Abstract
Background and aims
Cardiovascular outcome trials have documented a strong benefit of sodium glucose cotransporter-2 inhibitors (SGLT2i) on the risk of hospitalization for heart failure (HF) in patients with type 2 diabetes (T2D) with or without established cardiovascular disease or prior history of HF. The mechanisms, however, are not entirely clear. We aimed to evaluate whether treatment with SGLT2i affected cardiac function using impedance cardiography (ICG) in a randomized placebo-controlled trial.
Materials and methods
Thirty-three patients with T2D were randomized to receive blind dapagliflozin 10 mg or matching placebo for 12-week on top of their ongoing glucose lowering medication regimen. Cardiac function was evaluated by resting ICG at baseline and at the end of the 12-week treatment period. ICG is a non-invasive technology based on the continuous measurement of thoracic electrical conductivity to process a cardiodynamic parameters related to fluid content, blood flow, cardiac function, and circulatory function. We also evaluated changes in glycaemic control, blood pressure, and body weight.
Results
Thirty-one patients completed the study, 1 was excluded because ICG data was missing. Patients included in the final analysis were on average 63.4-year-old, with a known diabetes duration of 14.1 years and a baseline HbA1c of 8.2% (66 mmol/mol). 63.3% of patients had established cardiovascular disease (symptomatic or asymptomatic) and 36.7% had microangiopathy, but none had a prior history of HF. After 12 weeks, patients randomized to dapagliflozin, as compared to those randomized to placebo, showed improvements in HbA1c (− 1.2%; 13 mmol/mol), systolic blood pressure (− 3.7 mmHg), and body weight (− 3.3 kg). Based on ICG, in both groups, we detected no significant change in parameters of blood flow (stroke volume, cardiac output, cardiac index), systolic function (ejection fraction, acceleration and velocity indexes, systolic time ratio), circulatory function (systemic vascular resistance index), and fluid status (thoracic fluid content) after treatment.
Conclusion
This is the first study exploring cardiac effects of SGLT2i using ICG in T2D. We observed no change in cardiac function parameters estimated by ICG in T2D patients who received dapagliflozin versus placebo for 12 weeks.
Trial registration ClinicalTrial.gov NCT02327039. Registered 30 December 2014
Keywords: Type 2 diabetes, Sodium glucose cotransporter-2 inhibitor, Dapagliflozin, Heart failure, Impedance cardiography
Background
Patients with type 2 diabetes (T2D) have a two-to-fivefold increased risk of developing heart failure (HF) compare to non-diabetic patients [1]. This risk remains high despite control of known major cardiovascular risk factors [2]. HF is one of the first manifestations of T2D-related cardiovascular disease [3] and is one of the leading causes of hospitalizations in this population [4].
The presence of T2D negatively impacts HF outcomes. Patients with T2D are more likely to be hospitalized for HF [5], to be re-hospitalized for HF [6], and to experience a longer hospital stay [7] compared to patients without diabetes. Moreover, patients with T2D and HF have a higher risk of cardiovascular and all-cause mortality than HF patients without T2D [5].
Over the past decade, in patients with T2D, ischemic heart disease, and stroke mortality has declined, especially in men, but heart failure deaths did not change [8]. Therefore, therapeutic strategies able to reduce the HF risk are particularly appealing.
Sodium glucose co-transporter 2 inhibitors (SGLT2i) induce glycosuria, thereby reducing plasma glucose, blood pressure, and body weight [9]. The recent results of the four cardiovascular outcome trials (CVOTs) with SGLT2i have shown remarkable benefits in reducing HF hospitalization by about 30% in patients with T2D with or without established cardiovascular disease and also in patient with or without history of heart failure [10–13]. In addition, large retrospective studies confirmed that treatment with SGLT2i, when compared with other glucose-lowering medications (GLMs), was associated with lower rates of hospitalization for HF among patients with and without history of cardiovascular disease [14–16].
Several possible pathophysiological mechanisms for the protection exerted by SGLT2i on HF risk have been proposed [17], but not yet fully elucidated and mostly not confirmed in human studies.
In this study, we aimed to evaluate whether treatment with SGLT2i affected hemodynamic variables and cardiac function using impedance cardiography (ICG) in a randomized placebo-controlled trial.
ICG has been proposed as a non-invasive method of hemodynamic monitoring especially in critically ill and surgical patients [18]. ICG measures continuously the resistance (impedance) to the transmission of a low intensity electrical current through the chest. The changes in the resistance over time are proportional to the dynamic changes during each cardiac cycle. This allow the calculation of stroke volume (SV), cardiac output (CO) and other hemodynamic variables [19].
Materials and methods
Study design and participants
The study was approved by the Ethical Committee of the University Hospital of Padova and was conducted in accordance with the Declaration of Helsinki. All patients signed written informed consent. The trial was registered in ClinicalTrial.gov (NCT02327039). Patients were recruited between April 2015 and June 2016 at the diabetes outpatient clinic of the University Hospital of Padova. Eligible patients were randomly assigned (1:1) to one of 2 treatment groups, dapagliflozin 10 mg or matching placebo, on top of their GLMs for 12 weeks, based on a computer-generated sequence.
For safety reasons, the study was single blind meaning that patients, but not the clinical study staff, were unaware of the allocated treatment. However, the study staff in charge of the primary and secondary end-point evaluation was kept blind, thereby avoiding any interference on the study results. To guarantee concealment, pills and dispensers of dapagliflozin and placebo were identical.
Study details and the full eligibility criteria of the trial have been reported previously [20]. Briefly, inclusion criteria were: T2D patients aged 18 to 75 years, underlying therapy with oral GLMs and/or insulin. Major exclusion criteria were: acute illness or infection; recent surgery, trauma, or cardiovascular event; alcoholism; chronic liver disease; chronic kidney disease, defined as an estimated glomerular filtration rate (eGFR, calculated with CKD-EPI equation) < 60 mL/min/1.73 m2 [21]; HF New York Heart Association classes III to IV; history of hypotension or episodes of volume depletion/dehydration; previous history of recurrent urinary tract infections or genital infections; and pregnancy or lactation.
Diabetic retinopathy was defined based on digital fundus photography scored remotely by expert ophthalmologists and graded according to the Early Treatment of Diabetic Retinopathy Study (ETDRS) [22]. Somatic peripheral neuropathy was defined, after exclusion of non-diabetic causes, in the presence of typical sensory or motor symptoms (numbness, tingling, or pain in the toes, feet, legs, hands, arms, and fingers, or wasting of the muscles of the feet or hands), confirmed by clinical examination (ankle reflexes, vibratory perception threshold, pinprick, and 10-g monofilament sensitivity) and eventual determination of neural conduction velocity.
Coronary artery disease was defined as a history of myocardial infarction or angina, evidence of significant coronary artery disease at coronary angiography, or history of revascularization. History of HF was defined as a previous hospitalization for HF or clinical manifestations of HF. Echocardiographic abnormalities were evaluated according the current guidelines of American Society of Echocardiography/European Association of Cardiovascular Imaging [23, 24]. Systolic left ventricular (LV) dysfunction was defined as an ejection fraction < 40%. LV hypertrophy was defined by either an LV mass index of > 115 g/m2 for men and > 95 g/m2 for women indexed to body surface area. Diastolic LV disfunction was defined as recommended by the American Society of Echocardiography and the European Association of Cardiovascular Imaging [24, 25].
Peripheral arterial disease was defined as a history of claudication or rest pain, significant stenosis in leg arteries, or history of revascularization. Asymptomatic atherosclerosis was defined as the presence of carotid artery plaques (stenosis > 15%) at routine ultrasound examination.
The primary endpoint of the study was the change from baseline in cholesterol efflux capacity, which has been described previously [20]. ICG determination of cardiac function was an exploratory endpoint. At the beginning (before initiating randomized treatment) and at the end of the study (after 12 weeks of treatment) patients accessed the outpatient clinic and underwent a continuous ICG monitoring (Niccomo; Medis, Ilmenau, Germany) to record hemodynamic variables in a fasting condition for 20 min.
ICG
The ICG methodology used in this study was similar to that used in previous clinical studies [26, 27]. ICG is a non-invasive method based on the assumption that changes in intra-thoracic blood volume during the cardiac cycle induce changes in the electrical conductivity and impedance of the thorax and that these changes are mainly related to changes in aortic volume. The changes in the thoracic impedance are detected by electrodes assessing the difference between the applied voltage and the detected voltage after applying a small electrical continuous current through the thorax. Four couples of electrodes were placed at the neck and thorax of each subject to detect variations in thoracic bioimpedance. The system was coupled with a standard sphygmomanometer transducer that measured blood pressure at given intervals.
Measuring electrocardiogram (ECG) together with ICG, the left ventricular ejection time (LVET) was directly measured [28]. LV SV was calculated using the formula described by Sramek and Bernstein [29]. Thoracic fluid content (TFC) was calculated as 1000/baseline impedance.
The Medis Niccomo ICG device processed these changes with a dedicated algorithm (physiologic adaptive signal analysis) coupling impedance signal and waveform with ECG, noninvasively and continuously provided the following hemodynamic variables: heart rate (HR); systolic blood pressure (SBP), diastolic blood pressure (DBP); SV, stroke index [SI (SV normalized for body surface area)]; CO (SV × HR); cardiac index [CI (CO normalized for body surface area)]; ejection fraction (EF); acceleration index [AI (the maximum acceleration of blood flow in the aorta during systole)]; velocity index [VI (the peak velocity of blood flow in the aorta during systole)]; systolic time ratio (STR); LVET [the time interval between the opening and the closing of the aortic valve (i.e., mechanical systole)]; left cardiac work (LCW) and LCW index (LCWI), which reflected the myocardial oxygen demand; systemic vascular resistance [SVR (estimate of “afterload)] and SVR index [SVRI (SVR normalised to body size); TFC (indicator of chest fluid status); TFC Index [TFCI (TFC, normalized for body surface area)]; total arterial compliance [TAC (indicator of the degree of peripheral arterial stiffness/compliance)], TAC index, [TACI (TAC normalised to body size)];
ICG variables were calculated by using the mean of 2-min beat-to-beat values for 20 min. After completion of the study protocol, original ICG recordings were downloaded in a personal computer for off-line analysis.
Statistical analysis
Data are expressed as mean ± standard deviation if normal or as median (interquartile range) if not normal. Categorical variables are presented as numbers and percentages. Normality was checked using the Shapiro–Wilk test. Comparison between two groups were analyzed using the two-tailed unpaired Student’s t test for continuous variables and the χ2 test for categorical variables. For endpoints, we compared baseline with follow-up data using the two-tailed Wilcoxon rank test and calculated the change from baseline. Then, the changes from baseline in each group were compared using the two-tailed Mann–Whitney’s U test. Linear correlations were analyzed using the Pearson r coefficient. Statistical significance was accepted at p < 0.05 and SPSS version 22.0 was used.
Results
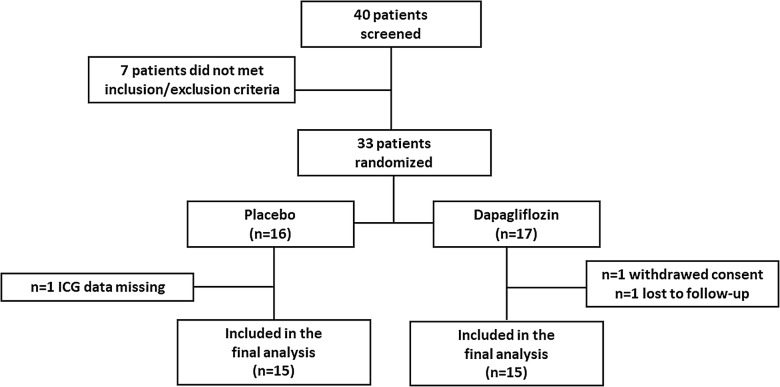
Thirty-three patients were enrolled in the study. Seventeen were assigned to dapagliflozin 10 mg, 16 to matching placebo. Two patients in the dapagliflozin group were excluded because they withdraw consent or were lost to follow-up, one patient in the placebo group was excluded because ICG data were missing, leaving 30 completers for the analysis, 15 in each group (Fig. 1).
Fig. 1.
Study flow-chart with number of patients screened, randomized and included in the final analysis
The baseline characteristics of the study population are summarized in Table 1. Patients were on average 63.7-year-old, with a known diabetes duration of 14.1 years and a baseline HbA1c of 8.2% (66 mmol/mol). The vast majority of patients (93.5%) were on metformin, 32.2% were on other oral GLMs, and 51.6% were concomitantly treated with insulin. 63.3% of patients had established cardiovascular disease (symptomatic or asymptomatic) and 35.4% had microangiopathy. No patient included in the study had a history of HF or a reduction of left ventricular ejection fraction. Almost half of the patients had LV hypertrophy (46.7%) and/or diastolic LV dysfunction (43.3%). After 12 weeks, dapagliflozin significantly reduced HbA1c by 0.9% and body weight by 3.1 kg. In the placebo group, HbA1c increased non-significantly by 0.4% and body weight remained stable (+ 0.2 kg).
Table 1.
Baseline characteristic of study patients
| Variable | All (n = 30) | Placebo (n = 15) | Dapagliflozin (n = 15) | p |
|---|---|---|---|---|
| Age, years | 63.4 ± 6.9 | 61.0 ± 7.2 | 65.7 ± 5.9 | 0.057 |
| Sex male, % | 66.7 | 66.7 | 66.7 | 1.000 |
| Body mass index, kg/m2 | 30.8 ± 5.2 | 32.8 ± 5.4 | 28.8 ± 4.3 | 0.032§ |
| HbA1c, % | 8.2 ± 0.8 | 8.2 ± 0.9 | 8.2 ± 0.6 | 0.981 |
| Diabetes duration, years | 14.1 ± 6.6 | 13.9 ± 5.2 | 14.2 ± 8.0 | 0.914 |
| Hypertension, % | 90.0 | 93.3 | 86.7 | 1.000 |
| Smoking habit, % | 16.7 | 20.0 | 13.3 | 1.000 |
| Dyslipidemia, % | 93.3 | 86.7 | 100 | 0.483 |
| Creatinine, mg/dl | 0.81 ± 0.2 | 0.81 ± 0.2 | 0.82 ± 0.2 | 0.921 |
| eGFR (ml/min/1.73 m2) | 90.6 ± 16.7 | 92.5 ± 16.9 | 88.7 ± 17.0 | 0.551 |
| Retinopathy, % | 26.7 | 33.3 | 20.0 | 0.682 |
| Nephropathy, % | 23.3 | 33.3 | 13.3 | 0.390 |
| Neuropathy, % | 3.3 | 6.7 | 0.0 | 1.000 |
| Coronary artery disease, % | 26.7 | 40.0 | 13.3 | 0.215 |
| History of HF or systolic LV dysfunction, % | 0.0 | 0.0 | 0.0 | 1.000 |
| LV hypertrophy, % | 46.7 | 53.3 | 40.0 | 0.715 |
| Diastolic LV disfunction, % | 43.3 | 46.7 | 40.0 | 1.000 |
| Peripheral arterial disease, % | 0.0 | 0.0 | 0.0 | 1.000 |
| Cerebrovascular disease, % | 56.7 | 53.3 | 60.0 | 1.000 |
| Metformin, % | 93.3 | 100 | 86.7 | 0.483 |
| Sulphonylureas, % | 20.0 | 20.0 | 20.0 | 1.000 |
| DPP-4 inhibitors, % | 20.0 | 13.3 | 26.7 | 0.651 |
| Basal insulin, % | 16.7 | 13.3 | 20.0 | 1.000 |
| Basal-bolus insulin, % | 36.7 | 46.7 | 26.7 | 0.500 |
| ACE inhibitors/ARBs, % | 83.3 | 86.7 | 80.0 | 1.000 |
| Diuretics, % | 33.3 | 26.7 | 40.0 | 0.700 |
| Calcium channel blockers, % | 30.0 | 33.3 | 26.7 | 1.000 |
| Beta blocker, % | 26.7 | 26.7 | 26.7 | 1.000 |
| Statins, % | 90.0 | 100.0 | 80.0 | 0.224 |
| Anti-platelets, % | 50.0 | 60.0 | 40.0 | 0.466 |
Data are expressed as mean ± standard, or percentages
§Not significant after correction of type I error
Compared with baseline, SBP declined by 4.7 ± 1.3 mmHg in the dapagliflozin group and by 1.0 ± 2.3 mmHg in the placebo group (p = 0.035). DBP declined by 1.3 ± 0.6 mmHg in the dapagliflozin group and by 0.4 ± 1.6 mmHg in the placebo group (p = 0.317) (Table 2).
Table 2.
Fluid content, blood flow, cardiac function, and circulatory function at baseline and at study end in the two groups
| Variable | Placebo (n = 15) | Dapagliflozin (n = 15) | p* | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Baseline | 12 weeks | Change | p | Baseline | 12 weeks | Change | p | ||
| HR (beats/min) | 68.6 (67.4; 78.3) | 72.4 (66.9; 76.3) | − 0.9 (− 4.4; 5.0) | 0.91 | 66.3 (61.1; 79.6) | 69.6 (64.1; 81.2) | 2.0 (− 3.1; 4.6) | 0.39 | 0.53 |
| SBP (mmHg) | 129.0 (118.9; 135.6) | 126.0 (118.1; 136.7) | 2.47 (− 9.3; 6.0) | 0.84 | 141.9 (133.4; 152.7) | 136.3 (130.1; 147.3) | − 7.40 (− 8.9; 1.5) | 0.03 | 0.04 |
| DBP (mmHg) | 76.1 (71.8; 81.4) | 77.7 (73.9; 82.1) | 2.3 (− 2.4; 4.6) | 0.31 | 81.9 (75.4; 87.5) | 82.0 (75.4; 84.7) | − 2.6 (− 3.8; 4.6) | 0.91 | 0.32 |
| SV (mL) | 98.9 (72.3; 113.6) | 85.7 (78.9; 100.8) | − 2.1 (− 16.6; 7.0) | 0.33 | 94.8 (81.2; 104.0) | 84.8 (70.3; 109.9) | − 7.8 (− 16.6; 14.4) | 0.50 | 0.92 |
| SI (mL/m2) | 48.0 (36.7; 51.7) | 42.9 (39.3; 44.7) | − 1.2 (− 8.2; 3.4) | 0.43 | 47.1 (38.7; 56.3) | 46.6 (39.2; 53.1) | − 3.3 (− 8.2; 7.4) | 0.61 | 0.76 |
| CO (L/min) | 6.63 (5.42; 7.97) | 6.31 (4.71; 7.98) | − 0.45 (− 0.79; 0.58) | 0.46 | 6.94 (5.62; 7.81) | 5.98 (5.52; 7.81) | − 0.49 (− 0.85; 1.06) | 0.87 | 0.49 |
| CI (L/min/m2) | 3.33 (2.86; 3.62) | 3.28 (2.47; 3.54) | − 0.21 (− 0.38; 0.29) | 0.50 | 3.49 (2.86; 3.79) | 3.45 (2.98; 3.66) | − 0.23 (− 0.37; 0.55) | 0.82 | 0.52 |
| EF (%) | 65.6 (60.8; 69.0) | 65.8 (62.3; 67.8) | 0.6 (− 1.3; 4.4) | 0.26 | 66.9 (61.5; 69.9) | 65.6 (60.4; 69.6) | − 0.3 (− 4.4; 2.8) | 0.43 | 0.19 |
| AI (/100/s2) | 47.6 (30.8; 53.6) | 43.1 (36.1; 50.9) | − 0.1 (− 5.8; 4.2) | 0.65 | 55.6 (39.8; 70.9) | 58.6 (41.2; 65.4) | − 2.9 (− 10.2; 5.4) | 0.39 | 0.85 |
| VI (/1000/s) | 33.1 (25.6; 42.4) | 29.9 (25.7; 40.5) | − 4.1 (− 6.4; 2.4) | 0.17 | 42.1 (35.4; 45.9) | 43.6 (31.6; 49.0) | 1.7 (− 3.0; 4.7) | 0.69 | 0.18 |
| STR | 0.29 (0.24; 0.37) | 0.28 (0.25; 0.34) | − 0.01 (− 0.07; 0.02) | 0.22 | 0.27 (0.22; 0.35) | 0.29 (0.23; 0.37) | 0.00 (− 0.05; 0.07) | 0.43 | 0.18 |
| LVET (ms) | 322.9 (311.7; 347.1) | 330.0 (300.0; 364.8) | 6.6 (− 10.4; 24.9) | 0.57 | 337.0 (294.6; 376.6) | 324.3 (298.8; 359.2) | 1.8 (− 31.2; 17.4) | 0.91 | 0.72 |
| LCW (kg/min) | 7.09 (6.18; 9.74) | 6.71 (5.59; 9.50) | − 0.16 (− 0.48; 0.52) | 0.89 | 9.30 (6.57; 9.82) | 7.50 (6.54; 9.68) | 0.44 (− 0.92; 1.05) | 0.96 | 0.85 |
| LCWI (kg × min × m−2) | 3.66 (3.20; 4.37) | 3.53 (2.90; 4.32) | − 0.08 (− 0.22; 0.26) | 0.98 | 4.48 (3.37; 4.58) | 4.12 (3.49; 4.93) | 0.23 (− 0.45; 0.57) | 0.82 | 0.77 |
| SVR (dyne × s × cm−5) | 924.0 (878.9; 1326.9) | 1030.9 (904.3; 1374.6) | 109.7 (− 76.6; 185.0) | 0.36 | 1116.0 (965.8; 1358.8) | 1157.3 (962.1; 1394.8) | 81.1 (− 190.5; 174.4) | 0.96 | 0.60 |
| SVRI (dyne × s × cm−5 × m−2) | 2051.9 (1770.6; 2581.4) | 2119.0 (1887.7; 2672.8) | 151.7 (− 150.86; 391.7) | 0.39 | 2162.1 (1953.4; 2494.4) | 2037.5 (1971.8; 2557.1) | 150.7 (− 437.4; 310.5) | 0.61 | 0.58 |
| TFC (k/Ohm) | 33.4 (29.0; 37.3) | 29.9 (27.7; 34.9) | − 0.86 (− 3.5; 0.6) | 0.16 | 31.4 (28.9; 35.1) | 31.6 (29.4; 36.3) | − 0.8 (− 1.6; 1.6) | 0.82 | 0.47 |
| TFCI (k/Ohm/m2) | 15.2 (13.5; 17.9) | 14.5 (12.8; 17.7) | − 0.3 (− 1.0; 0.2) | 0.28 | 15.7 (14.9; 17.6) | 15.6 (14.8; 18.1) | 0.0 (− 0.5; 0.4) | 0.86 | 0.35 |
| TAC (mL/mmHg) | 2.19 (1.65; 2.31) | 1.83 (1.38; 2.65) | 0.00 (− 0.39; 0.29) | 0.70 | 1.95 (1.2; 2.22) | 1.60 (1.19; 2.22) | 0.00 (− 0.20; 0.19) | 1.00 | 0.95 |
| TACI (mL/mmHg/m2) | 1.03 (0.78; 1.07) | 0.91 (0.71; 1.17) | 0.00 (− 0.18; 0.16) | 0.84 | 0.97 (0.72; 1.06) | 0.80 (0.68; 1.07) | 0.00 (− 0.09; 0.11) | 0.88 | 0.97 |
Data are expressed as median (interquartile range)
* p-values of comparison between changes observed in dapagliflozin group versus those in placebo group
At baseline, there was no significant difference in ICG parameters between the two groups. In both groups, comparing data recorded at end of treatment with dapagliflozin or placebo to those recorded at baseline, we detected no significant change in parameters of blood flow (stroke volume, stroke index, cardiac output, cardiac index), systolic function (ejection fraction, acceleration and velocity indexes, systolic time ratio, left ventricular ejection time), circulatory function (systemic vascular resistance and systemic vascular resistance index, total arterial compliance and total arterial compliance index), and fluid status (thoracic fluid content and thoracic fluid content index) (Table 2). ICG-derived STR has been recently validated as a marker of LV diastolic dysfunction defined using echocardiography, with an accuracy of 97% [30]. At baseline, diastolic dysfunction based on the STR cut-off of 0.31 was present in 63.3% of patients (66.7% in the dapagliflozin group and 60% in the placebo group). At follow-up, the prevalence of diastolic dysfunction based on STR declined by 6.7% in the dapagliflozin group and remained stable in the placebo group (p = 0.325).
No significant correlation was detected between change in HbA1c or body weight from baseline to the end of follow-up and change in ICG parameters (not shown). In the whole study cohort, TFC correlated directly with total body water evaluated by bioelectrical impedance analysis (BIA) (r = 0.49; p < 0.001), but the change in TFC was not correlated to the change in total body water (r = 0.14; p = 0.456).
Discussion
In this study, we found no significant effect of the SGLT2i dapagliflozin on measures of cardiac function evaluated by ICG. Since publication of the groundbreaking results of the EMPA-REG Outcome trial, the scientific community is struggling to understand the biological basis and the physiological mechanisms responsible for the cardiovascular benefits of SGLT2i, especially on HF.
Several possible pathophysiological mechanisms for the cardiovascular protection exerted by SGLT2i have been suggested, yet not formally proved. Briefly, these include reduction in preload, secondary to natriuresis and osmotic diuresis [31] and in afterload, secondary to reduction in blood pressure [32], myocardial Na+/H+ exchange inhibition [33, 34], reduction of necrosis and cardiac fibrosis [35, 36] and consequently of the development of HF. Reduction of inflammation and oxidative stress [37], restoration of the balance between pro- and anti-inflammatory adipokines and cytokine [38], reduction of epicardial adipose tissue mass [39] have been proposed as additional mechanisms. Moreover, the use of SGLT2i through an increased metabolism of free fatty acid and an increased production of ketone bodies may provide a more efficient source of energy for the myocardium [40].
Other possible mechanisms for the pleiotropic effects of SGLT2i on cardiovascular benefit involving the reduction of serum uric acid levels [41], haemoconcentration [42], improving endothelial function and aortic stiffness [43, 44] and may induce vasodilatation through activation of protein kinase G and the voltage-dependent K+ channel [45].
Some of these hypotheses result from studies in experimental models [33–37, 45] and should be confirmed in clinical studies, while other ones are just speculations [40] and require further research.
Despite all these mechanisms could contribute to protection against HF, information with respect to the direct effects of SGLT2i on myocardial function in humans is very limited. A small observational study showed that in patients with T2D and established cardiovascular disease, a short-term empagliflozin treatment was associated with a significant reduction in LV mass index and improved diastolic function measured by 2D echocardiography. No differences were found in LV systolic function, LV end diastolic volume, and LV end systolic volume [46]. Another observational study conducted in 37 patients with T2D with or without cardiovascular disease, showed that a treatment with canagliflozin improved LV diastolic function (E/e′ ratio) [47]. Similar results were found in a prospective observational study involving T2D with stable HF treated for 6 months with dapagliflozin [48]. However, these observational findings need to be confirmed in randomized controlled trials (RCTs). RCTs are currently being conducted to investigate the effects of SGLT2i on LV remodelling in patients with T2D and HF [49, 50]. Furthermore, large randomized-controlled trials investigating SGLT2i as a treatment for HF are ongoing and will enroll HF patients either with or without T2D, with reduced (DEFINE-HF, ClinicalTrial.gov registration no. NCT02653482) or preserved EF (PRESERVED-HF, ClinicalTrial.gov registration no. NCT03030235).
To the best of our knowledge, this is the first study exploring the cardiac effects of SGLT2i using ICG in T2D. This study suggests that, in T2D patients without a history of HF, a 12-week treatment with dapagliflozin exerted no overt effect on haemodynamic and cardiac function parameters compared to placebo. Power calculated a posteriori revealed that we could rule out an effect of dapagliflozin greater than 80 ms for LVET, 18 mL for SV (measures of systolic function) and 0.07 for STR.
Our data do not deny the strong protection provided by SGLT2i against the risk of HF, as demonstrated in solid and large CVOTs [10–13]. Rather, these negative findings may be attributed to several reasons that are at least in part related to study limitations. First, the observation time may be too short to detect changes in ICG parameters. However, in the 4 CVOTs with SGLT2i, the onset of the benefit in terms of reduction in HF hospitalization was very rapid. The curves started to separate in the first weeks after randomization, suggesting that diuretic or haemodynamic actions of SGLT2i could be at least in part responsible for the observed benefit.
Second, sample size may be too small to detect differences in ICG measures between the two groups of treatment. In fact, our study was designed to identify a significant change in the primary end-point, the effects of dapagliflozin compared to placebo on cholesterol efflux capacity [20] and power calculation was not performed based on ICG measurement variability. Thus, this exploratory re-analysis may be underpowered to detect significant changes in ICG parameters. Yet, in the same study, the analysis of body composition based on BIA clearly showed different effects of dapagliflozin versus placebo [20]. Therefore, we expected that the same sample size was sufficient to reveal overt effects of dapagliflozin on ICG, which is also based on impedance analysis. We detected a direct correlation between total body water and TFC, suggesting concordance of the two methods. Interestingly, while dapagliflozin reduced total body water by about 2.5 L [20], we herein found no change in TFC, suggesting that volume reduction occurred mainly in extra-thoracic compartments.
Furthermore, we recorded no parameter directly related to diastolic function. Although generally considered a measure of contractility, STR (the ratio between electric and mechanical systole) has a high accuracy for the diagnosis of diastolic dysfunction [30]. We found no effects of dapagliflozin on STR, either continuous or categorized according to the recommended cut-off [30], but we acknowledge that other parameters of diastolic function should be evaluated. Previous observational studies documented effects of SGLT2i on diastolic cardiac function in T2D, but a recent re-analysis of the DECLARE-TIMI58 study reported that dapagliflozin prevented HF in patients with a normal or reduced EF and improved survival especially in patients with reduced EF [51]. Thus, a selective effect of SGLT2i on diastolic function is unlikely to explain the observed benefit on HF rates.
Finally, the use of ICG for evaluation of cardiac variables has provided conflicting results in terms of reliability: studies comparing ICG with other methods to measure cardiac and hemodynamic parameters showed an agreement ranging from good [52–54] to poor [55, 56]. In addition, it should be mentioned that ICG is based on thoracic impedance triggering on cardiac cycle, from which all other measures are derived. Since SGLT2i typically reduce body fluid [57], it is also possible that the resulting change in impedance, that we have already demonstrated with BIA [20], masked the effects on cardiac function and hemodynamic parameters.
Conclusions
Despite strong evidence that SGLT2i prevent HF in T2D with or without prior HF episodes, we found no effects of dapagliflozin on parameters of cardiac function measured by ICG. Short duration of treatment, small sample size, lack or specific diastolic function measures, limited correlation of ICG parameters with gold standard examination of cardiac function, and the masking diuretic effects of SGLT2i are all possible explanations of these negative results. In the end, we also speculate that SGLT2i exert no effects on cardiac function parameters in patients with normal cardiac function but may play a major role at the very early onset of cardiac disfunction, preventing hospitalization and mortality. Further studies are needed to address this hypothesis.
Acknowledgements
None.
Abbreviations
- AI
acceleration index
- ARB
angiotensin receptor blockers
- BIA
bioelectrical impedance analysis
- CI
cardiac index
- CO
cardiac output
- CVOTs
cardiovascular outcome trials
- DBP
diastolic blood pressure
- DPP4
dipeptidyl peptidase-4
- ACE
angiotensin-converting enzyme
- EF
ejection fraction
- eGFR
estimated glomerular filtration rate
- GLMs
glucose-lowering medications
- HF
heart failure
- HR
heart rate
- ICG
impedance cardiography
- LCW
left cardiac work
- LCWI
left cardiac work index
- LV
left ventricular
- LVET
left ventricular ejection time
- RCTs
randomized-controlled trials
- SBP
systolic blood pressure
- SGLT2i
sodium glucose cotransporter-2 inhibitors
- SI
stroke index
- STR
systolic time ratio
- SV
stroke volume
- SVR
systemic vascular resistance
- SVRI
systemic vascular resistance
- T2D
type 2 diabetes
- TAC
total arterial compliance
- TACI
total arterial compliance index
- TFC
thoracic fluid content
- TFCI
thoracic fluid content index
- VI
velocity index
Authors’ contributions
BMB, study conduction, data collection, analysis and interpretation, manuscript writing. GPF, study design and conduction, data analysis and interpretation, manuscript writing. SVDK, study design, data analysis and interpretation, manuscript revision. AA, study design, data analysis and interpretation, manuscript revision. All authors read and approved the final manuscript.
Funding
The study was supported by a Grant from AstraZeneca (ESR-14-10088) to AA. The sponsor had no role in study design and conduction, data analysis and interpretation, and final decision to publish.
Availability of data and materials
Original data used to generate the present analysis can be obtained from the corresponding author upon reasonable request.
Ethics approval and consent to participate
The study was approved by the Ethical Committee of the University Hospital of Padova (No. 3302/AO/14). All participants signed a written informed consent.
Consent for publication
Not applicable.
Competing interests
B.M.B. received lecture or advisory board fees from Astra Zeneca, Eli Lilly, Boehringer Ingelheim, Novo Nordisk and Novartis, G.P.F. received grant support, lecture fees, or advisory board fees from AstraZeneca, Boehringer Ingelheim, Eli Lilly, Novo Nordisk, Sanofi, Genzyme, Abbott, Novartis, and Merck Sharp & Dohme. A.A. received research grants, lecture fees, or advisory board fees from Merck Sharp & Dome, AstraZeneca, Novartis, Boeringher Ingelheim, Sanofi, Mediolanum, Janssen, Novo Nordisk, Eli Lilly, Servier, and Takeda. The remaining authors have nothing to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kannel WB, Hjortland M, Castelli WP. Role of diabetes in congestive heart failure: the Framingham study. Am J Cardiol. 1974;34:29–34. doi: 10.1016/0002-9149(74)90089-7. [DOI] [PubMed] [Google Scholar]
- 2.Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, Svensson A-M, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018;379:633–644. doi: 10.1056/NEJMoa1800256. [DOI] [PubMed] [Google Scholar]
- 3.Shah AD, Langenberg C, Rapsomaniki E, Denaxas S, Pujades-Rodriguez M, Gale CP, et al. Type 2 diabetes and incidence of cardiovascular diseases: a cohort study in 1.9 million people. Lancet Diabetes Endocrinol. 2015;3:105–113. doi: 10.1016/S2213-8587(14)70219-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seferović PM, Petrie MC, Filippatos GS, Anker SD, Rosano G, Bauersachs J, et al. Type 2 diabetes mellitus and heart failure: a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018;20:853–872. doi: 10.1002/ejhf.1170. [DOI] [PubMed] [Google Scholar]
- 5.MacDonald MR, Petrie MC, Varyani F, Östergren J, Michelson EL, Young JB, et al. Impact of diabetes on outcomes in patients with low and preserved ejection fraction heart failure: an analysis of the Candesartan in Heart failure: Assessment of Reduction in Mortality and morbidity (CHARM) programme. Eur Heart J. 2008;29:1377–1385. doi: 10.1093/eurheartj/ehn153. [DOI] [PubMed] [Google Scholar]
- 6.Targher G, Dauriz M, Laroche C, Temporelli PL, Hassanein M, Seferovic PM, et al. In-hospital and 1-year mortality associated with diabetes in patients with acute heart failure: results from the ESC-HFA Heart Failure Long-Term Registry. Eur J Heart Fail. 2017;19:54–65. doi: 10.1002/ejhf.679. [DOI] [PubMed] [Google Scholar]
- 7.Kapoor JR, Fonarow GC, Zhao X, Kapoor R, Hernandez AF, Heidenreich PA. Diabetes, quality of care, and in-hospital outcomes in patients hospitalized with heart failure. Am Heart J. 2011;162(480–486):e3. doi: 10.1016/j.ahj.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 8.Cheng YJ, Imperatore G, Geiss LS, Saydah SH, Albright AL, Ali MK, et al. Trends and disparities in cardiovascular mortality among U.S. adults with and without self-reported diabetes, 1988–2015. Diabetes Care. 2018;41:2306–2315. doi: 10.2337/dc18-0831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomas MC, Cherney DZI. The actions of SGLT2 inhibitors on metabolism, renal function and blood pressure. Diabetologia. 2018;61:2098–2107. doi: 10.1007/s00125-018-4669-0. [DOI] [PubMed] [Google Scholar]
- 10.Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–2128. doi: 10.1056/NEJMoa1504720. [DOI] [PubMed] [Google Scholar]
- 11.Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:644–657. doi: 10.1056/NEJMoa1611925. [DOI] [PubMed] [Google Scholar]
- 12.Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380:347–357. doi: 10.1056/NEJMoa1812389. [DOI] [PubMed] [Google Scholar]
- 13.Perkovic V, Jardine MJ, Neal B, Bompoint S, Heerspink HJL, Charytan DM, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–2306. doi: 10.1056/NEJMoa1811744. [DOI] [PubMed] [Google Scholar]
- 14.Birkeland KI, Jørgensen ME, Carstensen B, Persson F, Gulseth HL, Thuresson M, et al. Cardiovascular mortality and morbidity in patients with type 2 diabetes following initiation of sodium-glucose co-transporter-2 inhibitors versus other glucose-lowering drugs (CVD-REAL Nordic): a multinational observational analysis. Lancet Diabetes Endocrinol. 2017;5:709–717. doi: 10.1016/S2213-8587(17)30258-9. [DOI] [PubMed] [Google Scholar]
- 15.Elisabetta P, Ajinkya P, Mehdi N, Anouk D-L, et al. Empagliflozin and the Risk of heart failure hospitalization in routine clinical care: a first analysis from the empagliflozin comparative Effectiveness and Safety (EMPRISE) Study. Circulation. 2019;139:2822–2830. doi: 10.1161/CIRCULATIONAHA.118.039177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kosiborod M, Cavender MA, Fu AZ, Wilding JP, Khunti K, Holl RW, et al. Lower Risk of heart failure and death in patients initiated on sodium-glucose cotransporter-2 inhibitors versus other glucose-lowering drugs: the CVD-REAL study. Circulation. 2017;136:249–259. doi: 10.1161/CIRCULATIONAHA.117.029190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Verma S, McMurray JJV. SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review. Diabetologia. 2018;61:2108–2117. doi: 10.1007/s00125-018-4670-7. [DOI] [PubMed] [Google Scholar]
- 18.Fellahi J-L, Fischer M-O. Electrical bioimpedance cardiography: an old technology with new hopes for the future. J Cardiothorac Vasc Anesth. 2014;28:755–760. doi: 10.1053/j.jvca.2013.12.026. [DOI] [PubMed] [Google Scholar]
- 19.Woltjer HH, Bogaard HJ, De Vries PMJM. The technique of impedance cardiography. Eur Heart J. 1997;18:1396–1403. doi: 10.1093/oxfordjournals.eurheartj.a015464. [DOI] [PubMed] [Google Scholar]
- 20.Fadini GP, Bonora BM, Zatti G, Vitturi N, Iori E, Marescotti MC, et al. Effects of the SGLT2 inhibitor dapagliflozin on HDL cholesterol, particle size, and cholesterol efflux capacity in patients with type 2 diabetes: a randomized placebo-controlled trial. Cardiovasc Diabetol. 2017;16:42. doi: 10.1186/s12933-017-0529-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Early Treatment Diabetic Retinopathy Study Research Group A new equation to estimate glomerular filtration rate development and comparison of a new equation to estimate GFR. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Early TDRSRG Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie house classification. Ophthalmology. 2013;98:786–806. [PubMed] [Google Scholar]
- 23.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the american society of echocardiography and the european association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging. 2015;16:233–271. doi: 10.1093/ehjci/jev014. [DOI] [PubMed] [Google Scholar]
- 24.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, III, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the american society of echocardiography and the european association of cardiovascular imaging. Eur Heart J Cardiovasc Imaging. 2016;17:1321–1360. doi: 10.1093/ehjci/jew082. [DOI] [PubMed] [Google Scholar]
- 25.Machino-Ohtsuka T, Seo Y, Ishizu T, Hamada-Harimura Y, Yamamoto M, Sato K, et al. Clinical utility of the 2016 ASE/EACVI recommendations for the evaluation of left ventricular diastolic function in the stratification of post-discharge prognosis in patients with acute heart failure. Eur Heart J Cardiovasc Imaging. 2019 doi: 10.1093/ehjci/jez082. [DOI] [PubMed] [Google Scholar]
- 26.Packer M, Abraham WT, Mehra MR, Yancy CW, Lawless CE, Mitchell JE, et al. Utility of impedance cardiography for the identification of short-term risk of clinical decompensation in stable patients with chronic heart failure. J Am Coll Cardiol. 2006;47:2245–2252. doi: 10.1016/j.jacc.2005.12.071. [DOI] [PubMed] [Google Scholar]
- 27.Vigili de Kreutzenberg S, Fadini GP, Boscari F, Rossi E, Guerra S, Sparacino G, et al. Impaired hemodynamic response to meal intake in insulin-resistant subjects: an impedance cardiography approach. Am J Clin Nutr. 2011;93:926–933. doi: 10.3945/ajcn.110.003582. [DOI] [PubMed] [Google Scholar]
- 28.Summers RL, Shoemaker WC, Peacock WF, Ander DS, Coleman TG. Bench to bedside: electrophysiologic and clinical principles of noninvasive hemodynamic monitoring using impedance cardiography. Acad Emerg Med. 2003;10:669–680. doi: 10.1111/j.1553-2712.2003.tb00054.x. [DOI] [PubMed] [Google Scholar]
- 29.Bernstein DP. A new stroke volume equation for thoracic electrical bioimpedance: theory and rationale. Crit Care Med. 1986;14:904–909. doi: 10.1097/00003246-198610000-00017. [DOI] [PubMed] [Google Scholar]
- 30.Nazário Leão R, Marques Silva P, Branco L, Fonseca H, Bento B, Alves M, et al. Systolic time ratio measured by impedance cardiography accurately screens left ventricular diastolic dysfunction in patients with arterial hypertension. Clin Hypertens. 2017;23:28. doi: 10.1186/s40885-017-0084-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Perkins BA, Udell JA, Cherney DZI. No need to sugarcoat the message: is cardiovascular risk reduction from SGLT2 inhibition related to natriuresis? Am J Kidney Dis. 2016;68:349–352. doi: 10.1053/j.ajkd.2016.03.410. [DOI] [PubMed] [Google Scholar]
- 32.Baker WL, Smyth LR, Riche DM, Bourret EM, Chamberlin KW, White WB. Effects of sodium-glucose co-transporter 2 inhibitors on blood pressure: a systematic review and meta-analysis. J Am Soc Hypertens. 2014;8(262–275):e9. doi: 10.1016/j.jash.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 33.Baartscheer A, Schumacher CA, Wüst RCI, Fiolet JWT, Stienen GJM, Coronel R, et al. Empagliflozin decreases myocardial cytoplasmic Na+ through inhibition of the cardiac Na+/H+ exchanger in rats and rabbits. Diabetologia. 2017;60:568–573. doi: 10.1007/s00125-016-4134-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Uthman L, Baartscheer A, Bleijlevens B, Schumacher CA, Fiolet JWT, Koeman A, et al. Class effects of SGLT2 inhibitors in mouse cardiomyocytes and hearts: inhibition of Na(+)/H(+) exchanger, lowering of cytosolic Na(+) and vasodilation. Diabetologia. 2018;61:722–726. doi: 10.1007/s00125-017-4509-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lee T-M, Chang N-C, Lin S-Z. Dapagliflozin, a selective SGLT2 Inhibitor, attenuated cardiac fibrosis by regulating the macrophage polarization via STAT3 signaling in infarcted rat hearts. Free Radic Biol Med. 2017;104:298–310. doi: 10.1016/j.freeradbiomed.2017.01.035. [DOI] [PubMed] [Google Scholar]
- 36.Li C, Zhang J, Xue M, Li X, Han F, Liu X, et al. SGLT2 inhibition with empagliflozin attenuates myocardial oxidative stress and fibrosis in diabetic mice heart. Cardiovasc Diabetol. 2019;18:15. doi: 10.1186/s12933-019-0816-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tahara A, Kurosaki E, Yokono M, Yamajuku D, Kihara R, Hayashizaki Y, et al. Effects of sodium-glucose cotransporter 2 selective inhibitor ipragliflozin on hyperglycaemia, oxidative stress, inflammation and liver injury in streptozotocin-induced type 1 diabetic rats. J Pharm Pharmacol. 2014;66:975–987. doi: 10.1111/jphp.12223. [DOI] [PubMed] [Google Scholar]
- 38.Garvey WT, Van Gaal L, Leiter LA, Vijapurkar U, List J, Cuddihy R, et al. Effects of canagliflozin versus glimepiride on adipokines and inflammatory biomarkers in type 2 diabetes. Metabolism. 2018;85:32–37. doi: 10.1016/j.metabol.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 39.Sato T, Aizawa Y, Yuasa S, Kishi S, Fuse K, Fujita S, et al. The effect of dapagliflozin treatment on epicardial adipose tissue volume. Cardiovasc Diabetol. 2018;17:6. doi: 10.1186/s12933-017-0658-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ferrannini E, Mark M, Mayoux E. CV protection in the EMPA-REG OUTCOME Trial: a “Thrifty Substrate” hypothesis. Diabetes Care. 2016;39:1108–1114. doi: 10.2337/dc16-0330. [DOI] [PubMed] [Google Scholar]
- 41.Bailey CJ. Uric acid and the cardio-renal effects of SGLT2 inhibitors. Diabetes Obes Metab. 2019;21:1291–1298. doi: 10.1111/dom.13670. [DOI] [PubMed] [Google Scholar]
- 42.Lambers Heerspink HJ, de Zeeuw D, Wie L, Leslie B, List J. Dapagliflozin a glucose-regulating drug with diuretic properties in subjects with type 2 diabetes. Diabetes Obes Metab. 2013;15:853–862. doi: 10.1111/dom.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Solini A, Giannini L, Seghieri M, Vitolo E, Taddei S, Ghiadoni L, et al. Dapagliflozin acutely improves endothelial dysfunction, reduces aortic stiffness and renal resistive index in type 2 diabetic patients: a pilot study. Cardiovasc Diabetol. 2017;16:138. doi: 10.1186/s12933-017-0621-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chilton R, Tikkanen I, Cannon CP, Crowe S, Woerle HJ, Broedl UC, et al. Effects of empagliflozin on blood pressure and markers of arterial stiffness and vascular resistance in patients with type 2 diabetes. Diabetes Obes Metab. 2015;17:1180–1193. doi: 10.1111/dom.12572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li H, Shin SE, Seo MS, An JR, Choi I-W, Jung W-K, et al. The anti-diabetic drug dapagliflozin induces vasodilation via activation of PKG and Kv channels. Life Sci. 2018;197:46–55. doi: 10.1016/j.lfs.2018.01.032. [DOI] [PubMed] [Google Scholar]
- 46.Verma S, Rawat S, Ho KL, Wagg CS, Zhang L, Teoh H, et al. Empagliflozin Increases cardiac energy production in diabetes: novel translational insights into the heart failure benefits of SGLT2 inhibitors. JACC Basic to Transl Sci. 2018;3:575–587. doi: 10.1016/j.jacbts.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Matsutani D, Sakamoto M, Kayama Y, Takeda N, Horiuchi R, Utsunomiya K. Effect of canagliflozin on left ventricular diastolic function in patients with type 2 diabetes. Cardiovasc Diabetol. 2018;17:73. doi: 10.1186/s12933-018-0717-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Soga F, Tanaka H, Tatsumi K, Mochizuki Y, Sano H, Toki H, et al. Impact of dapagliflozin on left ventricular diastolic function of patients with type 2 diabetic mellitus with chronic heart failure. Cardiovasc Diabetol. 2018;17:132. doi: 10.1186/s12933-018-0775-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Singh JSS, Fathi A, Vickneson K, Mordi I, Mohan M, Houston JG, et al. Research into the effect Of SGLT2 inhibition on left ventricular remodelling in patients with heart failure and diabetes mellitus (REFORM) trial rationale and design. Cardiovasc Diabetol. 2016;15:97. doi: 10.1186/s12933-016-0419-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Natali A, Nesti L, Fabiani I, Calogero E, Di Bello V. Impact of empagliflozin on subclinical left ventricular dysfunctions and on the mechanisms involved in myocardial disease progression in type 2 diabetes: rationale and design of the EMPA-HEART trial. Cardiovasc Diabetol. 2017;16:130. doi: 10.1186/s12933-017-0615-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kato ET, Silverman MG, Mosenzon O, Zelniker TA, Cahn A, Furtado RHM, Kuder J, Murphy SA, Bhatt DL, Leiter LA, McGuire DK, Wilding JPH, Bonaca MP, Ruff CT, Desai AS, Goto S, Johansson PA, Gause-Nilsson I, Johanson P, Langkilde AM, Raz I, Sabatine MS, Wiviott SD. Effect of dapagliflozin on heart failure and mortality in type 2 diabetes mellitus. Circulation. 2019;28(139):2528–2536. doi: 10.1161/CIRCULATIONAHA.119.040130. [DOI] [PubMed] [Google Scholar]
- 52.Blohm ME, Obrecht D, Hartwich J, Mueller GC, Kersten JF, Weil J, et al. Impedance cardiography (electrical velocimetry) and transthoracic echocardiography for non-invasive cardiac output monitoring in pediatric intensive care patients: a prospective single-center observational study. Crit Care. 2014;18:603. doi: 10.1186/s13054-014-0603-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schmidt C, Theilmeier G, Van Aken H, Korsmeier P, Wirtz SP, Berendes E, et al. Comparison of electrical velocimetry and transoesophageal Doppler echocardiography for measuring stroke volume and cardiac output. Br J Anaesth. 2005;95:603–610. doi: 10.1093/bja/aei224. [DOI] [PubMed] [Google Scholar]
- 54.Zhang H, Li JK. Noninvasive monitoring of transient cardiac changes with impedance cardiography. Cardiovasc Eng. 2008;8:225–231. doi: 10.1007/s10558-008-9062-z. [DOI] [PubMed] [Google Scholar]
- 55.Borzage M, Heidari K, Chavez T, Seri I, Wood JC, Blüml S. Measuring stroke volume: impedance cardiography vs phase-contrast magnetic resonance imaging. Am J Crit Care. 2017;26:408–415. doi: 10.4037/ajcc2017488. [DOI] [PubMed] [Google Scholar]
- 56.Kieback AG, Borges AC, Schink T, Baumann G, Laule M. Impedance cardiography versus invasive measurements of stroke volume index in patients with chronic heart failure. Int J Cardiol. 2010;143:211–223. doi: 10.1016/j.ijcard.2008.11.201. [DOI] [PubMed] [Google Scholar]
- 57.Hirose S, Nakajima S, Iwahashi Y, Seo A, Takahashi T, Tamori Y. Impact of the 8-week administration of tofogliflozin for glycemic control and body composition in japanese patients with type 2 diabetes mellitus. Intern Med. 2016;55:3239–3245. doi: 10.2169/internalmedicine.55.6367. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Original data used to generate the present analysis can be obtained from the corresponding author upon reasonable request.