Abstract
Background
The isolated liner and head exchange procedure has been an established treatment method for polyethylene wear and osteolysis when the acetabular component remains well fixed. In this study, the mid-term results of this procedure were evaluated retrospectively.
Methods
Among the consecutive patients operated on from September 1995, two patients (three hips) were excluded because of inadequate follow-up, and the results of remaining 34 patients (34 hips) were evaluated. There were 20 men and 14 women with a mean age of 49 years. A conventional polyethylene liner was used in 26 cases and a highly cross-linked polyethylene liner was used in eight cases. In three cases, the liner was cemented in a metal shell because a compatible liner could not be used.
Results
After a follow-up of 5 to 20.2 years, re-revision surgery was necessary in 10 cases (29.4%): in eight for wear and osteolysis at 55 to 101 months after liner exchange and in two for acetabular loosening at 1 and 1.5 years after liner exchange. Re-revision surgery included all component revision (four cases), cup revision (four cases), and liner exchange (two cases). In all re-revision cases, a conventional polyethylene liner was used initially. There was no failure in the cases in which a highly cross-linked polyethylene liner was used.
Conclusions
The results of this study suggest that isolated acetabular liner exchange is a reasonable option for wear and osteolysis when the metal shell is well fixed. More promising long-term results are expected with the use of highly cross-linked polyethylene liners.
Keywords: Humerus, Fracture fixation, Bone screws
For decades, total hip arthroplasty has been the most necessary procedure conducted for various hip disorders including degenerative arthritis, rheumatoid arthritis, and osteonecrosis.1) However, the polyethylene liners of acetabular components can wear out, which occasionally leads to periprosthetic osteolysis that necessitates revision surgery despite the well-fixed acetabular component.2,3,4,5,6,7)
It has been debated whether it is better to exchange the liner only or revise all the acetabular components including the well-fixed metal shell.8) Considering surgical invasiveness, bone preservation, and patient recovery, the isolated liner and head exchange procedure has been accepted as an effective treatment method for polyethylene wear and osteolysis when the acetabular component remains well fixed. There have been reports of good short-term results of the procedure.9,10,11,12,13,14,15) However, the number of reports of mid- to long-term results is limited.16,17,18) In this study, we performed a retrospective analysis of the results at a minimum follow-up of 5 years.
METHODS
This retrospective case series study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. H-1703-054-837). Informed consent was waived. Between September 1995 and August 2012, isolated liner exchange with curettage and bone graft for osteolysis was performed in 37 consecutive cases (36 patients). Two patients (three hips) were excluded because of inadequate follow-up, and the remaining 34 patients (34 hips) were included in the final analysis. There were 20 men and 14 women with an average age of 49 years (range, 21 to 81 years) at the time of index surgery that was performed 3 to 21 years (mean, 10.1 years) after the previous surgery. This procedure was indicated for severe wear of the polyethylene liner or marked periprosthetic osteolysis despite the well-fixed acetabular metal shell. The acetabular metal shell was considered to be well fixed when the patient could bear weight without pain or discomfort and some portion of the bone ingrowth area remained intact on plain radiographs and computed tomography (CT) images.
The initial diagnosis was osteonecrosis of the femoral head in 15 cases, infection sequelae in 10, fused hip in five and miscellaneous in four. The index surgery was the first revision in 28 cases, second in five cases, and third in one case. Surgery was performed in the lateral decubitus position through a transtrochanteric approach in 18 cases, posterolateral approach in 12, and anterolateral approach in four. After removal of the worn polyethylene liner and screws, the stability of the metal shell was confirmed by forceful manipulation.
The osteolytic area was curetted out using curved curettes through screw holes and so was the cortical defect at the outer margin of the metal shell. In two cases, an additional cortical window was made for thorough curettage. The curetted cavity was filled with autogenous and allogenic cancellous chip bone grafts in the first three cases and only with allogenic bone grafts in the remaining cases. The replacement liner was made of conventional polyethylene in 26 cases and highly cross-linked polyethylene in eight cases. In three cases, the liner was cemented in the metal shell because a compatible liner could not be used.
After surgery, all patients were instructed to maintain the hip abduction position with limited flexion and walk with crutches without weight bearing for the first 6 weeks like after complete cup revision. Patients were evaluated clinically and radiographically at postoperative 6 weeks, 3 months, 9 months, and then annually. The follow-up period was 8.3 years on average (range, 5 to 20.2 years). Polyethylene liner wear was measured by the method of Scheier and Sandel19) on anteroposterior radiographs taken preoperatively and at the latest follow-up.
RESULTS
After a minimum follow-up of 5 years (range, 5 to 20.2 years), re-revision surgery was necessary in 10 cases (29.4%): eight for wear and osteolysis at 55 to 101 months after liner exchange (mean, 77 months) (Fig. 1) and two for acetabular loosening at 1 and 1.5 years after liner exchange (Fig. 2). Re-revision surgery included all component revision (four cases), cup revision (four cases), and liner exchange (two cases). In all re-revision cases, a conventional polyethylene liner was used. There was no failure in the cases in which a highly cross-linked polyethylene liner was used.
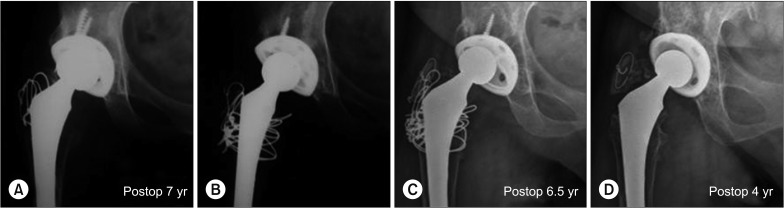
Fig. 1. A female patient who underwent total hip arthroplasty at the age of 32 years. (A) The anteroposterior radiograph taken at the 7-year follow-up demonstrates polyethylene wear and osteolysis. (B) The liner and head were exchanged. (C) At the 6.5-year follow-up after the liner and head exchange, the radiograph shows the worn-out polyethylene liner and osteolysis. (D) Anteroposterior radiograph taken at 4 years after re-revision surgery for liner and head exchange. Postop: postoperative.
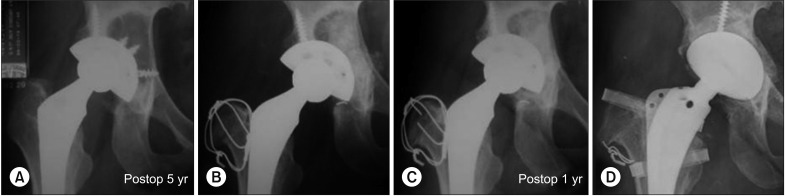
Fig. 2. A female patient who underwent total hip arthroplasty at the age of 31 years. (A) The radiograph taken at the 5-year follow-up shows polyehtylene wear and large osteolytic area. (B) Radiograph taken after liner and head exchange with bone graft. (C) At the 1-year follow-up after the liner and head exchange, the radiograph shows changes in cup position. (D) Anteroposterior radiograph taken after all component revision. Postop: postoperative.
Postoperative complications included greater trochanter nonunion in two cases, sciatic nerve palsy in one case, and heterotopic ossification in one case. One trochanteric nonunion was treated by open reduction and internal fixation and the other one was treated conservatively. Sciatic nerve palsy recovered gradually but not completely. There were no cases of dislocation. The average polyethylene wear rate was 0.28 mm per year before the index surgery. The wear rate of the replaced conventional polyethylene was 0.20 mm per year and that of the replaced highly cross-linked polyethylene was 0.02 mm per year on average.
DISCUSSION
In this study, re-revision was necessary in 10 out of 34 cases (29.4%). This re-revision rate is higher than those reported previously.16) However, we believe that this result is satisfactory because most re-revisions (eight cases) were performed because of wear and osteolysis again; even if revision of all acetabular components had been performed in these cases, re-revision would have been necessary.
There were two cases of loosening of the metal shell early after liner exchange. Early failure indicates that the preoperative evaluation on the stability of the metal shell was incorrect or inadequate. Mehin et al.20) recommended isolated polyethylene liner exchange when less than 50% of the circumference of the metal shell was affected by osteolysis on plain radiographs. However, evaluation on plain radiographs is not always clear and is known to underestimate the amount of osteolysis.21) Even on CT images, there are frequently limitations because of scattering. At present, a metal artifact reduction algorithm for orthopedic implants is used to analyze on CT scans. With the use of this algorithm, objective criteria for the evaluation of stability of the metal shell might be established.
Most studies reported a higher dislocation rate after isolated polyethylene liner exchange than after complete acetabular component revision, and dislocation was the most frequent cause of reoperation.22,23) In contrast to previous reports, there were no cases complicated by dislocation in this study, possibly owing to a strict postoperative care regimen.
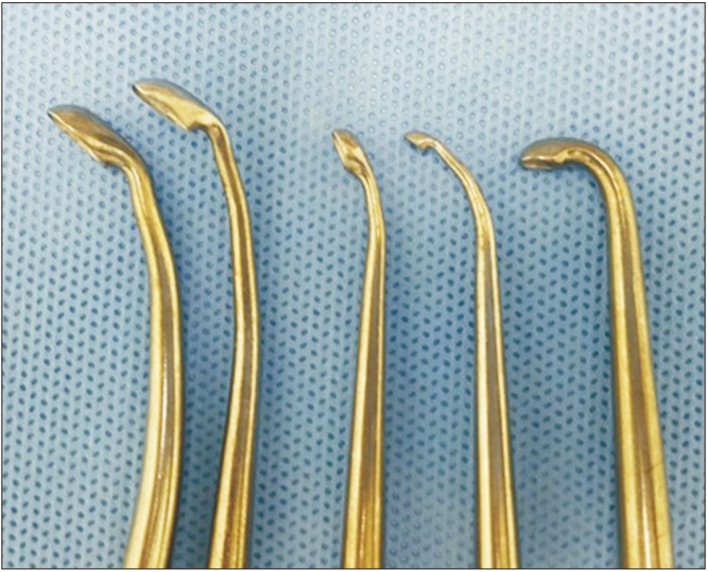
A limitation of this study is the retrospective evaluation of the relatively small number of cases. However, this study demonstrated a definite difference in the results between the use of conventional polyethylene and highly cross-linked polyethylene. Curettage and bone grafting through screw holes are time-consuming and tedious. Some studies reported the same results without bone grafting.5,7,13,24) Nevertheless, it is believed that bone grafting should be done for a future revision surgery. By using CT scanning, Egawa et al.25) found that a bone graft site was filled by about 50%. For this reason, they emphasized the necessity of developing proper tools for the bone graft procedure. In our cases, conventional curettes bent in various ways were used to make curettage easier (Fig. 3). For bone grafting, instruments named trumpets introduced by Chiang et al.2) would be helpful.
Fig. 3. Photograph of conventional curettes bent in various fashion.
In conclusion, the results of this study suggest that isolated acetabular liner exchange is a reasonable option for wear and osteolysis when the metal shell is well fixed. More promising long-term results are expected with the use of highly crosslinked polyethylene liners than liners made of conventional polyethylene.
ACKNOWLEDGEMENTS
This study was supported by a grant (06-03-0630) from Seoul National University Hospital.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Restrepo C, Ghanem E, Houssock C, Austin M, Parvizi J, Hozack WJ. Isolated polyethylene exchange versus acetabular revision for polyethylene wear. Clin Orthop Relat Res. 2009;467(1):194–198. doi: 10.1007/s11999-008-0533-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiang PP, Burke DW, Freiberg AA, Rubash HE. Osteolysis of the pelvis: evaluation and treatment. Clin Orthop Relat Res. 2003;(417):164–174. doi: 10.1097/01.blo.0000096816.78689.e5. [DOI] [PubMed] [Google Scholar]
- 3.Hamilton WG, Hopper RH, Jr, Engh CA, Jr, Engh CA. Survivorship of polyethylene liner exchanges performed for the treatment of wear and osteolysis among porous-coated cups. J Arthroplasty. 2010;25(6 Suppl):75–80. doi: 10.1016/j.arth.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Lombardi AV, Jr, Berend KR. Isolated acetabular liner exchange. J Am Acad Orthop Surg. 2008;16(5):243–248. doi: 10.5435/00124635-200805000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Maloney WJ, Paprosky W, Engh CA, Rubash H. Surgical treatment of pelvic osteolysis. Clin Orthop Relat Res. 2001;(393):78–84. doi: 10.1097/00003086-200112000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Naudie DD, Engh CA., Sr Surgical management of polyethylene wear and pelvic osteolysis with modular uncemented acetabular components. J Arthroplasty. 2004;19(4 Suppl 1):124–129. doi: 10.1016/j.arth.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 7.Schmalzried TP, Fowble VA, Amstutz HC. The fate of pelvic osteolysis after reoperation: no recurrence with lesional treatment. Clin Orthop Relat Res. 1998;(350):128–137. [PubMed] [Google Scholar]
- 8.Schmalzried TP, Guttmann D, Grecula M, Amstutz HC. The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994;76(5):677–688. doi: 10.2106/00004623-199405000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Deheshi BM, Allen DJ, Kim PR. Treatment of retroacetabular osteolysis with calcium sulfate and retention of original components. J Arthroplasty. 2008;23(8):1240.e9–1240.e12. doi: 10.1016/j.arth.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 10.Etienne G, Ragland PS, Mont MA. Use of cancellous bone chips and demineralized bone matrix in the treatment of acetabular osteolysis: preliminary 2-year follow-up. Orthopedics. 2004;27(1 Suppl):s123–s126. doi: 10.3928/0147-7447-20040102-08. [DOI] [PubMed] [Google Scholar]
- 11.Griffin WL, Fehring TK, Mason JB, McCoy TH, Odum S, Terefenko CS. Early morbidity of modular exchange for polyethylene wear and osteolysis. J Arthroplasty. 2004;19(7 Suppl 2):61–66. doi: 10.1016/j.arth.2004.06.014. [DOI] [PubMed] [Google Scholar]
- 12.Haidukewych GJ. Osteolysis in the well-fixed socket: cup retention or revision? J Bone Joint Surg Br. 2012;94(11 Suppl A):65–69. doi: 10.1302/0301-620X.94B11.30616. [DOI] [PubMed] [Google Scholar]
- 13.Maloney WJ, Herzwurm P, Paprosky W, Rubash HE, Engh CA. Treatment of pelvic osteolysis associated with a stable acetabular component inserted without cement as part of a total hip replacement. J Bone Joint Surg Am. 1997;79(11):1628–1634. doi: 10.2106/00004623-199711000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Stamenkov R, Neale SD, Kane T, Findlay DM, Taylor DJ, Howie DW. Cemented liner exchange with bone grafting halts the progression of periacetabular osteolysis. J Arthroplasty. 2014;29(4):822–826. doi: 10.1016/j.arth.2013.08.014. [DOI] [PubMed] [Google Scholar]
- 15.Walmsley DW, Waddell JP, Schemitsch EH. Isolated head and liner exchange in revision hip arthroplasty. J Am Acad Orthop Surg. 2017;25(4):288–296. doi: 10.5435/JAAOS-D-15-00144. [DOI] [PubMed] [Google Scholar]
- 16.Adelani MA, Mall NA, Nyazee H, Clohisy JC, Barrack RL, Nunley RM. Revision total hip arthroplasty with retained acetabular component. J Bone Joint Surg Am. 2014;96(12):1015–1020. doi: 10.2106/JBJS.L.01177. [DOI] [PubMed] [Google Scholar]
- 17.Beaule PE, Le Duff MJ, Dorey FJ, Amstutz HC. Fate of cementless acetabular components retained during revision total hip arthroplasty. J Bone Joint Surg Am. 2003;85(12):2288–2293. doi: 10.2106/00004623-200312000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Terefenko KM, Sychterz CJ, Orishimo K, Engh CA., Sr Polyethylene liner exchange for excessive wear and osteolysis. J Arthroplasty. 2002;17(6):798–804. doi: 10.1054/arth.2002.32705. [DOI] [PubMed] [Google Scholar]
- 19.Ilchmann T, Mjoberg B, Wingstrand H. Measurement accuracy in acetabular cup wear: three retrospective methods compared with Roentgen stereophotogrammetry. J Arthroplasty. 1995;10(5):636–642. doi: 10.1016/s0883-5403(05)80208-6. [DOI] [PubMed] [Google Scholar]
- 20.Mehin R, Yuan X, Haydon C, et al. Retroacetabular osteolysis: when to operate? Clin Orthop Relat Res. 2004;(428):247–255. [PubMed] [Google Scholar]
- 21.Suh DH, Han SB, Yun HH, Chun SK, Shon WY. Characterization of progression of pelvic osteolysis after cementless total hip arthroplasty: computed tomographic study. J Arthroplasty. 2013;28(10):1851–1855. doi: 10.1016/j.arth.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 22.Boucher HR, Lynch C, Young AM, Engh CA, Jr, Engh C., Sr Dislocation after polyethylene liner exchange in total hip arthroplasty. J Arthroplasty. 2003;18(5):654–657. doi: 10.1016/s0883-5403(03)00266-3. [DOI] [PubMed] [Google Scholar]
- 23.Lie SA, Hallan G, Furnes O, Havelin LI, Engesaeter LB. Isolated acetabular liner exchange compared with complete acetabular component revision in revision of primary uncemented acetabular components: a study of 1649 revisions from the Norwegian Arthroplasty Register. J Bone Joint Surg Br. 2007;89(5):591–594. doi: 10.1302/0301-620X.89B5.18623. [DOI] [PubMed] [Google Scholar]
- 24.O'Brien JJ, Burnett RS, McCalden RW, MacDonald SJ, Bourne RB, Rorabeck CH. Isolated liner exchange in revision total hip arthroplasty: clinical results using the direct lateral surgical approach. J Arthroplasty. 2004;19(4):414–423. doi: 10.1016/j.arth.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 25.Egawa H, Ho H, Huynh C, Hopper RH, Jr, Engh CA, Jr, Engh CA. A three-dimensional method for evaluating changes in acetabular osteolytic lesions in response to treatment. Clin Orthop Relat Res. 2010;468(2):480–490. doi: 10.1007/s11999-009-1050-0. [DOI] [PMC free article] [PubMed] [Google Scholar]