Abstract
Introduction
Health disparity affects both urban and rural residents, with evidence showing that rural residents have significantly lower health status than urban residents. Health equity is the commitment to reducing disparities in health and in its determinants, including social determinants.
Objective
This article evaluates the reach and context of a virtual urgent care (VUC) program on health equity and accessibility with a focus on the rural underserved population.
Materials and Methods
We studied a total of 5343 patient activation records and 2195 unique encounters collected from a VUC during the first 4 quarters of operation. Zip codes served as the analysis unit and geospatial analysis and informatics quantified the results.
Results
The reach and context were assessed using a mean accumulated score based on 11 health equity and accessibility determinants calculated for each zip code. Results were compared among VUC users, North Carolina (NC), rural NC, and urban NC averages.
Conclusions
The study concluded that patients facing inequities from rural areas were enabled better healthcare access by utilizing the VUC. Through geospatial analysis, recommendations are outlined to help improve healthcare access to rural underserved populations.
Keywords: Telemedicine, health disparities, health access, geospatial, social determinates
INTRODUCTION
Health disparities are measurable differences among population groups as a result of social, economic, racial, or ethnic characteristics, and among others.1,2 While health disparities affect both urban and rural residents, evidence shows that rural residents have significantly lower health status than urban residents do.3–5 This is a serious matter, given that approximately 14% of the U.S. population lives in rural areas.6
Reasons behind higher health disparities among rural residents are multifactorial. Rural residents travel 59% more miles than their urban counterparts do to receive health care.7 Rural residents also face other travel barriers such as lack of public transportation.8 The lack of tertiary care facilities also lowers the quality of rural health care.9 Subsequently, this isolation causes rural residents to utilize health care less. Additionally, many rural residents tend to be uninsured.5,10,11 One study hypothesized that only 28% of rural families are likely to be privately insured versus 35% of urban families.12
Health equity is the commitment to reduce disparities in health outcomes and in their determinants, including social aspects.13 Health equity is associated with social justice in health in which everyone receives the same quality of care despite socioeconomic conditions. Health disparity changes are the metrics used to measure progress toward achieving health equity.14 Therefore, reducing health disparities may lead to better health equity.
A consistent finding across the health disparity literature is that location matters.15–17 Significant inequities exist and can vary across scales from blocks to neighborhoods to regions.18 There are additional complex, myriad factors that can affect disparities.19 In rural contexts,20,21 aging populations, family structure, healthcare access,22,23 sparse populations, environmental exposures,24–26 and infrastructure27 are proven critical factors. The collection, integration, and use of these varied data are foundational to health equity research.
Geospatial technology enables researchers to input, store, manipulate, analyze, and visualize spatial information.28 Geospatial analytics uses geographic locations as points, lines, or polygons to link data and investigate spatial relationships among various factors. Overlay and intersection are used to build associations and assess the strength of those associations.29–32 Applications range from quantifying the association between alcohol outlet density and violence33 to monitoring climate changes.34 Geospatial technologies have been used in health care to measure spatial accessibility to primary care in rural areas34 or access to general health care.35 It has been applied to determine areas with a shortage of physicians.36 Finally, using a geospatial assessment, a Costa Rica study found that the healthcare reform showed substantial improvements in access to and an increase in equity of outpatient care between 1994 and 2000.37 Although promising, geospatial analysis is still underutilized in health care.
Telehealth is the delivery of health care via electronic and communication technology to patients separated by geographic, time, cultural, or social barriers.13,38–40 By employing telehealth in emergency departments, home health agencies reported a 75% reduction in unplanned hospitalizations and emergency room visits.41 Telehealth services provide a timely solution for rural communities facing many challenges in accessing health care.13 However, as rural populations age and present with more severe comorbidities, many rural hospitals struggle to coordinate care.14 Only about half of residents in rural states live within 30 minutes of an emergency department, and inadequate access to high-quality specialties remains a major barrier42,43 Therefore, there is a need to assess the reach of telehealth applications and their potential to address on equity issues in rural communities.
Through the combination of geospatial and data science approaches, we can study the relationships between areas with populations that may have higher health inequalities and the use, or reach, of the telehealth service.
The objective of this article was to delineate a telemedicine program and assess its reach in improving health accessibility among vulnerable, rural populations using geospatial analytics.
MATERIALS AND METHODS
This study delineated the service area and assessed the context of the first year, postdeployment, of a Southeastern tertiary healthcare system service called virtual urgent care (VUC). The purpose was to evaluate the reach of this online, on-demand urgent care service related to health equity and access. The 24-hour VUC service was developed to aid individuals with medical needs who may or may not be far from an in-person urgent care center, who need help when walk-in clinics are closed, or have limited independent mobility.
Intervention
The VUC web portal was designed such that any patient-provider encounter that could occur in person could be delivered through the synchronous online portal. VUC services were advertised through digital marketing such as social media and internet radio, radio channels, major highway billboards, direct mail, flyers in airports, and newsfeeds.
Patients are asked to register (an activation) an account and submit demographics and medical history information through a secure healthcare system–branded website. To manage patient’s expectations, a comprehensive list of nonemergency medical conditions is provided upon registration.
Prior to an on-demand appointment (an encounter), the patient chooses either video conference or phone call to interact with a physician. During the appointment, the online doctor reviews the patient’s medical history and symptoms to aid in diagnosis. If medication is needed, the doctor can send an electronic prescription to the pharmacy of the patients’ choice. For security and privacy, video chat and telephone connections are secure, and personal health information is protected. The fee associated with this service is a standard $49 per consultation session. Two institutional review board approvals were obtained for this study.
Setting and participants
All VUC doctors are board certified in family medicine, internal medicine, emergency medicine, or pediatrics. The online, on-demand service is available to the public regardless of their demographics.
The patient eligibility criteria for service is an age of 2 years old or older, access to a phone or computer with webcam and microphone, and residence in North Carolina (NC). Demographic information collected from patients included age, sex, zip code, dependency, insurance coverage, and a timestamp.
Variables and metrics
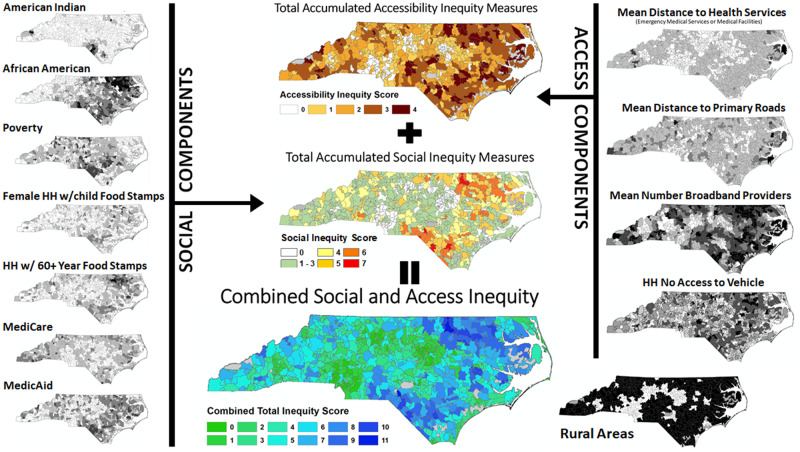
We constructed 3 health measures—social inequity score, access inequity score, and a combined inequity score—to assess and describe context. Eleven measures including social determinants and access measures were compiled per zip code.
We used publicly available data to calculate health social inequity scores by summing 7 independent social determinant scores that are based on percentages of each of the listed items: (1) American Indian, (2) African American, (3) poverty, (4) single-female household (HH) with children under the age of 18 years old who receive food stamps, (5) HH with individuals 60 years of age or older who receive food stamps, (6) Medicare patients, and (7) Medicaid patients.
Health accessibility was calculated based on 4 variables: access to health services (emergency medical services [EMS] and medical facilities), access to primary and secondary roadways that facilitate travel to health services, access to internet broadband, and personal vehicle access. A combined social and accessibility inequity score is the total of the 7 social factors and the 4 access factors.
Reach, then, is a measure of the extent to which the VUC service is able to spread into new areas. Reachability is the proportion of zip codes that has at least 1 VUC encounter, for a given inequity factor of interest.
Data collection, extraction, and cleaning
All activation and encounter data were automatically collected from the VUC web portal and stored in a secure SAP BusinessObjects enterprise system (SAP America, Newtown Square, PA). The BusinessObjects universe maintained 2 separate tables: activations and encounters. Both tables included the patients’ zip code and timestamp.
Geospatial database construction
The unit of analysis was set by the geographic resolution of the data—the zip code. An ArcGIS shapefile of the 2016 Zip Code Tabulation Area (ZCTA) was obtained from the Census Bureau. The ZCTA is the most consistent representation of actual Zip Code postal delivery areas and has the benefit of being used by the Census Bureau as a statistical geographic cataloging unit. The data from the encounters and activations tables were aggregated into counts by zip code. The zip code served as the link to census ZCTAs as well as other tabular information obtained. Other factors such as road, facility, and broadband access were analyzed and summarized by ZCTA zones to obtain measures.
The activations and encounters tables were then edited to ensure linkage to the ZCTA geospatial file. NC encounters were selected and aggregated to obtain a single total count per zip code. This process aided the de-identification of individual patient records. To enable temporal analysis, these tables were also summarized by calendar quarter. These summary tables were then linked by zip code and values moved to the ZCTA spatial database.
Primary sources of information for social determinants of interest were obtained using the Census Bureau’s American FactFinder. We used the 5-year 2016 American Community Survey to obtain demographic, health, race, mobility (access to vehicle status), and insurance variables by ZCTA. For the development of some factors it was necessary to perform tallies (Medicaid, Medicare, and access to vehicle). Others required calculation of percentages based on total population within the zip code for each associated factor. Six 2016 American Community Survey attribute tables were chosen and linked to the ZCTA-geospatial file from, which the selected social factors and access to vehicle factor were added.
Information for accessibility came from several sources. The Census Bureau’s 2016 TIGER (Topologically Integrated Geographic Encoding and Referencing) Line file was acquired to obtain all roads for NC. Using the census roads ensured that they were in sync with the Census ZCTA boundaries. The North Carolina Spatial Clearing House NC OneMap website was used to obtain point files of EMS and medical facilities. Finally, the broadband file was obtained from the Federal Communications Commission website (Form 477 file) for fixed broadband deployment at the block level.
Geospatial analysis
Accessibility was developed as a Euclidean distance layer at 100-m grid cell resolution for each of the NC primary and secondary roads (selection from NC TIGER roads), as well as the EMS and the medical facilities. To obtain a single health service access measure, the 2 distance grids for EMS and medical facilities were combined using cell statistics to preserve only the minimum distance at any location to the final output. Broadband data were mapped to the block level, then rasterized to a 100-m grid. For the road, health service, and broadband access grids, ZCTA polygon areas were then used as zones to summarize the raster measures by ZCTA. The summary tables were then linked by zip code to the geospatial file and attributes transferred. The health service access set a threshold of 3218 m (2 miles). Primary and secondary road access set a threshold of 5000 m (3.1 miles). Broadband access was set for a mean provider count threshold of <3.75. The mobility factor, as determined by HHs with no access to a vehicle, was set to a threshold of >15% of HHs within a zip code.
This research focused on encounters occurring in rural areas. A query for population density <100 people/square mile was used to define rural zip codes. Population density was calculated as the total population in ZCTA divided by land area within the ZCTA (removing areas over water). To assess social inequity, attributes were queried individually against all ZCTA in the state as well as just those representing the rural component (Table 1).
Table 1.
Social inequity factors and their assigned thresholds
| Social inequity factors | Threshold value |
|---|---|
| American Indian of total population of zip code | >5% |
| Black/African American of total population of zip code | >30% |
| Total population in poverty | >15% |
| Households with single female head of household with children under 18 years of age receiving food stamps | >5% |
| Households with person >60 years of age receiving food stamps | >5% |
| Total population on Medicare | >20% |
| Total population on Medicaid | >20% |
Within the rural selection, each of these factors was also queried by calendar quarter to delineate and evaluate reach and expansion of the online, on-demand VUC program across its first year. The selection of ZCTA areas resulting from each query then had that factor’s binary field calculated to 1. These fields were then summed across all 7 social inequity components and 4 accessibility components to calculate a final combined social and access equity score for each ZCTA. Figure 1 displays the geospatial flowchart for creation and calculation of the combined inequity score. Pearson correlation was used to measure the association of the final combined social and access equity score with each factor assessed. The correlation analysis was conducted across 4 aggregations of zip code: NC statewide, NC rural, and the NC rural with and without at least 1 VUC encounter.
Figure 1.
Flowchart process for the development of the social inequity and health access inequity metrics used to compile the Combined Inequity score by Zip Code Tabulation Area across North Carolina. HH: household.
RESULTS
We utilized data on VUC operations collected between January 11, 2018, an December 31, 2018. A total of 5343 patients registered to use VUC, and a total of 2195 unique encounters were completed. Of all registered patients, 646 (29.5%) patients were from rural areas and 1548 (70.5%) were from urban areas. Out of all 901 NC zip codes, VUC patient encounters occurred in 293 (32.5%) during the first year of operation, showing steady increases every quarter.
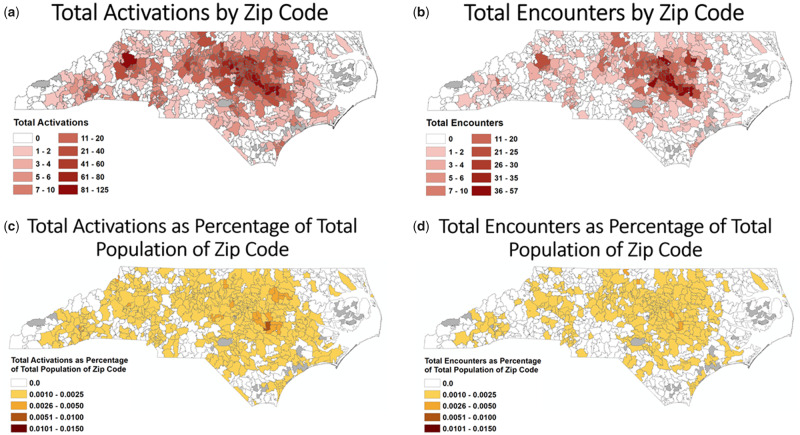
The VUC served patients across NC. Figure 2A displays the count distribution of registered VUC users by zip code. Regions with heavy activation counts are generally located around major cities, especially the Raleigh-Durham area and Charlotte. Figure 2B shows the total count of VUC encounters by zip code across the state. Comparing this with Figure 2A, the VUC consultation encounters were fewer but generally proportional with user activations.
Figure 2.
Total activations and total encounters by zip code. (a) Count of all Activations within each zip code during during the first year. (b) Count of all Encounters within each zip code during the first year. (c) Count of all Activations within each zip code as percentage of the total population of each zip code. (d) Count of all Encounters within each zip code as percentage of the total population of each zip code
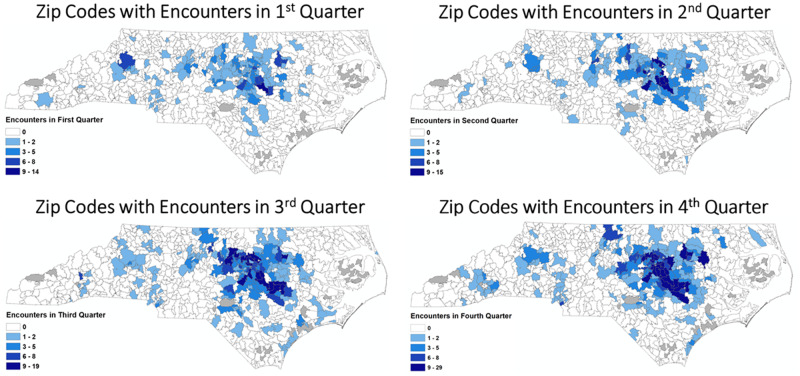
The VUC had growing acceptance and use over this first year. Figure 3 shows in 4 maps the catchment area of the VUC service as measured by encounters per zip code by calendar quarter. We observed that the initial users (Q1) originated from urban cores in the Research Triangle Area and Charlotte, which remained a center of activity through the program’s first year. Moreover, in later quarters, new zip codes in rural areas are added and VUC encounters tend to be more distributed across NC.
Figure 3.
Total encounters occurring by calendar quarter by zip code across the virtual urgent care program’s first year.
Rural vs urban
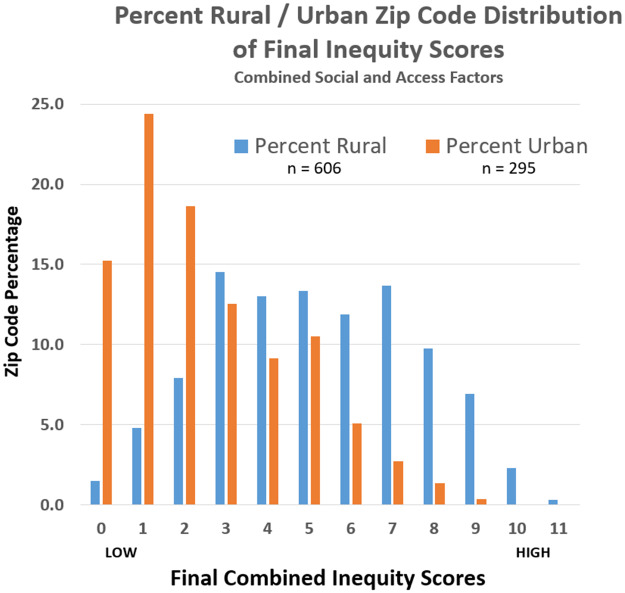
This study used a rural-urban stratification based on population density (rural <100 people/square mile). This approach identified 606 rural zip codes and 295 urban zip codes. It was theorized that there would be a difference between urban and rural inequity factors as compiled at the zip code level. As can be seen in Figure 4, when the rural and urban zip code counts within each combined inequity score (1 = low, 11 = high) are divided by their associated rural or urban total, the difference becomes apparent. This analysis primarily focuses on encounters occurring in rural zip codes. These also predominantly represent areas with high inequity.
Figure 4.
Rural (blue) vs urban (orange) percentages of zip codes by final combined inequity score across North Carolina.
Health inequity
On the one hand, VUC service demonstrated promising reachability performance across all 7 inequity metrics, as measured by the percentage of VUC users’ unique zip codes counts in relation to the state and rural totals. Across all social inequity parameters assessed, the VUC served an average of 18.54% of the zip codes labeled with at least 1 inequity criteria (Table 2). The inequity reach within the rural zip codes was higher than the entire population, in which percentages ranged from a low of 18.18% for percent American Indian to a high of 27.87% for the single-female HH with children and receiving food stamps factor, as shown in Table 2.
Table 2.
NC, NC rural, and the NC rural with at least 1 VUC encounter zip codes as a measure of the program’s service reach within each inequity component
| Inequity factor | Rural VUC zip codes | NC zip codes | NC rural zip codes |
|---|---|---|---|
| American Indian | 6 | 35 (17.14) | 33 (18.18) |
| African American | 32 | 164 (19.51) | 140 (22.86) |
| In poverty | 99 | 524 (18.89) | 388 (25.52) |
| Single-female HH with children receiving food stamps | 51 | 265 (19.24) | 183 (27.87) |
| >60 years of age receiving food stamps | 67 | 368 (18.21) | 296 (22.64) |
| Medicare | 85 | 493 (17.24) | 411 (20.68) |
| Medicaid | 81 | 414 (19.57) | 317 (25.55) |
| Health services access | 88 | 457 (19.26) | 431 (20.42) |
| Road access | 97 | 527 (18.41) | 430 (22.56) |
| Broadband access | 81 | 371 (21.83) | 325 (24.92) |
| No vehicle | 46 | 260 (17.69) | 181 (25.41) |
Values are n (%).
HH: household; NC: North Carolina; VUC: virtual urgent care.
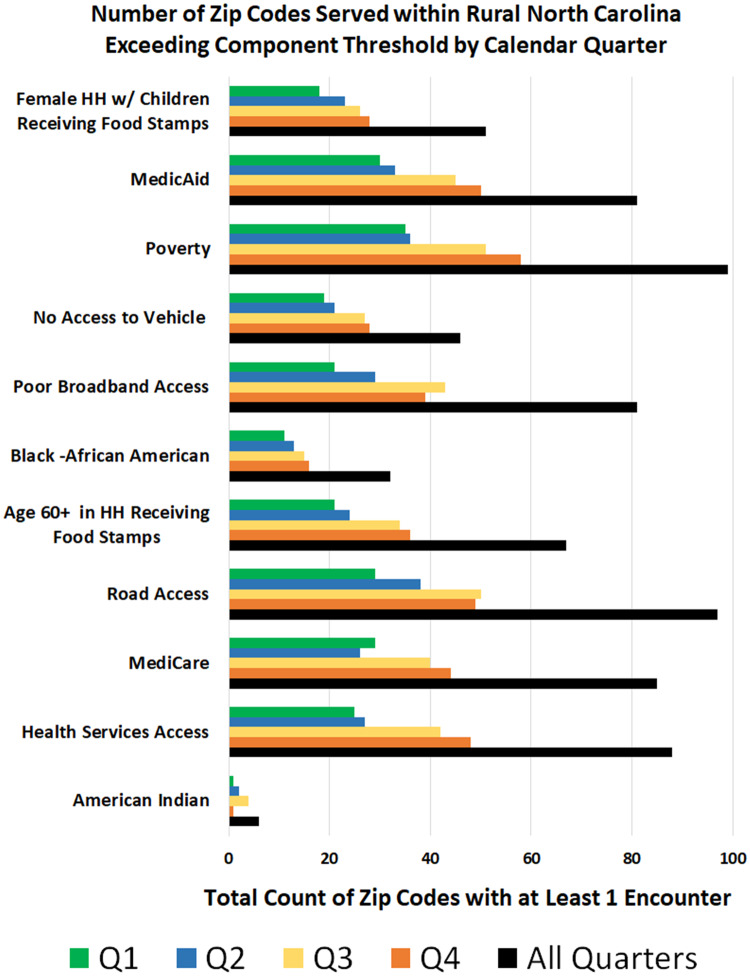
On the other hand, the rural reachability of VUC (n = 606) in NC for quarterly assessments as measured by number of zip codes with at least 1 encounter recorded consistently increased: in quarter 1, the number was 43 (7.1%); in quarter 2 it was 53 (8.7%); in quarter 3 it was 70 (11.5%); and in quarter 4 it was 74 (12.2%). Figure 5 displays this growth for all inequity factors and across all 4 quarters.
Figure 5.
Number of zip codes served that met individual factor thresholds within rural North Carolina per calendar quarter in the virtual urgent care’s first year of service. HH: household; Q: quarter.
We compared aggregated mean values based on 4 aggregations (accumulation of zip codes statewide, urban, rural, and rural with VUC encounter) for the social inequity score and accessibility score as shown in Figure 1. The social inequity aggregated mean was calculated to quantify the magnitude of social inequity in every VUC user’s zip code. On average, a zip code in the rural VUC dataset obtained 3.05 inequity metrics of the 7 possible, which is 21.5% higher than the state average of 2.51. As well, this value is 81.5% higher than the state urban zip code average of 1.68.
Health access
Access to health care was calculated by adding the score of available health services, road access, broadband options, and no personal vehicle access for each zip code (Table 3). Among regions identified with poor health services, poor road access, poor broadband options, and a higher percentage of population with no personal vehicle access, VUC encounters occurred in 20.41% 22.55%, 24.92%, and 25.41% of these rural zip codes, respectively.
Table 3.
Correlation analysis of the combined inequity score with each inequity component assessed at zip code aggregations of NC, NC rural, and the NC rural with and without at least 1 VUC encounter
| Correlation |
|||||
|---|---|---|---|---|---|
| Inequity factor | Statewide zip codes | Rural zip codes | Rural without encounter zip codes | Rural with encounter zip codes | NC rural zip codes |
| American Indian | 0.204 | 0.205 | 0.165 | 0.349 | 33 |
| African American | 0.483 | 0.529 | 0.527 | 0.603 | 140 |
| In poverty | 0.538 | 0.59 | 0.602 | 0.633 | 388 |
| Single-female HH with children receiving food stamps | 0.491 | 0.5 | 0.484 | 0.587 | 183 |
| >60 years of age receiving food stamps | 0.639 | 0.59 | 0.574 | 0.73 | 296 |
| Medicare | 0.29 | 0.13 | 0.167 | 0.18 | 411 |
| Medicaid | 0.645 | 0.61 | 0.616 | 0.702 | 317 |
| Health services access | 0.399 | 0.198 | 0.233 | 0.331 | 431 |
| Road access | 0.296 | 0.168 | 0.265 | –0.122 | 430 |
| Broadband access | –0.438 | –0.333 | –0.318 | –0.451 | 325 |
| No vehicle | 0.384 | 0.429 | 0.396 | 0.67 | 181 |
NC: North Carolina; VUC: virtual urgent care.
The accessibility inequity aggregated mean was calculated to quantify the magnitude of inequity access in every VUC user’s zip code. The higher the summation score is, the lower the potential level of healthcare access is. On average, a zip code in the rural VUC dataset obtained 2.26 inequity metrics of the 4 possible, which is 26.2% higher than the state average of 1.79 and 169% higher than the state urban zip code average of 0.84.
Combined inequity and access
The final combined score was calculated by adding the 7 health inequity and 4 health access determinants. This created a score ranging from 1 to 11; the greater the number is, the more inequity factors there are that are present at threshold levels within that zip code, thereby identifying regions with greater potential to suffer from social and access inequity issues related to health.
Correlation analysis was used to identify the strength of each factor’s association with the combined inequity score at the state and rural zip code levels as well as more detailed differences within the rural level based on presence or absence of at least 1 encounter. These correlations are presented in Table 3.
The correlations at the state and the rural levels showed little difference with the exception of percent Medicare, health services access, and percent no vehicle access. With this study’s focus on rural reachability, we further examined the rural zip codes. We compared correlations for those rural zip codes with at least 1 encounter to those rural zip codes with no encounter to date across the equity factors included in this research (Figure 5).
The rural zip codes in which we had at least 1 encounter showed more focus on elements of inequity, as correlations with all percentage-based factors were stronger and access factors generally showed poorer access. The access factor exception was health services access metric, which showed slightly better access for rural zip codes with at least 1 encounter.
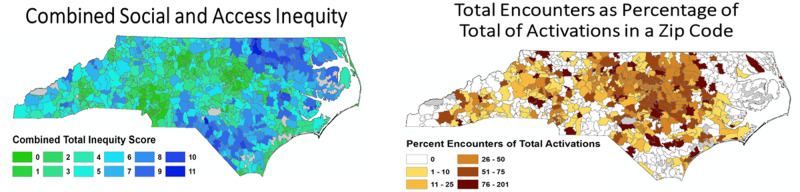
The combined inequity score map (Figure 6) shows the final combined inequity scores across NC. The areas located in the northeast and southern portion of the state, map communities with dominant American Indian and African American populations. These regions tend to have higher levels of inequity based on the measures used, but only 2 zip codes actually contain all 11 metrics. There was a proportional relationship between the level of combined inequity and the count of VUC encounters for zip codes. This demonstrates the VUC service reach into rural areas with average-to-high health inequity levels. Figure 6 shows the overall assessment of equity across NC and the regional nature of inequities.
Figure 6.
Combined social inequity and health services access: accumulation of inequity.
Overall reachability
To assess the overall context of the delineated reach of VUC, a mean combined inequity score was calculated for each zip code and for all zip codes. The mean combined inequity score for zip codes in which VUC had an encounter was 5.31. This is higher than all NC zip codes (4.30), similar to rural NC (5.17), and much higher than urban NC (2.52) (Table 4). In general, in zip codes where VUC encounters occurred, the population served by the program had higher levels of social inequity and lower access in comparison with the average inequity and access levels at both the state and rural levels.
Table 4.
Total combined inequity score averaged across the entire state of NC, all rural zip codes, urban zip codes, and rural zip codes with at least 1 VUC encounter
| Zip code | Combined inequity meana | |
|---|---|---|
| Rural VUC | 138 | 5.31 ± 2.48 |
| All NC | 901 | 4.30 ± 2.62 |
| Rural NC | 606 | 5.17 ± 2.42 |
| Urban NC | 295 | 2.52 ± 2.04 |
Values are mean ± SD.
NC: North Carolina; VUC: virtual urgent care.
aRange: 0–11 points.
DISCUSSION
This geoinformatics study evaluated the reachability of a VUC program on health inequity and access in rural regions. The VUC demonstrated promising reachability of vulnerable populations as associated with social and access factors measured. VUC reachability averaged 23.03% of rural zip codes with 1 or more health inequity factors.
The demand for receiving care via VUC steadily increased over the 4 quarters especially in rural areas. Among all 11 health equity factors, VUC had substantial reachability. The highest reachability of VUC was in zip codes with single-women HH with children under 18 years of age who receive food stamps (27.86%). The lowest reachability was in zip codes with core American Indian populations (18.18%). The ability to consistently reach a fifth of total zip codes in NC high health inequity levels suggests the continuity of developing affordable and on-demand telemedicine programs to provide care to rural populations facing inequities.
Previous research findings
Rural populations face major health disparities compared with urban regions.9,44–47 Past research has shown that telemedicine is an emerging modality in healthcare delivery, particularly in rural areas with geographical dispersed populations, that can provide high-quality, cost-effective care.48 Previous studies show that telemedicine can improve care quality, accessibility, and patient satisfaction in rural, underserved populations.49–54 This study supports the findings of the aforementioned research with regards to the acceptability of telemedicine among vulnerable populations who suffer health inequity and face accessibility barriers in rural regions.
Previous studies investigating the use of geographic information systems (GIS) to understand barriers among populations indicate that GIS approaches can inform policy-based interventions focused on eliminating geographic barriers and promoting social and health equity for the underserved.55,56 Over the past decade, epidemiology studies have utilized GIS to investigate areas of health disparities, resource availability, and health-related behaviors in fields such as cancer and environmental epidemiology.57 This geoinformatics study assessed the reachability, with a rural health equity focus, of an on-demand telemedicine service to potentially address current issues to healthcare access.
Limitations and future work
Reachability was defined in this research as the occurrence of at least 1 encounter within a zip code, which may introduce unweighted bias between zip codes with varying numbers of encounters. This research is focused on delineating the base VUC service area and assessing its composition with regard to inequity measures. Although the pricing for VUC is $49, which is minimal compared with a visit to the emergency room or urgent care clinics, the findings from this study may be sensitive to payer mix and insurance coverage. This is especially true among rural regions where insurance coverage may lack among vulnerable and underserved populations. This limited the use of the VUC by presenting an association between the use of VUC and geographical location of some underserved vulnerable populations. Another limitation was the ZCTA geospatial file. In certain areas of NC there exist “holes” in coverage where no zip code exists (military base, wilderness areas, etc.) and thus no census-related information was available at the zip code level. This study measures health access using surrogates of distance to primary road and distance to facility—both of which are greatly influenced by population density. These measures may influence the rurality scores achieved. The additional measures of no vehicle and broadband access aid in the buffering of this affect. Despite the ability for patients to choose between a video or phone call, there are remote areas where patients reported an inability to make calls either due to lack of internet service or cell phone signal. We recognize this as a limitation outside of our control that requires attention to facilitate the delivery of telehealth services.
Future work includes re-evaluating VUCs annually and compiling a report at the 5-year mark. Follow-up research work will include analyzing disease prevalence by studying the association between temporal factors (ie, influenza) and VUC use. This would include data such as chief complaints in rural and urban areas. Furthermore, in future studies, we plan to expand on the preliminary weighted analysis of zip code encounters (Supplementary Appendix), which is still premature given the recent implementation of VUC. In addition, we would like to investigate the long-term effect of VUC on health outcomes and quality-of-life measures among vulnerable populations, especially in rural areas. Finally, we aspire to present a list of recommendations on lessons learned to policymakers, the informatics community, and providers and patients.
CONCLUSION
A postdeployment evaluation study of the VUC, an online, on-demand urgent care service, has demonstrated the reachability, context, and continued growth of the service. The VUC has provided care to remote regions with vulnerable populations and limited health access. This geoinformatics approach provided visual, evidence-based information, which resulted in recommendations to better serve places experiencing social and access inequities. That comprises the informatics contribution of this research. Particularly, this research correlates telehealth encounters with health disparity factors to potentially improve health equity and access and inform policy solutions to reduce both health disparities and health care–related costs.
FUNDING
The project described was supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR002489. TLH was supported by the National Library of Medicine of the National Institutes of Health under award number 5T32LM012410. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
AUTHOR CONTRIBUTIONS
SK contributed to conception or design of the work; on the acquisition, analysis, or interpretation of data for the work, and manuscript writing. TLH performed geospatial data selection, mapping, figure creation, and manuscript writing. SL contributed to data cleaning, data analysis, and manuscript writing. TZ contributed to literature review and manuscript writing. BE supervised VUC program and data acquisition, and manuscript review. RG contributed to data acquisition and manuscript review. CS supervised data analysis and contributed to manuscript writing.
ACKNOWLEDGMENTS
The authors would like to acknowledge the efforts of the UNC Information Services Division team for their data collection and extraction efforts.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Carter-Pokras O, Baquet C.. What is a “health disparity”? Public Health Rep 2002; 117 (5): 426–34.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. US Department of Health and Human Services. The Secretary's Advisory Committee on National Health Promotion and Disease Prevention Objectives for 2020. Phase I report: recommendations for the framework and format of Healthy People 2020. Section IV. Advisory Committee findings and recommendations. 2010. Available at: http://www.healthypeople.gov/sites/default/ files/PhaseI_0.pdf. Rockville, MD. Accessed June 17, 2019.
- 3.Institute of Medicine (US) Committee on Monitoring Access to Personal Health Care Services. Millman M, editor. Access to Health Care in America. Washington (DC): National Academies Press (US); 1993. Available from: https://www.ncbi.nlm.nih.gov/books/NBK235882/ doi: 10.17226/2009. [DOI] [PubMed] [Google Scholar]
- 4. Mainous AG, 3rd, Kohrs FP.A comparison of health status between rural and urban adults. J Community Health 1995; 20 (5): 423–31. [DOI] [PubMed] [Google Scholar]
- 5. Laditka JN. Health care access in rural areas: evidence that hospitalization for ambulatory care-sensitive conditions in the United States may increase with the level of rurality. Health Place 2009; 15 (3): 761–70. [DOI] [PubMed] [Google Scholar]
- 6. Bureau, U.S.C., Pop Clock. 2017. https://www.census.gov/popclock/Accessed April, 23, 2019. Washington, DC.
- 7. Pucher J, Renne JL, Public Policy RU. Differences in mobility and U-R In: Mode Choice: Evidence From the NHTS 2001. New Brunswick, NJ: Bloustiein School of Public Planning and Policy, Rutgers University; 2004: 1–22. [Google Scholar]
- 8. Probst JC, Laditka SB, Wang JY, et al. Effects of residence and race on burden of travel for care: cross sectional analysis of the 2001 US national household travel survey. BMC Health Serv Res 2007; 7 (1): 40.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Merwin E, Snyder A, Katz E.. Differential access to quality rural healthcare: professional and policy challenges. Fam Community Health 2006; 29 (3): 186–94. [DOI] [PubMed] [Google Scholar]
- 10. Probst JC, Moore CG, Glover SH, et al. Person and place: the compounding effects of race/ethnicity and rurality on health. Am J Public Health 2004; 94 (10): 1695–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Glover S, Moore CG, Samuels ME, et al. Disparities in access to care among rural working-age adults. J Rural Health 2004; 20 (3): 193–205.. [DOI] [PubMed] [Google Scholar]
- 12. Ziller EC, Coburn AF, Anderson NJ, et al. Uninsured rural families. J Rural Health 2008; 24 (1): 1–11. [DOI] [PubMed] [Google Scholar]
- 13. Stenberg PL. Rural Individuals’ Telehealth Practices: An Overview Economic Information Bulletin Number 199. Washington, DC: U.S. Department of Agriculture Economic Research Service; 2018. Available from: https://www.ehidc.org/sites/default/files/resources/files/Rural%20Individuals%27%20Telehealth%20Practices.pdf. [Google Scholar]
- 14. Mohr NM, Harland KK, Chrischilles EA, et al. Emergency department telemedicine is used for more severely injured rural trauma patients, but does not decrease transfer: a cohort study. Acad Emerg Med 2017; 24 (2): 177–85. [DOI] [PubMed] [Google Scholar]
- 15. Arcaya MC, Tucker-Seeley R, Kim R, et al. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Soc Sci Med 2016; 168: 16–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. LaVeist T, Pollack K, Thorpe R Jr, et al. Place, not race: disparities dissipate in southwest Baltimore when blacks and whites live under similar conditions. Health Aff (Millwood) 2011; 30 (10): 1880–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Eberhardt MS, Pamuk ER.. The importance of place of residence: examining health in rural and nonrural areas. Am J Public Health 2004; 94 (10): 1682–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Graham H. Social determinants and their unequal distribution: clarifying policy understandings. Milbank Q 2004; 82 (1): 101–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bambra C, Gibson M, Sowden A, et al. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. J Epidemiol Community Health 2010; 64 (4): 284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bull CN, Krout JA, Rathbone-McCuan E, et al. Access and issues of equity in remote/rural areas. J Rural Health 2001; 17 (4): 356–9. [DOI] [PubMed] [Google Scholar]
- 21. Downey LH. Rural populations and health: determinants, disparities, and solutions. Prev Chron Dis 2013; 10: 130097 DOI: 10.5888/pcd10.130097. [DOI] [Google Scholar]
- 22. Wong ST, Regan S.. Patient perspectives on primary health care in rural communities: effects of geography on access, continuity and efficiency. Rural Remote Health 2009; 9: 1142. [PubMed] [Google Scholar]
- 23. Bissonnette L, Wilson K, Bell S, et al. Neighbourhoods and potential access to health care: the role of spatial and aspatial factors. Health Place 2012; 18 (4): 841–53. [DOI] [PubMed] [Google Scholar]
- 24. Shrestha R, Flacke J, Martinez J, et al. Environmental health related socio-spatial inequalities: identifying “hotspots” of environmental burdens and social vulnerability .Int J Environ Res Public Health 2016; 13 (7): 691.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stingone JA, Buck Louis GM, Nakayama SF, et al. Toward greater implementation of the exposome research paradigm within environmental epidemiology. Annu Rev Public Health 2017; 38: 315–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Guthman J, Mansfield B.. The implications of environmental epigenetics: a new direction for geographic inquiry on health, space, and nature-society relations. Prog Hum Geogr 2013; 37 (4): 486–504. [Google Scholar]
- 27. Marcin JP, Shaikh U, Steinhorn RH.. Addressing health disparities in rural communities using telehealth . Pediatr Res 2015; 79 (1–2): 169–76.. [DOI] [PubMed] [Google Scholar]
- 28. Higgs GJ. A literature review of the use of GIS-based measures of access to health care services. Health Serv Outcomes Res Methodol 2004; 5 (2): 119–39. [Google Scholar]
- 29. Elliott P, Wartenberg D.. Spatial epidemiology: current approaches and future challenges. Environ Health Perspectives 2004; 112 (9): 998–1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lawson AB. Statistical Methods in Spatial Epidemiology. Hoboken, NJ: Wiley; 2013. [Google Scholar]
- 31. Singh H, Fortington LV, Eime R, et al. Spatial epidemiology: a new approach for understanding and preventing sport injuries. Australasian Epidemiologist 2015; 22: 32–4. [Google Scholar]
- 32. Singh H, Fortington LV, Thompson H, et al. An overview of geospatial methods used in unintentional injury epidemiology. Injury Epidemiol 2016; 3 (1): 32.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. McGrail MR, Humphreys JS.. Measuring spatial accessibility to primary care in rural areas: Improving the effectiveness of the two-step floating catchment area method. Appl Geography 2009; 29 (4): 533–541. [Google Scholar]
- 34. Tang J-H. A flow-based statistical model integrating spatial and nonspatial dimensions to measure healthcare access. Health Place 2017; 47: 126–38. [DOI] [PubMed] [Google Scholar]
- 35. Luo W. Using a GIS-based floating catchment method to assess areas with shortage of physicians. Health Place 2004; 10(1): 1–11. [DOI] [PubMed] [Google Scholar]
- 36. Zhu L, Gorman DM, Horel S, et al. Alcohol outlet density and violence: a geospatial analysis. Alcohol Alcohol 2004; 39 (4): 369–75. [DOI] [PubMed] [Google Scholar]
- 37. Gorelick N, Hancher M, Dixon M, et al. Google Earth engine: planetary-scale geospatial analysis for everyone. Remote Sens Environ 2017; 202: 18–27. [Google Scholar]
- 38. Rosero-Bixby LJ. Spatial access to health care in Costa Rica and its equity: a GIS-based study. Soc Sci Med 2004; 58 (7): 1271–84. [DOI] [PubMed] [Google Scholar]
- 39. Hebert MJM. Telehealth success: evaluation framework development. Stud Health Technol Inform 2001; 84(Pt 2): 1145–9. [PubMed] [Google Scholar]
- 40. Field MJ. Telemedicine: A Guide to Assessing Telecommunications for Health Care. Washington, DC: National Academies Press; 1996. [PubMed] [Google Scholar]
- 41. TANGALOS EG, Tangalos EG. A Telemedicine Primer: Understanding the Issues. Telemed J 2009; 2(4): 331–2. [Google Scholar]
- 42. Suter P, Suter WN, Johnston D.. Theory-based telehealth and patient empowerment. Popul Health Manag 2011; 14 (2): 87–92. [DOI] [PubMed] [Google Scholar]
- 43. Peek-Asa C, Zwerling C, Stallones L.. Acute traumatic injuries in rural populations. Am J Public Health 2004; 94 (10): 1689–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Carr BG, Branas CC, Metlay JP, et al. Access to emergency care in the United States . Ann Emerg Med 2009; 54 (2): 261–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Dower C, McRee T, Grumbach K, et al. The Practice of Medicine in California: A Profile of the Physician Workforce. San Francisco, CA: California Workforce Initiative at the UCSF Center for the Health Professions. University of California, San Francisco; 2001. [Google Scholar]
- 46. Cull WL, Chang CH, Goodman DC.. Where do graduating pediatric residents seek practice positions? Ambul Pediatr Assoc 2005; 5 (4): 228–34. [DOI] [PubMed] [Google Scholar]
- 47. Hartley D. Rural health disparities, population health, and rural culture. Am J Public Health 2004; 94 (10): 1675–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Eberhardt MS, Ingram DD, Makuc DM, et al. Health, United States, 2001: Urban and Rural Health Chartbook. Hyattsville, MD: National Center for Health Statistics; 2001. Available from: https://www.cdc.gov/nchs/data/hus/hus01cht.pdf. [Google Scholar]
- 49. Marcin JP, Ellis J, Mawis R, et al. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics 2004; 113 (1 Pt 1): 1–6. [DOI] [PubMed] [Google Scholar]
- 50. Lamel S, Chambers CJ, Ratnarathorn M, et al. Impact of live interactive teledermatology on diagnosis, disease management, and clinical outcomes. Arch Dermatol 2012; 148 (1): 61–5. [DOI] [PubMed] [Google Scholar]
- 51. Xu CQ, Smith AC, Scuffham PA, et al. A cost minimisation analysis of a telepaediatric otolaryngology service. BMC Health Serv Res 2008; 8 (1): 30.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hilt RJ, Barclay RP, Bush J, et al. A statewide child telepsychiatry consult system yields desired health system changes and savings. Telemed J E Health 2015; 21 (7): 533–7. [DOI] [PubMed] [Google Scholar]
- 53. Arora S, Thornton K, Murata G, et al. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med 2011; 364 (23): 2199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Arora S, Kalishman S, Dion D, et al. Partnering urban academic medical centers and rural primary care clinicians to provide complex chronic disease care. Health Aff (Millwood) 2011; 30 (6): 1176–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Musa GJ, Chiang P-H, Sylk T, et al. Use of GIS mapping as a public health tool—from cholera to cancer. Health Serv Insights 2013; 6: 111–6.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Edward J, Biddle DJ, Using geographic information systems (GIS) to examine barriers to healthcare access for Hispanic and Latino Immigrants in the US South. J Racial Ethn Health Disparities 2017; 4 (2): 297–307. [DOI] [PubMed] [Google Scholar]
- 57. Auchincloss AH, Gebreab SY, Mair C, et al. A review of spatial methods in epidemiology, 2000–2010. Annu Rev Public Health 2012; 33: 107–22. [DOI] [PMC free article] [PubMed] [Google Scholar]