Abstract
IN BRIEF Diabetes applications for electronic devices (apps) leverage the computing power and wireless connectivity of smartphones to offer unique advantages over more traditional tools such as paper logbooks and glucose meters. As these apps and the devices they connect with continue to evolve, health care providers play an important role in guiding patients by recommending specific apps, demonstrating best practices on their usage, and cautioning against their limitations.
More than 10 years after the Apple App Store was first introduced to iPhone users in 2008, tens of thousands of smartphone applications (apps) now promise to help people living with diabetes. From logging tools to hardware companions, the scope and functionality of diabetes apps continue to expand at a breakneck pace. Despite the potential benefit of these apps, their ability to improve glycemic control and reduce complications remains unproven. A 2016 meta-analysis of 14 studies evaluating diabetes apps showed a mean A1C reduction of 0.49%, with most studies being unblinded and limited in sample size (1).
Regardless, diabetes smartphone apps only continue to grow in popularity as more diabetes devices pair with apps and as consumer-focused companies such as Google, Amazon, and Apple explore solutions that extend into chronic care management. Therefore, as trusted members of the care team, health care providers (HCPs) owe it to their patients to familiarize themselves with the available diabetes apps, to support their clinically beneficial features and advantages, and—equally important—to caution patients regarding their shortcomings and potential pitfalls.
Diabetes apps today offer a variety of features, including monitoring food intake and physical activity, tracking insulin/medication and blood glucose data, providing diabetes self-management education resources, and facilitating communication between patients and HCPs. Nutrition-focused apps can instantly search live-updating databases of millions of food entries. Diabetes apps can also leverage social networks and connect users to hundreds of thousands of others around the globe. Some glucose meters have their own corresponding app that allows glucose data to be wirelessly synchronized to an individual’s smartphone (e.g., the Contour diabetes app for the Ascensia Contour Next One meter). Another feature, specific to iPhone users, is the factory-installed Apple Health app, which can serve as a gateway for automatically sharing diabetes data such as insulin dosing, glucose information, and activity data across multiple apps. Once configured, Apple Health allows users to consolidate multiple data streams into a single app to help simplify daily diabetes management.
The Case for Diabetes Apps
Given their lack of large-scale, randomized clinical trials proving efficacy, why should HCPs take diabetes apps seriously and recommend them for patient use?
One primary reason is that smartphones are always within reach; nearly every patient (and clinician, for that matter) has a smartphone nearby at all times, regardless of insurance status, cultural background, and often even socioeconomic status. In contrast, traditional diabetes devices such as glucose meters are frequently left behind during social gatherings, work days, or trips to the doctor. Generally speaking, the best tool is one that is available when needed, and smartphones are almost always ready to answer the call of duty.
Contrary to popular belief, smartphone use is not limited to younger generations; smartphones have widespread appeal and usage across all age-groups. A 2017 Pew study (2) found that 42% of adults ≥65 years of age own a smartphone, 67% of senior citizens have or use the Internet, and 34% have or use social media (2). The study authors concluded that smartphone usage among the elderly had quadrupled in the previous 5 years.
Beyond simply being more available and accessible than other diabetes tools, smartphones are also exponentially more powerful and have more advanced functionality than more conventional diabetes tools such as paper logbooks or nutrition reference books. For example, diabetes logbook apps can beautifully and elegantly display data in charts and tables, with live-updating statistics and color-coding that were previously only available to the most computer-savvy users. From a sheer computer processing perspective, even basic modern-day smartphones easily outperform older-generation supercomputers (3).
Smartphone apps also prove incredibly useful for doing basic, mundane tasks repetitively without error, outperforming the attention span of any human being. For example, a continuous glucose monitoring (CGM) app (paired with a CGM device such as the Dexcom G6 or Senseonics Eversense) can automatically analyze each new glucose measurement every 5 minutes, 24 hours a day, and potentially alert the user to a concerning result or trend.
Another significant benefit of smartphones relates to the convenient and accurate transfer of diabetes data. Electronic data exchange eliminates the biochemical hazards of handling paper logbooks stained by blood drops and preserves the integrity of the data by removing possible sources of error such as illegible handwriting and fictitious or incomplete data entries. In one study, 25% of paper glucose logbooks provided by patients (n = 29 of 115) were inaccurate (4). Many smartphone apps wirelessly transfer glucose readings from a Bluetooth-enabled glucose meter, ensuring precise time stamps and glucose measurements.
Although conventional in-office glucose meter downloads also reliably and electronically transfer data, they require special software and proprietary cables that can dramatically slow down clinic workflows. Furthermore, they depend on patients actually bringing their device to their appointments, which frequently does not occur. Most smartphone apps can easily generate and share reports via email or even by fax. Alternatively, HCPs can usually access their patients’ data on their workstations via Cloud-based Web portals (e.g., Dexcom Clarity) or can view data directly on patients’ smartphone screens.
Pitfalls of Diabetes Apps
Unfortunately, despite their many benefits, diabetes apps are not without their downsides. First, mobile apps are constantly evolving, with new software updates being rolled out on a regular basis. Although new versions can introduce improved functionality, they can also introduce bugs and remove features without any advance warning. In addition, an updated version can also introduce a different pricing model, requiring payment to continue using features that were previously free to use. Perhaps worst of all, many diabetes apps are developed by individuals or small teams without a long-term commitment or sustainable business model, leading to apps that go abandoned and unsupported over time.
Along these lines, unlike a conventional diabetes device such as a glucose meter or insulin pump, the majority of diabetes apps are not regulated by a governing body such as the U.S. Food and Drug Administration. Therefore, a smartphone app might not properly perform an advertised function or might lack safeguards to prevent harmful mistakes from operator error. Consider a smartphone bolus calculator app that claims to help users calculate the appropriate dose of mealtime insulin. A 2015 study looked at 46 English-language bolus calculator apps available in the Apple App Store and in Google Play for Android devices. The authors found that only 14 (30%) provided documentation for the calculation formula, 42 (91%) lacked numeric input validation, and 27 (59%) allowed calculation when one or more inputs were missing (e.g., a correction bolus was calculated even though an insulin sensitivity factor parameter was not provided) (5). By lacking these features, many of the reviewed apps would not protect users against potentially harmful recommendations resulting from typographical or configuration errors. For example, adding an extra zero to a blood glucose reading (making it 1,200 instead of 120 mg/dL) could lead to a dose recommendation that is 10 times bigger than what is actually needed, which could lead to serious adverse events or even death.
In addition, the unregulated nature of many diabetes apps creates a Wild West environment with respect to the quality and accuracy of educational materials within the apps. Quite a few diabetes apps offer online communities where users can interact with one another. Although these communities provide valuable support networks and have the potential for offering helpful advice, misinformation can also circulate because of limited moderation and oversight.
The wireless connectivity of smartphone apps also presents potential cybersecurity risks to patients. The confidentially of health information is considered to be of utmost importance by patients and HCPs and is ensured through regulations such as the Health Insurance Portability and Accountability Act, but health data voluntarily stored in apps are often stored on remote servers that are inherently more vulnerable to security breaches. If Fortune 500 companies that claim to value privacy such as Facebook and Equifax can be hacked, it stands to reason that the smaller-scale companies behind diabetes apps are vulnerable as well. In March 2018, the most widely used health app of all time, MyFitnessPal, announced a security breach that allowed an unauthorized party to access data associated with the accounts of ∼150 million users (6).
Beyond the invasion of privacy, cybersecurity risks extend to potentially malicious hacking of diabetes apps and devices. Although there have been no documented episodes of which we are aware, the diabetes community must continue to safeguard against such disastrous scenarios. Toward that end, the Diabetes Technology Society (DTS) has created industry standards such as the DTS Cybersecurity Standard for Connected Diabetes Devices (DTSec) and DTS Use of Mobile Devices in Diabetes Control Contexts (DTMoSt), a consensus cybersecurity standard whose goal is to provide assurance that consumer mobile phones can safely control diabetes devices (7). Historically, to minimize risk, smartphone integration with insulin pumps has been limited to monitoring rather than control of the medical device. However, in light of rising consumer demand for mobile phone control of insulin delivery, the DTMoSt Standard provides a framework to eliminate safety issues that might arise from interruptions in wireless connectivity or malicious commands being sent by a foreign device.
Identifying High-Quality Diabetes Apps
How can HCPs know what to recommend when the app landscape is filled with so many options? One trusted resource on diabetes apps is the App Review Library (DANAapps.org), a service provided by the American Association of Diabetes Educators (AADE) Diabetes Advanced Network Access (DANA) online technology initiative. Currently available for AADE members, DANA’s App Review Library evaluates apps pertaining to diabetes management, fitness, nutrition, and conditions ranging from blood pressure to depression. DANA’s reviews are performed by an independent reviewing organization, DHX Labs, which uses a rigorous set of criteria and methodology to assess apps. Input from its multidisciplinary team of professionals further drives its reliability. Apps in DANA are evaluated on many factors, including privacy and security, performance, data management, functionality, usability, behavior science, and operability. They are then given a certification seal and a “trust score” to provide a quantitative and comparative assessment of risk (1 = exceptional, 2 = good, and 3 = average) (8). Directly from the website, users can download the apps and send them to colleagues or patients. An example of how an app review appears in DANA is shown in Figure 1.
FIGURE 1.
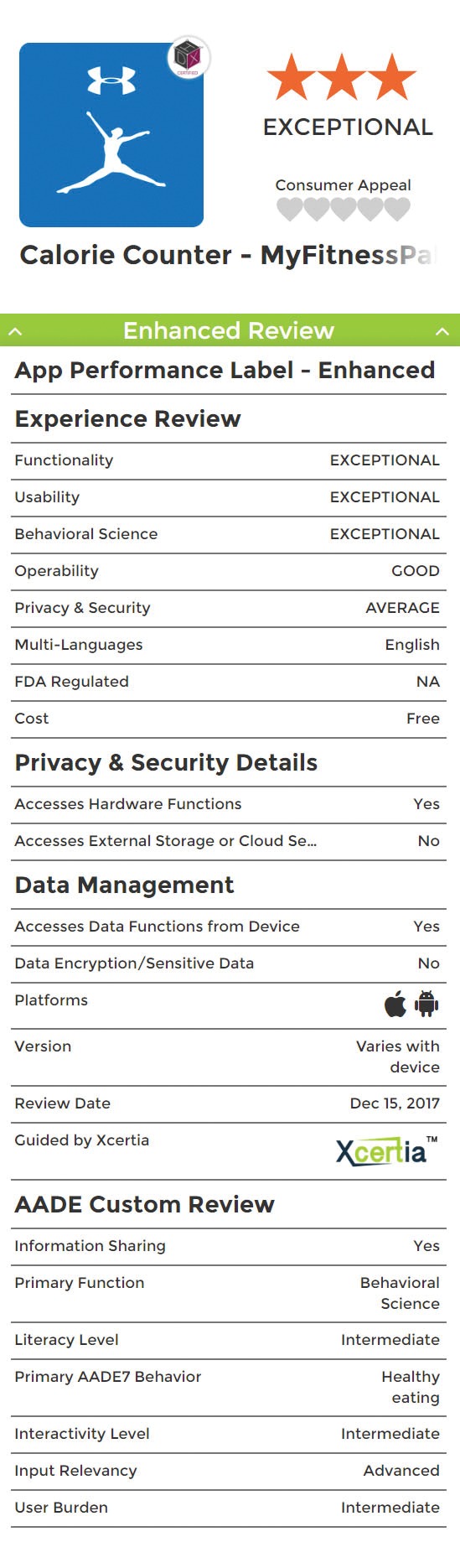
Example of DANA app review for MyFitness Pal. Graphic courtesy of DANAapps.org, from the American Association of Diabetes Educators.
In Table 1, we compiled a list of our top recommended diabetes apps, which cover a wide range of topics pertaining to diabetes management. The apps are available in the Apple App Store and/or Google Play for Android, and our recommendations were based on patient and peer feedback, with the following characteristics in mind:
-
• Functionality
○ Personalized goals
○ Reminders
○ Individualized feedback
○ Decision support
○ Social support
○ Connection to the seven key areas of diabetes self-management identified by the AADE (9): healthy eating, being active, monitoring, taking medication, problem solving, reducing risks, and healthy coping
-
• Reduction of user burden
○ User-friendly interface
○ Simplified data entry
○ Integration with diabetes devices (e.g., glucose meters or CGM devices)
○ Cost-effectiveness
-
• Facilitation of patient-provider relationship
○ Easy sharing of data
• Privacy and security
TABLE 1.
Authors’ Top Recommended Diabetes Apps
| Name of App | Compatibility | Cost | Category | Description |
|---|---|---|---|---|
| BD Briight: Diabetes Assistant | Apple/Android | Free | Management and monitoring | •Nutrition advice, healthy recipes, and activities |
| •Digital diabetes assistant available 24/7 | ||||
| •Voice recognition for logging insulin doses/blood glucose, asking questions | ||||
| CalorieKing | Apple | Free, with in-app purchases | Nutrition and fitness | •Curated food database of nutrition information |
| •Includes many fast-food chains and restaurants | ||||
| Figwee | Apple | Free, with in-app purchases | Nutrition and fitness | •Visualization tool for learning different portion sizes of food items with nutrition data |
| •Paid upgrade tracks what you eat, allows custom food entry, records progress | ||||
| Fooducate | Apple/Android | Free, with in-app purchases | Nutrition and fitness | •Nutrition tracking tool |
| •Individualized nutrition grade for each food | ||||
| •Personalization for age, sex, weight loss goal | ||||
| •Community support | ||||
| Glucagon | Apple/Android | Free | Management and monitoring | •Step-by-step instructions (text and video) for using glucagon for injection: 1 mg (1 unit) |
| •Tracker for glucagon kit locations and expiration dates | ||||
| •Reminder notifications | ||||
| MyFitnessPal | Apple/Android | Free, with in-app purchases | Nutrition and fitness | •Tracking tool for exercise, nutrition |
| •Connects with fitness trackers and other health apps | ||||
| •Large food database with nutrition information | ||||
| •Individualized based on sex, age, weight loss goal | ||||
| MySugr | Apple/Android | Free, with in-app purchases | Management and monitoring | •Tracking tool for blood glucose, mood, carbohydrates, medications |
| •Reports for HCPs | ||||
| •Paid upgrade adds reminders | ||||
| One Drop | Apple/Android | Free | Management and monitoring | •Tracking tool for blood glucose, mood, carbohydrates, medications |
| •Integrated nutrition database | ||||
| •Reminders | ||||
| •Reports for HCPs | ||||
| Relax Lite | Apple/Android | Free, with in-app purchases | Stress management | •Guided breathing and meditation exercises |
| Tidepool | Apple/Android | Free | Management and monitoring | •Compatibility with many devices (glucose meters, CGM devices, insulin pumps) |
| •Tracking tool for insulin, CGM, nutrition, and blood glucose data with notes | ||||
| •Reports for HCPs |
Best Practices for Recommending Diabetes Apps
Given the limited time HCPs have with patients, what are the best ways to implement and recommend diabetes apps in the context of the patient-provider relationship?
Experiment first-hand with apps before recommending them to patients. Consider strengths and weaknesses and how the app supports diabetes self-management. Often, apps are limited in scope, so the best app for one aspect of diabetes self-management (e.g., nutrition) might not be adequate for another area (e.g., glucose monitoring). In fact, in one recent analysis, only 4 of 89 apps integrated all six diabetes self-management tasks (i.e., physical activity, nutrition, blood glucose monitoring, medication or insulin dosage, health feedback, and education) (10).
Keep it personal. When recommending apps, always take into account the individual’s preferences, goals, and needs. Be sure to consider patients’ health literacy and numeracy skills.
Address barriers. Many patients may have a fear of incorporating something new or lack confidence in their ability to use new technology properly. Others may feel that using mobile apps may be too costly, think they will not have time, or feel they will have limited access to support. It is important for HCPs to understand their patients’ fears. Investigate costs and identify sources of ongoing support.
Consider data-sharing capabilities. Explore how each app might share data with HCPs since this can help provide an accurate snapshot of patients’ blood glucose patterns and create new insights to quickly visualize trends and make changes to medication regimens.
Practice “thorough onboarding.” Simply providing a patient with the name of a recommended app might not be helpful. Explain how the app can help the patient. Share your own experiences using the app. Support the person in downloading, registering, and customizing the app. The patient may need help adding information such as medications or insulin doses. Make your time with the patient a collaborative experience.
Education. Having a patient successfully install an app is not a replacement for proper diabetes education. For example, using an app for counting carbohydrates still requires proper dietary counseling. For best results, users must know how to interpret nutrition labels and how to properly visually estimate portion sizes. Furthermore, patients might benefit from education regarding how to take full advantage of their tools. Users with glucose meters covered by insurance (Ascencia Contour Next One, Accu-Check Guide, and OneTouch Verio) may not realize that their device can wirelessly synchronize glucose data to their smartphone if they install and run the official corresponding app (Contour Diabetes app, Accu-Chek Connect app, and OneTouch Reveal app).
Stay informed. Regularly check resources such as DANAapps.org, diaTribe.org, DiabetesMine.com, and the Facebook group Diabetes Technology Clinicians to learn more about new diabetes apps and diabetes technology.
Diabetes Apps Will Continue to Evolve
With the emergence of more connected digital diabetes tools such as smart insulin pens, app-enabled insulin pumps, and app-enabled CGM systems, we are still in the early innings of using diabetes apps in the clinical setting. The market will continue to introduce newer, more comprehensive smartphone app solutions that go beyond the fundamentals of monitoring and reach into digital therapeutics, in which apps will deliver individualized treatment advice suggested by remote human coaches or machine-based algorithms.
The app landscape will continue to evolve, and new products will become available. As when selecting from the growing array of diabetes pharmacotherapeutic and medical devices, HCPs should take an individualized, patient-centered approach rather than adopting a one-size-fits-all philosophy in recommending diabetes apps to their patients.
Acknowledgments
The authors would like to thank the editors for being invited to contribute to this issue and the reviewers, who greatly improved the manuscript.
Duality of Interest
D.T.A. has received honoraria for participating in scientific advisory boards for Ascensia and Mannkind. No other potential conflicts of interest relevant to this article were reported.
Author Contributions
D.T.A. and R.S. reviewed the literature and collected relevant information. D.T.A. wrote the first draft of the manuscript. R.S. reviewed and added significant portions to the manuscript. D.T.A. is the guarantor of this work, and, as such, takes responsibility for the integrity of the manuscript and the accuracy of the information presented.
References
- 1.Hou C, Carter B, Hewitt J, Francisa T, Mayor S. Do mobile phone applications improve glycemic control (HbA1c) in the self-management of diabetes? A systematic review, meta-analysis, and GRADE of 14 randomized trials. Diabetes Care 2016;39:2089–2095 [DOI] [PubMed] [Google Scholar]
- 2.Pew Research Center Tech adoption climbs among older adults. Available from www.pewinternet.org/2017/05/17/tech-adoption-climbs-among-older-adults. Accessed 11 December 2018
- 3.Experts Exchange Processing power compared. Available from pages.experts-exchange.com/processing-power-compared. Accessed 11 December 2018
- 4.Mazze RS, Shamoon H, Pasmantier R, et al. Reliability of blood glucose monitoring by patients with diabetes mellitus. Am J Med 1984;77:211–217 [DOI] [PubMed] [Google Scholar]
- 5.Huckvale K, Adomaviciute S, Prieto JT, Leow MK, Car J. Smartphone apps for calculating insulin dose: a systematic assessment. BMC Med 2015;13:106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Under Armour Under Armour notifies MyFitnessPal users of data security issue. Available from investor.underarmour.com/releasedetail.cfm?ReleaseID=1062368. Accessed 11 December 2018
- 7.Diabetes Technology Society DTMoSt: Diabetes Technology Society Mobile Platform Controlling a Diabetes Device Security and Safety Standard. Available from www.diabetestechnology.org/dtmost.shtml. Accessed 11 December 2018
- 8.DHX Group The review approach. Available from www.danaapps.org/our-approach. Accessed 23 February 2019
- 9.American Association of Diabetes Educators AADE7 self-care behaviors. Available from www.diabeteseducator.org/living-with-diabetes/aade7-self-care-behaviors. Accessed 7 April 2019
- 10.Chavez S, Fedele D, Guo Y, et al. Mobile apps for the management of diabetes. Diabetes Care 2017;40:e145–e146 [DOI] [PMC free article] [PubMed] [Google Scholar]


