Abstract
Social determinants of health (SDOH) are known to influence mental health outcomes, which are independent risk factors for poor health status and physical illness. Currently, however, existing SDOH data collection methods are ad hoc and inadequate, and SDOH data are not systematically included in clinical research or used to inform patient care. Social contextual data are rarely captured prospectively in a structured and comprehensive manner, leaving large knowledge gaps. Extraction methods are now being developed to facilitate the collection, standardization, and integration of SDOH data into electronic health records. If successful, these efforts may have implications for health equity, such as reducing disparities in access and outcomes. Broader use of surveys, natural language processing, and machine learning methods to harness SDOH may help researchers and clinical teams reduce barriers to mental health care.
INTRODUCTION
Research has consistently demonstrated that lower socioeconomic status (SES) has a strong association with poor overall health and prevalence of many chronic diseases including cardiovascular disease, hypertension, diabetes, and depression.1–6 The robust association, within and across populations of different countries, is referred to as the “social gradient of health.”7 The gradient is often thought of as linking SES to physical health, but a growing literature suggests its association with mental health issues is particularly important for at least 2 central reasons. First, mental illness is an independent risk factor for worse overall health status and higher rates of physical illness and premature death.8–12 The social determinants of health (SDOH) have wide-ranging and often unappreciated effects on the overall well-being of individuals and communities. Second, the link between SES and mental health can have large, long-lasting, often generational health effects. For example, adverse childhood experiences, which have an inverse dose-dependent relationship with SES, can lead to significant developmental disruptions; these are often expressed insidiously through higher prevalence of mental and physical disease in adulthood decades later.13,14
Better mental health equity is unlikely without a deeper understanding and targeting of the causal factors related to social determinants of health (SDOH). The importance of income, housing security, education, unemployment, child abuse and neglect, neighborhood conditions, and social support have repeatedly been demonstrated to influence mental health outcomes.7,15–17 But in clinical practice, these data are often collected in an ad hoc, incomplete manner—if at all—and thus have limited actionable utility in research and care delivery endeavors.
Currently, diverse streams of SDOH data are collected for ad hoc reasons by various stakeholders, including patients, practitioners, researchers, advocacy groups, government agencies, and other public-private entities.18,19 Data are rarely standardized, often come from unvalidated instruments and questionnaires, and typically facilitate community-level analyses over individual-level investigation.20 Their integration into electronic health records (EHRs), and by extension, research and clinical care, is not yet standard practice.21 But systematically capturing, structuring, and using this data holds the potential to create a new “data asset” in health systems design, clinical care, and research. In this article we highlight current challenges for collecting SDOH data, and provide an overview of possible paths forward, which may help reduce mental health disparities.
DATA COLLECTION AND STANDARDIZATION
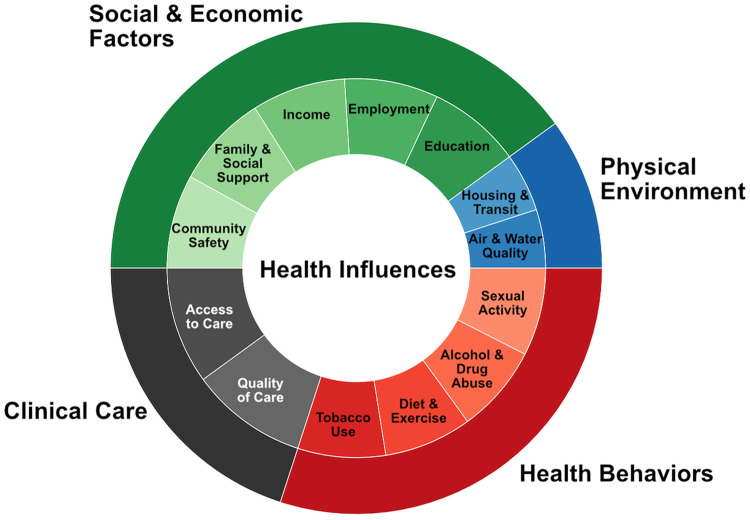
Currently, collecting patient-level SDOH data requires documentation by health care providers (eg, in an encounter note in the EHR), self-reported patient questionnaires (paper or electronic), or prospective data collection by researchers for a particular study. Beyond basic demographic information, home address, and history of smoking or substance use, key SDOH measures are not routinely collected by clinicians and health systems despite demonstrated association and causal impact on health outcomes (Figure 1).22,23 Relevant factors not generally collected include food and housing insecurity, employment barriers, past exposures to abuse (verbal, physical, and sexual), residence in social environments that perpetuate trauma risk, and estimates of social isolation. In the rare cases that such data are collected, care providers often do not use validated instruments raising concerns about data interpretation and secondary use.24 As a result, individual-level SDOH data collection typically exists in many different formats through various modalities of collection and without a robust underlying framework that could facilitate clinical care, research, and population health management.
Figure 1.
Health influences. Figure 1 has been adapted from County Health Rankings model © 2014 University of Wisconsin-Madison Public Health Institute. http://www.countyhealthrankings.org/what-is-health. The size of each section in the outer loop is associated with estimated influence. Inner loop is split evenly among groups.
Some efforts are being made to address this shortcoming. For example, the PRAPARE tool (Protocol for Responding to and Assessing Patients’ Assets, Risk, and Experiences) aims to standardize data collection on several actionable core domains of social determinants such as housing stability, income, and social integration and support.25 Domains were prioritized for screenings in community health centers, yet the tool has been adapted for use by other institutions in several US regions.26,27 The availability of PRAPARE and other similar tools, such as HealthBegins and WellRx, are necessary first steps, but they have yet to be implemented broadly across EHR systems or integrated into clinical workflows in facilities caring for patients with mental health disorders (such as primary care settings, specialty and mental health clinics, and free-standing acute mental health facilities).28–30 More widespread adoption would increase the rate at which such tools are validated across dimensions (ie, internal and external) and improve data collection efforts and our understanding of the health contributions of specific social risk factors.
Some progress can be made by supplementing existing tools. Whereas many of the existing survey tools capture data across a range of social needs, domain-specific question sets should be created and incorporated to supplement such tools and to target distal factors affecting mental health. These factors may include life satisfaction, life meaning and purpose, and beneficial and adverse events in the home or community that impact community stakeholders and neighborhood perception.31 Additional questions for patients already receiving mental health care could cover structural and attitudinal barriers to treatment, time until treatment is sought, and online resources used for answers or guidance (ie, forums, social media, non-/academic sites).32 By routinely collecting these data, we can start to address knowledge gaps around how social factors influence mental health outcomes and design care models to address them.
In addition to new prospective SDOH data collection methods, natural language processing (NLP) and advanced machine learning (ML) algorithms can be leveraged to mine existing sources to extract existing data. In many cases, at least some information about a patient’s social situation is recorded by clinicians in EHR notes. Current work at the intersection of social media and health has also shown that some people may also choose to discuss health-related information and behaviors online through social media channels. NLP, ML and other semantic methodologies (ie, abstracting meaningful data through contextualized processing) are currently being developed to extract race and ethnicity, suicidal ideation and attempts, and problem opioid use from EHR clinical notes and social media data.33–37 These methods could be extended to extract individual-level concepts such as emotional well-being, financial stability, and other social factors associated with mental health.38,39 Although these extraction methods may not be as comprehensive as rigorous, prospective data collection tools–and require significant effort to develop–they are able to generate “new” structured data from unstructured sources and potentially improve secondary use of relevant social and health information.
The integration of advanced analytical tools that incorporate SDOH within EHRs raises the issue of interoperability with internal and external systems as a key challenge. EHRs typically lack robust data interoperability and information exchange capabilities and suffer from information redundancy due to data silos. As the amount of SDOH data increases, so too will the work needed to track concept variations, account for duplicates, and maintain parsimonious data models. By adopting standardized health care data standards and vocabularies, such as LOINC (Logical Observation Identifiers Names and Codes) and SNOMED, to describe and classify SDOH concepts, health systems can reduce superfluous, nonstandardized data and better incorporate these concepts into clinical care and decision-support systems.40,41 Clinical research, community health reporting, and other forms of secondary data uses will benefit from a more unified and uniform representation of data. Whereas there remains the possibility of data multiplicity and variability even with standardized terminologies, health systems can take important steps toward increased data efficiency and interoperability by adopting such data standards.
IMPLICATIONS FOR HEALTH EQUITY
Better collection of SDOH data offers clinicians and health systems the opportunity to identify social correlates of health outcomes that may be missed by routine clinical data elements. Given the broad and profound impact social determinants have on mental and physical health outcomes, it may not be enough to collect narrowly defined social factors like gender, education, poverty, and disability.42 Further efforts should also aim to capture structural and contextual factors strongly associated with health inequity such as housing security, unemployment, child abuse/neglect, neighborhood conditions, and social support.43–45
A risk of many informatics-based interventions is that they may exacerbate inequities by disproportionately benefiting higher SES individuals through better access, adoption, adherence, and effectiveness measures.46 Patients struggling with mental health disorders may be particularly at risk given the continued stigma around mental illness in many communities.47–50
To minimize potential bias, SDOH data should be collected from both traditional (ie, clinical encounters) and non-traditional sources (ie, social media, forums, wearables, mobile apps, and chatbots). NLP, ML and semantically-enhanced methodologies can be applied to social media platforms to augment community-level health surveillance and thus “listen” to individuals who may not be seeking care, but who nonetheless publicly share details related to depression, suicidal ideation/attempts, or other mental health concerns.51,52 Relevant signals gleaned from social media can then be used to assess the risk factors of a particular community without invading the privacy of any 1 individual. These data streams can be mined in parallel with active and passive collection of individual-level social data to explore novel relationships through applied ML techniques. ML, in turn, may become hypothesis-generating for further investigations on the impacts of SDOH and potential interventions.
Bridging the knowledge gap is an attainable goal and may allow for carefully designed interventions and policies that increase access, reduce attrition, and improve effectiveness.53–58 Having access to a more robust set of patient social variables will also allow investigators to 1) perform more sophisticated sampling and recruitment methods, 2) report relevant SES, language, neighborhood, and demographic information; and 3) conduct subgroup analyses with greater accuracy by stratifying across multiple social statuses.59,60 Research can also take a step further from drawing simple associations by testing increased patient empowerments as well as interventions across groups to determine which interventions are most effective and for whom.61–63
CONCLUSION
Despite known associations between social determinants and mental illness, SDOH data are rarely captured in a structured and comprehensive manner by researchers, clinicians, and health systems. In response to increased interest in SDOH data, several collection tools and extraction methods are being developed to facilitate capture of this data and subsequent integration into EHRs. These include survey-based, NLP, and ML methods to collect and characterize attitudinal, structural, and social barriers to care. Incorporation of these data carry the potential to improve care but also to perpetuate or exacerbate existing health disparities if precautions are not taken. But if properly used, better data collection and analysis may allow for the development of new strategies to direct individual patients to appropriate community services, target care toward population-level needs, and reduce barriers to mental health care through informed policy-level decisions.
FUNDING
This work was supported by the National Institutes of Health grant number R01MH105384.
CONTRIBUTORS
JJD, SB, JP, and AS crafted the viewpoint and concept design. JJD, SB, DK, JP, and AS drafted the viewpoint. JJD, SB, DK, JP, AS and provided critical revision of the viewpoint for important intellectual content. JP obtained funding. All authors read and approved the final version of the viewpoint.
Conflict of interest statement
None declared.
REFERENCES
- 1. Freeman A, Tyrovolas S, Koyanagi A, et al. The role of socio-economic status in depression: results from the COURAGE (aging survey in Europe.). BMC Public Health 2016; 16 (1): 1098.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Clark AM, DesMeules M, Luo W, Duncan AS, Wielgosz A.. Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol 2009; 6 (11): 712–22. [DOI] [PubMed] [Google Scholar]
- 3. Leng B, Jin Y, Li G, Chen L, Jin N.. Socioeconomic status and hypertension: a meta-analysis. J Hypertens 2015; 33 (2): 221–9. [DOI] [PubMed] [Google Scholar]
- 4. Fan AZ, Strasser SM, Zhang X, Fang J, Crawford CG.. State socioeconomic indicators and self-reported hypertension among US adults, 2011 behavioral risk factor surveillance system. Prev Chronic Dis 2015; 12 (E27). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Colhoun HM, Hemingway H, Poulter NR.. Socio-economic status and blood pressure: an overview analysis. J Hum Hypertens 1998; 12 (2): 91–110. [DOI] [PubMed] [Google Scholar]
- 6. Rabi DM, Edwards AL, Southern DA, et al. Association of socio-economic status with diabetes prevalence and utilization of diabetes care services. BMC Health Serv Res 2006; 6: 124.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Fisher M, Baum F.. The social determinants of mental health: implications for research and health promotion. Aust N Z J Psychiatry 2010; 44 (12): 1057–63. [DOI] [PubMed] [Google Scholar]
- 8. Osborn DP. The poor physical health of people with mental illness. West J Med 2001; 175 (5): 329–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lawrence D, Hancock KJ, Kisely S.. The gap in life expectancy from preventable physical illness in psychiatric patients in Western Australia: retrospective analysis of population based registers. BMJ 2013; 346: f2539.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kilbourne AM, Morden NE, Austin K, et al. Excess heart-disease-related mortality in a national study of patients with mental disorders: identifying modifiable risk factors. Gen Hosp Psychiatry 2009; 31 (6): 555–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kendrick T. Cardiovascular and respiratory risk factors and symptoms among general practice patients with long-term mental illness. Br J Psychiatry 1996; 169 (6): 733–9. [DOI] [PubMed] [Google Scholar]
- 12. Robson D, Gray R.. Serious mental illness and physical health problems: a discussion paper. Int J Nurs Stud 2007; 44 (3): 457–66. [DOI] [PubMed] [Google Scholar]
- 13. Shonkoff JP, Boyce WT, McEwen BS.. Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA 2009; 301 (21): 2252–9. [DOI] [PubMed] [Google Scholar]
- 14. Suglia SF, Clark CJ, Link B, Koenen KC. Adverse child experiences and socioeconomic status in a nationally representative sample of young adults. In: Society for Epidemiologic Research Annual Meeting; June 16–19, 2015; Denver, CO.
- 15. Lahelma E, Laaksonen M, Martikainen P, Rahkonen O, Sarlio-Lähteenkorva S.. Multiple measures of socioeconomic circumstances and common mental disorders. Soc Sci Med 2006; 63 (5): 1383–99. [DOI] [PubMed] [Google Scholar]
- 16. Hasin DS, Goodwin RD, Stinson FS, Grant BF.. Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry 2005; 62 (10): 1097–106. [DOI] [PubMed] [Google Scholar]
- 17. Zimmerman FJ, Katon W.. Socioeconomic status, depression disparities, and financial strain: what lies behind the income-depression relationship? Health Econ 2005; 14 (12): 1197–215. [DOI] [PubMed] [Google Scholar]
- 18. Gold R, Cottrell E, Bunce A, et al. Developing electronic health record (EHR) strategies related to health center patients’ social determinants of health. J Am Board Fam Med 2017; 30 (4): 428.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Khullar D, Kaushal R. “Precision health” for high-need, high-cost patients. AJMC. https://www.ajmc.com/journals/issue/2018/2018-Vol0260809-n9/precision-health-for-highneed-highcost-patients. Accessed January 8, 2019. [PubMed]
- 20. Olson DP, Oldfield BJ, Morales Navarro S. Standardizing social determinants of health assessments. Health Affairs Blog. https://www.healthaffairs.org/do/10.1377/hblog20190311.823116/full/. Accessed March 20, 2019.
- 21. DeVoe JE, Bazemore AW, Cottrell EK, et al. Perspectives in primary care: a conceptual framework and path for integrating social determinants of health into primary care practice. Ann Fam Med 2016; 14 (2): 104.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Shim RS, Compton MT. Addressing the social determinants of mental health: if not now, when? If not us, who? https://www.ncbi.nlm.nih.gov/pubmed/29852822. Accessed January 8, 2019. [DOI] [PubMed]
- 23. Lund C, Brooke-Sumner C, Baingana F, et al. Social determinants of mental disorders and the Sustainable Development Goals: a systematic review of reviews. Lancet Psychiatry 2018; 5 (4): 357–69. [DOI] [PubMed] [Google Scholar]
- 24. Bolarinwa OA. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Niger Postgrad Med J 2015; 22 (4): 195–201. [DOI] [PubMed] [Google Scholar]
- 25.National Association of Community Health Centers. PRAPARE. https://www.nachc.org/research-and-data/prapare/. Accessed January 8, 2019.
- 26. Gold R, Bunce A, Cowburn S, et al. Adoption of social determinants of health EHR tools by community health centers. Ann Fam Med 2018; 16 (5): 399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Billioux A, Verlander K, Anthony S, Alley D Standardized Screening for Health-Related Social Needs in Clinical Settings: The Accountable Health Communities Screening Tool. NAM Perspectives. Discussion Paper. Washington, DC: National Academy of Medicine; 2017. [Google Scholar]
- 28. SIREN. Social Need Screening Tools Comparison Table. https://sirenetwork.ucsf.edu/tools-resources/mmi/screening-tools-comparison/adult-nonspecific. Accessed January 8, 2019.
- 29.HealthBegins. Resources for Social Determinants of Health. https://www.healthbegins.org/resources-for-social-determinants-of-health.html. Accessed March 17, 2019.
- 30. Page-Reeves J, Kaufman W, Bleecker M, et al. Addressing social determinants of health in a clinic setting: the WellRx pilot in Albuquerque, New Mexico. J Am Board Fam Med 2016; 29 (3): 414–8. [DOI] [PubMed] [Google Scholar]
- 31.HealthMeasures. Intro to PROMIS. http://www.healthmeasures.net/explore-measurement-systems/promis/intro-to-promis. Accessed February 21, 2019.
- 32. Mojtabai R, Olfson M, Sampson NA, et al. Barriers to mental health treatment: results from the National Comorbidity Survey Replication. Psychol Med 2011; 41 (08): 1751–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sholle ET, Adekkanattu P, Davila MA, et al. Supporting research in vulnerable populations through identification of patients’ race and ethnicity using natural language processing of free text clinical notes. JAMIA 2019. [Google Scholar]
- 34. Gaur M, Alambo A, Sain JP, et al. Knowledge-aware assessment of severity of suicide risk for early intervention. In: Association for Computing Machinery; 2019.
- 35. Alambo A, Gaur M, Lokala U, et al. Question answering for suicide risk assessment using reddit. In: IEEE; 2019.
- 36. Gaur M, Kursuncu U, Alambo A, et al. “Let Me Tell You About Your Mental Health!” Contextualized classification of reddit posts to DSM-5 for web-based intervention. In: Association for Computing Machinery;2018.
- 37. Saxena A. A Semantically Enhanced Approach to Identify Depression-Indicative Symptoms Using Twitter Data; 2018. https://corescholar.libraries.wright.edu/etd_all/1973/. Accessed February 28, 2019.
- 38. Viseu J, Leal R, deJesus SN, Pinto P, Pechorro P, Greenglass E. Relationship between economic stress factors and stress, anxiety, and depression: Moderating role of social support. Psychiatry Res 2018; 268:102–7. [DOI] [PubMed]
- 39. Caspi A, Sugden K, Moffitt TE, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT Gene. Science 2003; 301 (5631): 386–9. [DOI] [PubMed] [Google Scholar]
- 40. LOINC—The freely available standard for identifying health measurements, observations, and documents. https://loinc.org. Accessed January 8, 2019.
- 41. SNOMED Home page. SNOMED. http://www.snomed.org. Accessed January 8, 2019.
- 42. Marmot M, Friel S, Bell R, Houweling TAJ, Taylor S.; Commission on Social Determinants of Health. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 2008; 372 (9650): 1661–9. [DOI] [PubMed] [Google Scholar]
- 43. Braveman P, Gottlieb L.. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep 2014; 129 (Suppl 2): 19–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Ottersen OP, Dasgupta J, Blouin C, et al. The political origins of health inequity: prospects for change. Lancet 2014; 383 (9917): 630–67. [DOI] [PubMed] [Google Scholar]
- 45. Plamondon KM, Bottorff JL, Caxaj CS, Graham ID.. The integration of evidence from the Commission on Social Determinants of Health in the field of health equity: a scoping review. Crit Public Health 2018: 1–14. [Google Scholar]
- 46. Veinot TC, Mitchell H, Ancker JS.. Good intentions are not enough: how informatics interventions can worsen inequality. J Am Med Inform Assoc 2018; 25 (8): 1080–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ.. Stigmatisation of people with mental illnesses. Br J Psychiatry 2000; 177: 4–7. [DOI] [PubMed] [Google Scholar]
- 48. Sirey JA, Bruce ML, Alexopoulos GS, et al. Perceived stigma as a predictor of treatment discontinuation in young and older outpatients with depression. AJP 2001; 158 (3): 479–81. [DOI] [PubMed] [Google Scholar]
- 49. Berger M, Wagner TH, Baker LC.. Internet use and stigmatized illness. Soc Sci Med 2005; 61 (8): 1821–7. [DOI] [PubMed] [Google Scholar]
- 50. Davies MR. The stigma of anxiety disorders. Int J Clin Pract 2000; 54 (1): 44–7. [PubMed] [Google Scholar]
- 51. Nguyen QC, McCullough M, Meng H-W, et al. Geotagged US tweets as predictors of county-level health outcomes, 2015–2016. Am J Public Health 2017; 107 (11): 1776–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Nguyen QC, Meng H, Li D, et al. Social media indicators of the food environment and state health outcomes. Public Health 2017; 148: 120–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Osborne H. Health literacy: how visuals can help tell the healthcare story. J Vis Commun Med 2006; 29 (1): 28–32. [DOI] [PubMed] [Google Scholar]
- 54. Arcia A, Suero-Tejeda N, Bales ME, et al. Sometimes more is more: iterative participatory design of infographics for engagement of community members with varying levels of health literacy. J Am Med Inform Assoc 2016; 23 (1): 174–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Houts PS, Witmer JT, Egeth HE, Loscalzo MJ, Zabora JR.. Using pictographs to enhance recall of spoken medical instructions II. Patient Educ Couns 2001; 43 (3): 231–42. [DOI] [PubMed] [Google Scholar]
- 56. Greenhalgh T. Health literacy: toward system level solutions. BMJ 2015; 350 (13): h1026.. [DOI] [PubMed] [Google Scholar]
- 57. Hardy J, Veinot TC, Yan X, et al. User acceptance of location-tracking technologies in health research: implications for study design and data quality. J Biomed Inform 2018; 79: 7–19. [DOI] [PubMed] [Google Scholar]
- 58. Kukafka R, Khan SA, Hutchinson C, et al. Digital partnerships for health: steps to develop a community-specific health portal aimed at promoting health and well-being. AMIA Annu Symp Proc 2007; 2007: 428–32. [PMC free article] [PubMed] [Google Scholar]
- 59. O’Neill J, Tabish H, Welch V, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol 2014; 67 (1): 56–64. [DOI] [PubMed] [Google Scholar]
- 60. Attwood S, van Sluijs E, Sutton S.. Exploring equity in primary-care-based physical activity interventions using PROGRESS-Plus: a systematic review and evidence synthesis. Int J Behav Nutr Phys Act 2016; 13: 60.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Barreto ML, Garcia AM, Bobak M, Aquino R, Porta M.. JECH: new editorial directions. J Epidemiol Community Health 2009; 63 (1): 1–2. [DOI] [PubMed] [Google Scholar]
- 62. Bambra C, Gibson M, Sowden A, Wright K, Whitehead M, Petticrew M.. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. J Epidemiol Community Health 2010; 64 (4): 284–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Sheth A, Jaimini U, Thirunarayan K, Banerjee T.. Augmented personalized health: how smart data with IoTs and AI is about to change healthcare. RTSI 2017; 2017. doi: 10.1109/RTSI.2017.8065963. [DOI] [PMC free article] [PubMed] [Google Scholar]