Key Points
LPS-induced TF procoagulant activity in monocytes in vivo is dependent on LPS-induced activation of ASMase.
ASMase inhibitors attenuate LPS- and cytokine-induced TF procoagulant activity without decreasing the de novo synthesis of TF protein.
Abstract
Tissue factor (TF) is a cofactor for factor VIIa and the primary cellular initiator of coagulation. Typically, most TF on cell surfaces exists in a cryptic coagulant-inactive state but are transformed to a procoagulant form (decryption) following cell activation. Our recent studies in cell model systems showed that sphingomyelin (SM) in the outer leaflet of the plasma membrane is responsible for maintaining TF in an encrypted state in resting cells, and the hydrolysis of SM leads to decryption of TF. The present study was carried out to investigate the relevance of this novel mechanism in the regulation of TF procoagulant activity in pathophysiology. As observed in cell systems, administration of adenosine triphosphate (ATP) to mice enhanced lipopolysaccharide (LPS)-induced TF procoagulant activity in monocytes. Treatment of mice with pharmacological inhibitors of acid sphingomyelinase (ASMase), desipramine and imipramine, attenuated ATP-induced TF decryption. Interestingly, ASMase inhibitors also blocked LPS-induced TF procoagulant activity without affecting the LPS-induced de novo synthesis of TF protein. Additional studies showed that LPS induced translocation of ASMase to the outer leaflet of the plasma membrane and reduced SM levels in monocytes. Studies using human monocyte-derived macrophages and endothelial cells further confirmed the role of ASMase in LPS- and cytokine-induced TF procoagulant activity. Overall, our data indicate that LPS- or cytokine-induced TF procoagulant activity requires the decryption of newly synthesized TF protein by ASMase-mediated hydrolysis of SM. The observation that ASMase inhibitors attenuate TF-induced coagulation raises the possibility of their therapeutic use in treating thrombotic disorders associated with aberrant expression of TF.
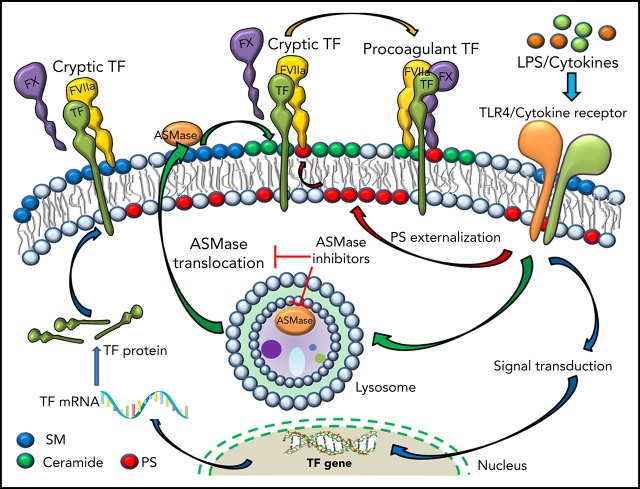
Visual Abstract
Introduction
Tissue factor (TF), the primary initiator of the coagulation cascade, is essential for hemostasis,1 but an aberrant expression of TF leads to thrombotic vascular occlusion, the precipitating event in acute myocardial infarction, unstable angina, and ischemic stroke.2,3 Currently, the pathophysiological processes that generate hemostatic and prothrombotic TF in health and disease are poorly understood. In health, TF expression is limited primarily to perivascular and epithelial cells,4,5 ensuring hemostasis when the circulating blood comes in contact with TF upon vascular injury. Infection and other disease states induce TF expression in vascular cells.6-8 In general, TF expressed on cells remains in a cryptic (coagulant-inactive) state until it is activated by a pathophysiologic stimulus.9-12 The cellular processes that regulate the transformation of cryptic TF to procoagulant TF, or vice versa, are not entirely clear. Most of the evidence in the literature suggests that externalization of phosphatidylserine (PS) following cell perturbation plays a critical role in TF activation at the cell surface.11 In addition to PS, thiol-disulfide exchange pathways mediated by protein disulfide isomerase or thioredoxin were shown to play a role in TF activation.10,13,14
Recently, we discovered that sphingomyelin (SM), the predominant phospholipid in the outer leaflet of the plasma membrane, plays a critical role in maintaining TF in an encrypted state in resting cells.15 Hydrolysis of SM in the plasma membrane by exogenously added bacterial sphingomyelinase or acid sphingomyelinase (ASMase) translocated to the plasma membrane in response to adenosine triphosphate (ATP)-induced cell signaling led to decryption of TF.15 Sphingomyelinase (SMase)-mediated TF decryption was independent of PS externalization and thiol-disulfide exchange pathways.15
SM metabolism is altered in many disease settings, including atherosclerosis, diabetes, sepsis, and cancer.16-24 The same disease settings were also known to induce aberrant activation of TF.2,25,26 A number of pathogenic stimuli (eg, lipopolysaccharide [LPS], cytokines, ATP, irradiation, and bacterial and viral infections) were found to translocate activated ASMase from lysosomes to the outer leaflet or secrete intracellular ASMase to the extracellular space.27 Platelets were shown to secrete ASMase upon thrombin stimulation,28,29 and functional inhibitors of ASMase blunted platelet degranulation and thrombus formation in the FeCl3 injury model.30 It is tempting to speculate that the observed effect of ASMase inhibitors on thrombus formation could have stemmed from inhibition of ASMase-mediated TF decryption following the injury. However, there is no published evidence showing that ASMase regulates TF procoagulant activity in vivo.
The present study was carried out to investigate the role of altered SM metabolism in the regulation of TF procoagulant activity in vivo. The data presented in this article provide evidence, for the first time, that LPS-induced TF procoagulant activity and thrombin generation were dependent on LPS-induced activation of ASMase. Treatment of mice with tricyclic antidepressant drugs, desipramine and imipramine, which work as functional inhibitors of ASMase, was shown to block LPS-induced TF procoagulant activity and thrombin generation. These findings open up the possibility of developing novel therapeutics for treating sepsis-induced intravascular coagulation and probably other thrombotic disorders associated with the generation of prothrombotic TF.
Materials and methods
Additional details can be found in supplemental Materials and methods (available on the Blood Web site).
Materials
LPS (Escherichia coli O111:B4), 2′(3′)-O-(4-benzoyl benzoyl)adenosine 5′-triphosphate triethyl ammonium salt (Bz-ATP), desipramine, and imipramine were obtained from Sigma-Aldrich (St. Louis, MO).
Cells
Primary human umbilical vein endothelial cells (HUVECs) were obtained from Lonza and grown to confluence at 37°C and 5% CO2 in a humidified incubator in EBM-2 basal media supplemented with 2% fetal bovine serum and growth supplements. Human monocyte-derived macrophages (MDMs) were prepared as described in our earlier report.15 Murine peripheral blood mononuclear cells (PBMCs) were isolated from murine blood using Ficoll gradient centrifugation.
Animal studies
Wild-type (C57BL/6J) mice were injected with saline or ASMase inhibitors, desipramine or imipramine (10 mg/kg body weight in 100 μL of saline), daily by intraperitoneal injection for 7 days. On day 7, mice were injected intraperitoneally with saline or LPS (E coli O111:B4, 5 mg/kg). Four hours after LPS challenge, Bz-ATP (50 mg/kg) was administered to mice via intraperitoneal injection. Fifteen minutes following ATP administration, animals were euthanized, and blood was collected by cardiac puncture. Whole blood was carefully loaded on a Ficoll gradient and centrifuged at 400g for 40 minutes to separate mononuclear cells and plasma. Mononuclear cells were processed for measuring TF procoagulant activity and analysis of TF and ASMase expression by western blotting, flow cytometry, and confocal microscopy. Plasma was processed for measuring thrombin generation and isolation of microvesicles (MVs). All studies involving animals were conducted in accordance with the animal welfare guidelines outlined in the Guide for the Care and Use of Laboratory Animals and by the Department of Health and Human Services and approved by the Institutional Animal Care and Use Committee.
Measurement of TF and prothrombinase activities
Cell surface TF activity was measured as the ability of intact cells to support the activation of factor X (FX) with the addition of FVIIa and FX, as described earlier.3,4,31 Cell surface prothrombinase activity was determined as described previously.4,5
Measurement of thrombin-antithrombin levels
Thrombin generation in murine blood was measured as levels of thrombin-antithrombin (TAT) complexes formed in the blood. TAT levels were measured using an AssayMax Mouse Thrombin-Antithrombin (TAT) Complex ELISA Kit (AssayPro, St. Charles, MO), following the instructions provided by the manufacturer.
Determination of ASMase levels in plasma
ASMase levels in plasma were measured using an Amplex Red Sphingomyelinase Assay Kit (Molecular Probes), following the instructions provided by the manufacturer. The assay was performed as a 2-step activity assay at a lower pH (pH 5.0) to exclude the activity of other SMases in plasma.
Immunofluorescence staining of ASMase and TF
For staining ASMase and TF, cells were first fixed in 4% paraformaldehyde, left intact, or permeabilized with 0.01% Triton X-100. Nonpermeabilized or permeabilized cells were incubated with rabbit anti-human ASMase immunoglobulin G (IgG; 2 μg/mL), which detects human and murine ASMase, and rat anti-murine TF monoclonal antibody (mAb; 1H1; 2 µg/mL) or mouse anti-human TF mAb (9C3; 10 µg/mL) overnight. After removing the unbound primary antibodies and washing the cells twice with phosphate-buffered saline, the cells were incubated with 4′,6-diamidino-2-phenylindole (5 μg/mL) and Alexa Fluor 488 (AF488)- and AF546-conjugated secondary antibodies (donkey anti-rabbit IgG, AF546 and donkey anti-rat or mouse IgG, AF488; 2 µg/mL) for 90 minutes. The cells were washed and processed for microscopy. To label PS, fixed intact cells were incubated with AF488–Annexin V (Invitrogen; 1:20 dilution) for 60 minutes.
Immunofluorescence microscopy, image acquisition, scoring, and colocalization
Immunofluorescence confocal microscopy, image acquisition, and colocalization analysis were performed essentially as described in our earlier publications.15,32
Data analysis
Each experiment was repeated ≥3 times, and data are expressed as mean ± standard error of the mean (SEM). Statistical significance among multiple groups was analyzed by 1-way ANOVA with Tukey’s HSD (honestly significant difference) post hoc test. Statistical significance between 2 groups was calculated using the Mann-Whitney U test. P < .05 was considered statistically significant. Prism (vs 7.03; GraphPad) software was used for preparing graphics and calculating statistical significance.
Results
ASMase inhibitors attenuate LPS- and LPS+ATP-induced TF procoagulant activity and thrombin generation in vivo
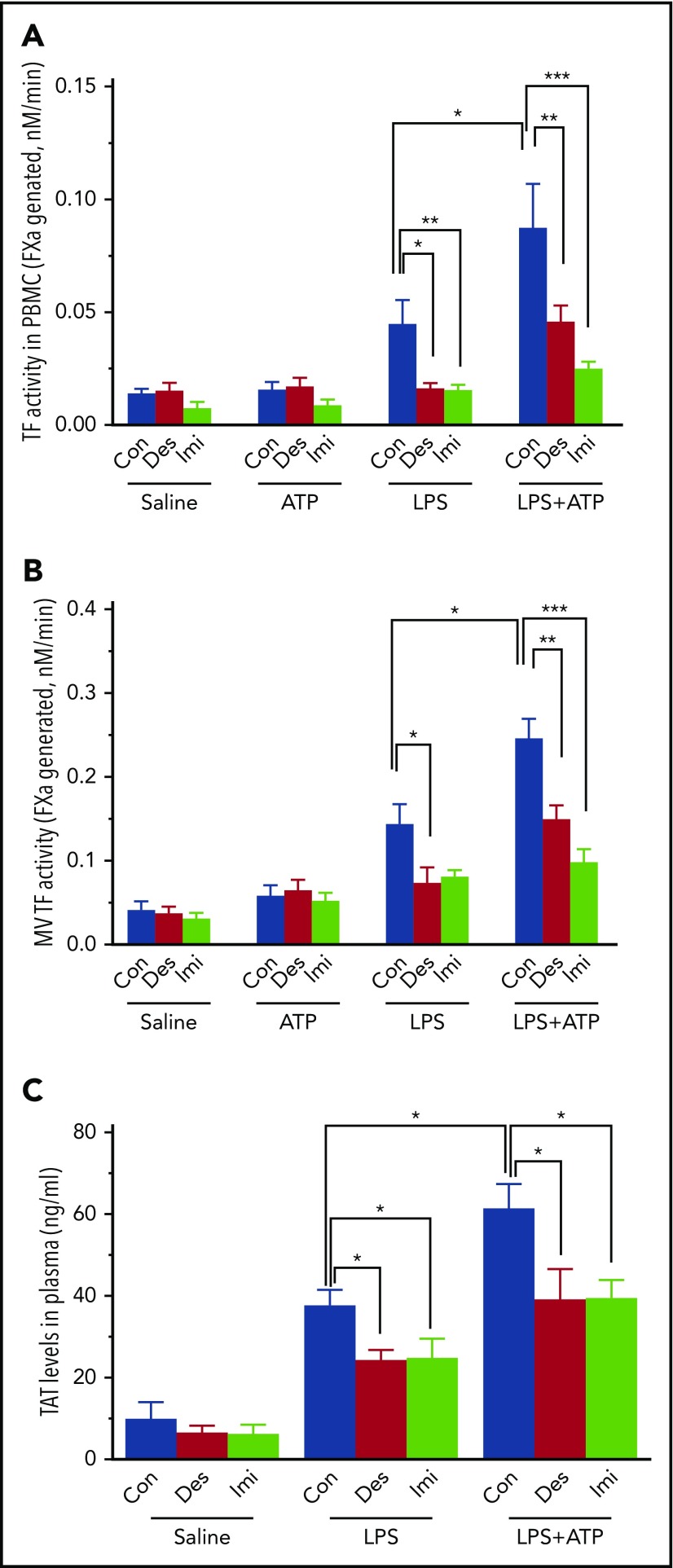
Our recent studies showed that ATP stimulation of human MDMs enhanced TF procoagulant activity on intact cells and promoted the release of TF+ MVs in a novel mechanism involving the activation of ASMase and the subsequent breakdown of SM.15 To investigate the relevance of this mechanism in regulating TF procoagulant activity in vivo and its pathophysiologic significance, wild-type mice were treated with functional inhibitors of ASMase (desipramine or imipramine, 10 mg/kg, for 7 days, intraperitoneally) and then challenged with LPS, ATP, or LPS+ATP. Measurement of TF activity in PBMCs isolated from mouse blood and MVs isolated from plasma showed that LPS treatment significantly increased TF activity in both fractions. ATP treatment itself did not increase the procoagulant activity of PBMCs or MVs but enhanced LPS-induced TF procoagulant activity (Figure 1A-B). Desipramine and imipramine treatments before LPS administration markedly reduced LPS- and LPS+ATP-induced TF procoagulant activity in PBMCs and MVs. Analysis of TF antigen levels by western blot analysis showed that LPS, as expected, induced de novo synthesis of TF protein in PBMCs. Treatment of mice with ASMase inhibitors before LPS administration or ATP treatment following LPS had no significant effect on LPS-induced TF antigen levels (supplemental Figure 1). Measurement of TAT levels in plasma showed that treatment of mice with ASMase inhibitors blocked LPS- and LPS+ATP-induced thrombin generation (Figure 1C). Overall, these data suggest that ATP enhances TF procoagulant activity in PBMCs in vivo through decryption, and this process is dependent on ASMase. It is somewhat unexpected to find that ASMase inhibitors also blocked LPS-induced TF procoagulant activity, because numerous studies showed that LPS induces TF procoagulant activity in monocytes through induction of TF gene expression at the level of gene transcription.33-35
Figure 1.
ASMase inhibitor treatment attenuates LPS-induced TF procoagulant activity and thrombin generation in vivo. Wild-type (C57BL/6J) mice were injected with saline (Con) or ASMase inhibitor desipramine (Des) or imipramine (Imi) (10 mg/kg body weight in 100 μL of saline) daily intraperitoneally for 7 days. After 7 days, mice were challenged with saline or LPS (E coli O111:B4, 5 mg/kg) by injecting them intraperitoneally in 100 µL volume. In a group of mice, 4 hours following LPS challenge, Bz-ATP (50 mg/kg in 100 µL) was administered. Fifteen minutes following ATP administration, animals were euthanized, and blood was drawn into citrate anticoagulant by cardiac puncture. Whole blood was loaded on a Ficoll gradient and centrifuged at 400g for 40 minutes to separate the plasma and PBMCs. PBMCs were washed and used to measure TF activity, and the plasma was processed for isolation of MVs or measuring thrombin generation. (A) TF activity of PBMCs. (B) TF activity associated with MVs. (C) Levels of TAT in plasma. Data are mean ± SEM (n = 6 mice per group). Differences between the group mean in all 3 panels, as determined by 1-way ANOVA, were highly statistically significant (P < .0001). *P < .05, **P < .01, ***P < .001, Tukey’s post hoc multiple comparisons.
LPS induces translocation of ASMase in monocytes and reduces SM levels
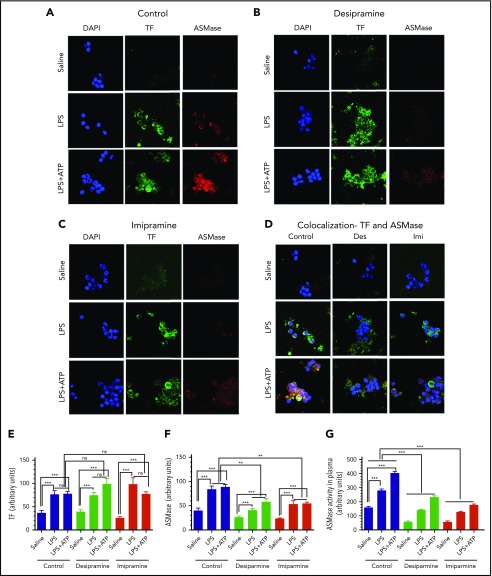
To further assess the role of ASMase and the SM metabolism in regulating TF activity in vivo, changes in the expression of ASMase in monocytes isolated from mice treated or not with ASMase inhibitors and challenged with saline, LPS, or LPS+ATP were evaluated by confocal microscopy. Monocytes constitutively express ASMase, but it is localized primarily in an intracellular compartment. Very faint or no expression of ASMase was found on the surface of nonpermeabilized monocytes isolated from control mice; however, it was clearly detectable in permeabilized monocytes (supplemental Figure 2). LPS treatment induced the translocation of ASMase to the surface of monocytes, and the levels of ASMase on the surface were increased slightly further by ATP treatment of mice for a brief duration (15 minutes) following LPS treatment (Figure 2A). As expected, TF antigen was barely detectable in monocytes from mice treated with control vehicle (saline) but was readily detectable in monocytes from mice treated with LPS. No detectable differences were found in the expression of TF levels in monocytes from mice treated with LPS or LPS+ATP (Figure 2A). Desipramine or imipramine treatment before LPS administration reduced the intensity of ASMase staining compared with control (saline) treatment of mice, indicating that these inhibitors reduced the expression of ASMase (Figure 2B-C,F). The inhibitors had no detectable effect on LPS-induced TF antigen levels in PBMCs (Figure 2B-C,E). Analysis of ASMase and TF staining indicates that these proteins are colocalized on the cell surface of monocytes (Figure 2D). Analysis of ASMase and TF expression in monocytes by flow cytometry further confirm that LPS and LPS+ATP induce the translocation of ASMase to the membrane in monocytes, and desipramine and imipramine treatment reduces the expression of ASMase (supplemental Figure 3). Measurement of ASMase levels in plasma revealed that LPS treatment also increased secretory ASMase (S-ASMase) levels significantly, which are increased further following ATP treatment. Desipramine or imipramine treatment reduced LPS- or LPS+ATP-induced increases in S-ASMase levels (Figure 2G).
Figure 2.
Effect of ASMase inhibitor treatment on LPS- and LPS+ATP-induced ASMase and TF expression in vivo in monocytes. Mice were treated with saline (Control) or ASMase inhibitor desipramine or imipramine and then challenged with saline, LPS, or LPS followed by ATP, as described in the legend for Figure 1. PBMCs isolated from whole blood of these groups of mice were fixed intact in 4% paraformaldehyde, coated on a glass coverslip, and stained for ASMase or TF using rabbit anti-human ASMase that recognizes murine ASMase and rat anti-murine TF mAb (1H1), respectively, followed by fluorophore-conjugated secondary antibodies. Representative images of immunofluorescence staining of TF and ASMase on PBMCs isolated from control mice (A) and mice treated with desipramine (B) or imipramine (C). (D) Colocalization of ASMase and TF in monocytes isolated from control, desipramine-treated (Des), and imipramine-treated (Imi) mice. Cells shown in the images are monocytes. Other PBMCs, whose cell size was much smaller than monocytes and stained very faintly, were not captured in the image. Quantification of fluorescence intensity of immunostaining of TF (E) or ASMase (F) of PBMCs isolated from control mice and mice treated with desipramine or imipramine. (G) Levels of S-ASMase in plasma of control mice and mice treated with desipramine or imipramine. Data shown are mean ± SEM (n = 6 mice). **P <.01, ***P < .001. DAPI, 4′,6-diamidino-2-phenylindole; ns, not statistically significant.
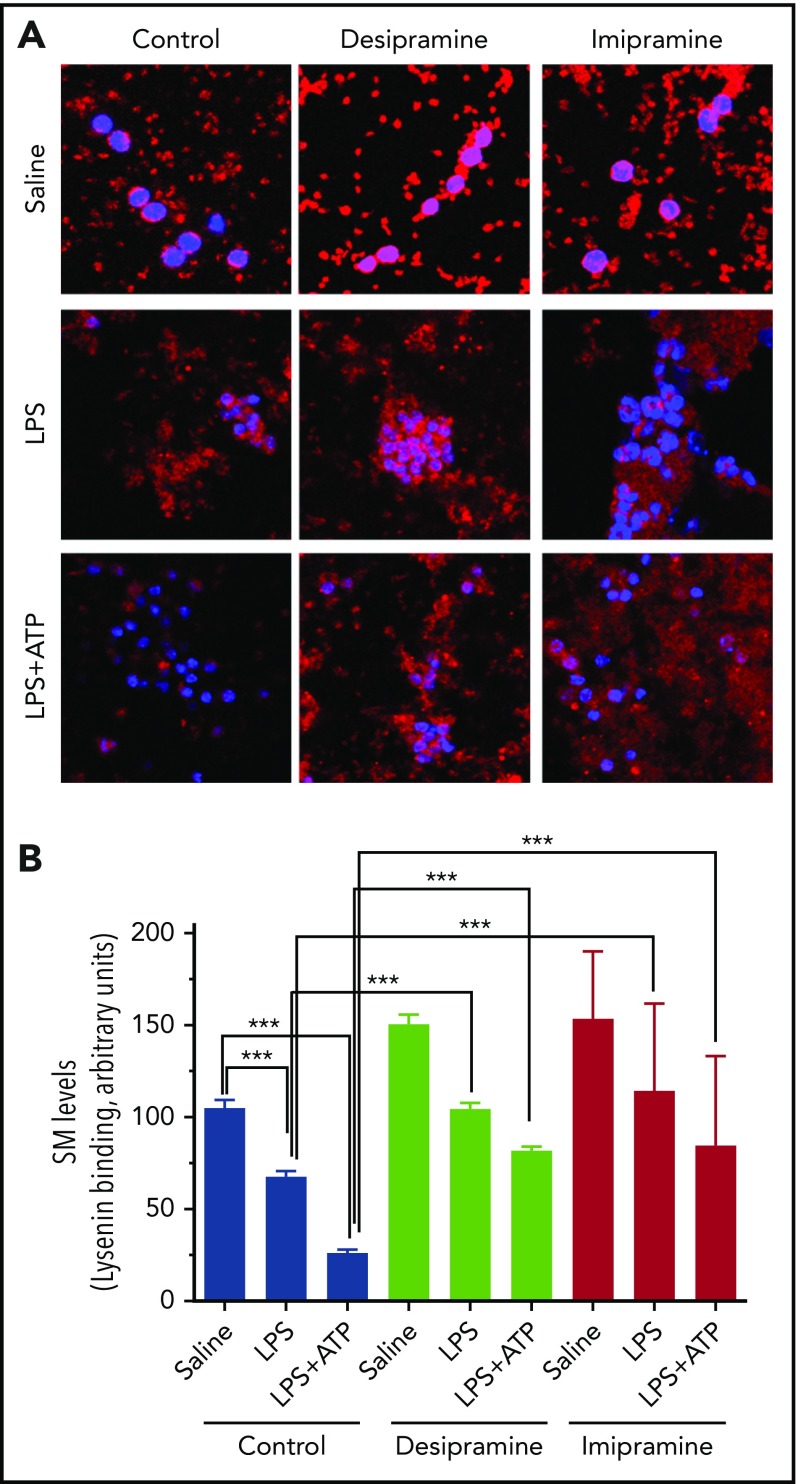
Next, we analyzed SM levels in monocytes by binding of lysenin, a protein that was shown to specifically bind SM.36 As shown in Figure 3, compared with saline, LPS or LPS+ATP treatment significantly reduced the levels of SM staining in monocytes. Treatment of mice with desipramine or imipramine increased SM levels in monocytes. Although LPS or LPS+ATP treatment also lowered SM levels in monocytes derived from desipramine- or imipramine-treated mice, it is important to note that SM levels in monocytes of desipramine- or imipramine-treated mice were significantly higher compared with those found in monocytes from mice treated with a control vehicle (saline) (Figure 3). Cumulatively, the above data (Figures 1-3) suggest that LPS-induced TF procoagulant activity and further decryption of TF by ATP stimulation are dependent on ASMase-mediated SM metabolism. These data also indicate that LPS-induced de novo synthesis of TF protein by itself does not suffice to generate procoagulant TF, and this requires LPS-induced activation of ASMase. Furthermore, the above data also suggest that ASMase inhibitors may be useful in preventing the generation of prothrombotic TF in sepsis.
Figure 3.
LPS treatment reduces SM levels in monocytes: effect of ASMase inhibitors on SM levels in monocytes. Mice were treated with saline (Control) or ASMase inhibitors desipramine or imipramine and then challenged with saline, LPS, or LPS followed by ATP, as described in the legend for Figure 1. PBMCs isolated from mice were stained for SM using lysenin, which specifically binds SM. The cells were incubated with lysenin (0.5 µg/mL) for 60 minutes in phosphate buffer containing 2% bovine serum albumin. The bound lysenin was detected using anti-lysenin antiserum (200× diluted), followed by secondary antibodies conjugated with AF567 fluorophore. (A) Representative images; original magnification ×126. (B) Quantified values for fluorescence intensity associated with monocytes (identified having a larger nucleus using DAPI staining; n = 30-70 cells). ***P < .001.
The reduction in SM levels in response to LPS or LPS+ATP challenge in mice treated with ASMase inhibitors (Figure 3) may reflect the inability of the inhibitors to fully block the function of ASMase or the presence of another mechanism that can partly contribute to the hydrolysis of SM in response to LPS and LPS+ATP. Expression of other sphingomyelinases, such as alkaline SMase and neutral SMases (nSMases) that are capable of hydrolyzing SM, was limited to specific tissues, or they are localized intracellularly.37,38 nSMase2, which localizes to the plasma membrane and whose expression is regulated by various pathophysiologic mediators, faces its catalytic site toward the cytosolic leaflet and, thus, is only capable of hydrolyzing SM in the inner leaflet of the plasma membrane.39 It is conceivable that reduced SM levels in response to LPS or LPS+ATP in mice treated with ASMase inhibitors could reflect the action of nSMase2 in the inner leaflet and the subsequent constitutive membrane lipid turnover.40
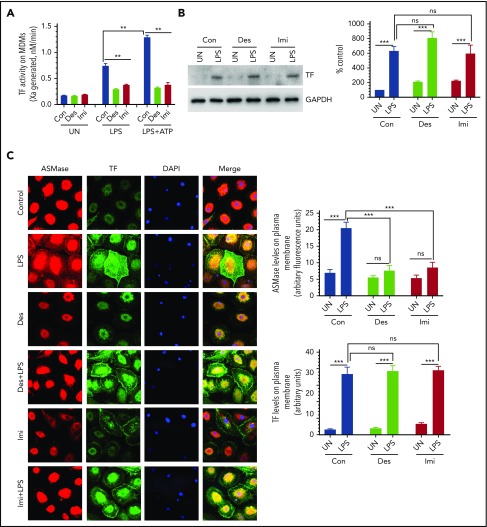
Inhibition of ASMase with pharmacological inhibitors attenuates LPS-induced TF procoagulant activity in human MDMs
Although we expected ASMase inhibitors to block ATP-induced TF decryption in vivo, it is unexpected to find that ASMase inhibitors would block LPS-induced TF procoagulant activity, because LPS-induced TF activity is believed to be primarily dependent on de novo synthesis of TF.33,34 To confirm the above novel finding, we extended our studies to an in vitro system using human MDMs. As observed in vivo in the murine system, treatment of human MDMs with desipramine or imipramine blocked ATP-induced TF decryption, as shown in our recent publication,15 as well as attenuated LPS-induced TF procoagulant activity (Figure 4A). Desipramine and imipramine treatment did not reduce LPS-induced de novo synthesis of TF protein (Figure 4B). Evaluation of ASMase expression in MDMs by confocal microscopy showed that LPS treatment mobilized the intracellular ASMase to the plasma membrane; desipramine and imipramine treatment blocked LPS-induced translocation of ASMase to the plasma membrane (Figure 4C). As observed in western blot analysis (Figure 4B), desipramine and imipramine had no detectable effect on LPS-induced TF protein expression (Figure 4C). The effect of desipramine and imipramine in curtailing LPS induction of TF activity appears to be specific to the inhibition of ASMase, because these inhibitors did not affect basal TF activity observed in unstimulated MDMs or increased TF activity following HgCl2- or ionomycin-induced TF activation, which is independent of ASMase (supplemental Figure 4). The role of ASMase in LPS-induced TF activity was further supported by the observation that knockdown of ASMase by small interfering RNA (siRNA) blocked the LPS-induced TF activity in MDMs (supplemental Figure 5). Treatment of ASMase–knocked down cells with ASMase inhibitors did not further reduce TF activity in response to LPS (supplemental Figure 5). In these experiments, as shown earlier,15 silencing ASMase with siRNA reduced ASMase levels by 70%, as evaluated by western blot analysis.
Figure 4.
Inhibition of ASMase by functional inhibitors of ASMase attenuates LPS-induced TF procoagulant activity and ATP-induced TF decryption in human macrophages. Human MDMs were treated with saline (Con) or ASMase inhibitors desipramine (Des; 10 µM) or imipramine (Imi; 10 µM) for 1 hour. Thereafter, MDMs were left unstimulated (UN) or were stimulated with LPS (1 µg/mL) for 4 hours alone or LPS for 4 hours followed by Bz-ATP (200 µM) for 15 minutes. Following the treatments, MDMs were processed to measure cell surface TF activity (A), TF antigen levels by western blot analysis (B), or expression of ASMase and TF on the cell surface by immunofluorescence confocal microscopy (C). (B) TF band intensities on western blots were quantified by densitometry analysis (right panel). (C) ASMase and TF levels in the plasma membrane were quantified by measuring the fluorescence intensity of ASMase and TF staining, respectively (right panels). Original magnification ×63 for panel C. **P < .01, ***P < .001.
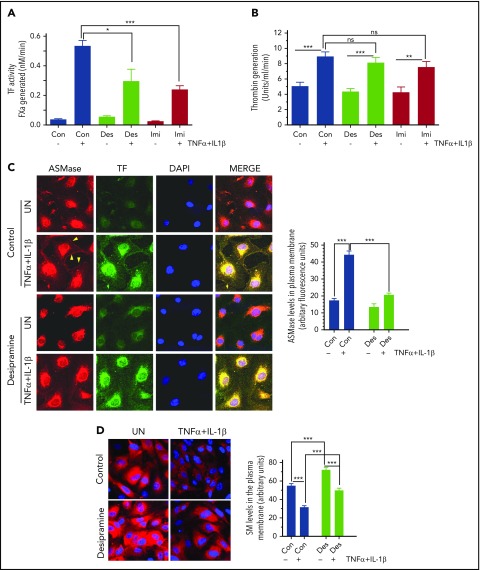
Inhibition of ASMase diminishes cytokine-induced TF procoagulant activity in endothelial cells
To determine whether the role of ASMase in regulating TF procoagulant activity is limited to monocytic cells or extends to another cell type, we investigated the effect of ASMase inhibitors on cytokine-induced TF activity in endothelial cells. As shown in Figure 5A, treatment of HUVECs with tumor necrosis factor-α + interleukin-1β (TNF-α+IL-1β) increased TF procoagulant activity >20-fold. Treatment of HUVECs with ASMase inhibitors desipramine or imipramine for 1 hour prior to TNF-α+IL-1β stimulation significantly reduced the cytokine-induced TF procoagulant activity. It is well known that endothelial cells do not constitutively express TF, and the cytokines induce TF expression by transcriptional activation of the TF gene. It is conceivable that the reduced expression of TF procoagulant activity in HUVECs treated with ASMase inhibitors could have come from a decreased de novo synthesis of TF protein. However, analysis of TF protein levels by western blot analysis showed that desipramine and imipramine did not reduce TNF-α+IL-1β–induced TF protein levels in endothelial cells (supplemental Figure 6). If anything, the inhibitors slightly increased basal levels of TF protein in unstimulated HUVECs. In additional experiments, we investigated the effect of ASMase inhibition by siRNA on TNF-α+IL-1β–induced TF activity. Inhibition of ASMase by siRNA partly, but significantly, attenuated TNFα+IL-1β–induced TF procoagulant activity in endothelial cells (supplemental Figure 7). The partial inhibition of TF activity in endothelial cells treated with ASMase inhibitors or ASMase-silenced cells may reflect the incomplete loss of ASMase function in these cells. It is also possible that other effectors, in addition to ASMase, are responsible for cytokine-induced TF activation. One such effector could be PS. As described below, cytokine stimulation also induces the externalization of PS, which can enhance TF activity independent of SM levels in the outer leaflet.14
Figure 5.
Inhibition of ASMase reduces TNFα+IL-1β–induced TF procoagulant activity in endothelial cells. HUVECs were treated with saline (Con), desipramine (Des; 10 µM), or imipramine (Imi; 10 µM) for 1 hour and then stimulated with TNF-α+IL-1β (10 ng/mL each) for 6 hours. Cell surface TF activity (A) and prothrombinase activity (B) were measured. (C) Fixed HUVECs were stained for expression of TF and ASMase by incubating cells with mouse anti-human TF mAb (9C3; 10 µg/mL) or rabbit anti-human ASMase antibody (2 µg/mL) overnight, followed by secondary antibodies conjugated with AF488 or AF546 fluorophore, and subjected to immunofluorescence confocal microscopy. Arrowheads point to expression of ASMase in the plasma membrane. The fluorescence intensity of TF and ASMase staining in the plasma membrane was quantified (right panel). (D) Representative image of staining of SM by lysenin binding (left panel). Quantification of fluorescence intensity of lysenin staining (right panel). Original magnification ×63 for panels C and D. *P < .05; **P < .01, ***P < .001.
Measurement of prothrombinase activity on the surface of HUVECs showed that TNFα+IL-1β stimulation increased the prothrombinase activity by approximately twofold (Figure 5B), suggesting that cytokine stimulation induces externalization of PS in endothelial cells. However, it is important to note that desipramine and imipramine treatment had no significant effect on the cytokine-induced enhanced prothrombinase activity, indicating that the inhibitors did not affect PS dynamics in the plasma membrane. Consistent with these data, we did not find any significant differences in annexin V binding to cells that were treated with saline, desipramine, or imipramine and then stimulated with TNFα+IL-1β (supplemental Figure 8).
Analysis of ASMase and TF expression in endothelial cells by immunofluorescence confocal microscopy did not reveal any detectable expression of ASMase on the cell surface, but it was abundant inside the cells (Figure 5C). TF staining was undetectable or gave a very faint signal. In HUVECs stimulated with TNFα+IL-1β, ASMase staining at the cell surface was evident. As expected, HUVECs stimulated with TNFα+IL-1β were stained brightly for TF. Treatment of HUVECs with desipramine reduced TNFα+IL-1β–induced cell surface expression of ASMase but had no detectable effect on TF expression. Similar data were obtained with imipramine-treated cells (data not shown). Additional analysis of SM levels using a lysenin binding assay showed that TNFα+IL-1β treatment markedly reduced SM levels in endothelial cells (Figure 5D). Treatment of HUVECs with desipramine (Figure 5D) or imipramine (data not shown) partly, but significantly, reversed the TNFα+IL-1β–induced decrease in SM levels.
Overall, the above data indicate that the cytokine-induced TF procoagulant activity comes from a cumulative effect of multiple cellular processes (ie, de novo synthesis of TF protein, externalization of PS, and the activation of ASMase and subsequent hydrolysis of SM).
Discussion
Most of TF in resting cells resides in an encrypted state with minimal procoagulant activity but becomes procoagulant following cell injury or activation.10,11 Our recent studies showed that SM, a major phospholipid in the outer leaflet of plasma membrane, plays an active role in maintaining TF in an encrypted state in macrophages and that the hydrolysis of SM following exogenously added bacterial SMase or ASMase translocated to the plasma membrane in response to ATP signaling leads to TF decryption.15 However, the relevance of this novel mechanism in regulating TF procoagulant activity in vivo or other cell types was unknown. Our present data show that treatment of mice with pharmacological inhibitors of ASMase blocks LPS and LPS+ATP-induced TF procoagulant activity in monocytes and thrombin generation in blood, suggesting that ASMase contributes to TF decryption. Our data also reveal that LPS-induced de novo synthesis of TF, in itself, is not sufficient to generate procoagulant TF and requires ASMase-mediated decryption of newly synthesized TF protein.
In a variety of diseases, including endotoxemia and sepsis, pathological activation of coagulation cascade leads to disseminated intravascular coagulation, which is associated with a poor prognosis and high mortality.41,42 Many studies demonstrated that inhibition of TF coagulant activity attenuates coagulopathy and reduces morbidity in sepsis, indicating that aberrant expression of TF in inflammation contributes to coagulopathy and morbidity.43-46 Although increased TF activity in inflammation is dependent on increased levels of nascent TF transcript in monocytes,47,48 recent studies suggest that decryption of TF and the release of thromboinflammatory MVs play a major role in inflammation-induced coagulopathy.49-51 It is well established that LPS induces TF activity, in vitro and in vivo, through transcriptional activation of TF gene and subsequent de novo synthesis of TF protein.47,52 However, there is no information on whether LPS-induced TF protein expression alone is sufficient to generate procoagulant TF or other cellular processes are required to generate the procoagulant TF. Our studies show that inhibition of ASMase attenuates LPS-induced TF procoagulant activity in in vitro and in vivo settings without affecting LPS-induced de novo synthesis of TF. Similar data were obtained with cytokine induction of TF procoagulant activity in endothelial cells. These data suggest that LPS- or cytokine-induced de novo synthesis of TF in itself is not sufficient to generate the high procoagulant state observed in sepsis; it requires ASMase-mediated activation of newly synthesized TF. Although one could also show the involvement of ASMase in generating procoagulant TF using ASMase genetically deficient mice, difficulties in procuring these mice in a timely fashion prevented us from performing these studies. Furthermore, inhibition of ASMase by pharmacological inhibitors is more relevant in investigating the potential therapeutic effect of ASMase inhibition on the attenuation of TF-induced coagulation.
Several studies suggest that ASMase plays a role in systemic inflammation and sepsis. Patients with severe sepsis are found to have increased levels of secretory SMase, one of the products of the ASMase gene, in plasma compared with healthy control subjects.53 During the clinical course, the increase in SMase activity paralleled the severity of illness, indicating that ASMase plays a critical role in the pathogenesis of severe sepsis.53 Consistent with this possibility that ASMase contributes to inflammation and development of sepsis, inhibition of ASMase by functional inhibitors was shown to improve the survival of mice in an endotoxemia model.53 Peng et al54 showed that genetic deficiency or pharmacologic inhibition of ASMase reduced lung edema and lethality in mice infected with Staphylococcus aureus. Inhibition of ASMase was also shown to reduce acute lung injury following transfusion of aged platelets in a murine model.55 In a more recent study, it was shown that partial genetic deficiency or pharmacologic inhibition of ASMase prevented liver damage and the development of sepsis following polymicrobial infection.56 The above studies suggest that inhibition of ASMase overcomes sepsis-induced organ failure and improves survival.
It is believed that ceramide, generated by the hydrolysis of SM by ASMase, is responsible for promoting inflammation and sepsis, because ceramides and their byproducts are capable of functioning as second messengers and modify a variety of molecular and cellular processes.27,57 Furthermore, ceramides in the plasma membrane promote the formation of ceramide-enriched microdomains in the membrane that leads to reorganization and clustering of receptor molecules that amplify stress-mediated signaling events.58,59 Because TF-induced coagulation was shown to play a role in inflammation and sepsis,44,60,61 and our current data demonstrate that ASMase is responsible for the generation of procoagulant TF in endotoxemia, it is likely that ASMase-mediated TF decryption plays a key role in coagulopathy, as well as in systemic inflammation associated with sepsis. Because many pathophysiologic stimuli increase ASMase levels or activity in a variety of cells in a wide range of diseases,27 it is possible that ASMase-mediated TF activation could be responsible for thrombotic disorders associated with various diseases.
In mammals, ASMase exists in 2 isoforms: S-ASMase and lysosomal ASMase (L-ASMase).62 Many stress mediators, including LPS and cytokines, were shown to induce secretion of S-ASMase into the extracellular space and/or translocate L-ASMase from intracellular compartments onto the outer leaflet of the plasma membrane.27 S-ASMase, unlike L-ASMase, requires zinc ions for sphingomyelinase activity.27 Our studies showed that both isoforms of ASMase were increased in vivo in response to LPS and LPS+ATP challenge, and treatment of mice with functional inhibitors of ASMase resulted in the reduction of both isoforms. Although it is not feasible to distinguish whether TF activation comes from the action of S-ASMase, L-ASMase, or both, it is likely that translocation of L-ASMase to the outer leaflet is responsible for decryption of TF on monocytes, because it conduces the enzyme in proximity to its substrate, SM, in the plasma membrane. It is also pertinent to point out that our cell treatments did not include zinc ions that are necessary for S-ASMase activity.
It is unknown how hydrolysis of SM influences cell surface TF activity. SM is the key constituent of membrane lipid rafts.63-65 TF in a variety of cell types was shown to be localized in membrane rafts66-69; TF associated with membrane rafts were found to be less active, and disruption of these structures enhanced TF procoagulant activity.66,70,71 It is possible that hydrolysis of SM by ASMase leads to disruption of membrane rafts, and this could be responsible for increased TF activity. It is also possible that SM, similar to PS, can directly interact with TF ectodomain. However, in contrast to PS, which alters TF-FVIIa conformation more favorable to FX activation,72 a direct interaction between TF and SM may keep TF-FVIIa conformation unfavorable to FX activation. Detailed studies are needed to elucidate mechanisms by which SM levels at the cell surface influence TF activity.
Desipramine and imipramine, US Food and Drug Administration–approved tricyclic antidepressants that are widely used in humans to treat many disorders, particularly major depression and neuropathic pain, were identified as functional inhibitors of ASMase.73,74 Because of their weak basicity and high lipophilicity, administration of these drugs results in their accumulation in lysosomes.73,74 This leads to detachment of ASMase from the inner lysosomal membrane and the subsequent proteolytic degradation of ASMase.74,75 ASMase functional inhibitors show minimal toxicity and fewer side effects. Because ASMase activity and ceramide formation were shown to contribute to the pathophysiology of a wide variety of diseases,24,27 it had been suggested that ASMase functional inhibitors could be useful in treating a variety of diseases, including sepsis.73,74 Our present data showing that administration of desipramine and imipramine block the generation of procoagulant TF and thrombin generation in vivo in a murine endotoxemia model suggest that tricyclic antidepressant drugs may be useful in preventing coagulopathy associated with sepsis. Because functional expression of ASMase is altered in many disease settings that are prone to thrombotic risk,27 it will be interesting to examine the potential therapeutic effect of ASMase inhibitors on various thrombotic disorders using appropriate model systems.
Supplementary Material
The online version of this article contains a data supplement.
Acknowledgments
This work was supported by National Institutes of Health, National Heart, Lung, and Blood Institute grant R01-HL124055 (L.V.M.R.), American Heart Association grant-in-aid 15GRNT22620004 (U.R.P.), and a postdoctoral fellowship award (19POST34380330) from the American Heart Association (J.W.).
Footnotes
For original data, please contact vijay.rao@uthct.edu.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: J.W. performed experiments, summarized the data, and wrote the initial draft of the manuscript; U.R.P. contributed to experimental design, data review, and editing of the manuscript; L.V.M.R. conceived and designed the study, analyzed the data, and wrote the manuscript; and all authors reviewed the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: L. Vijaya Mohan Rao, Department of Cellular and Molecular Biology, The University of Texas Health Science Center at Tyler, 11937 US Highway 271, Tyler, TX 75708; e-mail: vijay.rao@uthct.edu.
REFERENCES
- 1.Rapaport SI, Rao LVM. The tissue factor pathway: how it has become a “prima ballerina”. Thromb Haemost. 1995;74(1):7-17. [PubMed] [Google Scholar]
- 2.Taubman MB, Fallon JT, Schecter AD, et al. Tissue factor in the pathogenesis of atherosclerosis. Thromb Haemost. 1997;78(1):200-204. [PubMed] [Google Scholar]
- 3.Mackman N. Role of tissue factor in hemostasis, thrombosis, and vascular development. Arterioscler Thromb Vasc Biol. 2004;24(6):1015-1022. [DOI] [PubMed] [Google Scholar]
- 4.Drake TA, Morrissey JH, Edgington TS. Selective cellular expression of tissue factor in human tissues. Implications for disorders of hemostasis and thrombosis. Am J Pathol. 1989;134(5):1087-1097. [PMC free article] [PubMed] [Google Scholar]
- 5.Fleck RA, Rao LVM, Rapaport SI, Varki N. Localization of human tissue factor antigen by immunostaining with monospecific, polyclonal anti-human tissue factor antibody. Thromb Res. 1990;59(2):421-437. [DOI] [PubMed] [Google Scholar]
- 6.Drake TA, Cheng J, Chang A, Taylor FB Jr. Expression of tissue factor, thrombomodulin, and E-selectin in baboons with lethal Escherichia coli sepsis. Am J Pathol. 1993;142(5):1458-1470. [PMC free article] [PubMed] [Google Scholar]
- 7.Contrino J, Hair G, Kreutzer DL, Rickles FR. In situ detection of tissue factor in vascular endothelial cells: correlation with the malignant phenotype of human breast disease. Nat Med. 1996;2(2):209-215. [DOI] [PubMed] [Google Scholar]
- 8.Osterud B, Bjorklid E. Tissue factor in blood cells and endothelial cells. Front Biosci (Elite Ed). 2012;4(1):289-299. [DOI] [PubMed] [Google Scholar]
- 9.Bach RR. Tissue factor encryption. Arterioscler Thromb Vasc Biol. 2006;26(3):456-461. [DOI] [PubMed] [Google Scholar]
- 10.Langer F, Ruf W. Synergies of phosphatidylserine and protein disulfide isomerase in tissue factor activation. Thromb Haemost. 2014;111(4):590-597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rao LV, Pendurthi UR. Regulation of tissue factor coagulant activity on cell surfaces. J Thromb Haemost. 2012;10(11):2242-2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Versteeg HH, Ruf W. Thiol pathways in the regulation of tissue factor prothrombotic activity. Curr Opin Hematol. 2011;18(5):343-348. [DOI] [PubMed] [Google Scholar]
- 13.Zelaya H, Rothmeier AS, Ruf W. Tissue factor at the crossroad of coagulation and cell signaling. J Thromb Haemost. 2018;16(10):1941-1952. [DOI] [PubMed] [Google Scholar]
- 14.Ansari SA, Pendurthi UR, Rao LVM. Role of cell surface lipids and thio-disulfide exchange pathways in regulating the encryption and decryption of tissue factor. Thromb Haemost. 2019;119(6):860-870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang J, Pendurthi UR, Rao LVM. Sphingomyelin encrypts tissue factor: ATP-induced activation of A-SMase leads to tissue factor decryption and microvesicle shedding. Blood Adv. 2017;1(13):849-862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marathe S, Kuriakose G, Williams KJ, Tabas I. Sphingomyelinase, an enzyme implicated in atherogenesis, is present in atherosclerotic lesions and binds to specific components of the subendothelial extracellular matrix. Arterioscler Thromb Vasc Biol. 1999;19(11):2648-2658. [DOI] [PubMed] [Google Scholar]
- 17.Truman JP, Al Gadban MM, Smith KJ, Hammad SM. Acid sphingomyelinase in macrophage biology. Cell Mol Life Sci. 2011;68(20):3293-3305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Horres CR, Hannun YA. The roles of neutral sphingomyelinases in neurological pathologies. Neurochem Res. 2012;37(6):1137-1149. [DOI] [PubMed] [Google Scholar]
- 19.Milhas D, Clarke CJ, Hannun YA. Sphingomyelin metabolism at the plasma membrane: implications for bioactive sphingolipids. FEBS Lett. 2010;584(9):1887-1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holthuis JC, Luberto C. Tales and mysteries of the enigmatic sphingomyelin synthase family. Adv Exp Med Biol. 2010;688:72-85. [DOI] [PubMed] [Google Scholar]
- 21.Pavoine C, Pecker F. Sphingomyelinases: their regulation and roles in cardiovascular pathophysiology. Cardiovasc Res. 2009;82(2):175-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong ML, Xie B, Beatini N, et al. Acute systemic inflammation up-regulates secretory sphingomyelinase in vivo: a possible link between inflammatory cytokines and atherogenesis. Proc Natl Acad Sci USA. 2000;97(15):8681-8686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Górska M, Barańczuk E, Dobrzyń A. Secretory Zn2+-dependent sphingomyelinase activity in the serum of patients with type 2 diabetes is elevated. Horm Metab Res. 2003;35(8):506-507. [DOI] [PubMed] [Google Scholar]
- 24.Smith EL, Schuchman EH. The unexpected role of acid sphingomyelinase in cell death and the pathophysiology of common diseases. FASEB J. 2008;22(10):3419-3431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eilertsen KE, Østerud B. Tissue factor: (patho)physiology and cellular biology. Blood Coagul Fibrinolysis. 2004;15(7):521-538. [DOI] [PubMed] [Google Scholar]
- 26.Williams JC, Mackman N. Tissue factor in health and disease. Front Biosci (Elite Ed). 2012;4(1):358-372. [DOI] [PubMed] [Google Scholar]
- 27.Kornhuber J, Rhein C, Müller CP, Mühle C. Secretory sphingomyelinase in health and disease. Biol Chem. 2015;396(6-7):707-736. [DOI] [PubMed] [Google Scholar]
- 28.Romiti E, Vasta V, Meacci E, et al. Characterization of sphingomyelinase activity released by thrombin-stimulated platelets. Mol Cell Biochem. 2000;205(1-2):75-81. [DOI] [PubMed] [Google Scholar]
- 29.Simon CG Jr, Chatterjee S, Gear AR. Sphingomyelinase activity in human platelets. Thromb Res. 1998;90(4):155-161. [DOI] [PubMed] [Google Scholar]
- 30.Münzer P, Borst O, Walker B, et al. Acid sphingomyelinase regulates platelet cell membrane scrambling, secretion, and thrombus formation. Arterioscler Thromb Vasc Biol. 2014;34(1):61-71. [DOI] [PubMed] [Google Scholar]
- 31.Kothari H, Pendurthi UR, Rao LV. Analysis of tissue factor expression in various cell model systems: cryptic vs. active. J Thromb Haemost. 2013;11(7):1353-1363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nayak RC, Sen P, Ghosh S, et al. Endothelial cell protein C receptor cellular localization and trafficking: potential functional implications. Blood. 2009;114(9):1974-1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gregory SA, Morrissey JH, Edgington TS. Regulation of tissue factor gene expression in the monocyte procoagulant response to endotoxin. Mol Cell Biol. 1989;9(6):2752-2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Oeth P, Parry GCN, Mackman N. Regulation of the tissue factor gene in human monocytic cells. Role of AP-1, NF-kappa B/Rel, and Sp1 proteins in uninduced and lipopolysaccharide-induced expression. Arterioscler Thromb Vasc Biol. 1997;17(2):365-374. [DOI] [PubMed] [Google Scholar]
- 35.Mackman N, Oeth P. Lipopolysaccharide induction of the tissue factor gene in human monocytic cells is mediated by a member of the REL family of transcription factors. Thromb Haemost. 1993;69:2347. [Google Scholar]
- 36.Shogomori H, Kobayashi T. Lysenin: a sphingomyelin specific pore-forming toxin. Biochim Biophys Acta. 2008;1780(3):612-618. [DOI] [PubMed] [Google Scholar]
- 37.Gault CR, Obeid LM, Hannun YA. An overview of sphingolipid metabolism: from synthesis to breakdown. Adv Exp Med Biol. 2010;688:1-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bienias K, Fiedorowicz A, Sadowska A, Prokopiuk S, Car H. Regulation of sphingomyelin metabolism. Pharmacol Rep. 2016;68(3):570-581. [DOI] [PubMed] [Google Scholar]
- 39.Shamseddine AA, Airola MV, Hannun YA. Roles and regulation of neutral sphingomyelinase-2 in cellular and pathological processes. Adv Biol Regul. 2015;57:24-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dawidowicz EA. Dynamics of membrane lipid metabolism and turnover. Annu Rev Biochem. 1987;56(1):43-61. [DOI] [PubMed] [Google Scholar]
- 41.Gando S, Levi M, Toh CH. Disseminated intravascular coagulation. Nat Rev Dis Primers. 2016;2(1):16037. [DOI] [PubMed] [Google Scholar]
- 42.Fourrier F. Severe sepsis, coagulation, and fibrinolysis: dead end or one way? Crit Care Med. 2012;40(9):2704-2708. [DOI] [PubMed] [Google Scholar]
- 43.Taylor FB Jr, Chang A, Ruf W, et al. Lethal E. coli septic shock is prevented by blocking tissue factor with monoclonal antibody. Circ Shock. 1991;33(3):127-134. [PubMed] [Google Scholar]
- 44.Taylor FB., Jr Role of tissue factor and factor VIIa in the coagulant and inflammatory response to LD100 Escherichia coli in the baboon. Haemostasis. 1996;26(suppl 1):83-91. [DOI] [PubMed] [Google Scholar]
- 45.Pawlinski R, Pedersen B, Schabbauer G, et al. Role of tissue factor and protease-activated receptors in a mouse model of endotoxemia. Blood. 2004;103(4):1342-1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Welty-wolf KE, Carraway MS, Huang YC-T, et al. Blockade of extrinsic coagulation decreases lung injury in baboons with gram-negative sepsis. Am J Respir Crit Care Med. 2000;161:A517. [Google Scholar]
- 47.Mackman N. Regulation of the tissue factor gene. Thromb Haemost. 1997;78(1):747-754. [PubMed] [Google Scholar]
- 48.Rao LVM, Pendurthi UR. Tissue factor on cells. Blood Coagul Fibrinolysis. 1998;9(suppl 1):S27-S35. [PubMed] [Google Scholar]
- 49.Furlan-Freguia C, Marchese P, Gruber A, Ruggeri ZM, Ruf W. P2X7 receptor signaling contributes to tissue factor-dependent thrombosis in mice. J Clin Invest. 2011;121(7):2932-2944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rothmeier AS, Marchese P, Petrich BG, et al. Caspase-1-mediated pathway promotes generation of thromboinflammatory microparticles. J Clin Invest. 2015;125(4):1471-1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rothmeier AS, Marchese P, Langer F, et al. Tissue factor prothrombotic activity is regulated by integrin-arf6 trafficking. Arterioscler Thromb Vasc Biol. 2017;37(7):1323-1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mackman N, Brand K, Edgington TS. Lipopolysaccharide-mediated transcriptional activation of the human tissue factor gene in THP-1 monocytic cells requires both activator protein 1 and nuclear factor kappa B binding sites. J Exp Med. 1991;174(6):1517-1526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Claus RA, Bunck AC, Bockmeyer CL, et al. Role of increased sphingomyelinase activity in apoptosis and organ failure of patients with severe sepsis. FASEB J. 2005;19(12):1719-1721. [DOI] [PubMed] [Google Scholar]
- 54.Peng H, Li C, Kadow S, et al. Acid sphingomyelinase inhibition protects mice from lung edema and lethal Staphylococcus aureus sepsis. J Mol Med (Berl). 2015;93(6):675-689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McVey MJ, Kim M, Tabuchi A, et al. Acid sphingomyelinase mediates murine acute lung injury following transfusion of aged platelets. Am J Physiol Lung Cell Mol Physiol. 2017;312(5):L625-L637. [DOI] [PubMed] [Google Scholar]
- 56.Chung HY, Witt CJ, Jbeily N, et al. Acid sphingomyelinase inhibition prevents development of sepsis sequelae in the murine liver. Sci Rep. 2017;7(1):12348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chung HY, Hupe DC, Otto GP, et al. Acid sphingomyelinase promotes endothelial stress response in systemic inflammation and sepsis. Mol Med. 2016;22(1):412-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cremesti AE, Goni FM, Kolesnick R. Role of sphingomyelinase and ceramide in modulating rafts: do biophysical properties determine biologic outcome? FEBS Lett. 2002;531(1):47-53. [DOI] [PubMed] [Google Scholar]
- 59.Zhang Y, Li X, Becker KA, Gulbins E. Ceramide-enriched membrane domains–structure and function. Biochim Biophys Acta. 2009;1788(1):178-183. [DOI] [PubMed] [Google Scholar]
- 60.Pawlinski R, Pedersen B, Erlich J, Mackman N. Role of tissue factor in haemostasis, thrombosis, angiogenesis and inflammation: lessons from low tissue factor mice. Thromb Haemost. 2004;92(3):444-450. [DOI] [PubMed] [Google Scholar]
- 61.Chu AJ. Tissue factor mediates inflammation. Arch Biochem Biophys. 2005;440(2):123-132. [DOI] [PubMed] [Google Scholar]
- 62.Jenkins RW, Canals D, Hannun YA. Roles and regulation of secretory and lysosomal acid sphingomyelinase. Cell Signal. 2009;21(6):836-846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brown D. Structure and function of membrane rafts. Int J Med Microbiol. 2002;291(6-7):433-437. [DOI] [PubMed] [Google Scholar]
- 64.Simons K, Ikonen E. Functional rafts in cell membranes. Nature. 1997;387(6633):569-572. [DOI] [PubMed] [Google Scholar]
- 65.Jacobson K, Sheets ED, Simson R. Revisiting the fluid mosaic model of membranes. Science. 1995;268(5216):1441-1442. [DOI] [PubMed] [Google Scholar]
- 66.Mulder AB, Smit JW, Bom VJJ, et al. Association of smooth muscle cell tissue factor with caveolae. Blood. 1996;88(4):1306-1313. [PubMed] [Google Scholar]
- 67.Mulder AB, Smit JW, Bom VJJ, Blom NR, Halie MR, van der Meer J. Association of endothelial tissue factor and thrombomodulin with caveolae. Blood. 1996;88(9):3667-3670. [PubMed] [Google Scholar]
- 68.Mandal SK, Pendurthi UR, Rao LVM. Cellular localization and trafficking of tissue factor. Blood. 2006;107(12):4746-4753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Awasthi V, Mandal SK, Papanna V, Rao LV, Pendurthi UR. Modulation of tissue factor-factor VIIa signaling by lipid rafts and caveolae. Arterioscler Thromb Vasc Biol. 2007;27(6):1447-1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sevinsky JR, Rao LVM, Ruf W. Ligand-induced protease receptor translocation into caveolae: a mechanism for regulating cell surface proteolysis of the tissue factor-dependent coagulation pathway. J Cell Biol. 1996;133(2):293-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dietzen DJ, Page KL, Tetzloff TA. Lipid rafts are necessary for tonic inhibition of cellular tissue factor procoagulant activity. Blood. 2004;103(8):3038-3044. [DOI] [PubMed] [Google Scholar]
- 72.Ke K, Yuan J, Morrissey JH. Tissue factor residues that putatively interact with membrane phospholipids. PLoS One. 2014;9(2):e88675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kornhuber J, Tripal P, Reichel M, et al. Functional inhibitors of acid sphingomyelinase (FIASMAs): a novel pharmacological group of drugs with broad clinical applications. Cell Physiol Biochem. 2010;26(1):9-20. [DOI] [PubMed] [Google Scholar]
- 74.Beckmann N, Sharma D, Gulbins E, Becker KA, Edelmann B. Inhibition of acid sphingomyelinase by tricyclic antidepressants and analogons. Front Physiol. 2014;5:331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kölzer M, Werth N, Sandhoff K. Interactions of acid sphingomyelinase and lipid bilayers in the presence of the tricyclic antidepressant desipramine. FEBS Lett. 2004;559(1-3):96-98. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.