:897. doi: 10.1001/jama.2010.1205. [DOI] [PubMed] [Google Scholar]
- 34.Green AR, Hainsworth AH, Jackson DM. GABA potentiation: a logical pharmacological approach for the treatment of acute ischaemic stroke. Neuropharmacology. 2000;39:1483–94. doi: 10.1016/S0028-3908(99)00233-6. [DOI] [PubMed] [Google Scholar]
- 35.Costa C, Leone G, Saulle E, et al. Coactivation of GABAA and GABAB Receptor Results in Neuroprotection during In Vitro Ischemia. Stroke. 2004;35:596–600. doi: 10.1161/01.STR.0000113691.32026.06. [DOI] [PubMed] [Google Scholar]
- 36.Chumakov I, Milet A, Cholet N, et al (2014) Polytherapy with a combination of three repurposed drugs (PXT3003) down-regulates Pmp22 over-expression and improves myelination, axonal and functional parameters in models of CMT1A neuropathy. Orphanet J Rare Dis 9. 10.1186/s13023-014-0201-x [DOI] [PMC free article] [PubMed]
- 37.Fern R, Waxman SG, Ransom BR. Endogenous GABA attenuates CNS white matter dysfunction following anoxia. J Neurosci. 1995;15:699–708. doi: 10.1523/JNEUROSCI.15-01-00699.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Luyt K, Slade TP, Dorward JJ, et al. Developing oligodendrocytes express functional GABAB receptors that stimulate cell proliferation and migration. J Neurochem. 2007;100:822–840. doi: 10.1111/j.1471-4159.2006.04255.x. [DOI] [PubMed] [Google Scholar]
- 39.Magnaghi V, Ballabio M, Cavarretta IT, et al. GABAB receptors in Schwann cells influence proliferation and myelin protein expression. Eur J Neurosci. 2004;19:2641–2649. doi: 10.1111/j.0953-816X.2004.03368.x. [DOI] [PubMed] [Google Scholar]
- 40.Barker C. Exploratory method for summarizing concomitant medication data - The mean cumulative function. Pharm Stat. 2010;9:331–336. doi: 10.1002/pst.395. [DOI] [PubMed] [Google Scholar]
- 41.Warner FM, Cragg JJ, Jutzeler CR, et al. Early Administration of Gabapentinoids Improves Motor Recovery after Human Spinal Cord Injury. Cell Rep. 2017;18:1614–1618. doi: 10.1016/j.celrep.2017.01.048. [DOI] [PubMed] [Google Scholar]
- 42.Cragg JJ, Haefeli J, Jutzeler CR, et al. Effects of Pain and Pain Management on Motor Recovery of Spinal Cord-Injured Patients: A Longitudinal Study. Neurorehabil Neural Repair. 2016;30:753–61. doi: 10.1177/1545968315624777. [DOI] [PubMed] [Google Scholar]
- 43.Short DJ, El Masry WS, Jones PW (2000) High dose methylprednisolone in the management of acute spinal cord injury - A systematic review from a clinical perspective. Spinal Cord [DOI] [PubMed]
- 44.Drugs.com | Prescription Drug Information, Interactions & Side Effects. https://www.drugs.com/. Accessed 6 Apr 2018
- 45.Orange Book: Approved Drug Products with Therapeutic Equivalence Evaluations. https://www.accessdata.fda.gov/scripts/Cder/ob/index.cfm. Accessed 6 Apr 2018
- 46.Baclofen (Baclofen Tablets): Side Effects, Interactions, Warning, Dosage & Uses. https://www.rxlist.com/baclofen-drug.htm#indications_dosage. Accessed 6 Apr 2018
- 47.Smith C, LaRocca N, Giesser B, Scheinberg L (1991) High-dose oral baclofen: Experience in patients with multiple sclerosis. Neurology 1829–1831 [DOI] [PubMed]
- 48.Holtz KA, Szefer E, Noonan VK, et al (2018) Treatment patterns of in-patient spasticity medication use after traumatic spinal cord injury: a prospective cohort study. Spinal Cord. 10.1038/s41393-018-0165-0 [DOI] [PubMed]
- 49.Black N. Why we need observational studies to evaluate the effectiveness of health care. BMJ. 1996;312:1215–8. doi: 10.1136/bmj.312.7040.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Benson K, Hartz AJ. A comparison of observational studies and randomized, controlled trials. N Engl J Med. 2000;342:1878–86. doi: 10.1056/NEJM200006223422506. [DOI] [PubMed] [Google Scholar]
- 51.Hernández-Díaz S, McElrath TF, Pennell PB, et al. Fetal growth and premature delivery in pregnant women on antiepileptic drugs. Ann Neurol. 2017;82:457–465. doi: 10.1002/ana.25031. [DOI] [PubMed] [Google Scholar]
- 52.Devinsky O, Leppik I, James Willmore L, et al. Safety of intravenous valproate. Ann Neurol. 1995;38:670–674. doi: 10.1002/ana.410380418. [DOI] [PubMed] [Google Scholar]