Abstract
Objectives
This study aimed to validate the accuracy of panoramic radiographic risk signs through detection of presence or absence of corticalization between an impacted mandibular third molar and the inferior alveolar canal on cone beam computed tomography (CBCT).
Methods
This retrospective study analyzed 210 impacted mandibular third molars from 135 patients (aged 17–51 years) who showed one or more of the seven previously established panoramic radiographic risk signs of inferior alveolar nerve exposure. These patients were referred for CBCT examination. Three-dimensional images were used to assess the canal position relative to the third molar, the proximity between the canal and third molar, and third molar angulation. The correlation of panoramic findings and CBCT was evaluated using a Chi-square test.
Results
Panoramic findings of interruption of inferior alveolar canal wall, isolated or combined with one of these signs (darkening of third molar roots, narrowing of canal, and diversion of canal); darkening of the roots; and narrowing of canal were significantly correlated with direct contact between the inferior alveolar canal and impacted third molars on CBCT (P < 0.001).
Conclusion
Preoperative CBCT is recommended for cases showing interruption of canal wall; darkening of the roots or narrowing of the canal; or association between interruption and narrowing, diversion, or darkening of roots in a panoramic view. This study evaluated the risk relationship between the inferior alveolar nerve and impacted mandibular third molars, with the aim of reducing the occurrence of postoperative injury to the inferior alveolar nerve.
Keywords: Cone beam CT, Mandibular canal, Panoramic radiograph, Third molar
الملخص
أهداف البحث
هدفت هذه الدراسة إلى التحقق من دقة علامات الخطورة في التصوير الاشعاعي البانورامي من خلال الكشف عن وجود أو عدم وجود التكون القشري بين ضرس الرحى السفلي الثالث المدفون والقناة السنخية السفلية في الأشعة المقطعية المخروطية.
طرق البحث
دَرست هذه الدراسة الاسترجاعية ٢١٠ ضرسا فكيا سفليا ثالثا منغرسا من ١٣٥ مريضا (بأعمار من ١٧ -٥١ سنة) والذين أظهروا واحدا أو أكثر من علامات الخطر البانورامية السبع المقترحة للتعرض العصبي السنخي السفلي. أُحيل هؤلاء المرضى للفحص بالأشعة المقطعية المخروطية. واستُخدمت الصور ثلاثية الأبعاد لتقييم موقع القناة بالنسبة للضرس الثالث، وقرب القناة من الضرس الثالث وزاوية ميول الضرس الثالث. وقورنت نتائج الأشعة البانورامية والأشعة المقطعية المخروطية.
النتائج
كانت نتائج الأشعة البانورامية عندما بينت انقطاع جدار القناة السنخية السفلية، سواء كان ذلك مقترنا أو غير مقترن بإحدى هذه العلامات؛ سواد جذور الضروس الثالثة، وضيق القناة، وانحراف القناة، وبخاصة سواد الجذور، وضيق القناة كان مرتبطا ارتباطا ذا قيمة إحصائية بالاتصال المباشر بين قناة الفك السفلي والأضراس الثالثة المنغرسة في الأشعة المقطعية المخروطية.
الاستنتاجات
يُوصى بعمل الأشعة المقطعية المخروطية قبل العملية في الحالات التي تبين سواد الجذور، أو ضيق القناة، أو التي تبين الانقطاع والضيق معا، أو انحراف أو سواد الجذور معا في الأشعة البانورامية. وقد قيمت هذه الدراسة علاقة الخطورة بين العصب السنخي السفلي والأضراس الثالثة في الفك السفلي المنغرسة وآلية الحد من حدوث إصابة ما بعد الجراحة في العصب السنخي السفلي.
الكلمات المفتاحية: الأشعة المقطعية المخروطية, قناة الفك السفلي, صورة الأشعة البانورامية, الضرس الثالث
Introduction
Extraction of the mandibular third molar is a widely performed procedure in oral surgery.1 The most common complication of impacted mandibular third molar extraction surgery is injury to the inferior alveolar nerve (IAN), which may result in postoperative paresthesia.2, 3, 4 IAN paresthesia is described as a prolonged sensory deficiency and/or abnormal sensation in the lower jaw, mental area, and lower lip of the affected side, and may be temporary or permanent in nature.5 The frequency of IAN paresthesia following surgery is between 0.4% and 8%. Permanent paresthesia may lead to functional compromise and a decreased quality of life.6
The anatomical relationship between the mandibular third molar roots and the inferior alveolar canal (IAC) is the most predictable risk factor for IAN injury.7, 8 Exposure of the IAN upon extraction reveals a close relationship between the nerve and the roots of the mandibular third molar. There is a 15–25% increased risk of postoperative paresthesia following IAN exposure, and research shows high anatomical variability among individuals.7 Therefore, an accurate and detailed picture of the anatomical relationship of the mandibular third molar and IAN by radiographic imaging techniques is a critical preoperative tool to minimize risk during surgery and to prevent neurological complications.4, 9, 10, 11, 12
Panoramic radiography is the standard imaging technique performed before mandibular third molar extraction to assess the anatomical risk factors.8, 11 Specific radiographic signs have been identified on panoramic radiographic imaging that may suggest a close relationship between the IAN canal and third molars.13, 14, 15, 16 These radiographic signs include interruption of the radiopaque wall of the canal, narrowing of the canal, deviation of the canal, darkening of the tooth roots, narrowing of the tooth roots, as well as deviation of the tooth roots and the bifid apex.15
In some cases, panoramic radiographs are sufficient for preoperative evaluation of the anatomical relation of the IAN and third molars; however, this imaging modality does not provide any information regarding the buccolingual dimension.8 Assessment of the buccolingual dimension is important for cases in which there is a close anatomical proximity between the IAN and third molar17, 18 as the risk of IAN injury is significantly elevated when compared to other locations.8, 19 This could be because maxillofacial surgeons frequently approach from the buccal aspect of the third molar and produce pressure in a lingual direction.8 In these cases, cone beam computed tomography (CBCT) is recommended for accurate examination of the buccolingual relation.
In high-risk cases, CBCT data with respect to the buccolingual relation will enable maxillofacial surgeons to decide among retaining an asymptomatic impacted third molar, modifying their surgical approach, or performing a coronectomy.20
CBCT is a relatively novel diagnostic three-dimensional (3D) imaging modality for presurgical localization of the IAN.13 Compared with the two-dimensional panoramic radiograph, CBCT generates accurate 3D volumetric images in the axial, sagittal, and coronal planes.14 These reconstructed images can be manipulated using computer software to visualize the dentomaxillofacial region of interest for better surgical planning.1 CBCT is requested when the panoramic radiograph detects a close proximity between the impacted third molar and the inferior alveolar canal.21, 22, 23 However, although CBCT offers better image quality, it carries a higher exposure dose than panoramic radiography. Furthermore, CBCT is less available in certain areas, and its higher cost considering the socioeconomic situations of some developing countries justifies the use of panoramic radiography alone in the preoperative assessment of the third molar.23
Digital panoramic radiography is performed routinely at the Taibah University College of Dentistry (TUCD) for all patients as an initial radiographic assessment. Most of the patients who are referred for surgical removal of their impacted mandibular third molars showed a close relationship between the impacted tooth and the IAC. Nearly all of the panoramic radiograph risk signs of IAN injury proposed by Rood and Shehab15 were seen in these patients.
In such cases, it is unclear whether routine panoramic radiography only is sufficient as a preoperative diagnostic imaging technique before surgical removal of impacted molars, or whether CBCT should be conducted for more detailed information to reduce IAN injury.
Therefore, the aim of the current study was to validate the accuracy of the panoramic radiographic risk signs through detection of presence or absence of corticalization between impacted third molar and inferior alveolar canal on CBCT.
Materials and Methods
This retrospective observational study was conducted in the clinics of TUCD, Almadinah Almunawwarah, KSA and it was approved by TUCD-REC (Taibah University, College of Dentistry Research Ethics Committee) in February 2016. A waiver of consent was requested because this was a retrospective radiographic study, and data were anonymous and coded.
The study included all female patients who came to TU Dental Clinics (TUDC) from January 2014 to January 2017 and underwent preoperative digital panoramic radiography before extraction of impacted mandibular third molars. These patients also showed a close relationship between the inferior alveolar canal and impacted mandibular third molars as detected in their routine digital panoramic radiographs and were referred for examination of the inferior alveolar canal with CBCT, which had been archived using Carestream (CS) R4 Clinical and Practice Management Software database (CS Health, Inc. Rochester, NY, USA).
CBCT scans acquired using CS 9300 PREMIUM 3D CBCT device (Carestream SM 749, Rochester, NY, USA), operating at 90 kVp/4 mA and an exposure time of 11.3 s and 0.3 mm voxel size. Digital panoramic radiographs were obtained using CS CS9000, select 3D Extraoral Digital Imaging System (SM749, Rochester NY, USA), operating at 70 kVp/10 mA and an exposure time of 14.3 s. Panoramic radiographs with radiological evidence of intraosseous pathologies related to the third molars were excluded from the study.
Panoramic radiographs and CBCT images were independently assessed by an oral and maxillofacial surgeon and an oral radiologist with extensive experience in CBCT, on a 21-inch LCD computer monitor workstation, under dim illumination conditions. All image interpretation was conducted under standardized conditions, and any conflicts in the evaluations were decided by consensus.
Each CBCT volumetric image was viewed in the three orthogonal planes (axial, coronal, and sagittal views). Oblique sections were also examined to determine the anatomical relationship between the third molars and IAC. Cross-sectional slices were used to visualize the buccolingual position of the canal and presence of a cortical line between third molars and IAC. The radiographs were evaluated with the use of CS software tools for image manipulation, zoom, brightness, and contrast.
Digital panoramic radiographs were evaluated for the presence of one or more of the seven radiographic risk predictor signs according to the criteria established by Rood and Shehab:15
-
1.
Darkening of the root: Loss of root density in a tooth that is impinged upon by the canal.
-
2.
Interruption of the white line: Discontinuity of the superior radio-opaque line that constitutes the superior border of the inferior alveolar canal.
-
3.
Diversion of the canal: A change in the direction of the canal while crossing the mandibular third molar.
-
4.
Deflection of the root: An abrupt deviation of roots near the canal.
-
5.
Narrowing of the root: Narrowing of the tooth roots where the canal crosses.
-
6.
Narrowing of the canal: An abrupt decrease in the width of the canal while it crosses the root apices.
-
7.
Dark and bifid root apex: A loss of root density in a tooth that is impinged upon by the canal with bifid apex of the root.
CBCT images of the same patients were examined in the three planes for the exact anatomical relationship of impacted mandibular third molar with the IAN and compared with the panoramic radiograph findings. The following was evaluated on CBCT:
-
1.
Impacted mandibular third molar angulation was classified into a) mesioangular impaction; b) distoangular impaction; c) vertical impaction; and d) horizontal impaction (Winter's Classification 1926).24
-
2.
The buccolingual relationship between the impacted mandibular third molar and the IAC was classified as buccal, lingual, interradicular, or inferior.2
-
3.
The position of the IAC with respect to the third molar was classified as contact (no bone between the IAC and the third molar) or no contact (bone between the IAC and the third molar).8
Statistical analyses
The radiographic data were coded and analyzed using the Statistical Package for the Social Sciences software (SPSS-20, Chicago, IL, USA). Values of panoramic radiographic signs, the inferior alveolar canal position, impaction angulation, and bone contact were sorted according to their frequency and percentage. Pearson's chi-square test was applied to evaluate the correlation between signs detected on panoramic radiograph with nerve positioning, bone contact, and impaction angulation. Results with P < 0.05 were considered statistically significant.
Results
The study incorporated 210 impacted mandibular third molars from 135 patients (mean age, 25 ± 1 years; age range, 17–51 years) who attended TUDC.
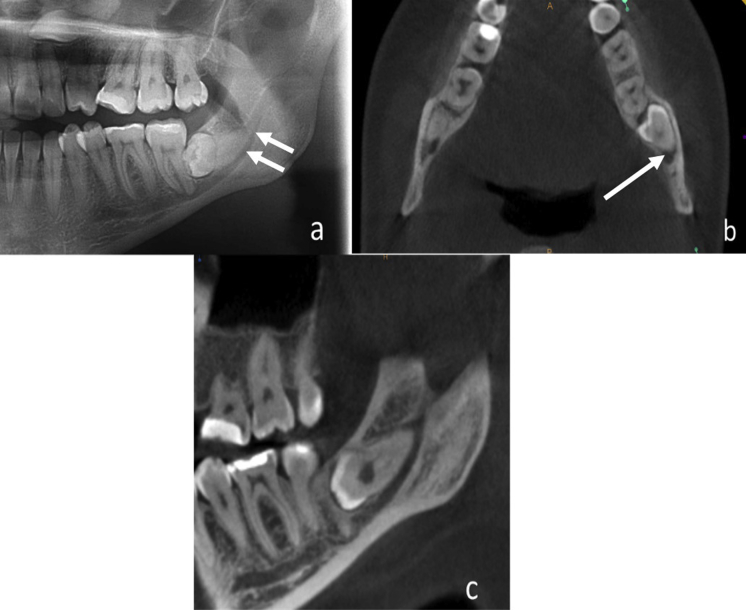
The most frequent risk predictor signs seen on panoramic radiographic images were interruption of the IAC wall, darkening in roots, and narrowing of the canal. Interruption of the IAC wall was the most frequent radiographic sign either in isolation or combined with other radiographic signs (interruption and narrowing of the canal, interruption and darkening of roots, interruption and diversion of the canal) (Figure 1).
Figure 1.
a. Cropped panoramic radiograph showing interruption with narrowing of IAC at 38. b. Axial CBCT showing contact between roots of 38 and the lingually positioned IAC. c. Reformatted panoramic radiograph showing mesioagular position of 38.
There was a statistically significant association between these three frequently seen signs and direct contact between the third molar and IAC on CBCT imaging (P < 0.001).
Table 1 summarizes the relationship between risk signs seen on panoramic radiography and presence or absence of contact between third molar and IAC on CBCT.
Table 1.
Relationship between panoramic radiographic signs and presence or absence of contact between the third molar and IAC on CBCT.
| Panoramic radiograph Sign | Contact |
No contact |
Total |
||
|---|---|---|---|---|---|
| No. | % | No. | % | No. | |
| Interruption of IAC white line | 63 | 52.2 | 63 | 72.4 | 126 |
| Darkening in the root apex | 12 | 9.8 | 12 | 13.8 | 24 |
| Narrowing of IAC | 12 | 9.8 | 0 | 0 | 12 |
| Interruption, narrowing of IAC | 15 | 12.2 | 3 | 3.4 | 18 |
| Interruption of IAC, darkening in root apex | 6 | 4.9 | 3 | 3.4 | 9 |
| Interruption, diversion of IAC | 12 | 9.8 | 3 | 3.4 | 15 |
| Diversion of IAC | 0 | 0 | 3 | 3.4 | 3 |
| Darkening in root apex, diversion of IAC | 3 | 2.4 | 0 | 0 | 3 |
| Total number of cases | 123 | 100 | 87 | 100 | 210 |
IAC, inferior alveolar canal.
Interruption of the canal seen on panoramic radiography was correlated with contact on CBCT (52.2%), followed by interruption and narrowing (12.2%), then darkening of roots (9.8%) and narrowing of the canal (9.8%). It is worth mentioning that all the cases observed with narrowing of the canal on panoramic radiography showed contact with IAC on CBCT.
There was a statistically significant correlation between the most frequent panoramic radiographic signs and the buccolingual position of the inferior alveolar canal with respect to the third molar roots on CBCT (P < 0.001).
An inferior position of the canal was more frequent in cases of interruption of canal followed by lingual, then buccal, then interradicular position (Figures 2 and 3). In cases of darkening of roots, canal position was most frequently inferior, then buccal, then lingual), and in cases of narrowing of canal, canal position was most frequently inferior, then lingual). Table 2 summarizes the relationship of panoramic radiographic signs and the position of the IAC canal on CBCT.
Figure 2.
a. Cropped panoramic radiograph showing interruption of the IAC wall with darkening of the root of 38. b. Axial CBCT showing interradicular position of IAC at 38. c. Reformatted panoramic radiograph showing mesioagular position of 38.
Figure 3.
a. Cropped panoramic radiograph showing interruption of IAC walls with darkening of roots of 48. b. Axial CBCT showing contact between roots of 48 and the inferiorly positioned IAC. c. Reformatted panoramic radiograph showing mesioagular position of 48.
Table 2.
Relationship between panoramic radiograph signs and position of the IAC on CBCT.
| Panoramic radiograph sign | Buccal |
Lingual |
Inferior |
Interradicular |
Total |
|---|---|---|---|---|---|
| No. | No. | No. | No. | No. | |
| Interruption of IAC white line | 27 | 39 | 54 | 6 | 126 |
| Darkening in root apex | 6 | 3 | 15 | 0 | 24 |
| Narrowing of IAC | 0 | 3 | 9 | 0 | 12 |
| Interruption, narrowing of IAC | 6 | 3 | 9 | 0 | 18 |
| Interruption and diversion of IAC | 0 | 3 | 12 | 0 | 15 |
| Interruption of IAC, darkening in root apex | 3 | 3 | 3 | 0 | 9 |
IAC, inferior alveolar canal.
The relationship between the panorama radiographic signs and third molar angulation was significant (P < 0.001). A mesioangular position was most commonly associated with interruption of the canal, darkening of roots, and narrowing of the canal (Table 3).
Table 3.
Relationship between panoramic radiograph signs and impacted tooth angulation.
| Panoramic radiograph sign | Tooth angulation |
||||
|---|---|---|---|---|---|
| D |
H |
M |
V |
Total |
|
| No. | No. | No. | No. | No. | |
| Interruption of IAC white line | 15 | 3 | 99 | 9 | 126 |
| Darkening in root apex | 0 | 0 | 21 | 3 | 24 |
| Narrowing of IAC | 3 | 3 | 6 | 0 | 12 |
| Interruption, narrowing of IAC | 0 | 9 | 9 | 0 | 18 |
| Interruption, diversion of IAC | 3 | 0 | 12 | 0 | 15 |
| Interruption of IAC, darkening in root apex | 0 | 0 | 9 | 0 | 9 |
IAC, inferior alveolar canal.
Discussion
Mandibular third molars are considered the most commonly impacted teeth, and surgical removal of impacted mandibular third molars is one of the most common dentoalveolar surgeries performed.3 A preoperative assessment detailing the exact relationship between the roots of third molar and the IAC would help in predicting risk and probably avoiding sensory damage after surgery. In oral and maxillofacial surgery, panoramic radiography is primarily requested to evaluate impacted mandibular third molars and estimate the risk of IAN damage.
Several studies have estimated risk factors based on panoramic radiographic findings.4, 26, 27, 28 However, as a two-dimensional evaluation, it does not offer precise diagnostic data regarding the relationship between the third molar and the IAC. CBCT can provide information regarding the presence of direct contact between the third molar and the IAC, which enables a well-designed treatment plan and secure surgical extraction in cases of severe impactions29; furthermore, CBCT can confirm accuracy of panoramic radiographic risk predictors.
Tantanapornkul et al.22 reported a higher accuracy of CBCT (80%) compared with panoramic radiography (64%) in the prediction of IAN exposure. In contrast, Ghaeminia et al.8 disclosed the accuracy for CBCT and panoramic radiograph were 55% and 45% respectively. Conversely, Ghaeminia et al.8 stated that sensitivity (panoramic radiograph: 100% and CBCT: 96%) and specificity (panoramic radiograph: 3% and CBCT: 23%) between the two imaging methods were not statistically different leading them to conclude that the two modalities weren't different in predicting exposure of the IAN before third molar extraction. While a recent research compared between, panoramic radiograph and CBCT reported that both are equally valued for investigation of mandibular third molar angulation, number and morphology of its roots.25
In the present retrospective study, only patients who showed a close relationship between impacted third molar and IAC and were referred for CBCT examination were selected. The parameters used in CBCT for evaluating the validity of panoramic radiographic signs were mainly contact between the third molar and IAC, a buccolingual canal position, and spatial angulation of the third molar.
The most frequently seen panoramic radiographic sign was interruption of the inferior alveolar canal white line (60%), consistent with findings of previously published studies22, 26, 27, 28, 29, 30, 31, 32 and in contrast with others that did not observe a high diagnostic value for interruption of the IAC white line.28
Among patients with interruption of the IAC, CBCT revealed 63 impactions of a total of 126 in contact with the IAC (50%); this was in accordance with Peker et al.33 who reported a significant correlation between darkening of the roots and interruption of the white line on panoramic radiography and the presence of contact on CBCT images.
The second most frequent risk sign on panoramic radiography was darkening of the roots (seen in 11.4%). In contrast, other studies4, 32, 34, 35 reported darkening of the roots to be the main panoramic radiographic sign. In our study, CBCT of these patients revealed 12 impactions of a total 24 in contact with the IAC (50%); this was similar to the results of Peker et al.33 Whereas, in another study conducted among Saudi patients, most of the impacted molars (74%) showed the IAC to be in contact with the lingual mandibular plate of bone, with no perforation.36
Narrowing of the inferior alveolar canal was the third most frequent panoramic radiographic sign (seen in 5.7%); this was in contrast to the study by Monaco et al. who reported narrowing to be the main panoramic radiographic sign.4
Among all patients observed with narrowing of canal, CBCT revealed contact between canal and third molar roots in all, in contrast with Neves et al.29 who did not observe any diagnostic value of this sign.
The presence of two or more signs on panoramic radiography may demonstrate an elevated risk of IAN exposure or injury,26, 29, 35, 37, 38 as shown in our results. The rate of contact between the two structures increased when there was an association between interruption of the IAC and narrowing of the canal, followed by interruption with diversion of canal, and interruption with darkening of the roots, which showed contact between the canal and third molar in 83%, 80%, and 66.6%, respectively.
The surgical approach for removal of an impacted third molar is mostly buccal in cases for which there are no data about the buccolingual position of the IAC before surgery. CBCT enables the surgeon to achieve comprehensive treatment planning and appropriate surgical approach according to precise canal position.17 Previous studies stated that the IAC is most often located on the lingual side of impacted third molars where contact between the IAC and these molars was found in those cases.8, 17, 39, 40
In the present study, the canal was predominantly in the inferior position (48.6%) in all observed risk signs (either separate or associated), followed by the lingual position (27%). In contrast, a previous study conducted in the eastern region of KSA found that the IAC was most commonly located lingually, rather than buccally, to the impacted mandibular third molar.36
Previous studies have categorized the impacted third molar as vertical, horizontal, or angular, based on its alignment to the mandible.16, 18 Our results showed that mesioangular was the most common angulation (77%) in all patients with panoramic radiographic risk signs, followed by distoangular (10%), horizontal (7%), and vertical (5.7%). This was in agreement with Msagati et al.41 who reported mesioangular angulation in 76% of their cases, and Syed et al.42 who reported the same in 50.75% of their Saudi population in Abha. As well, Hassan43 reported that the mesioangular angulation was most common angulation in the mandible (33.5%) in people living in the western region of KSA, which represented a variety of ethnic groups.
In contrast, Shujaat et al.36 reported that horizontally angulated impactions were the most common in KSA's eastern region, which has a less varied range of ethnic groups. Tantanapornkul et al.18 reported that the horizontal type was the most common (52%), followed by angular (32%) and vertical (16%). Similarly, Momin et al. reported horizontal (42%), angular (37%), and vertical (21%) angulated impactions.16
Szalma et al.26 identified three risk signs on panoramic radiography (interruption of white line, diversion of the inferior alveolar canal, and darkening of roots) that were expressly correlated with IAN paresthesia. In the present study, diversion of the inferior alveolar canal was not associated with more risk of contact between the molar roots and the inferior alveolar canal as an isolated finding, but when associated with other signs such as interruption of canal line or darkening in roots, the risk of contact between the canal and third molar increased.
Our study had one limitation in that only female patients were included. We had access to the panoramic and CBCT images for the female section only of our faculty's clinics, which are completely separated from the male section.
In the current study, 59% of all patients showed contact between IAC and impacted third molar roots; this confirms the high prevalence of patients attending TUDC with a high-risk association between the IAC and third molar.
Conclusion
A high prevalence of contact between impacted third molars and the IAC was detected radiographically in female patients living in Almadinah Almunawwarah and attending TUDC. Preoperative CBCT is recommended for cases showing interruption of the canal wall, darkening of the roots, or narrowing of the canal, or an association between interruption and narrowing, diversion of IAC, or darkening of roots on panoramic radiography. In such cases, CBCT is useful to assess the risk relationship of the IAN and the impacted mandibular third molars, and to reduce the occurrence of postoperative injury to the IAN.
Recommendations
To obtain clinically significant information, future prospective studies should be done on clinical cases with a high risk of intraoperative mandibular nerve injury to assess the significance of radiographic findings on nerve injuries.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
Taibah University, College of Dentistry Research Ethics Committee “TUCD-REC” approved this study in February 2016 (No: TUCDREC/2016202). A waiver of consent was requested because this was a retrospective radiographic study, and data were anonymous and coded. Confidentiality of data was guaranteed by the commitment of the principal investigator to use codes for all study subjects included in this study.
Authors' contributions
SMEK designed the research idea, wrote the literature review and Methodology, adjusted the figures and prepared the manuscript for submission for publication. SSA wrote the literature review, Methodology, Discussion, and Conclusion, interpreted and analyzed the data for the work, collected the references, composed the results, and adjusted the tables. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Manpower survey of oral surgery. Part I. J Oral Surg. 1977;35(special issue A):A55–A95. [PubMed] [Google Scholar]
- 2.Nakayama K., Nonoyama M., Takaki Y., Kagawa T., Yuasa K., Izumi K. Assessment of the relationship between impacted mandibular third molars and inferior alveolar nerve with dental 3-dimensional computed tomography. J Oral Maxillofac Surg. 2009;67(12):2587–2591. doi: 10.1016/j.joms.2009.07.017. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed A., Mohamed F., Hattab K. Surgical extraction of impacted mandibular third molars: postoperative complications and their risk factors. JMJ. 2009;9(4):272–275. [Google Scholar]
- 4.Monaco G., Montevecchi M., Bonetti G.A., Gatto M.R., Checchi L. Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc. 2004;135(3):312–318. doi: 10.14219/jada.archive.2004.0179. [DOI] [PubMed] [Google Scholar]
- 5.Benediktsdóttir I.S., Wenzel A., Petersen J.K., Hintze H. Mandibular third molar removal: risk indicators for extended operation time, postoperative pain, and complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97(4):438–446. doi: 10.1016/j.tripleo.2003.10.018. [DOI] [PubMed] [Google Scholar]
- 6.Loescher A.R., Smith K.G., Robinson P.P. Nerve damage and third molar removal. Dent Update. 2003;30(7):375–380. doi: 10.12968/denu.2003.30.7.375. [DOI] [PubMed] [Google Scholar]
- 7.Koong B., Pharoah M.J., Bulsara M., Tennant M. Methods of determining the relationship of the mandibular canal and third molars: a survey of Australian oral and maxillofacial surgeons. Aust Dent J. 2006;51(1):64–68. doi: 10.1111/j.1834-7819.2006.tb00403.x. [DOI] [PubMed] [Google Scholar]
- 8.Ghaeminia H., Meijer G.J., Soehardi A., Borstlap W.A., Mulder J., Berge S.J. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int J Oral Maxillofac Surg. 2009;38(9):964–971. doi: 10.1016/j.ijom.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Tay A.B., Go W.S. Effect of exposed inferior alveolar neurovascular bundle during surgical removal of impacted lower third molars. J Oral Maxillofac Surg. 2004;62(5):592–600. doi: 10.1016/j.joms.2003.08.033. [DOI] [PubMed] [Google Scholar]
- 10.Pawelzik J., Cohnen M., Willers R., Becker J. A comparison of conventional panoramic radiographs with volumetric computed tomography images in the preoperative assessment of impacted mandibular third molars. J Oral Maxillofac Surg. 2002;60(9):979–984. doi: 10.1053/joms.2002.34399. [DOI] [PubMed] [Google Scholar]
- 11.Ruga E., Gallesio C., Boffano P. Mandibular alveolar neurovascular bundle injury associated with impacted third molar surgery. J Craniofac Surg. 2010;21(4):1175–1177. doi: 10.1097/SCS.0b013e3181e20822. [DOI] [PubMed] [Google Scholar]
- 12.Ardakani F.E., Booshehri M.Z., Azam A.N., Ardakani F.F. Diagnostic accuracy of panoramic radiography in determining the position of impacted third molars in relation to the inferior dental canal compared with surgery. Iran J Radiol. 2010;7(2):91–96. [Google Scholar]
- 13.Flygare L., Ohman A. Preoperative imaging procedures for lower wisdom teeth removal. Clin Oral Investig. 2008;12(4):291–302. doi: 10.1007/s00784-008-0200-1. [DOI] [PubMed] [Google Scholar]
- 14.Scarfe W.C., Farman A.G. Cone-beam computed tomography. In: White S.C., Pharoah M.J., editors. Oral radiology: principles and interpretation. 6th ed. Elsevier Inc.; St. Louis: Mosby: 2009. pp. 225–243. [Google Scholar]
- 15.Rood J.P., Shehab A.A. The radiological predilection of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg. 1990;28:20. doi: 10.1016/0266-4356(90)90005-6. [DOI] [PubMed] [Google Scholar]
- 16.Momin M.A., Matsumoto K., Ejima K., Asaumi R., Kawai T., Arai Y., Honda K., Yosue T. Correlation of mandibular impacted tooth and bone morphology determined by cone beam computed topography on a premise of third molar operation. Surg Radiol Anat. 2013;35:311–318. doi: 10.1007/s00276-012-1031-y. [DOI] [PubMed] [Google Scholar]
- 17.Feifel H., Riediger D., Gustorf-Aeckerle R. High resolution computed tomography of the inferior alveolar and lingual nerves. Neuroradiology. 1994;36:236–238. doi: 10.1007/BF00588141. [DOI] [PubMed] [Google Scholar]
- 18.Lübbers H.T., Matthews F., Damerau G., Kruse A.L., Obwegeser J.A., Gratz K.W., Eyrich G.K. Anatomy of impacted lower third molars evaluated by computerized tomography: is there an indication for 3-dimensional imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:547–550. doi: 10.1016/j.tripleo.2010.06.010. [DOI] [PubMed] [Google Scholar]
- 19.Maegawa H., Sano K., Kitagawa Y., Ogasawara T., Miyauchi K., Sekine J. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(5):639–646. doi: 10.1016/s1079-2104(03)00356-1. [DOI] [PubMed] [Google Scholar]
- 20.Renton T., Hankins M., Sproate C., McGurk M. A randomised controlled clinical trial to compare the incidence of injury to the inferior alveolar nerve as a result of coronectomy and removal of mandibular third molars. Br J Oral Maxillofac Surg. 2005;43(4):7–12. doi: 10.1016/j.bjoms.2004.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Ghaeminia H., Meijer G.J., Soehardi A., Borstlap W.A., Mulder J., Vlijmen O.J., Bergé S.J., Maal T.J. The use of cone beam CT for the removal of wisdom teeth changes the surgical approach compared with panoramic radiography: a pilot study. Int J Oral Maxillofac Surg. 2011;40:834–839. doi: 10.1016/j.ijom.2011.02.032. [DOI] [PubMed] [Google Scholar]
- 22.Tantanapornkul W., Okouchi K., Fujiwara Y., Yamashiro M., Maruoka Y., Ohbayashi N., Kurabayashi T. A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(2):253–259. doi: 10.1016/j.tripleo.2006.06.060. [DOI] [PubMed] [Google Scholar]
- 23.Tantanapornkul W., Mavin D., Prapaiphittayakun J., Phipatboonyarat N., Julphantong W. Accuracy of panoramic radiograph in assessment of the relationship between mandibular canal and impacted third molars. Open Dent J. 2016;10:322–329. doi: 10.2174/1874210601610010322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Winter G.B. American Medical Books; St Louis: 1926. Principles of exodontia as applied to the impacted third molar. [Google Scholar]
- 25.Hauge Matzen L., Christensen J., Hintze H., Schou S., Wenzel A. Diagnostic accuracy of panoramic radiography, stereo-scanography and cone beam CT for assessment of mandibular third molars before surgery. Acta Odontol Scand. 2013 Nov;71(6):1391–1398. doi: 10.3109/00016357.2013.764574. [DOI] [PubMed] [Google Scholar]
- 26.Szalma J., Lempel E., Jeges S., Szabó G., Olasz L. The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(2):294–302. doi: 10.1016/j.tripleo.2009.09.023. [DOI] [PubMed] [Google Scholar]
- 27.Jerjes W., Swinson B., Moles D.R. Permanent sensory nerve impairment following third molar surgery: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102(4):e1–7. doi: 10.1016/j.tripleo.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 28.Nakamori K., Fujiwara K., Miyazaki A. Clinical assessment of the relationship between the third molar and the inferior alveolar canal using panoramic images and computed tomography. J Oral Maxillofac Surg. 2008;66(11):2308–2313. doi: 10.1016/j.joms.2008.06.042. [DOI] [PubMed] [Google Scholar]
- 29.Neves F.S., Souza T.C., Almeida S.M., Haiter-Neto F., Freitas D.Q., Bóscolo F.N. Correlation of panoramic radiography and cone beam CT findings in the assessment of the relationship between impacted mandibular third molars and the mandibular canal. Dentomaxillofac Radiol. 2012;41(7):553–557. doi: 10.1259/dmfr/22263461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gomes A.C., Vasconcelos B.C., Silva E.D., AdeF Caldas, Jr., Pita N.I.C. Sensitivity and specificity of pantomography to predict inferior alveolar nerve damage during extraction of impacted lower third molars. J Oral Maxillofac Surg. 2008;66(2):256–259. doi: 10.1016/j.joms.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 31.Nakagawa Y., Ishii H., Nomura Y., Watanabe N.Y., Hoshiba D., Kobayashi K. Third molar position: reliability of panoramic radiography. J Oral Maxillofac Surg. 2007;65:1303–1308. doi: 10.1016/j.joms.2006.10.028. [DOI] [PubMed] [Google Scholar]
- 32.Shahidi S., Zamiri B., Bronoosh P. Comparison of panoramic radiography with cone beam CT in predicting the relationship of the mandibular third molar roots to the alveolar canal. Imaging Sci Dent. 2013;43(2):105–109. doi: 10.5624/isd.2013.43.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Peker Panoramic radiography and cone-beam computed tomography findings in preoperative examination of impacted mandibular third molars. BMC Oral Health. 2014;14(1):1–7. doi: 10.1186/1472-6831-14-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sedaghatfar M., August M.A., Dodson T.B. Panoramic radiographic findings as predic-tors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg. 2005 Jan 31;63(1):3–7. doi: 10.1016/j.joms.2004.05.217. [DOI] [PubMed] [Google Scholar]
- 35.Bell G.W. Use of dental panoramic tomographs to predict the relation between man-dibular third molar teeth and the inferior alveolar nerve. Br J Oral Maxillofac Surg. 2004 Feb 29;42(1):21–27. doi: 10.1016/s0266-4356(03)00186-4. [DOI] [PubMed] [Google Scholar]
- 36.Shujaat S., Abouelkheir H.M., Al-Khalifa K.S., Al-Jandan B., Marei H.F. Pre-operative assessment of relationship between inferior dental nerve canal and mandibular impacted third molar in Saudi population. The Saudi dental journal. 2014 Jul 1;26(3):103–107. doi: 10.1016/j.sdentj.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Blaeser B.F., August M.A., Donoff R.B., Kaban L.B., Dodson T.B. Panoramic radiographic risk factors for inferior alveolar nerve injury after third molar extraction. J Oral Maxillofac Surg. 2003 Apr 30;61(4):417–421. doi: 10.1053/joms.2003.50088. [DOI] [PubMed] [Google Scholar]
- 38.Jhamb A., Dolas R.S., Pandilwar P.K., Mohanty S. Comparative efficacy of spiral computed tomography and orthopantomography in preoperative detection of relation of inferior alveolar neurovascular bundle to the impacted mandibular third molar. J Oral Maxillofac Surg. 2009 Jan 31;67(1):58–66. doi: 10.1016/j.joms.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 39.Xu G.Z., Yang C., Fan X.D., Yu C.Q., Cai X.Y., Wang Y., He D. Anatomic relationship between impacted third mandibular molar and the mandibular canal as the risk factor of inferior alveolar nerve injury. Br J Oral Maxillofac Surg. 2013 Dec 31;51(8):e215–e219. doi: 10.1016/j.bjoms.2013.01.011. [DOI] [PubMed] [Google Scholar]
- 40.Jung Y.H., Nah K.S., Cho B.H. Correlation of panoramic radiographs and cone beam computed tomography in the assessment of a superimposed relationship between the mandibular canal and impacted third molars. Imaging science in dentistry. 2012 Sep 1;42(3):121–127. doi: 10.5624/isd.2012.42.3.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Msagati F., Simon E.N., Owibingire S. Pattern of occurrence and treatment of impacted teeth at the Muhimbili National Hospital, Dar es Salaam, Tanzania. BMC Oral Health. 2013;13(37):1–6. doi: 10.1186/1472-6831-13-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Syed K.B., Zaheer K.B., Ibrahim M., Bagi M.A., Assiri M.A. Prevalence of impacted molar teeth among Saudi population in Asir region, Saudi Arabia – a retrospective study of 3 years. J Int Oral Health JIOH. 2013 Feb;5(1):43–47. [PMC free article] [PubMed] [Google Scholar]
- 43.Hassan A.H. Pattern of third molar impaction in a Saudi population. Clin Cosmet Invest Dent. 2010;2:109–113. doi: 10.2147/CCIDEN.S12394. [DOI] [PMC free article] [PubMed] [Google Scholar]