Abstract
Objectives
To estimate the prevalence of dyslipidemia and patterns of lipid profile and associated factors among Yemeni university students.
Methods
This cross-sectional study included 240 Yemeni students (116 males and 124 females) at Ibb University. The students were randomly selected from various faculties of the university. Demographic and clinical data were obtained from all participants. Fasting blood specimens were collected from all students for measurement of serum levels of total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C). The criteria of the National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP III) were used.
Results
The mean age of the studied cohort was 19.8 ± 1.8 years; 48.3% were men and 51.7% were women. About 56.7% of the participants were from rural areas. Qat chewers and cigarette smokers comprised 63.3% and 6.7% of the cohort, respectively. No obese students were found in this study; however, 11.7% were overweight. The overall prevalence of dyslipidemia, hypercholesterolemia, hypertriglyceridemia, high LDL-C, and low HDL-C among the participating students were 86.7%, 21.7%, 23.8%, 31.7%, and 81.7%, respectively. Mixed hyperlipidemia was present in 8.8% of the students. The prevalence of isolated hypercholesterolemia, hypertriglyceridemia, and low HDL-C was 12.9%, 15%, and 70%, respectively. Dyslipidemia was significantly associated with male sex, increasing age, urban residence, and medical and natural science faculties. In contrast, smoking, qat chewing, physical activity, and the consumption of fast food, fruits and vegetables, and fish were not significantly associated with dyslipidemia.
Conclusion
To our knowledge, this is the first human study conducted at Ibb University during wartime in Yemen. Dyslipidemia was highly prevalent among healthy Yemeni university students in Ibb city. Low HDL-C was the most prevalent type of dyslipidemia, followed by increased levels of LDL-C. Gender, age, residence, and type of faculty were also closely related to dyslipidemia. These results indicate the need for specialized programs to determine blood lipid levels and initiate intervention programs to reduce the prevalence and prevent the complications of dyslipidemia among Yemeni university students.
Keywords: Dyslipidemia, Hypercholesterolemia, Hypertriglyceridemia, Ibb, Students
الملخص
أهداف البحث
تقييم مدى انتشار اختلال الدهون في الدم وأنماط مستوى الدهون والعوامل المرتبطة بذلك بين طلاب الجامعة اليمنيين.
طرق البحث
أجريت هذه الدراسة -المقطعية على مجموعة من ٢٤٠ طالبا يمنيا (١١٦ ذكورا ١٢٤ إناثا) في جامعة إب. تم اختيار الطلاب بطريقة عشوائية من الكليات المختلفة للجامعة. كما تم الحصول على المعلومات الديمغرافية والسريرية من جميع المشاركين. تم جمع عينات الدم من جميع الطلاب وهم صائمون لقياس مستويات المصل لكل من الكولسترول الكلي، والدهون الثلاثية، وكوليسترول البروتينات الدهنية منخفضة الكثافة، وكوليسترول البروتينات الدهنية عالية الكثافة. تم استخدام معايير البرنامج الوطني الأمريكي التعليمي للكوليسترول – برنامج معالجة البالغين الثالث (NCEP-ATP III).
النتائج
كان متوسط العمر للمشاركين ١٩.٨± ١.٨ عاما؛ من بينهم ٤٨.٣٪ من الذكور و٥١.٧٪ من الإناث. كان ٥٦.٧٪ من المشاركين ينتمون إلى المناطق الريفية. وكان ماضغي القات والمدخنين ٦٣.٣٪ و٦.٧٪ على التوالي. لم يوجد طلاب يعانون من السمنة في هذه الدراسة، ولكن كان هناك ١١.٧٪ من الطلاب يعانون من زيادة الوزن. كان معدل الانتشار العام لاختلال الدهون في الدم بين الطلاب المشاركين ٨٦.٧٪، وارتفاع الكوليسترول في الدم ٢١.٧٪، وزيادة الدهون الثلاثية في الدم ٢٣.٨٪ وزيادة كوليسترول البروتينات الدهنية منخفضة الكثافة ٣١.٧٪ وانخفاض كوليسترول البروتينات الدهنية عالية الكثافة ٨١.٧٪. وكانت الدهون المختلطة منتشرة عند ٨.٨٪ من الطلاب. بلغ معدل الانتشار المنعزل لكلا من ارتفاع الكوليسترول، وزيادة الدهون الثلاثية، وانخفاض كوليسترول البروتينات الدهنية عالية الكثافة ١٢.٩٪، ١٥٪، و٧٠٪، على التوالي. كان اختلال الدهون في الدم مرتبطا بشكل كبير مع الجنس من الذكور، وتقدم العمر، والإقامة الحضرية، والكليات الطبية والعلوم الطبيعية. من ناحية أخرى، كان التدخين، ومضغ القات، والنشاط البدني، واستهلاك الوجبات السريعة، والفواكه والخضروات، وتناول الأسماك من العوامل غير المرتبطة باختلال الدهون في الدم.
الاستنتاجات
هذه هي أول دراسة بشرية أجريت في جامعة إب خلال الحرب في اليمن. وكان اختلال الدهون في الدم منتشرا كثيرا بين الطلاب الجامعيين اليمنيين الأصحاء في مدينة إب. وكان انخفاض كوليسترول البروتينات الدهنية عالية الكثافة أكثر أنواع الاختلالات الدهنية في الدم انتشارا، يليه زيادة مستويات كوليسترول البروتينات الدهنية منخفضة الكثافة. وارتبط الجنس، والعمر، ومكان الإقامة ونوع الكلية ارتباطا وثيقا باختلال الدهون في الدم. تشير هذه النتائج إلى الحاجة إلى برامج متخصصة لتحديد مستويات الدهون في الدم، لبدء برامج التدخل للحد من انتشار اختلال الدهون في الدم ومنع مضاعفاتها بين طلاب الجامعة اليمنيين.
الكلمات المفتاحية: اختلال الدهون في الدم, إب, الطلاب, ارتفاع الكوليسترول, زيادة الدهون الثلاثية في الدم
Introduction
Dyslipidemia is defined as elevated of plasma levels of total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), and triglycerides (TG), as well as lower plasma levels of high-density lipoprotein cholesterol (HDL-C). These increases can occur either singly or in combination.1, 2 Dyslipidemia is associated with atherosclerosis and increases the risk of cardiovascular disease (CVD).3 According to the World Health Organization (WHO), 17.7 million people die annually from CVD4 and approximately one-third of global deaths are attributable to CVD and stroke.5, 6 Dyslipidemia in adulthood increases the prevalence of CVD later on in life.7 Cholesterol levels at 22 years of age can predict the rate of CVD development over the ensuing 30–40 years.8 The treatment of dyslipidemia as a modifiable risk factor of CVD has been shown to reduce the incidence of CVD morbidity and mortality.9 For every 38.6 mg/dL reduction in LDL-C level, the annual rate of major vascular events decreases by one-fifth.10 CVD also represents a considerable economic burden to society. In the USA, the direct annual costs of CVD are projected to triple between 2010 and 2030, while the healthcare costs related to CVD represented 9% of the total healthcare expenditure across the European Union in 2009.11, 12 Dyslipidemia is also prevalent in the Arab Countries. The CVD-associated mortality rate in the Middle East (ME) is one of the highest in the world.13 According to WHO, the CVD mortality in Yemen accounts for 21% of total deaths among all ages of both sexes.14 The Ibb governorate is located in the inland south of Yemen. It has an area of 6484 km2 and an estimated population of around 2,560,000, making it the most densely populated governorate in Yemen. It has 20 districts.15 Ibb city is the capital of the governorate. Despite the war conditions in the country in the last three years, Ibb city remains one of the most secure and stable cities in the country, which explains the large wave of displacement from other provinces. To our knowledge, no previous study has measured the prevalence of dyslipidemia among university students in Ibb governorate. Therefore, this study aimed to estimate the prevalence of dyslipidemia and patterns of serum lipid profiles and associated risk factors among Yemeni students at Ibb University.
Materials and Methods
Population sample
This cross-sectional study was carried out at Ibb University in Ibb city, Yemen, between February 1 and June 2018. Ibb University is a state university in Yemen with ten faculties including more than 10,000 students (60% males and 40% females) originating from across the country. Data were collected using a predesigned interviewing schedule. Stratified random sampling was used to include students from the first to the last academic years. Students were selected using a clustering technique inside each faculty for each academic year. Students in the faculties are usually divided into small sections for practical and tutorial lessons. Each section includes from 10 to 30 students. One or two clusters were randomly selected in each academic year. The study sample was statistically calculated based on a 21% prevalence of CVD in Yemen according to WHO non-communicable diseases (NCD) country profiles.14 A significance level 0.05 and power of 90% were used. The estimated sample size was 180. A total of 300 students aged 17–25 years, were chosen randomly from five faculties (Science, Education, Dentistry, Engineering, and Arts). The inclusion criteria of the study were apparently healthy Yemeni university students (male or female) 17–25 years of age who agreed to participate in the study. A total of 240 students (116 males and 124 females) completed the study and were included in the final analysis. Students who refused to participate and those with hypertension, diabetes mellitus, and kidney diseases were excluded. Pregnant women, nursing mothers, or students receiving medications that could affect serum lipid profiles were not included. Students were asked to fast for 10–14 h prior to the time of blood collection. Ethical approval of the study was obtained from the ethical committee of Ibb University. The study conformed to the ethical standards of the Declaration of Helsinki. Written informed consent was obtained from each participant upon his/her agreement to participate in the study. Administrative approvals were also obtained.
Data collection and measurements
A written document explaining the aim of the study was prepared by the researchers. Participant students were asked to fast for 10–14 h at the time of the interview. Each participant visited the university clinic twice. During the first visit, the questionnaire was completed and clinical and physical measurements were performed. The second visit included the collection of blood samples and completion of deficient data. Personal data such as sex, age, and martial state were collected. Data regarding health and dietary habits (Qat chewing, smoking, frequency of fast food consumption, physical exercise, and vegetable and fruit consumption) were also collected. Height and weight were measured twice using a calibrated height–weight scale with the subjects standing in bare feet while wearing light clothing; the average values of the two measurements were then calculated. Body mass index (BMI) was calculated as the weight (kg) divided by the square of the height (m). Waist circumference (WC) was measured twice on standing participants at the midpoint between the lower edge of the costal arch and the upper edge of the iliac crest, with means calculated. Blood pressure was recorded by physicians using a sphygmomanometer after a 5-min sitting rest, with the average of three readings calculated. Venous blood samples were collected from each student after a 10–14-h fast. The samples were centrifuged immediately and stored at −70 °C until biochemical analysis. The samples were analyzed for total cholesterol (TC), triglycerides (TG), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) levels. Spinreact diagnostic enzymatic kits (Spain) were used. A spectrophotometer made by Spectronic Company (USA) was used.
Definitions of variables
According to the criteria of the National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATP III),16 dyslipidemia was defined as follows:
Hypertriglyceridemia: TG levels ≥ 150 mg/dL; hypercholesterolemia: TC ≥ 200 mg/dL; high LDL-C: levels ≥130 mg/dL; low HDL-C: levels < 40 mg/dL. Isolated hypercholesterolemia was defined as a total cholesterol ≥ 200 mg/dL and TG < 150 mg/dL; isolated hypertriglyceridemia was defined as serum TG ≥ 150 mg/dL and total cholesterol < 200 mg/dL; mixed hyperlipidemia was defined as TG ≥ 150 mg/dL and total cholesterol ≥ 200 mg/dL; isolated low HDL-C was defined as HDL-C ≤50 mg/dL in women and ≤40 mg/dL in men without hypertriglyceridemia or hypercholesterolemia. Overweight was defined as BMI ≥ 25.0 kg/m2 and < 30.0 kg/m2, while obesity was defined as BMI ≥ 30 kg/m2.17, 18 Central obesity was defined as a WC ≥ 102 cm in men and ≥82 in women.19
Qat chewers were defined as those who chewed qat for 4–6 h daily, usually in the afternoon, four times per week.20 Hypertension was defined as systolic blood pressure ≥140 mmHg and diastolic blood pressure ≥90 mmHg.21 Smoking was classified in terms of current smokers or non-smokers. Regular physical activity was defined as participation in moderate or vigorous activity for ≥30 min/day at least five days per week.22 Frequent fast consumption was defined as the consumption of foods like pizza, fried chicken, and hamburger at least three times per week.8
Statistical analysis
Data were collected, coded, and entered into an IBM-compatible computer using IBM SPSS Statistics for Windows, version 22.0. The results were presented as frequencies and percentages for qualitative data and as means and standard deviation for quantitative variables. Chi-square tests were used to assess the association of dyslipidemia with qualitative variables. Statistical significance was defined for P-values < 0.05.
Results
Among the 300 initial participants in the study, 60 were excluded for incomplete data. The personal data of the participating students are shown in Table 1. A total of 240 students (116 males and 124 females) aged 17–25 years (mean: 19.8 ± 1.8 years) were included in this study. Women comprised 51.7% of the participating students. The majority of the participants (56.7%) were from rural areas and 85% of them were ≥20 years of age. Qat chewers and smokers comprised 63.3% and 6.7% of the students, respectively. Overweight students represented 11.7% of the population and no students (0%) of both sexes were obese. Students from the faculty of Science comprised 70% of the participants. Only 11.7% of the participants practiced irregular or regular exercise. Daily consumption of fast food, fruits, and fish was reported by 41.7%, 11.7%, and 1.7% of students, respectively.
Table 1.
General characteristics of the participating students.
| Variables | Levels | Number (Percent) 240 |
|---|---|---|
| Sex | Male | 116 [48.3%] |
| Female | 124 [51.7%] | |
| Age (years) | <20 | 36 [15%] |
| ≥20 | 204 [85%] | |
| Faculty | Medicine | 24 [10%] |
| Natural Science | 168 [70%] | |
| Social Science | 48 [20%] | |
| Residence | Rural | 136 [56.7%] |
| Urban | 104 [43.3%] | |
| Weight | Normal | 212 [88.3%] |
| Overweight | 28 [11.7%] | |
| Obese | 0[0%] | |
| Exercise | None | 212 [88.3%] |
| Irregular | 16 [6.7%] | |
| Regular | 12 [5%] | |
| Smoking | Yes | 224 [93.3%] |
| No | 16 [6.7%] | |
| Qat consumption | Yes | 152 [63.3%] |
| No | 88 [36.7%] | |
| Fast food | Seldom | 82 [34.2%] |
| Three times a week | 58 [24.2%] | |
| Daily | 100 [41.7%] | |
| Fruits and vegetables | Seldom | 124 [51.7%] |
| Three times a week | 88 [36.7%] | |
| Daily | 28 [11.6%] | |
| Fish | Seldom | 216 [90%] |
| Three times a week | 20 [8.3%] | |
| Daily | 4 [1.7%] |
Table 2 shows the male/female anthropometric parameters of the students. There were no sex differences in BMI, but there was a significant difference in WC (P < 0.05) between male and female students. The mean systolic and diastolic blood pressures were significantly (P˂0.05) higher in male than those in female students.
Table 2.
Anthropometric parameters of the study participants according to sex.
| Male (n = 116) | Female (n = 124) | Total (N = 240) | P-value | |
|---|---|---|---|---|
| BMI (kg/m2) | 20.92 ± 3.6 | 20.56 ± 3.65 | 20.73 ± 3.63 | 0.53 |
| WC (cm) | 79.5 ± 13.4 | 71.24 ± 11.8 | 74.20 ± 12.14 | 0.00 |
| SBP (mmHg) | 112.34 ± 8.62 | 106.12 ± 4.46 | 108.24 ± 6.34 | 0.04 |
| DBP (mmHg) | 74.2 ± 6.2 | 70.82 ± 5.8 | 72.56 ± 6.2 | 0.01 |
Table 3 shows the mean lipid profile levels among students according to sex. Male students had higher lipid profile levels compared to those in female students. The mean ± SD of TC, TG, LDL-C, and HDL-C for males were 171.07 ± 46.28, 147.71 ± 65.05, 106.47 ± 45.90, and 35.07 ± 19.41, respectively, and 160.52 ± 42.29, 99.84 ± 37.49, 105.65 ± 58.54, and 34.94 ± 23.47, respectively, for females.
Table 3.
Mean concentrations of lipid profiles according to sex.
| Male (n = 116) | Female (n = 124) | Total (N = 240) | P-value | |
|---|---|---|---|---|
| TC (mg/dL) | 171.07 ± 46.28 | 160.52 ± 42.29 | 165.62 ± 44.48 | 0.06 |
| TG (mg/dL) | 147.71 ± 65.05 | 99.84 ± 37.49 | 122.98 ± 57.74 | 0.00 |
| LDL-C (mg/dL) | 106.47 ± 45.90 | 105.65 ± 58.54 | 106.04 ± 52.70 | 0.66 |
| HDL-C (mg/dL) | 35.07 ± 19.41 | 34.94 ± 23.47 | 35.00 ± 21.56 | 0.95 |
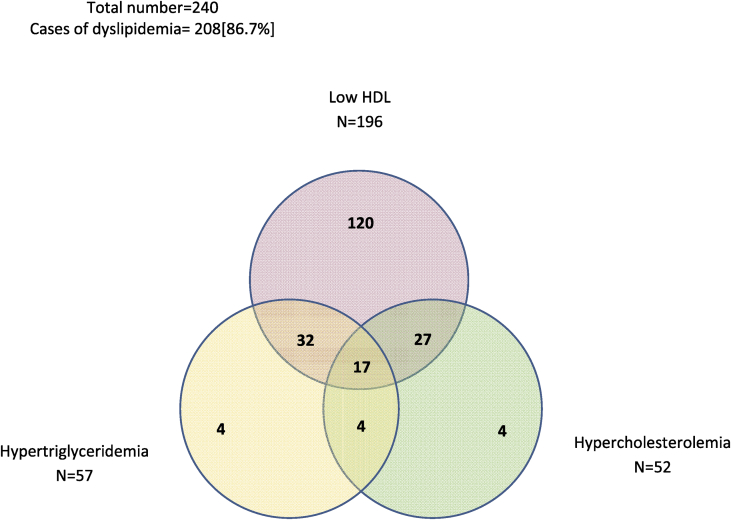
Table 4 examines the prevalence of dyslipidemia among the participating students. Dyslipidemia was highly prevalent (86.7%) among the students, while mixed hyperlipidemia was found only in 8.8% of the subjects. The prevalence of hypercholesterolemia, hypertriglyceridemia, high LDL-C, and low HDL-C was 21.7%, 23.8%, 31.7%, and 81.7% respectively. The prevalence of isolated hypercholesterolemia, isolated hypertriglyceridemia, and isolated low HDL-C was 12.9%, 15%, and 50%, respectively (Figure 1).
Table 4.
Prevalence of dyslipidemia among study participants.
| Prevalence of | N = 240 |
|---|---|
| Hypercholesterolemia | 52 [21.7%] |
| Hypertriglyceridemia | 57 [23.8%] |
| High LDL-C | 76 [31.7%] |
| Low HDL-C | 196 [81.7%] |
| Isolated hypercholesterolemia | 31 [12.9%] |
| Isolated hypertriglyceridemia | 36 [15%] |
| Isolated low HDL-C | 120 [50%] |
| Mixed hyperlipidemia | 21 [8.8%] |
| Dyslipidemia (at least one factor affected) | 208 [86.7%] |
Figure 1.
Venn diagram showed interaction between dyslipidemia types. Three circles: green circle for hypercholesterolemia, yellow circle for hypertriglyceridemia, pink circles for low HDL-C.
Table 5 illustrates the factors associated with dyslipidemia. A significantly higher prevalence of hypercholesterolemia and hypertriglyceridemia was observed in male students compared to those in female students (31% and 49% versus 12.9% and 6.5%) (P = 0.005); while low HDL-C and high LDL-C were more prevalent in female students than in male students (83.9% and 32.3% versus 79.3% and 31%), the difference was not statistically significant. Hypertriglyceridemia was observed in 27.5% of students aged ≥20 years and was significantly (P< 0.005) associated with this age group, while high LDL-C was significantly associated in those less than 20 years of age (P < 0.005). Hypercholesterolemia, hypertriglyceridemia, and high LDL-C accounted for 30.8%, 31.7%, and 38.5%, respectively, of urban students (P-values: 0.005, 0.01, and 0.04 respectively). Significant differences in the prevalence of dyslipidemia were observed between faculties, with a higher percentage of abnormalities among medical and natural science students (Table 5).
Table 5.
Association of dyslipidemia with demographic characteristics and obesity.
| Demographic | High TC n = 52 | High TG n = 57 | High LDL-C n = 76 | Low HDL-C n = 196 | |
|---|---|---|---|---|---|
| Sex | Male | 36 [31.0%] | 49 [42.2%] | 36 [31.0%] | 92 [79.3%] |
| Female | 16 [12.9%] | 8 [6.5%] | 40 [32.3%] | 104 [83.9%] | |
| P-value | 0.00 | 0.00 | 0.83 | 0.36 | |
| Age (years) | <20 | 8 [22.2%] | 1 [2.8%] | 20 [55.6%] | 32 [88.9%] |
| ≥20 | 44 [21.6%] | 56 [27.5%] | 56 [27.5%] | 164 [80.4%] | |
| P-value | 0.93 | 0.00 | 0.00 | 0.22 | |
| Residence | Rural | 20 [14.7%] | 24 [17.6%] | 36 [26.5%] | 108 [79.4%] |
| Urban | 32 [30.8%] | 33 [31.7%] | 40 [38.5%] | 88 [84.6%] | |
| P-value | 0.00 | 0.01 | 0.04 | 0.30 | |
| Faculty | Medicine | 16 [66.7%] | 5 [20.8%] | 16 [66.7%] | 24 [100%] |
| Natural Science | 36 [21.4%] | 52 [31.0%] | 48 [28.6%] | 124 [73.8%] | |
| Social Science | 0 [0%] | 0 [0%] | 12[25%] | 48 [100%] | |
| P-value | 0.00 | 0.00 | 0.00 | 0.00 | |
| Obesity | Normal | 44 [20.8%] | 52 [24.5%] | 64 [30.2%] | 177 [83.5%] |
| Overweight | 8 [28.6%] | 5 [17.9%] | 12 [42.9%] | 19 [67.9%] | |
| Obese | 0[0%] | 0 [0%] | 0 [0%] | 0 [0%] | |
| P-value | 0.34 | 0.43 | 0.17 | 0.04 |
Table 5 also shows the non-significant association of different types of dyslipidemia with normal and overweight students with the exception of low HDL-C, which was significantly associated with body weight (P< 0.05) and accounted for 83.5% and 67.9% of normal and overweight students, respectively. In our study, obesity was not detected among the participating students (Table 5).
Table 6 illustrates the association of dyslipidemia with lifestyle factors and dietary habits. Only low HDL-C-hypoalphalipoproteinemia was significantly associated with smoking (P = 0.005); the other types of dyslipidemia were not significantly associated with smoking and qat chewing (Table 6).
Table 6.
Associations of dyslipidemia with lifestyle factors and dietary habits.
| Lifestyle factor | High TC N = 52 | High TG N = 57 | High LDL-C N = 76 | Low HDL-C N = 196 | |
|---|---|---|---|---|---|
| Smoking | No | 48 [21.4%] | 53 [23.7%] | 72 [32.1%] | 188 [83.9%] |
| Yes | 4 [25%] | 4 [25%] | 4 [25%] | 8 [50%] | |
| P-value | 0.73 | 0.90 | 0.55 | 0.00 | |
| Qat chewing | Yes | 20 [22.7%] | 16 [18.2%] | 28 [31.8%] | 76 [86.4%] |
| No | 32 [21.1%] | 41 [27%] | 48 [31.6%] | 120 [78.9%] | |
| P-value | 0.76 | 0.12 | 0.96 | 0.15 | |
| Exercise | No | 48 [22.6%] | 45 [21.2%] | 69 [32.5%] | 170 [80.2%] |
| Irregular | 2 [12.5%] | 11 [68.8%] | 3 [18.8%] | 16 [100%] | |
| Regular | 2 [16.5%] | 1 [8.3%] | 4 [33.3%] | 10 [83.3%] | |
| P-value | 0.58 | 0.00 | 0.51 | 0.14 | |
| Fast food consumption | Seldom | 18 [22%] | 17 [20.7%] | 26 [31.7%] | 69 [84.1%] |
| Three times per week | 10 [17.2%] | 5 [8.6%] | 15 [25.9%] | 44 [75.9%] | |
| Daily | 24 [24%] | 35 [35%] | 35 [35%] | 83 [83%] | |
| P-value | 0.60 | 0.00 | 0.49 | 0.41 | |
| Fruit & vegetable consumption | Seldom | 24 [19.4%] | 28 [22.6%] | 36 [29%] | 108 [87.1%] |
| Three times per week | 21 [23.9%] | 21 [23.9%] | 30 [34.1%] | 67 [76.1%] | |
| Daily | 7 [25%] | 8 [28.6%] | 10 [35.7%] | 21 [75%] | |
| P-value | 0.66 | 0.79 | 0.65 | 0.07 | |
| Fish consumption | Seldom | 49 [22.7%] | 49 [22.7%] | 71 [32.9%] | 177 [81.9%] |
| Three times per week | 3 [15%] | 7 [35%] | 5 [25%] | 16 [80%] | |
| Daily | 0 [0%] | 1 [25%] | 0 [0%] | 3 [75%] | |
| P-value | 0.41 | 0.46 | 0.30 | 0.92 |
Hypertriglyceridemia was significantly (P< 0.005) associated with physical inactivity and accounted for 68.8% of students practicing irregular exercise. The other types of dyslipidemia were not associated with exercise (P > 0.05). A significant relation between dyslipidemia and fast food consumption was observed, with an increased prevalence of hypertriglyceridemia by 35% among students with daily fast food consumption (P = 0.005. No significant association was observed between dyslipidemia and fruit and vegetable and fish consumption (Table 6).
Discussion
Recently, the increasing prevalence of dyslipidemia is a worldwide public health problem. Its prevalence varies widely according to ethnic, socioeconomic, and cultural characteristics. To our knowledge, the current study is the first to examine the prevalence of types of dyslipidemia among Yemeni students at Ibb University. It may be also the first study in Yemen conducted during war conditions. Our results show that 63.3% of the students chewed qat daily. Qat chewing is a highly prevalent habit in Yemen, Ethiopia, and other countries of the Horn of Africa.23 This finding is concordant with those of other studies. The reported prevalence of qat chewing in Yemen, Ethiopia, and the Jazan region of KSA is 61.12%, 42%, and 28.7%, respectively.24, 25, 26 Students chew qat believing that it improves memory, alertness, and clear thinking.27 An interesting finding in the current study was the absence of obesity among Yemeni university students. Our finding is inconsistent with those of other studies. Many regional and international studies reported obesity to be a significant risk factor for dyslipidemia.28, 29, 30, 31 The absence of obesity in our study is likely related to widespread poverty among Yemeni families, particularly during the last three years of war. Yemen is one of the poorest countries in the Middle East. According to the United Nations (UN), about half of Yemen's population of about 26.8 million lives below the poverty line.32 Traditional Yemeni food is low in fats and calories. This may also explain the absence of obesity among our students. In addition, the majority of students in this study reported that, due to the high cost of transportation, they leave and return to the university on foot. In other words, students practice daily exercise. Exercise can help promote weight loss and works best when combined with lower-calorie diet.33 Finally, the widespread of qat chewing among Yemeni students may also play a role in the absence of obesity. It is common for Yemeni students to eat a good meal only once a day for lunch. They spend most of their money to buy qat for chewing many hours daily. The students believe that qat improves memory, alertness and clear thinking. They do not care about breakfast and dinner. Qat also suppresses appetite.34 However, Al-Sharafi and Gunaid reported a higher prevalence of normal BMI among qat chewers than among non-qat chewers.35 Our results showed significantly higher prevalences of hypercholesterolemia and hypertriglyceridemia in male than those in female students. This finding is consistent with those of other studies.29, 36 However, other studies have reported no difference in dyslipidemia between men and women.37, 38 The increasing prevalence of dyslipidemia is a worldwide public health problem. In our study, the overall prevalence of dyslipidemia (at least one abnormal lipid profile value) was 86.7%. This result is similar to that reported in an Iranian study (83.4%) study.39 However, our figures are higher than those in other studies. Al-Sabah et al. reported an estimated prevalence of 75% in young adults aged 20–40 years in Baghdad city, Iraq.40 Hamam reported a 60% prevalence among Saudi university students at Taif University.41 Other studies in China, Kuwait, Oman, and KSA also reported lower estimates of dyslipidemia.22, 29, 36, 42 The current study showed a significant increase in dyslipidemia in the form of hypercholesterolemia, hypertriglyceridemia, and high LDL-C among urban students compared to the levels in rural students. This is in accordance with other studies.7, 43 This difference may be due to urban lifestyles and dietary habits including the consumption of fast food and high-fat diets. Another interesting finding of the current study was the high prevalence of low HDL-C (81.7%) among Yemeni university students. This prevalence is much higher than that in their counterparts in KSA (46.3%), Iraq (38.5%), and Egypt (27.1%).41, 40, 8 The prevalence of isolated low HDL-C in our study was 70%. This prevalence appears to be one of the highest compared to those reported by similar studies. Qi et al.22 reported an isolated low HDL-C prevalence of 10.5%, while Mula-Abed and Chilmeran reported a prevalence of 49.9% among adult Iraqi population.44 However, this finding is similar to those of one study conducted among rural populations in Uganda.45 The association of genetic factors with variations in LDL-C level has been elaborated. Genetic factors determine about 50% of the variability in HDL-C levels, while acquired factors such as diet, smoking, diabetes mellitus type 2, physical inactivity, and drugs affect the other 50%.46, 47 Furthermore, the high prevalence of isolated low HDL-C among populations consuming low-fat diets may be due to decreased apolipoproteins in HDL-C.48, 49 Finally, the present study was conducted during war conditions in the country that had lasted for more than three years. Psychological stress is also a risk factor for lipid disorders.50, 51 Thus, Yemeni university students are at high risk for developing CVD.52 According to WHO, CVD mortality accounts for 21% of total deaths among all age groups of men and women in Yemen.14
The prevalence of hypercholesterolemia in the current study was 21.7%, much lower than the prevalence in Egyptian,8 Turkish,53 and Jordanian adults.36 In contrast, our result is concordant with a Spanish study.54 However, our figures are much higher than other studies on this age group.29, 41 Young adults with hypercholesterolemia have five times the risk of CVD and nine times the risk of myocardial infarction (MI) in the following 30–40 years compared to the risk in young adults with low cholesterol levels.55 The current results revealed hypertriglyceridemia in only 23.8% of students. The Egyptian estimate of hypertriglyceridemia among university students (29.7%) was comparable to that in the current study.8 Desouky et al. reported a 33.6% prevalence of hypertriglyceridemia among Saudi female university students.56 Our results also show the increasing prevalence of dyslipidemia among medical and natural science students compared to those in students from social science faculties. This may be linked to the type of study in these faculties, which may encourage students physical inactivity for long periods of time to read lessons or work on computers. This result is similar to those of another study.8 The current study revealed the insignificant association of dyslipidemia with eating habits and the intake of most of the investigated food, a result consistent with those of previous studies.8, 41
Limitations
Our study has some limitations, mainly related to the nature of the study. The data were based on the number of Yemeni university students at one state University and likely do not represent the actual prevalence of dyslipidemia among the whole population. Therefore, we recommend intervention programs for university students at an earlier age through screening, health education, and counseling. Our results provide a foundation for further studies to reduce dyslipidemia prevalence and prevent its complications.
Conclusion
To our knowledge, is the first human study conducted at Ibb University during wartime in Yemen. Dyslipidemia was prevalent among healthy Yemeni university students in Ibb city. Low HDL-C was the most prevalent type of dyslipidemia, followed by increased levels of LDL-C. Gender, age, residence, and type of faculty were associated with to dyslipidemia. These results indicate the need for specialized programs for the study of blood lipid levels as well as appropriate intervention programs to reduce the prevalence and prevent complications of dyslipidemia among Yemeni university students.
Source of funding
This work was not funded by any organizations and/or institutions.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
Ethics approval of the study was obtained from the ethical committee of Ibb University. The whole study was conformed to the ethical standards of the Helsinki Declaration. A written informed consent was taken from each participant upon his/her acceptance to participate in the study. In addition, all administrative approvals were taken. And the Ibb University approval paper will be attached below with this email.
Authors' contributions
Mohammed Al-Duais designed the plan of the study, designed the methodology, organized, and prepared the initial draft of the paper. Yahya Al-Awthan conducted the study, collected and provided statistical analysis of the results. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgments
We are grateful to the study participants for their active cooperation. Special thanks to Azhar Al-Ezzy and Zinab Sufian from the Department of Biology for their assistance in filling the questioners and collection of the samples.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Bibbins-Domingo K., Grossman D.C., Curry S.J., Davidson K.W., Epling J.W., García F.A., US Preventive Services Task Force Screening for lipid disorders in children and adolescents: US Preventive Services Task Force recommendation statement. J Am Med Assoc. 2016;316(6):625–633. doi: 10.1001/jama.2016.9852. [DOI] [PubMed] [Google Scholar]
- 2.Manjunath C.N., Rawal J.R., Irani P.M., Madhu K. Atherogenic dyslipidemia. Indian J Endocrinol Metab. 2013;17(6):969–976. doi: 10.4103/2230-8210.122600. PubMed PMID: 24381869, Pubmed Central PMCID: PMC3872713, Epub 2014/01/02. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Expert Panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents; national heart, lung, and blood institute: expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: summary report. Pediatrics. 2011;128:213–256. doi: 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.http://www.who.int/cardiovascular_diseases/en/.
- 5.Townsend N., Nichols M., Scarborough P., Rayner M. Cardiovascular disease inEurope - epidemiological update 2015. Eur Heart J. 2015;36:2696–2705. doi: 10.1093/eurheartj/ehv428. [DOI] [PubMed] [Google Scholar]
- 6.GBD 2013 Mortality and Causes of Death Collaborators Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;385:117–171. doi: 10.1016/S0140-6736(14)61682-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Joshi S.R., Anjana R.M., Deepa M., Pradeepa R., Bhansali A., Dhandania V.K. Prevalence of dyslipidemia in urban and rural India: the ICMRINDIAB study. PLoS One. 2014;9(5) doi: 10.1371/journal.pone.0096808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abdel Wahed W.Y., El-Khashab K., Hassan S.K. Prevalence of Dyslipidaemia among Healthy University Students: Fayoum Governorate, Egypt. Epidemiol Biostatistics Public Health. 2016;13(1–9) [Google Scholar]
- 9.Brown B.G., Stukovsky K.H., ZhaoX -Q. Simultaneous low-density lipoprotein- C lowering and high-density lipoprotein-C elevation for optimum cardiovascular disease prevention with various drug classes, and their combinations: a meta-analysis of 23 randomized lipid trials. Curr Opin Lipidol. 2006;17(6):631–636. doi: 10.1097/MOL.0b013e32800ff750. [DOI] [PubMed] [Google Scholar]
- 10.Baigent C., Blackwell L., Emberson J., Holland L.E., Reith C., Bhala N. Cholesterol Treatment Trialists' (CTT) Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–1681. doi: 10.1016/S0140-6736(10)61350-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heidenreich P.A., Trogdon J.G., Khavjou O.A., Butler J., Dracup K., Ezekowitz M.D. Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation. 2011;123:933–944. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 12.Nichols M., Townsend N., Luengo-Fernandez R., Leal J., Gray A., Scarborough P., Rayner M. European Heart Network; Brussels: 2012. European cardiovascular disease Statistics, 2012.https://www.escardio.org/static_file/Escardio/Press-media/press-releases/2013/EU-cardiovascular-disease-statistics-2012.pdf [Google Scholar]
- 13.RamahiTM Cardiovascular disease in the Asia Middle East region: global trends and local implications. Asia Pac J Public Health. 2010;22(3):83S–89S. doi: 10.1177/1010539510373034. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization . 2018. Non-communicable diseases (NCD) country profiles.http://www.who.int/nmh/countries/yem_en.pdf Retrieved 21 August 2018. Available at: [Google Scholar]
- 15."Statistical Yearbook 2011". Central Statistical Organization. Retrieved 24 February 2013. Available at: https://en.wikipedia.org/wiki/Ibb_Governorate.
- 16.Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. Executive summary of the third report of the national cholesterol education program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 17.Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363:157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 18.Anuurad E., Shiwaku K., Nogi A., Kitajima K., Enkhmaa B., Shimono K. The new BMI criteria for Asians by the regional office for the western pacific region of who are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J Occup Health. 2003;45:335–343. doi: 10.1539/joh.45.335. [DOI] [PubMed] [Google Scholar]
- 19.WHO . 2008. Waist circumference and Waist–Hip ratio: report of a WHO expert consultation Geneva.http://apps.who.int/iris/bitstream/handle/10665/44583/9789241501491_eng.pdf;jsessionid=D2E418D4CBF0B6D1B15F51ED10FF4A08?sequence=1 8–11 December. [Google Scholar]
- 20.Al-Motarreb A., Al-Habori M., Broadley K.J. Khat chewing, cardiovascular diseases and other internal medical problems: the current situation and directions for future research. J Ethnopharmacol. 2010;132:540–548. doi: 10.1016/j.jep.2010.07.001. [DOI] [PubMed] [Google Scholar]
- 21.Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC7) The seventh report of the joint national committee on the prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 22.Qi L., Ding X., Tang W., Li Q., Mao D., Wang Y. Prevalence and risk factors associated with dyslipidemia in Chongqing, China. Int J Environ Res Publ Health. 2015;12:13455–13465. doi: 10.3390/ijerph121013455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kassim S., Islam S., Croucher R. Validity and reliability of a severity of dependence scale for khat (SDS-khat) J Ethnopharmacol. 2010;132(3):570–577. doi: 10.1016/j.jep.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 24.Ali A.A. Qat habit in Yemen society: a causative factor for oral periodontal diseases. Int J Environ Res Publ Health. 2007;4(3):243–247. doi: 10.3390/ijerph2007030008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Teni F.S., Surur A.S., Hailemariam A., Aye A., Mitiku G., Gurmu A.E. Prevalence, reasons, and perceived effects of Khat chewing among students of a college in Gondar town, Northwestern Ethiopia: a cross-sectional study. Ann Med Health Sci Res. 2015;5:454–460. doi: 10.4103/2141-9248.177992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mahfouz M.S., Rahim B.E.A., Solan Y.M.H., Makeen A.M., Alsanosy R.M. Khat Chewing Habits in the Population of the Jazan Region, Saudi Arabia: prevalence and Associated Factors. PLoS One. 2015;10(8) doi: 10.1371/journal.pone.0134545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Engidawork E. Pharmacological and toxicological effects of catha edulis F. (Khat) Phytother Res. 2017;31(7):1019–1028. doi: 10.1002/ptr.5832. [DOI] [PubMed] [Google Scholar]
- 28.Khader Y.S., Batieha A., El-Khateeb M., Al Omari M., Ajlouni K. Prevalence of dyslipidemia and its associated factors among Jordanian adults. J Clin Lipidol. 2010;4(1):53–58. doi: 10.1016/j.jacl.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 29.AlMajed H.T., AlAttar A.T., Sadek A.A., AlMuaili T.A., AlMutairi O.A., Shaghouli A.S. Prevalence of dyslipidemia and obesity among college students in Kuwait. Alexandria J Med. 2011;47:67–71. [Google Scholar]
- 30.Aguilar-Salinas C.A., Gomez- Perez F.J., Rull J., Villalpando S., Barquera S., Rojas R. Prevalence of dyslipidemias in the Mexican national health and nutrition survey 2006. Salud Publica Mex. 2010;52(Suppl 1):S44–S53. doi: 10.1590/s0036-36342010000700008. [DOI] [PubMed] [Google Scholar]
- 31.Sawant A.M., Shetty D., Mankeshwar R., Ashafid T.F. Prevalence of dyslipidemia in young adult Indian population. J Assoc Phys India. 2008;56:99–102. [PubMed] [Google Scholar]
- 32.World development Indicators 2010. The World Bank; Washington, DC, USA: 2014. [Google Scholar]
- 33.U.S. Dept. of Health and Human Services . 2008. 2008 physical activity Guidelines for Americans.https://health.gov/paguidelines/pdf/paguide.pdf January 30, 2012. [Google Scholar]
- 34.Lemieux A.M., Li B., Al' Absi M. Khat use and appetite: an overview and comparison of amphetamine, khat and cathinone. J Ethnopharmacol. 2015;160:78–85. doi: 10.1016/j.jep.2014.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al-Sharafi B.A., Gunaid A.A. Effect of habitual khat chewing on glycemic control, body mass index, and age at diagnosis of diabetes in patients with type 2 diabetes mellitus in Yemen. Clin Med Insights Endocrinol Diabetes. 2015;8:47–53. doi: 10.4137/CMED.S26045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shawar S.M., Al-Bati N.A., Al-Mahameed A., Nagalla D.S., Obeidat M. Hypercholesterolemia among apparently healthy university students. Oman Med J. 2012;27(4):274–280. doi: 10.5001/omj.2012.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Al-Kaabba A.F., Al-Hamdan N.A., Ahmed El Tahir, Abdalla A.M., Saeed A.A., Hamza M.A. Prevalence and correlates of dyslipidemia among adults in Saudi Arabia: results from a national survey open. J Endocrine Metabolic Dis. 2012;2:89–97. [Google Scholar]
- 38.Grabauskas V., Miseviciene I., Klumbiene J., Petkeviciene J., Milasauskiene Z., Plieskiene A. Prevalence of dyslipidemias among Lithuanian rural population (CINDI program) Medicina (Kaunas) 2003;39(12):1215–1222. [PubMed] [Google Scholar]
- 39.Darroudi S., Saberi-Karimian M., Tayefi M., Arekhi S., Motamedzadeh Torghabeh A., Seyedzadeh Sani S.M.R. Prevalence of combined and noncombined dyslipidemia in an Iranian population. J Clin Lab Anal. 2018 doi: 10.1002/jcla.22579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Al-Sabah H.A., Hussain N.H., Ali D.T. Dyslipidemia in young adults aged (20-40) years attending Baghdad teaching hospital and Al-mansour primary health care center in Baghdad city. Iraqi Postgrad Med J. 2014;13:320–327. [Google Scholar]
- 41.Hamam F. Dyslipidemia and related risk factors in a Saudi university community. Food Nutr Sci. 2017;8:56–69. [Google Scholar]
- 42.Allam A.R., Taha I.M., Al-Nozha O.M., Sultan I.E. Nutritional and health status of medical students at a university in Northwestern Saudi Arabia. Saudi Med J. 2012;12:1296–1303. [PubMed] [Google Scholar]
- 43.Ahmed A.M., Elabid B.H., Elhassan K.H., Waggiallah H.A. Metabolic syndrome among undergraduate students attending medical clinics for obligatory medical screening. Trop J Pharmaceut Res. 2015;14(2):317–321. [Google Scholar]
- 44.Mula-Abed W.A., Chilmeran S.K. Prevalence of dyslipidemia in the Iraqi adult population. Saudi Med J. 2007;12:1868–1874. [PubMed] [Google Scholar]
- 45.Asiki G., Murphy G.A.V., Baisley K., Nsubuga R.N., Karabarinde A., Newton R. Prevalence of Dyslipidaemia and Associated Risk Factors in a Rural Population in South-Western Uganda: a Community Based Survey. PLoS One. 2015;10(5) doi: 10.1371/journal.pone.0126166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stone N.J. Secondary causes of hyperlipidemia. Med Clin. 1994;78:117–141. doi: 10.1016/s0025-7125(16)30179-1. PMID: 8283927. [DOI] [PubMed] [Google Scholar]
- 47.Chait A., Brunzell J.D. Acquired hyperlipidemia (secondary dyslipoproteinemias) Endocrinol Metab Clin N Am. 1990;19:259–278. PMID: 2192873. [PubMed] [Google Scholar]
- 48.Aguilar-Salinas C.A., Olaiz G., Valles V., Torres J.M.R., Pérez F.J.G., Rull J.A. High prevalence of low HDL cholesterol concentrations and mixed hyperlipidemia in a Mexican nationwide survey. J Lipid Res. 2001;42:1298–1307. PMID: 11483632. [PubMed] [Google Scholar]
- 49.Brinton E.A., Eisenberg S., Breslow J.L. A low-fat diet decreases high density lipoprotein (HDL) cholesterol levels by decreasing HDL apolipoprotein transport rates. J Clin Invest. 1990;85:144. doi: 10.1172/JCI114405. PMID: 2104877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Assadi S.N. What are the effects of psychological stress and physical work on blood lipid profiles? Medicine (Baltim) 2017;96(18) doi: 10.1097/MD.0000000000006816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Catalina-Romero C., Calvo E., Sánchez-Chaparro M.A., Valdivielso P., Sainz J.C., Cabrera M. The relationship between job stress and dyslipidemia. Scand J Publ Health. 2013;41(2):142–149. doi: 10.1177/1403494812470400. [DOI] [PubMed] [Google Scholar]
- 52.Bartlett J., Predazzi I.M., Williams S.M., Bush W.S., Kim Y., Havas S. Is isolated low HDL-C a CVD risk factor?: new insights from the framingham offspring study. Circ Cardiovasc Qual Outcomes. 2016;9(3):206–212. doi: 10.1161/CIRCOUTCOMES.115.002436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Erem C., Hacihasanoglu A., Deger O., Kocak M., Topbas M. Prevalence of dyslipidemia and associated risk factors among Turkish adults: trabzon lipid study. Endocrine. 2008;34:36–51. doi: 10.1007/s12020-008-9100-z. [DOI] [PubMed] [Google Scholar]
- 54.Bibiloni M.M., Salas R., Pons A., Tur J.A. Prevalence of dyslipidaemia and associated risk factors among balearic islands adolescents, a mediterranean region. Eur J Clin Nutr. 2015;69:722–728. doi: 10.1038/ejcn.2014.236. [DOI] [PubMed] [Google Scholar]
- 55.Washington R.L. Interventions to reduce cardiovascular risk factors in children and adolescents. Am Fam Phys. 1999;59(8):2211–2218. [PubMed] [Google Scholar]
- 56.Desouky D.S., Omar M.S., Nemenqani D.M., Jabbar J., Tarak-Khan N.M. Risk factors of non-communicable diseases among female university students of the health colleges of Taif university. Int J Med Sci. 2004;6:97–107. [Google Scholar]