Abstract
Objectives
Complementary and alternative medicine (CAM) includes various therapies that are not recognized by modern scientific medicine. However, in chronic diseases, such as diabetes, the use of CAM is quite common. Data on the use of CAM are needed to understand the health behaviour of individuals and to identify possible side effects. In this study, we aimed to obtain data on the pattern of CAM use in a population in eastern India.
Methods
This was a hospital-based quantitative cross-sectional survey involving adult patients. The study was conducted simultaneously in an urban university hospital and a rural hospital. Data on the demographic characteristics of the participants and their reasons for CAM use were collected.
Results
In total, 442 participants were included in the study, and among them, approximately 50% were aged 31–50 years. Moreover, around 26.7% of the participants belonged to the tribal population, 36.7% used CAM within the last year, and 57.2% used CAM in their lifetime. Body ache and dyspepsia were the most common indications for CAM use among the participants. The pattern of CAM use was significantly higher in the tribal population (p < 0.001). On logistic regression analysis, being part of the tribal population was the only demographic factor related with CAM use within the last year (odds ratio [OR]: 3.205) or with lifetime CAM use (OR: 2.885).
Conclusion
The use of CAM for certain symptoms was quite significant in the study population, particularly in the tribal population.
Keywords: Complementary and alternative medicine, Herbal therapy, Prevalence, Tribal
الملخص
أهداف البحث
يشمل الطب التكميلي والبديل” العلاجات” المختلفة التي لم يتم التعرف عليها عند الطب العلمي الحديث. ولكن استخدام الطب التكميلي والبديل معروف إلى حد ما في الأمراض المزمنة مثل السكري. هناك حاجة للبيانات عن استخدام الطب التكميلي والبديل، وذلك لفهم السلوك الصحي للناس وأيضا، لتوقع الآثار الجانبية المحتملة. في هذه الدراسة، نهدف إلى إنتاج بيانات عن نمط استخدام الطب التكميلي والبديل في عينة من سكان الهند الشرقية.
طرق البحث
أجري هذا المسح – المقطعي الكمي بالمستشفى على مرضى بالغين. وقد أجريت هذه الدراسة في وقت واحد في المستشفى الجامعي الحضري والمستشفى الريفي. وتم جمع البيانات عن الخصائص الديموغرافية للأشخاص ودوافعهم لاستخدام الطب التكميلي والبديل، إن وجدت.
النتائج
كان لدينا ٤٤٢ شخصا، وينتمي ٥٠٪ إلى الفئة العمرية ٣١-٥٠ عاما. من بينهم ٢٦.٧٪ ينتمون إلى السكان القبليين. ومن بين الأشخاص في الدراسة، ٣٦.٧٪ استخدموا الطب التكميلي والبديل خلال العام الماضي و٥٧.٢٪ من الأشخاص استخدموا الطب التكميلي والبديل في حياتهم من قبل. كانت آلام الجسم وعسر الهضم أكثر الأعراض شيوعا لاستخدام الطب التكميلي والبديل. الميل لاستخدام الطب التكميلي والبديل كان أعلى كثيرا بين السكان القبليين، في تحليل الانحدار اللوجستي أيضا، وكان الانتماء إلى السكان القبليين هو العامل الديموغرافي الوحيد المرتبط باستخدام الطب التكميلي والبديل في العام الماضي أو استخدام الطب التكميلي والبديل في السابق.
الاستنتاجات
استخدام الطب التكميلي والبديل لأعراض معينة كان كبيرا جدا في البحث السكاني، خصوصا بين السكان القبليين.
الكلمات المفتاحية: قبلي, الطب التكميلي والبديل, العلاج بالأعشاب, انتشار
Introduction
Complementary and alternative medicine (CAM) encompasses modern or rejuvenated ancient practises that are claimed to have preventive or curative medical effects.1 Generally, these practices are not recognised in medical science. Moreover, they are not based on evidence or sound scientific hypotheses.1 CAM includes various therapies such as homeopathy, massage-based therapy, naturopathy, diet therapy, and other similar practices. For the purpose of this study, any form of medical therapy that is not included in modern scientific guidelines or not recommended by major scientific associations has been classified under CAM.
The use of CAM significantly increased worldwide within the past century. For example, in the USA, a national health survey showed a considerable increase in the popularity of different CAM therapies, such as acupuncture and naturopathy, over the last few years.1 This was observed in different age groups among almost all social strata. In the UK, a national health survey also showed quite high levels of CAM use.2 In the survey conducted in the UK, individuals often used prescription drugs along with CAM.2 Factors, such as poor mental health and lack of perceived social support, were related with CAM use.
The use of CAM is also quite high in low- and middle-income countries in Asia. A recent review found that almost half of the pregnant women in these countries used herbal medicines that had unknown or potentially harmful side effects.3 However, the use of alternative therapies is often not documented, and their effects remain unknown. Thus, the study on the pattern of CAM use in a population is important for identifying their possible side effects and drug interactions. Physicians rarely discuss or ask about the use of such alternative therapies during consultations. Thus, this lack of enquiry keeps its use unknown to physicians and prevents an open discussion about their relevance in modern therapy.
Data from the different parts of India have shown that the use of CAM is quite high.4 For example, a survey among patients with cancer in Delhi, the capital of India, found that more than 30% of individuals used some form of CAM.4 Such parallel use of CAM is also observed in individuals with other major illnesses such as diabetes and asthma. The biological nature and efficacy of these therapies are often unknown. Moreover, data on the use of CAM are not available from all parts of the country. In a vast country, such as India, with different cultural practices and religious beliefs, the pattern of CAM use is likely to vary within the region. In specific populations, such as tribal and other ethnic minorities, that are known to use natural remedies, data on CAM use are often limited.
Thus, loco-regional data on CAM use is needed to identify the health behaviour of individuals. These data can be used to identify the vulnerable section of the population who are prone to use ineffective CAM therapies and to plan for local health education measures. For the ethnic minority groups who often have limited access to healthcare, such data are even more important for understanding their healthcare-seeking behaviour and beliefs about natural remedies.
In this study, we aimed to obtain data on the pattern of CAM use in a population in eastern India, including tribal and ethnic minority groups. For the purposes of this study, the term tribal is used to denote indigenous communities recognized by the law of India.5 The members of such communities are provided with government certificates and identity documents indicating that they are scheduled tribes.
Materials and Methods
This study was carried out at a tertiary-care urban hospital and rural hospital in eastern India. The study was conducted for 2 months between 1 October 2017 and 30 November 2017. This was a hospital-based cross-sectional survey involving adult (aged >12 years) patients attending the outdoors. Informed consent was obtained from participants older than 16 years. For those aged between 12 and 16 years, informed consent was obtained from a parent or person with parental responsibility, which is similar to the international protocol for including minors in a medical study. The study protocol was approved by the institutional ethics committee of the tertiary-care hospital. The local health administrator of the rural hospital, who is the block medical officer of health, also approved the study. The rural hospital is located in a region with a considerable population of tribal communities.6
The prevalence rate of CAM use in the general population in previous studies ranged from 30% to 40%. Considering this as a reference for 80% power, 5% precision, and 95% confidence interval (CI), the projected sample size was 370,7 and it was increased by 20% to account for some data loss and faulty data. Thus, the final proposed sample size was 440.
This was a questionnaire-based survey. The questionnaire was structured and modelled based on similar surveys conducted earlier in the country.8 It was pilot tested on a group of 30 volunteers where validity and reliability were established (Cronbach's alpha: 0.79). The first part of the questionnaire involved the demographic data of the participants, such as age, gender, educational level, occupation, and whether they belonged to any ethnic minority. The second part contained questions about the use of CAM, influencing factors for the use of CAM, and their choice of therapy for any illness. In the second part, data on CAM use were recorded as a binary response (yes/no). Questions, such as those for the influencing factor on the use of CAM, were open ended. After the ethics approval, the interviewers were trained to conduct the survey. Informed consent was obtained before each interview. Conversation with the study participants was in their native language. In case the interviewer was unfamiliar with the native language of the participant, help was sought from any native language speaker who was not related to or not known to the participant.
The participants were randomly selected from the patients attending medicine and general outdoors of the two hospitals. A total of 629 participants were included in the study. However, some of them opted out after the explanation about the survey protocol. Anyone associated with the business of alternative medicine, such as practitioners, shopkeepers, or complementary medicine manufacturing unit workers, were excluded from the study. In addition, anyone with dementia (based on patient history or results of the abbreviated mental test at the clinic) or speech problems was excluded.
Data were entered in the Microsoft excel worksheet and analysed using the SPSS software version 16. The chi-square test was used to analyse categorical data. A P value of <0.05 was considered significant. Percentage and proportions are presented with their 95% CIs. A logistic regression analysis was conducted where CAM was used as a dependent binary variable (yes/no).
Results
In this study, after applying the proper exclusion criteria and permitting participants to opt out from the study, a total of 442 patients were included. Thus, the response rate was 70.3%. The mean age of the patients was 40.7 ± 13.7 years. Most of the participants (49.3%) were aged 31–50 years. Among the study participants, 231 (52.3%) were men. Out of 442 patients, 118 (26.7%) belonged to some tribal or other ethnic minority groups. A total of 347 (78.5%) patients had residence in village areas, whereas 95 lived in cities. These and other demographic characteristics are shown in Table 1.
Table 1.
Demographic characteristics of the study participants.
| Parameter | Number (percentage) | |
|---|---|---|
| Age (years) | ≤20 | 32 (7.2) |
| 21–30 | 92 (20.8) | |
| 31–40 | 110 (24.9) | |
| 41–50 | 108 (24.4) | |
| 51–60 | 69 (15.6) | |
| >60 | 31 (7.1) | |
| Sex | Male | 231 (52.3) |
| Female | 211 (47.7) | |
| Belonging to a tribal group | Yes | 118 (26.7) |
| No | 324 (73.3) | |
| Residence | Village | 347 (78.5) |
| City | 95 (21.5) | |
| Occupation | Housewife/home manager | 169 (38.2) |
| Farmer | 80 (18.1) | |
| Labourer | 62 (14) | |
| Business man/woman | 32 (7.2) | |
| Student | 32 (7.2) | |
| Office worker | 18 (4.1) | |
| Others | 49 (11.2) | |
| Educational level | Illiterate or primary | 366 (82.8) |
| Secondary | 44 (10) | |
| College or higher | 32 (7.2) | |
Among our study participants, 162 (36.7%; 95% CI: 32.1–41.3%) used CAM within the last year and 253 (57.2%; 95% CI: 52.5–61.9%) used CAM at least once in their lifetime. Out of 442 participants, 165 (37.3%; 95% CI: 32.8–42%) stated that CAM was their first choice of treatment for any illness. Out of the 253 individuals who used CAM in their lifetime, 110 (43.5%) used it according to their own will and 51 (20.2%) used it based on the recommendation of their friends. Of these participants, 83 used CAM based on the advice by a family member. Among those (n = 253) who used CAM, only 85 (33.6%; 95% CI: 27.8–39.8%) had some perceived benefits after using CAM. Among the participants who used CAM, 26 (10.3%) experienced side effects.
The symptoms or diseases for which CAM was used varied. Out of the 253 participants who used CAM in their lifetime, the following conditions are the most common reasons for CAM use: body ache (n = 44), dyspepsia (n = 24), and abdominal pain (n = 15). Other common symptoms included respiratory tract infection (n = 18), weakness (n = 12), and headache (n = 10).
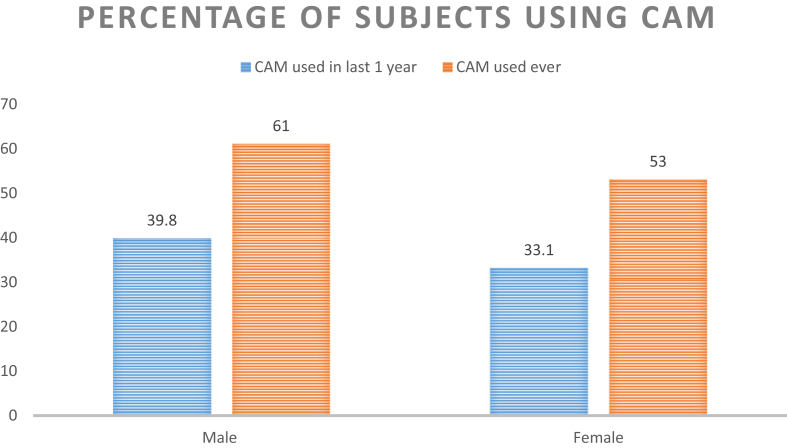
Figure 1 shows the use of CAM according to gender. Male participants were more likely to use CAM compared to female participants (61% lifetime use in male participants vs 53.1% in female participants). However, the difference was not statistically significant (p = 0.102; 2-sided chi-square test). Among the male participants, 46.8% had used CAM by themselves. Meanwhile, among female participants, 39.3% had used it according to their own will, and 41.1% had used it based on the recommendation of a family member.
Figure 1.
Bar diagram showing the use of CAM among the study participants according to sex.
Considering the tribal and ethnic minority groups (n = 118) in our study, 65 (55.1%; 95% CI: 45.7–64.3%) participants had used CAM within the last year, and 87 (73.7%; 95% CI: 64.8–81.4%) had used CAM at least once in their lifetime. By contrast, 30% of the non-tribal participants had used CAM within the last year, and 51.2% had used CAM in their lifetime. The difference in CAM use was found to be statistically significant (p < 0.001 for CAM use within the last year; p < 0.001 for CAM use in their lifetime: both by 2-tailed chi-square test). CAM is the first choice of treatment in 45 (38.1%) and 120 (37%) participants from the tribal and ethnic minority groups as well as from the non-tribal population, respectively.
Considering the educational qualification of the study participants in the group (n = 366) with no or only primary-level education, 130 (35.5%) had used CAM within the last year, whereas, in those with higher education (n = 76), 42.1% had used CAM within the last year (p = 0.296; chi-square test). With regard to the lifetime use of CAM, the results were similar (56.3% vs. 61.8%; p = 0.445). Educational level was not a statistically significant determinant of CAM use, although the participants with higher education level used it more often.
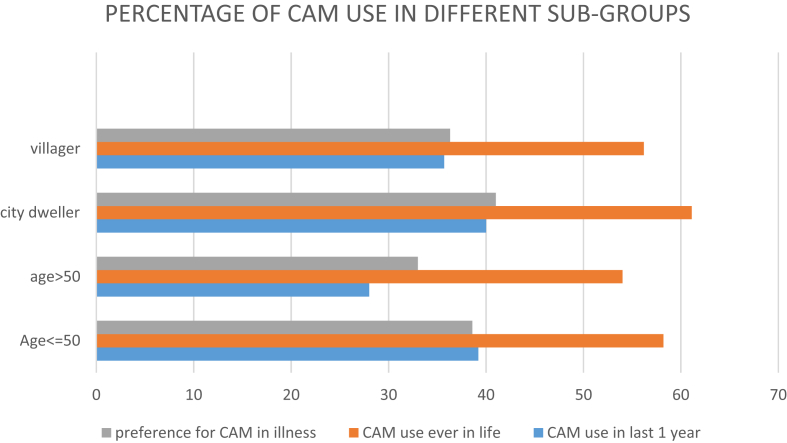
Figure 2 shows the use of CAM according to the demographic characteristics of the participants. Participants who were ≤50 years of age were more likely to use CAM within the last year compared to those over 50 years (39.2% vs 28%; p = 0.04). However, the preference for CAM for any illness was similar in both age groups. In all the subgroups shown in Figure 2, the proportion of participants who had used CAM at least once in their lifetime was significantly higher than that in participants who used CAM within the year (p = 0.0045 for village dwellers; p = 0.0047 for city dwellers; p = 0.0002 for those aged >50 years; p = 0.01 for those aged ≤50 years; chi-square test).
Figure 2.
Horizontal bar diagram showing the use of CAM according to demographic features.
Logistic regression analysis was carried out with the use of CAM (yes/no) as a dependent variable. It was performed twice, once with CAM use within the last year as the dependent variable and second with CAM use at least once in their lifetime as the dependent variable. Being part of the tribal population was a factor favouring the use of CAM within the last year (OR: 3.205; 95% CI: 2.039–5.039) and also the use of CAM in their lifetime (OR: 2.885; 95% CI: 1.791–4.648). For other variables, such as gender, place of residence, and education level, the OR was not significant.
Discussion
In our cross-sectional survey, more than 1 in 3 individuals from the general population had used CAM within the last year. For the tribal and ethnic minority population, the use of CAM was significantly higher, with more than 7 out of every 10 individuals using CAM in their lifetime.
In India, CAM is used both at institutional and social levels. There are registered health facilities in India that dispense CAM drugs. A survey by the government of India in 2014 found that around 7% of the population (both urban and rural) received CAM treatment from these recognized institutions within the last 15 days prior to the survey.9 However, the pattern of use was not similar throughout the country. Its use was quite low in areas, such Andhra Pradesh, and quite high in regions, including Mizoram and Chattisgarh.9 While this survey is only limited to healthcare utilization within the last 15 days, it does provide an idea that a significant number of individuals regularly use CAM. One of the benefits of CAM is the fact that is it more cost-effective than technology-based modern therapies. However, proper economic evaluations of this benefit are still limited.10 Moreover, this survey in India has shown that the costs of CAM therapies are not significantly different from modern medicines. In urban areas, the average cost per treatment episode of CAM was Rupees 378, whereas that of modern medicine was Rupees 454.
The recommendation for the rate of non-institutional use of CAM by local practitioners are significantly higher. A survey in North India has found that 46% of individuals with Parkinson's disease (PD) used CAM along with their prescription drugs.11 In another study in Singapore, the use of CAM among patients with PD was also high. The prevalence of CAM use increased with the duration of the disease, with 75% of patients of more than 10 years of chronic disease using CAM.12 In individuals with such non-curable chronic disorders, the use of CAM is often high. For example, a study in Kerala, India, has found that approximately 40% of patients with diabetes use CAM regularly, of which 30% used it along with modern medicines.13 In our survey, all the patients who were using CAM also used modern medicines. Such polypharmacy of the different systems of therapy may cause drug interactions and other side effects.
The use of CAM and traditional systems of therapy is quite common among indigenous populations. A survey among Garo and Khasi tribes of India has found that 34% used tribal medicine for minor ailments and 23% also used it for major illnesses.14 Approximately 87% of individuals from those communities believed in the efficacy of traditional medicine.14 The use of other forms of CAM was also quite high in this population. We found that 74% of the participants from the tribal population had used CAM at least once in their lifetime. In a study from Pakistan, several women from the Pashtun tribe used various plants for different gynaecological ailments.15
The domain of CAM is heterogeneous. There are various so-called therapies, such as diet-based therapies, which are only marketing strategies and are easier to debunk. However, therapies, such as homeopathy, are deep entrenched in the mentality of the population, and despite numerous negative evidences, individuals are difficult to convince that these therapies are not effective. A systematic review in 2017 has found that a considerable proportion (up to 10%) of the population from the different parts of the world still use homeopathy regularly, and the trend has not changed over the last two decades.16 However, as scientific evidence has repeatedly shown, homeopathy is not effective in treating any illness, and its continued use just delays the effects of appropriate therapies.17 Thus, alternative medicines, such as homeopathy, has a traditionally high popularity, despite scientific evidence on the contrary. A recent research has shown that factors, such as endorsement by notable social leaders and celebrities, perceived lack of side effects, and support from the government in legalizing homeopathic treatment, are associated with the social acceptance of this therapy in some countries, including India.18
For traditional medicine, including traditional medicines for indigenous people, the argument is more complex. The United Nations has clearly stated that indigenous people from any country has the right to use their own traditional medicines.19 This is not a question of scientific efficacy but rather a preservation of indigenous cultures. Moreover, the WHO has declared that indigenous people must have culturally appropriate healthcare.14 Hence, the imposition of modern medicine on ethnic minority groups with the exclusion of their traditional therapies is not appropriate. However, all traditional therapies are not effective for the diseases for which they are used. Once data on the prevalence of CAM use among different population groups are available, a scientific study of the different forms of medicine must be conducted to identify their efficacy. This can help in formulating a plan where effective traditional medicines are combined with evidence-based modern medicines.
The widespread use of CAM is likely to result in side effects and drug interactions. The ingredients in these medicines are of variable concentration, and their effects are often not predictable.20 In India, herbal remedies are often used, and there are several reports on herbal-drug interactions.21 Thus, physicians must discuss such untoward reactions with their patients if there is a history of polypharmacy with the different systems of therapy.
Medical pluralism, which is the parallel use of the different systems of therapy, is a common practice worldwide.14 Surveys, such as the present survey, will help identify the actual extent of this phenomenon. Moreover, this will help physicians in predicting possible drug interactions and other side effects as well as policy makers understand the extent of reliance (particularly in indigenous populations) on traditional medicines. Thus, a culturally appropriate health policy can be established.
Conclusion
Physicians should be aware of the possibility of medical pluralism in their patients. In several cases, such alternative therapies are part of the indigenous culture. Thus, an open discussion with patients in a culturally sensitive manner is essential to formulate an effective treatment plan. In a diverse country, such as India, the loco-regional patterns of CAM use must be investigated to understand the behaviour of individuals toward illness.
Source of funding
None.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
Taken.
Authors' contributions
RP and KS collected the data; JR, RP, and DC wrote the manuscript. DC and RP were responsible for the statistical calculations. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgement
We would like to thank the Kolkata Medical College and Hospital and BMOH, Salboni.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Barnes P.A., Bloom B. National Health Statistics Reports. U.S Department of Health & Human Services; Atlanta: 2008. Complementary and alternative medicine use among adults and children; United States, 2007. [PubMed] [Google Scholar]
- 2.Hunt K.J., Coelho H.F., Wider B., Perry R., Hung S.K., Terry R. Complementary and alternative medicine use in England: results from a national survey. Int J Clin Pract. 2010;64:1496–1502. doi: 10.1111/j.1742-1241.2010.02484.x. [DOI] [PubMed] [Google Scholar]
- 3.Ahmed M., Hwang J.H., Choi S., Han D. Safety classification of herbal medicines used among pregnant women in Asian countries: a systematic review. BMC Complement Altern Med. 2017;17:489. doi: 10.1186/s12906-017-1995-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Broom A., Nayar K.R., Tovey P., Shirali R., Thakur R., Seth T. Indian cancer patients' use of traditional, complementary and alternative medicine (TCAM) and delays in presentation to hospital. Oman Med J. 2009;24:99–102. doi: 10.5001/omj.2009.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.NCST . Government of India; New Delhi: 2005. National Commission for Scheduled Tribes [Online]http://ncst.nic.in/index.asp?langid=1 [Cited 2017 Nov 15]. Available from: [Google Scholar]
- 6.Salboni (community development block) [Internet]. [Cited 2017 Dec 3]. Available from https://ipfs.io/ipfs/QmXoypizjW3WknFiJnKLwHCnL72vedxjQkDDP1mXWo6uco/wiki/Salboni_(community_development_block).html.
- 7.Pourhoseingholi M.A., Vahedi M., Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6:14–17. [PMC free article] [PubMed] [Google Scholar]
- 8.Roy V., Gupta M., Ghosh R.K. Perception, attitude and usage of complementary and alternative medicine among doctors and patients in a tertiary care hospital in India. Indian J Pharmacol. 2015;47:137–142. doi: 10.4103/0253-7613.153418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rudra S., Kalra A., Kumar A., Joe W. Utilization of alternative systems of medicine as health care services in India: evidence on AYUSH care from NSS. PLoS One. 2014;12 doi: 10.1371/journal.pone.0176916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Herman P.M., Craig B.M., Caspi O. Is complementary and alternative medicine (CAM) cost-effective? a systematic review. BMC Complement Altern Med. 2005;5:11. doi: 10.1186/1472-6882-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pandit A.K., Vibha D., Srivastava A.K., Shukla G., Goyal V., Behari M. Complementary and alternative medicine in Indian Parkinson's disease patients. J Tradit Complement Med. 2016;6:377–382. doi: 10.1016/j.jtcme.2015.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tan L.C.S., Lau P.N., Jamora R.D.G., Chan E.S.Y. Use of complementary therapies in patients with Parkinson's disease in Singapore. Mov Disord Off J Mov Disord Soc. 2006;21:86–89. doi: 10.1002/mds.20662. [DOI] [PubMed] [Google Scholar]
- 13.Vishnu N., Mini G.K., Thankappan K.R. Complementary and alternative medicine use by diabetes patients in Kerala, India. Global Health Epidemiol Genom. 2017;2:e6. doi: 10.1017/gheg.2017.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Albert S., Nongrum M., Webb E.L., Porter J.D.H., Kharkongor G.C. Medical pluralism among indigenous peoples in northeast India - implications for health policy. Trop Med Int Health. 2015;7:952–960. doi: 10.1111/tmi.12499. [DOI] [PubMed] [Google Scholar]
- 15.Adnan M. Ethnogynaecological assessment of medicinal plants in Pashtun's tribal society. BioMed Res Int. 2015;2015 doi: 10.1155/2015/196475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Relton C., Cooper K., Viksveen P., Fibert P., Thomas K. Prevalence of homeopathy use by the general population worldwide: a systematic review. Homeopathy. 2017;106:69–78. doi: 10.1016/j.homp.2017.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Science and Technology Committee - Fourth Report . House of Commons UK; London: 2010. Evidence Check 2: Homeopathy. [Cited 2017 Dec 3]. Available online from https://publications.parliament.uk/pa/cm200910/cmselect/cmsctech/45/4502.htm. [Google Scholar]
- 18.Dekkers J.T.H. University of Utrecht; The UK, India and The Netherlands: 2009. What about Homeopathy? A comparative investigation into the causes of current popularity of homeopathy in the USA. [Google Scholar]
- 19.United Nations . United Nations; New York: 2008. United Nations Declaration on the Rights of Indigenous Peoples [Online]http://www.un.org/esa/socdev/unpfii/documents/DRIPS_en.pdf [Cited 2017 Dec 10]. Available from: [Google Scholar]
- 20.National centre for Complementary and integrative health . NCCIH; Maryland: 2017. Homeopathy [Internet]https://nccih.nih.gov/health/homeopathy [Cited 2017 Dec 12]. Available from. [Google Scholar]
- 21.Gohil K.J., Patel J.A. Herb-drug interactions: a review and study based on assessment of clinical case reports in literature. Indian J Pharmacol. 2007;39:129–139. [Google Scholar]