Abstract
Primary amyloidosis results from the deposition of amyloid protein fibrils in the extracellular space and rarely involves the urinary bladder. We present a 41-year-old man who was diagnosed with primary amyloidosis of the urinary bladder and underwent two sessions of transurethral resection of the bladder mass 4 years prior. Recently, the patient was admitted through the emergency with painless frank haematuria. Computed tomography of the abdomen and pelvis revealed a bladder mass that was larger than the previously reported mass. A repeat cystoscopy and resection of the mass was performed. Histopathological examination of the resected tissue revealed primary amyloidosis of the urinary bladder. A comprehensive examination was performed to exclude systemic amyloidosis.
Keywords: Amyloidosis, Benign tumour, Haematuria, Progressive, Recurrent, Urinary bladder
الملخص
ينتج الداء النشواني الأولي من ترسب لييفات بروتين الأميلويد في المساحة خارج الخلية، وفي كثير من الأحيان يشمل المثانة البولية. نعرض حالة مريض ذكر عمره ٤١ عاما تم تشخيصه بالداء النشواني الأولي للمثانة البولية، وتم استئصال ورم في المثانة عن طريق الإحليل مرتين قبل ٤ أعوام. دخل المريض المستشفى مؤخرا، عن طريق وحدة الطوارئ يعاني من بول دموي واضح غير مؤلم. وأظهرت الأشعة المقطعية للبطن والحوض ورما في المثانة أكبر من الذي تم ذكره سابقا. وتم إعادة تنظير للمثانة واستئصال الورم وأظهر التشريح المرضي للنسيج الداء النشواني الأولي للمثانة البولية. كما تم إجراء فحص شامل لاستبعاد الداء النشواني الشامل.
الكلمات المفتاحية: المثانة البولية, ورم حميد, الداء النشواني, متكرر, مترقي, بول دموي
Introduction
Amyloidosis is a disorder of protein metabolism characterised by the deposition of amyloid protein fibrils in the extracellular spaces of different body tissues. It may remain localised to a single organ or present as a systemic disorder involving multiple organs.1, 5 Primary localised amyloidosis of the urinary bladder is a rare condition, first described by Solomin in 1897,1 with less than 200 cases reported worldwide.2 The main presentations of primary amyloidosis of the urinary bladder are intermittent, painless frank haematuria with irritative voiding symptoms.1, 2, 3 The condition can be easily mistaken for a malignancy on the basis of imaging and cystoscopy findings.6, 7 Therefore, transurethral resection of the lesion and histopathological examination are considered the standard strategy for diagnosis and treatment and to exclude malignancy.6, 7
Case report
A 41-year-old man presented for the first time to the Accident and Emergency department in 2012 complaining of haematuria that lasted for 10 days duration that was intermittent, painless, terminal and frank, with passage of clots associated with mild dysuria. The patient was a non-smoker with no comorbidities.
The results of a urinalysis and a urine culture were negative. His urine cytology showed atypical urothelial cells and was negative for malignancy. Ultrasound of the kidney, ureters and bladder revealed a normal upper urinary tract and two echogenic lesions measuring 0.87 × 0.65 cm and 1.7 × 1.4 cm, respectively, in the posterior wall of the urinary bladder (Figure 1).
Figure 1.

Ultrasonographic image showing a bladder mass.
He underwent a cystoscopy that revealed a polypoid nodular lesion measuring approximately 2 cm in size, with hyperaemia and ulceration involving the posterior bladder wall; this was highly suggestive of malignancy. Both ureteric orifices were not affected by the lesion. Transurethral resection of the lesion was performed. His histopathological findings were consistent with amyloidosis and were confirmed using special stains such as CD 138, Congo red, and haematoxylin & eosin (H&E) (Figure 2a,b,c).
Figure 2.
a: Histopathological examination of a specimen using CD138 stain. b: Histopathological examination of a specimen using Congo red stain. c: Histopathological examination of a specimen using haematoxylin & eosin (H&E) stain.
The patient was fine and appeared healthy at follow-up. Systemic investigations were performed to exclude systemic amyloidosis. His 24-h urine protein electrophoresis and urinary Bence Jones protein test results were negative. Additionally, the sigmoid colon biopsy result was also negative. His electrocardiogram was normal.
One year later he developed similar symptoms and underwent computed tomography (CT) which revealed a plaque-like, focal mural thickening along the left posterolateral aspect of his urinary bladder with a maximal thickness of 4–5 mm (Figure 3).
Figure 3.
CT scan of the urinary bladder showing bladder wall thickening of 4–5 mm.
Urine cytology was negative for malignancy. He was treated conservatively.
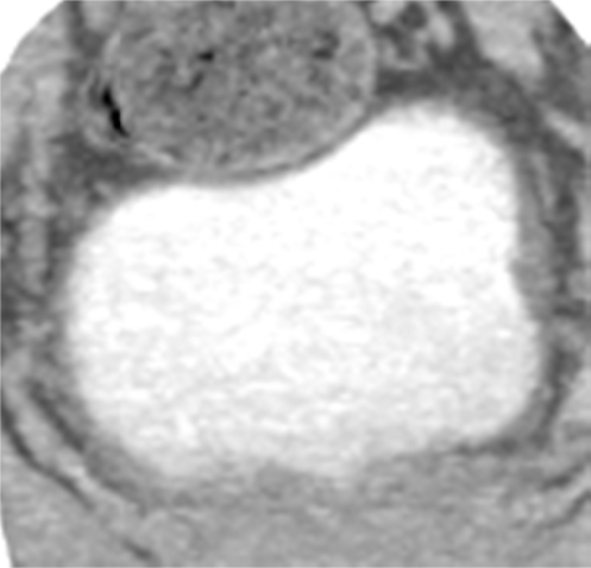
One year later, intermittent, gross painless haematuria with passage of clots recurred. CT was repeated and revealed that the urinary bladder was moderately distended, with focal wall thickening along the left posterolateral aspect with maximum thickness of 9 mm. The vesicoureteral junction was also affected and showed wall thickening (Figure 4).
Figure 4.

CT scan of the urinary bladder showing bladder wall thickening measuring 9 mm.
The patient was offered a check cystoscopy and transurethral resection of bladder tumour; but he refused and was lost to follow-up for approximately a year. He visited the Accident and Emergency again in November 2016 with painless, intermittent frank haematuria associated with the passage of clots and mild dysuria. All his blood test results were normal, and urine cytology was negative.
CT revealed that the urinary bladder was well distended with an enhancing, plaque-like, focal, nodular, polypoidal mural lesion along its left posterolateral aspect measuring approximately 4.3 × 1.5 cm in size. The adjoining vesicoureteral junction was also affected and showed wall thickening (Figure 5).
Figure 5.
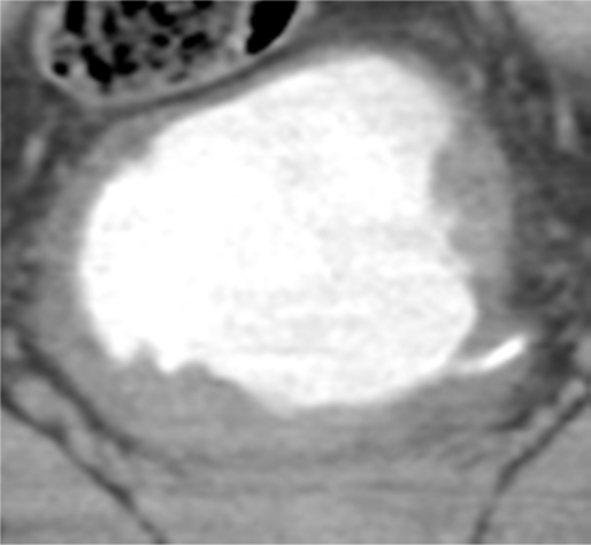
CT scan of the urinary bladder showing a nodular bladder mass.
He underwent cystoscopy, which showed a nodular lesion with ulceration, hyperaemia and a whitish layer involving almost the entire bladder wall (Figure 6a and 6b).
Figure 6.

a: Cystoscopic image showing a bladder mass. b: Cystoscopic image showing a bladder mass.
Near-complete transurethral resection of the lesion was performed.
Histopathological findings were consistent with amyloidosis of the urinary bladder.
Presently, the patient has been followed-up postoperatively over 6 months and has been asymptomatic. Should he develop recurrent tumour, re-TURBT has been planned. He has also been re-evaluated to exclude any systemic involvement, which was unproven in the findings.
Discussion
Primary isolated amyloidosis of the urinary bladder is a rare disease with 200 cases reported by Michael et al.1 The amyloid was first described by Virchow in 1854. The first case of isolated urinary bladder amyloidosis was described by Solomin in 1897.1 This condition is a disease of protein metabolism characterised by amyloid protein fibril deposition in the extracellular spaces of body tissues. Most patients with primary urinary bladder amyloidosis commonly present with intermittent, painless gross haematuria and some of them presented with irritative urinary symptoms that mimic transitional cell carcinoma.4, 9, 10 The disease is commonly seen in patients aged 50–70 years and the amyloid deposition is found predominantly in the posterior bladder wall (68%), followed by in the trigone (26%).15 The aetiology of localised primary amyloidosis is unknown. According to the proposed mechanism, chronic inflammation of the bladder causes an influx of lymphoplasmacytic cells into the submucosa of the bladder; these cells become monoclonal cells that secrete an abnormal light chain type immunoglobulin. Transurethral resection of the lesion and histopathological examination are important to establish a diagnosis and to exclude malignancy. Primary urinary bladder amyloidosis shows a high rate of recurrence. Tirzaman et al. followed 31 patients with localised bladder amyloidosis and observed that in 25% of patients the condition resolved and the patients became disease-free, 21% had persistent disease and 54% showed recurrence.11 Localised amyloidosis of the urinary bladder may not require systemic treatment,12 and surgical resection and fulguration may be the standard treatment even though other treatment modalities, such as the intravesical administration of dimethyl sulphoxide13 or the use of oral colchicine,14 have been reported in literature; however, their clinical utility remains limited. A cystectomy may be indicated in those with severe and uncontrolled haemorrhage. According to literature, this disease requires close long-term follow-up with annual check cystoscopy, as the rate of recurrence is high.
Conclusion
Primary amyloidosis of the urinary bladder is a rare disorder. The aetiology remains unknown and most patients present with intermittent, painless gross haematuria. Cystoscopic and histopathological examination are important to diagnose this condition as it resembles bladder malignancy. This case demonstrates that primary amyloidosis of the urinary bladder is a recurrent and progressive non-malignant disease. Transurethral resection and fulguration of the lesion remain the standard treatment. Long-term follow-up with annual check cystoscopy is recommended, as the rate of recurrence is high.
Source of funding
None.
Conflict of interest
There is no conflict of interest for any author.
Ethical approval
The ethics committee of Hamad Medical Corporation approved this study.
Consent
Only patient’s data is used in the study. Waiver of consent approved from ethical and research committees of institute obtained.
Guarantor
FSG.
Authors' contributions
FSG researched literature and conceived the study. FSG was involved in protocol development, gaining ethical approval, patient recruitment and data analysis. FSG wrote the first draft of the manuscript. FSG reviewed and edited the manuscript and approved the final version of the manuscript.
NS, AMS, AAY, KMA and KH reviewed the manuscript, helped in finalizing it and approved the final version of the manuscript.
EA studied and reported the histopathology specimen. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Jain M., Kumari N., Chhabra P., Gupta R.K. Localized amyloidosis of urinary bladder: a diagnostic dilemma. Indian J Pathol Microbiol. 2008;51(2):247–249. doi: 10.4103/0377-4929.41671. [DOI] [PubMed] [Google Scholar]
- 2.Merrimen J.L., Alkhudair W.K., Gupta R. Localized amyloidosis of the urinary tract: case series of nine patients. Urology. 2006;67(5):904–909. doi: 10.1016/j.urology.2005.11.029. [DOI] [PubMed] [Google Scholar]
- 3.Tan S.Y., Pepys M.B. Amyloidosis. Histopathology. 1994;25(5):403–414. doi: 10.1111/j.1365-2559.1994.tb00001.x. [DOI] [PubMed] [Google Scholar]
- 4.Auge B.K., Haluszka M.M. Primary amyloidosis of the bladder. J Urol. 2000;163(6):1867–1868. [PubMed] [Google Scholar]
- 5.Gupta N.P., Yadav S.P., Safaya R. Primary amyloidosis of urinary bladder. Indian J Urol. 1993;10:11–13. [Google Scholar]
- 6.Livneh A., Shtrasburg S., Martin B.M., Baniel J., Gal R., Pras M. Light chain amyloidosis of the urinary bladder: a site restricted deposition of an externally produced immunoglobulin. J Clin Pathol. 2001;54:920–923. doi: 10.1136/jcp.54.12.920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palmero Marti J.L., Budia Alba J., Arlandis Guzman S., Benedicto Redon A., Hernandez Marti M., Jimenez Cruz J.F. Secondary vesical amyloidosis. Actas Urol Esp. 2004;28:238–242. doi: 10.1016/s0210-4806(04)73066-1. [DOI] [PubMed] [Google Scholar]
- 9.Biewend M.L., Menke D.M., Calamia K.T. The spectrum of localized amyloidosis: a case series of 20 patients and review of the literature. Amyloid. 2006;13(3):135–142. doi: 10.1080/13506120600876773. [DOI] [PubMed] [Google Scholar]
- 10.Gupta P., Hanamshetti S., Kulkarni J.N. Primary amyloidosis with high grade transitional cell carcinoma of bladder: a rare case report. J Canc Res Therapeut. 2012;8(2):297–299. doi: 10.4103/0973-1482.98994. [DOI] [PubMed] [Google Scholar]
- 11.Tirzaman O., Wahner-Roedler D.L., Malek R.S., Sebo T.J., Li C.Y., Kyle R.A. Primary localized amyloidosis of the urinary bladder: a case series of 31 patients. Mayo Clin Proc. 2000;75:1264–1268. doi: 10.4065/75.12.1264. [DOI] [PubMed] [Google Scholar]
- 12.Chan E.S., Ng C.-F., Chui K.-L. Primary bladder amyloidosis e case report of a patient with delayed upper urinary tract obstruction 3 years after the diagnosis. Amyloid. 2010 May;17(1):36–38. doi: 10.3109/13506121003619377. [DOI] [PubMed] [Google Scholar]
- 13.Malek R.S., Wahner-Roedler D.L., Gertz M.A., Kyle R.A. Primary localized amyloidosis of the bladder: experience with dimethyl sulfoxide therapy. J Urol. 2002;168:1018–1020. doi: 10.1016/S0022-5347(05)64564-8. [DOI] [PubMed] [Google Scholar]
- 14.Livingstone R.R., Sarembock L.A., Barnes R.D., Folb P.I. Colchicine therapy in primary amyloidosis of the bladder: a case report. J Urol. 1989;142:1570–1571. doi: 10.1016/s0022-5347(17)39168-1. [DOI] [PubMed] [Google Scholar]
- 15.Tirzaman O., Wahner-Roedlar D.L., Malek R.S., Sebo T.J., Li C.Y., Kyle R.A. Primary localized amyloidosis of urinary bladder: a case series of 31 patients. Mayo Clin Proc. 2000;75:1264–1268. doi: 10.4065/75.12.1264. [PubMed] [DOI] [PubMed] [Google Scholar]



