Abstract
Background
The rapid development in big data analytics and the data-rich environment of intensive care units together provide unprecedented opportunities for medical breakthroughs in the field of critical care. We developed and validated a machine learning-based model, the Pediatric Risk of Mortality Prediction Tool (PROMPT), for real-time prediction of all-cause mortality in pediatric intensive care units.
Methods
Utilizing two separate retrospective observational cohorts, we conducted model development and validation using a machine learning algorithm with a convolutional neural network. The development cohort comprised 1445 pediatric patients with 1977 medical encounters admitted to intensive care units from January 2011 to December 2017 at Severance Hospital (Seoul, Korea). The validation cohort included 278 patients with 364 medical encounters admitted to the pediatric intensive care unit from January 2016 to November 2017 at Samsung Medical Center.
Results
Using seven vital signs, along with patient age and body weight on intensive care unit admission, PROMPT achieved an area under the receiver operating characteristic curve in the range of 0.89–0.97 for mortality prediction 6 to 60 h prior to death. Our results demonstrated that PROMPT provided high sensitivity with specificity and outperformed the conventional severity scoring system, the Pediatric Index of Mortality, in predictive ability. Model performance was indistinguishable between the development and validation cohorts.
Conclusions
PROMPT is a deep model-based, data-driven early warning score tool that can predict mortality in critically ill children and may be useful for the timely identification of deteriorating patients.
Electronic supplementary material
The online version of this article (10.1186/s13054-019-2561-z) contains supplementary material, which is available to authorized users.
Keywords: Machine learning; Mortality; Intensive care units, pediatric; Prognosis; Risk assessment
Background
Hospitalized children, particularly those in high-acuity environments such as the pediatric intensive care unit (PICU), are inevitably susceptible to clinical deterioration. Several outcome prediction models such as the Pediatric Index of Mortality (PIM) and the Pediatric Risk of Mortality (PRISM) are widely used in PICUs [1, 2]. However, these acuity scores are based on “snapshot” values gathered during the early period following PICU admission. These static scores fail to adapt with the patient’s clinical progression and offer little assistance for the management of individual patients [3, 4].
Previous studies demonstrating that acute deterioration in patients is often preceded by subtle changes in physiological parameters [5, 6] led to the development of the Early Warning Score (EWS) [7]. Accurate and generalizable risk stratification tools may contribute to the timely identification of high-risk patients and facilitate earlier clinical intervention leading to improved patient outcomes [8]. Since its introduction, the EWS has undergone many alterations, and its modified forms are widely used in general hospitals today [9, 10]. However, the primary target population is usually confined to relatively healthy patients in general wards [9, 11] or emergency department settings [12] and may not be applicable to intensive care settings [13].
Current literature frequently calls for the development of diverse intensive care warning scores [14–16]. The rapid development in machine learning, coupled with the richness of data from extensive patient monitoring in the intensive care unit (ICU), provides unprecedented opportunities for the development of new prediction scores in the field of critical care [17–19]. Challenges in the analytics of PICU data, including pathologic diversity and complexity [20] and the wide range of age and developmental stages, are anticipated to be addressed by the implementation of innovative predictive modeling [18, 21].
Curtis et al. developed a cardiac arrest prediction model by time series trend analysis using a support vector machine algorithm that achieved excellent performance [22]. In addition, Zhengping et al. adopted Gradient Boosting Trees to learn an interpretable model, which demonstrated strong performance for the prediction of mortality and ventilator-free days in the PICU [23]. Despite their successful application of data-driven analytics, the above studies were limited by the lack of external validation. To allow practical application in a real-world setting, the preliminary results would require further refinement regarding data elements, extraction, processing, and operation with acceptable false alarms.
In this paper, we describe the development and evaluation of a new tool, the Pediatric Risk of Mortality Prediction Tool (PROMPT), for real-time mortality prediction in PICUs. We also assessed PROMPT’s suitability for practical application in the clinical care of critically ill children.
Methods
Study population and data sources
We used data from the electronic health records (EHRs) of all patients under 19 years old admitted to the medical ICU at Severance Hospital (Seoul, Korea) between January 2011 and December 2017. The primary cohort contained 1445 patients with 1977 ICU admissions. For external validation, we used a separate dataset provided by Samsung Medical Center (Seoul, Korea) containing data on 278 patients with 364 PICU admissions from January 2016 to November 2017. Details on these datasets are presented in Additional file 1: Table S1. All data were anonymized, and a waiver was obtained from the Institutional Review Board of each hospital (#4-2017-0060 and #2019-09015-001, respectively).
Feature selection and data processing
The extracted data contained sets of static features, such as demographic and clinical information, and temporal features such as time-stamped vital signs. To construct a mortality prediction tool, we adopted two descriptive features—age and weight—and seven vital signs: systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MBP), heart rate (HR), respiratory rate (RR), peripheral capillary oxygen saturation (SpO2), and body temperature (BT). We selected vital signs as objective predictor variables because they are routinely and frequently collected from all patients regardless of clinical situation and the values are rarely affected by the examiner. Most vital signs of ICU patients are automatically measured by monitoring devices at minimum once an hour, and the values are recorded on the EHR.
The following cleaning process ensured that the EHR data was ready for analysis and did not contain errors. Non-numeric values were removed. In addition, a set of defined ranges of physiologically possible values for selected variables were used to eliminate outliers (Additional file 1: Table S2). Carry-forward/carry-backward methods were employed for imputations. In case of multiple measurements within an hour, the most extreme values were used. Policy-based preprocessing was automated and resulted in an average coverage of 96.1% of all data with an accuracy of 97.5% compared to manual corrections. Finally, for modeling, each variable was standardized to fit an isotropic Gaussian distribution.
Machine learning
The primary outcome was all-cause mortality in the ICU. For this binary outcome, we extracted positive instances from all cases who died in ICU and negative instances from all cases who survived (Additional file 1: Figure S1). The 24-h window of vital signs up to 6 to 60 h prior to death was extracted as a positive instance, and 24-h window of vital signs randomly chosen from during ICU stay of the survivor was assigned as a negative instance. For simplicity, only a single instance was selected from each encounter, and both sampled positive and negative instances were designated to be similar in their mean lengths to avoid possible biases (Additional file 1: Table S3).
Model development was carried out using convolutional neural networks (CNNs) [24], a class of deep, feed-forward artificial neural networks consisting of alternating convolutional and subsampling layers that replicate the complexities of the animal visual cortex. The convolution operation involves combining input data with a convolution kernel to form transformed data. The filters in the convolutional layers are modified based on learned parameters to incorporate the most useful information for a specific task. This method adjusts automatically to determine the best feature based on the task and has achieved great success in feature representation learning in images [25]. Recent reports have also demonstrated its utility in predicting sepsis in adult [26] and pediatric populations [27] and cardiac arrhythmias [28]. A detailed architecture of our CNN, which consisted of two layers of one-dimensional convolutional operations followed by max pooling is presented in the supplementary materials for reproducibility (Additional file 1: Table S4). A fivefold cross-validation with five repetitions on the development cohort was adopted to validate PROMPT’s performance, and external validation was followed to assess its generalizability.
Statistical analysis
We compared the performance of PROMPT with other standard machine learning algorithms, such as Gradient Boosting Decision Trees (GBDT) [29], Long Short-Term Memory (LSTM) [30], and the Pediatric Index of Mortality 3 (PIM 3), which is currently widely used in PICUs [1]. Model performance was assessed based on discrimination using the area under the receiver operating characteristic curve (AUROC), one of the most commonly used metrics, and the area under the precision-recall curve (AUPRC), which, because the outcome of interest was mortality, was calculated considering a skewed large domain of true negatives [31]. Sensitivity, specificity, positive predicted value (PPV), negative predicted value (NPV), and accuracy were also evaluated for all prediction tools assessed in this study.
Results
Dataset statistics
As shown from the descriptive statistics for each cohort (Additional file 1: Table S1), the development cohort consisted of 1977 patient encounters, in which 303 cases of mortality (15.3%) were identified. The validation cohort showed 9.6% mortality. Significant differences were noted between the two datasets in terms of age, PIM 3, mortality, length of ICU stay, and inclusion period.
Mortality prediction performance
The performance metrics of PROMPT on mortality prediction compared to other standard machine learning algorithms and PIM 3 are summarized in Table 1. The best performance was achieved for predicting mortality 6 h prior to death (AUROC 0.965, AUPRC 0.831) with a slight decrease, although still high-performance, as the time window increased to 60 h prior to death. In detecting mortality 60 h in advance, PROMPT (AUROC 0.887, AUPRC 0.565) consistently outperformed GBDT (AUROC 0.831, AUPRC 0.419), LSTM (AUROC 0.814, AUPRC 0.429), and PIM 3 (AUROC 0.785, AUPRC 0.298) in the development cohort (Table 1), also shown in the micro-averaged performance comparisons (Additional file 1: Figure S2). Similar results were found on external validation (Table 1).
Table 1.
Summary of model mortality detection performance
| Development cohort | Validation cohort | |||||||
|---|---|---|---|---|---|---|---|---|
| Lead time window | AUROC | 95% CI | AUPRC | 95% CI | AUROC | 95% CI | AUPRC | 95% CI |
| PROMPT | ||||||||
| 6 h | 0.965 | ± 0.006 | 0.831 | ± 0.018 | 0.922 | ± 0.004 | 0.716 | ± 0.016 |
| 12 h | 0.948 | ± 0.009 | 0.745 | ± 0.029 | 0.945 | ± 0.004 | 0.701 | ± 0.023 |
| 24 h | 0.933 | ± 0.009 | 0.733 | ± 0.027 | 0.946 | ± 0.005 | 0.605 | ± 0.024 |
| 48 h | 0.899 | ± 0.013 | 0.570 | ± 0.041 | 0.849 | ± 0.007 | 0.360 | ± 0.023 |
| 60 h | 0.887 | ± 0.018 | 0.565 | ± 0.052 | 0.881 | ± 0.011 | 0.445 | ± 0.031 |
| GBDT | ||||||||
| 6 h | 0.944 | ± 0.008 | 0.767 | ± 0.022 | 0.877 | ± 0.005 | 0.499 | ± 0.032 |
| 12 h | 0.927 | ± 0.008 | 0.684 | ± 0.028 | 0.915 | ± 0.005 | 0.605 | ± 0.022 |
| 24 h | 0.908 | ± 0.014 | 0.612 | ± 0.032 | 0.897 | ± 0.007 | 0.442 | ± 0.021 |
| 48 h | 0.853 | ± 0.014 | 0.452 | ± 0.031 | 0.805 | ± 0.009 | 0.342 | ± 0.025 |
| 60 h | 0.831 | ± 0.022 | 0.419 | ± 0.051 | 0.790 | ± 0.012 | 0.403 | ± 0.035 |
| LSTM | ||||||||
| 6 h | 0.945 | ± 0.010 | 0.808 | ± 0.019 | 0.875 | ± 0.006 | 0.547 | ± 0.039 |
| 12 h | 0.915 | ± 0.016 | 0.703 | ± 0.031 | 0.870 | ± 0.012 | 0.520 | ± 0.034 |
| 24 h | 0.889 | ± 0.013 | 0.644 | ± 0.032 | 0.837 | ± 0.012 | 0.348 | ± 0.032 |
| 48 h | 0.844 | ± 0.014 | 0.530 | ± 0.029 | 0.770 | ± 0.013 | 0.348 | ± 0.027 |
| 60 h | 0.814 | ± 0.025 | 0.429 | ± 0.050 | 0.759 | ± 0.019 | 0.353 | ± 0.034 |
| PIM 3 | ||||||||
| Total | 0.767 | – | 0.509 | – | 0.881 | – | 0.500 | – |
| Subset 1* | 0.787 | – | 0.315 | – | 0.876 | – | 0.462 | – |
| Subset 2** | 0.785 | – | 0.298 | – | 0.876 | – | 0.462 | – |
AUROC area under the receiver operating characteristic curve, CI confidence interval, AUPRC area under the precision-recall curve, PROMPT pediatric risk of mortality prediction tool, GBDT Gradient Boosting Decision Trees, LSTM Long Short-Term Memory, PIM 3 Pediatric Index of Mortality 3
*Subset of the cohort with data of at least 48 h
**Subset of the cohort with data of at least 60 h
Additional paired comparison metrics at a sensitivity of 0.8 for specificity, PPV, NPV, and accuracy for each model are presented in Table 2. Within the development cohort, PROMPT identified 80% of patients who were to die in 24 h, yielded 7% false alarms (specificity = 0.931), and was the most consistently accurate of all metrics. Comparison of sensitivity according to the number of false alarms showed that PROMPT provided fewer false alarms than existing models, including PIM 3, in both cohorts (Additional file 1: Figure S3).
Table 2.
Comparison of model’s accuracy for mortality prediction
| Development cohort | Validation cohort | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lead time window | Sensitivity | Specificity | PPV | NPV | Accuracy | Sensitivity | Specificity | PPV | NPV | Accuracy |
| PROMPT | ||||||||||
| 6 h | 0.846 | 0.963 | 0.663 | 0.986 | 0.953 | 0.800 | 0.850 | 0.288 | 0.982 | 0.846 |
| 12 h | 0.800 | 0.946 | 0.555 | 0.983 | 0.935 | 0.800 | 0.890 | 0.336 | 0.985 | 0.884 |
| 24 h | 0.800 | 0.931 | 0.454 | 0.985 | 0.922 | 0.849 | 0.887 | 0.334 | 0.989 | 0.884 |
| 48 h | 0.800 | 0.834 | 0.224 | 0.986 | 0.832 | 0.800 | 0.752 | 0.177 | 0.983 | 0.755 |
| 60 h | 0.800 | 0.882 | 0.268 | 0.988 | 0.878 | 0.800 | 0.772 | 0.190 | 0.983 | 0.773 |
| GBDT | ||||||||||
| 6 h | 0.800 | 0.933 | 0.509 | 0.982 | 0.922 | 0.800 | 0.805 | 0.238 | 0.981 | 0.805 |
| 12 h | 0.801 | 0.898 | 0.398 | 0.982 | 0.891 | 0.800 | 0.854 | 0.276 | 0.984 | 0.850 |
| 24 h | 0.800 | 0.854 | 0.283 | 0.983 | 0.850 | 0.800 | 0.818 | 0.227 | 0.984 | 0.817 |
| 48 h | 0.800 | 0.769 | 0.172 | 0.985 | 0.771 | 0.800 | 0.629 | 0.126 | 0.979 | 0.640 |
| 60 h | 0.800 | 0.693 | 0.123 | 0.985 | 0.698 | 0.800 | 0.551 | 0.107 | 0.976 | 0.567 |
| LSTM | ||||||||||
| 6 h | 0.800 | 0.951 | 0.588 | 0.982 | 0.939 | 0.800 | 0.770 | 0.209 | 0.981 | 0.772 |
| 12 h | 0.800 | 0.888 | 0.374 | 0.981 | 0.881 | 0.800 | 0.782 | 0.204 | 0.982 | 0.783 |
| 24 h | 0.800 | 0.828 | 0.251 | 0.983 | 0.826 | 0.800 | 0.740 | 0.170 | 0.982 | 0.743 |
| 48 h | 0.800 | 0.729 | 0.150 | 0.984 | 0.733 | 0.800 | 0.537 | 0.104 | 0.976 | 0.554 |
| 60 h | 0.800 | 0.626 | 0.103 | 0.983 | 0.635 | 0.800 | 0.505 | 0.098 | 0.974 | 0.524 |
| PIM 3 | ||||||||||
| Total | 0.800 | 0.617 | 0.392 | 0.909 | 0.661 | 0.800 | 0.799 | 0.298 | 0.974 | 0.799 |
| Subset 1* | 0.806 | 0.643 | 0.218 | 0.964 | 0.661 | 0.818 | 0.754 | 0.182 | 0.984 | 0.758 |
| Subset 2** | 0.800 | 0.643 | 0.200 | 0.966 | 0.659 | 0.818 | 0.754 | 0.182 | 0.984 | 0.758 |
PPV positive predictive value, NPV negative predictive value, PROMPT pediatric risk of mortality prediction tool, GBDT Gradient Boosting Decision Trees, LSTM Long Short-Term Memory, PIM 3 Pediatric Index of Mortality 3
*Subset of the cohort with data of at least 48 h
**Subset of the cohort with data of at least 60 h
Visualization of prediction trajectory
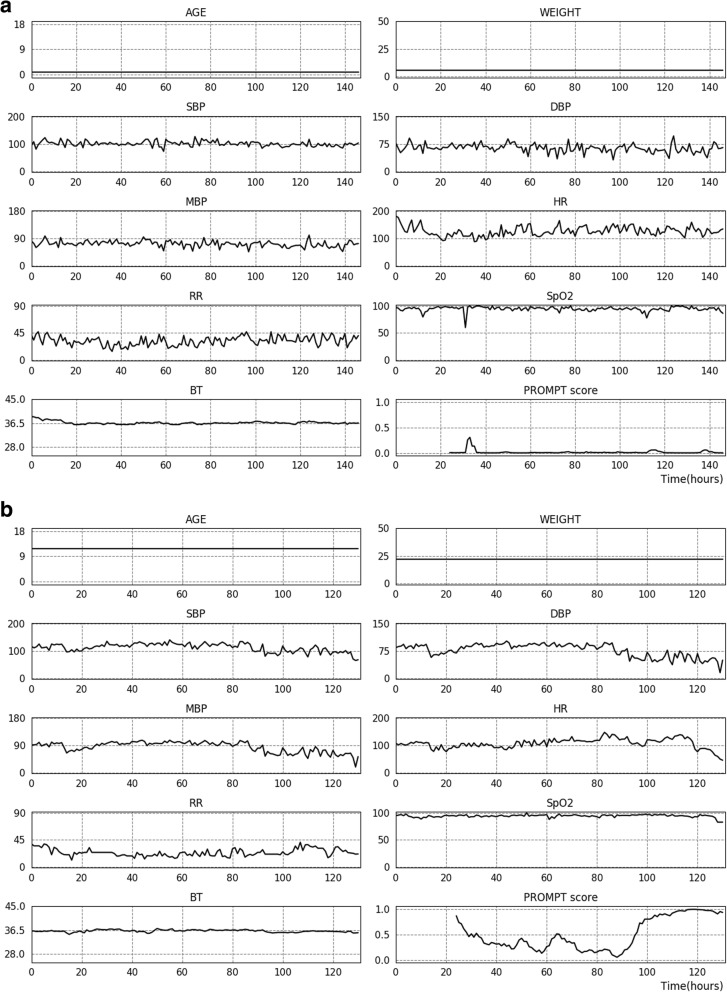
PROMPT produced an averaged mortality risk score over multiple prediction models trained from development cohorts to predict mortality in the preceding 6, 12, 24, 48, and 60 h (examples are presented in Fig. 1). Where t is the current time point, the input data composed of two descriptive features and vital signs in a range of [t − 24, t] transformed to an averaged risk score. The same procedure was repeated at the t + 1 time points to generate prediction trajectory. A sliding window (0 to 24 h) moved hour-by-hour through the time series to generate predicted mortality for each time point during the ICU stay.
Fig. 1.
Prediction trajectory using PROMPT. Serial trends of recorded vital signs during ICU stay and hourly calculated predicted mortality rate using PROMPT shown for patients from the validation cohort who survived (a) and died (b), respectively. Predicted mortality was averaged over multiple prediction models trained from development cohort using the dataset to predict mortality in the preceding k hours (where k = 6, 12, 24, 48, and 60). SBP, systolic blood pressure; DBP, diastolic blood pressure; MBP, mean blood pressure; HR, heart rate; RR, respiratory rate; SpO2, peripheral capillary oxygen saturation; BT, body temperature; ICU, intensive care unit
Designation of time and feature contributions
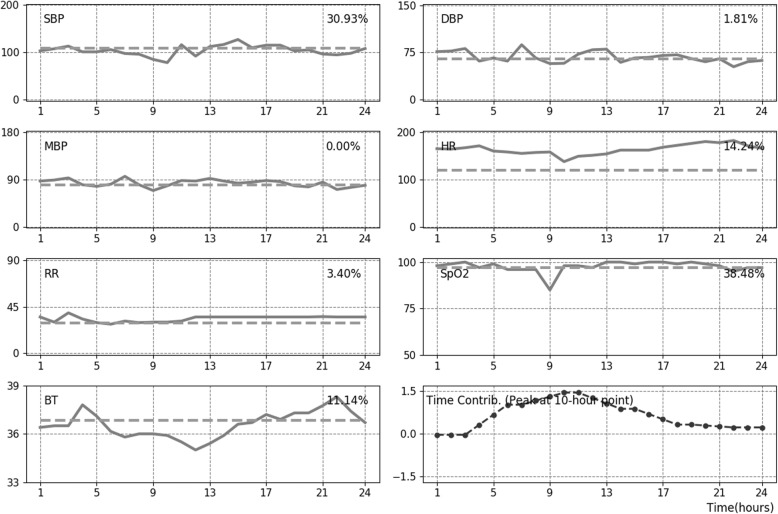
An interpretation module that quantitatively measured the contribution of time series features for mortality was developed. Every time-stamped vital sign was substituted for an age-dependent mean value and, following changes in predicted mortality, produced quantitative contributions of each feature (%). In addition, algebraic manipulation demonstrated that the contribution of each time point was captured by the importance of six blocks in making a prediction. This is because a temporal relationship is lost due to pooling operations. Accordingly, 24 h data was grouped by six blocks for which the contribution to the prediction was computed. An average filter was then applied for smoothing the signal. Figure 2 depicts illustrative examples of a deceased case showing the measured contribution of each time point and those of features at the most critical time point, as well as the linear trend of vital signs for 24 h.
Fig. 2.
Depiction of time and feature contributions for mortality using PROMPT. Measured contribution (%) for mortality at the critical time point and serial trend of vital signs over 24 h are plotted on each panel. The last sub-figure presents the time contribution. The height of the graph represents the level of importance, and the positive/negative conversion distinguishes the time point contributed to make positive or negative predictions for mortality. In the presented case, the critical time point (i.e., a peak of time contribution) was about 10 h, of which fluctuations in SpO2, blood pressure, and HR are shown to contribute to instability which can be associated with mortality. SBP, systolic blood pressure; DBP, diastolic blood pressure; MBP, mean blood pressure; HR, heart rate; RR, respiratory rate; SpO2, peripheral capillary oxygen saturation; BT, body temperature
Interpretability of PROMPT
Individual feature importance was plotted by computing a sensitivity heat map on a total of 363 test instances in the development cohort to measure the importance of individual input variables (Additional file 1: Figure S4). The sensitivity was defined as the derivative of the predicted mortality according to the input variables, and the relative importance of input variables was normalized to satisfy the sum-to-one constraint. RR showed the highest relative importance among all other features, followed by SBP and HR.
Individual Conditional Expectation plots are shown in Additional file 1: Figure S5. These six plots show the test instances in the development cohort. The predicted mortality probability was computed by creating variants of each input variable while keeping all other features as it is. For blood pressures, predicted mortality tends to increase when pressure values are too low or too high, and it declines as the feature value falls within the physiological range. A similar trend was observed in other vital signs, such as HR, RR, and BT. In SpO2, predicted mortality tends to decrease as the degree of saturation increases to 100%. However, several instances were identified with a high mortality probability despite a high SpO2, due to the correlation between the features.
Discussion
In this study, we developed and validated a targeted real-time early warning score, PROMPT, based on a CNN algorithm using a PICU dataset with routine vital signs. Utilizing a handful of variables, PROMPT achieved high performance with high sensitivity and specificity for predicting mortality in PICU patients. In predictive ability, it outperformed the conventional severity scoring system, PIM 3, as well as other models that use GBDT and LSTM.
Existing risk prediction tools in ICU use static physiological parameters from early in the course of critical illness (often within the first 24 h following admission), along with other components, such as age and diagnosis, to assess severity and risk of death for the purpose of predicting outcomes [32]. For pediatric populations, PIM and PRISM are the most representative [1, 2]. However, it is generally agreed that they are poor surrogates for risk stratification and should not be used as the basis for individual treatment decisions [4, 33, 34]. Generic severity scores were originally developed and calibrated to maximize the capacity for mortality risk assessment for populations of interest, and not for clinical decision-making concerning individuals within those populations [4]. Moreover, utilizing the poorest values within a fixed time window, regardless of the outcome of interventions, fails to reflect the dynamic clinical course including differential treatment responses. Thus, these systems are unable to distinguish which patients are at higher risk of developing specific acute conditions. In our study, this was demonstrated by the notably low discriminative ability of PIM 3 in mortality prediction.
Predictive analytics on time series monitoring data were introduced [35, 36] based on evidence that physiologic signatures preceded acute deterioration of patients prior to the arousal of clinical suspicion [5, 6, 37]. Widespread adoption of EHRs which could be queried in real time enabled the development of EWS with the ability to identify clinically deteriorating patients in need of intervention [8, 38]. Accordingly, a wide variety of different tools now exist and are operated alongside rapid response teams in different hospital contexts [9, 10, 39]. For instance, the Bedside Pediatric Early Warning Score (PEWS) is used across the UK National Health Service for the detection of patients in wards who are at risk of acute deterioration, facilitating their timely upgrade to higher level care [40, 41]. Similarly, many other EWS systems have been developed and validated primarily on general wards [11, 40], and their use has been extended to emergency departments [12, 42] and prehospital settings [43].
The ICU environment, where patients are clinically unstable and change rapidly between states of improvement and deterioration, calls for meticulous monitoring and clinical support. This has facilitated the development of ICU early warning systems [18, 44, 45]. The development of more sophisticated monitoring devices has resulted in an exponential growth in sensor data. This, coupled with recent advances in machine learning, artificial intelligence techniques, and data archiving hardware, has facilitated the discovery of data-driven characteristics and patterns of diseases [18, 36, 46–48]. However, the numerous developmental stages, baseline age-related differences in physiologic parameters, and the wide range of underlying pathologic diversity present unique challenges for the analysis of PICU patient data [20, 21]. Moreover, physiological data of the patient is continuously influenced by clinical interventions such as oxygen supplement, volume resuscitation, and vasopressor use, given that the core principle of intensive care is to maintain the steady state [20]. Because variations in physiological data occur within a complex biological system composed of multiple components that interact together, more sophisticated deep learning models such as neural networks, which automatically learn features, have demonstrated better performance than traditional machine learning [49].
Our study makes several significant contributions to the existing literature on mortality prediction in the PICU setting. PROMPT utilized changing vital signs of individuals; employed CNN, a deep model primarily used in image analytics; and achieved high accuracy and discriminative ability in predicting mortality. Prediction performance decreased slightly as the time window ahead of the event lengthened from 6 to 60 h, and the performance of this earlier identification was relatively lower in the validation cohort. Nevertheless, PROMPT provided AUROC above 0.88 for predicting mortality 60 h in advance from both cohorts. Moreover, it consistently achieved higher sensitivity and specificity compared to other standard machine learning algorithms and PIM 3.
Accuracy and false alarm rate are important issues to consider in the practical implementation of EWS in ICU settings. Because sensitivity and specificity mutually interact, the performance of EWS and alarm fatigue should be weighed and optimized [50]. Notably, PROMPT consistently provided higher specificity than PIM 3 and other algorithms against which it was tested. In addition, PROMPT maintained a higher level of accuracy than other models even with a small number of alarms (Additional file 1: Figure S3).
In this study, PROMPT used seven vital signs along with the patient’s age and body weight on PICU admission. The model does not require any custom data entry and relies entirely on data elements that are usually available from the EHRs of most hospitals. Incorporating further parameters such as laboratory tests would be expected to enhance PROMPT’s performance. However, we note that models based on continuously updated physiologic monitoring data are better able to provide timely warning of pending deterioration. Thus, using only the most basic and commonly measured critical care data streamed from the bedside monitor has an advantage for the broader adoption of this model in other ICUs. Relatively minimal data requirements, few manual data entry requirements, and automated operation on data extracted from EHRs save additional labor and cost and may lighten the burden of application in the clinical setting.
This study has several limitations. First, we could not determine the generalizability of our results to other populations. In addition, the retrospective study design did not allow the determination of model performance in a prospective setting. Our model remains a population-based estimate, as we did not validate its efficacy for individual prognostication in a prospective way. Moreover, despite PROMPT’s high performance in detecting and predicting mortality, this knowledge alone is insufficient to affect patient outcomes. Clinician input is required to determine clinical interventions and shape patient-centered outcomes.
However, considering that clinicians in the PICU environment face limited clinical resources and that rationing of health care is a reality in some respects, PROMPT may have the potential to benefit clinical practice. If the risk of critical adverse outcomes is identified earlier, clinicians could allocate staffing and other medical resources with a higher level of certainty. Our model utilizes easily collected data and, therefore, may be particularly suitable for bedside prognostications in relatively low-resourced environments.
In addition, because the predictive window of PROMPT is up to 60 h before death, earlier warnings may give physicians more time to intervene and prevent or mitigate mortality. Alternatively, once physicians are alerted and prepared for the likelihood of death, there are opportunities for preference-concordant, high-value care in PICUs by initiating goals of care discussions earlier and revising treatment plans. Hence, our future work will focus on the practical impact of early recognition of at-risk patients on clinically relevant outcomes.
Lastly, we would like to stress the additional implications of our model. Although our current model does not tell the clinician precisely how to treat a deteriorating patient, the trajectory of predicted risk and designation for time and feature contributions are expected to provide additional information, indirectly. Changes in the trend of predicted mortality over time, coupled with an event or specific intervention with a patient, may provide clinicians intuitive insight into potential associations with a favorable or unfavorable clinical course in individual cases.
Conclusion
In this two-center retrospective study, we validated an easily implementable deep model-based real-time mortality prediction system for critically ill children. Using seven vital signs routinely recorded in standard critical care practice, along with patient age and body weight on ICU admission, our results indicate that PROMPT provides high sensitivity, specificity, and discriminative ability for the prediction of patients at high risk for mortality up to 60 h prior to death. This data-driven early warning score may be an effective tool for the timely recognition of deteriorating patients.
Additional file
Supplementary figures and tables. (DOCX 980 kb)
Acknowledgements
We would like to thank Young Ah Kim (Division of Medical Information and Technology, Yonsei University Health System, Seoul, Korea) for her generous cooperation in data extraction, Jinkyu Yoo (AITRICS, Seoul, Korea) for his contribution in the study design and regular critical discussions and Yu Rang Park (Department of Biomedical Systems Informatics, Yonsei University College of Medicine, Seoul, Korea) for the review and feedback on the manuscript.
Abbreviations
- AUPRC
Area under the precision-recall curve
- AUROC
Area under the receiver operating characteristic curve
- BT
Body temperature
- CNN
Convolutional Neural Network
- DBP
Diastolic blood pressure
- EHR
Electronic health records
- EWS
Early Warning Score
- GBDT
Gradient Boosting Decision Trees
- HR
Heart rate
- ICU
Intensive care unit
- LSTM
Long Short-Term Memory
- MBP
Mean blood pressure
- NPV
Negative predicted value
- PICU
Pediatric intensive care unit
- PIM 3
Pediatric Index of Mortality 3
- PPV
Positive predicted value
- PRISM
Pediatric Risk of Mortality
- PROMPT
Pediatric Risk of Mortality Prediction Tool
- RR
Respiratory rate
- SBP
Systolic blood pressure
- SpO2
Peripheral capillary oxygen saturation
Authors’ contributions
All authors were involved in the conceptualization and design of the study and the discussion of the results. SYK, KWK, and JC were responsible for acquiring the data. SK, YS, IC, and MP contributed to the analysis of the data and interpretation of the result. SYK and SK wrote the manuscript. YSK, ISS, HJ, YHK, KWK, and MHS revised the article critically for important intellectual content. KWK, as the corresponding author, takes responsibility for the content of the manuscript, including the data and analysis. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
K.W.K. was supported by the Institute for Information & Communications Technology Promotion (IITP) grant, funded by the Korea government (MSIT, No. 2017-0-00599, Development of Big Data Analytics Platform for Military Health Information). S.K. was supported by the Institute for Information & Communications Technology Promotion (IITP) grant funded by the Korea government (MSIT, No. 2017-0-01779, A Machine Learning and Statistical Inference Framework for Explainable Artificial Intelligence).
Availability of data and materials
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available because they contain information that could compromise research participant privacy.
Ethics approval and consent to participate
The institutional review boards of Severance Hospital and Samsung Medical Center granted a waiver of consent for this study (#4-2017-0060 and #2019-09015-001, respectively).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Soo Yeon Kim and Saehoon Kim contributed equally to this work.
References
- 1.Straney L, Clements A, Parslow RC, Pearson G, Shann F, Alexander J, Slater A. Paediatric index of mortality 3: an updated model for predicting mortality in pediatric intensive care*. Pediatr Crit Care Med. 2013;14:673–681. doi: 10.1097/PCC.0b013e31829760cf. [DOI] [PubMed] [Google Scholar]
- 2.Pollack MM, Holubkov R, Funai T, Dean JM, Berger JT, Wessel DL, Meert K, Berg RA, Newth CJ, Harrison RE, Carcillo J, Dalton H, Shanley T, Jenkins TL, Tamburro R. The pediatric risk of mortality score: update 2015. Pediatr Crit Care Med. 2016;17:2–9. doi: 10.1097/PCC.0000000000000558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skrobik Y, Kavanagh BP. Scoring systems for the critically ill: use, misuse and abuse. Can J Anaesth. 2006;53:432–436. doi: 10.1007/BF03022613. [DOI] [PubMed] [Google Scholar]
- 4.Vincent JL, Opal SM, Marshall JC. Ten reasons why we should NOT use severity scores as entry criteria for clinical trials or in our treatment decisions. Crit Care Med. 2010;38:283–287. doi: 10.1097/CCM.0b013e3181b785a2. [DOI] [PubMed] [Google Scholar]
- 5.Berlot G, Pangher A, Petrucci L, Bussani R, Lucangelo U. Anticipating events of in-hospital cardiac arrest. Eur J Emerg Med. 2004;11:24–28. doi: 10.1097/00063110-200402000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Moss TJ, Lake DE, Calland JF, Enfield KB, Delos JB, Fairchild KD, Moorman JR. Signatures of subacute potentially catastrophic illness in the ICU: model development and validation. Crit Care Med. 2016;44:1639–1648. doi: 10.1097/CCM.0000000000001738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Monaghan A. Detecting and managing deterioration in children. Paediatr Nurs. 2005;17:32–35. doi: 10.7748/paed.17.1.32.s27. [DOI] [PubMed] [Google Scholar]
- 8.Alam N, Hobbelink EL, van Tienhoven AJ, van de Ven PM, Jansma EP, Nanayakkara PW. The impact of the use of the Early Warning Score (EWS) on patient outcomes: a systematic review. Resuscitation. 2014;85:587–594. doi: 10.1016/j.resuscitation.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 9.Parshuram CS, Hutchison J, Middaugh K. Development and initial validation of the Bedside Paediatric Early Warning System score. Crit Care. 2009;13:R135. doi: 10.1186/cc7998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skaletzky SM, Raszynski A, Totapally BR. Validation of a modified pediatric early warning system score: a retrospective case-control study. Clin Pediatr (Phila) 2012;51:431–435. doi: 10.1177/0009922811430342. [DOI] [PubMed] [Google Scholar]
- 11.Churpek MM, Yuen TC, Winslow C, Robicsek AA, Meltzer DO, Gibbons RD, Edelson DP. Multicenter development and validation of a risk stratification tool for ward patients. Am J Respir Crit Care Med. 2014;190:649–655. doi: 10.1164/rccm.201406-1022OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Egdell P, Finlay L, Pedley DK. The PAWS score: validation of an early warning scoring system for the initial assessment of children in the emergency department. Emerg Med J. 2008;25:745–749. doi: 10.1136/emj.2007.054965. [DOI] [PubMed] [Google Scholar]
- 13.Royston P, Moons KG, Altman DG, Vergouwe Y. Prognosis and prognostic research: developing a prognostic model. Bmj. 2009;338:b604. doi: 10.1136/bmj.b604. [DOI] [PubMed] [Google Scholar]
- 14.Baronov D, McManus M, Butler E, Chung D, Almodovar MC. Next generation patient monitor powered by in-silico physiology. Conf Proc IEEE Eng Med Biol Soc. 2015;2015:4447–4453. doi: 10.1109/EMBC.2015.7319382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rusin CG, Acosta SI, Shekerdemian LS, Vu EL, Bavare AC, Myers RB, Patterson LW, Brady KM, Penny DJ. Prediction of imminent, severe deterioration of children with parallel circulations using real-time processing of physiologic data. J Thorac Cardiovasc Surg. 2016;152:171–177. doi: 10.1016/j.jtcvs.2016.03.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yun C, Hui Y. Heterogeneous postsurgical data analytics for predictive modeling of mortality risks in intensive care units. Conf Proc IEEE Eng Med Biol Soc. 2014;2014:4310–4314. doi: 10.1109/EMBC.2014.6944578. [DOI] [PubMed] [Google Scholar]
- 17.Pollard TJ, Celi LA. Enabling machine learning in critical care. ICU Manag Pract. 2017;17:198–199. [PMC free article] [PubMed] [Google Scholar]
- 18.Johnson AEW, Mark RG. Real-time mortality prediction in the intensive care unit. AMIA Annu Symp Proc. 2017;2017:994–1003. [PMC free article] [PubMed] [Google Scholar]
- 19.Bailly S, Meyfroidt G, Timsit JF. What’s new in ICU in 2050: big data and machine learning. Intensive Care Med. 2018;44:1524–1527. doi: 10.1007/s00134-017-5034-3. [DOI] [PubMed] [Google Scholar]
- 20.Wong HR, Dalton HJ. The PICU perspective on monitoring hemodynamics and oxygen transport. Pediatr Crit Care Med. 2011;12:S66–S68. doi: 10.1097/PCC.0b013e3182211c60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olive MK, Owens GE. Current monitoring and innovative predictive modeling to improve care in the pediatric cardiac intensive care unit. Transl Pediatr. 2018;7:120–128. doi: 10.21037/tp.2018.04.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kennedy CE, Turley JP. Time series analysis as input for clinical predictive modeling: modeling cardiac arrest in a pediatric ICU. Theor Biol Med Model. 2011;8:40. doi: 10.1186/1742-4682-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Che Z, Purushotham S, Khemani R, Liu Y. Interpretable deep models for ICU outcome prediction. AMIA Annu Symp Proc. 2016;2016:371–380. [PMC free article] [PubMed] [Google Scholar]
- 24.Rawat W, Wang Z. Deep convolutional neural networks for image classification: a comprehensive review. Neural Comput. 2017;29:2352–2449. doi: 10.1162/neco_a_00990. [DOI] [PubMed] [Google Scholar]
- 25.Anwar SM, Majid M, Qayyum A, Awais M, Alnowami M, Khan MK. Medical image analysis using convolutional neural networks: a review. J Med Syst. 2018;42:226. doi: 10.1007/s10916-018-1088-1. [DOI] [PubMed] [Google Scholar]
- 26.Kam HJ, Kim HY. Learning representations for the early detection of sepsis with deep neural networks. Comput Biol Med. 2017;89:248–255. doi: 10.1016/j.compbiomed.2017.08.015. [DOI] [PubMed] [Google Scholar]
- 27.Kamaleswaran R, Akbilgic O, Hallman MA, West AN, Davis RL, Shah SH. Applying artificial intelligence to identify physiomarkers predicting severe sepsis in the PICU. Pediatr Crit Care Med. 2018;19:e495–e503. doi: 10.1097/PCC.0000000000001666. [DOI] [PubMed] [Google Scholar]
- 28.Savalia Shalin, Emamian Vahid. Cardiac Arrhythmia Classification by Multi-Layer Perceptron and Convolution Neural Networks. Bioengineering. 2018;5(2):35. doi: 10.3390/bioengineering5020035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen T, Guestrin C. XGBoost: a scalable tree boosting system. Proceedings of the 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining. San Francisco: ACM; 2016. pp. 785–794. [Google Scholar]
- 30.Hochreiter S. #252, Schmidhuber r. long short-term memory. Neural Comput. 1997;9:1735–1780. doi: 10.1162/neco.1997.9.8.1735. [DOI] [PubMed] [Google Scholar]
- 31.Davis J, Goadrich M. The relationship between Precision-Recall and ROC curves. Proceedings of the 23rd international conference on Machine learning. Pittsburgh: ACM; 2006. pp. 233–240. [Google Scholar]
- 32.Keegan MT, Gajic O, Afessa B. Severity of illness scoring systems in the intensive care unit. Crit Care Med. 2011;39:163–169. doi: 10.1097/CCM.0b013e3181f96f81. [DOI] [PubMed] [Google Scholar]
- 33.Murphy-Filkins R, Teres D, Lemeshow S, Hosmer DW. Effect of changing patient mix on the performance of an intensive care unit severity-of-illness model: how to distinguish a general from a specialty intensive care unit. Crit Care Med. 1996;24:1968–1973. doi: 10.1097/00003246-199612000-00007. [DOI] [PubMed] [Google Scholar]
- 34.Booth FV, Short M, Shorr AF, Arkins N, Bates B, Qualy RL, Levy H. Application of a population-based severity scoring system to individual patients results in frequent misclassification. Crit Care. 2005;9:R522–R529. doi: 10.1186/cc3790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bailey TC, Chen Y, Mao Y, Lu C, Hackmann G, Micek ST, Heard KM, Faulkner KM, Kollef MH. A trial of a real-time alert for clinical deterioration in patients hospitalized on general medical wards. J Hosp Med. 2013;8:236–242. doi: 10.1002/jhm.2009. [DOI] [PubMed] [Google Scholar]
- 36.Henry KE, Hager DN, Pronovost PJ, Saria S. A targeted real-time early warning score (TREWScore) for septic shock. Sci Transl Med. 2015;7:299ra122. doi: 10.1126/scitranslmed.aab3719. [DOI] [PubMed] [Google Scholar]
- 37.Hillman KM, Bristow PJ, Chey T, Daffurn K, Jacques T, Norman SL, Bishop GF, Simmons G. Duration of life-threatening antecedents prior to intensive care admission. Intensive Care Med. 2002;28:1629–1634. doi: 10.1007/s00134-002-1496-y. [DOI] [PubMed] [Google Scholar]
- 38.Smith ME, Chiovaro JC, O'Neil M, Kansagara D, Quinones AR, Freeman M, Motu'apuaka ML, Slatore CG. Early warning system scores for clinical deterioration in hospitalized patients: a systematic review. Ann Am Thorac Soc. 2014;11:1454–1465. doi: 10.1513/AnnalsATS.201403-102OC. [DOI] [PubMed] [Google Scholar]
- 39.Cater DT, Tori AJ, Moser EAS, Rowan CM. Modification and assessment of the bedside pediatric early warning score in the pediatric allogeneic hematopoietic cell transplant population. Pediatr Crit Care Med. 2018;19:483–488. doi: 10.1097/PCC.0000000000001521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Akre M, Finkelstein M, Erickson M, Liu M, Vanderbilt L, Billman G. Sensitivity of the pediatric early warning score to identify patient deterioration. Pediatrics. 2010;125:e763–e769. doi: 10.1542/peds.2009-0338. [DOI] [PubMed] [Google Scholar]
- 41.Parshuram CS, Dryden-Palmer K, Farrell C, Gottesman R, Gray M, Hutchison JS, Helfaer M, Hunt EA, Joffe AR, Lacroix J, Moga MA, Nadkarni V, Ninis N, Parkin PC, Wensley D, Willan AR, Tomlinson GA. Effect of a pediatric early warning system on all-cause mortality in hospitalized pediatric patients: the EPOCH randomized clinical trial. JAMA. 2018;319:1002–1012. doi: 10.1001/jama.2018.0948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gold DL, Mihalov LK, Cohen DM. Evaluating the Pediatric Early Warning Score (PEWS) system for admitted patients in the pediatric emergency department. Acad Emerg Med. 2014;21:1249–1256. doi: 10.1111/acem.12514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Williams TA, Tohira H, Finn J, Perkins GD, Ho KM. The ability of early warning scores (EWS) to detect critical illness in the prehospital setting: a systematic review. Resuscitation. 2016;102:35–43. doi: 10.1016/j.resuscitation.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 44.Vincent JL, Moreno R. Clinical review: scoring systems in the critically ill. Crit Care. 2010;14:207. doi: 10.1186/cc8204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Liu V. Keeping score of severity scores: taking the next step. Crit Care Med. 2016;44:639–640. doi: 10.1097/CCM.0000000000001501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Williams JB, Ghosh D, Wetzel RC. Applying machine learning to pediatric critical care data. Pediatr Crit Care Med. 2018;19:599–608. doi: 10.1097/01.pcc.0000537876.83337.e2. [DOI] [PubMed] [Google Scholar]
- 47.Delahanty RJ, Kaufman D, Jones SS. Development and evaluation of an automated machine learning algorithm for in-hospital mortality risk adjustment among critical care patients. Crit Care Med. 2018;46:e481–e4e8. doi: 10.1097/CCM.0000000000003011. [DOI] [PubMed] [Google Scholar]
- 48.Nemati S, Holder A, Razmi F, Stanley MD, Clifford GD, Buchman TG. An interpretable machine learning model for accurate prediction of Sepsis in the ICU. Crit Care Med. 2018;46:547–553. doi: 10.1097/CCM.0000000000002936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bengio Y, Courville A, Vincent P. Representation learning: a review and new perspectives. IEEE Trans Pattern Anal Mach Intell. 2013;35:1798–1828. doi: 10.1109/TPAMI.2013.50. [DOI] [PubMed] [Google Scholar]
- 50.Capan M, Hoover S, Miller KE, Pal C, Glasgow JM, Jackson EV, Arnold RC. Data-driven approach to Early Warning Score-based alert management. BMJ Open Qual. 2018;7:e000088. doi: 10.1136/bmjoq-2017-000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figures and tables. (DOCX 980 kb)
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available because they contain information that could compromise research participant privacy.