Abstract
Objectives
Community-based education (CBE) has an impact on the types of medical students produced at the end of medical training. However, its impact on professional identity development (PID) has not been clearly understood. This study thus explores the effect of the CBE program on PID.
Methods
A qualitative phenomenological study was conducted on a group of Universiti Sains Malaysia medical students who had finished the Community and Family Case Study (CFCS) program. Data were gathered through focused group discussions and student reflective journals. Participants were sampled using the maximal variation technique of purposive sampling. Three steps of thematic analysis using the Atlasti software were employed to identify categories, subthemes, and themes.
Results
Personal, role, social, and research identities were generated that contribute to the PID of medical students through the CFCS program. The results indicate that the CFCS program nurtured personal identity through the development of professional skills, soft skills, and personal values. Pertaining to role identity, this is related to patient care in terms of primary care and interprofessional awareness. Pertaining to social identity, the obvious feature was community awareness related to culture, society, and politics. A positive outcome of the CFCS program was found to be its fostering of research skills, which is related to the use of epidemiology and research methods.
Conclusion
The findings indicate that the CFCS program promotes PID among medical students. The current data highlight and provide insights into the importance of integrating CBE into medical curricula to prepare future doctors for their entry into the profession.
Keywords: Community-based education, Medical students, Political awareness, Professional identity, Qualitative study
الملخص
أهداف البحث
التعليم القائم على المجتمع له تأثير على أنواع طلاب الطب الذين يتخرجون في نهاية التدريب الطبي. لكن، لم يتم تحديد تأثيره على تطوير الهوية المهنية بوضوح. تكشف هذه الدراسة أدوار برنامج التعليم القائم على المجتمع على تطوير الهوية المهنية.
طرق البحث
أجريت دراسة ظاهرية نوعية على مجموعة من طلاب الطب بجامعة العلوم بماليزيا الذين انهوا برنامج دراسة حالة المجتمع والأسرة. تم جمع المعلومات من خلال مناقشات جماعية مركزة والمجلات التي تعكس رأي الطلبة. أُخذت عينات المشاركين من خلال تقنية الاختلاف القصوى للعينات الهادفة. كما تم استخدام ثلاث خطوات للتحليل المواضيعي باستخدام برنامج أطلس لتحديد الفئات والمواضيع الفرعية والموضوعات.
النتائج
تم إنشاء الشخصية، والدور، والهويات الاجتماعية والبحثية التي تساهم في تطوير الهوية المهنية لطلاب الطب من خلال برنامج دراسة حالة المجتمع والأسرة. أظهرت النتائج أن برنامج دراسة حالة المجتمع والأسرة قام برعاية الهوية الشخصية من خلال مهارات التعلم، والمهارات الناعمة والقيم الشخصية. أما المتعلقة بدور الهوية فارتبطت برعاية المرضى من حيث الرعاية الأولية والوعي بين المهنيين. وأما المتعلقة بالهوية الاجتماعية فكانت السمات الواضحة هي الوعي المجتمعي ذو الصلة الثقافية والاجتماعية والسياسية. وكانت النتائج الإيجابية لبرنامج دراسة حالة المجتمع والأسرة هي رعاية مهارات البحث، المتعلقة باستخدام علم الأوبئة وطرق البحث.
الاستنتاجات
تشير النتائج إلى أن برنامج دراسة حالة المجتمع والأسرة عزز تطوير الهوية المهنية بين طلاب الطب. البيانات الحالية سلطت الضوء وقدمت أفكارا على أهمية دمج التعليم القائم على المجتمع في منهج الطب لإعداد أطباء المستقبل.
الكلمات المفتاحية: المعتمد على المجتمع, الهوية المهنية, الوعي السياسي, طلاب الطب, النوعي
Introduction
There are three aspects of identity: (a) Personal identity is characterized by individual history, experience, personality, feelings, goals, and values; (b) role identity refers to one's assumed social or professional functions, activities, and responsibilities; and (c) social identity is the commitment to the values and goals of a specific group.1 In medical education, professional identity development (PID) plays an essential role in the transition medical students undergo when becoming doctors.2 Medical student professional identities are formed due to different factors such as various experiences, role models, and curricula.3, 4 Medical students' identities are conceptualized as both socially constructed and deeply personalized, whereby they develop medical professional identity through formal, non-formal, and hidden curricula.5
Upon entering medical school, baseline professional identity factors, which include gender, profession, previous working experience in the field, understanding of team work, knowledge of the profession, and cognitive ability, were found to be valid predictors of future PID.6 Studies have shown that medical students build up professional identity through their life experiences.2, 4 Therefore, medical school serves as a training ground for the development of professional identity among tomorrow's doctors, in which desirable professional behaviors are cultivated.7 In 1984, Harden et al. were the first of many investigators to demonstrate the movement in medical education away from traditional, didactic curricula to innovative curricula incorporating community-based education (CBE).8, 9 In CBE, students learn and acquire professional competencies (i.e., basic clinical, research, and communication skills) in a community setting established through community-campus collaboration, which provides students with contextualized and experiential learning that prepares them for providing patient care in local communities.9, 10, 11, 12, 13, 14 However, despite nearly 40 years of CBE program implementation worldwide,15 its effect on PID among medical students has not yet been adequately explored.
The Community and Family Case Study program
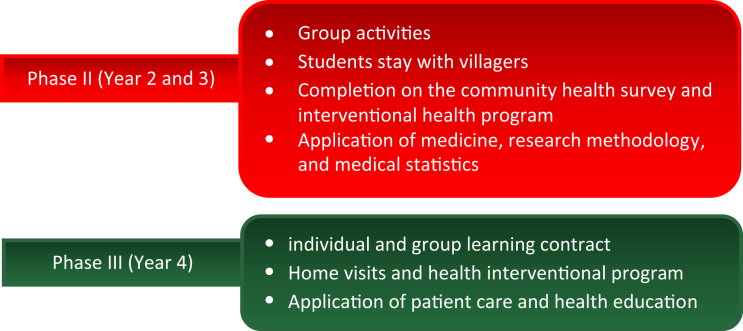
Concerning CBE, the School of Medical Sciences (SMS) at Universiti Sains Malaysia (USM) began implementing the Community and Family Case Study (CFCS) program in 1981,16 and the program has been evolving ever since. It is a compulsory CBE program for medical students during their medical training, and it is a key requirement that must be completed prior to their final examinations.16 Based on the CBE taxonomy,17 the CFCS program is categorized as a community-based research program, in which, in addition to CBE, research methods are learned through community engagements. Using this approach, students are expected to apply and acquire the necessary knowledge, values, and skills to become competent and professional doctors.16 Figure 1 summarizes the structure of the CFCS program and student activities at different phases of medical training.
Figure 1.
The structure of the CFCS program and student activities at different phases of medical training.
Phase II of the CFCS program is completed during the second and third year of medical studies. The purpose of Phase II is to develop communication skills, soft skills, and research skills through community-based learning experiences. The program begins with classroom-based theoretical lessons on public health, specifically on the principles of biostatistics, epidemiology, and occupational and environmental health.16 The students (about 20 students per group) are then placed in rural communities in the Kelantan district where they participate in homestays in local villagers' houses for 10-day visits. The students need to complete health, social, and educational issues surveys in their villages and then conduct statistical analyses to identify the main health problems in the village. Based on this research, the students must then propose an intervention program to address the issues.16 Subsequently, the students are required to conduct pre- and post-intervention survey analyses. At the end of Phase II of the CFCS program, the students present their community intervention project to their class and professor as an oral presentation as well as in a written report.
Phase III of the CFCS program consists of an individual as well as a group project during year 4 of the medical program. This phase aims to develop self-directed learning skills, foster a sense of responsibility for the students' own professional development, and encourage students to explore community health services.16 For the individual project, each student needs to partner with a patient of low socioeconomic status and generate a learning contract. For the group project, each group (consisting of 15–20 students) must select a group of patients suffering from a chronic disease.18 For both the individual and group projects, the students need to work with their supervisors to identify the problems faced by their patients and set their learning objectives, strategies to achieve the objectives, evidence of accomplishment of the learning objectives, and propose criteria for assessment.16, 18 At the end of the program, they must produce evidence of their accomplishment based on the learning contract, which will be assessed by their supervisors and peers.
Having discussed PID and CBE, it is worthwhile highlighting the important issue of unprofessional behaviors in the medical profession, such as greedy doctors who deceive patients by having them undergo unnecessary procedures and tests19 and those who breach patient confidentiality by disclosing medical records.20 These concerns reflect the need to educate quality medical professionals though CBE programs who will serve their nation and society in a professional and honest manner. In light of these concerns, the present study explored the experiences of medical students during the CFCS program and discussed its role in PID.
Materials and Methods
Study design, setting, and sample
A qualitative study was conducted and the phenomenology approach was employed to explore the experience of medical students related to their PID during the CFCS program. A purposive sampling method was performed, since it is the most reliable sampling method available for qualitative research.21 The maximum variation sampling technique was performed to select participants representative of different ethnic groups and of both genders. The sample size was estimated based on the saturation concept,22 in which saturation was achieved when there was no new theme generated in relation to the research objectives.
There were two eligibility criteria for participants in this study:
-
i.
The participants had to be in their final year of the medical program at USM;
-
ii.
The participants had to have completed all phases of the CFCS program.
A pool of participants was identified with the assistance of the Undergraduate Academic Office in the SMS at USM. To promote participation, the students were briefed with an explanation of the study aims and research method, and were provided with a consent form. Only those who consented participated in the focus group discussion (FGD) sessions. The participants were informed that they could withdraw from the study at any time for any reason. Their identity was kept anonymous and withdrawal from the study did not have any academic repercussions.
Data collection and analysis
Prior to data collection, ethical approval for the study was obtained from the Human Research Ethics Committee of USM. Data were collected through FGDs and student reflective journals (SRJ). The participants were then assigned with a unique code (ID) to maintain their anonymity and confidentiality. The students who agreed to participate were contacted by phone and the FGD sessions were arranged according to their availability.
An interview protocol was developed to standardize the FGD interviews. It consisted of an introduction, main interview questions, probing questions, and conclusion (see Appendix A). During the FGD sessions, researcher bracketing was applied to avoid internal and external bias.23 One method applied to ensure researcher bracketing was writing notes on important points mentioned by the participants and observable feelings during the FGDs.23
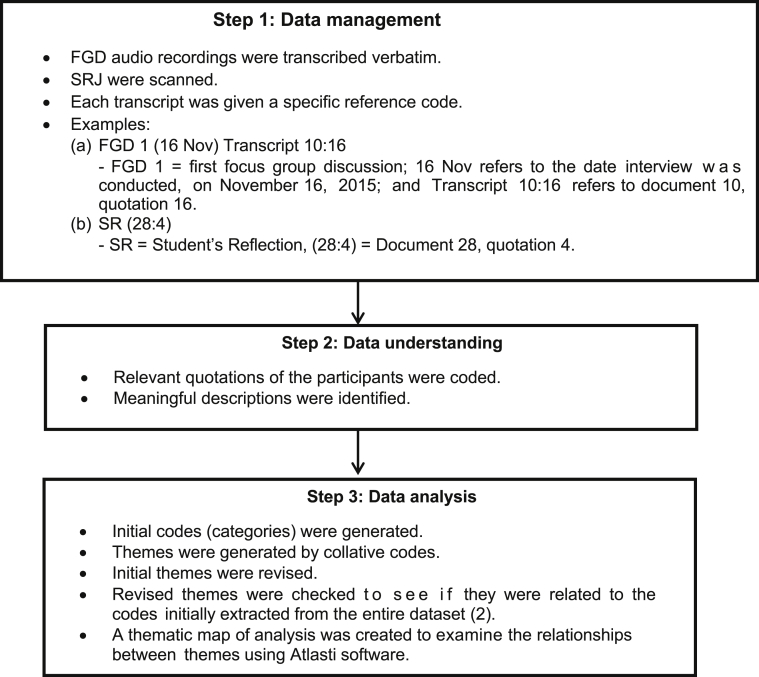
In this study, three steps of data analysis were employed (see Figure 2). Data management was commenced with the first data set gathered from the FGD sessions and SRJ. Thematic analysis was carried out to identify categories, subthemes, and themes.
Figure 2.
Steps in the data analysis.
Ethical considerations
This study obtained the ethical approval of the USM Human Research Ethics Committee. All participants who volunteered to participate in the FGD sessions were given a detailed participant information sheet and were clearly briefed on the study's procedures, de-identified information, risks, and benefits. To ensure no data leakage and to maintain the confidentiality of sensitive material/information regarding the CFCS, each participant agreed not to discuss the details of the study outside of the FGD sessions. The participants received a token of appreciation to prevent undue influence. The incentive was deemed appropriate for this group of participants to recognize their time and effort spent participating in the FGD sessions despite their busy academic schedules.
Results
A total of 21 students, including 15 Malays, four Chinese, and one Indian, voluntarily participated in the FGD sessions. A saturation point was reached during the third session, but we continued with the fourth session to ensure that no new theme could be generated. A total of 116 SRJs were collected from the USM CFCS office.
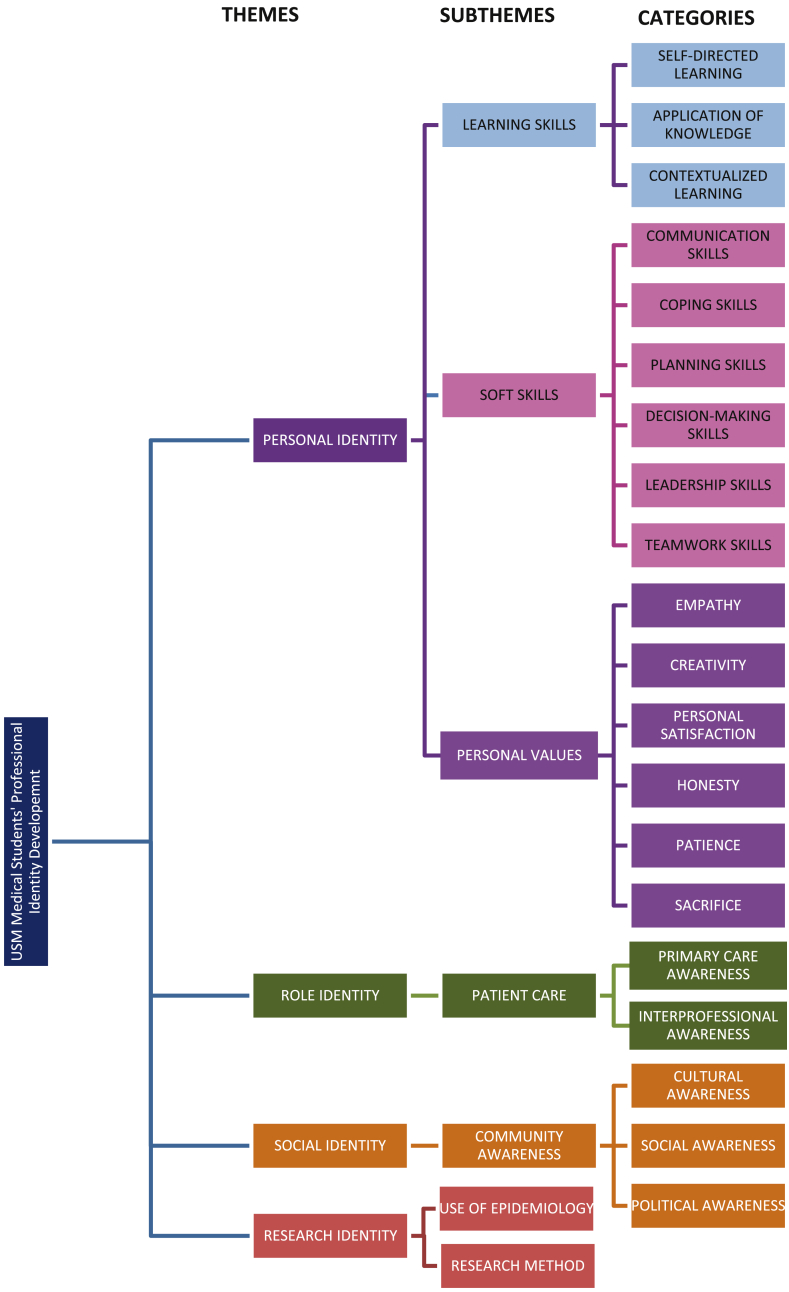
From the thematic analysis, four themes and seven subthemes were identified, and 20 categories were generated that related to PID during the CFCS program based on the experiences described by the medical students (see Figure 3).
Figure 3.
USM medical students' professional identity development through the CFCS program.
Theme 1: Personal identity
Every individual builds their personal identity through multiple factors throughout their personal life experiences.1 In the present study, the participants expressed that the CFCS program gave them opportunities to choose their own patient based on their preferred case. They were able to apply their knowledge in context, and knowledge transfer occurred through communication with the community. As the program allowed them to interact directly with the community members, it enhanced their soft skills such as teamwork, leadership, decision-making, coping, planning, and communication skills. In addition, the participants also shared that they developed personal attributes such as empathy, creativity, personal satisfaction, honesty, patience, and sacrifice. Some of the students' quotes concerning PID from the FGD sessions and SRJ are displayed in Table 1.
Table 1.
Participants' quotes from the FGD and SRJ on personal identity.
| Subthemes | FGD quote | SRJ quote |
|---|---|---|
| Learning skills |
“… then I tried to explain it … not only just explain what will happen but why it happened.” [FGD 1 (16 Nov) Transcript – 28:32] |
“I am able to deliver my knowledge about chronic kidney disease, its risk factors, symptoms, and how to control the disease …” [SR (15:60)] |
| Soft skills |
“… so, I made a decision, I want to deal with only one person.” [FGD 2 (18 Nov) Transcript – 31:27] |
“Whenever I visited her, I tried to listen to her life problems …” [SR (35:5)] |
| Personal values |
“… (I felt) pity for her (patient) because she lives with her daughter who divorced and had many children.” [FGD 324 Transcript – 32:38] |
“I learned how to communicate … by putting myself in their shoes.” [SR (18:12)] |
Theme 2: Role identity
Role identity for a doctor is an expansive process and essential part of medical students' PID.2 The participants mentioned that the CFCS program helped them to develop their role identity by providing experiences in patient care, particularly primary care and interprofessional awareness. Several quotes generated from the participants on role identity are displayed in Table 2.
Table 2.
Participants' quotes from the FGD and SRJ on role identity.
| Subthemes | FGD quotes | SRJ quotes |
|---|---|---|
| Primary care awareness |
“We promote any healthy lifestyle to them (the villagers) … such as advising them to reduce their salt intake …” [FGD 1 (16 Nov) Transcript – 28:8] |
“… we must ensure a mutual understanding of disease between patient and doctor … thus, we achieved a desirable and optimal patient condition.” [SR (16:6)] |
| Interprofessional practice |
“… having connected to different people from different angles, like from nutrition, etc.” [FGD 4 (10 Dec) Transcript - 34:42] |
“… multidisciplinary approach from psychiatry, occupational therapy, behavioral therapy, psychotherapy …” [SR (15:24)] |
Theme 3: Social identity
Social identity is formed when an individual undergoes experiences and observations in a community setting, and develops a new social awareness of themselves.1 The CFCS program contributes a unique opportunity for medical students to develop their social identities in a local community. Table 3 shows some interesting quotes shared by the participants about developing their cultural, social, and political awareness through the CFCS program.
Table 3.
Participants' quotes from FGD and SRJ on social identity.
| Subthemes | FGD quotes | SRJ quotes |
|---|---|---|
| Cultural awareness |
“But not everyone (villagers) goes to the 'surau' (mosque) … some of them there, missed (the announcement).” [FGD 1 (16 Nov) Transcript – 28:6] |
“… especially in Kelantan, … food preparation is more prone to sweetness.” [SR (15:32)] |
| Social awareness |
“… we went for a house visit, and we saw that he (the patient) did not have family support.” [FGD 324 Transcript – 32:43] |
“… factors that influence the patient's progression, such as financial burden, accessibility to healthcare, and preconceived knowledge.” [SR (15:7)] |
| Political awareness |
“… if we (show support for) one side (political party), another side of the villagers and their supporters don't come to our activity.” [FGD 1 (16 Nov) Transcript - 28:14)] |
Theme 4: Research identity
It was found that the participants gained some experience in developing their research identity during the CFCS program. Research skills are essential for academics in the evidence-based era. In this study, two subthemes were identified under research skills, which are the use of epidemiology and research methodology (Table 4).
Table 4.
Participants' quotes from the FGD and SRJ on research identity.
| Use of epidemiology | “… compared to national prevalence, the people in that village have more … heart attacks than the national average.” [FGD 1 (16 Nov) Transcript – 28:3] |
“That time, we had to conduct surveys … on the dominant illness surveyed.” [SR (21:1)] |
| Research methodology |
“… we gave the same questionnaire … there was an improvement in terms of knowledge … and objectives, which was to assess the knowledge.” [FGD 4 (10 Dec) Transcript – 34:37] |
“That time, we had to conduct surveys and determine a few interventions …” [SR (21:1)] |
Discussion
Personal identity
This study found that developing personal skills and values were perceived as being beneficial learning experiences that facilitated the development of self-competency. It is worth noting that personal identity is not exclusively developed through a single life event; rather, it is a continuous development process that occurs through individual life experiences that also contribute to role and social identity development.1 The data shows that learning skills are acquired through various learning techniques and life experiences, and are considered to be a part of professional competency.25 An earlier study reported that USM medical graduates who underwent the CFCS program had better learning skills, which suggests the greater development of personal identity as was found in the present study.26 One possible explanation is that students are allowed to choose their own clinical case study for their learning project that must be approved by supervisors. Many of the students expressed that they learned to how to conduct their own research on relevant information related to their clinical case study, and later to plan appropriate interventions to address the needs of their patient. Furthermore, the students admitted that they were able to apply theoretical and clinical knowledge to the real context during the community intervention project, and considered themselves as knowledge providers. It is worth mentioning that the aforementioned attributes are considered to be essential elements of medical professional identity,27 thus indicating that the CFCS program exposes students to authentic learning environments that enable them to immediately exchange knowledge with patients and communities. These results are aligned with the goal of CBE to produce medical graduates who are equipped with applicable professional knowledge.9, 10, 13
Soft skills are essential elements of life-long learning that enhance personal development such as interpersonal skills and desirable career attributes.28, 29 Communication skills are one of the essential soft skills targeted by CBE programs.9, 18 The present study found that the medical students developed several soft skills as a result of the CFCS program, including communication skills, coping skills, planning skills, decision-making skills, leadership skills, and teamwork skills. Students gained these skills through various experiences during the CFCS program. For example, their interactions with community members, patients, peers, and supervisors; modeling behavior based on their observations and experiences during the CBE30; and their effort to understand the local dialect and culture all contributed to their development of soft skills.31 These findings are consistent with those of a previous study, which found that USM medical students improved their communication skills through participation in the CFCS program.32 In addition, another study obtained similar results whereby students who participated in a CBE program developed better communication skills than those who did not.33 Joubert et al. (2006) also found that students' communication skills improved through observations and experiences during CBE. Another important soft skill is the ability to cope with stressful situations, because medical students are vulnerable to psychological distress, as evidenced by the high prevalence of psychological distress among them, which is often higher than that of the general population.34, 35, 36 Interestingly, among the coping skills frequently mentioned by the students were active coping (e.g., finding alternative ways to achieve their goal and create an effective team), positive thinking (i.e., maintaining a positive mind-set), and planning (e.g., effective time management and discussion with supervisors/committee). These strategies are classified as functional coping strategies that can help to mitigate the effects of stress.37, 38, 39, 40 A possible explanation for their high levels of stress is that the students were exposed to various challenges during the CFCS program, including financial challenges, transportation planning, human resource management, handling patient diversity, and communicating effectively with supervisors, yet the students dealt with these stressful circumstances tactfully and effectively.
As indicated previously, the soft skills related to group dynamics such as decision-making skills, leadership skills, and teamwork skills are as important as communication skills and coping skills.32 The students shared their experience of being a leader in terms of collaborating with other parties in the community, delegating jobs and tasks to other group members, as well as planning and decision-making. It is noteworthy that a CBE program in the United States reported that leadership skills were enhanced during the program.41 Apart from leadership skills, teaching medical students about teamwork skills is a real challenge,42 as evidenced by medical schools employing various teaching methods such as case studies, non-medical teambuilding activities, and role plays43 for that purpose. Despite the common challenge of fostering the development of teamwork skills in educational programs, the CFCS program was found to effectively contribute to their development through the group project task. An interesting finding from a previous study conducted on a pre-registered house officer, reported that students rarelygot the opportunity to make clinical decisions in patient management.44 Therefore, the CFCS program may serve as a good platform for medical students to experience making clinical decisions in patient management.
Another important aspect of personal identity found in this study was personal values, including empathy, creativity, personal satisfaction, honesty, patience, and sacrifice. While other medical programs attempt to nurture the growth of empathy in medical students through drama and role play,45 the USM students believed that the CFCS program helped to build their empathy through exposure to real people's health and living conditions (i.e., socioeconomic, psychosocial, and sociocultural), thus fostering feelings of empathy and a better understanding of patients' conditions.46 A previous study has echoed that empathy is an area of concern among medical students; therefore, any opportunities to nurture empathy during medical training are highly valuable.47 Regarding creativity, the medical students were forced to become more creative to deliver the best community project at the end of the CFCS program–creativity was not explicitly taught in the classroom. This finding is supported by previous studies that demonstrated that medical students had unique ways of expressing their creativity in their own contexts.2, 27, 48 Another interesting finding is that personal satisfaction, honesty, patience, and sacrifice generated from the analysis correspond to the framework of Malaysian medical professionalism.49 This fact further supports the positive impact of the CFCS program in the PID of medical students.
Role identity
The most obvious finding to emerge pertaining to role identity is related to primary care and interprofessional awareness in patient care. This suggests that the CFCS program provided authentic learning experiences in medical PID as the students were responsible for assuming the role of doctors during patient management and home visits. As echoed by Tan (2014), professional experiences considered to be authentic learning contributed to PID. Similarly, a mixed-method study on CBE in Japan demonstrated comparable results in creating primary care awareness among medical students through community hospital and clinical postings for several weeks.50 These facts explain the reason for some medical schools adopting primary care-oriented training programs as CBE.17 The CFCS program is a unique CBE program because students are exposed to hospital-, community-, and home-based patient care over a three-year period.16, 18 Another important finding related to role identity in interprofessional collaboration as reflected by the medical students, which is, in fact, an important element of the recent Malaysian medical professionalism framework.49 The CFCS individual and community projects that involved other disciplines such as dietetics and nutrition, family medicine, and community medicine demonstrated to the students the importance of inter-disciplinary collaboration as a part of a holistic approach to patient management. Consistent with the literature, an interdisciplinary curriculum coupled with community involvement was shown to expose medical students to public service and social activism.51, 52 It can therefore be stated that medical schools should adopt these common features of CBE, as community projects and a holistic approach to patient care are essential for students to appreciate the importance of interprofessional collaboration in the field of medicine.
Social identity
The obvious feature of social identity was community awareness related to culture, society, and politics. Social identity is directly related to group activities and interactions with people that contribute to the development of social skills.1 The common goal of medical schools that employ CBE is to foster the development of the social skills of their students.9, 11, 17, 53 In the present study, the medical students were exposed to a unique local culture, which required them to understand the community they were working with in order to be tactful in their approach to treating patients. This feature was also addressed by an Australian study on medical education, in which they had implemented a program to foster the development of competence and cultural sensitivity among medical students.54 An earlier study also showed that medical students who underwent CBE were able to relate psychosocial issues to human rights, which helped them to gain insight into the psychosocial contexts of their patients.55 An interesting aspect related to community awareness is political awareness, and a previous study showed that good public health professionals must be aware of political conditions.56 This study explained that medical students encountered challenges while planning and implementing a community project due to different political beliefs in the community. This experience had been an eye-opener to them regarding the possible influence of political beliefs on community behavior toward health intervention.
Research identity
Despite the barriers preventing the development of research skills among undergraduate medical students, such as the lack of time due to heavy academic demands, the lack of motivation and rewards, the lack of proper mentoring by lecturers, the lack of knowledge and research skills, and the lack of funding for research,57, 58 USM has positioned the CFCS program as a research-oriented program and the main agenda in its curriculum since 1979.17 This theme was found to be exclusive, as it is not included in any of the three categories in professional identity theory.1 While other medical students are less aware of research activities,59 the present study found that students gained two research skills as a result of participation in a CBE program, including the use of epidemiology and research methods. In the medical profession, research skills are not directly related to the roles of a doctor. However, research skills serve as added value to a doctor's set of professional skills. The expanding medical world requires a lot of research and evidence-based medical practice. Thus, research skills may soon be included as one of the required competencies of medical students, as studies have demonstrated the favorable effect of integrating research skills into medical curricula.8, 57, 60 A recent study reported that a one-month research rotation improved research activity and enhanced students' chances of being accepted to postgraduate programs.60 In addition, a study comparing biology students who underwent community-based research training developed higher critical thinking abilities than those who attended traditional lectures.8 These initial results are suggestive of a link between CBE and research skills among medical students. Therefore, future studies on the current topic are recommended. It is worth noting that the CFCS program has successfully attained its purpose of fostering the development of research skills among medical students since its inception.16, 17, 53
Limitations and recommendations
Despite the promising outcomes of the present study, there are several limitations that should be noted. First, the transferability of these findings should be made within the individual context of each university, since CBE practices differ from institution to institution. Therefore, we recommend that the PID of CBE at different institutions should be explored and compared to verify the transferability of the present study's findings. Second, this study mainly depended on qualitative measures; therefore, the results may only apply to the medical student sample of the present study. Thus, adding quantitative measures in future research may enable the findings to be generalized to the population. Lastly, the research method was based on phenomenology; therefore, adding other research methods such as ethnography, discourse analysis, or action research will enable the data to be triangulated from different perspectives on PID.
Conclusion
The findings clearly indicate that the CBE program promoted the development of professional identity among medical students through personal identity, role identity, social identity, and research identity. These data highlight and provide insights into the importance of integrating CBE into medical curricula to prepare medical students to become competent and qualified medical professionals.
Authors' contributions
AA, MZMN, and WZWM designed the study and the data collection methods. AA and MSBY analyzed and interpreted the data, provided logistical support, and conducted the final review of the results. AA wrote the initial and final draft of the article. All authors are responsible for the findings, have critically reviewed the paper, and have approved of the final draft.
Conflicts of interest
The authors declare that there is no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Acknowledgements
The authors would like to thank the USM medical students who participated in this study for sharing their experiences in the CFCS program. This study also received funding through a Short-Term Grant from the Universiti Sains Malaysia (301/PPSP/61313105).
Footnotes
Peer review under responsibility of Taibah University.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jtumed.2017.12.001.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Stets J.E., Burke P.J. Identity theory and social identity theory. Soc Psychol Q. 2000:224–237. [Google Scholar]
- 2.Tan C.P. 2014. Educating for professional identity development: Faculty of Social Sciences (FSS) [Google Scholar]
- 3.Niemi P. Medical students' professional identity: self-reflection during the preclinical years. Med Educ. 1997;31(6):408–415. doi: 10.1046/j.1365-2923.1997.00697.x. [DOI] [PubMed] [Google Scholar]
- 4.Wilson I., Cowin L.S., Johnson M., Young H. Professional identity in medical students: pedagogical challenges to medical education. Teach Learn Med. 2013;25(4):369–373. doi: 10.1080/10401334.2013.827968. [DOI] [PubMed] [Google Scholar]
- 5.Frost H.D., Regehr G. “I AM a Doctor”: negotiating the discourses of standardization and diversity in professional identity construction. Acad Med. 2013;88(10):1570–1577. doi: 10.1097/ACM.0b013e3182a34b05. [DOI] [PubMed] [Google Scholar]
- 6.Adams K., Hean S., Sturgis P., Clark J.M. Investigating the factors influencing professional identity of first-year health and social care students. Learn Heatlh Soc Care. 2006;5(2):55–68. [Google Scholar]
- 7.Yusoff M.S.B. Professional behaviour: what does it means? Educ Med J. 2009;1(1) [Google Scholar]
- 8.Quitadamo I.J., Faiola C.L., Johnson J.E., Kurtz M.J. Community-based inquiry improves critical thinking in general education biology. CBE-Life Sci Educ. 2008;7(3):327–337. doi: 10.1187/cbe.07-11-0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mariam D.H., Sagay A.S., Arubaku W., Bailey R.J., Baingana R.K., Burani A. Community-based education programs in Africa: faculty experience within the Medical Education Partnership Initiative (MEPI) network. Acad Med. 2014;89(8):S50–S54. doi: 10.1097/ACM.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 10.Okayama M. Community-based medical education. Gen Med. 2014;15(1):3–4. [Google Scholar]
- 11.Hunt J.B., Bonham C., Jones L. Understanding the goals of service learning and community-based medical education: a systematic review. Acad Med. 2011;86(2):246–251. doi: 10.1097/ACM.0b013e3182046481. [DOI] [PubMed] [Google Scholar]
- 12.Mennin S., Petroni-Mennin R. Community-based medical education. Clin Teach. 2006;3(2):90–96. [Google Scholar]
- 13.Seifer S. Recent and emerging trends in undergraduate medical education. Curricular responses to a rapidly changing health care system. West J Med. 1998;168(5):400. [PMC free article] [PubMed] [Google Scholar]
- 14.Kennedy E.M. Beyond vertical integration: community based medical education. Aust Fam Phys. 2006;35(11):901. [PubMed] [Google Scholar]
- 15.Harden R.M., Sowden S., Dunn W.R. Educational strategies in curriculum development: the SPICES model. Med Educ. 1984;18(4):284–297. doi: 10.1111/j.1365-2923.1984.tb01024.x. [DOI] [PubMed] [Google Scholar]
- 16.Zabidi-Hussin Z.A.M.H. Curricular trends in Malaysian medical schools: innovations within. Ann Acad Med Singap. 2006;35:647–654. [PubMed] [Google Scholar]
- 17.Magzoub M.E.M., Schmidt H.G. A taxonomy of community-based medical education. Acad Med. 2000;75(7):699–707. doi: 10.1097/00001888-200007000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Taib F., Mohd Fakri N.M.R. Revitalizing community and Family Case Study (CFCS) programme. Educ Med J. 2014;6(3):e46–e50. [Google Scholar]
- 19.Stanley S. The Star; 2013. Beware of unethical doctors. [Google Scholar]
- 20.Hari D.K.K. 2014. Krishnan. Malaysian Medical Association – Dr. Krishna Kumar Hari Krishnan, President Pharmaboardroom.http://pharmaboardroom.com/interviews/malaysian-medical-association-dr-krisha-kumar-hari-krishnan-president/ Available from: [Google Scholar]
- 21.Liamputtong P. 3rd ed. 2009. Qualitative research methods. ed: oxford. [Google Scholar]
- 22.Ritchie J., Lewis J., Nicholls C.M., Ormston R. Sage; 2013. Qualitative research practice: a guide for social science students and researchers. [Google Scholar]
- 23.Tufford L., Newman P. Bracketing in qualitative research. Qual Soc Work. 2012;11(1):80–96. [Google Scholar]
- 24.Mykytyn K., Pearson A., Paul S., Mykytyn P.P. The use of problem-based learning to enhance MIS education. Decis Sci J Innovat Educ. 2008;6(1):89–113. [Google Scholar]
- 25.Boud D., Keogh R., Walker D. Routledge; 2013. Reflection: turning experience into learning. [Google Scholar]
- 26.Hassan S. Commitment of medical graduates educated with and without community-based medical education towards community health care: a study from Malaysia. Educ Med J. 2013;5(4) [Google Scholar]
- 27.Korkmaz H., Senol Y.Y. Exploring first grade medical students' professional identity using metaphors: implications for medical curricula. Med Educ Online. 2014;19 doi: 10.3402/meo.v19.20876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Robles M.M. Executive perceptions of the top 10 soft skills needed in today's workplace. Bus Commun Q. 2012;75(4):453–465. [Google Scholar]
- 29.Gibb S. Soft skills assessment: theory development and the research agenda. Int J Lifelong Educ. 2014;33(4):455–471. [Google Scholar]
- 30.Joubert P.M., Krüger C., Bergh A.-M., Pickworth G.E., Van Staden C., Roos J.L. Medical students on the value of role models for developing'soft skills'-" that's the way you do it. Afr J Psychiatr. 2006;9(1):28–32. [Google Scholar]
- 31.Khaw Y.-M.J., Tan T.-P. A fast adaptation technique for building dialectal malay speech synthesis acoustic model. Jurnal Teknologi. 2015;77(19) [Google Scholar]
- 32.Salam A. Community and family case study: a community-based educational strategy to promote five star doctors for the 21st century. South-East Asian J Med Educ. 2009;3(1):20–24. [Google Scholar]
- 33.Oswald N., Alderson T., Jones S. Evaluating primary care as a base for medical education: the report of the Cambridge community-based clinical course. Med Educ. 2001;35(8):782–788. doi: 10.1046/j.1365-2923.2001.00981.x. [DOI] [PubMed] [Google Scholar]
- 34.Yusoff M.S.B., Rahim A.F.A., Yaacob M.J. Prevalence and sources of stress among Universiti Sains Malaysia medical students. Malays J Med Sci: MJMS. 2010;17(1):30. [PMC free article] [PubMed] [Google Scholar]
- 35.Yusoff M.S.B., Abdul Rahim A.F., Baba A.A., Ismail S.B., Mat Pa M.N., Esa A.R. The impact of medical education on psychological health of students: a cohort study. Psychol Health Med. 2013;18(4):420–430. doi: 10.1080/13548506.2012.740162. [DOI] [PubMed] [Google Scholar]
- 36.Puthran R., Zhang M.W., Tam W.W., Ho R.C. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50(4):456–468. doi: 10.1111/medu.12962. [DOI] [PubMed] [Google Scholar]
- 37.Carver C.S. You want to measure coping but your protocol too long: consider the brief cope. Int J Behav Med. 1997;4(1):92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- 38.Carver C.S., Scheier M.F., Weintraub J.K. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- 39.Yusoff M.S.B., Ahmad Hamid A., Rosli N.R., Zakaria N.A., Che Rameli N., Abdul Rahman N. Prevalence of stress, stressors and coping strategies among secondary school students in Kota Bharu, Kelantan, Malaysia. Int J Stud Res. 2011;1(1):2. [Google Scholar]
- 40.Arifin W.N., Yusoff M.S.B., Naing N.N. Confirmatory factor analysis (CFA) of USM Emotional Quotient Inventory (USMEQ-i) among medical degree program applicants in Universiti Sains Malaysia (USM) Educ Med J. 2012;4(2) [Google Scholar]
- 41.Carufel-Wert D.A., Younkin S., Foertsch J., Eisenberg T., Haq C.L., Crouse B.J. LOCUS: immunizing medical students against the loss of professional values. Fam Med-Kansas City- 2007;39(5):320. [PubMed] [Google Scholar]
- 42.O Connell M.T., Pascoe J.M. Undergraduate medical education for the 21st century: leadership and teamwork. Fam Med-Kansas City- 2004;36(1; SUPP):S51–S56. [PubMed] [Google Scholar]
- 43.Chakraborti C., Boonyasai R.T., Wright S.M., Kern D.E. A systematic review of teamwork training interventions in medical student and resident education. J Gen Intern Med. 2008;23(6):846–853. doi: 10.1007/s11606-008-0600-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lempp H., Seabrook M., Cochrane M., Rees J. The transition from medical student to doctor: perceptions of final year students and preregistration house officers related to expected learning outcomes. Int J Clin Pract. 2005;59(3):324–329. doi: 10.1111/j.1742-1241.2005.00438.x. [DOI] [PubMed] [Google Scholar]
- 45.Deloney L.A., Graham C.J. DEVELOPMENTS: Wit: using Drama to teach first-year medical students about empathy and compassion. Teach Learn Med. 2003;15(4):247–251. doi: 10.1207/S15328015TLM1504_06. [DOI] [PubMed] [Google Scholar]
- 46.Wong A., Trollope-Kumar K. Reflections: an inquiry into medical students' professional identity formation. Med Educ. 2014;48(5):489–501. doi: 10.1111/medu.12382. [DOI] [PubMed] [Google Scholar]
- 47.Hojat M., Vergare M.J., Maxwell K., Brainard G., Herrine S.K., Isenberg G.A. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182–1191. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 48.Graves G.O., Ingersoll R.W., Evans L.R. The creative medical student: a descriptive study. J Creativ Behav. 1967;1(4):371–382. [Google Scholar]
- 49.Roslan N.S., Yusoff M.S., Rahim A.F.A., Hussin Z.A.M. Together we stand, divided we fall: interprofessional collaborative practice competencies from Malaysian medical professionals' perspectives. J Taibah Univ Med Sci. 2016;11(6):533–540. [Google Scholar]
- 50.Kikukawa M., Oda Y., Ishii K., Ono M., Nabeta H., Yoshida M. Mixed-method outcome evaluation of a community-based education program for medical students. Gen Med. 2014;15(1):21–28. [Google Scholar]
- 51.Donohoe M., Danielson S. A community-based approach to the medical humanities. Med Educ. 2004;38(2):204–217. doi: 10.1111/j.1365-2923.2004.01756.x. [DOI] [PubMed] [Google Scholar]
- 52.Goodrow B., Olive K.E., Behringer B., Kelley M.J., Bennard B., Grover S. The community partnerships experience: a report of institutional transition at East Tennessee State University. Acad Med. 2001;76(2):134–141. doi: 10.1097/00001888-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 53.WMZW M., Rahman A.A., Sidek M.Y., Shafei M.N., Daud A., Aziz A.A. Community engagement through a community-based medical curriculum in a North-eastern State in Malaysia. Int e-J Community Ind Engagem. 2014;1(2):31–39. [Google Scholar]
- 54.Fox G.J., Thompson J.E., Bourke V.C., Moloney G. Medical students, medical schools and international health. Med J Aust. 2007;187(9):536. doi: 10.5694/j.1326-5377.2007.tb01400.x. [DOI] [PubMed] [Google Scholar]
- 55.O'Sullivan M., Martin J., Murray E. Students' perceptions of the relative advantages and disadvantages of community-based and hospital-based teaching: a qualitative study. Med Educ. 2000;34(8):648–655. doi: 10.1046/j.1365-2923.2000.00623.x. [DOI] [PubMed] [Google Scholar]
- 56.Gillam S., Maudsley G. Public health education for medical students: rising to the professional challenge. J Public Health. 2010;32(1):125–131. doi: 10.1093/pubmed/fdp108. [DOI] [PubMed] [Google Scholar]
- 57.Laidlaw A., Aiton J., Struthers J., Guild S. Developing research skills in medical students: AMEE Guide No. 69. Med Teach. 2012;34(9):754–771. doi: 10.3109/0142159X.2012.704438. [DOI] [PubMed] [Google Scholar]
- 58.Amin T.T., Kaliyadan F., Al Qattan E.A., Al Majed M.H., Al Khanjaf H.S., Mirza M. Knowledge, attitudes and barriers related to participation of medical students in research in three Arab Universities. Educ Med J. 2012;4(1):e43–e56. [Google Scholar]
- 59.Burgoyne L.N., O'Flynn S., Boylan G.B. Undergraduate medical research: the student perspective. Med Educ Online. 2010:15. doi: 10.3402/meo.v15i0.5212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ayuob N.N., Banjari M.A., AlMarghoub M.A., AlQulayti W., Eldeek B. Effect of integrating research skills in the medical curriculum: a comparative cross sectional study on students’ research practices and their perception at King Abdulaziz University, Jeddah. Educ Med J. 2016;8(2):e27–e39. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.