Abstract
Objectives
This study aimed to evaluate the psychological effects of cleft lip and palate (CLP) on children and their parents and to determine any relationship between social support and timing of surgical repairs for these defects.
Methods
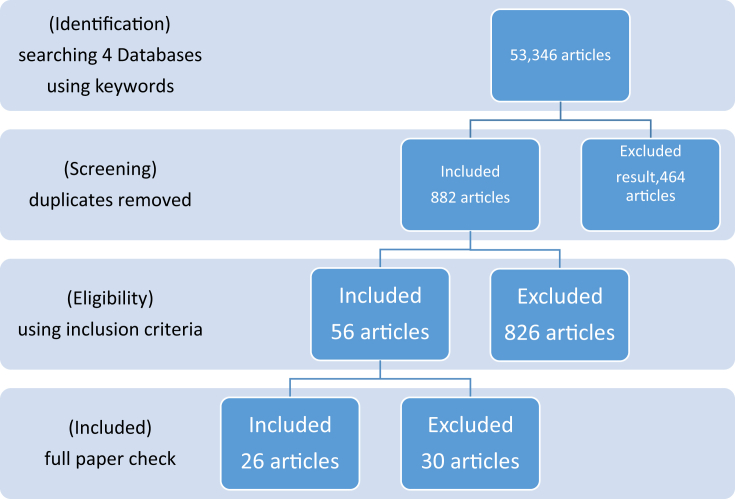
A systematic review that followed the problem, intervention, comparison, outcome and setting (PICOS) method was used. The participants were children with CLP, interventions were surgical corrections and/or social support, comparison occurred with children with neither surgical corrections nor social support, outcomes were psychological effects and the study design was a systematic review. Four electronic databases, EBSCO, ProQuest, Science Direct, and PsycInfo were used to search for studies over the period of ten years (January 2007 until January 2017). The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2009 guidelines on systematic review reporting were used for this study.
Results
Searching through four databases revealed 53,346 articles; however, only 26 articles that met the inclusion criteria were included. There were few articles about children.
Conclusions
CLP is not only connected to psychological effects which distress children's self-esteem and psychological functions, it also extends to their parents, particularly their mothers. However, parental and social support seem to have positive influences by reducing these psychological effects.
Keywords: Children, Cleft, Lip, Palate, Psychological
الملخص
أهداف البحث
تهدف هذه الدراسة لتقييم الآثار النفسية للشفة والحنك المشقوق على الأطفال وأولياء أمورهم وتحديد أي علاقة بين الدعم الاجتماعي، ووقت الإصلاحات الجراحية لهذه العيوب.
طرق البحث
مراجعة منهجية باستخدام طريقة المشكلة، والتدخل، والمقارنة، والنتيجة والإعداد. وشارك في الدراسة أطفال لديهم شفة وحنك مشقوق، والتدخلات هي التصحيحات الجراحية، و/أو الدعم الاجتماعي، وكانت المقارنات مع الأطفال الذين ليس لديهم تصحيحات جراحية ولا دعم اجتماعي، وكانت النتائج هي الآثار النفسية، وكان تصميم الدراسة هو مراجعة منهجية. تم البحث في أربع قواعد بيانات إلكترونية: إبسكو، وبروكويست، وسسينس دايريكت، وسيك انفو على مدى عشر سنوات (يناير ٢٠٠٧ إلى يناير ٢٠١٧). واستخدمت القواعد الإرشادية لعناصر التقارير المفضلة للمراجعة المنهجية وتحليل – ميتا (بريزما) ٢٠٠٩ بشأن الإبلاغ عن المراجعات المنهجية في هذه الدراسة.
النتائج
كشف البحث في أربع قواعد للبيانات ٥٣٣٤٦ مقالة; ولكن، استوفت ٢٦ مقالة فقط معايير الاشتمال وتم إدراجها. كان هناك عدد قليل من المقالات التي تعنى بالأطفال.
الاستنتاجات
الشفة والحنك المشقوق لا ترتبط فقط بالآثار النفسية التي كانت تزعج تقدير الذات لدى الأطفال ووظائفهم النفسية، بل تمتد أيضا إلى آبائهم، وخاصة الأمهات. ومع ذلك، بدا أن الدعم الأبوي والاجتماعي له نتائج إيجابية على الحد من هذه الآثار النفسية.
الكلمات المفتاحية: نفسي, الأطفال, الشق, الشفة, الحنك
Introduction
In recent decades, there has been a great increase in emphasis related to the rights of children in policy and research health, psychology and the wider society.1 Cleft lip and/or palate (CLP) is one of the most common congenital anomalies that affect the orofacial area. The cleft pathogenesis occurs because of failure of the fusion of numerous facial processes early in the embryonic development.2 Orofacial clefts involve the structures around the oral cavity and could be extended to the surrounding area in a comprehensive craniofacial deformity. The isolated cleft lips, with/or without the cleft palate, are the core categories that children could have as part of a child's syndrome.3, 4
Although there have been several attempts to record the frequency of birth defects,5 in some parts of the world, namely Africa, Asia, and Eastern Europe, there is no continuous availability of data on CLP frequency.6 In the Middle East, there is lack of data on CLP occurrence; there seems to be a general idea of facial cleft incidences in the region. A study by Fida et al. found that 1.9 orofacial malformations per 1000 live births were reported in the western area of KSA.7 Another hospital-based study in Riyadh found a high rate of cranial anomalies; 7.98 per 1000 pregnancies were reported at a women's specialized hospital (King Fahad medical city).8 In the United Arab of Emirates, 0.3 per 1000 births had orofacial cleft congenital.9 In Oman, the rate of oral clefts was 1.5 per 1000 births; whereas in Jordan, it was at 2.4 facial orofacial clefts.10
Studies have shown that environment and genetics are considered as the core aetiology of CLP. Moreover, the deficiency of folic acid, maternal age, mothers who smoke or consume alcohol, and viral infection were all risk factors that correlated to cleft development.3, 4
CLP is not considered as a detriment to life. However, there are real consequences that resulted from a cleft even if there is an intervention early in the child's life; in addition to the potential of adverse health effects in the long term that were related to functional and psychological problems.3, 4 Children with orofacial clefts may endure numerous surgical and non-surgical treatments from birth until adulthood, which psychologically affects both the children and their family members.11 Treatment of infants with cleft palate requires a multidisciplinary approach. In many cases, infants of age two to six months already had lip repair; however, the palate was deferred until they were one to two years old as negative effects on the growth and development of the maxilla might be caused due to early repair via scar tissue of the maxilla.11 While delaying the surgical procedure, it is essential that adequate nutrition is maintained to allow for normal growth of the newborn as this would prepare the infant for future surgery to counter the abnormality.11
According to several studies conducted around the globe on this issue, it was agreed that physical and psychological rehabilitations are on the same level of importance, and should not be ignored so that a full recovery could be attained, as well as to elevate the patient's self-esteem and mental health.12 The psychosocial issues of children with CLP during their developmental age affect normal social interaction by increasing the chances of low self-esteem and shyness.13 Therefore, the objectives of this study are to evaluate the psychological effects of CLP on children and their parents, and to investigate the relationship between social support and time of surgical repairs for these effects. This systematic review using the PICOS method comprises children with CLP as participants, interventions of surgical corrections and social support compared to those with neither surgical corrections nor social support, and the outcomes of psychological effects.
Materials and Methods
A systematic review using the PICOS method, considering children with CLP as participants, interventions of surgical corrections and social support compared to those with no surgical corrections nor social support, the outcomes of psychological effects, and a systematic review study design that followed the PRISMA 2009 checklist on reporting systematic reviews was used in this study. However, some items in the methods and results sections were not applicable to a systematic review, but were applicable to meta-analysis; so, they were represented as not applicable (N/A) as shown in Table 1.
Table 1.
PRISMA checklist.
| Section/topic | # | Checklist item | Reported on page # |
|---|---|---|---|
|
Title | |||
| Title |
1 |
Identify the report as a systematic review, meta-analysis or both. |
1 |
|
Abstract | |||
| Structured summary |
2 |
Provide a structured summary including background, objectives, data sources, study eligibility criteria, participants, interventions, study appraisal and synthesis methods, results, limitations, conclusions and implications of key findings, and a systematic review registration number, as applicable. |
2 |
|
Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | 3 |
| Objectives |
4 |
Provide an explicit statement of questions addressed according to participants, interventions, comparisons, outcomes and study design (PICOS). |
4 |
|
Methods | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g. Web address) and, if available, provide registration information including a registration number. | N/A |
| Eligibility criteria | 6 | Specify the study characteristics (e.g. PICOS, length of follow-up) and report characteristics (e.g. years considered, language, publication status) used as criteria for eligibility and provide a rationale for use. | 5 |
| Information sources | 7 | Describe all the information sources (e.g. databases with dates of coverage, contact with the research authors to identify additional studies) used in the search and the date they were last searched. | 5 |
| Search | 8 | Present a full electronic search strategy for at least one database, including any limits used so that it could be repeated. | 5 |
| Study selection | 9 | State the process for selecting studies (i.e. screening, eligibility, inclusion in the systematic review and, if applicable, inclusion in the meta-analysis). | 5 |
| Data collection process | 10 | Describe the method of data extraction from reports (e.g. piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | 5 |
| Data items | 11 | List and define all the variables for which data were sought (e.g. PICOS, funding sources) and any assumptions and simplifications made. | N/A |
| Risk of bias in individual studies | 12 | Describe the methods used for assessing individual studies' risk of bias (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | N/A |
| Summary measures | 13 | State the principal summary measures (e.g. risk ratio, difference in means). | N/A |
| Synthesis of results | 14 | Describe the methods of handling data and combining the results of studies, if this occurred, including measures of consistency (e.g. I2) for each meta-analysis. | N/A |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g. publication bias, selective reporting within studies). | N/A |
| Additional analyses |
16 |
Describe the methods of additional analyses (e.g. sensitivity or subgroup analysis, meta-regression), if these occurred, indicating which were pre-specified. |
N/A |
|
Results | |||
| Study selection | 17 | Provide the numbers of studies screened, assessed for eligibility and included in the review, with reasons for exclusions at each stage ideally with a flow diagram. | 6 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g. study size, PICOS, follow-up period) and provide citations. | N/A |
| Risk of bias within studies | 19 | Present the data on risk of bias of each study and, if available, any outcome level assessment (see item 12). | N/A |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms) and for each study present (a) simple summary data for each intervention group and (b) effect estimates and confidence intervals, ideally with a forest plot. | 6–9 |
| Synthesis of results | 21 | Present results of each meta-analysis done including confidence intervals and measures of consistency. | N/A |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15). | N/A |
| Additional analysis |
23 |
Provide results of additional analyses, if these occurred (e.g. sensitivity or subgroup analyses, meta-regression [see Item 16]). |
N/A |
|
Discussion | |||
| Summary of evidence | 24 | Summarise the main findings including the strength of evidence for each main outcome and consider their relevance to key groups (e.g. healthcare providers, users, policy makers). | 10 |
| Limitations | 25 | Discuss limitations at the study, outcome level (e.g. risk of bias) and review level (e.g. incomplete retrieval of identified research, reporting bias). | 10 |
| Conclusions |
26 |
Provide a general interpretation of the results in the context of other evidence and implications for future research. |
11 |
|
Funding | |||
| Funding | 27 | Describe sources of funding for the systematic review, other support (e.g. supply of data) and the role of funders for the systematic review. | No Funding |
The first step in this study started by AA who searched four electronic databases, EBSCO, ProQuest, Science Direct, and PsycInfo, over a period of ten years (January 2007 to January 2017) using the following keywords psychological, effects, children, cleft lip and/or palate, the repeated results were deleted. The second step was completed by AH, who screened articles based on the inclusion criteria of children of age (birth to 18 years), healthy children with American Society of Anesthesiologists scale class I and II, articles that were published in English and all types of studies that were published between January 2007 and January 2017, excluding those that did not meet the inclusion criteria. The third step was the extraction of results, which was completed by both authors using a standard formulated table based on the inclusion criteria for data collection.
The primary outcome was the psychological effects of CLP on children and their parents, whereas the secondary outcomes comprised the relationship between social support, time of the surgical treatment (the age of the child) and these psychological effects.
Results
After an extensive electronic search of four databases using appropriate keywords, 53,346 articles were identified including duplicate research. Most of the identified studies were about surgical corrections and/or analysis of complications related to CLP surgical corrections or were among adult participants; therefore, they were excluded and only 26 articles were included. Details of the process of article selection throughout the study is presented in the flow diagram shown in Figure 1. The summary of the 26 included articles is shown in Table 2.
Figure 1.
Articles flow diagram.
Table 2.
Summary of the 26 included articles.
| First author | Year of publication | Country | Participants' age | Sample size | Main findings | Presence of psychological problems |
|---|---|---|---|---|---|---|
| 1-Stock NM | 2016 | United Kingdom | Diagnosis at 18 months, 3 years, 5 years and 8 years old | Not reported | Adjustment and other risk/protective factors that are measurable across key developmental periods | Yes |
| 2-Feragen KB | 2015 | United Kingdom | 16 years | 857 | Cognitive, emotional, behavioural, appearance-related and psychosocial adjustment | Yes |
| 3-Feragen KB | 2016 | United Kingdom | 10 years | 845 | Satisfaction with appearance and associated conditions | No |
| 4-Nilsson S | 2012 | Sweden | Children born in 1987–1993 until 1st of January 2008 | Not reported | Psychological health of children and their mothers, and wither the higher effect of CL alone or associated with OFC | Yes |
| 5-Klassen AF | 2011 | United Kingdom | Not reported | Ranged from 23 to 661 in 9 countries | Quality of life involving physical, psychological and social aspects | Yes |
| 6-Feragen KB | 2014 | United Kingdom | 10 years | Not reported | Visibility of the cleft, adjustment and associated conditions | Yes |
| 7-Chimruang J | 2011 | Thailand | Not reported | 18 | Parental support, physical symptoms, functional limitations, emotional wellbeing and social wellbeing | Yes |
| 8-Hexem KR | 2013 | Tegucigalpa, Honduras | Not reported | 45 | Expectations of parents about feeding, speech and overall wellbeing of their children, and postoperative satisfaction. | Yes |
| 9-Pradubwong S | 2014 | Thailand | 5–6 years | 39 | Quality of life, speech, hearing, dental treatment and communication skills | No |
| 10-Broder HL | 2014 | United States | 11.8 years (mean) | 1200 | Preoperative psychological health | Yes |
| 11-Mahalingam S | 2013 | United Kingdom | Not reported | 24 | Ethnic group, effect of teasing and bullying on the child self-esteem | Yes |
| 12-Chua HD | 2012 | Hong Kong | Not reported | Not reported | Comparison of maxillary distraction osteogenesis and conventional orthognathic surgery and patients satisfaction. | Yes |
| 13-Lorot-Marchand | 2015 | United States | 15 years (mean) | 55 | Taunting, daily lives, self-perception and effect on educational level | Yes |
| 14-Jeong JH | 2013 | Korea | Not reported | 36 | Psychological states and stress levels of the Korean mothers of CLP patients | Yes |
| 15-Wang Y | 2013 | China | Not reported | 102 | Significance of somatisation, obsessive-compulsive symptoms, depression and anxiety among mothers | Yes |
| 16-Grollemund B | 2012 | France | Parents and children were seen twice, when the child is 4 months old and when the child was one year old | Not reported | Child distress, withdrawal, importance of prenatal diagnosis, relational development with the child, self-image and quality of life. | Yes |
| 17-Hasanzadeh N | 2014 | Iran | Not reported | 55 | Coping strategies and psychological distress among mothers | Yes |
| 18-Feragen KB | 2014 | United Kingdom | Not reported | 754 | Prevalence of conditions that affect cognitive and/or psychosocial functioning | Yes |
| 19-Broder HL | 2014 | United States | 11.8 years (mean) | 1200 | Self-esteem and it's relation | Yes |
| 20-Wang Y | 2009 | United States | Not reported | 204 | Anxiety and depression among parents | Yes |
| 21-Gajarao HM | 2015 | India | Not reported | 60 | Psychiatric problems among mothers | Yes |
| 22-Beluci ML | 2016 | Sau Paulo, Brazil | Not reported | 50 | Psychological disability, social disability and physical handicap | Yes |
| 23-Alansari R | 2014 | KSA | Not reported | 11 | Stigma, negative self-perception and defectiveness | Yes |
| 24-Augsornwan D | 2011 | Thailand | 8–18 years | 15 | Postoperative self-perception, worrying about scaring and further treatment | No |
| 25-Zamora Linares CE | 2010 | Spain | 10 years | 92 | Self-esteem and dependence on others | Yes |
| 26-Gong C | 2011 | China | Not reported | 100 | Effect of psychological counselling among parents | Yes |
Discussion
The aesthetics of children with CLP was not the only issue among the research participants. They had considerable functional difficulties including “speech anomaly, and difficulty feeding/swallowing because of the oral seal issue. Moreover, they could also have hearing loss, and recurring ear infection due to palatal musculature abnormality”.3, 4 The psychological effects were not just associated with children with CLP, but also extended to their family facing different levels of anxiety and depression.14
In general, the literature suggested that individuals' psychosocial health was not deeply affected by having CLP.15 However, it revealed that the psychosocial functioning of children with CLP was concealed by certain issues that they had in relation to additional conditions such as coping and adjustment strategies, self-confidence, being bullied, acceptance of their facial appearance, surgical outcome satisfaction, communication, parents' anxiety, depression, and burden on family income.15, 16, 17, 18, 19
Children's overall psychosocial functioning appeared to be satisfactory among children with non-syndromic CLP.15 Few influencing factors have been reported that led to this satisfaction such as social support which had a dominant impact of leading to better psychological results assessed using multiple psychological assessment tools.15, 16, 17, 18, 19, 20 In addition, socioeconomic status had a prominent effect on both patients' wellbeing and family satisfaction.15 On the other hand, psychological analysis of depression, anxiety, obsessive compulsive disorder and stress levels of parents indicated weak psychosomatic states.21, 22
Depression was higher among non-working mothers when compared to working mothers.23 The birth order of the child had a major impact on mothers' psychological status; higher anxiety and depression were associated with the eldest child.23 There were higher parent self-blaming scores among mothers compared to fathers.24 Anxiety and depression were reported more in mothers of girls with CLP and if the child's age was less than three months when compared to boys and older children.23
Long duration of hospitalisation appeared to have negative outcomes on both the child and mother; mothers may experience physical and/or psychological issues from the distressing events of having a child with CLP.25 Anxious children are more likely to show behavioural problems and be more introverted in expressing their judgement regarding doctors. Therefore, they will be more difficult to treat.15 The choice of behavioural management techniques must be based on an evaluation that weighs the risks versus benefits for the child.15 There were several considerations included in the decision-making process for the selection of appropriate behavioural management methods; urgency of care, need for cooperation, practitioner's skill, facilities available at each clinic, and parental considerations and expectations.15 Moreover, the use of video modelling with children with CLP could be an effective method to reduce anxiety and the fear of the unknown among anxious children.26
Girls with CLP showed higher symptoms of mood swings and emotional instability than boys.20, 27 Children with CLP who had at least one condition in addition to the cleft such as “developmental delay, attention deficient hyperactive disorder, a specific language impairment or dyslexia have reported more significant psychological difficulties than children with cleft alone”.20, 28 Reports have shown that no support was found for cleft visibility as a risk factor for psychological impairment by itself.29, 30 The experience of patients with CLP during the treatment course has changed over time, while among youth and adolescents most patients experienced stigma, negative self-perception, and lower self-esteem.16, 17, 18, 19
Taunting was common among children with CLP, which had an immense effect on the daily lives and self-confidence of patients with CLP or CLP repair process.19 Bullying usually started in primary school and reached the peak of violence in middle school.19 These children were reported as experiencing long-lasting sadness and depression due to intimidation caused by bullying, which also affected their school attendance and educational level; eventually, half of these children repeated their first few years of primary school.19 Conversely, one study showed no differences in school function between children with CLP and those without CLP.31 A Chinese study analysed the causes of psychological deviation and uniqueness of cleft patients and found that psychological interference was one of the most important aspects in CLP management plans.14
After some children with CLP were interviewed about their lifelong experience with CLP, it was reported that they recalled the long complicated and painful treatment process and that the hardest part was their feelings of being different to their peers; stigmatised, socially undesirable, and receiving more attention than others, which was worse than the physical burden.16 These thoughts had affected their self-perception as worthless, strange and abnormal, which resulted in less desirable psychological outcomes of the treatment process.16 Several events exaggerated these feelings such as waiting in a clinic with patients categorised as having facial deformities or having the immediate postsurgical look, which was even more annoying because of bandages, stitches, bruises, and fixation devices.16
The timing of surgical corrections appeared to be an important factor. Hence, the longer the delay before the first surgical interference, the higher the chance of affecting the parents' psychological perceptions.32
A comparative study of the outcomes of two types of surgical corrections, maxillary distraction ontogenesis (DO) and conventional orthognathic surgery (CO), found that social avoidance, low self-esteem and high stress levels were reported among patients who received DO.33 Since DO patients were wearing maxillary distractors with activating rods sticking into the oral cavity just immediately after their surgical correction and for three months postoperatively, they had limited physical and social activities.33 Whereas, CO group were satisfied with their immediate reasonable results and were capable to get back normally to their usual social life.33 These two temporary factors were proof of how facial appearance could affect those patients. However, reports showed that DO and CO patients had equal social avoidance and distress years after their surgical procedure.33 In contrast, another study confirmed that surgical repair of dentofacial anomaly enhanced patients' quality of life and encouraged the impact upon their oral health state.15 It was found that after definitive surgical correction, patients' self-perception improved which led them to recognise treatment advantages and reconsider the treatment journey as acceptable rather than burdensome.16
In earlier studies, two subgroups seemed to be identified as adolescents and adults in which the adolescent subgroup tended to have lower self-esteem than the adult subgroup. In the case of the adolescent subgroup, it was found that family support was key in increasing their self-esteem.34, 35 Indeed, family and social support have had significant positive effects.15, 20, 21, 22, 23 There is a lack of randomised clinical trials among children with CLP, which could be due to the difficulty to use blind randomisation with these patients. However, a randomised clinical trial study design is always recommended.
Regarding the limitations of this systematic review, it could include adults and children as most of the psychological effects of CLP studies were performed in adult populations. However, the aim of this study was to review the psychological effects of CLP on children and their parents. Moreover, this systematic review included articles that were published in English; if other languages were included it could have revealed more articles. Hence, it is highly recommended that future studies include articles in multiple languages. Furthermore, as children were all treated in the same way in this study, future research could study each age group separately since psychological impacts would potentially vary among toddlers, pre-teens and teenagers. It is also useful if future studies address the cultural background and age of mothers of children with CLP, as these factors could have a direct effect on their psychological status.
Conclusions
CLP is not only related to psychological effects which distress children's self-esteem and their psychological functions, it also extends to their parents, especially mothers. However, parental and social support seem to have positive influences on reducing these psychological effects.
Source of funding
No funds were received for this study.
Conflict of interest
Both authors confirm that there are no conflicts of interest.
Ethical approval
Not required as this study was a systematic review of articles.
Consent
Not required as this study was a systematic review of articles.
Authors' contribution
AA was the one who designed this research methods, analysed results and wrote this paper. AH was the one who extracted results and helped in preparing of this paper. However, both authors have worked together in searching for articles. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.James A., Jenks C., Prout A. Polity Press; Cambridge: 1998. Theorising childhood. [Google Scholar]
- 2.Proffit W.R., Fields H.W. 3rd ed. Elsevier Mosby; St. Louis, MO: 2000. Contemporary orthodontics; pp. 66–69. [Google Scholar]
- 3.Wong F.W., King N.M. The oral health of children with clefts, a review. Cleft Palate Craniofac J. 1998;35:248–254. doi: 10.1597/1545-1569_1998_035_0248_tohocw_2.3.co_2. [DOI] [PubMed] [Google Scholar]
- 4.Hunt O., Burden D., Hepper P., Johnston C. The psychosocial effects of cleft lip and palate: a systematic review. Eur J Orthod. 2005;27:274–285. doi: 10.1093/ejo/cji004. [DOI] [PubMed] [Google Scholar]
- 5.Health-care burden of craniofacial anomalies: report of WHO meetings on international collaborative research on craniofacial anomalies, Geneva, Switzerland, 5–8 November 2000. 24-26 May 2001. Park City, Utah, U. S. A. [Google Scholar]
- 6.WHO 2001 . 2001. Global registry and database on craniofacial anomalies: report of a WHO registry meeting on craniofacial anomalies WHO registry meeting on craniofacial anomalies. Bauru, Brazil. [Google Scholar]
- 7.Fida N.M., Al-Aama J., Nichols W., Alqahtani M. A prospective study of congenital malformations among live born neonates at a University Hospital in Western Saudi Arabia. Saudi Med J. 2007;28:1367–1373. [PubMed] [Google Scholar]
- 8.Sallout B.I., Al-Hoshan M.S., Attyyaa R.A., Al Suleimat A.A. Antenatal diagnosis, prevalence and outcome of major congenital anomalies in Saudi Arabia: a hospital-based study. Ann Saudi Med. 2008;28:272–276. doi: 10.5144/0256-4947.2008.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al Hosani H., Salah M., Abu-Zeid H., Farag H.M., Saade D. The national congenital anomalies register in the United Arab Emirates. East Mediterr Health J. 2005;11:690–699. [PubMed] [Google Scholar]
- 10.Aqrabawi H.E. Facial cleft and associated anomalies: incidence among infants at a Jordanian medical centre. East Mediterr Health J. 2008;14:356–359. [PubMed] [Google Scholar]
- 11.Grabber T.M., Vanarsdall R.L., Vig K.W.L. 4th ed. Elsevier Mosby; St. Louis, MO: 2005. Orthodontics: current principals and techniques; pp. 1097–1121. [Google Scholar]
- 12.Khargekar N., Khargekar V., Rajan S. Cleft lip and palate-A psychology insight. Sci Publ Group. 2016;5(4):37. [Google Scholar]
- 13.De Sousa A., Devare S., Ghanshani J. Psychological issues in cleft lip and cleft palate. J Indian Assoc Pediatr Surg. 2009;14(2) doi: 10.4103/0971-9261.55152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi B., Zheng Q. It is necessary to do psychological intervention for patients with cleft lip and palate. West China J Stomatol. 2010;28(4) [PubMed] [Google Scholar]
- 15.Chimruang J., Soadmanee O., Srisilapanan P., Patjanasoontorn N., Nanthavanich N., Chuawanlee W. A qualitative study of health-related quality of life and psychosocial adjustments of Thai adolescents with repaired cleft lips and palates. J Med Assoc Thai. 2011;94(6):S45–S50. [PubMed] [Google Scholar]
- 16.Alansari R., Bedos C., Allison P. Living with cleft lip and palate: the treatment journey. Cleft Palate Craniofac J. 2014;51(2):229. doi: 10.1597/12-255. [DOI] [PubMed] [Google Scholar]
- 17.Augsornwan D., Namedang S., Pongpagatip S., Surakunprapha P. Quality of life in patients with cleft lip and palate after operation. J Med Assoc Thai. 2011;94:124–128. [PubMed] [Google Scholar]
- 18.Zamora LinaresC.E., Sanchez C.N. Psychological aspects in children with cleft lip. Acta Pediatr Esp. 2010;68(4):178. [Google Scholar]
- 19.Lorot-Marchand A., Guerreschi P., Pellerin P., Martinot V., Gbaguidi C.C., Neiva C. Frequency and socio-psychological impact of taunting in school-age patients with cleft lip-palate surgical repair. Int J Pediatr Otorhinolary. 2015;79(7):1041–1048. doi: 10.1016/j.ijporl.2015.04.024. [DOI] [PubMed] [Google Scholar]
- 20.Feragen K.B., Stock N.M., Kvalem I.L. Risk and protective factors at age 16: psychological adjustment in children with a cleft lip and/or palate. Cleft Palate Craniofac J. 2015;52(5):555–573. doi: 10.1597/14-063. [DOI] [PubMed] [Google Scholar]
- 21.Jeong J.H., Kim B.N., Choi T.H., Kim S. A psychological analysis of the Korean mothers of cleft lip and palate patients: screening for psychological counseling and neuropsychiatric treatment. J Craniofac Surg. 2013;24(5):1515–1520. doi: 10.1097/SCS.0b013e31828f2372. [DOI] [PubMed] [Google Scholar]
- 22.Wang Y., Xin Y., Ma J., Xin X., Shi B., Huang Y. Effects of an early psychological intervention on parents of children with cleft lip/palate. Hua xi kou qiang yi xue za zhi. 2013;31(4):372–376. [PubMed] [Google Scholar]
- 23.Gajarao H.M., Podaralla R. Psychiatric problems in mothers of children with cleft lip and palate (CLP) using standardized interviews. Indian J Psychiatry: 67th Annual National Conference of the Indian Psychiatric Society. 2015:S50. [Google Scholar]
- 24.Nelson J., O'Leary C., Weinman J. Causal attributions in parents of babies with a cleft lip and/or palate and their association with psychological well-being. Cleft Palate Craniofac J. 2009;46(4):425–434. doi: 10.1597/07-194.1. [DOI] [PubMed] [Google Scholar]
- 25.Nilsson S., Van L.W., Psouni E., Lyberg-Ahlander V., Merlo J. The psychological health at adolescent age in children born with an orofacial cleft: a life course study. Eur J Epidemiol. 2012;27(1):S42. [Google Scholar]
- 26.Al-Namankany A., Petrie A., Ashley P. Video modelling and reducing anxiety related to dental injections-a randomised clinical trial. Br Dent J. 2014;216(12):675–679. doi: 10.1038/sj.bdj.2014.497. [DOI] [PubMed] [Google Scholar]
- 27.Broder H.L., Wilson-Genderson M., Sischo L., Norman R.G. Examining factors associated with oral health-related quality of life for youth with cleft. Plast Reconstr Surg J. 2014;133(6):828e–834e. doi: 10.1097/PRS.0000000000000221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feragen K.B., Stock N.M., Rumsey N. Toward a reconsideration of inclusion and exclusion criteria in cleft lip and palate: implications for psychological research. Cleft Palate Craniofac J. 2014;51(5):569–578. doi: 10.1597/12-326. [DOI] [PubMed] [Google Scholar]
- 29.Feragen K.B., Stock N.M. Risk and protective factors at age 10: psychological adjustment in children with a cleft lip and/or Palate. Cleft Palate Craniofac J. 2016;53(2):179. doi: 10.1597/14-062. [DOI] [PubMed] [Google Scholar]
- 30.Feragen K.B., Stock N.M. When there is more than a cleft: psychological adjustment when a cleft is associated with an additional condition. Cleft Palate Craniofac J. 2014;51(1) doi: 10.1597/12-328. [DOI] [PubMed] [Google Scholar]
- 31.Klassen A.F., Tsangaris E., Forrest C.R., Wong K.W., Pusic A.L., Cano S.J. Quality of life of children treated for cleft lip and/or palate: a systematic review. J Plast Reconstr Aesthet Surg. 2012;65(5):547–557. doi: 10.1016/j.bjps.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 32.Grollemund B., Guedeney A., Vazquez M.P., Picard A., Soupre V., Pellerin P. Relational development in children with cleft lip and palate: influence of the waiting period prior to the first surgical intervention and parental psychological perceptions of the abnormality. BMC Pediatr. 2012;12:65. doi: 10.1186/1471-2431-12-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chua H.D., Ho S.M., Cheung L.K. The comparison of psychological adjustment of patients with cleft lip and palate after maxillary distraction osteogenesis and conventional orthognathic surgery. Oral Surg Oral Med Oral Pathol Oral Radiol J. 2012;114(5):S5–S10. doi: 10.1016/j.tripleo.2011.07.047. [DOI] [PubMed] [Google Scholar]
- 34.Tabaquim Maria de LourdesMerighi, Marquesini Matilde Aparecida Motta. Study of the stress of parents of patients with cleft lip and palate in a surgical process. Estud Psicolog. 2013;30(4) [Google Scholar]
- 35.Cheung Lim K., Loh John Ser Pheng, Ho Samuel M.Y. Psychological profile of Chinese with cleft lip and palate deformities. Cleft Palate Craniofac J. 2007;52(5):543–554. doi: 10.1597/05-053. [DOI] [PubMed] [Google Scholar]