Abstract
Objectives
Communication between physicians and parents is the cornerstone of their relationship to reach a common goal of better child health. To deliver proper communication, a physician needs to learn certain skills that are not included in the curriculum of medical schools or paediatrics residency training in KSA. This study probed the physicians' attitude towards their styles of communication based on the parents' perception.
Methods
The data were collected from a randomly selected sample of physicians and parents from general paediatrics wards at King Saud University Medical City (KSUMC), Riyadh, KSA. We used a validated Criteria Cognitive Aptitude Test (CAT-T) questionnaire and a translated version of the CAT-T questionnaire for the physicians and parents, respectively. The data were then analyzed using variable qualitative and quantitative statistical methods.
Results
The data were collected from 63 physicians and 100 parents in the pediatric wards at KSUMC. We observed an increased level of confidence in communication skills (CS) among experienced physicians, while young physicians expressed concerns regarding their communication with parents concerning decision-making. The parents rated the physicians' skill of active listening as poor. However, the parents rated the physicians' introduction as higher than their own self-rating. In addition, the parents' satisfaction with the physicians' CS was inversely related to the parents' level of education.
Conclusion
Our data suggests a clear discrepancy between the physicians' insights and the parents' perceptions about the CS. This finding emphasizes a need for further training among physicians to satisfy parents and in ultimately improving child health in the KSA.
Keywords: Communication, KSA, Parents, Perception, Physicians, Skills
الملخص
أهداف البحث
يُعد التواصل بين الأطباء والآباء حجر الزاوية في علاقتهم للوصول إلى هدف مشترك هو صحة أفضل للطفل. يحتاج الطبيب٬ حتى يتمكن من توفير التواصل المناسب٬ أن يتعلم مهارات معينة لا تشملها مناهج كليات الطب ولا برامج تدريب مقيمي الأطفال في المملكة العربية السعودية. سَبّرت هذه الدراسة انطباع الآباء تجاه أساليب تواصل الأطباء.
طرق البحث
جُمعت البيانات من عينة من الأطباء والآباء تم اختيارها بشكل عشوائي من أجنحة أمراض الأطفال العامة في مدينة جامعة الملك سعود الطبية بالرياض، في المملكة العربية السعودية. استخدمنا استبانة لاختبار الكفاءة المعرفية٬ وتم التحقق من صحة معاييرها للأطباء٬ ونسخة محررة ومترجمة من الاستبانة للآباء. بعد ذلك تم تحليل البيانات باستخدام أساليب إحصائية كمية ونوعية مختلفة.
النتائج
جُمعت البيانات من ٦٣ طبيبا و ١٠٠ من الآباء في أجنحة الأطفال في مدينة جامعة الملك سعود الطبية. لاحظنا مستوى مرتفعا من الثقة في مهارات التواصل بين الأطباء ذوي الخبرة٬ بينما أعرب الأطباء حديثو التخرج عن قلقهم بخصوص تواصلهم مع الآباء حول الأمور المتعلقة باتخاذ القرار. في حين أن الآباء قيّموا مهارات الأطباء في الاستماع الفعال بأنها ضعيفة. إضافة إلى ذلك فقد قيّم الآباء مهارات الأطباء في التقديم أعلى من تقييمهم الشخصي. كما أن رضى الآباء تجاه مهارات التواصل لدى الأطباء تناسبت تناسبا عكسيا مع المستوى التعليمي للآباء.
الاستنتاجات
تشير البيانات المتوفرة لدينا إلى فارق كبير بين انطباعات الأطباء ورؤى الآباء في ما يتعلق بمهارات الاتصال لدى الأطباء. تؤكد هذه النتيجة الحاجة إلى المزيد من التدريب بين الأطباء لبلوغ رضى الآباء وذلك للوصول في نهاية المطاف إلى تحسين صحة الطفل في المملكة العربية السعودية.
الكلمات المفتاحية: الاتصال, الآباء, الإدراك, الأطباء, المملكة العربية السعودية, مهارات
Introduction
The verbal and non-verbal communication between physicians and patients is a crucial element of everyday practice.1 The communication extends to include not only the patients, but, when dealing with children, their parents.2 Such communication helps in building an essential partnership between the healthcare providers, the children and their families. Without adequate communication, such partnership is in jeopardy, leading to poor health outcomes and decreased patient and family satisfaction.3
In paediatrics, those skills can be even more challenging.4 Beyond the sensitivity of dealing with delicate age groups, paediatricians have to tailor their communication according to each child's and parents' needs.5 Additionally, paediatricians address a wide spectrum of children in different developmental age groups that require variable communication styles.6
Communication skills are not well taught as part of the curriculum at medical schools or residency programs, especially in the Middle East.7, 8 Physicians, therefore, at different levels of their career might lack proper communication skills.9 While some practicing paediatricians have received further communication training in the postgraduate period, others have expressed contentment about their level of communication.6
The patients' and parents' views, attitudes and prospective differ from the physicians' insight on their communication skills.10 This study confronted the physicians' insights towards their styles of communication from the parents' perspective. We hypothesize that physicians in KSA, regardless of their level of training, overestimate their communication skills and assume certain aspects of what should be considered as a routine communication as impractical. The hypothesis extends to explore which domains of communication skills physicians lack, corresponding to their gender and level of training.
To assess communication, a widely used and validated Communication Assessment Tool-Team (CAT-T) was employed. It has been tested in 39 countries, including KSA.10, 11 A translated Arabic version of this validated tool was published and used in the pediatric settings.3
This study attempts to compare physicians' insights and parents' perceptions towards communication skills (CS) in general pediatric settings in KSA. Such a comparison might shed light on a deficiency in the CS from the perspectives of both parties. Additionally, it explores which components of CS are valued by both.
Materials and Methods
This study took place at the King Saud University Medical City (KSUMC) over a period of six months, including a pilot period (June to December 2015). The KSUMC is a leading tertiary teaching hospital in Riyadh, KSA. The data were collected from a proportionate number (n = 100) of physicians and primary caregivers of children in stable condition in the pediatric wards. Prior to being surveyed, parents were given a minimum of 24 h after admission to the ward to allow time for communication to occur with their treating general pediatric medical team.
Parents' data
A published Arabic version of the CAT-T questionnaire was employed for our Arabic-speaking patients/parents.3 Inclusion criteria included all children admitted to general paediatrics, regardless of their ages, those who have no chronic illnesses that require follow-up and their primary caregivers have no barriers to fully communicating with their medical teams. Exclusion criteria included a short stay (i.e., less than 24 h), children in follow-up with pediatric subspecialties for chronic diseases and an inability to give an informed consent.
Physicians' data
Physicians data was collected using the validated English CAT-T questionnaire was adopted for physicians.12 The physicians' questionnaire was retained in English to avoid any translation bias and maintain its validity. Physicians at different levels of training were requested to complete a self-rating questionnaire, with consideration of their age and gender, in a period and setting similar to the parents' data. The main inclusion criteria were to be a practicing physician in in-patient general paediatrics and to consent to answering the CAT-T questionnaire completely. Based on KSUMC practice, each intern cares for 4 patients, while each resident cares for 5 patients and each consultant usually interacts with 10 patients.
An informed consent was sought from each of the respondent physicians and parents/patients to answer the questionnaire completely and the study has an IRB approval.
Statistical analysis
The raw data were transferred into an Excel spreadsheet and analyzed utilizing the commercial software SPSS, version 20. Furthermore, categorical data were described utilizing percentages, means and medians when necessary for continuous variables that were obtained via summative analysis.
Principal Component Analysis (PCA) and Exploratory Factor Analysis (EFA), with the correlation matrix as an input, were used to identify interdependencies of the items of the CAT-T and existing constructs that may be revealed by the responses from parents and physicians. Furthermore, non-parametric Kruskal–Wallis and Mann–Whitney U tests were used due to the unknown distribution of the outcomes and sample size. They were employed to test the differences of median ranks of specific demographic factors. Additionally, summative analysis, a new qualitative statistical analysis tool focusing on outcomes,13 was adopted to calculate the total score of the CAT-T scale. Finally, the Student t-test was employed to compare the differences among the means of the ratings between the parents and physicians.
Results
Parents' characteristics
One hundred female participants consented to enroll in the study, i.e., the gender of all respondents was female (100%). Those women were the primary caregivers for the children admitted to the pediatric wards at KSUMC; 93% of them were the biological mothers while the remaining 7% were either older sisters, aunts or grandmothers. Their ages varied between twenty-one and forty years old or more. The age distribution was almost consistent among the different age categories, except those older than forty who composed less than 8%. The education level varied from illiterate women, who composed 6% of the parents' study population; followed by women who had basic education between elementary to secondary high school education, who were nearly the largest proportion of study participants (48%); and the remainder were women with a higher education (college, graduate and post graduate, 46%). The children, on the other hand, were nearly of equal gender distribution and their ages ranged from less than 1–14 years old (Table 1).
Table 1.
The respondent caregivers' and children's characteristics.
| Frequency | Percentage | |
|---|---|---|
| Age | ||
| 21 to 25 years | 21 | 21% |
| 25 to 30 years | 30 | 30% |
| 31 to 35 years | 16 | 16% |
| 36 to 40 years | 25 | 25% |
| >40 years | 8 | 8% |
| Education | ||
| Illiterate | 6 | 6% |
| Elementary to Secondary | 20 | 20% |
| High School | 28 | 28% |
| University Degree | 36 | 36% |
| Post Graduate | 10 | 10% |
| Child sex | ||
| Male | 54 | 54.00% |
| Female | 46 | 46% |
| Child age | ||
| <1 year old | 42 | 42% |
| 1 to 3 years | 27 | 27% |
| 4 to 5 years | 11 | 11% |
| 6 to 11 years | 10 | 10% |
| >11 years | 10 | 10% |
| Relation to child | ||
| Mothers | 93 | 93% |
| Other close relatives | 7 | 7% |
Physicians' characteristics
One hundred self-reporting CAT-T questionnaires were distributed, with an overall response rate of 63% (n = 63 fully answered questionnaires). The distribution of male (52%) versus female (48%) physicians was almost equal. Most of the participating physicians were less than thirty years old (80.9%). The junior physicians (interns and pediatric residency trainees) represented 79.4% of the respondents. The remaining physicians consisted of fellows (3.2%), consultants with less than ten years' of experience (7.9%) and consultants with more than ten years of experience (9.5%) (Table 2).
Table 2.
The characteristics of the respondent physicians, N = 63.
| Frequency | Percentage | |
|---|---|---|
| Sex | ||
| Male | 33 | 52.40% |
| Female | 30 | 47.60% |
| Age | ||
| 21–25 years | 30 | 47.60% |
| 26–30 years | 21 | 33.30% |
| 31–40 years | 4 | 6.30% |
| >40 years | 8 | 12.70% |
| Level of training | ||
| Intern | 25 | 39.70% |
| Resident level 1 | 11 | 17.50% |
| Resident level 2 | 8 | 12.70% |
| Resident level 3 | 4 | 6.30% |
| Resident level 4 | 2 | 3.20% |
| Fellow | 2 | 3.20% |
| Consultant <10 years | 5 | 7.90% |
| Consultant >10 years | 6 | 9.50% |
Parents' perceptions vs. physicians' insights
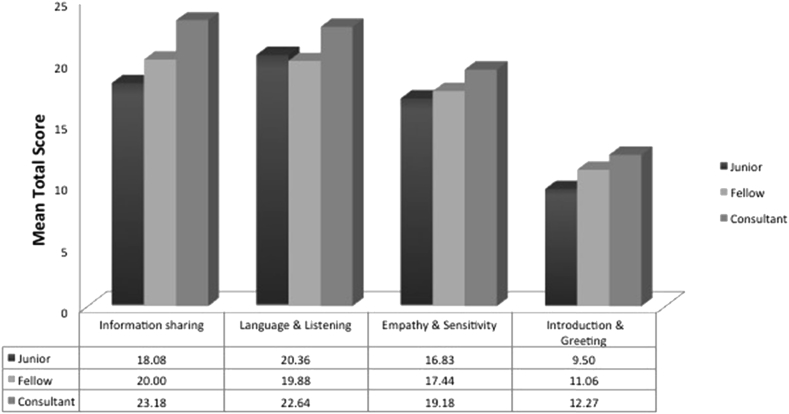
Overall, a significant difference was evident between the parents' response and the physicians' self-rating in the following items: physicians' full introduction, listening, time spent in communication and interaction with the children (Table 3). In fact, the physicians under-rated themselves in how they introduce their specialty compared to the ratings provided by parents, which was statistically significant (P < 0.001). In general, the physicians were self-conscious about how they introduce themselves. In contrast, the parents gave a lower score (statistically significant, P < 0.001) than the physicians regarding listening and understanding. Moreover, the parents found time invested in communication less satisfactory than the physicians (P = 0.003). Conversely, the physicians over-rated themselves with regards to proper interaction with children compared to the parents (P < 0.001) (Figure 1).
Table 3.
The mean of the CAT-T scale scoring. The difference between physicians' insights and parents' perceptions has been statistically significant in four main domains.
| Parents | Physicians | P | |
|---|---|---|---|
| Introducing name | 4.26 | 3.86 | 0.99 |
| Introducing specialty | 4.01 | 3.60 | <0.001 |
| Introducing level of training | 3.37 | 2.98 | 0.994 |
| Listening | 2.79 | 4.16 | <0.001 |
| Providing explanation and treatment plan | 4.50 | 4.30 | 0.99 |
| Avoiding medical terminology and difficult words | 4.61 | 4.27 | 0.99 |
| Providing reassurance | 4.39 | 4.43 | 0.325 |
| Spending enough time | 3.61 | 3.86 | 0.003 |
| Engaging with children | 3.76 | 4.35 | <0.001 |
| Involving parents in decision-making | 4.26 | 3.46 | 0.99 |
| Counselling and lifestyle modification | 3.36 | 3.87 | 0.99 |
| Providing congruent information | 4.60 | 3.83 | 0.99 |
Figure 1.
The comparison between physicians' insights and parents' perceptions of physicians' communication skills showed a clear discrepancy in certain domains, mainly listening and decision-making and the engagement of physicians with children.
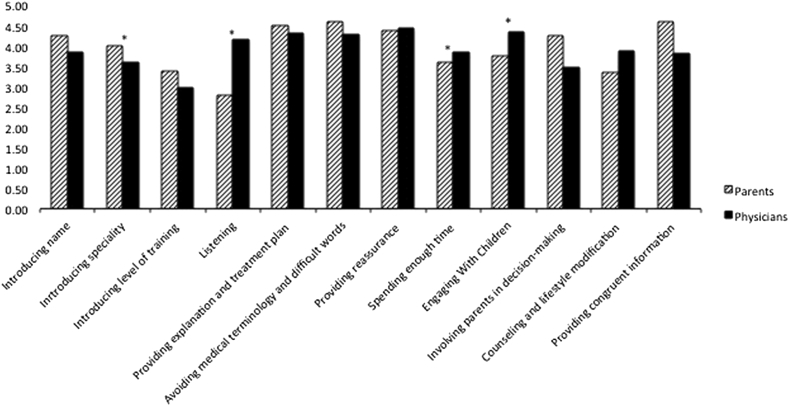
Principle component analysis (PCA)
Although the PCA of physicians rating themselves revealed a one-dimensional scale, the rotated factor solution uncovered four existing constructs. These constructs contained four domains of CS (information sharing, language & listening, empathy & sensitivity and introduction & greeting). The lowest ratings were in the introduction & greeting domain while the highest were in information sharing. Clearly, the physicians' ratings differed according to their rank (Figure 2).
Figure 2.
The effect of physicians' training on their confidence in the four domains of CS (information sharing, language & listening, empathy & sensitivity and introduction & greeting) was evident utilizing summative and principle component analyses.
Determining factors in physicians' confidence and parents' satisfaction
Using summative analysis, a total composite score for the CAT-T questionnaire was obtained for all respondent physicians by adding the items together (total score of 80). The consultant physicians were the most confident on their communication ability and rated their skills the highest (Mean = 77, SD = 6.4) and were the most consistent, as evidenced by the smallest standard deviation. They were followed by the fellow physicians (Mean = 68.4, SD = 12). Finally, the junior physicians rated themselves the lowest (Mean = 64.7, SD = 8.6). A non-parametric Kruskal–Wallis test indicated that the difference between the three physician ranks (junior, fellows and consultants) was significant (P = 0.001). However, a non-parametric Mann–Whitney U test was used to evaluate the impact of the physicians' gender on their communication self-reporting when the difference was found to be non-significant (P = 0.85).
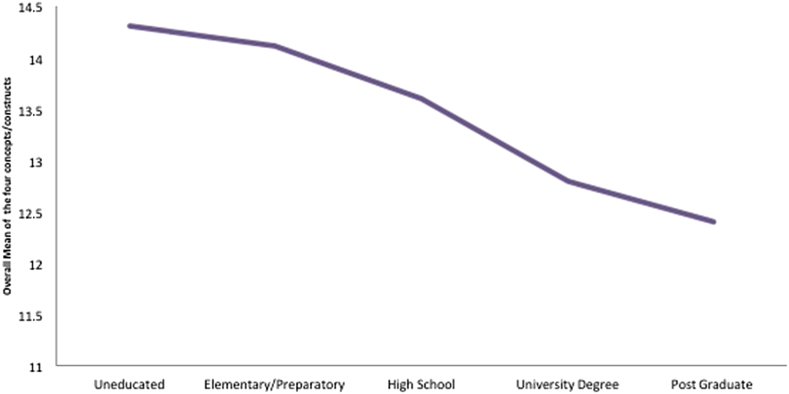
To analyze the parents' total perception/satisfaction score with physicians' communication skills, a series of non-parametric Mann–Whitney U and Kruskal–Wallis tests showed that that parents' level of education had a negative effect on their perceived satisfaction with the physicians' communication. Those with a higher education rated the physicians' communication less than those with a lower education (P = 0.016) (Figure 3). The parents' age and child's sex and age did not have a significant effect on the parents' perception and satisfaction with their physicians' communication skills.
Figure 3.
The satisfaction of the physicians' CS was inversely related to the mothers' level of education, indicated by principle component analysis.
Discussion
Communication in pediatric settings can be very challenging and a complex process.2, 14 The skills utilized to address multiple parties require different techniques and styles.15 Additionally, those skills have to consider geographic and cultural sensitivities.16
In KSA, health experts have raised concerns regarding physicians' communication skills due to a variety of reasons.17 Such concerns might affect child and public health, increase second-opinion visits, raise malpractice claims, decrease adherence to therapy, and escalate costs.1, 15, 16, 17 With the major impact of CS on health outcomes, proper training should be offered to those involved in child care.8 This study shows that confidence in CS amongst physicians is dependent on their years of experience and the physicians' rank. With the lack of CS courses in medical schools' curricula in KSA, trainees and younger physicians are unprepared to communicate with their patients properly.18 Our results provide indirect evidence to support previous demands and pleas to incorporate CS courses into undergraduate curricula.7 Still, practicing physicians have demanded further training in communication more than trainees or CME credit-earners.8 That might be explained by their deeper understanding of the impact of CS on child health.
Evidence of cultural sensitivity in CS was also apparent in the insights into and the satisfaction with the amount of time invested in communication. Several Western studies have reported physicians' complaints regarding insufficient time to provide proper communications.5, 9 In contrast, this study revealed high self-assurance of physicians in the amount of time spent in communication. However, parents found the provided time less satisfactory. With less time, counseling might be less detailed and ineffective.19
Communication can be addressed by defining the characteristics of every individual involved. All of the included parents were females, which might have an impact on our results. Females, especially mothers, usually demand better and more detailed communications about their children20; this could explain some low ratings. However, females are known to give lower ratings in self-reporting scales, yet, there was no difference in physician insights towards their CS based on gender.21 Despite earlier reports of higher CS among female physicians, this study did not show higher confidence in CS among female physicians.22, 23
Although previous research showed acceptable satisfaction of Saudi patients with their physicians' CS,11 more recent research has showed lower satisfaction.17, 24 Our finding of the inverse correlation between the parents' satisfaction and their level of education was supported by another study within the region.20 As the Saudi population is expanding and getting more educated, paediatricians' CS have to meet this evolution.
Although physicians were worried about how they introduced their name, rank and specialty, parents rated them above average in all three components. This could be explained by the general public's lack of knowledge and interest in knowing the different specialties and ranks of doctors.25
This study supports previous reports of a defect in listening skills, a major domain of communication, among the physicians in KSA.17 Despite the low ratings of listening skills by parents, physicians had rated themselves high on this domain, which suggests a serious lack of insight into this deficient aspect of their communication. In addition to observing poor listening skills, parents were not pleased with the physicians' interaction with their children. This finding supports earlier findings by Zolaly et al.3 Dissimilarly, Zolaly et al. reported low parents' satisfaction of their involvement in decision-making; that was not observed in this study. Actually, physicians expressed concern that they were involving parents to little in decision-making. Additionally, physicians were more concerned regarding the discrepancy of information provided by the team than the parents. This concern might be attributed to the hierarchy among medical teams and the number of physicians caring for a given patient.26 However, the lack of disagreement between physicians' and parents' ratings in certain domains sheds a light on which competency should be addressed in the future to improve communication and parents' satisfactions within in-patient general pediatric settings in KSA.
Conclusion
There is an obvious discrepancy between physicians' insights and parents' perceptions of communication skills in the in-patient general paediatrics settings in KSA. Unless interventions are made, this gap is expected to continue to increase with the expansion in the Saudi population as well as improvements in the level of education. We recommend introducing CS training into the curricula of the Saudi medical schools and paediatrics residencies.
Conflict of interest
All authors declare no conflict of interest during study design, data collection, data analysis and writing of this manuscript. They also disclose no financial or any secondary gain. This study adhered to KSU ethical committee roles and conditions in every step.
Authors' contribution
YF, HBN, ABB, LAE, ZAM conceived and designed the study. YF, HBN, ZAM, LAE, AES conducted research, provided research materials, and collected and organized data. YF, HBN, AES analyzed and interpreted data. YF, ABB, AES wrote initial and final draft of article, and provided logistic support. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Footnotes
Peer review under responsibility of Taibah University.
References
- 1.Zolnierek K.B.H., Dimatteo M.R. Physician communication and patient adherence to treatment: a meta-analysis. Med Care. 2009;47(8):826–834. doi: 10.1097/MLR.0b013e31819a5acc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Howells R., Lopez T. Better communication with children and parents. Paediatr Child Health (Oxford) 2008;18(8):381–385. [Google Scholar]
- 3.Zolaly M.A. Satisfaction of parents of paediatric patients with physicians' communication skills in Almadinah Almunawwarah, Kingdom of Saudi Arabia. J Taibah Univ Med Sci. 2012;7(1):29–34. Taibah University. [Google Scholar]
- 4.Pantell R.H., Stewart T.J., Dias J.K., Wells P., Ross A.W. Physician communication with children and parents. Pediatrics. 1982:396–402. [PubMed] [Google Scholar]
- 5.DiMatteo M.R. The role of effective communication with children and their families in fostering adherence to pediatric regimens. Patient Educ Couns. 2004;55(3):339–344. doi: 10.1016/j.pec.2003.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Levinson W., Lesser C.S., Epstein R.M. Developing physician communication skills for patient-centered care. Health Aff. 2010;29(7):1310–1318. doi: 10.1377/hlthaff.2009.0450. [DOI] [PubMed] [Google Scholar]
- 7.AL-Shehri M. Communication skills courses: a plea for inclusion in the medical curriculum. Saudi J Heal Sci [Internet] 2012;1(1):2. http://www.saudijhealthsci.org/text.asp?2012/1/1/2/94976 Available from: [Google Scholar]
- 8.Cegala D.J., Broz S.L. Physician communication skills training: a review of theoretical backgrounds, objectives and skills. Med Educ. 2002;36(11):1004–1016. doi: 10.1046/j.1365-2923.2002.01331.x. [DOI] [PubMed] [Google Scholar]
- 9.Harrington N.G., Norling G.R., Witte F.M., Taylor J., Andrews J.E. The effects of communication skills training on pediatricians' and parents' communication during “sick child” visits. Health Commun. 2007;21(2):105–114. doi: 10.1080/10410230701306974. [DOI] [PubMed] [Google Scholar]
- 10.Mercer L.M., Tanabe P., Pang P.S., Gisondi M.A., Courtney D.M., Engel K.G. Patient perspectives on communication with the medical team: pilot study using the communication assessment tool-team (CAT-T) Patient Educ Couns. 2008;73(2):220–223. doi: 10.1016/j.pec.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Network W.I. 2011. Doctor–patient global communication performance. [Google Scholar]
- 12.Asiimwe C., Kyabayinze D.J., Kyalisiima Z., Nabakooza J., Bajabaite M., Counihan H. Early experiences on the feasibility, acceptability, and use of malaria rapid diagnostic tests at peripheral health centres in Uganda-insights into some barriers and facilitators. Implement Sci. 2012 Jan;7(1):5. doi: 10.1186/1748-5908-7-5. BioMed Central Ltd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rapport F. Summative analysis: a qualitative method for social science and health research. Int J Qual Methods. 2010:270–290. [Google Scholar]
- 14.Marten G.W., Mauer A.M. Interaction of health-care professionals with critically ill children and their parents. Clin Pediatr (Phila) 1982;21(9):540–544. doi: 10.1177/000992288202100905. [DOI] [PubMed] [Google Scholar]
- 15.Razavi D., Merckaert I., Marchal S., Libert Y., Conradt S., Boniver J. How to optimize physicians' communication skills in cancer care: results of a randomized study assessing the usefulness of posttraining consolidation workshops. J Clin Oncol. 2003;21(16):3141–3149. doi: 10.1200/JCO.2003.08.031. [DOI] [PubMed] [Google Scholar]
- 16.Sue D.W., Sue D. Barriers to effective cross-cultural counseling. J Couns Psychol. 1977;24(5):420–429. [Google Scholar]
- 17.Al-misfer M.F., Al-zahrani B.S. Knowledge, attitude, practice and barriers of effective communication skills during medical consultation among center, Riyadh, Saudi Arabia. MIDDLE EAST J Fam Med. 2015;13(4):5–17. [Google Scholar]
- 18.Alofisan T., Alaiyan Al S., Abdulsalam Al M., Siddiqui K., Bin Hussain I., Qahtani Al M.H. Communication skills in pediatric training program: national-based survey of residents' perspectives in Saudi Arabia. J Family Community Med. 2016:43–47. doi: 10.4103/2230-8229.172233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Al-Muhsen S., Dulgom S., Assiri Z., Al-Jahdali H., Horanieh N., Vazquez-Tello A. Poor asthma education and medication compliance are associated with increased emergency department visits by asthmatic children. Ann Thorac Med. 2015;10(2):123. doi: 10.4103/1817-1737.150735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abadel F., Hattab A. Patients' assessment of professionalism and communication skills of medical graduates. BMC Med Educ. 2014;14(28):1–8. doi: 10.1186/1472-6920-14-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bowring A.L., Peeters A., Freak-poli R., Lim M.S.C., Gouillou M., Hellard M. Measuring the accuracy of self-reported height and weight in a community-based sample of young people. BMC Med Res Methodol. 2012;12(175) doi: 10.1186/1471-2288-12-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mohamed B.A. How physician gender shapes the communication of medical care in Saudi Arabia: the case of female patients. Sudan J Public Health. 2011;6(1):14–22. [Google Scholar]
- 23.Bernzweig J., Takayama J., Phibbs C., Lewis C., Pantell R. Gender differences in physician-patient communication. Arch Pediatr Adolesc Med [Internet] 1997;151:586–591. doi: 10.1001/archpedi.1997.02170430052011. http://eprints.kingston.ac.uk/4975/ Available from: [DOI] [PubMed] [Google Scholar]
- 24.Elzubier A.G. Doctor-patient communication: a skill needed in Saudi Arabia. J Family Community Med. 2002;9(1):51–56. [PMC free article] [PubMed] [Google Scholar]
- 25.Santen S.A., Rotter T.S., Hemphill R.R. 2007. Patients do not know the level of training of their doctors because doctors do not tell them. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liberatore M.J., Nydick R.L. The analytic hierarchy process in medical and health care decision making: a literature review. Eur J Oper Res. 2008;189:194–207. [Google Scholar]