Abstract
Photobiomodulation (PBM) is a rapidly growing as an innovative therapeutic modality for various types of diseases in recent years. Neuronal degeneration is irreversible process and it is proven to be difficult to slow down or stop the progression. Pharmacologic approaches to slow neuronal degeneration have been studied, but are limited due to concerns about the side effects. Therefore, it is necessary to develop a new therapeutic approach to stabilize neuronal degeneration and achieve neuronal protection against several neurodegenerative diseases. In this review, we have introduced several previous studies showing the positive effect of PBM over neurodegenerative disorders such as Alzheimer’s disease, Parkinson’s disease and different types of epilepsy. Despite excellent outcomes of animal researches, not many clinical studies are conducted or showed positive outcome of PBM against neurodegenerative disease. To achieve clinical application of PBM against neurodegenerative disorder, determination of exact mechanism and establishment of effective clinical protocol seems to be necessary.
Keywords: Photobiomodulation, Neurodegenerative diseases, Alzheimer’s diseases, Parkinson’s diseases, Epilepsy
Introduction
Photobiomodulation (PBM) is a therapy that utilizes light energy as a treatment for a variety of diseases. This technique uses low-power light from red to near-infrared wavelengths from a laser or light-emitting diode (LED) to modulate biological functions or induce therapeutic effects. The light source of PBM is usually obtained from a laser or LED. The laser source can produce consistent light energy at a single wavelength. Lasers has the high tissue penetration and a constant beam width. It also enables a large amount of rapid energy delivery with high efficiency. However, the area of tissues exposed with lasers can be insufficient for some kind of transcranial applications, and repeated single beam exposure may be required. LED typically has a bandwidth of 20–40 nm at the full width at half maximum and it is not coherent and collimated beam. In addition, LED can be mounted on ergonomic arrays for efficient energy delivery, which has suitability for a large surface area organ such as the brain. Recently, PBM has attracted attention as a novel therapeutic application for various medical conditions including retinal diseases, stroke, neuromuscular disorders, and mood disorders. PBM can occur a wide variety of processes that can benefit various brain disorders [1]. PBM increases the oxygen consumption of intracellular mitochondria and induces more ATP production. In addition, PBM produces more ROS that leads to gene transcription and then to cell recovery and healing. It is also known that to promote blood circulation through the release of nitric oxide (NO). Additionally, the use of PBM for the treatment of neurodegenerative diseases has increased over the last decade [1–4]. It has been suggested that PBM may be an alternative treatment for the prevention or attenuation of neuronal degeneration that does not induce biological side effects, which is a limitation of drugs that affect brain function.
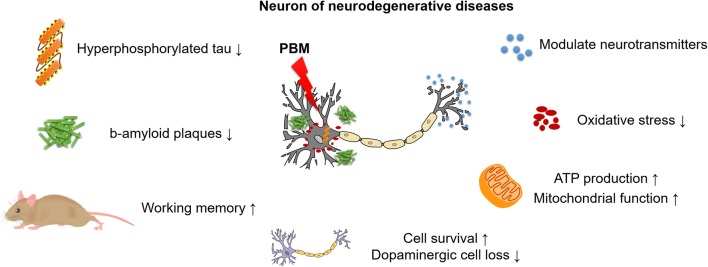
Two of the most common neurodegenerative disorders are Alzheimer’s disease and Parkinson’s disease, which both result in progressive degeneration and death in a significant number of neurons. Although many pharmacological treatments have been employed to treat these disorders, the progressive degeneration and death of neurons in patients remain severe and it is difficult to slow their progression. Current trends in clinical therapies alleviate the memory and cognitive deficits associated with Alzheimer’s disease and contribute to a lack of motor symptoms in patients with Parkinson’s disease but do not slow the progression of neuronal degeneration or exert neuroprotective effects. However, several recent studies using animal models of Alzheimer’s disease and Parkinson’s disease have shown that PBM has neuroprotective effects that slow neuronal cell death (Fig. 1).
Fig. 1.
Benefits of Photobiomodulation (PBM) on neurons of neurodegenerative diseases
The present review will investigate current trends in research on these diseases and the effects of PBM treatment with a focus on evidence of neuroprotection and its underlying mechanisms. Additionally, the possible applications of PBM for other neurodegenerative diseases will be discussed.
Alzheimer’s disease and PBM
Among seniors, Alzheimer’s disease is a main cause of death due to progressive memory deficits and cognitive impairments that result in mental disability and impaired executive functions [5, 6]. In general, individuals with Alzheimer’s disease suffer from neuronal damage in many areas of the brain, particularly the cortex and hippocampus [5, 7], as well as clinical consequences such as confusion, language disturbances, visual deficits, hallucinations, and behavioral disturbances. Alzheimer’s disease begins with dementia, which typically includes memory failures referred to as mild cognitive impairment (MCI), and is characterized by the over-phosphorylation of β-amyloid plaques and tau proteins and wide-ranging gliosis. β-amyloid plaques are produced from amyloid precursors, and the hyperphosphorylation of tau proteins results in intracellular neurofibrillary tangles [8–10]. The pathological effects of extracellular plaques during the early stages of Alzheimer’s disease include the accumulation of intracellular β-amyloid proteins, which leads to axonal defects, synaptic damage, and neuronal death [11]. Tau, which is a microtubule-associated protein, is more abundant in neurons than astrocytes or oligodendrocytes and plays a key role in stimulating tubulin in microtubules in the brain [12]. However, the abnormal hyperphosphorylation of tau proteins disassembles microtubules and results in the destabilization of tau and other microtubule-associated proteins. These abnormal structures alter cytoplasmic functions and interfere with neuronal transportation, which may lead to cell death.
In general, both of these disease processes occur in the cerebrum but tend to exhibit different patterns of development. β-amyloid plaques are initially observed in the cortex and subsequently in subcortical regions whereas hyperphosphorylated tau proteins are first found in subcortical regions and then in the cortex [13]. Although the underlying causes and mechanisms of these pathologies remain unclear, the most common hypothesis is that the accumulation of β-amyloid leads to the formation of neurofibrillary tangles and subsequent cell death [10]. This hypothesis also posits that the aging process will induce damage to cerebral capillaries that results in microhemorrhages, β-amyloid accumulation, the formation of neurofibrillary tangles, neuronal degeneration and, ultimately, cell death that will lead to downstream cerebral vascular damage and mitochondrial dysfunction in damaged neurons [14–22]. The current treatment options for patients with Alzheimer’s disease are not very effective and have limitations. In fact, these drugs are ineffective for most patients and are associated with a variety of toxic side effects [6].
Alzheimer’s disease-induced neuronal death is likely to be accompanied by a significant decline in cellular energy production [23], which can be ameliorated by PBM [24–30]. PBM may protect against the neuronal death and mitochondrial dysfunction associated with Alzheimer’s disease, which is why this novel treatment has such broad potential (Table 1). In transgenic animal models associated with β-amyloid or tau, PBM reduces cognitive deficits, β-amyloid plaques, tau-associated neurofibrillary tangles, and oxidative stress while increasing the production of adenosine triphosphate (ATP) and enhancing mitochondrial function [31–36]. Additionally, in vitro studies have shown that PBM decreases β-amyloid plaques while increasing cell survival and ATP production [37]. However, although PBM exerts neuroprotective effects in various experimental models of Alzheimer’s disease, there is little clinical evidence of its therapeutic efficacy.
Table 1.
Photobiomodulation studies relevant to neuroprotection in Alzheimer’s disease
| Source | Parameters | Models | Effect | References |
|---|---|---|---|---|
| Laser | 1070 nm, 6 min for 10 days | In vivo (mouse) | Improved acquisition of working memory in middle-aged mice | Michalikova et al. [33] |
| Laser | 808 nm, 0.5 W/cm2, 2.8 W/cm2 and 5.6 W/cm2, 675 J/cm2, 336 J/cm2 and 672 J/cm2 for 6 months | In vivo (mouse) | Decreased escape latency in Morris water maze, Decreased brain b-amyloid aggregates and pro-inflammatory cytokines, Increased ATP concentration and oxygen consumption | De Taboada et al. [31] |
| Laser | 670 nm, 33 mW, l × l04 Jm−2 | In vitro (human) | Increased cell survival and ATP production, Decreased b-amyloid aggregates | Sommer et al. [37] |
| LED | 1072 nm, 5 mW/cm2 for 6 min for two consecutive days, biweekly for 5 months | In vivo (mouse) | Decreased b-amyloid plaques. Increased heat shock proteins (HSPs) | Grillo et al. [32] |
| LED | 670 nm, 4 J/cm2 for 5 days per week | In vivo (mouse) | Decreased b-amyloid plaques. Oxidative stress and hyperphosphorylated tau | Purushothuman et al. [34, 35] |
| LED | 627 nm, 7 J/cm2 (70 mW) for 21 days | In vivo (rat) | Decreased b-amyloid. Improved spatial memory and behavioral state | da Luz Eltchechem et al. [36] |
Parkinson’s disease and PBM
Although Alzheimer’s disease and Parkinson’s disease both result in neurodegeneration, the causes, brain lesions, and clinical symptoms associated with each disorder differ. Unlike Alzheimer’s disease, Parkinson’s disease does not result in plaques or tangles, causes a limited number of neurodegenerative lesions in the early phase of the disease, and only produces cognitive deficits during its later stages [38]. Patients with Parkinson’s disease exhibit unique motor symptoms that include tremor, rigidity, akinesia, bradykinesia, and postural instability [39, 40]. These symptoms are commonly associated with a significant degree of neuronal death in the brain stem and, particularly, with the loss of dopaminergic cells in the substantia nigra pars compacta (SNc) of the midbrain [39, 41, 42]. This type of cell damage decreases dopamine levels in the striatum and is the first symptom of Parkinson’s disease [39, 41]. Although the specific cause of Parkinson’s disease remains unknown, it has been reported that genetic mutations, neurotoxicity, and vascular dysfunction initiate neuronal death [43–49]. Additionally, mitochondrial dysfunction due to these factors has been suggested to play a key role in the pathogenesis of Parkinson’s disease [50, 51]. These types of dysfunction lead to neuronal damage and death and may occur concomitantly with apoptotic mechanisms similar to those associated with Alzheimer ‘s disease; each of these processes may contribute to the symptoms of Parkinson’s disease.
The primary clinical treatment for patients with Parkinson’s disease is the administration of a drug that enhances dopamine levels by supplying a precursor, L-dopa, which replaces dopamine that could not pass through the blood–brain barrier. Although this therapeutic method effectively improves motor symptoms during the initial stages of the disease, its efficacy decreases with long-term use and can cause side effects such as dyskinesia [39, 40]. During this phase, high-frequency brain stimulation can be performed to correct abnormal function within the basal ganglia that is caused by the loss of dopamine [52]. However, few studies have investigated the neuroprotective effects of these pharmacological therapies and/or surgical interventions [40, 53–55].
In attempts to overcome the limitations of therapies used to treat Parkinson’s disease, PBM has been investigated as an alternative treatment modality using various animal models (Table 2). Initial in vitro studies that employed parkinsonian insults to induce Parkinson’s disease found that PBM reduces apoptosis and oxidative stress while increasing ATP production in neurons [28, 30, 56]. It has also been reported that the application of PBM to human cells improves mitochondrial dysfunction and movement while reducing oxidative stress [57, 58]. The neuroprotective effects of PBM have also been observed in various animal models. In mice treated with methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) to induce Parkinson’s disease, PBM protects a significant number of dopaminergic neurons and improves motor performance [59–66]. In K369I transgenic mice, which exhibit motor signs of Parkinson’s disease, PBM decreases oxidative stress and increases the survival of SNc dopaminergic neurons [67–69]. Furthermore, in a MPTP monkey model, subjects treated with PBM exhibit a greater number of dopaminergic neurons than those not treated with PBM, and also show fewer clinical and behavioral symptoms [70]. These results suggest that PBM exerts neuroprotective effects in various models of Parkinson’s disease. However, further clinical evidence from systematic and large-scale clinical trials will be required to confirm its efficacy.
Table 2.
Photobiomodulation studies relevant to neuroprotection in Parkinson’s disease
| Source | Parameters | Models | Effect | References |
|---|---|---|---|---|
| LED | 670 nm, 50 mW/cm2, 4 J/cm2 twice a day for 2 days | In vitro (rat) | Increased cell survival, cytochrome oxidase activity and ATP content Decreased ROS and NO production | Liang et al. [28] and Ying et al. [30] |
| LED | 810 nm, 50 mW/cm2 for 40 s | In vitro (human) | Increased mitochondrial movement | Trimmer et al. [58] |
| Laser | 670 nm. 40 mW/cm2, 2 J/cm2 in four fractions | In vivo (mouse) | Protected dopaminergic cell loss in substantia against MPTP toxicity | Shaw et al. [66] |
| LED | 670 nm, 40 mW/cm2, 14.4 J/cm2 over 30 h | In vitro (human) | Improved mitochondrial function and Oxidative stress | Quirk et al. [57] |
| LED | 670 nm, 5.5 mW/cm2, 2 J/cm2 in four fractions | In vivo (mouse) | Improved locomotor activity, preserved tyrosine hydroxylase-positive cells | Moro et al. [62] |
| LED | 670 nm, 80 J/cm2 once a day, 5 days a week over 4 weeks | In vivo (mouse) | Reduced oxidative stress and overexpression of hyperphosphorylated tau, mitigated dopaminergic cell loss | Purushothuman et al. [69] |
| LED | 808 nm, 25 rnW/cni2 during 100 s, 2.5 J/cm2 | In vivo (mouse) | Improved Complex IV-dependent respiration and functional defects in mitochondria | Vos et al. [56] |
| Laser | 670 nm, 0.634 J (0.16 mW for 90 s twice a day), 0.634 J (333 nW continuous) 304 J (0.16 mW continuous) | In vivo (rat) | Improved cell survival and behavioral movement | Reinhart et al. [65] |
| Laser | 670 nm, 25 J over, 5 days, 35 J over 7 days | In vivo (monkey) | Increased cell survival and behavioral activity | Darlot et al. [70] |
| LED | 670 nm, 0.16 mW, 10 mW | In vivo (mouse, rat, monkey) | Protected dopaminergic cell loss and increased expression of GDNF | El Massri et al. [67] |
| LED | 670 nm, 50 mW/cm2, 4.5 J/cm2, 90 s once daily | In vivo (mouse) | Attenuated dopaminergic cell loss, regulation of genes associated with cell signaling | Ganeshan et al. [68] |
PBM for other types of neurodegeneration
Epilepsy is a serious neurological disorder that degrades one’s quality of life. Approximately 65 million people worldwide suffer from epilepsy and more than 100,000 new epileptic cases develop annually [71]. In epilepsy, chronic seizures are caused by abnormal paroxysmal electrical activity between neurons and eventually result in irreversible damage to brain cells and their surroundings. Temporal lobe epilepsy (TLE) is the most common partial epilepsy and is most often the result of head trauma, brain malformation, and infections [72]. Factors associated with TLE may initiate more seizures or status epilepticus (SE), which, in humans, is defined as a continuous seizure lasting for 30 min or more or at least two seizures that result in a lack of consciousness [73–75]. SE is considered to be a clinical emergency due to its severe morbidity and mortality [76]. Previous studies have shown that damage to inhibitory neurons in the hippocampus during SE alters the balance of excitatory and inhibitory neurons and results in hyperexcitability [77, 78]. This hyperexcitability mediates gliosis and causes mitochondrial dysfunction in neurons in the hippocampus and dentate gyrus. Mitochondrial dysfunction frequently occurs during epileptogenesis after seizures and these changes are closely related to neurodegenerative diseases [79].
A variety of anticonvulsants with various underlying mechanisms, including the inactivation of ion channels or the regulation of γ-aminobutyric acid (GABA) activity, have been used to treat epilepsy [80]. Unfortunately, the current anticonvulsants are ineffective for approximately 30% of epilepsy patients and can also induce deleterious side effects, such as systemic toxicity. The primary disadvantage of anticonvulsant therapies is that the brain may be more vulnerable to recurrent seizures due to drug withdrawal and the seizures may worsen over time [81, 82]. Thus, there is a need to overcome these limitations by developing novel therapies that can effectively prevent epileptogenesis.
PBM can be an effective treatment that overcomes the shortcomings associated with anticonvulsants. Several studies have investigated the effects of PBM using in vitro and in vivo models of epilepsy (Table 3). For example, in a rodent model of epilepsy, PBM can modulate the imbalance between neurotransmitters by regulating glutamate and GABA release in the cortex and hippocampus [83, 84]. Additionally, an in vitro study that employed an SE-inducing drug demonstrated that PBM increases cell viability in neurons and improves mitochondrial dysfunction, which subsequently increases the production of ATP [85]. The neuroprotective effects of PBM against Alzheimer’s disease and Parkinson’s disease appear to be similar in that this novel technique ameliorates imbalances in neurotransmitter levels via the alleviation of mitochondrial dysfunction in neurons. Although there is currently insufficient evidence from various models of epilepsy to support the efficacy of PBM or to identify its underlying mechanisms, the present findings suggest that PBM may be a novel treatment for epilepsy in the future.
Table 3.
Photobiomodulation studies relevant to neuroprotection in epilepsy
| Source | Parameters | Models | Effect | References |
|---|---|---|---|---|
| Laser | 808 nrn arid 830 nm, 5.5 W/cm2, 3.1 W/cm2 and 2.8 W/cm2, 30 J/point, 11 J/point and 5 J/point | In vivo (rat) | Decreased aspartate, glutamate and taurine in cortex and decreased liippocampal GABA | Ahmed et al. [83] |
| Laser | 830 nm, 90 mW, 2.87 W/cm2 daily | In vivo (rat) | Decreased glutamic acid, glutamine. glycine, taurine and ALT activity in cortex. Decreased aspartate, AST, ALT activity in hippocampus | Radwan et al. [84] |
| LED | 810 nm, 25 mW/cm2, 3 J/cm2 | In vitro (mouse) | Increased cell survival, ATP production and MMP. decreased Ca2+ release, ROS and NO production | Huang et al. [85] |
Conclusions
Although the potential of PBM as a novel treatment for neurodegenerative diseases remains uncertain, a variety of studies have demonstrated the efficacy of PDM for epilepsy, Alzheimer’s disease, Parkinson’s disease and other neurodegenerative diseases. Thus, PBM may be an effective alternative therapy for these disorders in the future and, as a result, several points must be considered regarding its application. First, PBM should be administered during the early phases of disease development. Most studies assessing PBM for the treatment of neurodegenerative diseases have been conducted during the early phase of progression and shown that, like other therapies, PBM cannot rescue neurons already undergoing degeneration from apoptosis or return them to normal cell conditions. Taken together, these findings indicate that PBM should be used as a technique to inhibit neuronal degeneration and apoptosis. Second, one major advantage of PBM is the relative lack of side effects, which suggests that it may be used as an adjunctive therapy with current effective treatments. For example, pharmacological side effects can be reduced by lowering the concentration of the drug and the drug effects can be maximized by the application of PBM. Third, it is important to consider how to apply PBM to the appropriate brain lesion or region using a helmet with LED or by surgically implanting fiber optics. The current state of research and development for the clinical application of PBM therapy remains insufficient. However, the therapeutic possibilities and efficacy of PBM for the treatment of neurodegenerative diseases are evident and should warrant the attention of researchers.
Acknowledgements
The author thanks Prof. Jin-Chul Ahn and Dr. Min Young Lee for helpful comments on the manuscript.
Funding
This research was a part of the project titled ‘Development of marine material based near infrared fluorophore complex and diagnostic imaging instruments’, funded by the Ministry of Oceans and Fisheries, Korea (Grant Number 20170263), and also supported by the Ministry of Trade, Industry & Energy, Republic of Korea (Grant Numbers 20002777 and 20002831).
Compliance with ethical standards
Conflict of interest
The author declares no conflicts of interest.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hamblin MR. Shining light on the head: photobiomodulation for brain disorders. BBA Clin. 2016;6:113–124. doi: 10.1016/j.bbacli.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hennessy M, Hamblin MR. Photobiomodulation and the brain: a new paradigm. J Opt. 2017;19(1):013003. doi: 10.1088/2040-8986/19/1/013003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Naeser MA, Hamblin MR. Potential for transcranial laser or LED therapy to treat stroke, traumatic brain injury, and neurodegenerative disease. Photomed Laser Surg. 2011;29(7):443–446. doi: 10.1089/pho.2011.9908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Naeser MA, Hamblin MR. Traumatic brain injury: a major medical problem that could be treated using transcranial, red/near-infrared LED photobiomodulation. Photomed Laser Surg. 2015;33(9):443–446. doi: 10.1089/pho.2015.3986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Herrup K. The case for rejecting the amyloid cascade hypothesis. Nat Neurosci. 2015;18(6):794–799. doi: 10.1038/nn.4017. [DOI] [PubMed] [Google Scholar]
- 6.Nelson L, Tabet N. Slowing the progression of Alzheimer’s disease; what works? Ageing Res Rev. 2015;23(Pt B):193–209. doi: 10.1016/j.arr.2015.07.002. [DOI] [PubMed] [Google Scholar]
- 7.Goedert M. NEURODEGENERATION. Alzheimer’s and Parkinson’s diseases: the prion concept in relation to assembled Abeta, tau, and alpha-synuclein. Science. 2015;349(6248):1255555. doi: 10.1126/science.1255555. [DOI] [PubMed] [Google Scholar]
- 8.Braak H, Braak E. Staging of Alzheimer’s disease-related neurofibrillary changes. Neurobiol Aging. 1995;16(3):271–278. doi: 10.1016/0197-4580(95)00021-6. [DOI] [PubMed] [Google Scholar]
- 9.Goedert M, Spillantini MG. A century of Alzheimer’s disease. Science. 2006;314(5800):777–781. doi: 10.1126/science.1132814. [DOI] [PubMed] [Google Scholar]
- 10.Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297(5580):353–356. doi: 10.1126/science.1072994. [DOI] [PubMed] [Google Scholar]
- 11.Umeda T, Tomiyama T, Sakama N, Tanaka S, Lambert MP, Klein WL, et al. Intraneuronal amyloid beta oligomers cause cell death via endoplasmic reticulum stress, endosomal/lysosomal leakage, and mitochondrial dysfunction in vivo. J Neurosci Res. 2011;89(7):1031–1042. doi: 10.1002/jnr.22640. [DOI] [PubMed] [Google Scholar]
- 12.Gong CX, Iqbal K. Hyperphosphorylation of microtubule-associated protein tau: a promising therapeutic target for Alzheimer disease. Curr Med Chem. 2008;15(23):2321–2328. doi: 10.2174/092986708785909111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brettschneider J, Del Tredici K, Lee VM, Trojanowski JQ. Spreading of pathology in neurodegenerative diseases: a focus on human studies. Nat Rev Neurosci. 2015;16(2):109–120. doi: 10.1038/nrn3887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chaturvedi RK, Beal MF. Mitochondrial approaches for neuroprotection. Ann N Y Acad Sci. 2008;1147:395–412. doi: 10.1196/annals.1427.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coppede F, Migliore L. DNA damage in neurodegenerative diseases. Mutat Res. 2015;776:84–97. doi: 10.1016/j.mrfmmm.2014.11.010. [DOI] [PubMed] [Google Scholar]
- 16.Cullen KM, Kocsi Z, Stone J. Pericapillary haem-rich deposits: evidence for microhaemorrhages in aging human cerebral cortex. J Cereb Blood Flow Metab. 2005;25(12):1656–1667. doi: 10.1038/sj.jcbfm.9600155. [DOI] [PubMed] [Google Scholar]
- 17.Cullen KM, Kocsi Z, Stone J. Microvascular pathology in the aging human brain: evidence that senile plaques are sites of microhaemorrhages. Neurobiol Aging. 2006;27(12):1786–1796. doi: 10.1016/j.neurobiolaging.2005.10.016. [DOI] [PubMed] [Google Scholar]
- 18.de la Torre JC. Is Alzheimer’s disease a neurodegenerative or a vascular disorder? Data, dogma, and dialectics. Lancet Neurol. 2004;3(3):184–190. doi: 10.1016/S1474-4422(04)00683-0. [DOI] [PubMed] [Google Scholar]
- 19.Gonzalez-Lima F, Barksdale BR, Rojas JC. Mitochondrial respiration as a target for neuroprotection and cognitive enhancement. Biochem Pharmacol. 2014;88(4):584–593. doi: 10.1016/j.bcp.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 20.Stone J. What initiates the formation of senile plaques? The origin of Alzheimer-like dementias in capillary haemorrhages. Med Hypotheses. 2008;71(3):347–359. doi: 10.1016/j.mehy.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 21.Stone J, Johnstone DM, Mitrofanis J, O’Rourke M. The mechanical cause of age-related dementia (Alzheimer’s disease): the brain is destroyed by the pulse. J Alzheimer’s Dis JAD. 2015;44(2):355–373. doi: 10.3233/JAD-141884. [DOI] [PubMed] [Google Scholar]
- 22.Swerdlow RH, Khan SM. A “mitochondrial cascade hypothesis” for sporadic Alzheimer’s disease. Med Hypotheses. 2004;63(1):8–20. doi: 10.1016/j.mehy.2003.12.045. [DOI] [PubMed] [Google Scholar]
- 23.Galluzzi L, Kepp O, Trojel-Hansen C, Kroemer G. Mitochondrial control of cellular life, stress, and death. Circ Res. 2012;111(9):1198–1207. doi: 10.1161/CIRCRESAHA.112.268946. [DOI] [PubMed] [Google Scholar]
- 24.Begum R, Powner MB, Hudson N, Hogg C, Jeffery G. Treatment with 670 nm light up regulates cytochrome C oxidase expression and reduces inflammation in an age-related macular degeneration model. PLoS ONE. 2013;8(2):e57828. doi: 10.1371/journal.pone.0057828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR. The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng. 2012;40(2):516–533. doi: 10.1007/s10439-011-0454-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Desmet KD, Paz DA, Corry JJ, Eells JT, Wong-Riley MT, Henry MM, et al. Clinical and experimental applications of NIR-LED photobiomodulation. Photomed Laser Surg. 2006;24(2):121–128. doi: 10.1089/pho.2006.24.121. [DOI] [PubMed] [Google Scholar]
- 27.Gkotsi D, Begum R, Salt T, Lascaratos G, Hogg C, Chau KY, et al. Recharging mitochondrial batteries in old eyes. Near infra-red increases ATP. Exp Eye Res. 2014;122:50–53. doi: 10.1016/j.exer.2014.02.023. [DOI] [PubMed] [Google Scholar]
- 28.Liang HL, Whelan HT, Eells JT, Wong-Riley MT. Near-infrared light via light-emitting diode treatment is therapeutic against rotenone- and 1-methyl-4-phenylpyridinium ion-induced neurotoxicity. Neuroscience. 2008;153(4):963–974. doi: 10.1016/j.neuroscience.2008.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rojas JC, Gonzalez-Lima F. Low-level light therapy of the eye and brain. Eye Brain. 2011;3:49–67. doi: 10.2147/EB.S21391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ying R, Liang HL, Whelan HT, Eells JT, Wong-Riley MT. Pretreatment with near-infrared light via light-emitting diode provides added benefit against rotenone- and MPP + -induced neurotoxicity. Brain Res. 2008;1243:167–173. doi: 10.1016/j.brainres.2008.09.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.De Taboada L, Yu J, El-Amouri S, Gattoni-Celli S, Richieri S, McCarthy T, et al. Transcranial laser therapy attenuates amyloid-beta peptide neuropathology in amyloid-beta protein precursor transgenic mice. J Alzheimer’s Dis JAD. 2011;23(3):521–535. doi: 10.3233/JAD-2010-100894. [DOI] [PubMed] [Google Scholar]
- 32.Grillo SL, Duggett NA, Ennaceur A, Chazot PL. Non-invasive infra-red therapy (1072 nm) reduces beta-amyloid protein levels in the brain of an Alzheimer’s disease mouse model, TASTPM. J Photochem Photobiol, B. 2013;123:13–22. doi: 10.1016/j.jphotobiol.2013.02.015. [DOI] [PubMed] [Google Scholar]
- 33.Michalikova S, Ennaceur A, van Rensburg R, Chazot PL. Emotional responses and memory performance of middle-aged CD1 mice in a 3D maze: effects of low infrared light. Neurobiol Learn Mem. 2008;89(4):480–488. doi: 10.1016/j.nlm.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 34.Purushothuman S, Johnstone DM, Nandasena C, Eersel J, Ittner LM, Mitrofanis J, et al. Near infrared light mitigates cerebellar pathology in transgenic mouse models of dementia. Neurosci Lett. 2015;591:155–159. doi: 10.1016/j.neulet.2015.02.037. [DOI] [PubMed] [Google Scholar]
- 35.Purushothuman S, Johnstone DM, Nandasena C, Mitrofanis J, Stone J. Photobiomodulation with near infrared light mitigates Alzheimer’s disease-related pathology in cerebral cortex—evidence from two transgenic mouse models. Alzheimers Res Ther. 2014;6(1):2. doi: 10.1186/alzrt232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.da Luz Eltchechem C, Salgado ASI, Zangaro RA, da Silva Pereira MC, Kerppers II, da Silva LA, et al. Transcranial LED therapy on amyloid-beta toxin 25–35 in the hippocampal region of rats. Lasers Med Sci. 2017;32(4):749–756. doi: 10.1007/s10103-017-2156-3. [DOI] [PubMed] [Google Scholar]
- 37.Sommer AP, Bieschke J, Friedrich RP, Zhu D, Wanker EE, Fecht HJ, et al. 670 nm laser light and EGCG complementarily reduce amyloid-beta aggregates in human neuroblastoma cells: basis for treatment of Alzheimer’s disease? Photomed Laser Surg. 2012;30(1):54–60. doi: 10.1089/pho.2011.3073. [DOI] [PubMed] [Google Scholar]
- 38.Cosgrove J, Alty JE, Jamieson S. Cognitive impairment in Parkinson’s disease. Postgrad Med J. 2015;91(1074):212–220. doi: 10.1136/postgradmedj-2015-133247. [DOI] [PubMed] [Google Scholar]
- 39.Bergman H, Deuschl G. Pathophysiology of Parkinson’s disease: from clinical neurology to basic neuroscience and back. Mov Disord. 2002;17(Suppl 3):S28–S40. doi: 10.1002/mds.10140. [DOI] [PubMed] [Google Scholar]
- 40.Poewe W, Mahlknecht P, Jankovic J. Emerging therapies for Parkinson’s disease. Curr Opin Neurol. 2012;25(4):448–459. doi: 10.1097/WCO.0b013e3283542fde. [DOI] [PubMed] [Google Scholar]
- 41.Blandini F, Nappi G, Tassorelli C, Martignoni E. Functional changes of the basal ganglia circuitry in Parkinson’s disease. Prog Neurobiol. 2000;62(1):63–88. doi: 10.1016/s0301-0082(99)00067-2. [DOI] [PubMed] [Google Scholar]
- 42.Rinne JO. Nigral degeneration in Parkinson’s disease. Mov Disord. 1993;8(Suppl 1):S31–S35. doi: 10.1002/mds.870080507. [DOI] [PubMed] [Google Scholar]
- 43.Blesa J, Phani S, Jackson-Lewis V, Przedborski S. Classic and new animal models of Parkinson’s disease. J Biomed Biotechnol. 2012;2012:845618. doi: 10.1155/2012/845618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carvey PM, Hendey B, Monahan AJ. The blood–brain barrier in neurodegenerative disease: a rhetorical perspective. J Neurochem. 2009;111(2):291–314. doi: 10.1111/j.1471-4159.2009.06319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Corti O, Brice A. Mitochondrial quality control turns out to be the principal suspect in parkin and PINK1-related autosomal recessive Parkinson’s disease. Curr Opin Neurobiol. 2013;23(1):100–108. doi: 10.1016/j.conb.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 46.Farkas E, De Jong GI, de Vos RA, Jansen Steur EN, Luiten PG. Pathological features of cerebral cortical capillaries are doubled in Alzheimer’s disease and Parkinson’s disease. Acta Neuropathol. 2000;100(4):395–402. doi: 10.1007/s004010000195. [DOI] [PubMed] [Google Scholar]
- 47.Gitler AD, Chesi A, Geddie ML, Strathearn KE, Hamamichi S, Hill KJ, et al. Alpha-synuclein is part of a diverse and highly conserved interaction network that includes PARK9 and manganese toxicity. Nat Genet. 2009;41(3):308–315. doi: 10.1038/ng.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Grammas P, Martinez J, Miller B. Cerebral microvascular endothelium and the pathogenesis of neurodegenerative diseases. Expert Rev Mol Med. 2011;13:e19. doi: 10.1017/S1462399411001918. [DOI] [PubMed] [Google Scholar]
- 49.Kortekaas R, Leenders KL, van Oostrom JC, Vaalburg W, Bart J, Willemsen AT, et al. Blood–brain barrier dysfunction in parkinsonian midbrain in vivo. Ann Neurol. 2005;57(2):176–179. doi: 10.1002/ana.20369. [DOI] [PubMed] [Google Scholar]
- 50.Exner N, Lutz AK, Haass C, Winklhofer KF. Mitochondrial dysfunction in Parkinson’s disease: molecular mechanisms and pathophysiological consequences. EMBO J. 2012;31(14):3038–3062. doi: 10.1038/emboj.2012.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fukae J, Mizuno Y, Hattori N. Mitochondrial dysfunction in Parkinson’s disease. Mitochondrion. 2007;7(1–2):58–62. doi: 10.1016/j.mito.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 52.Benabid AL, Chabardes S, Mitrofanis J, Pollak P. Deep brain stimulation of the subthalamic nucleus for the treatment of Parkinson’s disease. Lancet Neurol. 2009;8(1):67–81. doi: 10.1016/S1474-4422(08)70291-6. [DOI] [PubMed] [Google Scholar]
- 53.Bezard E, Yue Z, Kirik D, Spillantini MG. Animal models of Parkinson’s disease: limits and relevance to neuroprotection studies. Mov Disord. 2013;28(1):61–70. doi: 10.1002/mds.25108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Olanow CW, Kieburtz K, Schapira AH. Why have we failed to achieve neuroprotection in Parkinson’s disease? Ann Neurol. 2008;64(Suppl 2):S101–S110. doi: 10.1002/ana.21461. [DOI] [PubMed] [Google Scholar]
- 55.Schapira AH, Olanow CW, Greenamyre JT, Bezard E. Slowing of neurodegeneration in Parkinson’s disease and Huntington’s disease: future therapeutic perspectives. Lancet. 2014;384(9942):545–555. doi: 10.1016/S0140-6736(14)61010-2. [DOI] [PubMed] [Google Scholar]
- 56.Vos M, Lovisa B, Geens A, Morais VA, Wagnieres G, van den Bergh H, et al. Near-infrared 808 nm light boosts complex IV-dependent respiration and rescues a Parkinson-related pink1 model. PLoS ONE. 2013;8(11):e78562. doi: 10.1371/journal.pone.0078562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Quirk BJ, Desmet KD, Henry M, Buchmann E, Wong-Riley M, Eells JT, et al. Therapeutic effect of near infrared (NIR) light on Parkinson’s disease models. Front Biosci. 2012;4:818–823. doi: 10.2741/E421. [DOI] [PubMed] [Google Scholar]
- 58.Trimmer PA, Schwartz KM, Borland MK, De Taboada L, Streeter J, Oron U. Reduced axonal transport in Parkinson’s disease cybrid neurites is restored by light therapy. Mol Neurodegener. 2009;4:26. doi: 10.1186/1750-1326-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.El Massri N, Johnstone DM, Peoples CL, Moro C, Reinhart F, Torres N, et al. The effect of different doses of near infrared light on dopaminergic cell survival and gliosis in MPTP-treated mice. Int J Neurosci. 2016;126(1):76–87. doi: 10.3109/00207454.2014.994063. [DOI] [PubMed] [Google Scholar]
- 60.Johnstone DM, el Massri N, Moro C, Spana S, Wang XS, Torres N, et al. Indirect application of near infrared light induces neuroprotection in a mouse model of parkinsonism—an abscopal neuroprotective effect. Neuroscience. 2014;274:93–101. doi: 10.1016/j.neuroscience.2014.05.023. [DOI] [PubMed] [Google Scholar]
- 61.Moro C, Massri NE, Torres N, Ratel D, De Jaeger X, Chabrol C, et al. Photobiomodulation inside the brain: a novel method of applying near-infrared light intracranially and its impact on dopaminergic cell survival in MPTP-treated mice. J Neurosurg. 2014;120(3):670–683. doi: 10.3171/2013.9.JNS13423. [DOI] [PubMed] [Google Scholar]
- 62.Moro C, Torres N, El Massri N, Ratel D, Johnstone DM, Stone J, et al. Photobiomodulation preserves behaviour and midbrain dopaminergic cells from MPTP toxicity: evidence from two mouse strains. BMC Neurosci. 2013;14:40. doi: 10.1186/1471-2202-14-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Peoples C, Spana S, Ashkan K, Benabid AL, Stone J, Baker GE, et al. Photobiomodulation enhances nigral dopaminergic cell survival in a chronic MPTP mouse model of Parkinson’s disease. Parkinsonism Relat Disord. 2012;18(5):469–476. doi: 10.1016/j.parkreldis.2012.01.005. [DOI] [PubMed] [Google Scholar]
- 64.Reinhart F, Massri NE, Chabrol C, Cretallaz C, Johnstone DM, Torres N, et al. Intracranial application of near-infrared light in a hemi-parkinsonian rat model: the impact on behavior and cell survival. J Neurosurg. 2016;124(6):1829–1841. doi: 10.3171/2015.5.JNS15735. [DOI] [PubMed] [Google Scholar]
- 65.Reinhart F, Massri NE, Darlot F, Torres N, Johnstone DM, Chabrol C, et al. 810 nm near-infrared light offers neuroprotection and improves locomotor activity in MPTP-treated mice. Neurosci Res. 2015;92:86–90. doi: 10.1016/j.neures.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 66.Shaw VE, Keay KA, Ashkan K, Benabid AL, Mitrofanis J. Dopaminergic cells in the periaqueductal grey matter of MPTP-treated monkeys and mice; patterns of survival and effect of deep brain stimulation and lesion of the subthalamic nucleus. Parkinsonism Relat Disord. 2010;16(5):338–344. doi: 10.1016/j.parkreldis.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 67.El Massri N, Lemgruber AP, Rowe IJ, Moro C, Torres N, Reinhart F, et al. Photobiomodulation-induced changes in a monkey model of Parkinson’s disease: changes in tyrosine hydroxylase cells and GDNF expression in the striatum. Exp Brain Res. 2017;235(6):1861–1874. doi: 10.1007/s00221-017-4937-0. [DOI] [PubMed] [Google Scholar]
- 68.Ganeshan V, Skladnev NV, Kim JY, Mitrofanis J, Stone J, Johnstone DM. Pre-conditioning with remote photobiomodulation modulates the brain transcriptome and protects against MPTP insult in mice. Neuroscience. 2019;400:85–97. doi: 10.1016/j.neuroscience.2018.12.050. [DOI] [PubMed] [Google Scholar]
- 69.Purushothuman S, Nandasena C, Johnstone DM, Stone J, Mitrofanis J. The impact of near-infrared light on dopaminergic cell survival in a transgenic mouse model of parkinsonism. Brain Res. 2013;1535:61–70. doi: 10.1016/j.brainres.2013.08.047. [DOI] [PubMed] [Google Scholar]
- 70.Darlot F, Moro C, El Massri N, Chabrol C, Johnstone DM, Reinhart F, et al. Near-infrared light is neuroprotective in a monkey model of Parkinson disease. Ann Neurol. 2016;79(1):59–75. doi: 10.1002/ana.24542. [DOI] [PubMed] [Google Scholar]
- 71.Kwan P, Schachter SC, Brodie MJ. Drug-resistant epilepsy. N Engl J Med. 2011;365(10):919–926. doi: 10.1056/NEJMra1004418. [DOI] [PubMed] [Google Scholar]
- 72.Wiebe S. Epidemiology of temporal lobe epilepsy. Can J Neurol Sci. 2000;27(Suppl 1):S6–S10. doi: 10.1017/s0317167100000561. [DOI] [PubMed] [Google Scholar]
- 73.ILAE Commission Report The epidemiology of the epilepsies: future directions. International League Against Epilepsy. Epilepsia. 1997;38(5):614–618. [PubMed] [Google Scholar]
- 74.Cherian A, Thomas SV. Status epilepticus. Ann Indian Acad Neurol. 2009;12(3):140–153. doi: 10.4103/0972-2327.56312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Knake S, Hamer HM, Rosenow F. Status epilepticus: a critical review. Epilepsy Behav E&B. 2009;15(1):10–14. doi: 10.1016/j.yebeh.2009.02.027. [DOI] [PubMed] [Google Scholar]
- 76.DeLorenzo RJ, Pellock JM, Towne AR, Boggs JG. Epidemiology of status epilepticus. J Clin Neurophysiol. 1995;12(4):316–325. [PubMed] [Google Scholar]
- 77.Olney JW. Inciting excitotoxic cytocide among central neurons. Adv Exp Med Biol. 1986;203:631–645. doi: 10.1007/978-1-4684-7971-3_48. [DOI] [PubMed] [Google Scholar]
- 78.Sloviter RS, Dempster DW. “Epileptic” brain damage is replicated qualitatively in the rat hippocampus by central injection of glutamate or aspartate but not by GABA or acetylcholine. Brain Res Bull. 1985;15(1):39–60. doi: 10.1016/0361-9230(85)90059-0. [DOI] [PubMed] [Google Scholar]
- 79.Patel MN. Oxidative stress, mitochondrial dysfunction, and epilepsy. Free Radic Res. 2002;36(11):1139–1146. doi: 10.1080/1071576021000016391. [DOI] [PubMed] [Google Scholar]
- 80.Bialer M, White HS. Key factors in the discovery and development of new antiepileptic drugs. Nat Rev Drug Discov. 2010;9(1):68–82. doi: 10.1038/nrd2997. [DOI] [PubMed] [Google Scholar]
- 81.Berg AT, Shinnar S. Relapse following discontinuation of antiepileptic drugs: a meta-analysis. Neurology. 1994;44(4):601–608. doi: 10.1212/wnl.44.4.601. [DOI] [PubMed] [Google Scholar]
- 82.Schmidt D, Loscher W. Uncontrolled epilepsy following discontinuation of antiepileptic drugs in seizure-free patients: a review of current clinical experience. Acta Neurol Scand. 2005;111(5):291–300. doi: 10.1111/j.1600-0404.2005.00408.x. [DOI] [PubMed] [Google Scholar]
- 83.Ahmed NA, Radwan NM, Ibrahim KM, Khedr ME, El Aziz MA, Khadrawy YA. Effect of three different intensities of infrared laser energy on the levels of amino acid neurotransmitters in the cortex and hippocampus of rat brain. Photomed Laser Surg. 2008;26(5):479–488. doi: 10.1089/pho.2007.2190. [DOI] [PubMed] [Google Scholar]
- 84.Radwan NM, El Hay Ahmed NA, Ibrahim KM, Khedr ME, Aziz MA, Khadrawy YA. Effect of infrared laser irradiation on amino acid neurotransmitters in an epileptic animal model induced by pilocarpine. Photomed Laser Surg. 2009;27(3):401–409. doi: 10.1089/pho.2008.2275. [DOI] [PubMed] [Google Scholar]
- 85.Huang YY, Nagata K, Tedford CE, Hamblin MR. Low-level laser therapy (810 nm) protects primary cortical neurons against excitotoxicity in vitro. J Biophotonics. 2014;7(8):656–664. doi: 10.1002/jbio.201300125. [DOI] [PMC free article] [PubMed] [Google Scholar]