Abstract
The inflammasome is a multiprotein complex assembled in response to Pathogen Associated Molecular Patterns (PAMPs) and Danger Associated Molecular Patterns (DAMPs). Inflammasome activation occurs through a two-step mechanism, with the first signal facilitating priming of inflammasome components while the second signal triggers complex assembly. Once assembled, the inflammasome recruits and activates pro-caspase-1, which in turn processes pro-interleukin (IL)-18 and pro-IL-1β into their bio-active forms. Owing to its key role in the regulation of innate immune responses, the inflammasome has emerged as a therapeutic target for the treatment of inflammatory conditions. In this study we demonstrate that IRE1α, a key component of the Unfolded Protein Response, contributes to assembly of the NLRP3 inflammasome. Blockade of IRE1α RNase signaling lowered NLRP3 inflammasome assembly, caspase-1 activation and pro-IL-1β processing. These results underscore both the importance and potential therapeutic relevance of targeting IRE1α signaling in conditions of excessive inflammasome formation.
Subject terms: Stress signalling, Inflammasome
Introduction
Protein folding and processing of transmembrane and secretory proteins occur within the endoplasmic reticulum (ER). Exposure to physiological or pathological conditions, such as infections, nutrient deprivation, or hypoxia, reduces the ability of the ER to function leading to a build-up of unfolded or misfolded proteins—a condition referred to as ER stress. The accumulation of unfolded/misfolded proteins activates three ER-anchored transmembrane receptors—inositol-requiring enzyme 1α (IRE1α)1,2, protein kinase RNA (PKR)-like ER kinase (PERK)3, and activating transcription factor-6 (ATF6)4—triggering a signaling cascade termed the unfolded protein response (UPR). The UPR is an evolutionarily conserved stress response pathway tasked with reducing levels of unfolded/misfolded proteins and returning homeostasis to the ER5.
IRE1α, a bifunctional transmembrane protein comprised of both a serine/threonine kinase domain and an endoribonuclease (RNase) domain, is the most evolutionarily conserved UPR sensor present in all eukaryotes. Similar to PERK and ATF6, the N-terminus of IRE1α juts into the ER lumen where, under nonstress conditions, it associates with the ER chaperone glucose-regulated protein 78 (Grp78)6. Accumulation of unfolded proteins initiates Grp78 dissociation from IRE1α permitting IRE1α dimerization and trans-autophosphorylation leading to activation of its RNase domain. IRE1α RNase activity has two principal outputs; splicing of a 26-nucleotide intron from X-box binding protein 1 (XBP1) mRNA7 and IRE1α-dependent decay of mRNA (RIDD), the sequence specific cleavage of non-XBP1 mRNAs and selected miRNAs localized to the ER membrane8,9. Splicing of XBP1 mRNA leads to the translation of a stable transcription factor termed XBP1s, which regulates expression of ER chaperones and components of the ER-associated degradation machinery thus enhancing the capacity of the ER to reduce unfolded/misfolded proteins10,11.
Although IRE1α has a well-established role in the UPR, its influence may extend beyond monitoring ER homeostasis. IRE1α signaling has been demonstrated to contribute to the development of several immune cell types, including secretory plasma cells12 and dendritic cells13. IRE1α-mediated regulation of macrophage polarization under conditions of metabolic stress has also been reported14. In addition to immune cell development, several studies have also demonstrated that IRE1α-XBP1 signaling contributes to innate immune responses triggered by various toll-like receptor (TLR) ligands including lipopolysaccharide (LPS)15, attenuated Brucella abortus strain16 and Methicillin-resistant Staphylococcus aureus (MRSA) infection17. Furthermore, IRE1α activity was also shown to be upregulated in inflammatory arthritis18 as well as in lipid-induced inflammation19.
In this study, we examined the contribution of IRE1α RNase activity to inflammasome formation and in particular the nucleotide-binding oligomerization domain, leucine rich repeat and pyrin domain containing 3 (NLRP3) inflammasome. Structurally, the NLRP3 inflammasome is composed of three components—NLRP3 that functions as a sensor protein; the adapter apoptosis-associated speck-like protein containing a caspase recruitment domain (ASC) and pro-caspase-120. Activation is achieved via a two-step mechanism with the first step (priming step) involving transcriptional upregulation of key components including NLRP3 as well as pro-IL-1β through TLR activation and subsequent NF-κB signaling21,22. The second step (signal II) promotes NLRP3 inflammasome assembly and activation. The precise mechanisms facilitating NLRP3 inflammasome activation remain unclear with several models proposed23–25. Ultimately, signal II enables structural assembly of the inflammasome with NLRP3 recruiting ASC via pyrin:pyrin domain interactions, which in turn triggers ASC oligomerisation leading to the formation of long ASC filaments26. Pro-caspase-1 is recruited to ASC via CARD:CARD interactions leading to auto-processing resulting in the generation of activate caspase-1.
We now report that inhibition of IRE1α RNase activity, while not impacting on inflammasome priming, selectively reduces structural assembly of the inflammasome. This suggests that small molecule inhibitors of IRE1α RNase activity may offer a new therapeutic opportunity for diseases mediated by excessive or prolonged NLRP3 inflammasome activity.
Material and methods
Antibodies and reagents
Primary antibodies used were as follows: mouse anti-XBP1s (Biolegend, 647502), rabbit anti-IRE1 (Cell Signaling, 3294), rabbit anti-PERK (Cell Signaling Technology, 3192), rabbit anti-eIF2α (Cell Signaling Technology, 5324), rabbit anti-p(S51)-eIF2α (Cell Signaling Technology, 3398), mouse anti-ATF6 (CosmoBio, BAM-73-500-EX), rabbit anti-NLRP3 D2P5E (Cell signaling technology, 13158), rabbit anti-NF-κB p65 (D14E12) (Cell signaling technology, 8242), mouse anti-IL-1β (R&D Systems, MAB601), rabbit anti-ASC (Santa Cruz, sc-22514-R), rabbit anti-caspase 1 (Santa Cruz, sc-622), rabbit anti-caspase-1 p10 (Santa Cruz, sc-515), TXNIP (Santa Cruz, sc-166234), and rabbit anti-Actin (Sigma, A2066). Secondary antibodies were horseradish peroxidase-tagged goat anti-mouse (Jackson Laboratories, 115-035-003) and goat anti-rabbit antibodies (Jackson Laboratories, 111-035-003). Tunicamycin (T7765), Phorbol 12-myristate 13-acetate (PMA) (P8139), LPS (L2630), and ATP (A6419) were purchased from Sigma-Aldrich while nigericin (tlrl-nig) was obtained from Invivogen. IRE1 inhibitor MKC8866 was provided by Fosun Orinove.
Cell culture
THP-1 cells were purchased from ATCC and cultured in RPMI 1640 media (Sigma, R0883) supplemented with 10% heat-inactivated fetal bovine serum (Sigma, F7524) and 2 mM l-glutamine (Sigma, G7513). Blood sampling of healthy volunteers was carried out following informed consent at the National University of Ireland, Galway (NUI Galway) under a protocol entitled “Immunological research using healthy human blood cells” approved by the NUIG Research Ethics Committee on 30/4/14 (Protocol no. 14/MAR/01). Human peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll-Hypaque density gradient centrifugation from freshly drawn EDTA-anticoagulated peripheral venous blood. Briefly, 3 ml aliquots of EDTA-anticoagulated peripheral venous blood was layered over 3 ml of Ficoll Paque Plus (Sigma, GE17-1440-02) in a 15 ml tube and centrifuged at 400 × g for 22 min at 4 °C. The thin cloudy layer of PBMCs present at the interface of plasma and red blood cell layers was removed and transferred to a fresh 15 ml tube. The PBMCs were washed in 10 ml FACS buffer (2% fetal calf serum, PBS and 0.05% NaN3) and were pelleted by centrifugation at 300 × g for 10 min at 4 °C. The supernatant was discarded and the cell pellet was resuspended in 5 ml FACS buffer and washed a second time using the same protocol. The final cell pellet was resuspended in 1 mL FACS buffer and counted using a haemocytometer. Freshly isolated PBMCs were diluted in complete media containing RPMI‐1640 (Sigma, R0883) supplemented with 1% l‐glutamine (Sigma, G7513) 100 U/ml penicillin/100 mg/ml streptomycin (Sigma, P0781) and 5% clotted male human AB serum (Sigma, H6914). All cells were grown at 37 °C and 5% CO2.
Transfections
Prior to transfection THP-1 cells were treated with PMA (50 ng/ml) for 24 h following which they were transfected with siRNA using TransIT-TKO (Mirus, MIR 2154) and according to the manufacturer’s protocol. siRNAs (ON-TARGET plus smart pool) ERN1/IRE1 (L-004951-02-0005); non-coding siRNA (D-001810-10-20) was obtained from Dharmacon. The media was changed 6 h post transfection and cells were left to recover for 72 h.
Inflammasome activation
THP-1 cells were plated in six-well plates at a density of 1 × 106 cells/ml and treated with 1 μg/ml LPS with or without IRE1 inhibitor MKC8866 (20 μM) for 24 h. After 24 h, LPS primed cells were treated with 10 μM nigericin for 45 min following which cells and conditioned medium were collected for analysis. To suppress NLRP3 inflammasome activation, 100 mM KCl was added to the culture medium at the time of LPS addition. For inflammasome activation, PBMCs were plated at a density of 1 × 106 cells/ml and primed with 0.5 ng/ml LPS for 2 h in the presence or absence of MKC8866 (20 μM). After 2 h of priming 5 mM ATP was added for 45 min and cells and conditioned medium were collected for analysis.
ASC crosslinking
Following treatment THP-1 cells were resuspended in 500 μl of ice-cold buffer (20 mM HEPES-KOH, pH 7.5, 150 mM KCl, 1 mM Na3VO4, 0.1 mM PMSF, 1% NP-40, and a protease inhibitor cocktail) and lysed by shearing ten times using a 21 gauge needle. Lysates were centrifuged at 300 × g for 5 min at 4 °C. Supernatants were filtered through a 5 μM filter (GE Healthcare, 6784-1350). Filtrates were centrifuged at 6800 × g for 15 min at 4 °C to pellet ASC-insoluble specks. Supernatants were transferred to new tubes (ASC-soluble fractions). The ASC-insoluble pellets were washed with PBS twice and then suspended in 200 μl PBS. The ASC-insoluble pellets were cross-linked at room temperature for 30 min by adding 2 mM bis[sulfosuccinimidy]suberate (BS3). The solutions were then centrifuged at 6800 × g for 15 min at 4 °C to pellet the cross-linked ASC which was then dissolved directly in SDS sample buffer.
Caspase-1 activity assay
THP-1 cells were treated as indicated and whole-cell caspase-1 activity was determined using the FLICA 660 in vitro Caspase-1 detection Kit (Immunochemistry Technologies, 9122) by the use of flow cytometry. Cell suspensions were aliquoted into 96‐well flat‐bottom cell culture plates at a final concentration of 1 × 106 cells/ml in complete medium and a total incubation volume of 200 μl. At the time of signal II addition, 10 μl of FLICA reagent (reconstituted as directed by manufacturer and diluted to 1:10 in FACS buffer 5 min prior to staining) was added to each well. The cells were incubated for 45 min at 37 °C, 5% CO2 then washed using 1 ml PBS and pelleted by centrifugation at 300 × g for 5 min at 4 °C. Live cells were analysed on a BD Accuri C6 Flow Cytometer (BD Biosciences).
Cytokine analysis
Conditioned medium was collected from treated THP-1 cells and PBMCs and assayed for cytokines using sandwich ELISA according to the manufacturer’s instructions (DuoSet, R&D Systems). Cytokines analysed included IL-1β (DY201-05), TNF-α (DY210-05), IL-6 (DY206-05), and CXCL8/IL-8 (DY208-05).
RNA extraction, PCR and Q-PCR
RNA extraction from THP-1 cells and PBMCs was performed using the RNeasy micro kit (Qiagen) according to the manufacturer’s protocol, and cDNA was generated from 250 ng of RNA using Superscript III first strand RT-PCR system and random hexamers (Invitrogen). Semiquantitative RT-PCR was performed using GoTaq green master mix (Promega, M7123) with primers specific for XBP1s (Forward: 5′-TCTGCTGAGTCCGCAGCAGG-3′ and reverse: 5′-CTCTAAGACTAGAGGCTTGG-3′) and the endogenous control GAPDH (Forward: 5′-ACCACAGTCCATGCCATC-3′ and reverse: 5′-TCCACCACCTGTTGCTG-3′). Q-PCR reactions were performed using Takyon ROX Master Mix (Eurogentec UFRP5XC0501) and the StepOne Plus platform (Applied Biosystems). Target transcript levels were normalized to GAPDH, and relative abundance was determined using the ΔΔCt method. Transcript-specific TaqMan assays were purchased from Integrated DNA Technologies. The sequences of primers and probes used are detailed in the table below.
| NLRP3 |
| Probe: 5′-TGCAGGTTACACTGTGGATTCTTGGC-3′ |
| Primer 1: 5′-AGATTCTGATTAGTGCTGAGTACC-3′ |
| Primer 2: 5′-GAATGCCTTGGGAGACTCAG-3′ |
| IL-1β |
| Probe: 5′-AGAAGTACCTGAGCTCGCCAGTGA-3′ |
| Primer 1: 5′-GAACAAGTCATCCTCATTGCC-3′ |
| Primer 2: 5′-CAGCCAATCTTCATTGCTCAAG-3′ |
| Caspase-1 |
| Probe: 5′-AGTCTTCCAATAAAAACAGAGCCCATTGTG-3′ |
| Primer 1: 5′-CACATCACAGGAACAGGCATA-3′ |
| Primer 2: 5′-TGAAGGACAAACCGAAGGTG-3′ |
| TXNIP |
| Probe: 5′ TTGCGGAGTGGCTAAAGTGCTTTG-3′ |
| Primer 1: 5′-GTGATAGTGGAGGTGTGTGAAG-3′ |
| Primer 2: 5′-CAGGTACTCCGAAGTCTGTTTG-3′ |
| GAPDH |
| Probe: 5′-AAGGTCGGAGTCAACGGATTTGGTC-3′ |
| Primer 1: 5′-ACATCGCTCAGACACCATG-3′ |
| Primer 2: 5′-TGTAGTTGAGGTCAATGAAGGG-3′ |
Immunoblotting
Protein samples lysed in 1× SDS-PAGE (2% sodium dodecyl sulfate (SDS), 50 mM Tris-HCl pH 6.8, 5% glycerol, 0.05% bromphenol blue, 357 mM β-mercaptoethanol) or RIPA (0.1% SDS, 1% NP-40, 0.5% sodium deoxycholate, 50 mM Tris-HCl pH 8.8, 150 mM NaCl) buffer were separated by SDS-PAGE and blotted onto nitrocellulose membranes (Amersham). Membranes were blocked with 5% nonfat dry milk in PBS-0.1% Tween 20 and then incubated at 4 °C overnight with primary antibodies specified above. Next day membranes were incubated with corresponding secondary horseradish peroxidase or IRDye–conjugated antibodies for 1 h at room temperature and bands were visualized using ECL Western blotting detection reagents (Amersham, GE Healthcare) or scanned using the Odyssey Infrared Imaging System (Li-Core Biosciences).
Propidium iodide assessment of cell death
THP-1 cells were plated in a 12-well plate at a density of 1 × 106 cells/ml and treated with 1 μg/ml LPS with or without indicated concentrations of MKC8866 for 24 h. After 24 h, LPS primed cells were treated with 10 μM nigericin for 45 min prior to cell death analysis. Cells were pelleted at 4000 × g for 5 min and resuspended in 100 μl of ice-cold PBS. Five minutes prior to analysis, 1.5 μg/ml Propidium Iodide (PI) (Sigma, P4170) was added and PI uptake analysed using BD Accuri C6 flow cytometer (BD Biosciences).
Statistical analysis
Data are expressed as mean ± SD for at least three independent experiments. Statistical analysis was performed using GraphPad Prism (GraphPad Software, San Diego, CA). Significance was determined using a Student’s t test, with P < 0.05 being considered significant and annotated by *P < 0.05, **P < 0.001, ***P < 0.0001, and ****P < 0.00001.
Results
IRE1α RNase activity is selectively activated upon TLR4 stimulation
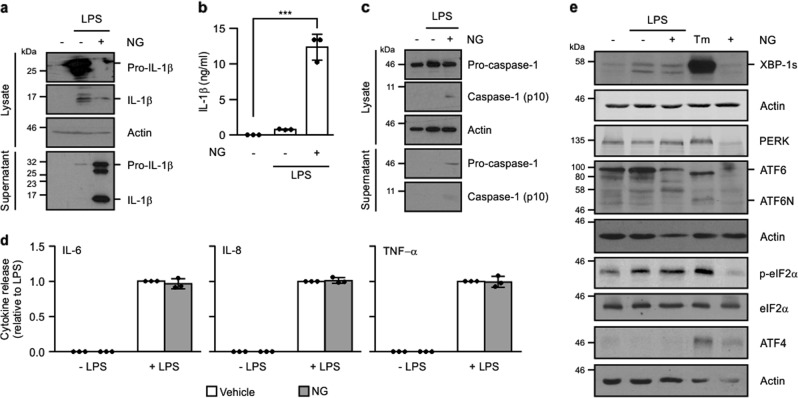
The human monocytic cell line, THP-1, was treated with LPS (signal I) alone or LPS followed by a brief incubation with the K+ ionophore, nigericin (signal II) to stimulate NLRP3 inflammasome assembly. Addition of nigericin enhanced processing and secretion of pro-IL-1β compared with cells treated with LPS alone (Fig. 1a, b). Likewise, a similar increase in pro-caspase-1 processing was observed following nigericin addition confirming inflammasome formation (Fig. 1c). Nigericin addition did not alter levels of IL-6, IL-8, or TNF-α in LPS-treated THP-1 cell conditioned medium (Fig. 1d).
Fig. 1. IRE1α-XBP1 axis of the UPR is selectively activated upon TLR4 stimulation.
THP-1 cells were primed with either 1 μg/ml LPS alone for 24 h or 1 μg/ml LPS for 24 h followed by addition of 10 μM nigericin (NG) for 45 min. a Processing of pro-IL-1β was analysed in cell lysates and conditioned medium by immunoblotting for full-length pro-IL-1β and processed p17 IL-1β. b Levels of IL-1β were quantified in conditioned medium from untreated, LPS, LPS and NG-treated THP-1 cells by ELISA (n = 3). c Processing of caspase-1 was analysed in cell lysates and conditioned medium by immunoblotting for pro-caspase-1 and processed p10 caspase-1. d IL-6, IL-8, and TNF-α levels were quantified in conditioned medium from untreated, LPS, LPS and NG, and NG-only treated THP-1 cells by ELISA (n = 3). e UPR markers XBP1s, PERK, ATF6, phospho-eIF2α, total eIF2α, and ATF4 were analysed by immunoblotting in THP-1 post treatment with LPS alone or LPS and NG. Tunicamycin (Tm)-treated THP-1 cells served as a positive control for the UPR activation. Actin was used as a loading control. ***P < 0.001 based on a Student’s t test. Error bars represent SD.
To determine if UPR signaling was triggered during inflammasome formation we assessed activation of IRE1α, PERK, and ATF6 in THP-1 cells following LPS and LPS/nigericin treatment. In agreement with published data15, IRE1α activation, as determined by XBP1 splicing, was detected by immunoblotting in cell lysates following both LPS and LPS/nigericin treatment (Fig. 1e). Activation of ATF6 or PERK arms of the UPR was not detected following treatment with either LPS alone or with LPS/nigericin. However, processing of ATF6 as signified by the appearance of amino terminal fragment of ATF6 (ATF6N), and PERK activation (as indicated by an upshift in PERK molecular weight, indicative of phosphorylation, and induction of ATF4 expression) was readily detected following treatment with tunicamycin, a pharmacological inducer of ER stress (Fig. 1e). Collectively, these results indicate that (a) addition of nigericin post-LPS treatment stimulates inflammasome formation in THP-1 cells and (b) LPS treatment leads to selective activation of the IRE1α branch of the UPR.
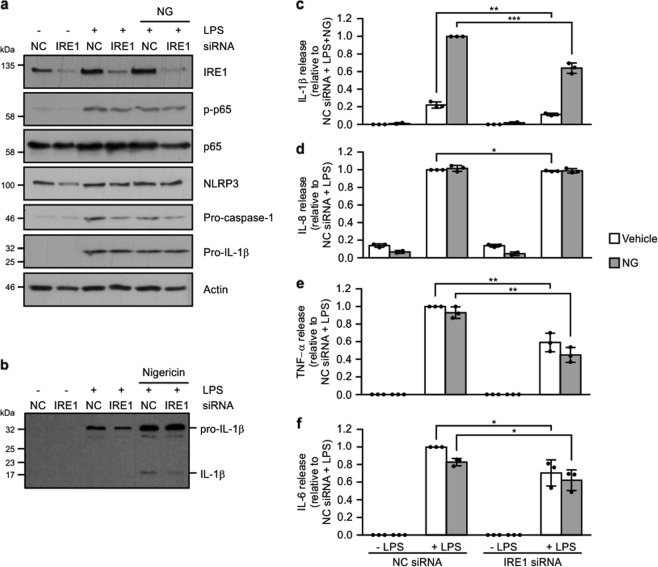
IRE1α signaling contributes to LPS/nigericin inflammasome activity
To determine if IRE1α signaling actively contributes to NLRP3 inflammasome formation, or if it was merely a by-stander effect due to TLR4 activation, we transiently transfected THP-1 cells with siRNA targeting IRE1α. Efficient knockdown of IRE1α was verified by western blotting 72 h after siRNA transfection (Fig. 2a). Knockdown of IRE1α significantly reduced processing of pro-IL-1β and secretion of p17 IL-1β (Fig. 2b, c). In agreement with previous results15 assessment of IL-6 and TNF-α levels also indicated a role for IRE1α signaling with reduced IL-6 and TNF-α evident in conditioned medium from both LPS and LPS/nigericin-treated IRE1α siRNA transfected cells compared with their noncoding counterparts (Fig. 2d–f).
Fig. 2. Knockdown of IRE1α reduces LPS-induced cytokine production.
THP-1 cells transfected with either noncoding (NC) or IRE1α targeting siRNA were treated with either 1 μg/ml LPS alone for 24 h or 1 μg/ml LPS for 24 h followed by addition of 10 μM nigericin (NG) for 45 min. a Cell lysates were analysed via immunoblotting for IRE1α, phospho-p65, total p65, NLRP3, pro-caspase-1 and pro-IL-1β. Actin was used as a loading control. b Cell conditioned medium was analysed via immunoblotting for pro-IL-1β processing. c–f Levels of IL-1β, IL-8, TNF-α, and IL-6 were assayed in cell conditioned medium by ELISA (n = 3). *P < 0.05, **P < 0.01, and ***P < 0.001 based on a Student’s t test. Error bars represent SD.
Recent reports have linked IRE1α, through its kinase activity, to initiation of NF-κB signaling27. Given the importance of NF-κB activation in mediating inflammasome activation we asked if knockdown of IRE1α dampened NF-κB signaling and, through this mechanism, reduced priming of essential components of the inflammasome such as NLRP3. While addition of LPS or LPS/nigericin clearly triggered NF-κB activation, as determined by an increase in phospho-p65 levels (Fig. 2a), this was not altered by IRE1α knockdown.
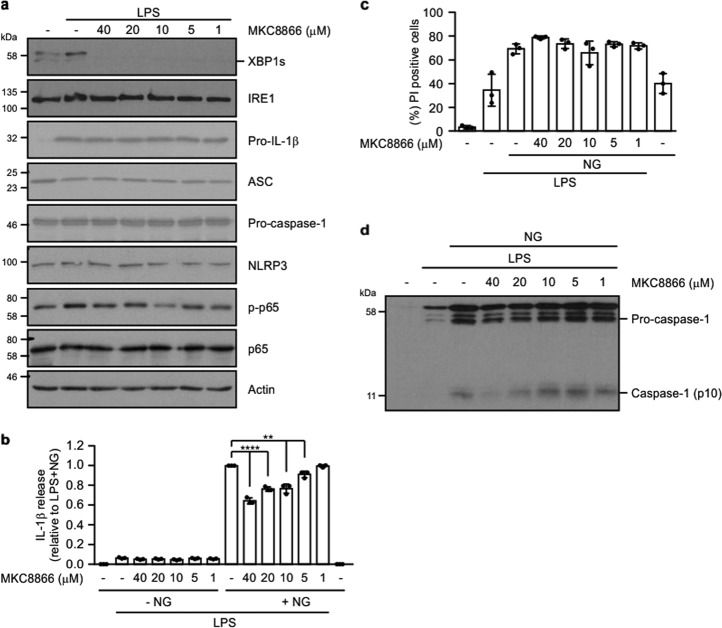
Owing to its structure and mode of activation IRE1α represents a druggable target. Indeed, over the past 6 years, a number of small molecule inhibitors selectively targeting IRE1α RNase activity have been reported. One such inhibitor, the salicylaldehyde analog MKC8866, is a selective, noncompetitive, potent, and reversible inhibitor of IRE1α RNase activity28. Treatment of THP-1 cells with MKC8866 efficiently abolished LPS-induced activation of IRE1α RNase signaling as demonstrated by a clear reduction in XBP1 splicing (Fig. 3a). Similar to IRE1α knockdown, MKC8866 significantly reduced levels of secreted IL-1β post-LPS/nigericin treatment in a dose-dependent manner (Fig. 3b).
Fig. 3. MKC8866 reduces LPS-induced IRE1α signaling and suppresses NLRP3 inflammasome activation.
a THP-1 cells were treated with 1 μg/ml LPS alone or in combination with indicated concentrations of IRE1α inhibitor (MKC8866) for 24 h following which cell lysates were collected and analysed via immunoblotting for XBP1s, IRE1α, pro-IL-1β, ASC, pro-caspase-1, NLRP3, phospho-p65 and total p65. Actin was used as a loading control. b Conditioned medium from THP-1 cells treated with 1 μg/ml LPS alone or in combination with 10 μM nigericin (NG) in the presence or absence of indicated concentrations of MKC8866 were analysed by ELISA for IL-1β secretion (n = 3). c Propidium iodide (PI) uptake was assessed in THP-1 cells following treatment with 1 μg/ml LPS alone or in combination with 10 μM nigericin (NG) plus the indicated concentrations of MKC8866 (n = 3). d Conditioned medium from b was immunoblotted for pro- and cleaved caspase-1. **P < 0.01 and ****P < 0.0001 based on a Student’s t test. Error bars represent SD.
Recent reports have suggested that release of IL-1β from cells following NLRP3 inflammasome activation is facilitated by signal II-induced cell death29. Based on these reports, we asked if the reduced IL-1β levels we observed in the conditioned medium of LPS/MKC8866/nigericin-treated THP-1 cells could be a consequence of decreased cell death. To answer this we assessed cell death, via propidium iodide (PI) uptake, in THP-1 cells treated with LPS alone or in combination with MKC8866. In agreement with recently published data29, we observed increased cell death following addition of signal II (nigericin) in LPS-stimulated cells. However, the level of cell death observed was similar in those cells treated with LPS alone and a combination of LPS and MKC8866 (Fig. 3c). This suggests that the reduced IL-1β levels we observed upon IRE1α inhibition is not a consequence of reduced cell death.
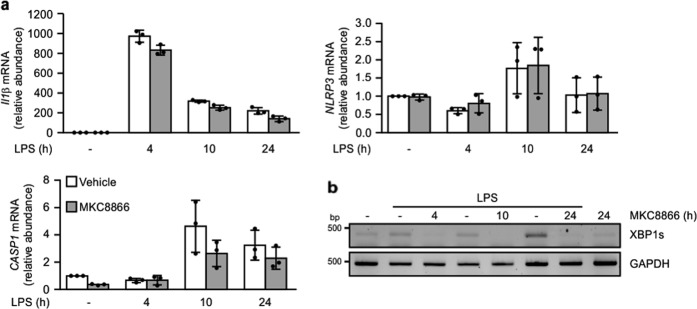
Processing of pro-capsase-1 is a hallmark of NLRP3 inflammasome formation. Analysis of processed (p10) caspase-1 in conditioned medium from LPS/nigericin-treated THP-1 cells revealed a dose-dependent reduction associated with addition of MKC8866 (Fig. 3d). To understand how inhibition of IRE1α RNase activity reduced caspase-1 processing, we examined LPS-mediated regulation of inflammasome components in the presence and absence of MKC8866. Examination of pro-IL-1β, pro-caspase-1, ASC and NLRP3 protein expression in the lysate of LPS/nigericin-treated cells with and without MKC8866 did not show any alterations in their expression (Fig. 3a). In addition, we also examined transcript levels of each component over a 24 h LPS treatment. Following 4 h treatment with LPS, increases in pro-IL-1β transcript levels were apparent. By 10 h, elevated levels of NLRP3 and pro-caspase-1 transcripts were also observed verifying priming of the inflammasome (Fig. 4a). Similar to the results for protein expression, we observed no alteration in the transcript levels of pro-IL-1β, pro-caspase-1, ASC and NLRP3 upon MKC8866 addition (Fig. 4a). In contrast, there was a clear reduction in XBP1s expression, verifying MKC8866 functionality (Fig. 4b). This suggests that the suppression in pro-caspase-1 processing observed upon inhibition of IRE1α RNase activity is not a consequence of reduced expression of principal inflammasome components.
Fig. 4. Addition of MKC8866 does not impact upon LPS-mediated increases in CASP1, IL1β, or NLRP3 transcript.
THP-1 cells were treated with 1 μg/ml LPS in the presence or absence of 20 μM MKC8866 for the indicated times after which RNA was extracted. a Q-PCR was carried out to assess relative expression of IL1β and NLRP3 and CASP1 transcripts (n = 3). Error bars represent SD. b RT-PCR was carried out to assess XBP1 splicing and GAPDH mRNA expression.
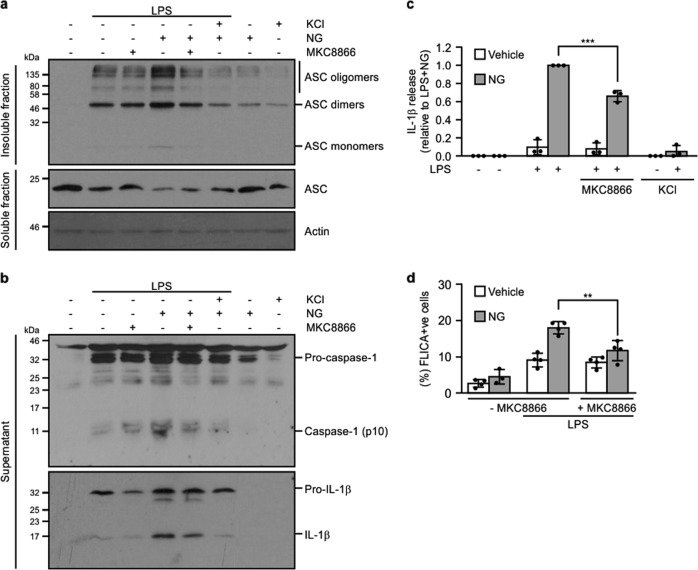
Addition of MKC8866 reduces LPS/nigericin-induced inflammasome formation
To determine if the decreased pro-caspase-1 processing and pro-IL1β processing observed upon IRE1α inhibition was a consequence of reduced assembly of the inflammasome complex, we assessed ASC oligomerisation following LPS and LPS/nigericin treatment in the presence and absence of MKC8866. Treatment of THP-1 cells with LPS/nigericin triggered an increase in ASC oligomerization compared with LPS alone highlighting the need for signal II to potentiate inflammasome formation (Fig. 5a). As previously reported23, inclusion of high extracellular K+ negated the ability of nigericin to enhance ASC oligomerization (Fig. 5a). While combination with MKC8866 substantially reduced ASC oligomerization, it was not to the extent observed with high extracellular K+ (Fig. 5a). Analysis of IL-1β levels in conditioned medium revealed a similar pattern with addition of high extracellular K+ completely suppressing IL-1β processing with a significant but not complete inhibition observed upon addition of MKC8866 (Fig. 5b, c).
Fig. 5. Addition of MKC8866 reduces NLRP3 inflammasome assembly.
THP-1 cells were treated with either 1 μg/ml LPS alone or in combination with 20 μM MKC8866 for 24 h followed by addition of 10 μM nigericin (NG) alone or in combination with 100 mM KCl for 45 min after which cells and conditioned medium were harvested. Immunoblotting was used to determine a ASC oligomerization status and b caspase-1 (pro- and cleaved p10) and IL-1β processing. c IL-1β levels were quantified by ELISA in THP-1 conditioned medium following indicated treatments (n = 3). d The percentage of THP-1 cells displaying caspase-1-like activity following the indicated treatments was assessed by the FLICA assay (n = 4). **P < 0.01 and ***P < 0.001 based on a Student’s t test. Error bars represent SD.
Following ASC oligomerization pro-caspase-1 is recruited to the inflammasome via CARD:CARD interactions resulting in the generation of active caspase-1 thus enabling pro-IL-1β processing. Any suppression in inflammasome formation would be expected to correlate with a decrease in caspase-1-like activity. Examination of pro-caspase-1 processing via western blotting demonstrated reduced p10 caspase-1 present in the conditioned medium of those THP-1 cells treated with LPS/nigericin plus MKC8866 or 100 mM KCl compared with those treated with LPS/nigericin alone (Fig. 5b). Similarly, addition of MKC8866 efficiently suppressed intracellular caspase-1 like activity as assessed by a flow cytometry-based FLICA assay in LPS/nigericin-treated cells (Fig. 5d). Collectively, these results indicate that selective inhibition of IRE1α RNase activity in THP-1 cells diminishes assembly of the NLRP3 inflammasome and, thereby, reduces processing of pro-IL-1β and release of active p17 IL-1β.
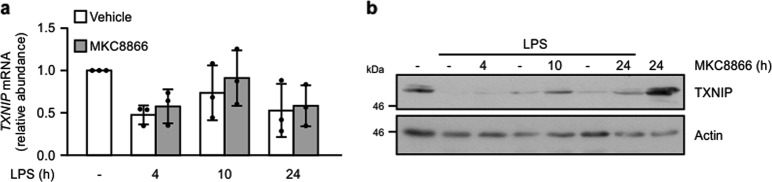
Thioredoxin interacting protein (TXNIP) has been demonstrated to bind NLRP3 during oxidative stress leading to increased inflammasome activation24. Furthermore, several reports have proposed that IRE1α signaling increases TXNIP expression and, thereby, inflammasome formation30,31. Based on these studies, we asked if IRE1α activation promotes inflammasome formation through regulation of TNXIP expression. To answer this, we examined TNXIP expression following inflammasome stimulation in the presence and absence of MKC8866. Rather than observe an increase in TXNIP expression we found that LPS addition led to decreased expression of TXNIP transcript, which was partially suppressed by addition of MKC8866 (Fig. 6a). Likewise, when we examined expression of TXNIP protein, we observed a similar trend with LPS causing decreased TNXIP expression, which again was partially blocked by combination with MKC8866 (Fig. 6b). Therefore, in this experimental setting, it is unlikely that IRE1α RNase signaling promotes inflammasome formation by increasing TXNIP expression.
Fig. 6. TXNIP expression decreases in THP-1 cells upon LPS treatment.
THP-1 cells were treated for the indicated times with 1 μg/ml LPS alone or in combination with 20 μM MKC8866 and after which a TXNIP expression was determined by Q-PCR (n = 3) and b by immunoblotting. Error bars represent SD.
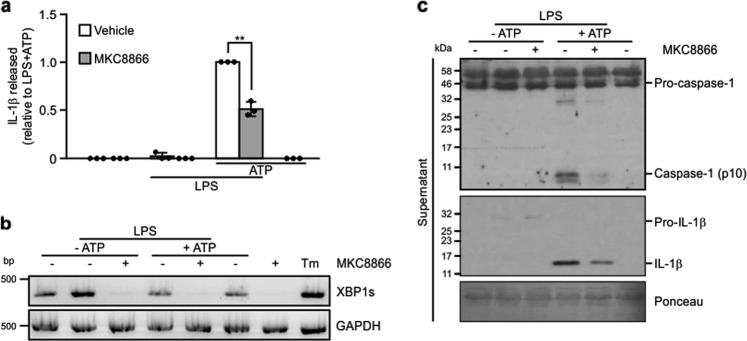
MKC8866 reduces inflammasome activation in primary PBMCs
To verify that MKC8866 suppression of NLRP3 inflammasome formation is not restricted to THP-1 cells, we isolated PBMCs from healthy adults. Following priming with 0.5 ng/ml LPS for 2 h, primary PBMCs were stimulated with 5 mM ATP for 45 min. Similar to nigericin, ATP triggers K+ efflux by selectively activating the P2X7 receptor32. Similar to THP-1 cells, treatment with MKC8866 diminished IL-1β secretion and reduced XBP1 splicing in primary PBMCs stimulated with LPS and ATP (Fig. 7a, b). Immunoblots using the conditioned medium of LPS/ATP-treated PBMCs confirmed that MKC8866 treatment was associated with reductions in the release of p17 IL-1β and processed pro-caspase-1 (Fig. 7c). Collectively, these results indicate that IRE1α RNase activity also contributes to NLRP3 inflammasome formation in primary human PBMCs.
Fig. 7. IRE1α RNase inhibition reduces activation of the NLRP3 inflammasome in primary PBMCs.
PBMCs isolated from healthy individuals were treated for 2 h with either 0.5 ng/ml LPS alone or in combination with 20 μM MKC8866 followed by addition of 5 mM ATP for 45 min following which cell lysates and conditioned medium was collected. a Levels of IL-1β in cell conditioned medium were quantified by ELISA (n = 3). b IRE1α RNase activity was assessed by monitoring levels of XBP1 splicing via RT-PCR. Tunicamycin (Tm) treatment served as a positive control for XBP1 splicing. c Immunoblotting for caspase-1 (pro- and p10) and IL-1β (pro- and p17) was performed using PBMC conditioned medium collected following the indicated treatments. *P < 0.05 based on a Student’s t test. Error bars represent SD.
Discussion
Classically IRE1α activation is associated with resolution of ER stress via activation of the adaptive, pro-survival UPR. However, an important role for IRE1α signaling is emerging within the innate immune system where it has been linked to the function of several cell types including dendritic cells, macrophages, and natural killer cells13. In this study we asked whether IRE1α signaling contributed to activation of the NLRP3 inflammasome in monocytic cells. Similar to the findings reported by Martinon et al., using murine bone marrow derived macrophages (BMDMs)15, we observed selective activation of the IRE1α-XBP1 axis in the human monocytic cell line, THP-1 following stimulation with LPS. Addition of signal II, via nigericin treatment, while not altering IRE1α-dependent signaling, significantly enhanced inflammasome activation and pro-IL-1β processing. By selectively inhibiting IRE1α signaling using a small molecule IRE1α RNase inhibitor we observed a substantial reduction in processing of pro-IL-1β in both THP-1 cells and primary PBMCs. Similar to our findings, Tufanli et al. recently reported blocking IRE1α RNase signaling reduced pro-IL-1β processing in PBMCs and NLRP3 inflammasome activation in murine BMDMs19 but did not explore the mechanism underpinning these observations.
By assessing the various signaling steps driving NLRP3 inflammasome assembly we demonstrate IRE1α signaling, while not required in THP-1 cells for priming of inflammasome components or induction of pro-IL1β expression, is required for efficient assembly of the NLRP3 inflammasome complex. The reduction we observe in inflammasome assembly, upon IRE1α RNase inhibition, while substantial is not complete. This suggests that IRE1α signaling likely promotes the efficiency of inflammasome assembly by fine-tuning it in some manner but is not an absolute requirement. Similar results were obtained in primary PBMCs where treatment with MKC8866 reduced but did not inhibit pro-IL1β processing and release in response to LPS/ATP treatment.
The signaling pathways initiating structural assembly of the inflammasome are not fully understood, with diverse processes including ion efflux, generation of mitochondrial reactive oxygen species and posttranslational modification of inflammasome components including NLRP3 and ASC implicated33. Recent reports have suggested that IRE1α RNase activity can increase NLRP3 inflammasome formation in the pancreatic B cell line INS-1 via regulation of thioredoxin-interacting protein (TXNIP) expression30,31. Increased IRE1α RNase activity, induced in INS-1 cells via treatment with pharmacological inducers of ER stress, was demonstrated to degrade miR-17, a microRNA that normally represses TXNIP mRNA resulting in increased TXNIP expression and enhanced inflammasome formation30. Similarly, Oslowski et al. reported addition of thapsigargin or tunicamycin to INS-1 cells induced TXNIP expression, which increased levels of pro-IL1β31.
In assessing the contribution of TXNIP in our system, we found that LPS treatment decreased TXNIP expression in THP-1 cells. Furthermore, LPS-induced decreases in TXNIP expression were partly blocked upon addition of MKC8866 suggesting that IRE1α-mediated signaling leads to a loss of TXNIP expression in our system. The discrepancy between our work and previously reported results may be a consequence of several factors including the amplitude of IRE1α signaling triggered and the cell types used. We have modeled physiological activation of IRE1α signaling within the innate immune system rather than IRE1α signaling induced by pharmacological inducers of ER stress. Although we have clearly demonstrated a role for IRE1α signaling in fine-tuning assembly of the NLRP3 inflammasome in monocytes following TLR ligation, further studies are required to determine the mechanisms underpinning this observation.
While our results indicate that IRE1α signaling contributes to but is not an essential requirement for inflammasome activation in LPS-stimulated monocytes, it is likely that the importance of this pathway may be heightened in particular settings. Elevated IRE1α signaling, as determined by increased XBP1 splicing, has been reported in monocytes obtained from rheumatoid arthritis and tumor necrosis factor receptor associated periodic syndrome patients34,35. Within these specific disease settings, it is plausible that constitutively elevated IRE1α signaling helps drive hyper-stimulation of the inflammasome leading to excessive production of IL-1β. Therefore, selective, targeted use of IRE1α inhibitors could yield benefits in these clinical settings. Indeed, genetic ablation of IRE1α signaling in a mouse model of rheumatoid arthritis has been demonstrated to confer significant therapeutic benefits18.
In summary, our study highlights a previously unknown role for IRE1α-dependent signaling in the structural assembly of the NLRP3 inflammasome. We demonstrate blockade of IRE1α signaling, through the use of a small molecule inhibitor, efficiently reduces NLRP3 inflammasome formation and pro-IL1β processing in both THP-1 cells and primary PBMCs. Our findings further support the emergence of IRE1α as a driver of innate immune responses and suggest therapeutically targeting IRE1α could yield clinical benefit in conditions characterized by excessive NLRP3 inflammasome formation.
Acknowledgements
We would like to acknowledge the contribution Prof. Padraic Fallon, Trinity College Dublin, for his input into this study and Kalpana Santharan for the generation of preliminary data, which lead to this study. We also acknowledge the Flow Cytometry Core Facility at NUI Galway, which is funded by NUI Galway, Science Foundation Ireland and the Irish Government’s Programme for Research in Third Level Institutions, Cycle 5, National Development Plan 2007–2013 and the technical assistance of Dr Shirley Hanley. This work was funded by Health Research Board (grant number HRA-POR-2014-643), Science Foundation Ireland (SFI) grant co-funded under the European Regional Development Fund (grant number 13/RC/2073), SFI Starting Investigator Grant (grant number 15/SIRG/3528), Canada Research Chairs program, Irish Research Council Fellowship (EBPPG/2014/74), European Commission [Horizon 2020 Collaborative Health Project NEPHSTROM (grant number 634086), FP7 Collaborative Health Project VISICORT (grant number 602470), Science Foundation Ireland [REMEDI Strategic Research Cluster (grant number 09/SRC-B1794), CÚRAM Research Centre (grant number 13/RC/2073) and a Molecular Medicine Ireland Clinical and Translational Research Scholarship funded by the Irish Government’s Programme for Research in Third Level Institutions, Cycle5 and by the College of Medicine, Nursing and Health Sciences of the National University of Ireland Galway.
Author contributions
S.D., A.T., M.L., K.M., S.E.L., D.Q., S.D.N., designed and performed experiments. S.D, A.T., M.L., S.E.L., K.M. contributed to data compilation and paper preparation. J.B.P. and Q.Z. provided access to MKC8866. A.M.G., M.D.G., A.S. provided critical feedback on the study and contributed to preparation of the paper. S.E.L. devised the study and oversaw the research program. All authors listed reviewed the paper and provided feedback.
Conflict of interest
A.S. and A.M.G are co-founders and shareholders of Cell Stress Discoveries Ltd. Q.Z. and J.B.P. are employees and shareholders of Fosun Orinove PharmaTech Inc. The remaining authors declare that they have no conflict of interest.
Footnotes
Edited by H.-U. Simon
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Aaron Talty, Shane Deegan, Mila Ljujic
Change history
1/6/2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
- 1.Cox JS, Shamu CE, Walter P. Transcriptional induction of genes encoding endoplasmic reticulum resident proteins requires a transmembrane protein kinase. Cell. 1993;73:1197–1206. doi: 10.1016/0092-8674(93)90648-A. [DOI] [PubMed] [Google Scholar]
- 2.Mori K, Ma W, Gething MJ, Sambrook J. A transmembrane protein with a cdc2+/CDC28-related kinase activity is required for signaling from the ER to the nucleus. Cell. 1993;74:743–756. doi: 10.1016/0092-8674(93)90521-Q. [DOI] [PubMed] [Google Scholar]
- 3.Harding HP, Zhang Y, Ron D. Protein translation and folding are coupled by an endoplasmic-reticulum-resident kinase. Nature. 1999;397:271–274. doi: 10.1038/16729. [DOI] [PubMed] [Google Scholar]
- 4.Haze K, et al. Identification of the G13 (cAMP-response-element-binding protein-related protein) gene product related to activating transcription factor 6 as a transcriptional activator of the mammalian unfolded protein response. Biochem. J. 2001;355:19–28. doi: 10.1042/bj3550019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ron D, Walter P. Signal integration in the endoplasmic reticulum unfolded protein response. Nat. Rev. Mol. Cell Biol. 2007;8:519–529. doi: 10.1038/nrm2199. [DOI] [PubMed] [Google Scholar]
- 6.Bertolotti A, Zhang Y, Hendershot LM, Harding HP, Ron D. Dynamic interaction of BiP and ER stress transducers in the unfolded-protein response. Nat. Cell Biol. 2000;2:326–332. doi: 10.1038/35014014. [DOI] [PubMed] [Google Scholar]
- 7.Calfon M, et al. IRE1 couples endoplasmic reticulum load to secretory capacity by processing the XBP-1 mRNA. Nature. 2002;415:92–96. doi: 10.1038/415092a. [DOI] [PubMed] [Google Scholar]
- 8.Hollien J, et al. Regulated Ire1-dependent decay of messenger RNAs in mammalian cells. J. Cell Biol. 2009;186:323–331. doi: 10.1083/jcb.200903014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hollien J, Weissman JS. Decay of endoplasmic reticulum-localized mRNAs during the unfolded protein response. Science. 2006;313:104–107. doi: 10.1126/science.1129631. [DOI] [PubMed] [Google Scholar]
- 10.Sriburi R, Jackowski S, Mori K, Brewer JW. XBP1: a link between the unfolded protein response, lipid biosynthesis, and biogenesis of the endoplasmic reticulum. J. Cell Biol. 2004;167:35–41. doi: 10.1083/jcb.200406136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaufman RJ. Orchestrating the unfolded protein response in health and disease. J. Clin. Investig. 2002;110:1389–1398. doi: 10.1172/JCI0216886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reimold AM, et al. Plasma cell differentiation requires the transcription factor XBP-1. Nature. 2001;412:300–307. doi: 10.1038/35085509. [DOI] [PubMed] [Google Scholar]
- 13.Osorio F, et al. The unfolded-protein-response sensor IRE-1α regulates the function of CD8α+ dendritic cells. Nat. Immunol. 2014;15:248–257. doi: 10.1038/ni.2808. [DOI] [PubMed] [Google Scholar]
- 14.Shan B, et al. The metabolic ER stress sensor IRE1α suppresses alternative activation of macrophages and impairs energy expenditure in obesity. Nat. Immunol. 2017;18:519–529. doi: 10.1038/ni.3709. [DOI] [PubMed] [Google Scholar]
- 15.Martinon F, Chen X, Lee AH, Glimcher LH. TLR activation of the transcription factor XBP1 regulates innate immune responses in macrophages. Nat. Immunol. 2010;11:411–418. doi: 10.1038/ni.1857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bronner DN, et al. Endoplasmic reticulum stress activates the inflammasome via NLRP3- and aspase-2-driven mitochondrial damage. Immunity. 2015;43:451–462. doi: 10.1016/j.immuni.2015.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abuaita BH, Burkholder KM, Boles BR, O’Riordan MX. The endoplasmic reticulum stress sensor inositol-requiring enzyme 1α augments bacterial killing through sustained oxidant production. MBio. 2015;6:e00705. doi: 10.1128/mBio.00705-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qiu Q, et al. Toll-like receptor-mediated IRE1alpha activation as a therapeutic target for inflammatory arthritis. EMBO J. 2013;32:2477–2490. doi: 10.1038/emboj.2013.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tufanli O, et al. Targeting IRE1 with small molecules counteracts progression of atherosclerosis. Proc. Natl Acad. Sci. USA. 2017;114:E1395–E1404. doi: 10.1073/pnas.1621188114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schroder K, Tschopp J. The inflammasomes. Cell. 2010;140:821–832. doi: 10.1016/j.cell.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 21.Bauernfeind FG, et al. Cutting edge: NF-kappaB activating pattern recognition and cytokine receptors license NLRP3 inflammasome activation by regulating NLRP3 expression. J. Immunol. 2009;183:787–791. doi: 10.4049/jimmunol.0901363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O’Connor W, Harton JA, Zhu X, Linhoff MW, Ting JP. Cutting edge: CIAS1/cryopyrin/PYPAF1/NALP3/CATERPILLER 1.1 is an inducible inflammatory mediator with NF-kappa B suppressive properties. J. Immunol. 2003;171:6329–6333. doi: 10.4049/jimmunol.171.12.6329. [DOI] [PubMed] [Google Scholar]
- 23.Petrilli V, et al. Activation of the NALP3 inflammasome is triggered by low intracellular potassium concentration. Cell Death Differ. 2007;14:1583–15895. doi: 10.1038/sj.cdd.4402195. [DOI] [PubMed] [Google Scholar]
- 24.Zhou R, Tardivel A, Thorens B, Choi I, Tschopp J. Thioredoxin-interacting protein links oxidative stress to inflammasome activation. Nat. Immunol. 2010;11:136–140. doi: 10.1038/ni.1831. [DOI] [PubMed] [Google Scholar]
- 25.Hornung V, et al. Silica crystals and aluminum salts activate the NALP3 inflammasome through phagosomal destabilization. Nat. Immunol. 2008;9:847–856. doi: 10.1038/ni.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoss F, Rodriguez-Alcazar JF, Latz E. Assembly and regulation of ASC specks. Cell. Mol. Life Sci. 2017;74:1211–1229. doi: 10.1007/s00018-016-2396-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tam AB, Mercado EL, Hoffmann A, Niwa M. ER stress activates NF-kappaB by integrating functions of basal IKK activity, IRE1 and PERK. PLoS ONE. 2012;7:e45078. doi: 10.1371/journal.pone.0045078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Volkmann K, et al. Potent and selective inhibitors of the inositol-requiring enzyme 1 endoribonuclease. J. Biol. Chem. 2011;286:12743–12755. doi: 10.1074/jbc.M110.199737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cullen SP, Kearney CJ, Clancy DM, Martin SJ. Diverse activators of the NLRP3 inflammasome promote IL-1beta secretion by triggering necrosis. Cell Rep. 2015;11:1535–1548. doi: 10.1016/j.celrep.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 30.Lerner AG, et al. IRE1alpha induces thioredoxin-interacting protein to activate the NLRP3 inflammasome and promote programmed cell death under irremediable ER stress. Cell Metab. 2012;16:250–264. doi: 10.1016/j.cmet.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Oslowski CM, et al. Thioredoxin-interacting protein mediates ER stress-induced beta cell death through initiation of the inflammasome. Cell Metab. 2012;16:265–273. doi: 10.1016/j.cmet.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kahlenberg JM, Dubyak GR. Mechanisms of caspase-1 activation by P2X7 receptor-mediated K+ release. Am. J. Physiol. Cell Physiol. 2004;286:C1100–C1108. doi: 10.1152/ajpcell.00494.2003. [DOI] [PubMed] [Google Scholar]
- 33.He Y, Hara H, Nunez G. Mechanism and Regulation of NLRP3 Inflammasome Activation. Trends Biochem. Sci. 2016;41:1012–1021. doi: 10.1016/j.tibs.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Savic S, et al. TLR dependent XBP-1 activation induces an autocrine loop in rheumatoid arthritis synoviocytes. J. Autoimmun. 2014;50:59–66. doi: 10.1016/j.jaut.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dickie LJ, et al. Involvement of X-box binding protein 1 and reactive oxygen species pathways in the pathogenesis of tumour necrosis factor receptor-associated periodic syndrome. Ann. Rheum. Dis. 2012;71:2035–2043. doi: 10.1136/annrheumdis-2011-201197. [DOI] [PubMed] [Google Scholar]