Abstract
Objective
The purpose of this study was to compare the effectiveness of balance training using the Biodex balance system and a conventional balance training programme on balance score and on gross motor skills of children with spastic diplegia.
Methods
A randomized controlled study was conducted on 48 spastic diplegic children with cerebral palsy (26 boys and 22 girls) in the age range of 5–8 years. The children were randomly allocated to two equal groups. The investigators performed balance and gross motor function assessments for every child using the paediatric Berg balance scale and the gross motor function measure −88 scale (dimensions D and E) before and after the treatment programme. Passive repositioning sense was measured by a Biodex III isokinetic dynamometer. The study group received Biodex balance training and traditional physical therapy programme training, whereas the control group received conventional balance training in addition to the traditional physical therapy programme training, 3 times per week for 12 weeks.
Results
Significant improvement was observed in all outcome measures of the two groups, comparing their pre- and post-treatment mean values. Furthermore, the results revealed a significant (P < 0.05) improvement in mean post-treatment values for the Biodex balance training group.
Conclusion
Balance training using the Biodex balance system is superior to conventional balance training for improving the balance abilities and gross motor functions of children with cerebral palsy and spastic diplegia.
Keywords: Berg balance, Biodex, Cerebral palsy, Conventional balance, Spastic diplegia
الملخص
أهداف البحث
تهدف هذه الدراسة لمقارنة فاعلية تدريبات التوازن باستخدام جهاز التوازن ”بيودكس“ ببرنامج التوازن التقليدي على نتيجة التوازن والمهارات الحركية الإجمالية للأطفال المصابين بالشلل المزدوج التشنجي.
طرق البحث
أجريت هذه الدراسة العشوائية على ٤٨ طفلا مصابا بالشلل الدماغي التشنجي المزدوج (٢٦ طفلا و٢٢ طفلة) في عمر يتراوح من ٥ إلى ٨ سنوات. تم توزيع الأطفال عشوائيا إلى مجموعتين متساويتين. أجرى الباحثون تقييم التوازن والوظائف الحركية الإجمالية لكل طفل باستخدام مقياس ”بيرغ“ لتوازن الأطفال وإجمالي مقياس الوظيفة الحركية -٨٨ (الأبعاد ”د“ و ”إي“) قبل وبعد برنامج العلاج. تم قياس إعادة الوضع السلبي بواسطة بيودكس ٣ المقوي الحركي. تلقت مجموعة الدراسة التدريب بجهاز التوازن بيودكس وبرنامج العلاج الطبيعي التقليدي في حين تلقت المجموعة الضابطة التدريب بالتوازن التقليدي بالإضافة إلى برنامج العلاج الطبيعي التقليدي ٣ مرات أسبوعيا لمدة ١٢ أسبوعا.
النتائج
تم ملاحظة تحسنا كبيرا في جميع نتائج القياسات للمجموعتين بمقارنة القيم الرئيسة قبل وبعد العلاج. بالإضافة إلى ذلك، أظهرت النتائج تحسنا كبيرا في القيم الرئيسة بعد العلاج لصالح مجموعة التدريب بجهاز بيودكس.
الاستنتاجات
تفوقت تدريبات التوازن باستخدام جهاز التوازن بيودكس على التدريب بالتوازن التقليدي لتحسين القدرة على التوازن والوظائف الحركية الإجمالية عند الأطفال المصابين بالشلل الدماغي والشلل التشنجي المزدوج.
الكلمات المفتاحية: ميزان بيرغ, جهاز بيودكس, الشلل الدماغي, التوازن التقليدي, الشلل المزدوج التشنجي
Introduction
Cerebral palsy (CP) is a term used to denote a group of chronic, non-progressive neurodevelopmental disorders caused by brain damage or malfunction originating early in life and persisting throughout the lifespan. CP affects posture, volitional movement and the ability to produce coordinated and purposeful movements. The wide spectrum of disorders affect motor skills, sensation, communication skills, cognitive abilities, perception and psychosocial behaviour.1 Molina et al.2 reported that motor imagery impairment is prevalent in children with diplegic CP and is spatially constrained by the covered distance, but that in general, children with CP tend to perform worse than typical children. Balance disorders constitute a major challenge for children with spastic diplegic cerebral palsy (SDCP) and cause difficulties in attaining and maintaining stability.3, 4 Children with SDCP tend to have a limited capacity for perceptual neuromotor control, poor performance of stance stability under challenging sensory environments,5 delayed anticipatory adjustment and inconsistent preparatory activation.6, 7
Lack of neuromotor control has been reported as a possible cause of poor performance in balance control,5, 6, 7 but it seems that conventional balance training falls short of adequately addressing the neuromotor aspect of balance disorders. Children with CP require multidisciplinary management to address the wide spectrum of cognitive and motor disabilities.8 Long-term muscle imbalance results in several deformities that increase disability with age.9 Moreover, children with spastic diplegia always have proprioception disorders. Knee joint proprioception disorders can be attributed to the increase in muscle tone and abnormal firing of muscles, in addition to abnormal weight bearing and posture.10
Researchers have used several conventional balance approaches to improve balance and motor abilities and recover stability in children with cerebral palsy.3, 4, 11 However, none, to the best of our knowledge, have investigated and compared the Biodex balance system with the conventional balance approach for improving balance and motor control in children with SDCP. Therefore, this study was designed to examine the effect of using the Biodex balance system for improving the balance scores and gross motor functions of children with SDCP.
Materials and Methods
Forty-eight children with spastic diplegic CP (26 boys and 22 girls) were recruited from the outpatient clinic of the rehabilitation centre, Almadinah Almunawwarah. Ethical Approval (approval No. CMR-PT-2016-007) was obtained from the College of Medical Rehabilitation, Taibah University, which is operated according to the Saudi regulations of the national bioethics committee and according to the Declaration of Helsinki. Inclusion Criteria: Children aged from 5 to 8 years who are able to independently maintain the standing position for balance training using the Biodex balance training system, who have a grade 1 to 1+ spasticity according to the modified Ashworth scale,12 who have a minimum height of one metre, and who are able to follow verbal commands were included in the study. Exclusion Criteria: Children with cognitive disorders, perceptual, visual or auditory problems, or significant tightness at any joint of the lower limbs were excluded from the study. Children were randomly allocated to group A (n = 24) and group B (n = 24).
Evaluative and therapeutic tools
We used the Paediatric Berg balance scale and the gross motor functional measure scale (GMFMS), in addition to the Biodex Isokinetic Dynamometer (Biodex medical system, Shirley, New York, USA) which was used for assessment of knee proprioception. The Biodex balance training system was used for balance training. It is a unique system that allows the researcher to set the movable balance platform at variable degrees of instability.
Evaluation procedures
The researcher explained the study protocol to the parents or legal guardians. Written informed consent was obtained after deciding to participate. The children's demographics were collected. The Pediatric Balance Scale is a modified version of the Berg balance scale, which is designed to evaluate balance in children with mild to moderate motor impairment. Fifty-six points is the maximum score.13, 14 This scale evaluates performance of fourteen activities common in everyday life.
Gross motor function
Gross motor functional performance was evaluated with GMFM-88.15 It includes 88 items that cover 5 dimensions, from lying and rolling to walking and running. We only assessed dimensions D (standing) and E (walking). A 4-point scale was used and scores are expressed as percentages.
Knee proprioception testing (Passive angle reproduction)
Passive angle reproduction was performed using a Biodex Isokinetic Dynamometer. The system uses an electrogoniometer that is sensitive to 1° increments. The right limb was tested while subjects were blindfolded. After sitting with hips in 90° flexion, the tester passively drove the leg from 90° to 45° knee flexion and maintained the leg at the target angle for 10 s before returning to the initial position. The tester used 15°/s. angular velocity and paused for 5 s before repeating the cycle. Subjects pushed the button once they felt the target angle. The tester recorded the time elapsed and identified the angle. The average of three readings was calculated using the absolute difference between the perceived- and the target-angle.
Treatment procedures
The control group
Children were given a traditional physical therapy programme in addition to postural control exercises. The therapist used a one-hour session, 3×/wk for three successive months. A number of therapeutic activities were used, as stated in Appendix A.
A conventional balance training programme includes static and dynamic balance training. Static balance training includes maintaining a quadruped position, kneeling, standing, and shifting weight to balance on one limb. Dynamic balance training measures the ability to control the body when the support surface is unstable. The researcher used a gym ball to train automatic postural reactions. Dynamic disturbance prompts an equilibrium reaction on one side and a protective reaction on the other side, in addition to righting reactions on the axial body.
The study group
Children in the study group received dynamic balance training using the Biodex balance system, in addition to traditional physical therapy programme. After familiarization, each child was instructed to stand with both legs on the “locked” platform. The researcher advanced the platform to an unstable state while instructing the child to focus on the visual feedback screen. Arms were free at the side of the body and not grasping handrails. A stability level of 6 was suitable for the majority of the children as a starting training level. Fourteen children were trained starting with a stability level of 8, while 10 were trained starting with a stability level of 6. The transition between levels was based on the progress of balance capability.
Statistical analysis
Using the Shapiro–Wilk test, the Paediatric Berg balance scale data were normally distributed, while those of the GMFMS were not. Descriptive statistics, including mean ± standard deviation, were calculated for the Berg balance scale data for both groups. A paired sample t-test was used to ascertain within group differences. The unpaired sample t-test was used for between group differences in all post-intervention outcome measures. For GMFMS, comparison within and between groups was performed using a Wilcoxon signed rank test and a Mann–Whitney U-test. SPSS 22 was the software used for all data analysis. Statistical significance was set at alpha level ≤0.05.
Results
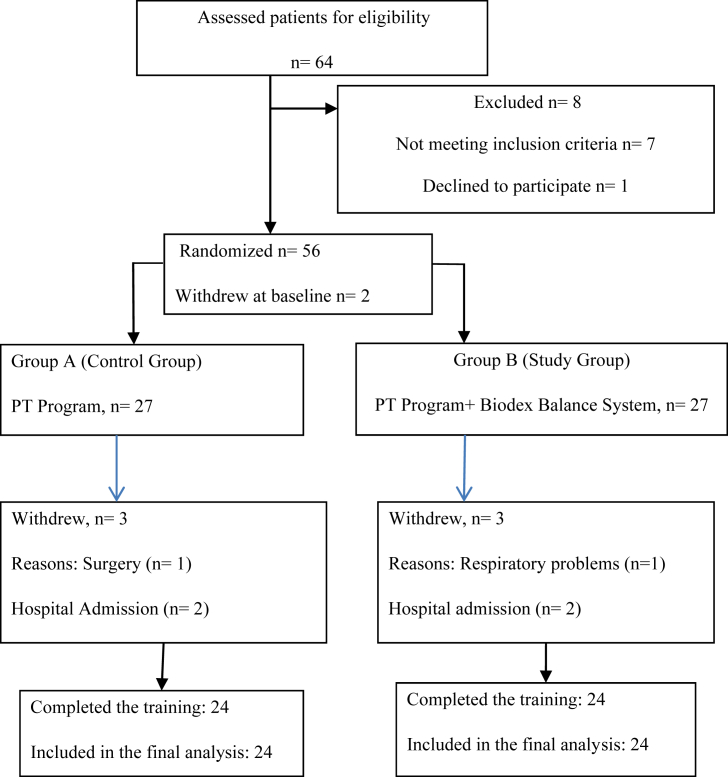
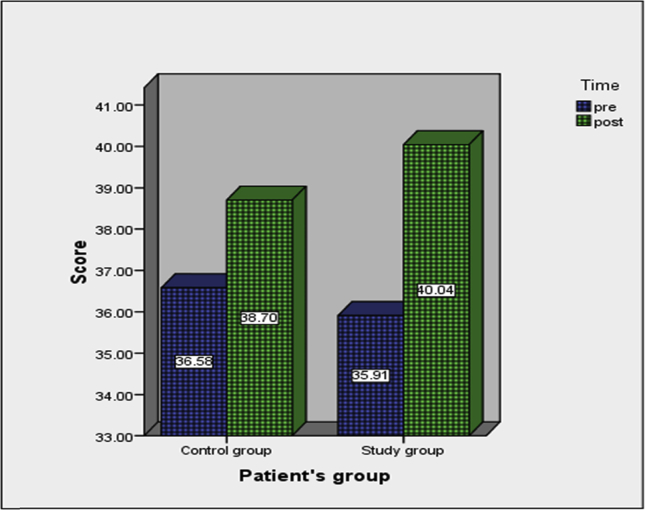
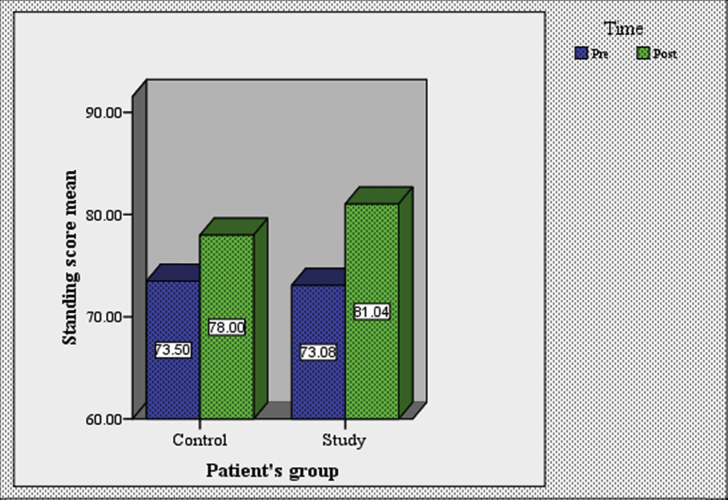
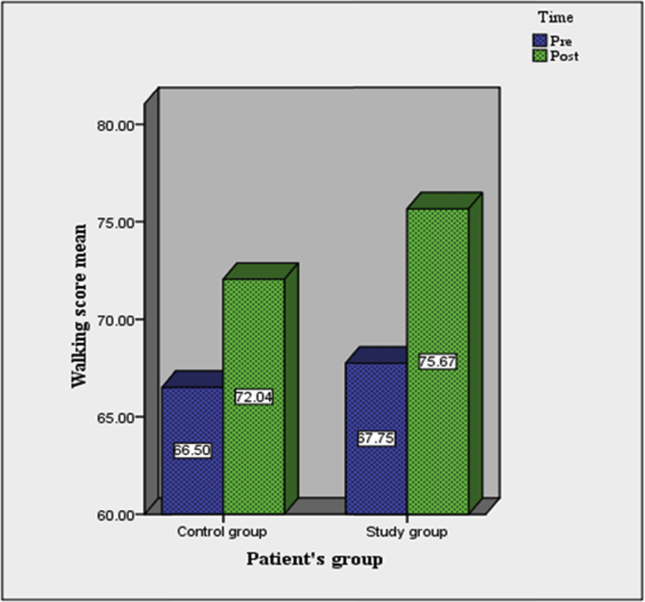
The total number of children studied, from screening to analysis, is shown in (Figure 1). The paired sample t-test was carried out to check for any differences between pre- and post-mean values of the paediatric Berg balance scale. Children's mean values are included in (Table 1). The mean values of the pre- and post-balance training scores for the control and study groups are shown in (Figure 2). All post-treatment mean values were significantly greater than the pretreatment mean values for both the study and the control groups (P < 0.05) (see Figure 3, Figure 4).
Figure 1.
Flowchart of children's retention and recruitment.
Table 1.
Characteristics of participants in the study.
| Age P > 0.05 |
Gender | Weight P > 0.05 |
Height P > 0.05 |
Orthotics | Assistive devices | MAS | |
|---|---|---|---|---|---|---|---|
| Group A | 8.63 SD 0.71 | 11 F 13 M |
29.2 SD 0.97 | 131 SD 1.4 cm | 12 using AFO 4 using KAFO 8 using med. shoes |
12 using walker | 1+ Ten 1 Fourteen |
| Group B | 8.93 SD 0.55 | 10 F 14 M |
27.9 SD 1.1 | 129 SD 2.1 cm | 9 using AFO 5 using KAFO 10 using med. shoes |
3 using walker | 1+ Thirteen 1 Eleven |
Figure 2.
Pre- and post-intervention mean values of the Paediatric Berg balance scale.
Figure 3.
Pre and post mean values of dimension D (standing) of GMFMS.
Figure 4.
Pre and post treatment values of GMFMS (walking dimension) for both groups.
The unpaired sample t-test was carried out to determine the difference in the post-treatment mean values of both groups. Children in the study group had mean values of 40.04 ± 2.17 compared with 38.70 ± 2.25 for the control group. This difference indicates superior improvement of the study group. The post-treatment mean value of the study group was significantly greater than the post-treatment mean value of the control group (P < 0.05).
Regarding GMFMS, the pre-test scores of both groups displayed no statistical significant difference (P > 0.05), which established baseline equivalency. In the study group, the difference in the mean from the pre-test to post-test was statistically significant (P < 0.05). In the control group, the improvement was statistically significant with P < 0.05. Both groups displayed a statistically significant improvement, with P values less than 0.05 (Table 2). In the post-treatment groups, the results showed statistically significant differences between the groups, with the Biodex training group favoured (see Table 3, Table 4, Table 5).
Table 2.
Continuous variables of the paediatric Berg balance scale scores for both groups.
| Paediatric Berg balance scale | Mean ± SD |
t-value | P-value | |
|---|---|---|---|---|
| Pre | Post | |||
| Group A | 36.58 ± 2.20 | 38.70 ± 2.25 | −7.647 | 0.000* |
| Group B | 35.91 ± 1.74 | 40.04 ± 2.17 | −13.621 | 0.000* |
*Significant difference, P value: probability value, SD, standard deviation.
Table 3.
Mean ± SD of dimension D (standing) of gross motor function measures within and between the Biodex and conventional balance training groups.
| GMFMS “D” (%) | Mean ± SD |
Z-value | P value | |
|---|---|---|---|---|
| Pre | Post | |||
| Group A | 73.54 ± 5.28 | 78.00 ± 4.67 | −3.87 | 0.000* |
| Group B | 73.08 ± 4.53 | 81.042 ± 3.544 | −4.31 | 0.000* |
| U | 264.00 | 191.5 | ||
| P value | 0.618 | 0.04 | ||
*Significant difference; P value: probability value; SD: standard deviation.
Table 4.
Mean ± SD of dimension E (walking) of gross motor function measures within and between the Biodex and conventional balance training groups.
| GMFMS “E” (%) | Mean ± SD |
Z-value | P value | |
|---|---|---|---|---|
| Pre | Post | |||
| Group A | 66.50 ± 3.7 | 72.05 ± 3.70 | −4.33 | 0.000* |
| Group B | 67.75 ± 4.93 | 75.67 ± 4.99 | −4.27 | 0.000* |
| U | 246.00 | 152.5 | ||
| P value | 0.385 | 0.005 | ||
*Significant difference; P value: probability value; SD: standard deviation.
Table 5.
Pre and post mean values of angular error of the knee for the control and study groups.
| Group | Mean ± SD |
t-value | P value | |
|---|---|---|---|---|
| Pre | Post | |||
| Control group | 13.1 ± 1.803 | 11.000 ± 1.685 | 14.685 | 0.000 |
| Study group | 13.5 ± 1.316 | 9.95 ± 0.945 | 11.461 | 0.000 |
| t-value | 0.100 | 2.430 | ||
| P value | 0.05 | 0.02 | ||
Discussion
Cerebral palsy is one of the most prevalent and often encountered health conditions that can benefit from physical therapy intervention. It has also been extensively studied, based on evidence in the current literature.16 In the present study, children in the study group who received balance training using the Biodex balance system in addition to the traditional physical therapy programme showed more improvement as measured by post-treatment mean values than the control group who received the conventional balance training in addition to the traditional physical therapy programme. The progress can be described and illustrated by improvements in: first, neuromotor planning strategy; second, sensory-perceptual motor integration; and third, neuromusculoskeletal functional capabilities.
First, children with spastic diplegia have different recruitment patterns compared with non-disabled children, and tend to have a limited capacity to modulate postural activity.17 Kane and Barden6, 7 reported that postural control difficulties may be associated with delayed anticipatory adjustment and inconsistent preparatory activation.
Biodex balance training might subtly have modulated the recruitment pattern and the anticipatory adjustment mechanisms through targeting the somatosensory and neuromuscular aspects of balance control. The labile support surface disturbs balance, which prompts the child to maintain the centre of gravity within the base of support. The instantaneous feedback while training on the Biodex system helps the child to relate body parts and repeat the motion as well as restore kinaesthetic sense for proper body positioning to maintain balance. This result is in harmony with the finding reported by Zadnikar and Kastrin8 who showed that adequate anticipatory postural adjustments, which precede active movement, are essential to having coordinated volitional movement.
Second, children with cerebral palsy tend to have balance impairments.18 Consequently, they rely on visual input to enhance their control, which may reflect impairments in proprioception.19 Wingert et al.10 examined joint-position sense and kinaesthesia in children with CP and in age-matched controls. Their results showed that participants with cerebral palsy have proprioception impairments in all limbs.
The Biodex balance training system might have improved the integration of different types of sensory information, promoting better balance and postural control through providing gradual challenges to the children to improve their motor abilities to meet the demands of motor control in sensory conflict conditions. Children with SDCP tend to stand on tiptoes. The perturbation of the balance base allows the feet to touch the platform while the children look at the peripheral visual signals. The central nervous system incorporates the peripheral somatosensory, visual and vestibular inputs, integrates them, and selects the most appropriate muscular responses to control body posture.
Biodex balance system training could also have influenced the process of integration between the central and peripheral nervous systems to have a meaningful body control response.20, 21 This concept is in agreement with the findings of Mawase et al.,22 who reported a larger postural sway when there was loss of somatosensory feedback information from the feet.,Additionally, it is supported by the findings of Tomita et al.,23 who showed that sensory-perceptual motor training for children with SDCP had a measurable, significant effect that was greater than that of the controls.
Third, SDCP children tend to suffer from poor posture and poor balance.24 Poor posture results in poor kinematics, trunk instability25, 26 and poor coordination.8, 9 Ju et al.27 reported that trunk instability is exhausting for children with SDCP. Borstad et al.28 revealed that exhaustion and muscle fatigue contribute to the poor kinematics and are potential risk factors for the continuation of the poor mechanics associated with the physical disorder. El-gohary et al.29 found measurable differences in muscle endurance ability at different ranges of spine kinematics. Heyrman et al.26 added that children with SDCP tend to show significantly higher kinematic parameters than typically developing children.
The Biodex balance training system might have improved the neuromusculoskeletal functional abilities through decreasing postural mal-alignment and improving spinal kinematics with subsequent improvement in balance control. The findings of the present study coincide with the findings of Bahramizadeh et al.30 and El-shamy and Abd El kafy11 who recorded progress in postural control after balance training. They added that postural adjustment plays a substantial role in quality of movement by creating a stable foundation during the active movement of extremities. Lacoste et al.31 added that maintenance of adequate postural stability is the foundation for functional motor activities. Liao et al.19 agreed with the role of functional strengthening exercises for improving functional motor abilities in SDCP children. Auld and Johnston32 showed that children with cerebral palsy had significant improvement in balance and strength even when practising low doses of group exercises. Artilheiro et al.33 and Liao et al.19 concluded that functional muscle strength correlates with gross motor skills in children with mild spastic diplegia.
The improvements in the passive reproduction of movement could be attributed to the relaxation and the control of spasticity when using Biodex balance training. This finding is in harmony with Chrysagias et al.,34 who studied kinaesthetic ability in a group of children with spastic cerebral palsy, compared with a control group. Researchers found a difference in outcome measures that was attributed to the kinaesthetic deficits in children with cerebral palsy. Promoting relaxation helps to control muscle tone, which has a significant relationship to improvement in passive reproduction of movement.
In essence, the labile standing surface of the Biodex balance training system is more likely to simulate the unstable nature of a walking terrain. Moreover, Biodex balance training provides a gradual, step-by-step functional training simulation.
Conclusion
In conclusion, the Biodex balance training system is an effective and efficient tool that can be used to improve balance and gross motor capabilities in children with SDCP.
Funding
None.
Authorship
This work is original, has not been published and is not under consideration elsewhere.
Authors' contributions
TME and HAE conceived and designed the study and conducted the data collection. TME and FAH analysed and interpreted the data in addition to reviewing the final results. TME and AMA provided logistical support and wrote the initial and final drafts of the article. All authors are responsible for the findings and have critically reviewed and approved the final draft of the article.
Conflicts of interest
The authors have no conflict of interest to declare.
Acknowledgment
Thanks to children and families who participated in the study and to the therapists at the outpatient clinic of the medical rehabilitation hospital, Almadinah Almunawwarah, KSA.
Footnotes
Peer review under responsibility of Taibah University.
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.jtumed.2017.07.002.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Richards C.L., Malouin F. Cerebral palsy: definition, assessment and rehabilitation. Handb Clin Neurol. 2013;111:183–195. doi: 10.1016/B978-0-444-52891-9.00018-X. [DOI] [PubMed] [Google Scholar]
- 2.Molina M., Kudlinski C., Guilbert J., Spruijt S., Steenbergen B., Jouen F. Motor imagery for walking: a comparison between cerebral palsy adolescents with hemiplegia and diplegia. Res Dev Disabil. 2015;37:95–101. doi: 10.1016/j.ridd.2014.10.053. [DOI] [PubMed] [Google Scholar]
- 3.Emara H.A., El-gohary T.M., Al-Johany A.H. Effect of body-weight suspension training versus treadmill training on gross motor abilities of children with spastic diplegic cerebral palsy. Eur J Phys Rehabil Med. 2016;52:356–363. [PubMed] [Google Scholar]
- 4.Brien M., Sveistrup H. An intensive virtual reality program improves functional balance and mobility of adolescents with cerebral palsy. Pediatr Phys Ther. 2011;23:258–266. doi: 10.1097/PEP.0b013e318227ca0f. [DOI] [PubMed] [Google Scholar]
- 5.Hwang J.H., Lee C.-H., Chang H.J., Park D.-S. Sequential analysis of postural control resource allocation during a dual task test. Ann Rehabil Med. 2013;37:347–354. doi: 10.5535/arm.2013.37.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kane K., Barden J. Frequency of anticipatory trunk muscle onsets in children with and without developmental coordination disorder. Phys Occup Ther Pediatr. 2014;34:75–89. doi: 10.3109/01942638.2012.757574. [DOI] [PubMed] [Google Scholar]
- 7.Kane K., Barden J. Contributions of the trunk muscles to anticipatory postural control in children with and without developmental coordination disorder. Hum Mov Sci. 2012;31:707–720. doi: 10.1016/j.humov.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 8.Zadnikar M., Kastrin A. Effects of hippotherapy and therapeutic horseback riding on postural control or balance in children with cerebral palsy: a meta-analysis. Dev Med Child Neurol. 2011;53:684–691. doi: 10.1111/j.1469-8749.2011.03951.x. [DOI] [PubMed] [Google Scholar]
- 9.Tarakci D., Ozdincler A.R., Tarakci E. Wii-based balance therapy to improve balance function of children with cerebral palsy: a pilot study. J Phys Ther Sci. 2013;25:1123–1127. doi: 10.1589/jpts.25.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wingert J.R., Burton H., Sinclair R.J., Brunstrom J.E., Damiano D.L. Joint-position sense and kinesthesia in cerebral palsy. Arch Phys Med Rehabil. 2009;90:447–453. doi: 10.1016/j.apmr.2008.08.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.El-Shamy S.M., Abd El kafy E.M. Effect of balance training on postural balance control and risk of fall in children with diplegic cerebral palsy. Disabil Rehabil. 2013:1–8. doi: 10.3109/09638288.2013.833312. [DOI] [PubMed] [Google Scholar]
- 12.Numanoglu A., Gunel M.K. Intraobserver reliability of modified Ashworth scale and modified Tardieu scale in the assessment of spasticity in children with cerebral palsy. Acta Orthop Traumatol Turc. 2012;46:196–200. doi: 10.3944/aott.2012.2697. [DOI] [PubMed] [Google Scholar]
- 13.Chen C.-L., Shen I.-H., Chen C.-Y., Wu C.-Y., Liu W.-Y., Chen C.-Y. Validity, responsiveness, minimal detectable change, and minimal clinically important change of pediatric balance scale in children with cerebral palsy. Res Dev Disabil. 2013;34:916–922. doi: 10.1016/j.ridd.2012.11.006. [DOI] [PubMed] [Google Scholar]
- 14.Franjoine M.R., Darr N., Held S., Kott K., Young B.L. The performance of children developing typically on the pediatric balance scale. Pediatr Phys Ther. 2010;22:350–359. doi: 10.1097/PEP.0b013e3181f9d5eb. [DOI] [PubMed] [Google Scholar]
- 15.Imran S., Moeliono M.A., Prabowo T. Loaded and unloaded sit-to-stand strengthening exercises effect to gross motor function measure in spastic diplegia cerebral palsy patients. IJIHS. 2016;4:8–14. [Google Scholar]
- 16.Rapport M.J., Furze J., Martin K., Schreiber J., Dannemiller L.A., DiBiasio P.A. Essential competencies in entry-level pediatric physical therapy education. Pediatr Phys Ther. 2014;26:7–18. doi: 10.1097/PEP.0000000000000003. [DOI] [PubMed] [Google Scholar]
- 17.de Graaf-Peters V.B., Blauw-Hospers C.H., Dricks T. Development of postural control in typically developing children and children with cerebral palsy: possibilities for intervention? Neurosci Biobehav Rev. 2007;31:1191–1200. doi: 10.1016/j.neubiorev.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 18.Chang C.F., Wang T.M., Lo W.C., Lu T.W., Hong S.W., Haung S.W. Balance control during level walking in children with spastic diplegic cerebral palsy. Biomed Eng Appl Basis Commun. 2011;23:509–517. [Google Scholar]
- 19.Liao H.F., Liu Y.C., Liu W.Y., Lin Y.T. Effectiveness of loaded sit-to-stand resistance exercise for children with mild spastic diplegia: a randomized clinical trial. Arch Phys Med Rehabil. 2007;88:25–31. doi: 10.1016/j.apmr.2006.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.El-gohary T.M., Khaled O.A., Ibrahim S.R., Al-shenqiti A.M., Ibrahim M.I. Effect of proprioception cross training on repositioning accuracy and balance among healthy individuals. J Phys Ther Sci. 2016;28:3178–3182. doi: 10.1589/jpts.28.3178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Elangovan N., Herrmann A., Konczak J. Assessing proprioceptive function: evaluating joint position matching methods against psychophysical thresholds. Phys Ther. 2014;94:553–561. doi: 10.2522/ptj.20130103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mawase F., Bar-Haim S., Karniel A. Lack of predictive control in lifting series of virtual objects by individuals with diplegic cerebral palsy. IEEE. 2011;19:686–695. doi: 10.1109/TNSRE.2011.2170589. [DOI] [PubMed] [Google Scholar]
- 23.Tomita H., Fukaya Y., Totsuka K., Tsukahara Y. Deficits in anticipatory inhibition of postural muscle activity associated with load release while standing in individuals with spastic diplegic cerebral palsy. J Neurophysiol. 2013;109:1996–2006. doi: 10.1152/jn.00253.2012. [DOI] [PubMed] [Google Scholar]
- 24.Khan Md Sadique, Pettnaik M., Mohanty P. Effect of arm movement without specific balance control training to improve trunk postural control in children with spastic diplegic cerebral palsy. Asian J Sci Technol. 2015;6:1907–1913. [Google Scholar]
- 25.Heyrman L., Feys H., Molenaers G., Jaspers E., Monari D., Nieuwenhuys A. Altered trunk movements during gait in children with spastic diplegia: compensatory or underlying trunk control deficit? Res Dev Disabil. 2014;35:2044–2052. doi: 10.1016/j.ridd.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 26.Heyrman L., Feys H., Molenaers G., Jaspers E., Monari D., Meyns P. Three-dimensional head and trunk movement characteristics during gait in children with spastic diplegia. Gait Posture. 2013;38:770–776. doi: 10.1016/j.gaitpost.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 27.Ju Y.H., Hwang I.S., Cherng R.J. Postural adjustment of children with spastic diplegic cerebral palsy during seated hand reaching in different directions. Arch Phys Med Rehabil. 2012;93:471–479. doi: 10.1016/j.apmr.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 28.Borstad J.D., Szucs K., Navalgund A. Scapula kinematic alterations following a modified push up plus task. Hum Mov Sci. 2009;28:738–751. doi: 10.1016/j.humov.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 29.El-gohary T.M., Hellman M.A., Ibrahim M.I., Abdel-Aziem A.A., Khaled U.A., Ahmed S.R. Partial versus full range of back extension endurance testing using the Swiss ball in discogenic low back pain patients: a comparative study. Eur J Physiother. 2014;16:113–120. [Google Scholar]
- 30.Bahramizadeh M., Mousavi M.E., Rassafiani M., Aminian G., Ebrahim I., Karimlou M. The effect of floor reaction ankle foot orthosis on postural control in children with spastic cerebral palsy. Prosthet Orthot Int. 2011;36:71–76. doi: 10.1177/0309364611429855. [DOI] [PubMed] [Google Scholar]
- 31.Lacoste M., Therrien M., Prince F. Stability of children with cerebral palsy in their wheelchair seating: perceptions of parents and therapists. Disabil Rehabil Assist Technol. 2009;4:143–150. doi: 10.1080/17483100802362036. [DOI] [PubMed] [Google Scholar]
- 32.Auld M.L., Johnston L.M. “Strong and steady”: a community based strength and balance exercise group for children with cerebral palsy. Disabil Rehabil. 2014;1:1–7. doi: 10.3109/09638288.2014.891054. [DOI] [PubMed] [Google Scholar]
- 33.Artilheiro M.C., Correa J.C.F., Cimolin V., Lima M.O., Galli M., de Gody W. Three-dimensional analysis of performance of an upper limb functional task among adults with dyskinetic cerebral palsy. Gait Posture. 2014;39:875–881. doi: 10.1016/j.gaitpost.2013.11.022. [DOI] [PubMed] [Google Scholar]
- 34.Chrysagis N.K., Skordilis E.K., Koutsouki D., Evans E. Kinesthetic ability in children with spastic hemiplegia. Adapt Phys Act Q. 2007;42:332–351. doi: 10.1123/apaq.24.4.332. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.