Abstract
Background
Health-related quality of life and glycaemic control are some of the central outcomes in clinical diabetes care and research. The purpose of this study was to describe the health-related quality of life and assess its association with glycaemic control in adults with type 1 and type 2 diabetes in a nationwide setting.
Methods
In this cross-sectional survey, people with type 1 (n = 2479) and type 2 diabetes (n = 2469) were selected at random without replacement from the Swedish National Diabetes Register. Eligibility criteria were being aged 18–80 years with at least one registered test of glycated haemoglobin (HbA1c) the last 12 months. The generic 36-item Short Form version 2 (SF-36v2) was answered by 1373 (55.4%) people with type 1 diabetes and 1353 (54.8%) with type 2 diabetes.
Results
Correlation analyses showed weak correlations between scores on the SF-36v2 and glycaemic control for both diabetes types. After the participants were divided into three groups based on their levels of HbA1c, multivariate regression analyses adjusted for demographics, other risk factors and diabetes complications showed that among participants with type 1 diabetes, the high-risk group (≥70 mmol/mol/8.6%) had statistically significantly lower means in five out of eight domains of the SF-36v2 and the mental component summary measure, as compared with the well-controlled group (< 52 mmol/mol/6.9%). Among the participants with type 2 diabetes, the high-risk group had the lowest statistically significantly means in seven domains and both summary measures.
Conclusions
Among people with type 1 and type 2 diabetes, adults with high-risk HbA1c levels have lower levels of health-related quality of life in most but not all domains of the SF-36v2. This finding was not explained by demographics, other risk factors, or diabetes complications. The weak individual-level correlations between HRQOL scores and levels of glycaemic control argues for the need to not focus exclusively on either HbA1c levels or HRQOL scores but rather on both because both are important parts of a complex, life-long, challenging condition.
Electronic supplementary material
The online version of this article (10.1186/s12955-019-1212-z) contains supplementary material, which is available to authorized users.
Keywords: Diabetes mellitus, type 1; Diabetes mellitus, type 2; Health-related quality of life; SF-36; Cross-sectional study
Introduction
Health-related quality of life (HRQOL) together with glycaemic control as measured by glycated haemoglobin (HbA1c) levels are some of the central outcomes in clinical diabetes care and research [1–8]. Through a suggested bidirectional relationship, diabetes and self-management demands might diminish HRQOL, possibly leading to worse glycaemic control and complications [3].
The medical outcomes study health survey short form (SF)-36 is a widely used generic HRQOL measurement tool recommended for comparisons and descriptions across subgroups with the same or different diseases. The RAND-36 has equivalent items but is scored differently [2, 4, 9, 10]. Cross-sectional associations between either the SF-36 or the RAND-36 and HbA1c levels in adults have been addressed in a few studies of people with type 1 diabetes [11–13] and more commonly in studies of people with type 2 diabetes [14–20]. There are also studies of both groups combined [21, 22]. However, there have been inconsistent results. Previous studies have presented varying degrees of support both for [13, 14, 17, 19, 22] and against a relationship between HRQOL and glycaemic control [11–13, 15–18, 20, 21].
As a generic measure of HRQOL, the SF-36 has been criticized for not being specific enough for diabetes-related aspects [4, 9, 10, 23]. However, unlike diabetes-specific tools, a generic measure adds the potential to be able to relate the results to the overall population and to other health conditions. Among generic measures, the SF-36 is widely used in diabetes research and has been suggested as a reasonable choice in diabetes research as well as for application in diabetes care, with reference to the inclusion of a broad range of relevant aspects and supporting evidence for measurement quality [9, 10, 24, 25]. Furthermore, generic HRQOL in people with diabetes as measured by the SF-36 or the RAND-36 has been suggested to be a marker for mortality [26–28]. Despite the critique, it is suggested important to further research generic HRQOL in people with diabetes using the SF-36 [9].
Diabetes care continuously advances with new medical treatments, technical aids for insulin administration and the continuous monitoring of glucose levels, and skills facilitating self-management [1, 7, 29, 30]. Despite previous studies, there is a lack of updated data on HRQOL in people with diabetes. The aim of this study was thus to describe the HRQOL as measured by the SF-36 questionnaire and assess associations of that HRQOL and glycaemic control in adults with type 1 and type 2 diabetes in a nationwide setting with current diabetes care.
Participants and methods
Sample and data collection
In this cross-sectional postal survey, 2479 people with type 1 diabetes and 2469 with type 2 diabetes were selected at random without replacement from the Swedish National Diabetes Register (NDR), a nationwide quality register for diabetes care. In 2015, the NDR had above 95% coverage for people with type 1 diabetes and above 90% for people with type 2 diabetes. In total, there were about 40,000 people with type 1 diabetes and about 347,000 with type 2 diabetes registered in the NDR. Eligibility criteria were patients registered in the NDR during the period from September 30th 2014 to October 1st 2015, being alive, aged 18–80 years and having at least one HbA1c level registered during the last 12 months. With these inclusion criteria there were 29,245 people with type 1 diabetes at hospital out-patient clinics and 208,852 people with type 2 diabetes at primary health care centres eligible for recruitment.
In October 2015, the SF-36v2 and a prepaid return envelope were sent by mail together with a newly developed diabetes-specific questionnaire. Data about the diabetes-specific questionnaire are reported elsewhere [31–33]. Non-responders received one reminder including the same material after 30 days. In total, 1373 (55.4%) people with type 1 diabetes and 1353 (54.8%) with type 2 diabetes answered the SF-36v2.
Clinical data (diabetes type defined by clinical diagnosis, diabetes duration, HbA1c level, medical treatment, physical activity level, cardiovascular risk factors, and complications) and demographic data were obtained from the NDR. The clinical data collected from the NDR are registered in the NDR because of their important roles for high quality diabetes care.
SF-36 version 2
SF-36 is a 36-item self-administered generic HRQOL questionnaire from the medical outcomes study. The SF-36 is internationally established with support for its validity and reliability [33, 34]. We used the SF-36 version 2 (SF-36v2) standard form in Swedish. An eight-domain profile is generated. The eight domains are physical functioning (PF); role-physical (RP), i.e., role limitations due to physical health problems; bodily pain (BP); general health (GH); vitality (VT); social functioning (SF); role-emotional (RE), i.e., role limitations due to mental health; and mental health (MH). The domains are scored from 0 to 100. The domains are aggregated in the Physical Component Summary (PCS) and the Mental Component Summary (MCS) measures, reported as norm-based T-scores. T-scores are standardized to the 2009 US general population with a mean of 50 and a standard deviation of 10. The average range for groups is a mean T-score between 47 and 53. Higher scores represent better HRQOL [33, 34].
Statistical analysis
All analyses were performed separately for participants with type 1 and type 2 diabetes. Descriptive statistics are presented as the means and standard deviations for normally distributed continuous variables, the median and interquartile range for skewed distributions, or number and percentages for categorical variables. The descriptive statistics for each variable are based on non-missing observations. For variables given as percentage, the denominator is defined as all individuals with non-missing observations.
The SF-36v2 data were scored according to the manual using licensed software from QualityMetric Inc. To examine associations between SF-36v2 scores and HbA1c levels, we first used Spearman’s rank correlation with HbA1c as a continuous variable. For the group-level analysis, HbA1c was considered a categorical variable and was divided into the following three clinically relevant groups with differing levels of glycaemic control and therefore differing levels of the risk of diabetes complications according to international and Swedish treatment guidelines: well-controlled (< 52 mmol/mol/6.9%), sub-optimal (52–69 mmol/mol/6.9–8.5%), and high-risk (≥70 mmol/mol/8.6%). Between the HbA1c groups, the data balance and the deviation from the means in the clinical and demographic data were examined using the standardized mean difference.
Unadjusted and adjusted multivariate regression analyses were used to calculate the least square mean estimates and 95% confidence intervals for the SF-36v2 domains and summary measures in the three HbA1c groups. The observations in each SF-36v2 domain and summary measure were modelled using a linear model with fixed effects for the HbA1c group (exposure), age, sex, diabetes duration, body mass index (BMI), systolic blood pressure (SBP), LDL cholesterol level, micro and macro albuminuria, estimated glomerular filtration rate (eGFR), retinopathy, smoking status, physical activity level, receipt of antihypertensive and lipid lowering treatments, previous coronary heart disease (CHD) and previous stroke. The results are presented as least square mean estimates with 95% confidence intervals. The amount of missing data was 0% for demographics, 7.2% for clinical data (range 0–36.5%), and 1.7% for SF-36 domains (range 0–3.3% for individual dimensions). Missing data were imputed ten times using multiple chained equations. The analyses were performed separately for each imputed data set, and the results were subsequently combined using Rubin’s rules.
A significance level of 5% was used throughout; no allowance was made for multiplicity of statistical tests.
SAS 9.4 and R 3.4.4 were used for the clinical and demographic descriptive statistics and the correlation and regression analyses.
Ethical considerations
The study conforms to the Declaration of Helsinki and was approved by the Regional Ethical Review Board in Gothenburg, Sweden (No. 029–15, T600–15). The letter to the participants informed them about the study’s purpose, the voluntary nature of their participation, the confidentiality measures and methods of handling of their personal data, the NDR, contact details, and the right to end participation. Participants gave their informed consent.
Results
The clinical and demographic characteristics of the responders separated by diabetes type and HbA1c level are presented in Table 1. Among those with type 1 diabetes, 50.3% of the responders were men, the average age was 48.6 years, the average diabetes duration was 24.7 years, and the average HbA1c level was 62 mmol/mol (7.8%). Among those with type 2 diabetes, the corresponding numbers were 60.8% men, average age of 66.6 years, average duration of 9.4 years, and average HbA1c level of 53 mmol/mol (7.0%) (Table 1). The crude means and standard deviations for the SF-36v2 domains for participants with type 1 diabetes and those with type 2 diabetes are found in Table 2. The clinical characteristics of the non-responders are described in detail in Additional file 1: Table S1.
Table 1.
Clinical and demographic characteristics of the responders separated by diabetes type and HbA1c level
| Variable | Type 1 diabetes | Type 2 diabetes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | HbA1c < 52 mmol/mol (< 6.9%) | HbA1c 52–69 mmol/mol (6.9–8.5%) | HbA1c ≥70 mmol/mol (≥8.6%) | Standardized mean difference, SMD | p-value | All | HbA1c < 52 mmol/mol (< 6.9%) | HbA1c 52–69 mmol/mol (6.9–8.5%) | HbA1c ≥70 mmol/mol (≥8.6%) | Standardized mean difference, SMD | p-value | |
| Number (%) | 1373 | 284 (20.7) | 781 (56.9) | 308 (22.4) | 1353 | 725 (53.6) | 503 (37.2) | 125 (9.2) | ||||
| Men, n (%) | 690 (50.3) | 152 (53.5) | 391 (50.1) | 147 (47.7) | 0.077 | 0.366 | 822 (60.8) | 444 (61.2) | 302 (60.0) | 76 (60.8) | 0.016 | 0.914 |
| Age, years (SD) | 48.6 (16.4) | 46.9 (17.0) | 49.6 (16.1) | 47.8 (16.3) | 0.113 | 0.028 | 66.6 (9.1) | 66.5 (9.1) | 66.9 (9.0) | 65.5 (9.7) | 0.103 | 0.274 |
| Diabetes duration, years (IQR) | 22.0 (12.0–36.0) | 19.0 (7.0–32.0) | 23.0 (13.0–37.0) | 24.0 (13.0–37.0) | 0.150 | < 0.001 | 8.0 (4.0–14.0) | 6.0 (3.0–11.0) | 10.0 (6.0–16.0) | 13.0 (6.0–17.0) | 0.443 | < 0.001 |
| HbA1c mmol/mol (SD) | 62 (12.7) | 53 (12.5) | ||||||||||
| HbA1c, % (SD) | 7.8 (1.2) | 7.0 (1.1) | ||||||||||
| BMI, kg/m2 (SD) | 26.0 (4.2) | 25.2 (3.8) | 26.0 (4.2) | 26.7 (4.6) | 0.239 | < 0.001 | 29.9 (5.3) | 29.3 (5.2) | 30.3 (5.4) | 32.0 (5.5) | 0.332 | < 0.001 |
| Systolic blood pressure, mmHg (SD) | 127.0 (14.0) | 124.8 (14.0) | 127.5 (13.8) | 127.8 (14.2) | 0.145 | 0.009 | 134.3 (14.3) | 134.0 (14.4) | 134.5 (13.7) | 135.1 (16.5) | 0.046 | 0.687 |
| Antihypertensive medication, n (%) | 589 (44.7) | 99 (36.9) | 341 (45.3) | 149 (50.2) | 0.179 | 0.006 | 1070 (80.1) | 572 (79.6) | 404 (81.9) | 94 (76.4) | 0.091 | 0.327 |
| LDL-cholesterol, mmol/L (SD) | 2.4 (0.8) | 2.5 (0.8) | 2.4 (0.8) | 2.5 (0.8) | 0.077 | 0.262 | 2.5 (0.9) | 2.5 (0.9) | 2.4 (0.9) | 2.5 (1.0) | 0.026 | 0.810 |
| Lipid-lowering medication, n (%) | 642 (48.4) | 94 (34.6) | 378 (49.8) | 170 (57.6) | 0.315 | < 0.001 | 900 (68.1) | 472 (66.6) | 344 (70.1) | 84 (69.4) | 0.050 | 0.421 |
| Microalbuminuria, n (%) | 132 (10.3) | 12 (4.6) | 70 (9.5) | 50 (17.6) | 0.285 | < 0.001 | 194 (18.0) | 80 (13.9) | 83 (20.1) | 31 (34.1) | 0.323 | < 0.001 |
| Macro albuminuria, n (%) | 31 (2.6) | 5 (2.1) | 12 (1.8) | 14 (5.2) | 0.126 | 0.010 | 52 (5.0) | 27 (4.8) | 20 (5.1) | 5 (6.1) | 0.037 | 0.884 |
| Estimated Glomerular Filtration Rate, eGFR, mL/min (SD) | 90.0 (23.5) | 90.6 (20.7) | 89.1 (22.6) | 91.6 (27.7) | 0.071 | 0.263 | 82.3 (23.5) | 82.5 (22.3) | 81.9 (24.0) | 83.4 (27.9) | 0.038 | 0.826 |
| Retinopathy, n (%) | 875 (65.9) | 137 (50.6) | 520 (68.2) | 218 (74.1) | 0.333 | < 0.001 | 327 (29.4) | 128 (21.7) | 153 (36.3) | 46 (47.0) | 0.366 | < 0.001 |
| Coronary heart disease, n (%) | 83 (6.3) | 9 (3.3) | 53 (7.0) | 21 (7.1) | 0.113 | 0.083 | 279 (22.4) | 136 (20.2) | 111 (24.0) | 32 (28.6) | 0.130 | 0.081 |
| Stroke, n (%) | 48 (3.6) | 5 (1.9) | 32 (4.2) | 11 (3.7) | 0.093 | 0.196 | 96 (7.8) | 48 (7.2) | 40 (8.9) | 8 (7.1) | 0.043 | 0.576 |
| Smoker, n (%) | 135 (10.1) | 14 (5.1) | 78 (10.2) | 43 (14.4) | 0.214 | 0.001 | 162 (12.9) | 79 (11.7) | 58 (12.3) | 25 (23.1) | 0.203 | 0.004 |
| Physical activity, daily, n (%) | 359 (27.6) | 90 (33.5) | 203 (27.2) | 66 (23.2) | 0.334 | < 0.001 | 426 (34.9) | 251 (38.7) | 157 (33.9) | 18 (16.7) | 0.410 | < 0.001 |
| Diabetes treatment | 0.136 | 0.138 | 0.813 | < 0.001 | ||||||||
| Diet alone, n (%) | 195 (14.4) | 172 (23.7) | 19 (3.8) | 4 (3.3) | ||||||||
| Oral hypoglycaemic agent alone, n (%) | 718 (53.1) | 419 (57.8) | 261 (52.0) | 38 (30.9) | ||||||||
| Insulin alone, n (%) | 1335 (97.2) | 271 (95.4) | 764 (97.8) | 300 (97.4) | 130 (9.6) | 46 (6.3) | 63 (12.5) | 21 (17.1) | ||||
| Insulin and oral agent, n (%) | 32 (2.3) | 9 (3.2) | 15 (1.9) | 8 (2.6) | 266 (19.7) | 76 (10.5) | 140 (27.9) | 50 (40.7) | ||||
| Insulin pump users among insulin users, n (%) | 356 (26.2) | 66 (23.8) | 221 (28.5) | 69 (22.5) | 0.091 | 0.082 | 2 (0.5) | 1 (0.9) | 1 (0.5) | 0 (0.0) | 0.093 | 0.729 |
The descriptive statistics are presented as the means and standard deviations (SD) for normally distributed continuous variables, the median and interquartile range (IQR) for skewed distributions, or number and percentages for categorical variables
Table 2.
Crude means and standard deviations for the SF-36v2 domains for participants with type 1 diabetes and those with type 2 diabetes
| SF-36v2 domains | Type 1 diabetes | Type 2 diabetes |
|---|---|---|
| PF | 84.4 (21.3) | 70.6 (27.0) |
| RP | 80.2 (26.5) | 73.6 (29.3) |
| BP | 69.2 (28.0) | 62.5 (28.8) |
| GH | 60.3 (23.8) | 60.8 (23.7) |
| VT | 54.4 (24.5) | 58.8 (24.1) |
| SF | 81.3 (23.9) | 79.2 (28.0) |
| RE | 83.2 (24.2) | 81.0 (24.8) |
| MH | 72.7 (20.0) | 74.6 (21.7) |
| PCS | 50.2 (9.4) | 46.5 (9.9) |
| MCS | 48.8 (11.2) | 50.8 (11.1) |
PF Physical functioning, RP Role-physical, BP Bodily pain, GH General health, VT Vitality, SF Social functioning, RE Role-emotional, MH Mental health, PCS Physical component summary measure, MCS Mental component summary measure
In the correlation analysis, the HbA1c level showed weak negative correlations with the SF-36v2 dimensions (− 0.19 to − 0.06) in both type 1 and type 2 diabetes (Table 3).
Table 3.
Spearman’s rank correlations with p-values between SF-36v2 domain scores and glycated haemoglobin (HbA1c) level in type 1 and type 2 diabetes
| SF-36v2 domain | Type 1 diabetes | Type 2 diabetes |
|---|---|---|
| PF | −0.15 (<.0001) | −0.17 (<.0001) |
| RP | −0.12 (<.0001) | − 0.18 (<.0001) |
| BP | −0.14 (<.0001) | − 0.13 (<.0001) |
| GH | −0.19 (<.0001) | − 0.14 (<.0001) |
| VT | −0.13 (<.0001) | − 0.13 (<.0001) |
| SF | −0.08 (0.0025) | − 0.12 (<.0001) |
| RE | −0.08 (0.0056) | − 0.12 (<.0001) |
| MH | −0.06 (0.0319) | −0.08 (0.0059) |
PF Physical functioning, RP Role-physical, BP Bodily pain, GH General health, VT Vitality, SF Social functioning, RE Role-emotional, MH Mental health
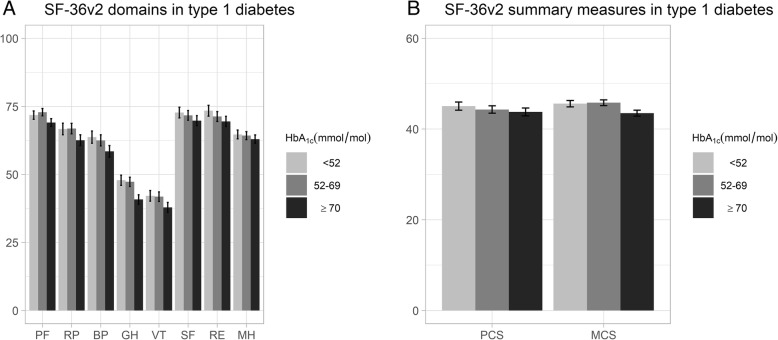
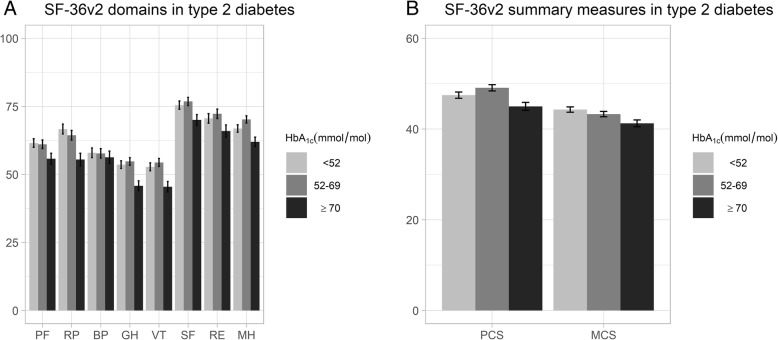
The results from the adjusted regression analyses are presented separately for participants with type 1 and type 2 diabetes in Figs. 1 and 2. The detailed least square mean estimates and confidence intervals from the unadjusted and adjusted analyses are provided in Additional file 1: Table S2.
Fig. 1.
Adjusted regression analyses of HbA1c level and SF-36v2 domains and summary measures in type 1 diabetes. Adjusted least square mean estimates with 95% confidence intervals for SF-36v2 domains (a) and for summary measures (b) in type 1 diabetes separated by HbA1c level. Adjusted for age, sex, diabetes duration, body mass index, systolic blood pressure, LDL cholesterol level, micro and macro albuminuria, estimated glomerular filtration rate, retinopathy, smoking status, physical activity level, receipt of antihypertensive and lipid lowering treatments, previous coronary heart disease and previous stroke. PF: physical functioning; RP: role-physical; BP: bodily pain; GH: general health; VT: vitality; SF: social functioning; RE: role-emotional; MH: mental health; PCS: physical component summary measure; MCS: mental component summary measure
Fig. 2.
Adjusted regression analyses of HbA1c level and SF-36v2 domains and summary measures in type 2 diabetes. Adjusted least square mean estimates with 95% confidence intervals for SF-36v2 domains (a) and for summary measures (b) in type 2 diabetes separated by glycated haemoglobin (HbA1c) level. Adjusted for age, sex, diabetes duration, body mass index, systolic blood pressure, LDL cholesterol level, micro and macro albuminuria, estimated glomerular filtration rate, retinopathy, smoking status, physical activity level, receipt of antihypertensive and lipid lowering treatments, previous coronary heart disease and previous stroke. PF: physical functioning; RP: role-physical; BP: bodily pain; GH: general health; VT: vitality; SF: social functioning; RE: role-emotional; MH: mental health; PCS: physical component summary measure; MCS: mental component summary measure
Among those with type 1 diabetes, the adjusted analysis of the HbA1c groups showed that the high-risk group (≥70 mmol/mol/8.6%) had statistically significantly lower means than the well-controlled (< 52 mmol/mol/6.9%) group in five domains (RP, BP, GH, VT, RE), with the largest between-group difference in the GH domain. In the summary components, compared with the well-controlled group, the high-risk group had a statistically significantly lower mean MCS score. There were no statistically significant differences in PCS scores. Both the adjusted PCS and adjusted MCS scores were below the US normal range for all HbA1c groups (Fig. 1, Additional file 1: Table S2).
Among those with type 2 diabetes, the adjusted analysis showed that the high-risk group had the statistically significantly lowest means in all domains except BP. In the MH domain, the sup-optimal group (52–69 mmol/mol/6.9–8.5%) had the statistically significantly highest mean. The clearest differences were observed in the RP, GH, and VT domains. With regard to MCS and PCS, the high-risk group still had the statistically significantly lowest means, which were below the US normal range. The sub-optimal and well-controlled groups were both within the range for PCS but below the range for MCS (Fig. 2, Additional file 1: Table S2).
Discussion
Summary of results
With a large randomly selected nationwide sample of adults with type 1 and type 2 diabetes, this study adds current data to the body of research that uses the SF-36 to evaluate HRQOL and assesses its associations with glycaemic control. At the individual level, we observed only weak correlations between scores on the SF-36v2 and glycaemic control. After dividing the samples into three clinically relevant groups according to levels of glycaemic control, the adjusted analyses showed that among participants with type 1 diabetes, compared with the well-controlled group, the high-risk group had statistically significantly lower means in five domains (RP, BP, GH, VT, RE), as well as in the MCS score. For the high-risk group; the largest difference in comparison to the other two groups was seen in the GH domain. In the adjusted analyses for participants with type 2 diabetes, the high-risk group had the statistically significantly lowest means in both summary measures and all domains except BP. The largest differences between the high-risk group and the other two groups were found in the domains RP, GH and VT for participants with type 2 diabetes.
Comparisons to previous studies in people with type 1 diabetes
For people with type 1 diabetes, we found few previous and no recent studies of HRQOL based on the SF-36 or the RAND-36 and the association of HRQOL with glycaemic control. Compared to the previous studies, our sample size was larger, with a wider age span and a lower mean HbA1c level. Our study adds a new aspect by dividing the sample into three clinically relevant HbA1c groups according to their risk of diabetes complications. The results of a US study including 150 participants support our results, with higher SF-36 scores among those with lower HbA1c levels than among those with higher HbA1c levels [22]. In the present study, GH was the domain with the largest difference among the HbA1c groups, with the lowest score in the high-risk group. This finding is supported by the results in another US study (n = 397) that showed that a higher HbA1c level was correlated with worse GH scores [13]. However, in that study, the results were not confirmed in the adjusted analyses [13]. Furthermore, in 2003, no relationship between RAND-36 score and HbA1c level was found in a study conducted in the Netherlands (n = 281) [12]. The Diabetes Control and Complications Trial (n = 1441) found no differences in SF-36 scores between the intensive insulin treatment group with an HbA1c level of 7.4% (57 mmol/mol) compared to the standard treatment group with an HbA1c level of 9.1% (76 mmol/mol) at the end of the study [11, 35].
Comparisons to previous studies in people with type 2 diabetes
Among people with type 2 diabetes, previous larger studies using the SF-36 or RAND-36 are more common and include data that are more recent. Some studies divided their sample according to HbA1c level, but the cut-off values for the groups differed from those used in our study. Our results showing lower levels of HRQOL in groups with higher HbA1c levels are supported by SF-36 data from Italy [19] and the ADDITION trial with participants from Denmark, the Netherlands and the UK [17]. The Italian study (n = 2499) reported a negative association between the MCS score and the HbA1c level, but after adjustment for hypo- and hyperglycaemic events, this association was no longer significant [19]. In the ADDITION trial (n = 1876), participants with HbA1c levels below 7% (53 mmol/mol) had higher PCS and MCS scores than those with higher HbA1c levels [17]. Two studies suggested the lack of an association, namely, a study from the Netherlands (n = 1006) that used the RAND-36 and three HbA1c groups [16] and an Estonian study (n = 200) that used the SF-36 and divided the sample using a cut-off HbA1c level of 7.5% (58.5 mmol/mol) [15]. The ADDITION and the Italian cohorts are similar to the cohort in our study with regard to age, and the ADDITION cohort had slightly lower HbA1c levels than those in our study [17, 19]. The other studies in which the results were not in agreement with those of our study included younger participants with higher HbA1c levels in comparison to our sample [15, 16]. Among the studies that treated HbA1c as a continuous variable, the results differed. Three studies showed no relationship [17, 18, 20], and two studies supported a relationship [14, 22].
Complexity
The reasons for the inconsistencies between previous studies and our study could be related to differences in sample characteristics, HbA1c groups, available clinical and demographic data, or reporting results for domains or summary measures. Other reasons could be differences in diabetes care and treatment or their development over time. Norris et al. [9] have also highlighted large differences among studies in a review published in 2011. Norris et al. suggest that the effect of type 2 diabetes on HRQOL might be underestimated because study samples often represent selected groups that are different from the largely heterogeneous type 2 diabetes population. Furthermore, Norris et al. question the use of previously published SF-36 norms for diabetes [9]. As suggested by many, it might also be speculated that the SF-36 is not specific enough with regard to diabetes [4, 9, 10, 23]. Our results add to this complexity based on large heterogeneous samples from a nationwide diabetes register. We found weak correlations between glycaemic control and HRQOL at the individual level. However, when the samples were divided into clinically relevant groups according to levels of glycaemic control, we found that adults with high-risk HbA1c levels have lower levels of HRQOL as measured by the SF-36 in both type 1 and type 2 diabetes.
While there are criticisms of the SF-36, Norris et al. [9] argue that it is important to continue to further research generic HRQOL in people with diabetes using this tool. Given continuous advances in diabetes care, including new medical treatments, technical aids for insulin administration and glucose monitoring, and support for self-management, research results on HRQOL in people with diabetes need to be continuously updated.
It is well known that a high HbA1c level is a risk factor for diabetes complications and death in people with type 1 diabetes and those with type 2 diabetes [36, 37]. In addition, generic HRQOL has been suggested to be a marker for mortality in people with diabetes [26–28]. Our findings show that among people with type 1 diabetes and those with type 2 diabetes, the group with a high-risk HbA1c level has a lower HRQOL. We suggest that the lower HRQOL is not explained by diabetes risk factors or complications, as the results persisted in the adjusted analyses. Our results strengthen the argument that we should focus on these high-risk groups to learn how to further improve their HRQOL and risk factor control. The weak associations on an individual level argues for the need to not focus exclusively on either glycaemic control or HRQOL but rather on both, because both are important parts of the complex life-long challenge of living with diabetes. Another observation is that there are still individuals with well-controlled HbA1c level that have low HRQOL scores, underlining the need to measure HRQOL. A central task for diabetes care and diabetes research is to provide suitable interventions that adequately can support adults with diabetes in their self-management, a desirable glycaemic control as well as a satisfying quality of life. However, the choice of suitable questionnaires to assess quality of life after interventions is a challenge because generic quality of life questionnaires, such as the SF-36, are probably less susceptible for effects on diabetes related problems [28, 38]. Despite that the diabetes care not always can intervene on non-diabetes-specific aspects of HRQOL, it is valuable to increase the awareness of quality of life as interventions related to HRQOL assessments might affect glycaemic control [1, 6, 7].
Limitations and strengths
Our study has limitations. Owing to the cross-sectional design, causal conclusions cannot be drawn. The analysis was limited to the responders, and the fact that the SF-36 was only offered in Swedish could had resulted in bias, as the proportion of foreign-born individuals might be higher among the non-responders than among the responders. While adding data from a heterogeneous sample, the wide range in age might be a limitation. Despite access to a number of diabetes-related variables, other comorbidities and various other variables not accounted for in our analyses might have influenced the results. The present analyses lack socio-economic data, which is a limitation we will address in future studies. Furthermore, the SF-36 might not capture important diabetes-specific aspects [4, 5, 9, 23]. While generic HRQOL measurements are important, we suggest that it is also important to focus on diabetes-specific aspects to be able to support person-centred care [31, 32, 39]. In our continued work, this is where our main focus will be. Future analyses on the diabetes-specific aspects will provide data on different subgroups, for example regarding age.
The strengths of this study are the updated, large, randomly selected, nationwide sample of people with type 1 diabetes and people with type 2 diabetes and the use of a well-known measure of HRQOL with evidence supporting its validity and reliability. Another strength is the access to clinical and demographic data for both responders and non-responders through the NDR. The responders were representative of the population in the NDR in 2015 for people with type 1 diabetes and those with type 2 diabetes (data on file). Given the 90% coverage rate of the NDR, the results can be deemed representative of the Swedish adult population with diabetes. Our study fills a gap by updating the scores of HRQOL in a broad sample of adults with type 1 and type 2 diabetes.
Conclusions
This study provides current data in a large nationwide randomly selected sample of adults with type 1 and type 2 diabetes. In people with type 1 diabetes and those with type 2 diabetes, adults with high-risk HbA1c levels have lower levels of HRQOL in most but not all domains of the SF-36v2. The largest differences between the high-risk group and the other two groups was seen in the GH domain for participants with type 1 diabetes and in the domains RP, GH and VT for participants with type 2 diabetes. This was not explained by demographics, other risk factors or diabetes complications. The weak individual-level correlations between HRQOL scores and levels of glycaemic control argues for the need to not focus exclusively on either HbA1c levels or HRQOL scores but rather on both because both are important parts of a complex, life-long, challenging condition.
Additional file
Table S1. Clinical and demographic characteristics for non-responders separated for type 1 and type 2 diabetes. Table S2. Least square mean estimates and 95% confidence intervals for SF-36v2 domains and summary measures in three glycated haemoglobin (HbA1c) groups for type 1 and type 2 diabetes. (PDF 190 kb)
Acknowledgements
Foremost, the authors wish to thank all study participants for making this research possible. In addition, we thank Ebba Linder, Mervete Miftaraj and Ann-Marie Svensson at Register Center Västra Götaland, Gothenburg for facilitating different parts of the study.
Abbreviations
- MCS
The Mental Component Summary measure
- BP
Bodily pain
- GH
General health
- HbA1c
Glycated haemoglobin
- HRQOL
Health-related quality of life
- MH
Mental health
- NDR
The Swedish National Diabetes Register
- PCS
The Physical Component Summary measure
- PF
Physical functioning
- RE
Role-emotional
- RP
Role-physical
- SF
Social functioning
- SF-36
A self-report questionnaire for generic health-related quality of life, the medical outcomes study health survey short form with 36 items
- SF-36v2
The SF-36 version 2
- VT
Vitality
Authors’ contributions
MSE made substantial contributions to the design of the work, applying for ethical approval and funding, interpreted the data and was the major contributor in writing and revising the manuscript. JL and UBJ supervised and made substantial contributions to the design of the work, applying for funding, made intellectual contributions in interpretation of the data, and in writing and revising the manuscript as well as contributed experience and knowledge from diabetes care and research in diabetes and health-related quality of life. SB made substantial contributions to the design of the work, made intellectual contributions in interpretation of the data, and in writing and revising the manuscript. BP made substantial contributions to the design of the work, performed the selection of the random sample, made intellectual contributions in interpretation of the data, and in writing and revising the manuscript as well as contributed statistical advice, experience and knowledge in the research of generic health-related quality of life. SF made substantial contributions to the design of the work, contributed substantial statistical advice, was the major contributor in analysing the data, made substantial intellectual contributions in interpretation of the data, and in writing and revising the manuscript. SG supervised and made substantial contributions to the design of the work, applying for ethical approval and funding, made intellectual contributions in interpretation of the data, and in writing and revising the manuscript as well as contributed medical experience and knowledge from diabetes care, diabetes research and research using health-care quality registers. KEO supervised and made substantial contributions to the design of the work, applying for ethical approval and funding, the generation of the SF-36v2 data, the interpretation of the data and in writing the manuscript as well as contributed medical experience and knowledge from diabetes care, diabetes research and research using health-care quality registers. All authors read and approved the final manuscript.
Funding
Financial support was received from Dalarna University, Falun; Uppsala University, Uppsala; the Sahlgrenska University Hospital, Gothenburg; the Swedish Diabetes Foundation; and the Sophiahemmet Foundation, Stockholm. Unrestricted grants were provided by Astra Zeneca, MSD, Novo Nordisk, and the Swedish state under the agreement between the Swedish government and the county councils, the ALF-agreement (No. ALFGBG-725311 and ALFGBG-698991). None of the funding providers has influenced the design of the study, the collection, analysis, or interpretation of data, or in writing the manuscript, or publication decision at any stage.
Availability of data and materials
The data that support the findings of this study are not publicly available. The study presented here have been subject to an application to an ethical board and approved for publication related to the specific aim of our research project. With reference to the European General Data Protection Regulation (GDPR), the data are personal data and thereby protected by secrecy.
Ethics approval and consent to participate
The study conforms to the Declaration of Helsinki and was approved by the Regional Ethical Review Board in Gothenburg, Sweden (No. 029–15, T600–15). Participants gave their informed consent.
Consent for publication
Not applicable.
Competing interests
SG has received personal fees (lecture fees and research grants) from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Merck Sharp & Dohme, Novo Nordisk, and Sanofi. KEO has received personal lecture fees from Eli Lilly and Abbott. The other authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial Care for People with diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(12):2126–2140. doi: 10.2337/dc16-2053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fisher L, Tang T, Polonsky W. Assessing quality of life in diabetes: I. a practical guide to selecting the best instruments and using them wisely. Diabetes Res Clin Pract. 2017;126:278–285. doi: 10.1016/j.diabres.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 3.Polonsky WH. Emotional and quality-of-life aspects of diabetes management. Curr Diab Rep. 2002;2(2):153–159. doi: 10.1007/s11892-002-0075-5. [DOI] [PubMed] [Google Scholar]
- 4.Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev. 1999;15(3):205–218. doi: 10.1002/(SICI)1520-7560(199905/06)15:3<205::AID-DMRR29>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 5.Luscombe FA. Health-related quality of life measurement in type 2 diabetes. Value Health. 2000;3(Suppl 1):15–28. doi: 10.1046/j.1524-4733.2000.36032.x. [DOI] [PubMed] [Google Scholar]
- 6.American Diabetes Association 4. Comprehensive medical evaluation and assessment of comorbidities: standards of medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S34–S45. doi: 10.2337/dc19-S004. [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association 5. Lifestyle management: standards of medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S46–S60. doi: 10.2337/dc19-S005. [DOI] [PubMed] [Google Scholar]
- 8.American Diabetes Association 6. Glycemic targets: standards of medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S61–S70. doi: 10.2337/dc19-S006. [DOI] [PubMed] [Google Scholar]
- 9.Norris SL, McNally TK, Zhang X, Burda B, Chan B, Chowdhury FM, et al. Published norms underestimate the health-related quality of life among persons with type 2 diabetes. J Clin Epidemiol. 2011;64(4):358–365. doi: 10.1016/j.jclinepi.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 10.Speight J, Reaney MD, Barnard KD. Not all roads lead to Rome—a review of quality of life measurement in adults with diabetes. Diabet Med. 2009;26:315–327. doi: 10.1111/j.1464-5491.2009.02682.x. [DOI] [PubMed] [Google Scholar]
- 11.The Diabetes Control and Complications Trial Research Group. Influence of intensive diabetes treatment on quality-of-life outcomes in the diabetes control and complications trial. Diabetes Care. 1996;19(3):195–203. 10.2337/diacare.19.3.195 [DOI] [PubMed]
- 12.Hart HE, Bilo HJ, Redekop WK, Stolk RP, Assink JH, Meyboom-de JB. Quality of life of patients with type I diabetes mellitus. Qual Life Res Int J Qual Life Asp Treat Care Rehab. 2003;12(8):1089–1097. doi: 10.1023/a:1026197119569. [DOI] [PubMed] [Google Scholar]
- 13.Lloyd CE, Orchard TJ. Physical and psychological well-being in adults with type 1 diabetes. Diabetes Res Clin Pract. 1999;44(1):9–19. doi: 10.1016/S0168-8227(99)00004-2. [DOI] [PubMed] [Google Scholar]
- 14.de Visser CL, Bilo HJ, Groenier KH, de Visser W, Jong M-d B. The influence of cardiovascular disease on quality of life in type 2 diabetics. Qual Life Res Int J Qual Life Asp Treat Care Rehab. 2002;11(3):249–261. doi: 10.1023/a:1015287825660. [DOI] [PubMed] [Google Scholar]
- 15.Kalda R, Ratsep A, Lember M. Predictors of quality of life of patients with type 2 diabetes. Patient Prefer Adherence. 2008;2:21–26. [PMC free article] [PubMed] [Google Scholar]
- 16.Kleefstra N, Ubink-Veltmaat LJ, Houweling ST, Groenier KH, Meyboom-de Jong B, Bilo HJ. Cross-sectional relationship between glycaemic control, hyperglycaemic symptoms and quality of life in type 2 diabetes (ZODIAC-2) Neth J Med. 2005;63(6):215–221. [PubMed] [Google Scholar]
- 17.Kuznetsov L, Griffin SJ, Davies MJ, Lauritzen T, Khunti K, Rutten GE, et al. Diabetes-specific quality of life but not health status is independently associated with glycaemic control among patients with type 2 diabetes: a cross-sectional analysis of the ADDITION-Europe trial cohort. Diabetes Res Clin Pract. 2014;104(2):281–287. doi: 10.1016/j.diabres.2013.12.029. [DOI] [PubMed] [Google Scholar]
- 18.Lloyd A, Sawyer W, Hopkinson P. Impact of long-term complications on quality of life in patients with type 2 diabetes not using insulin. Value Health. 2001;4(5):392–400. doi: 10.1046/j.1524-4733.2001.45029.x. [DOI] [PubMed] [Google Scholar]
- 19.Nicolucci A, Cucinotta D, Squatrito S, Lapolla A, Musacchio N, Leotta S, et al. Clinical and socio-economic correlates of quality of life and treatment satisfaction in patients with type 2 diabetes. Nutr Metab Cardiovasc Dis. 2009;19(1):45–53. doi: 10.1016/j.numecd.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 20.Weinberger M, Kirkman MS, Samsa GP, Cowper PA, Shortliffe EA, Simel DL, et al. The relationship between glycemic control and health-related quality of life in patients with non-insulin-dependent diabetes mellitus. Med Care. 1994;32(12):1173–1181. doi: 10.1097/00005650-199412000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Larsson D, Lager I, Nilsson PM. Socio-economic characteristics and quality of life in diabetes mellitus--relation to metabolic control. Scand J Public Health. 1999;27(2):101–105. doi: 10.1177/14034948990270020901. [DOI] [PubMed] [Google Scholar]
- 22.Nerenz DR, Repasky DP, Whitehouse FW, Kahkonen DM. Ongoing assessment of health status in patients with diabetes mellitus. Med Care. 1992;30(5 Suppl):MS112–MS124. doi: 10.1097/00005650-199205001-00010. [DOI] [PubMed] [Google Scholar]
- 23.Woodcock AJ, Julious SA, Kinmonth AL, Campbell MJ. Diabetes care from diagnosis group. Problems with the performance of the SF-36 among people with type 2 diabetes in general practice. Qual Life Res Int J Qual Life Asp Treat Care Rehab. 2001;10(8):661–670. doi: 10.1023/a:1013837709224. [DOI] [PubMed] [Google Scholar]
- 24.Fitzpatrick R, Bowling A, Gibbons E, Haywood K, Jenkinson C, Mackintosh A, et al. A structured review of patient-reported measures in relation to selected chronic conditions, perceptions of quality of care and carer impact National Centre for health outcomes development (Oxford site): unit of health-care epidemiology. Oxford: Department of Public Health, University of Oxford; 2006.
- 25.Gibbons E, Fitzpatrick R. Patient reported outcome measurement group. Oxford: A structured review of patient-reported outcome measures (PROMs) for diabetes: University of Oxford; 2009.
- 26.Kleefstra N, Landman GW, Houweling ST, Ubink-Veltmaat LJ, Logtenberg SJ, Meyboom-de Jong B, et al. Prediction of mortality in type 2 diabetes from health-related quality of life (ZODIAC-4) Diabetes Care. 2008;31(5):932–933. doi: 10.2337/dc07-2072. [DOI] [PubMed] [Google Scholar]
- 27.Landman GW, van Hateren KJ, Kleefstra N, Groenier KH, Gans RO, Bilo HJ. Health-related quality of life and mortality in a general and elderly population of patients with type 2 diabetes (ZODIAC-18) Diabetes Care. 2010;33(11):2378–2382. doi: 10.2337/dc10-0979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bjorner JB, Lyng Wolden M, Gundgaard J, Miller KA. Benchmarks for interpretation of score differences on the SF-36 health survey for patients with diabetes. Value Health. 2013;16(6):993–1000. doi: 10.1016/j.jval.2013.06.022. [DOI] [PubMed] [Google Scholar]
- 29.American Diabetes Association 7. Diabetes technology: standards of medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S71–S80. doi: 10.2337/dc19-S007. [DOI] [PubMed] [Google Scholar]
- 30.American Diabetes Association 9. Pharmacologic approaches to glycemic treatment: standards of medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S90–S102. doi: 10.2337/dc19-S009. [DOI] [PubMed] [Google Scholar]
- 31.Borg S, Eeg-Olofsson K, Palaszewski B, Svedbo Engstrom M, Gerdtham UG, Gudbjornsdottir S. Patient-reported outcome and experience measures for diabetes: development of scale models, differences between patient groups and relationships with cardiovascular and diabetes complication risk factors, in a combined registry and survey study in Sweden. BMJ Open. 2019;9(1):e025033. doi: 10.1136/bmjopen-2018-025033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Svedbo Engstrom M, Leksell J, Johansson UB, Eeg-Olofsson K, Borg S, Palaszewski B, et al. A disease-specific questionnaire for measuring patient-reported outcomes and experiences in the Swedish National Diabetes Register: development and evaluation of content validity, face validity, and test-retest reliability. Patient Educ Couns. 2018;101(1):139–146. doi: 10.1016/j.pec.2017.07.016. [DOI] [PubMed] [Google Scholar]
- 33.Maruish ME. User’s manual for the SF-36v2 health survey. 3. Lincoln: QualityMetric Incorporated; 2011. [Google Scholar]
- 34.Ware JE., Jr SF-36 health survey update. Spine. 2000;25(24):3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 35.Nathan DM, Cleary PA, Backlund JY, Genuth SM, Lachin JM, Orchard TJ, et al. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N Engl J Med. 2005;353(25):2643–2653. doi: 10.1056/NEJMoa052187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.American Diabetes Association 10. Cardiovascular disease and risk management: standards of medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S103–SS23. doi: 10.2337/dc19-S010. [DOI] [PubMed] [Google Scholar]
- 37.American Diabetes Association 11. Microvascular complications and foot care: standards of medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S124–SS38. doi: 10.2337/dc19-S011. [DOI] [PubMed] [Google Scholar]
- 38.Nair R, Kachan P. Outcome tools for diabetes-specific quality of life: study performed in a private family practice clinic. Can Fam Physician. 2017;63(6):e310–e3e5. [PMC free article] [PubMed] [Google Scholar]
- 39.Svedbo Engström Maria, Leksell Janeth, Johansson Unn-Britt, Gudbjörnsdottir Soffia. What is important for you? A qualitative interview study of living with diabetes and experiences of diabetes care to establish a basis for a tailored Patient-Reported Outcome Measure for the Swedish National Diabetes Register. BMJ Open. 2016;6(3):e010249. doi: 10.1136/bmjopen-2015-010249. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Clinical and demographic characteristics for non-responders separated for type 1 and type 2 diabetes. Table S2. Least square mean estimates and 95% confidence intervals for SF-36v2 domains and summary measures in three glycated haemoglobin (HbA1c) groups for type 1 and type 2 diabetes. (PDF 190 kb)
Data Availability Statement
The data that support the findings of this study are not publicly available. The study presented here have been subject to an application to an ethical board and approved for publication related to the specific aim of our research project. With reference to the European General Data Protection Regulation (GDPR), the data are personal data and thereby protected by secrecy.