Abstract
Background
The incidence of flatfoot is approximately 5% in children and adults. The symptomatic form of a flexible flatfoot produces subjective and objective complaints, including gait disturbances. Surgical intervention is considered when conservative management fails. The arthroereisis procedure provides a stable foot and durable correction. However, to the best of our knowledge, no study has evaluated the effectiveness of this procedure on gait parameters.
Methods
Fifteen children with painful flatfeet (10 males; 5 females) with a mean age of 12 years and 6 months underwent the calcaneo stop procedure. Radiographic, gait analysis and functional measures were evaluated to assess the changes pre- and post-operatively.
Results
All children were followed up for a mean period of 4 years and 6 months. The overall results of the study exhibited statistically significant improvement for all radiographic variables, functional measures and range of motion investigated in the study (p < 0.05). Although the study showed improvement in all temporal parameters (p < 0.05) measured in the gait analysis, the results demonstrated there were no statistically significant differences in the kinematic and kinetic variables (p > 0.05) before and after surgery.
Conclusions
Although there was no significant improvement in the kinematic and kinetic variables investigated, this study supports the calcaneo-stop procedure as a reliable and effective procedure for treating paediatric flexible flatfoot.
Keywords: Biomechanical phenomena, Flatfoot, Gait, Surgery mutation
الملخص
أهداف البحث
إن نسبة الأقدام المسطحة في الأطفال والبالغين هي حوالي ٥٪. ويُنتج النوع المصحوب بالأعراض من الأقدام المسطحة المرنة شكاوى ذاتية وموضوعية مثل اضطرابات المشية. ويُلجأ إلى التدخل الجراحي عند فشل العلاج التحفظي. وقد بينت الأبحاث أن إجراءات التقييد المفصلي توفر قدما مستقرة وتصحيحا متينا٬ إلا أنه لم تقم أي من الدراسات بتقييم فاعلية هذا الإجراء على معالم المشية.
طرق البحث
أُجريت عملية “إيقاف عظمة العقب” على ١٥ طفلا لديهم أقداما مسطحة مؤلمة (١٠ أولاد و٥ بنات) بمتوسط عمر ١٢ سنة و٦ أشهر. وتم تقييم الأشعة وتحليل المشية والقياسات الوظيفية لمعرفة التغيرات قبل وبعد العملية.
النتائج
تمت متابعة جميع الأطفال لمدة متوسطها ٤ سنوات و٦ أشهر. وأظهرت النتائج العامة للدراسة تحسنا ذا قيمة إحصائية لجميع المتغيرات الإشعاعية والقياسات الوظيفية ومدى الحركة التي تم التحقق منها في الدراسة. على الرغم من أن الدراسة أظهرت تحسنا في جميع المعالم الزمنية التي تم قياسها عند تحليل المشية٬ إلا أن النتائج لم تُظهر أي اختلافات ذات قيمة إحصائية في المتغيرات الحركية القياسية والحركية قبل وبعد الجراحة.
الاستنتاجات
على الرغم من عدم وجود تحسن ذي قيمة في المتغيرات الحركية القياسية والحركية التي تم التحقيق فيها٬ نستنتج بأن عملية “إيقاف عظمة العقب” هي عملية فعالة ويمكن الاعتماد عليها في علاج القدم المسطحة المرنة لدى الأطفال.
الكلمات المفتاحية: القدم المسطحة, المشية؛ ظاهرة حركية حيوية, الجراحة؛ طفرة جينية, عملية إيقاف عظمة العقب
Introduction
Flatfoot is a developmental or acquired deformity that is progressive, and it is characterized by plantar medial rotation of the talus, a decrease in the medial arch height, and abduction of the forefoot.1 The incidence of flat foot is approximately 5% in children and adults.2, 3 Flexible paediatric flatfoot is one of the most common deformities of the human body.4 Flexible flatfoot is characterized by the normal architecture of the medial longitudinal arch during non-weight bearing and flattening of the arch during stance or weight bearing.5, 6 Flexible flatfoot may be symptomatic or asymptomatic.5
Symptomatic forms of flexible flatfoot produce subjective and objective complaints, including pain along the medial side of the foot, sinus tarsi, leg, and knee. Flatfoot decreases endurance and leads to gait disturbances.5 Pronation of the subtalar joint during the propulsive phase of gait is mostly responsible for major deformities in adult life.7 Flatfoot may also lead to hallux valgus, metatarsalgia, tarsal tunnel syndrome, posterior tibial tendon dysfunction, and osteoarthritis of the subtalar and midtarsal joints.8, 9 Flat foot is associated with bio-mechanical changes and leads to a general structural deformity of the lower extremity.10 Initial management for flatfoot includes activity modifications, orthoses,11 foot exercises12 and nonsteroidal anti-inflammatory medications. If conservative management fails, surgical intervention can be considered.13, 14, 15
Surgical management of flatfoot can be grouped into the following three types: soft tissue, bone (osteotomies and arthrodesis) and arthroereisis.16 Soft tissue reconstruction of the flexible flatfoot is rarely successful as an isolated procedure and should always be combined with bony procedures or arthroereisis.17 Excellent results from the reconstructive bony procedures of flatfoot have been reported. However, the long-term results are not satisfactory.18 Arthrodesis (extra-articular subtalar arthrodesis for symptomatic plano-valgus feet and triple arthrodesis for failed surgical treatment) provides a stable foot and durable correction. However, this procedure transfers energy to the non-fused adjacent joints, which may lead to early arthritis.19, 20
Arthroereisis limits subtalar joint pronation through insertion of an implant or material into the sinus tarsi.21, 22, 23 The presence of an implant achieves correction by stimulating the proprioceptive foot receptors, allowing for normal subtalar joint motion,16 while blocking excessive movement. Different shapes and implant designs have been proposed, including bone grafts, polyethylene, silicone, bioresorbable materials, and metallic implants.24 Kellermann et al., 201125 reported better short-term outcomes for pedographic parameters using a screw through the sinus tarsi into the talus. Pavone et al., 201326 reported good results on clinical evaluation, podoscopic examination, and radiologic assessment in 242 patients who were treated using the calcaneo-stop procedure. In a meta-analysis of the literature regarding arthroereisis in children with a flexible flatfoot, Metcalfe and colleagues27 found that the majority of the studies were case reports and retrospective case series (Levels III and IV evidence). Hence, the purpose of this study is to evaluate the effectiveness of this procedure in a prospective manner and to observe if significant improvements in radiographic parameters would result in gait changes, as measured by kinetic and kinematic variables.
Materials and Methods
All children who presented to our institute with painful flatfeet were considered for screening of inclusion and exclusion criteria. A clinical diagnosis of plano-valgus deformity was based on an increased valgus position at rest and during the tip toe standing test as well as restriction of dorsiflexion of the ankle joint in the neutral varus/valgus position. Inclusion criteria for the study were failure with conservative treatment procedures, which included foot exercises and medial heel and sole raise exercises with arch support for a period of one and half years to 2 years. Children were excluded if there were no adequate records for documentation of conservative management and if the flatfoot was secondary to joint hyperlaxity, dystrophy, post-traumatic, neurogenic, or neuromuscular disorders.
A total of 55 children (92 feet) reported they had flatfeet during the study period (Jan 2007–Oct 2010). Nineteen children had no documented evidence of conservative management and were referred for physiotherapy and orthotic management. Sixteen children did not meet the inclusion criteria or met some of the exclusion criteria. The parents of 3 children opted against surgery. Two children were lost to follow-up. Fifteen children (10 males and 5 females) (25 feet) (mean age 12 years and 6 months) fully participated in and completed the study (Table 1). The children were followed for a mean duration of 4 years and 6 months (range of 2 years and 8 months to 6 years and 3 months). The institute ethical committee provided ethical clearance for the study and all the primary caregivers of the children provided informed consent.
Table 1.
Mean age, height and weight of the 15 analysed children.
| Sex | 10 boys and 5 girls |
| Age | 12 years and 6 months |
| Height (in cm) | 127.4 ± 8.4 |
| Weight (in kg) | 33.4 ± 4.6 |
Outcome measures
Passive ankle and subtalar range of motion (ROM) using a 360-degree goniometer
A 360-degree plastic goniometer with 1-degree increments was used. The children were positioned on the bed for long sitting and reclined to approximately 45° with a pillow under the upper part of their lower legs to flex the knee to 20–30°. The angles were measured from the neutral (plantigrade) position (0°). The ankle ROM was measured by placing the stationary arm of the goniometer parallel to the longitudinal axis of the fibula, lining up with the fibula head and moveable arm parallel to the longitudinal axis of the 5th metatarsal. The axis of the goniometer was placed approximately 1.5 cm inferior to the lateral malleolus. The examiner passively pulled the foot towards dorsiflexion and the ROM was recorded by measuring the angle between the movable and stationary arms of the goniometer in degrees.
The subtalar ROM was measured by keeping the axis of the goniometer on the front of the ankle at the midpoint between the medial and lateral malleoli. The stationary arm of the goniometer was placed along the tibial crest and the moveable arm was kept in line with the 2nd metatarsal. The examiner then maximally inverted the heel, and the ROM was recorded by measuring the angle between the movable and stationary arms of the goniometer in degrees.
Visual analogue scale for foot and ankle (VASFA)
The VASFA consists of a 20-question questionnaire based on three different question categories (pain, n = 4 questions; function, n = 11; and other complaints, n = 5). The total value for the entire score, when all 20 questions were answered, ranged between 0 and 100 points. VASFA is a valid and reliable metric.28
The American orthopaedic foot & ankle society score (AOFAS)
The AOFAS is the gold-standard score for the foot and ankle.29 AOFAS is easy to apply and understand, and it can be applied to different kinds of injuries and treatments.30
The Oxford ankle foot questionnaire for children (OxAFQ-C)
The OxAFQ-C31 is a self-report health status measure questionnaire for foot and ankle conditions that children (aged 5–16 years) can complete. The OxAFQ-C has 3 domains (a total of 15 items), Physical (6 items), School and Play (4 items) and Emotional (4 items). The three domain scores are reported separately and there is no total score.
Radiographic indices
The following angles were measured from weight bearing dorsoplantar (DP) and lateral foot radiographs:
Costa-Bartani angle
The angle created by the line formed from the lower point of the 5th metatarsal to the lower point of the calcaneocuboid joint, and the line formed from the lower point of the calcaneocuboid joint to the lower point of the posterior calcaneal tuberosity in the lateral view.
Kite angle
The angle formed between the lines drawn down the axis of the talus and calcaneus measured on the loaded DP foot radiograph.
Calcaneal inclination angle
The angle between the calcaneal inclination axis and the supporting surface on a weight-bearing lateral foot radiograph.
Talar declination angle
The angle between the mid-talar axis and supporting surface on the weight-bearing lateral foot radiograph.
Talo-metatarsal angle (Meary's angle)
The angle between the line drawn from the centres of the longitudinal axes of the talus and the first metatarsal on the weight-bearing lateral foot radiograph.
Kinematic and kinetic analysis
Kinematic and kinetic data were collected with a six-camera motion capture system (BTS Smart- DX system, NY, USA; sampling rate: 200 Hz) and 1 force-plate (sensing area 1800 × 800 mm) during barefoot level walking. The analyse-space for the cameras was calibrated daily on the day of measurements by moving and rotating a rod with reflecting markers in the space that the children had walked. The analysis of foot movement during gait was performed according to the simple Helen Hayes protocol by an independent experienced assessor. The simple Helen Hayes protocol was selected because this protocol requires minimal patient preparation and fewer trajectories to track and edit the studied parameters.32, 33 All children's’ sex, height (in cm) and weight (in kg) were noted. The following anthropometric measures were calculated: anterior superior iliac spine breadth, pelvis depth, leg length, knee diameter and malleolus width. The markers were applied while the patient held an orthostatic position. The Markers were secured at anatomical landmarks that determine embedded axes for segments. For the analysis, 15 numbers of 10-mm lower extremity markers were attached; 2 markers were attached to the anterior superior iliac spines (one right and one left), 1 marker to the second sacral vertebra, 1 marker to each of the lateral femoral condyles, one each on the lateral bar that was securely attached to the thigh using an adaptable strap, 1 marker to each lateral malleolus, one fixed on a rigid bar attached to the side of the shank using an adaptable strap, 1 marker each in the space between the heads of the second and third metatarsals, and one on each heel.
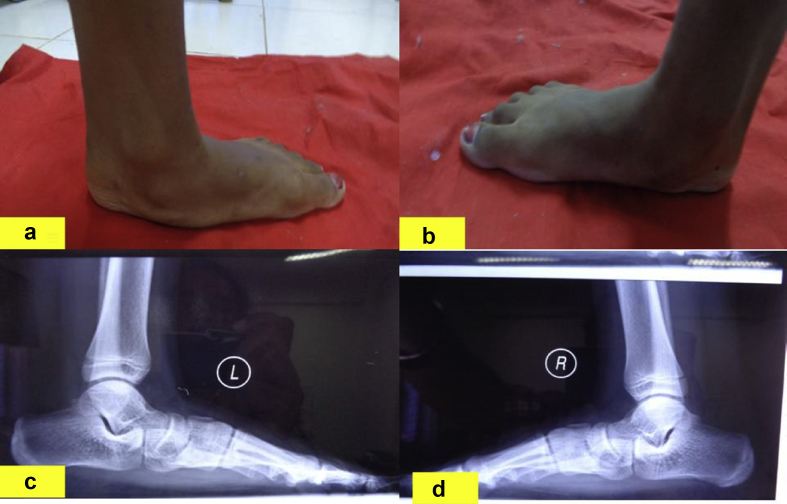
All participants were instructed to perform 2 different tasks. One practice trial was allowed before the actual trial. The children were required to stand in a normal, relaxed upright position, standing in a shoulder-width stance for 3–5 s on the force platform. This ensured that the participants' feet were aligned, which avoided having one foot in a more anterior or posterior position than the other (Figure 1).
Figure 1.
Pre-operative foot of a patient with pes-planovalgus (a and b), Pre-operative X-ray of the same patient with pes-planovalgus (c and d).
The children were instructed to walk along a nine-metre walkway at a comfortable walking speed. The markers placed on the subject were clearly within the field of view of the cameras during the entire acquisition. It was ensured that all children hit the force-plates once with the measured foot during walking. The children were instructed to hit the force-plate spontaneously, and they were not forced to achieve this result. The force plates were used to determine the resulting moments and power in the subject's hip, knee and ankle joints for the measured leg. The protocol requires a single acquisition while the subject performs the standing task and at least one acquisition during a walking sequence. Although both legs of each participant were measured, data from only one leg were analysed (the affected ones for unilateral feet and the more affected one (maximum heel valgus in standing position, as determined by a physiotherapist) in bilateral cases).
Procedure
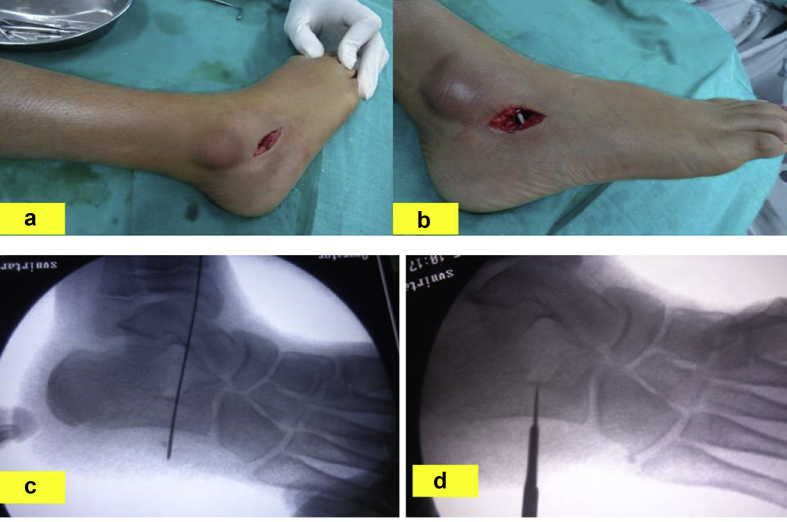
Operative procedure
The children were placed in the supine position under general anaesthesia with a tight tourniquet with the foot was internally rotated. An incision of 2 cm was made under the skin lines on the lateral aspect of the sinus tarsi (Figure 2a). Soft tissue dissection was performed, taking care to avoid the sural nerve. A guidewire was vertically inserted into the calcaneus from the superior to the inferior aspect opposite of the sinus tarsi after reduction of the subtalar eversion under fluoroscopic control (Figure 2c). This was followed by drilling with a 3.2-mm bit and insertion of a 6.5-mm cortical, stainless self-tapping screw (8 mm head) with a length of 30–35 mm (Figure 2d). The surgeon ensured that the screw head impinged against the lateral aspect of the talus, preventing eversion at the subtalar joint. The dorsiflexion of the foot was evaluated with the knee extended after appropriate placement of the screw had been radiographically verified. Concomitant lengthening of the Achilles tendon was performed if dorsiflexion was not possible for at least to 5–10° after surgery. The patients were allowed full weight bearing within 3 days. Three weeks of cast immobilization was applied in patients in whom Achilles tendon lengthening had been performed. The screws were removed an average of 3 years after surgery following growth arrest of the foot.
Figure 2.
a & b: 6.5-mm cortical stainless self-tapping screw in situ; c & d: Calcaneo-stop procedure with a 6.5-mm cortical, stainless self-tapping screw.
Statistical analysis
Data were analysed with SPSS 16.0 (IBM Corp., Chicago, Illinois, USA). The paired Student's t test was used to compare the pre-operative outcome assessed by the physiotherapist under supervision of a surgeon at 6 months before surgery, 3 months before surgery and the day before surgery; also, post-operative clinical, radiographic and gait variables outcomes were measured at 3, 6 and 12 months and then once every year. The p value was set at 0.05.
Results
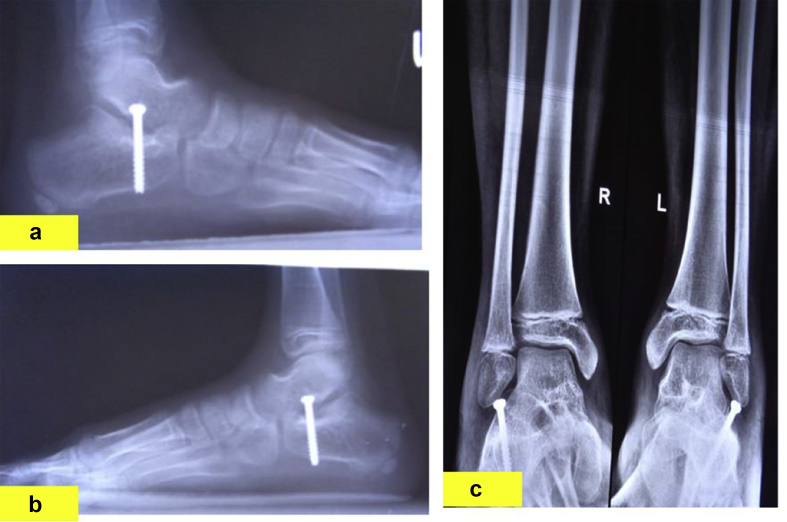
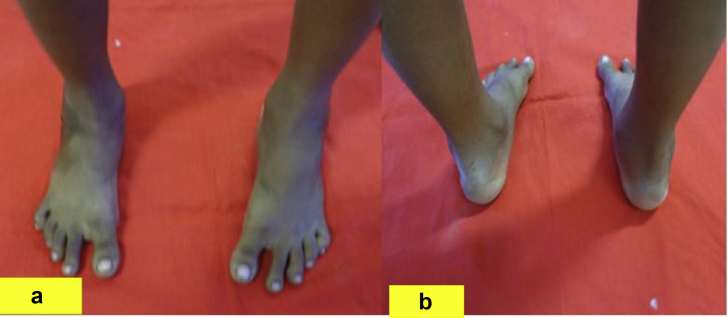
Only those children who complained of severe pain and discomfort in the ankle and foot were considered for surgery. All children reported a satisfactory clinical result; the valgus deformity of the hindfoot was corrected, a longitudinal arch was created and the prominence of the talar head was reduced during weight-bearing activities (Figure 3a,b,c). Children and their caretakers were pleased with the outcomes of surgery (Figure 4a and b). Seven feet (28%) required concomitant lengthening of the Achilles tendon. None of the children required post-operative braces.
Figure 3.
a, b & c Post-operative X-ray of the same patient.
Figure 4.
b: Foot of a participant after surgery.
Table 2 lists the baseline and follow-up scores of all radiographic variables, functional measures and the range of motion investigated in the study. The overall results of the study showed statistically significant differences between the pre-operative and post-operative measurements for each radiographic and functional variable (p < 0.05) (Table 2). Gait analysis showed improvement in the temporal gait parameters (Table 3). However, the analysis showed no statistically significant differences in the kinematic and kinetic variables (p > 0.05) before and after surgery (Table 4). One patient had a complication of a loosened screw that caused pain and restricted motion of the subtalar joint. The implant was removed and arthroereisis was performed using a new screw. Other minor complications included (n = 3) local symptoms at the incision and delayed wound healing as well as contracture of the peroneal muscles (treated with physiotherapy).
Table 2.
Pre-operative and post-operative outcome.
| Outcome measures |
Pre-operative (mean ± SD) |
Post-operative (mean ± SD) |
t value |
p value |
|---|---|---|---|---|
| Radiographic angles | ||||
| Costa Bartani angle | 147.88 (3.12) | 135.48 (2.69) | 16.30 | 0.00 |
| Kite angle | 30.92 (1.42) | 23.07 (0.94) | 22.58 | 0.00 |
| Calcaneal inclination angle | 14.87 (0.56) | 21.60 (1.00) | 39.44 | 0.00 |
| Talar declination angle | 44.32 (2.12) | 24.65 (1.12) | 46.45 | 0.00 |
| Talo-metatarsal angle | 32.70 (0.43) | 18.0 (0.41) | 115.62 | 0.00 |
| Functional scales | ||||
| VASFA | 72.86 (7.33) | 55.70 (7.16) | 7.82 | 0.00 |
| AOFAS | 35.44 (8.31) | 62.68 (8.11) | 19.03 | 0.00 |
| OAFQC | ||||
| Physical | 73.20 (6.71) | 82.79 (5.59) | 12.39 | 0.00 |
| Sports | 70.24 (5.79) | 80.16 (3.84) | 9.51 | 0.00 |
| Emotional | 72.33 (7.26) | 82.64 (7.08) | 5.71 | 0.00 |
| Range of motion | ||||
| Ankle – dorsiflexion | 11.88 (2.22) | 21.64 (2.81) | 12.09 | 0.00 |
| Subtalar-supination | 6.72 (1.74) | 14.48 (2.84) | 11.73 | 0.00 |
Table 3.
Temporal parameters.
| Measures | Pre-operative | Post-operative | p value |
|---|---|---|---|
| Stride time (in seconds) | 0.82 (0.34) | 1.07 (0.6) | 0.00 |
| Stance time (in seconds) | 0.59 (0.02) | 0.67 (0.12) | 0.02 |
| Swing time (in seconds) | 0.3 (0.09) | 0.39 (0.04) | 0.03 |
| Stance phase (as a percentage) | 61.42 (27.11) | 58.35 (4.13) | 0.01 |
| Swing phase (as a percentage) | 26.75 (14.86) | 45.64 (2.18) | 0.00 |
| Double support phase (as a percentage) | 17.56 (16.27) | 19.21 (12.4) | 0.03 |
| Mean velocity (in metres/second) | 0.8 (0.5) | 1.3 (0.1) | 0.00 |
| Mean velocity (in percentage height/seconds) | 49.56 (33.81) | 79.0 (6.72) | 0.00 |
| Cadence (steps/min) | 90.34 (57.2) | 118.65 (20.30) | 0.00 |
Table 4.
Values of the joint rotations obtained on gait analysis.
| Pre-operative | Post-operative | p value | |
|---|---|---|---|
| Values for the joint rotations obtained with gait analysis | |||
| Rotations (in degrees) | |||
| Pelvic obliquity | 4.4 (1) | 4.2 (1.1) | 0.08 |
| Pelvic tilt | 10.9 (0.9) | 12.4 (1.5) | 0.54 |
| Pelvic rotation | 8.3 (1) | 8.4 (1.2) | 0.05 |
| Hip flexion-extension | 10.1 (2.9) | 9.8 (2.8) | 0.1 |
| Knee flexion-extension | 8.0 (2.6) | 8.3 (2.4) | 0.23 |
| Ankle dorsi-plantar flexion | 9.9 (1.5) | 11.3 (1.4) | 0.054 |
| Hip abduction/adduction | −2.8 (1.3) | - 2.1 (0.4) | 0.034 |
| Hip rotation | 6.9 (1.9) | 7.8 (1.6) | 0.00 |
| Foot progression | 2.3 (0.3) | 2.1 (0.2) | 0.051 |
| Values for the joint moments obtained with gait analysis | |||
| Moments (in % BW X H) | |||
| Hip flexion-extension | −1.2 (0.8) | −1 (0.3) | 0.87 |
| Knee flexion-extension | −0.5 (0.03) | −0.5 (0.02) | 1.0 |
| Ankle dorsi-plantar flexion | 2.7 (0.5) | 2.9 (1.1) | 0.06 |
| Hip abduction/adduction | 3.6 (0.2) | 3.5 (0.9) | 0.9 |
| Hip rotation | 0.2 (0.01) | 0.1 (0.08) | 1.0 |
BW = body weight; H = height.
Discussion
The results of the study showed that the calcaneo stop procedure has good outcomes for all measured parameters, except gait analysis. The procedure showed significant positive changes both clinically and radiographically (Figure 3a,b,c).
It has been estimated that 63% of children with flatfeet have functional impairment.34 This impairment has been related to early muscle fatigue and foot-and-ankle-complex instability.35 Numerous treatment options have been recommended, but no single procedure shows adequate correction and resolution of the patient's symptoms.
Arthroereisis procedures are designed to limit subtalar joint motion and improve the weight-bearing position of the foot by placing a motion-blocking implant into the sinus tarsi. The surgical technique adopted in this study was a simple, small lateral incision at the sinus tarsi, as described by Giannini et al., 200136 and Carranza et al., 2000.37 This procedure is less invasive than the combined medial and lateral approaches described by Viladot, 1975.38 The results are similar to those reported by Brancheau et al., 201239 Jerosch et al., 200940 and Pavone et al., 2001.26
The significant improvement in all radiological parameters may be explained by the biomechanics behind the surgery. In flatfoot deformities, the intersection site of the talus and first metatarsal axis mostly occur at the talonavicular joint. If Paley's concept of the centre of rotation of angulation of the deformity is applied to the foot, the calcaneo-stop procedure acts at the centre of rotation of angulation of the deformity.41 The insertion of the implant into the sinus tarsi restricts the motion between the talus and calcaneus, restricting valgus deformity. By orienting the calcaneus more vertically beneath the talus and ankle joint, the subtalar joint axis is altered, correcting the hindfoot alignment and mid and forefoot deformities. When the calcaneus and cuboid are inverted, the talus dorsiflexes and externally rotate and the navicular inverts, confirming the supinatory effects of the subtalar arthroereisis.42 However, the improvement in static radiographic measures did not alter the movement patterns associated with gait.
The results showed changes in the temporal parameters with relatively little change in the collected kinematic and kinetic data before and after surgery. The absence of an effect of procedure on the evaluated kinematic variables may be hypothesized to be because the subtalar joint arthroereisis does not alter the normal closed kinetic chain mechanics.42 The mean velocity and cadence improved to near normal values after the surgery, which may be due to the reduction in pain following surgery. Twomey, 201043 showed that the kinematic differences between the normal arched and low arched feet in children between 9 and 12 years old, using the Heidelberg foot measurement method during walking, were relatively small. Gait analysis is also prone to human errors because the interpretation relies heavily on the skill of the assessors in placing the markers.44 Furthermore, there is uncertainty about the capacity of the Helen Hayes marker set to accurately capture ankle motion.33
The reduction in pain and improvement in function, as observed in this procedure, may be attributed to the neuro proprioceptive45, 46, 47 role of this surgical procedure. The calcaneo-stop procedure is completely extra-articular, resulting in fewer biomechanical stress symptoms.45 Needleman suggested that the improvement seen in functional scores and symptom release after the procedure are biomechanical in nature.6
Although the surgical procedure treated the bio-mechanical aspects, the muscle activities were not studied. Furthermore, recruitment of patients with bilateral and unilateral flatfoot might have influenced the gait variables. Based on prior reports, the muscle tone and stiffness of the tibialis anterior and medial gastrocnemius muscle vary between the bilateral and unilateral flatfoot population.48 The study used one marker on the foot and one on the ankle, which made it difficult to evaluate frontal and transverse plane motion as well as to de-identify multiple foot joints. Additionally, there was no control group for comparison of our outcomes. The potential biases related to measuring the radiographic angles and the biases related to identifying the potentially eligible patients may not be ruled out.
Future studies should consider a comparative gait analysis of flat footed children that is corrected by this surgical approach and normal children by simultaneously evaluating clinical variables, joint kinematics, muscle activations, ground reaction forces and net joint moments to fully evaluate the effectiveness of this procedure.
Conclusions
The calcaneo-stop procedure is a simple, reliable, effective and minimally invasive procedure for treating paediatric flexible flatfoot. The lack of improvement in gait parameters may be attributed to the foot modelling technique used in the study rather than the operating technique. We recommend further studies use a multi-segment kinematic model, such as the Oxford Foot Model.
Conflict of interest
The authors have no conflict of interest to declare.
Authors' contributions
SPD conceived, designed study, provided research materials and wrote the initial draft for the article. PBD conducted research and collected, organized data and provided logistic support and wrote the final draft of the article. GS documented all the data generated from the experiments, helped in the design of the study and final drafting of the article. MCS analyzed and interpreted data. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Arangio G., Reinert K., Salathe E. A biomechanical model of the effect of subtalar arthroereisis on the adult flexible flatfoot. Clin Biomech. 2004;19:847–852. doi: 10.1016/j.clinbiomech.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Feciot C.F. The etiology of developmental flatfoot. Clin Orthop. 1972;85:7–10. doi: 10.1097/00003086-197206000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Nelson S., Haycock D., Little E. Flexible flatfoot treatment with arthroereisis: radiographic improvement and child health survey analysis. J Foot Ankle Surg. 2004;43:144–155. doi: 10.1053/j.jfas.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 4.Pfeiffer M., Kotz R., Ledl T., Hauser G., Sluga M. Prevalence of flat foot in preschool-aged children. Pediatrics. 2006;118:634–639. doi: 10.1542/peds.2005-2126. [DOI] [PubMed] [Google Scholar]
- 5.Harris E.J., Vanore J.V., Thomas J.L., Kravitz S.R., Mendelson S.A., Mendicino R.W., Silvani S.H., Gassen S.C. Diagnosis and treatment of paediatric flatfoot. J Foot Ankle Surg. 2004;43:341–372. doi: 10.1053/j.jfas.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 6.Needleman R.L. Current topic review: subtalar arthroereisiss for the correction of flexible flatfoot. Foot Ankle Intl. 2005;26:336–346. doi: 10.1177/107110070502600411. [DOI] [PubMed] [Google Scholar]
- 7.Root M.L., Orien W.P., Weed J.H. Normal and abnormal function of the foot. Clin Biomech. 1977:295–339. [Google Scholar]
- 8.Giannini S. Operative treatment of the flatfoot: why and how. Foot Ankle Int. 1998;19:52–58. doi: 10.1177/107110079801900111. [DOI] [PubMed] [Google Scholar]
- 9.Giannini S., Ceccarelli F. The flexible flat foot. Foot Ankle Clin. 1998;3:573–592. [Google Scholar]
- 10.Lee S.Y. Daegu University Rehabilitation Science Graduate School, a Master’s degree; 2002. The effect of on CTA and Q-angle with the different position of the foot in the standing status. [Google Scholar]
- 11.Wenger D.R., Leach J. Foot deformities in infant and children. Pediatr Clin North Am. 1986;33:1411–1427. doi: 10.1016/s0031-3955(16)36151-x. [DOI] [PubMed] [Google Scholar]
- 12.Bettmann E. The treatment of flat-foot by means of exercise. J Bone Joint Surg Am. 1937;19:821–825. [Google Scholar]
- 13.Cappello T., Song K.M. Determining treatment of flatfeet in children. Curr Opinb Pediatr. 1998;10:77–81. doi: 10.1097/00008480-199802000-00016. [DOI] [PubMed] [Google Scholar]
- 14.Cohen-Sobel E., Giorgini R., Velez Z. Combined technique for surgical correction of pediatric severe flexible flatfoot. J Foot Ankle Surg. 1995;34:183–194. doi: 10.1016/S1067-2516(09)80043-4. [DOI] [PubMed] [Google Scholar]
- 15.Roye D.P., Jr., Raimondo R.A. Surgical treatment of the child's and adolescent's flexible flatfoot. Clin Podiatr Med Surg. 2000;17:515–530. [PubMed] [Google Scholar]
- 16.Mosca V.S. Flexible flatfoot in children and adolescents. J Child Orthop. 2010;4:107–121. doi: 10.1007/s11832-010-0239-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Roth S., Sestan B., Tudor A., Ostojic Z., Sasso A., Durbesic A. Minimal invasive calcaneo-stop method for idiopathic flexible per planovalgus in children. Foot Ankle Int. 2007;28(9):991–995. doi: 10.3113/FAI.2007.0991. [DOI] [PubMed] [Google Scholar]
- 18.Staheli L.T. Planovalgus foot deformity. Current status. J Am Podiatr Med Assoc. 1999;89:94–99. doi: 10.7547/87507315-89-2-94. [DOI] [PubMed] [Google Scholar]
- 19.Crego C.H., Jr., Scheer G.E. A two-stage stabilization procedure for correction of calcaneocavus. J Bone Joint Surg. 1956;38A:1247–1253. [PubMed] [Google Scholar]
- 20.Sekiya J.K., Saltzman C.L. Long term follow-up of medial column fusion and tibialis anterior transposition for adolescent flatfoot deformity. Iowa Orthop J. 1997;17:121–129. [PMC free article] [PubMed] [Google Scholar]
- 21.Smith S.D., Millar E.A. Arthroereisis by means of a subtalar polyethylene peg implant for correction of hindfoot pronation in children. Clin Orthop. 1983;181:15–23. [PubMed] [Google Scholar]
- 22.Forg P., Feldman K., Flake E., Green D.R. Flake-Austin modification of the STA-Peg arthroereisis: a retrospective study. J Am Podiatr Med Assoc. 2001;91:394–405. doi: 10.7547/87507315-91-8-394. [DOI] [PubMed] [Google Scholar]
- 23.Maxwell J.R., Carro A., Sun C. Use of the Maxwell-Brancheau arthroereisis implant for the correction of posterior tibial tendon dysfunction. Clin Podiatr Med Surg. 1999;16:479–489. [PubMed] [Google Scholar]
- 24.Cook E.A., Cook J.J., Basile P. Identifying risk factors in subtalar arthroereisis explantation: a propensity-matched analysis. J Foot Ankle Surg. 2011;50:395–401. doi: 10.1053/j.jfas.2011.03.019. [DOI] [PubMed] [Google Scholar]
- 25.Kellermann P., Roth S., Gion K., Boda K., Tóth K. Calcaneo-stop procedure for paediatric flexible flatfoot. Arch Orthop Trauma Surg. 2011;131(10):1363–1367. doi: 10.1007/s00402-011-1316-3. [DOI] [PubMed] [Google Scholar]
- 26.Pavone V., Costarella L., Testa G., Conte G., Riccioli M., Sessa G. Calcaneo-stop procedure in the treatment of the juvenile symptomatic flatfoot. J Foot Ankle Surg. 2013;52(4):444–447. doi: 10.1053/j.jfas.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 27.Metcalfe S.A., Bowling F.L., Reeves N.D. Subtalar joint arthroereisis in the management of pediatric flexible flatfoot: a critical review of the literature. Foot Ankle Int. 2011;32(12):1127–1139. doi: 10.3113/FAI.2011.1127. [DOI] [PubMed] [Google Scholar]
- 28.Richter M., Zech S., Geerling J., Frink M., Knobloch K., Krettek C. A new foot and ankle outcome score: questionnaire based, subjective, Visual- Analogue-Scale, validated and computerized. Foot Ankle Surg. 2006;12:191–199. [Google Scholar]
- 29.SooHoo N.F., Shuler M., Fleming L.L. Evaluation of the validity of the AOFAS clinical rating systems by correlation to the SF-36. Foot Ankle Int. 2003;24(1):50–55. doi: 10.1177/107110070302400108. [DOI] [PubMed] [Google Scholar]
- 30.Kitaoka H.B., Alexander I.J., Adelaar R.S., Nunley J.A., Myerson M.S., Sanders M. Clinical rating systems for the ankle-hindfoot, mid-foot, hallux and lesser toes. Foot Ankle Int. 1994;15:135–149. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 31.Morris C., Doll H., Davies N., Wainwright A., Theologis T., Willett K., Fitzpatrick R. The Oxford Ankle Foot Questionnaire for children: responsiveness and longitudinal validity. Qual Life Res. 2009;18:1367–1376. doi: 10.1007/s11136-009-9550-7. [DOI] [PubMed] [Google Scholar]
- 32.Kadaba Ramakrishnan H.K. Wootten ME, Gainey J, Gorton G, Cochran GVB. Repeatability of kinematic, kinetic and electromyographic data in normal adult gait. J Orthop Res. 1989;7(6):849–860. doi: 10.1002/jor.1100070611. [DOI] [PubMed] [Google Scholar]
- 33.Kadaba M.P., Ramakrishnan H.K., Wootten M.E. 1990. “Measurement of lower extremity kinematics during level walking”. J Orthop Res. 1990;8(3):383–392. doi: 10.1002/jor.1100080310. [DOI] [PubMed] [Google Scholar]
- 34.Benedetti M.G., Ceccarelli F., Berti L., Luciani D., Catani F., Boschi M., Giannini S. Diagnosis of flexible flatfoot in children: a systematic clinical approach. Orthopedics. 2011;34(2):94. doi: 10.3928/01477447-20101221-04. [DOI] [PubMed] [Google Scholar]
- 35.Franco A.H. Pes cavus and pes planus. Analyses and treatment. Phys Ther. 1987;67(5):688–694. doi: 10.1093/ptj/67.5.688. [DOI] [PubMed] [Google Scholar]
- 36.Giannini S., Ceccarelli F., Benedetti M.G., Catani F., Faldini C. Surgical treatment of flexible flatfoot in children a four-year follow-up study. J Bone Joint Surg. 2001;83A(Suppl. 22):73–79. doi: 10.2106/00004623-200100022-00003. [DOI] [PubMed] [Google Scholar]
- 37.Carranza A., Gimeno V., Gomez J.A., Gutierrez M. Giannini's prosthesis in the treatment of juvenile flatfoot. J Foot Ankle Surg. 2000;6:11–17. [Google Scholar]
- 38.Viladot A. Nouvelle technique pour le traitement chirugical du pied-platvalgus essential. Cah Chirugie. 1975;16:8–10. [Google Scholar]
- 39.Brancheau S.P., Walker K.M., Northcutt D.R. An analysis of outcomes after use of the Maxwell-Brancheau arthroereisis implant. J Foot Ankle Surg. 2012;51:3–8. doi: 10.1053/j.jfas.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 40.Jerosch J., Schunck J., Abdel-Aziz H. The stop screw technique—a simple and reliable method in treating flexible flatfoot in children. Foot Ankle Surg. 2009;15:174–178. doi: 10.1016/j.fas.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 41.Paley D. Springer-Verlag; Berlin: 2002. Principles of deformity correction. [Google Scholar]
- 42.Christensen J.C., Campbell N., Dinucci K. Closed kinetic chain tarsal mechanics of subtalar joint arthroereisis. J Am Pod Med Assoc. 1996;86:467–473. doi: 10.7547/87507315-86-10-467. [DOI] [PubMed] [Google Scholar]
- 43.Twomey D., McIntosh A.S., Simon J., Lowe K., Wolf S.I. Kinematic differences between normal and low arched feet in children using the Heidelberg foot measurement method. Gait Posture. 2010;32(1):1–5. doi: 10.1016/j.gaitpost.2010.01.021. [DOI] [PubMed] [Google Scholar]
- 44.McGinley J.L., Baker R., Wolfe R., Morris M.E. The reliability of three-dimensional kinematic gait measurements: a systematic review. Gait Posture. 2009 Apr;29(3):360–369. doi: 10.1016/j.gaitpost.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 45.Kwon J., Myerson M. Management of the flexible flat foot in the child: a focus on the use of osteotomies for correction. Foot Ankle Clin N Am. 2010;15:309–322. doi: 10.1016/j.fcl.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 46.Pisani G. About the pathogenesis of the so-called adult acquired pes planus. Foot Ankle Surg. 2010;16:1–2. doi: 10.1016/j.fas.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 47.Magnan B., Baldrighi C., Papadia D. Flatfeet: comparison of surgical techniques. Result of study group into retrograde endorthesis with calcaneus-stop. Ital J Pediatr Orthop. 1997;13:28–33. [Google Scholar]
- 48.Um G.-M., Wang J.-S., Park S.-E. An analysis on muscle tone of lower limb muscles on flexible flat foot. J Phys Ther Sci. 2015;27(10):3089–3092. doi: 10.1589/jpts.27.3089. [DOI] [PMC free article] [PubMed] [Google Scholar]