Abstract
Humanitarian crises represent a major global health challenge as record numbers of people are being displaced worldwide. The Syrian crisis has resulted in >4 million refugees and 6 million people who are internally displaced within Syria. In 2017, there were 705,700 reported cases of adult diabetes in Syria. During periods of conflict, people with diabetes face numerous challenges, including food insecurity, inadequate access to medications and testing supplies, and a shortage of providers with expertise in diabetes care. Access to insulin represents a major challenge during a crisis, especially for individuals with type 1 diabetes, for whom the interruption of insulin constitutes a medical emergency. In the short term (days to weeks) during a crisis, it is vital to 1) prioritize insulin for patients with type 1 diabetes, 2) ensure continuous access to essential diabetes medications, and 3) provide appropriate diabetes education for patients, with a focus on hypoglycemia and sick-day guidelines. In the long term (weeks to months) during a crisis, it is important to 1) provide access to quality diabetes care and medications, 2) train local and international health care providers on diabetes care, and 3) develop clinical guidelines for diabetes management during humanitarian crises. It is imperative that we work across all sectors to promote the health of people with diabetes during humanitarian response.
Humanitarian crises are ever growing and represent a major global health challenge. Political instability and conflict have resulted in record numbers of people being displaced from their homes. In addition, natural disasters are on the rise. The United Nations High Commissioner for Refugees (UNHCR) estimates that >65 million people have been displaced worldwide (1).
Health care during emergency response has understandably focused on trauma, infectious diseases, and other acute conditions. Chronic diseases have historically been given low priority, especially during natural disasters, which are often of short duration. However, as humanitarian crises become widespread and prolonged, chronic conditions such as diabetes and hypertension are becoming increasingly important.
There are numerous publications on natural disasters and their consequences on the lives of people with diabetes (2,3). However, there are limited data on diabetes during manmade disasters. War and conflict present serious challenges for patients, health care providers (HCPs), and humanitarian workers. Furthermore, these crises often arise in developing countries where national disaster plans may not exist and local resources for health care are already exhausted.
Worldwide, various conflicts affect people living with diabetes, but in this article, we focus primarily on the Syrian crisis. The war in Syria, now in its seventh year, has become the most significant humanitarian crisis of our time, resulting in >5 million Syrians who have fled the country as refugees and another 6.1 million who are internally displaced within Syria (1).
In Syria before the conflict began in 2011, the prevalence of diabetes in the city of Aleppo was found to be 14.8% for individuals >25 years of age, and type 2 diabetes was only well controlled in 16.7% of individuals under treatment (4). In 2017, there were 705,700 reported adult cases of diabetes in Syria, with a prevalence of 12.6% among females and 11.2% among males (5). It is estimated that there are currently 400,000 Syrians whose survival depends on insulin (6). These figures reflect the overall trend of soaring rates of diabetes worldwide. The International Diabetes Federation (IDF) estimates that 425 million adults had diabetes in 2017 (7).
Challenges in Diabetes Care
In normal circumstances, the management of diabetes is challenging and requires medication, glucose monitoring, attention to diet, diabetes education, and regular visits to HCPs. In developing countries, access to health care and medications is often limited and, in some cases, unavailable, even in stable environments. During humanitarian crises, people who are displaced face a myriad of obstacles when it comes to diabetes care. Food insecurity, limited access to health care facilities and medications, and economic hardship are only a few of the many difficulties faced by refugees.
Quality of food and timing of meals is also unpredictable as high-carbohydrate foods become the mainstay of the diet. A dietary assessment of Syrian refugees in Lebanon showed that 21% of households reported low dietary diversity (<4.5 food groups daily), and only 18% reported high dietary diversity (>6.5 food groups daily) (8). Among refugees from Burma, a dietary assessment of 1,159 refugees showed that carbohydrates accounted for 84% of total calories (9). Physical activity is also decreased, in part due to limited space and safety concerns.
Perhaps the biggest barrier faced by those in crisis is the psychosocial trauma that makes health care low on their list of priorities. This is especially true because the majority of chronic diseases are asymptomatic until advanced disease is present. During a crisis, women are especially vulnerable (10) because they are relied on as the primary caregivers for their families but may not prioritize their own health. Language barriers may also be present, as refugee populations are diverse, and interpreters may be required to facilitate communication during the provision of health care.
Access to medications represents a major challenge for people who are displaced. It is estimated that the majority of those with chronic illness have been forced to interrupt their treatment for some duration (11). Access to quality diabetes care is also difficult, as fragile health systems in host countries are overwhelmed with the large influx of people during a crisis. In the case of the Syrian crisis, in countries such as Lebanon and Jordan, most refugees do not live in camps but are interspersed in urban areas and therefore obtain health care in many of the same centers as the host population. A 2018 health survey published by the UNHCR showed that, among Syrian refugees living in non-camp settings in Jordan, 39% reported difficulty accessing health services for chronic diseases (12). In Lebanon, 18,014 Syrian patients received chronic medications through 420 YMCA centers in 2017 (13). Many countries also face a severe shortage of human resources, as very few HCPs have training and expertise in diabetes. Testing supplies such as glucose meters and test strips can be scarce and lack a uniform standard, so patients are unable to monitor their glucose levels safely. Furthermore, donated meters and strips are often incompatible with supplies available locally, leaving patients to scramble for testing supplies.
The situation for people with type 1 diabetes is extremely dire and deserves special mention. During a crisis, insulin may not be readily available, and this can lead to severe hyperglycemia or diabetic ketoacidosis (DKA). On the other hand, patients on NPH or pre-mixed insulin are at risk for life-threating hypoglycemia when food supplies and the timing of meals are unpredictable. For individuals with type 1 diabetes, the interruption of insulin therapy is a matter of life or death. For example, Raghad Hasoun was an 11-year-old Syrian girl who died from DKA after her insulin was thrown overboard by traffickers who had promised her family safe passage to Italy (14). Raghad’s tragic story reveals the plight of many children with type 1 diabetes throughout the world who are also victims of conflict. As we recognize the growing importance of diabetes care during humanitarian response, priority should be given to those with type 1 diabetes.
Prevalence of Diabetes and Control Rates Among Syrian Refugees
The vast majority of Syrian refugees now live in the neighboring countries of Turkey, Lebanon, and Jordan. These three nations have experienced the greatest stress on their health systems since the beginning of the crisis. It is difficult to estimate the number of refugees living with diabetes due to limited documentation and data. Compared to the general Syrian population, the majority of refugees are women and children. Elderly people with diabetes are an especially vulnerable group, being at high risk for complications such as nephropathy, retinopathy, and amputations. A cross-sectional survey of 1,550 Syrian refugees in Jordan showed the overall prevalence of diabetes was 5.3%, and for adults >60 years of age, the prevalence was 32% (15). Cross-sectional surveys have also shown that more than half of Syrian refugee households in Jordan and Lebanon reported a family member with a chronic disease (16). By comparison, among Palestine refugees, a report from the United Nations Works and Relief Agency showed the prevalence of diabetes was 11.0% in adults >40 years of age attending their health centers (17).
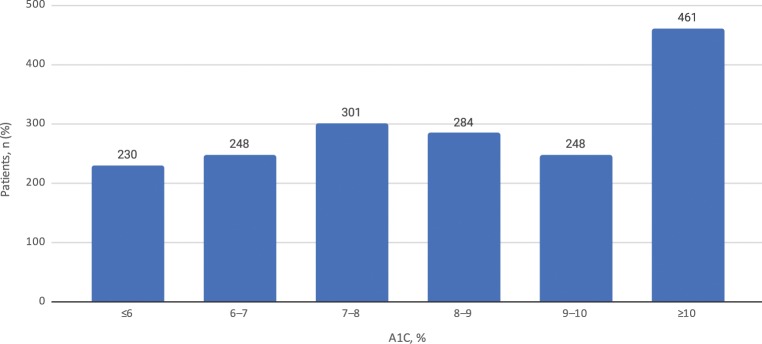
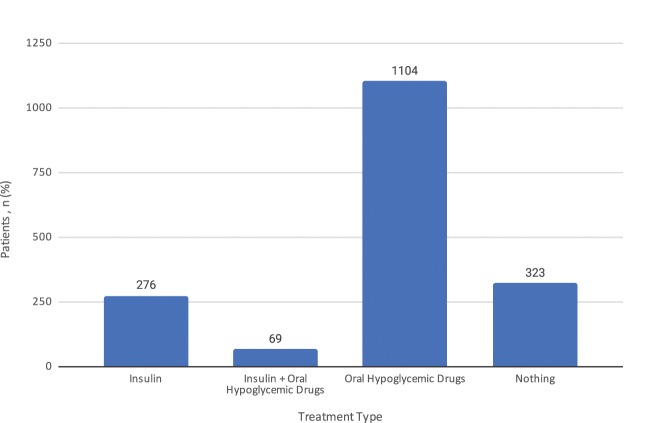
Recent cross-sectional data compiled from the Syrian American Medical Society (SAMS) and Multi Aid Programs (MAPS) in collaboration with IDF from specialty diabetes clinics for refugees in Lebanon show that of 1,722 patients presenting for diabetes management, only 28% were well controlled with an A1C of <7% (Figure 1). The majority of patients (62.8%) were treated with oral medication alone, whereas 15.9% of patients were treated with insulin therapy, and 19.1% did not take any treatment at the time of presentation to the clinic (Figure 2). The A1Cs of patients who were not on any treatment at the time of presentation were in the range of 8–9%.
FIGURE 1.
Baseline A1C results for patients presenting to nine free diabetes clinics in Lebanon from 2016 to 2018.
FIGURE 2.
Treatment modalities for patients presenting to nine free diabetes clinics in Lebanon from 2016 to 2018.
Diabetes Care for Syrian Refugees
Many local and international humanitarian organizations are working tirelessly to provide health care for Syrian refugees. Many of these groups have now expanded their work to include chronic conditions such as hypertension and diabetes. UNHCR, the International Organization for Migration, the World Health Organization (WHO), and Medecins Sans Frontieres have established chronic disease programs in Jordan, Lebanon, and Iraq in response to the increased demand for diabetes care.
Other groups are also paving the way for diabetes care for refugees. The IDF MENA (Middle East and North Africa) region is collaborating with SAMS and MAPS to provide free medical care, medications, insulin, and laboratory testing for refugees living with diabetes in Lebanon. IDF has also provided workshops to train HCPs in the MENA region. SAMS has been at the forefront of providing health care to Syrians since the start of the crisis, with a strong emphasis on chronic diseases such as cardiovascular disease (CVD) and diabetes. Although there is much work still to be done, it is encouraging to see the growing importance of chronic disease care in these vulnerable populations.
Access to Insulin During Humanitarian Crises
Almost 100 years after the discovery of insulin, global access to insulin remains a major challenge. This is due to a number of factors, including cost, availability, and distribution of insulin. In Syria before the crisis, insulin was produced in-country and was free for all registered users in the national diabetes program. Currently, many Syrians who are living with diabetes and are in need of insulin are struggling to obtain it. WHO, IDF, SAMS, Life for a Child, Direct Relief, and T1International are among the many organizations working to provide insulin for Syrian refugees.
Even when insulin is available, the distribution of insulin and other essential medications can be difficult because of geographical and political barriers. Furthermore, insulin requires cold-chain transportation and maintenance of temperatures between 2 and 8°C. Storage of insulin by patients is an additional challenge, as lack of refrigeration and exposure to high temperatures can compromise the integrity of insulin.
Although analog insulin may be ideal for some patients, overall, human insulin remains the most cost-effective insulin. The WHO recently made the decision to exclude long-acting analog insulin from its 2017 list of essential medications (18) in favor of less expensive human insulin. International aid organizations should include human insulin vials (NPH, regular, and 70/30 premixed) along with syringes in their core medication lists and emergency kits. During triage, patients with type 1 diabetes should be identified and given first priority with respect to insulin supply. The goal of increasing availability of insulin in crisis settings can be seen as part of a larger movement to advocate for insulin as a global human right. Organizations such as the International Insulin Foundation, T1International, the Endocrine Society, JDRF, and the American Diabetes Association are advocating for more affordable insulin, and we call on the global diabetes community to join them in the battle for universal access to this life-saving drug.
Essential Diabetes Medications
In addition to insulin, oral medications are a mainstay of treatment for type 2 diabetes. The WHO Model List of Essential Medicines (18), updated every 2 years, serves as a blueprint for the most important medicines of a health system and is a means to promote health equity. Included in the 2017 list are metformin and gliclazide, both of which are low-cost treatments for type 2 diabetes that are readily available worldwide. Gliclazide is preferable to glibenclamide because it has a lower risk of hypoglycemia (19). Also on the list are antihypertensive agents (enalapril, hydrochlorothiazide, and losartan), cardiovascular medications (aspirin and simvastatin), and glucagon. It is important to state that, in the long term, a comprehensive approach to diabetes care that also emphasizes treatment for hypertension and CVD is favored.
In addition to these essential medications, optimal management of diabetes requires testing supplies. Health centers providing care during a crisis should be equipped with glucose meters, test strips, syringes, intravenous 50% dextrose (D50), and ketone strips. Specialized diabetes kits have also been used previously with success in an emergency context (20).
Where resources permit, laboratory tests for A1C, lipids, creatinine, and urine microalbumin are essential to the long-term management of patients with diabetes. In areas where laboratory testing is not readily available, point-of-care A1C technology can provide valuable test results within 5–10 minutes using only a small sample of blood, allowing for use in camps and other temporary settings. A1C and glucose testing are particularly valuable for making medication adjustments over time, given the chronic nature of diabetes. A suggested list of essential medications and supplies for emergency kits and health centers is provided in Table 1.
TABLE 1.
Essential Diabetes Medications and Diagnostic Supplies for Emergency Kits and Health Centers
| Medications and Related Supplies |
|---|
| Insulin vials (NPH, regular, and 70/30 premixed) |
| Insulin syringes |
| Glucagon |
| D50 |
| Glucose tablets |
| Metformin |
| Gliclazide or glipizide |
| Losartan |
| Diagnostic Supplies |
| Glucose meters (locally available brands are preferred) |
| Glucose test strips |
| Ketone strips |
| Urine test strips |
| A1C testing (if available) |
Recommendations for Diabetes Management During a Crisis
Short Term (Days to Weeks)
In the initial days to weeks after any crisis, one of the main priorities for local and international health care teams is to identify people with diabetes and ensure continuous access to vital medications such as insulin (Table 2). For people with type 1 diabetes, the interruption of insulin and food supply constitutes an emergency and should be recognized as such. Other vulnerable groups include pregnant women with diabetes, the elderly, and patients with complications such as end-stage renal disease or foot ulcers. These patients should be prioritized with respect to insulin and diabetes care. For patients with diabetes who are able to test blood glucose, tight glycemic control is not indicated or appropriate during a crisis.
TABLE 2.
Recommendations for Diabetes Management During Humanitarian Crises
| Short Term (Days to Weeks) |
|---|
| Systematically identify patients with type 1 diabetes and prioritize insulin for this group. |
| Prioritize diabetes care for other vulnerable populations (pregnant women, the elderly, and those with complications from diabetes). |
| Ensure continuous access to essential medications. |
| Ensure that health centers and emergency kits are equipped with essential diabetes medications and diagnostic supplies. (See Table 1.) |
| Train humanitarian health care workers to handle insulin administration and diabetes emergencies. |
| Provide diabetes education for patients with a focus on hypoglycemia, sick-day guidelines, and medication management. |
| Long Term (Weeks to Months) |
| Ensure continuous access to essential medications. |
| Ensure that health centers have essential medications, supplies, and laboratory testing for A1C, lipids, creatinine, and microalbumin. |
| Provide comprehensive care for diabetes, hypertension, and CVD in primary health centers. |
| Provide comprehensive and culturally appropriate diabetes education for patients and their families. |
| Build local capacity by training HCPs on diabetes care. |
| Include access to insulin and diabetes care in national emergency response plans. |
| Further develop clinical guidelines for diabetes care during humanitarian crises. |
Medical relief organizations can update their emergency aid kits to include insulin vials (NPH, regular, and 70/30 premixed), syringes, and glucagon. Local health centers should be equipped with essential diabetes medications, glucose meters, test strips, and ketone strips. In addition, health care workers in the field should receive training on administration of insulin, as well as the management of diabetic emergencies such as hypoglycemia and DKA. It is encouraging that minimum standards for humanitarian care are now being revised to expand guidelines for management of chronic diseases (21). Finally, diabetes education at this stage should focus on medication management and sick-day guidelines (symptoms of DKA, hypoglycemia, and dehydration) rather than diet and lifestyle.
Long Term (Weeks to Months)
As crises become more prolonged in nature, there is a shift in priority for diabetes care. It is imperative that we provide comprehensive management of diabetes, hypertension, and CVD. In the long term, this is best accomplished by integrating diabetes care into primary health care so that both displaced and host populations may benefit. This requires investing in health systems to improve infrastructure, human resources, availability of insulin and medications, and accessibility of quality diabetes care for all.
There is an enormous strain on the health systems of countries that host a large number of refugees. Many countries face a shortage of health care workers with expertise in diabetes. Diabetes training programs for physicians and other HCPs are vital to build a diabetes workforce in countries affected by crisis. Academic health centers can play a leading role in the education and training of a diabetes workforce, and this can even be done remotely. It is also crucial to ensure that health care facilities have essential medications, testing supplies, and laboratory capability. In the future, the introduction of low-cost A1C testing and universal glucose test strips would be extremely beneficial in these resource-limited settings. National emergency response plans should include a strategy for diabetes care and for provision of insulin during a crisis. In addition, humanitarian organizations should ensure that staff members receive training in caring for patients with diabetes, and especially diabetic emergencies.
Diabetes education and support remain a cornerstone of treatment, and in the long term should be comprehensive and culturally appropriate, with an emphasis on nutrition and self-management skills. Attention to mental health is also crucial, as people with diabetes face very high levels of emotional distress during a crisis. Stress is a major risk factor for diabetes, and stress reduction can improve long-term glycemic control (22). Providing support through group diabetes education has been shown to be cost-effective and can also facilitate the development of meaningful social networks. Activating social networks can, in turn, promote healthy behaviors and improve diabetes management (23,24).
Other cost-effective interventions for management of type 2 diabetes include the use of metformin, statins, and ACE inhibitors, as well as screening for gestational diabetes, microalbuminuria, retinopathy, and diabetic foot conditions (25). These interventions can all be incorporated into long-term diabetes care plans. Digital health solutions for diabetes can also be introduced, as smartphone use is widespread among refugee families. A recent survey from the Zaatari camp in Jordan showed that 86% of youth owned a mobile handset, and more than half were using the Internet either once or multiple times per day (26). Finally, improved surveillance and data collection are needed to gain a better understanding of the needs of displaced populations and barriers to diabetes care. Global support and funding from governments, private organizations, academic centers, and philanthropic organizations are urgently needed to achieve these goals.
In summary, we must recognize the growing importance of chronic diseases during humanitarian crises. People with diabetes are faced with numerous obstacles in these settings. It is the responsibility of the international community across all sectors to rise and meet these challenges and promote the health and dignity of all people with diabetes during humanitarian response.
Duality of Interest
R.A.G. has been a consultant for Health Reveal and Onduo. No other potential conflicts of interest relevant to this article were reported.
Author Contributions
Y.K. contributed to the conception and writing of the manuscript, literature search, revision, and approval of the final version. N.A. and I.A. contributed to the writing of the manuscript, literature search, data collection, and data analysis. R.A.G. contributed to the writing of the manuscript and critically revised the work for intellectual content. Y.K. is the guarantor of this work and, as such, had full access to all the data presented and takes responsibility for the integrity and accuracy of the content.
References
- 1.United Nations High Commissioner for Refugees Figure at a glance. Available from www.unhcr.org/en-us/figures-at-a-glance.html. Accessed 4 April 2019
- 2.Fonseca V, Smith H, Kuhadiya N, et al. Impact of a natural disaster on diabetes: exacerbation of disparities and long-term consequences. Diabetes Care 2009;32:1632–1638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kishimoto M, Noda M. Diabetes care: after the great east Japan earthquake. J Diabetes Investig 2013;4:97–102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Albache N, Al Ali R, Rastam S, et al. Epidemiology of type 2 diabetes mellitus in Aleppo, Syria. J Diabetes 2010;2:85–91 [DOI] [PubMed] [Google Scholar]
- 5.International Diabetes Federation Middle East and North Africa. Available from www.idf.org/our-network/regions-members/middle-east-and-north-africa/members/48-syria.html. Accessed 4 April 2019
- 6.World Health Organization WHO helps diabetes patients in Syria. Available from www.who.int/en/news-room/feature-stories/detail/who-helps-diabetes-patients-in-syria. Accessed 4 April 2019
- 7.International Diabetes Federation IDF Diabetes Atlas. 8th ed. Available from www.diabetesatlas.org. Accessed 1 April 2018
- 8.United Nations High Commission for Refugees Vulnerability Assessment of Syrian Refugees in Lebanon - VASyR 2017. Available from data2.unhcr.org/en/documents/details/61312. Accessed 15 December 2018
- 9.Banjong O, Menefee A, Sranacharoenpong K, et al. Dietary assessment of refugees living in camps: a case study of Mae La Camp, Thailand. Food Nutr Bull 2003;24:360–367 [DOI] [PubMed] [Google Scholar]
- 10.United Nations Population Fund Worlds apart: reproductive health and rights in an age of inequality. Available from www.unfpa.org/sites/default/files/sowp/downloads/UNFPA_PUB_2017_EN_SWOP.pdf. Accessed 4 April 2019
- 11.Kherallah M, Alahfez T, Sahloul Z, et al. Health care in Syria before and during the crisis. Avicenna J Med 2012;2:51–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.United Nations High Commission for Refugees Health access and utilization survey: access to health services in Jordan among Syrian and non-Syrian refugees. Available from data2.unhcr.org/en/documents/download/62404. Accessed 4 April 2019
- 13.Holmes D. Chronic disease care crisis for Lebanon’s Syrian refugees. Lancet Diabetes Endocrinol 2015;3:102. [DOI] [PubMed] [Google Scholar]
- 14.Robert H. Diabetic Syrian refugee, 11, dies in her parents’ arms during sea crossing from Egypt to Italy after traffickers ‘destroy her insulin.’ Daily Mail 19 July 2015. Available from www.dailymail.co.uk/news/article-3167214. Accessed 4 April 2019
- 15.Doocy S, Lyles E, Roberton T, et al. Prevalence and care-seeking for chronic diseases among Syrian refugees in Jordan. BMC Public Health 2015;15:1097–2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Doocy S, Lyles E, Hanquart B, et al. Prevalence, care-seeking, and health service utilization for non-communicable diseases among Syrian refugees and host communities in Lebanon. Confl Health 2016;10:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.United Nations Relief and Works Agency for Palestine Refugees in the Near East. UNRWA Health Department Annual Report; 2012. Amman, Jordan, United National Relief and Works Agency for Palestinian Refugees in the Near East, 2013 [Google Scholar]
- 18.World Health Organization WHO model list of essential medicines, 2017. Available from www.who.int/medicines/publications/essentialmedicines/20th_EML2017.pdf. Accessed 4 April 2019 [DOI] [PubMed]
- 19.Tessier D, Dawson K, Tetrault JP, et al. Glibenclamide vs. gliclazide in type 2 diabetes of the elderly. Diabet Med 1994;11:974–980 [DOI] [PubMed] [Google Scholar]
- 20.Besançon S, Fall I, Doré M, et al. Diabetes in an emergency context: the Malian case study. Confl Health 2015;9:15–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sphere The Sphere Handbook: Humanitarian Charter and Minimum Standards in Humanitarian Response . (Standard 2.6). Available from handbook.spherestandards.org. Accessed 4 April 2019
- 22.Harris M, Oldmeadow C, Hure A, et al. Stress increases the risk of type 2 diabetes onset in women: a 12-year longitudinal study using causal modelling. PLoS One 2017;12:e0172126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zoughbie D, Rushakoff J, Watson K, et al. A social-network behavioral health program on sustained long-term body weight and glycemic outcomes: 2-year follow-up of a 4-month Microclinic Health Program in Jordan. Prev Med Rep 2018;13:160–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murphy A, Biringanine M, Roberts B, et al. Diabetes care in a complex humanitarian emergency setting: a qualitative evaluation. BMC Health Serv Res 2017;17:431–440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fernandes J, Zhang P. Cost-effective and cost-saving interventions for prevention and control of diabetes. Diabetes Voice 2016,62:16–20 [Google Scholar]
- 26.Maitland C, Xu Y. A social informatics analysis of refugee mobile phone use: a case study of Zaatari Syrian refugee camp. 2 April 2015. Available from papers.ssrn.com/sol3/papers.cfm?abstract_id=2588300 (doi: 10.2139/ssrn.2588300)