Abstract
Objectives
ABO blood groups have been shown to be associated with different diseases. Very few studies have attempted to detect the association of ABO blood groups with obesity. The goal of this study is to find any potential relation between ABO blood groups and high body mass index (BMI) among a Saudi population, which may contribute to underlying genetic disorders.
Methods
A cross-sectional descriptive study was conducted using a structured questionnaire that contained general demographic data, including weight, height, type of ABO blood group and the participants' opinion, to determine the association between the ABO blood groups and obesity.
Results
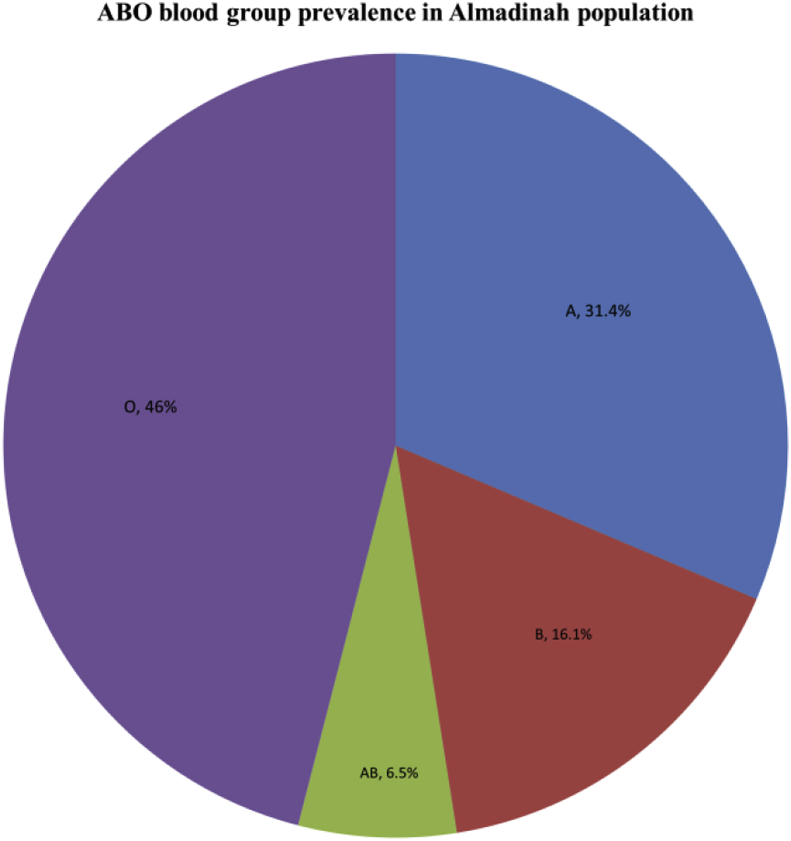
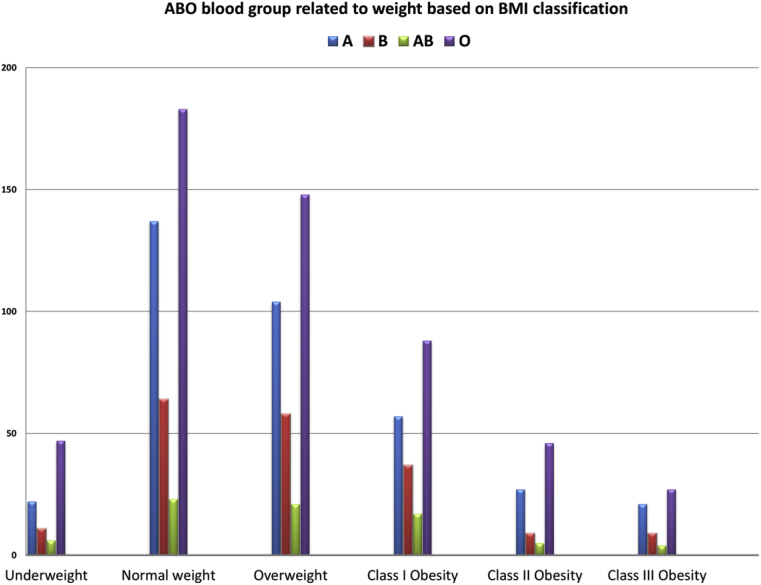
Our study included 1171 participants, including 596 (50.9%) women. A plurality of participants' ages (47%) was between 15 and 25 years. The prevalence of obesity was 35.7% in men and 20.3% in women, while the prevalence of overweight was 30% in men and 25.3% in women. Blood group O was reported to be the most common blood group (46%), followed by blood group A (31.4%), while blood groups B and AB were found in 16.1% and 6.5% of participants, respectively. The prevalence of obesity (BMI ≥ 30) among participants based on blood group O, A, B, and AB was 13.7%, 9%, 4.8%, and 2.2%, respectively. There was no statistically significant difference between the prevalence of obesity or high BMI and ABO blood groups.
Conclusion
Overall, our study did not show a significant relation between overweight and obesity and ABO blood groups. However, the elevation of the prevalence of overweight and obesity, mainly among the younger generations of the Saudi population, requires more awareness and educational programs.
Keywords: ABO blood groups, BMI, Body mass index, Obesity, Overweight
الملخص
أهداف البحث
أظهرت بعض الدراسات أن هناك ارتباطا بين فصيلة الدم وبعض الأمراض. وقد أجريت دراسات قليلة جدا حاولت الكشف عن ارتباط بين فصيلة الدم والسمنة وبنتائج غير مؤكدة. الهدف من هذه الدراسة هو العثور على أي علاقة محتملة بين فصائل الدم ومؤشر كتلة الجسم المرتفع بين السكان السعوديين والتي قد تسهم في اضطرابات جينية كامنة.
طرق البحث
أُجريت دراسة وصفية مقطعية باستخدام استبانة منظمة تحتوي على بيانات ديموغرافية عامة، ووزن، وطول، وفصيلة دم المشاركين، ورأيهم حول الارتباط بين فصيلة الدم والبدانة.
النتائج
شملت دراستنا ١١٧١ مشاركا بما في ذلك ٥٩٦ (٥٠.٩٪) امرأة. وكانت غالبية أعمار المشاركين (٤٧٪) بين ١٥ و٢٥ سنة. كانت نسبة انتشار السمنة ٣٥.٧٪ في الرجال و٢٠.٣٪ في النساء، في حين كانت نسبة انتشار زيادة الوزن٣٠٪ في الرجال و٢٥.٣٪ في النساء. سُجلت فصيلة الدم O على أنها الأكثر انتشارا (٤٦٪)، تليها فصيلة الدم A (٪٣١.٤) في حين شكلت فصائل دم B و AB١٦.١٪ و٦.٥٪ على التوالي.و كانت نسبة انتشار السمنة (مؤشر كتلة الجسم < أو = ٣٠) بين المشاركين بناءً على فصيلة الدم O وA وB وAB ١٣.٧٪ و٩٪ و٤.٨٪ و٢.٢٪ على التوالي. ولم يكن هناك فرق ذو دلالة إحصائية بين نسبة انتشار السمنة أو ارتفاع مؤشر كتلة الجسم وفصائل الدم.
الاستنتاجات
عموما، لم تُظهر دراستنا علاقة ذات قيمة بين زيادة الوزن والسمنة وبين فصيلة الدم. على الرغم من ذلك، فإن ارتفاع نسبة الإصابة بزيادة الوزن والبدانة، وخاصة بين الأجيال الشابة من السكان السعوديين تتطلب المزيد من الوعي والبرامج التعليمية.
الكلمات المفتاحية: السمنة, زيادة الوزن, مؤشر كتلة الجسم, فصيلة الدم
Introduction
Obesity is related to abnormal or excessive fat accumulation in the body, which may impair health. Obesity has been classified according to a specifically calculated index called the body mass index (BMI); it is a simple weight-for-height index that is defined as a person's weight in kilogrammes divided by the square of his or her height in metres (kg/m2).1 Based on the WHO classification for obesity in adults, a BMI between 25 and 29.9 is considered to be overweight, and a BMI ≥30 is considered to be obese.1, 2 Thirteen percent of the world's adult population (11% of men and 15% of women) were obese in 2014 and 39% of adults were overweight.1 According to the National Nutrition Survey in 2007, the prevalence of obesity in KSA was 23.6% in women and 14% in men, and the prevalence of overweight in the community was determined to be 30.7% for men compared to 28.4% for the women.3 Obesity is a major risk factor for a group of diseases and death.4, 5 Recognition of the role of an elevated BMI in different developing countries has made obesity and its underlying factors a high priority for health authorities worldwide. Overweight and obesity are linked to more morbidities and mortalities worldwide than underweight.4, 5, 6, 7 Human red blood cells (RBCs) have been classified into four ABO blood groups: A, B, AB, and O, which is determined by the presence of antigen A and antigen B on the surface membrane of RBCs, which are specific inherited carbohydrate chains that act as antigens on the extracellular surface of the red blood cell plasmalemma.8 ABO blood groups have been shown to be particularly associated with different diseases, as observed in some studies.9, 10, 11, 12 The evidence of the association of some ABO blood types with diseases is accumulating as this may relate to a direct or indirect role of ABO blood types.11 The ABO blood type should not be clinically used as a biomarker of risk because risk associations with blood type may be affected by other genetic and environmental factors.12 As an example, the high prevalence of H. pylori, which increases the risk of stomach cancer in blood type A, may explain the increased risk of stomach cancer among blood type A patients.12
Few studies have been carried out to detect the association of ABO blood groups with obesity, with uncertain results.13, 14, 15 The goal of this study is to find any potential relation between the ABO blood groups and obesity or increases of BMI among a population of Saudis, which may contribute to underlying genetic or environmental factors and can be considered in future studies.
Materials and Methods
Study design and participants
A cross-sectional descriptive study was conducted using a structured questionnaire among males and females aged 15 years and above from Almadinah Almunawwarah. A total 1204 of Almadinah Almunawwarah participants in this study was obtained after obtaining informed consent for participation. A cross-sectional descriptive study was conducted using a structured questionnaire among the males and females aged above 15 years. All participants with incomplete or missing data, or of an age below 15 years were excluded.
Data collection and analysis
The questionnaire was designed in a very comprehensive manner, consisting of 6 questions related to general demographic data, including weight, height, type of ABO blood group and general opinions related to the association between the ABO groups and obesity. Obesity was conveniently quantified using BMI. It is calculated as the person's weight in kilogrammes divided by the square of his or her height in metres (kg/m2).1, 2 The weight classification was based on the WHO BMI classification as follows: underweight (BMI < 18.5), normal weight (BMI 18.50–24.99), overweight (BMI 25–29.99), obese class I (BMI 30–34.99), obese class II (BMI 35–39.99), obese class III (BMI ≥ 40.00).2 The data were analysed by using SPSS to determine any association between obesity and different ABO blood groups.
Results
Our study included 1171 of 1204 participants of an Almadinah Almunawwarah population; 33 participants' data were excluded because of missing or incomplete data; 575 (49.1%) participants were male and 596 (50.9%) participants were female. The ages of the subjects were classified into five categories, and the majority of participants were younger than 35 years old (77.9%), as 553 (47%) participants were between 15 and 25 years old and 359 (33.7%) participants were between 25 and 35 years old (Table 1). Most participants' nationality (95.6%) was Saudi, while the remaining participants were not Saudi (4.4%). The classification of participants according to BMI were 86 (7.3%) underweight, 407 (34.8%) normal weight, 331 (28.3%) overweight, and 347 (29.6%) obese (Table 2). The prevalence of obesity was 35.7% of male participants and 20.3% of female participants, while the prevalence of overweight was 30% of male participants and 25.3% of female participants. Over half of the participants (57.9%) were classified as overweight or obese based on BMI.
Table 1.
Participants' age classification.
| Age (years) | Participants (n = 1171) | Percent (%) | Cumulative percent (%) |
|---|---|---|---|
| 15–<25 | 553 | 47.2 | 47.2 |
| 25–<35 | 359 | 30.7 | 77.9 |
| 35–<45 | 175 | 14.9 | 92.8 |
| 45–<55 | 68 | 5.8 | 98.6 |
| ≥55 | 16 | 1.4 | 100.0 |
Table 2.
Relation between BMI and blood groups among participants.
| BMI classification | ABO blood group n = 1171 |
P value | ||||
|---|---|---|---|---|---|---|
| A n = 368 (31.4%) |
B n = 188 (16.1%) |
AB n = 76 (6.5%) |
O n = 539 (46.0%) |
|||
| Underweight (BMI < 18.5) | n = 86 (7.3%) | 22 (25.6%) | 11 (12.8%) | 6 (7%) | 47 (54.7%) | 0.55 |
| % within ABO blood group | 6.0% | 5.9% | 7.9% | 8.7% | ||
| % of all participants | 1.9% | 0.9% | 0.5% | 4.0% | ||
| Normal weight (BMI 18.50–24.99) | n = 407 (34.8%) | 137 (33.7%) | 64 (15.7%) | 23 (5.7%) | 183 (45.0%) | 0.51 |
| % within ABO blood group | 37.2% | 34.0% | 30.3% | 34.0% | ||
| % of all participants | 11.7% | 5.5% | 2.0% | 15.6% | ||
| Overweight (BMI 25–29.99) | n = 331 (28.3%) | 104 (31.4%) | 58 (17.5%) | 21 (6.3%) | 148 (44.7%) | 0.84 |
| % within ABO blood group | 28.3% | 30.9% | 27.6% | 27.5% | ||
| % of all participants | 8.9% | 5.0% | 1.8% | 12.6% | ||
| Class I obesity (BMI 30–34.99) | n = 199 (17%) | 57 (28.6%) | 37 (18.6%) | 17 (8.5%) | 88 (44.2%) | 0.11 |
| % within ABO blood group | 15.5% | 19.7% | 22.4% | 16.3% | ||
| % of all participants | 4.9% | 3.2% | 1.5% | 7.5% | ||
| Class II obesity (BMI 35–39.99) | n = 87 (7.4%) | 27 (31.0%) | 9 (10.3%) | 5 (5.7%) | 46 (52.9%) | 0.39 |
| % within ABO blood group | 7.3% | 4.8% | 6.6% | 8.5% | ||
| % of all participants | 2.3% | 0.8% | 0.4% | 3.9% | ||
| Class III obesity (BMI ≥ 40) | n = 61 (5.2%) | 21 (34.4%) | 9 (14.8%) | 4 (6.6%) | 27 (44.3%) | 0.77 |
| % within ABO blood group | 5.7% | 4.8% | 5.3% | 5.0% | ||
| % of all participants | 1.8% | 0.8% | 0.3% | 2.3% | ||
The frequencies of ABO blood groups among all participants were: O group 46% (n = 539), A group 31.4% (n = 368), B group 16.1% (n = 188), and AB group 6.5% (n = 76) (Figure 1). Most of the participants' RhD group (rhesus blood group) was positive (89%), and the RhD negative prevalence according to each ABO blood groups was: 4.4% O-negative, 3.4% A-negative, 2.3% B-negative, and 0.9% AB-negative. The prevalence of obesity (BMI ≥ 30) among participants based on ABO blood groups O, A, B, and AB was 13.7%, 9%, 4.8%, and 2.2%, respectively (Figure 2). The prevalence of obesity was correlated to the prevalence ABO blood groups, and there was no statistically significant relation detected between ABO blood groups and an increase of BMI as overweight and obesity (Table 2).
Figure 1.
ABO blood group prevalence in the Almadinah Almunawwarah population.
Figure 2.
ABO blood group related to weight based on BMI classification among participants.
Most participants (41.7%) believe that there is no relation between obesity and ABO blood types, while 324 (27.7%) participants believe in the presence of a relation between obesity and ABO blood type, based on their best knowledge by direct question (Table 3).
Table 3.
Beliefs of participants regarding the relation between obesity and ABO blood groups.
| Answers | Participants (n = 1171) | Percent (%) | Cumulative percent (%) |
|---|---|---|---|
| Yes, there is relation | 324 | 27.7 | 27.7 |
| No, I don't think so | 488 | 41.7 | 69.4 |
| I don't know | 359 | 30.6 | 100 |
Discussion
This cross-sectional study showed the prevalence of obesity among an Almadinah Almunawwarah population of KSA in 20.3% of female participants and 35.7% of male participants, reflecting a higher obesity prevalence in the Almadinah Almunawwarah population mainly among males compared to the prevalence of obesity in other regions of KSA based on the National Nutrition Survey in 2007 (23.6% in women and 14% in men and compared to WHO data in 2014, which was representative of 13% of the world's adult population).1, 3 This increase in the prevalence of obesity mainly in younger generations requires more public and medical awareness, with specific educational programs to prevent the expansion of these numbers and to avoid the long-term morbidities related to obesity and its impact on society. A larger national study in the future is needed given the limitations of this study regarding the sample size and geographic distribution.
Previous studies showed uncertain results regarding the relation of ABO blood groups and other environmental cofactors to the prevalence of obesity.13, 14, 15 Recently, a study from India showed that there was a correlation between the B blood group and prevalence of obesity and hypertension among blood donors.13 However, another study from India showed a correlation between the O blood group in children and obesity and overweight.14 In contrast, Suadicani and colleagues reported no difference in the prevalence of obesity among male participants with the O blood group and other ABO blood groups, but the prevalence of obesity was increased among men with the O blood group who had long-term occupational exposure to various respirable airborne pollutants.15 Additionally, Kelso and colleagues showed no relation between the ABO blood types and body weight among four samples from different culturally distinct populations.16 Our study showed no statistically significant difference regarding the relation of the prevalence of an increase of BMI (overweight and obesity) and ABO blood types (Table 2). Our results were supported by a recent study from the Northern area of KSA that showed no association between obesity and ABO and Rh blood types.27
From another prospective, the blood type diet, also known as the blood group diet, was popularized by a naturopathic physician called Dr. Peter D'Adamo in the year 1996 in his book “Eat Right 4 Your Type”.17 The hypothesis of health benefits of specific diets for each ABO blood type was not scientifically based as there is no evidence that supports it.18 Some studies attributed this hypothesis to the influence of ABO blood types as a host factor that might modulate the composition of the human intestinal microbiota.19, 20 Recently, Wang and colleagues showed no specific associations between adherence to ABO blood type diets and their effects on cardio-metabolic risk factors in a study that included 1455 participants.21 The commercial use of blood type diets is not recommended without supporting evidence that validate its health benefits.
Finally, the distribution of the ABO blood groups varies worldwide depending on different factors, such as genetics, race and ethnicity, and this distribution is important in understanding lifesaving procedures, such as blood transfusions and organ transplants. It is also important in research since it potentially associates with the incidence of some diseases.9, 10, 11, 12, 13 Our results regarding the prevalence of ABO blood types showed the O group as the most common blood group (46%), followed by the A group (31.4%), B group (16.1%) and AB group (6.5%). Most of this study's participants (89%) were RhD-positive. These results are comparable to previous results of other studies from other regions of KSA.22, 23, 24, 25, 26, 27
Conclusion
Our study showed that there was no relation between high BMI and ABO blood groups. However, the elevation of the prevalence of overweight and obesity, mainly among the younger generations of population of KSA, requires more public and medical awareness and educational programs to prevent its expansion in the future. Larger future national studies are required to assess the current prevention and treatment programs and to study the potential genetic and environmental factors of the increasing prevalence of obesity.
Authors' contribution
TA, SKA, RAA and OBA: Conceived and designed the study. SKA, RAA, OBA, MAJ and AAA conducted research and collected and organized data. TA and SKA were analyzed and interpreted data. All authors were drafting of the article. TA wrote final draft of the article, critical revised of the important intellectual content and provided administrative support. All authors have critically reviewed and approved final draft and are responsible for the content and similarity index of the manuscript.
Conflict of interest and funding
The authors have no conflict of interest to declare. Additionally, authors have not received any research grant from any company or organization for this project.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.World Health Organization, Media centre: fact sheet, cardiovascular diseases. Last Update: June 2016, available from: http://www.who.int/mediacentre/factsheets/fs311/en/. Accessed Nov 25, 2016.
- 2.WHO. BMI classification for adults, The International Classification of adult underweight, overweight and obesity according to BMI. Available from: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Accessed Nov 25, 2016.
- 3.Obesity Research Center, Patient & Public. https://www.obesitycenter.edu.sa/pages/patients.aspx?id=258. Accessed Nov 15, 2016.
- 4.DeNicola E., Aburizaiza O.S., Siddique A., Khwaja H., Carpenter D.O. Obesity and public health in the Kingdom of Saudi Arabia. Rev Environ Health. 2015;30(3):191–205. doi: 10.1515/reveh-2015-0008. [DOI] [PubMed] [Google Scholar]
- 5.Haslam D.W., James W.P. Obesity. Lancet. 2005;366(9492):1197–1209. doi: 10.1016/S0140-6736(05)67483-1. [DOI] [PubMed] [Google Scholar]
- 6.Manson J.E., Willett W.C., Stampfer M.J., Colditz G.A., Hunter D.J., Hankinson S.E. Body weight and mortality among women. N Engl J Med. 1995 Sep 14;333(11):677–685. doi: 10.1056/NEJM199509143331101. [DOI] [PubMed] [Google Scholar]
- 7.Malik V.S., Willett W.C., Hu F.B. Global obesity: trends, risk factors and policy implications. Nat Rev Endocrinol. 2013;9(1):13–27. doi: 10.1038/nrendo.2012.199. [DOI] [PubMed] [Google Scholar]
- 8.Gartner L.P., Hiatt J.L. 3rd ed. Saunders, Elsevier inc.; Philadelphia: 2015. Color textbook of histology. [Chapter 10] [Google Scholar]
- 9.Aird I., Bentall H.H., Roberts J.A. A relationship between cancer of stomach and the ABO blood groups. Br Med J. 1953;1(4814):799–801. doi: 10.1136/bmj.1.4814.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gillum Richard F. Blood groups, serum cholesterol, serum uric acid, blood pressure and obesity in adolescents. J Natl Med Assoc. 1991;83(8):682–688. [PMC free article] [PubMed] [Google Scholar]
- 11.Liumbruno G.M., Franchini M. Beyond immunohaematology: the role of the ABO blood group in human diseases. Blood Transfuse. 2013;11:491–499. doi: 10.2450/2013.0152-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rummel S.K., Ellsworth R.E. The role of the histoblood ABO group in cancer. Future Sci OA. 2016 Mar 15;2(2):FSO107. doi: 10.4155/fsoa-2015-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chandra Tulika, Gupta Ashish. Association and distribution of hypertension, obesity and ABO blood groups in blood donors. Iran J Ped Hematol Oncol. 2012;2(4):140–145. [PMC free article] [PubMed] [Google Scholar]
- 14.Siva K., Umesh P.L., Satyanarayana P. Correlation between obesity & ABO blood group in school going children in India. Indian J Basic Appl Med Res. 2012;1(4):280–284. [Google Scholar]
- 15.Suadicani P., Hein H.O., Gyntelberg F. Airborne occupational exposure, ABO phenotype, and risk of obesity. Int J Obes (Lond) 2005 Jun;29(6):689–696. doi: 10.1038/sj.ijo.0802956. [DOI] [PubMed] [Google Scholar]
- 16.Kelso A.J., Maggi W., Beals K.L. Body weight and ABO blood types: are AB females heavier? Am J Hum Biol. 1994;6:385–387. doi: 10.1002/ajhb.1310060313. [DOI] [PubMed] [Google Scholar]
- 17.D'Adamo PJ, Whitney C. Eat right 4 your type. GP Putnam's Sons Publishers.
- 18.Cusack L., De Buck E., Compernolle V., Vandekerckhove P. Blood type diets lack supporting evidence: a systematic review. Am J Clin Nutr. 2013 Jul;98(1):99–104. doi: 10.3945/ajcn.113.058693. [DOI] [PubMed] [Google Scholar]
- 19.Mäkivuokko H., Lahtinen S.J., Wacklin P., Tuovinen E. Association between the ABO blood group and the human intestinal microbiota composition. BMC Microbiol. 2012 Jun 6;12:94. doi: 10.1186/1471-2180-12-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Langman M.J., Leuthold E., Robson E.B., Harris J. Influence of diet on the “intestinal” component of serum alkaline phosphatase in people of different ABO blood groups and secretor status. Nature. 1966 Oct 1;212(5057):41–43. doi: 10.1038/212041a0. [DOI] [PubMed] [Google Scholar]
- 21.Wang Jingzhou, García-Bailo Bibiana, Nielsen Daiva E., El-Sohemy Ahmed. ABO genotype, ‘Blood-Type’ diet and cardiometabolic risk factors. PLoS One. 2014;9(1):e84749. doi: 10.1371/journal.pone.0084749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sarhan M.A., Saleh K.A., Bin-Dajem S.M. Distribution of ABO blood groups and rhesus factor in Southwest Saudi Arabia. Saudi Med J. 2009;30(1):116–119. [PubMed] [Google Scholar]
- 23.Eweidah M.H., Rahiman S., Ali Hassan, Al-Shamary A.M.D. Distribution of ABO and Rhesus (RHD) blood groups in Al-Jouf Province of the Saudi Arabia. Anthropologist. 2011;13(2):99–102. [Google Scholar]
- 24.LA1 Bashwari, Al-Mulhim A.A., Ahmad M.S., Ahmed M.A. Frequency of ABO blood groups in the Eastern region of Saudi Arabia. Saudi Med J. 2001 Nov;22(11):1008–1012. [PubMed] [Google Scholar]
- 25.Ozsoylu S., Alhejaily M. The distribution of ABO and Rh blood groups in the Tabuk region and Medina Munewera, Saudi Arabia. Turk J Pediatr. 1987 Oct–Dec;29(4):239–241. [PubMed] [Google Scholar]
- 26.AlSuhaibani E.S., Kizilbash N.A., Malik S. Heterogeneity and diversity of ABO and Rh blood group genes in select Saudi Arabian populations. Genet Mol Res. 2015 Jul 14;14(3):7850–7863. doi: 10.4238/2015.July.14.11. [DOI] [PubMed] [Google Scholar]
- 27.Aboel-Fetoh N.M., Alanazi A.R., Alanazi A.S., Alruwili A.N. ABO blood groups and risk for obesity in Arar, Northern Saudi Arabia. J Egypt Public Health Assoc. 2016 Dec;91(4):169–173. doi: 10.1097/01.EPX.0000508457.31670.20. [DOI] [PubMed] [Google Scholar]