Abstract
Objective
The study sought to determine whether interoperable, electronic health record–based referral (eReferral) produces higher rates of referral and connection to a state tobacco quitline than does fax-based referral, thus addressing low rates of smoking treatment delivery in health care.
Materials and Methods
Twenty-three primary care clinics from 2 healthcare systems (A and B) in Wisconsin were randomized, unblinded, over 2016-2017, to 2 smoking treatment referral methods: paper-based fax-to-quit (system A =6, system B = 6) or electronic (eReferral; system A = 5, system B = 6). Both methods referred adult patients who smoked to the Wisconsin Tobacco Quitline. A total of 14 636 smokers were seen in the 2 systems (system A: 54.5% women, mean age 48.2 years; system B: 53.8% women, mean age 50.2 years).
Results
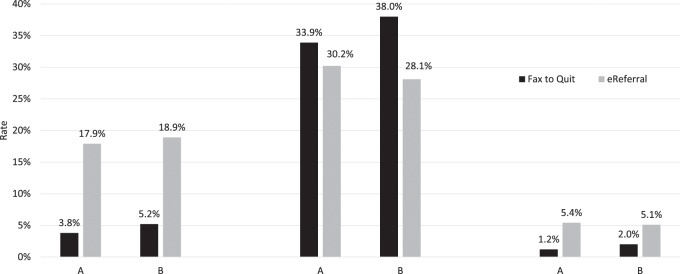
Clinics with eReferral, vs fax-to-quit, referred a higher percentage of adult smokers to the quitline: system A clinic referral rate = 17.9% (95% confidence interval [CI], 17.2%-18.5%) vs 3.8% (95% CI, 3.5%-4.2%) (P < .001); system B clinic referral rate = 18.9% (95% CI, 18.3%-19.6%) vs 5.2% (95% CI, 4.9%-5.6%) (P < .001). Average rates of quitline connection were higher in eReferral than F2Q clinics: system A = 5.4% (95% CI, 5.0%-5.8%) vs 1.3% (95% CI, 1.1%-1.5%) (P < .001); system B = 5.3% (95% CI, 5.0%-5.7%) vs 2.0% (95% CI, 1.8%-2.2%) (P < .001).
Discussion
Electronic health record–based eReferral provided an effective, closed-loop, interoperable means of referring patients who smoke to telephone quitline services, producing referral rates 3-4 times higher than the current standard of care (fax referral), including especially high rates of referral of underserved individuals.
Conclusions
eReferral may help address the challenge of providing smokers with treatment for tobacco use during busy primary care visits.
ClinicalTrials.gov; No. NCT02735382.
Keywords: electronic health record, eReferral, smoking cessation, interoperability
INTRODUCTION
Counseling and medication can double or triple a smoker’s chance of quitting successfully.1,2 Yet, despite the severe health toll of smoking,3,4 the great majority of smokers making healthcare visits do not receive these treatments during their visits.1,5–7 This article evaluates an innovative strategy using the electronic health record (EHR) to address this treatment gap.
The steps needed to effectively deliver smoking treatment in health care can be organized using the 5 A’s1: asking about smoking status, advising the patient to quit, assessing willingness to try to quit, assisting the smoker to quit with counseling and medication, and arranging follow-up to provide additional support and treatment. It has proven very difficult to ensure that the 5 A’s are consistently delivered or offered when patients make healthcare visits.1,6,8
Strategies such as academic detailing and expanding the vital signs to include smoking can increase rates of execution of the first 3 A’s (asking, advising, and assessing willingness to quit),6 but are less effective in increasing rates of assisting in the quit attempt or arranging follow-up.6,9–11 It has been especially difficult to use the healthcare visit to increase rates of delivery of both counseling and pharmacotherapy, the treatment recommended in the 2008 Public Health Service Clinical Practice Guideline1 and the U.S. Preventive Services Task Force 2015 recommendations.12
The EHR can be used to facilitate referral of patients to outside evidence-based treatment resources such as state tobacco quitlines, which are available nationwide in the United States and often provide both smoking counseling and medication. In theory, EHR referrals (eReferral) to quitlines could address obstacles to systematically intervening with smoking during primary care visits,13–15 and could redress persistent racial and socioeconomic disparities in smoking cessation treatment access by prompting referral offers for every patient.8,16,17 Such disparities contribute to increased burden from tobacco use among minority and socioeconomically disadvantaged smokers, and reducing these disparities is a high priority.3,18,19 One strategy is to use the EHR to prompt paper-fax referrals to smoking treatment quitlines (fax-to-quit [F2Q]). However, even with EHR prompting, referrals to quitline via paper faxes tend to be rare (eg, rates of quitline referral and connection of 0.7% and 0.4%, respectively).14,15,20–22
eReferral to the quitline (entirely EHR-based) may be more effective than F2Q because it is less burdensome and less disruptive to existing clinic workflows that are increasingly facilitated by the EHR. For instance, eReferral can prefill referral forms with key patient information and facilitate referral orders via several EHR clicks. This kind of computerized decision support (CDS) has been shown to influence clinician performance,23–25 particularly in preventive care,25,26 and be useful in preventing illness.26 However, if eReferral is to work effectively and be adopted, it must overcome the key challenge of interoperability (ie, secure and Health Insurance Portability and Accountability Act–compliant exchange of health information between a health system and an outside treatment resource such as a quitline).27 If interoperability can be achieved, eReferral efficiencies may foster higher clinic-based quitline referral rates.
In 1 nonexperimental study of eReferral,28 we developed EHR resources that include a secure, closed-loop EHR referral system to refer patients making healthcare visits to a state tobacco quitline with treatment service data electronically returned from the quitline to clinics, including updating the patient’s medication list. When these EHR enhancements were implemented in the 2 clinics in this study, quitline referrals increased from 0.3% to 14% of adult patients who smoked.28 eReferral has been evaluated in other nonexperimental studies.29,30
No prior randomized experiment has evaluated interoperable eReferral to external smoking cessation treatment resources. Building on our pilot findings,28 the present randomized controlled trial comprises 23 clinics from 2 healthcare systems that had previously used paper F2Q quitline referral, with 12 randomized to continue using F2Q and 11 switched to eReferral. Clinic performance was compared over 6 months before and after implementation.
METHODS
Study Design
This 2-group cluster-randomized trial compared eReferral vs paper-based F2Q referral of primary care adult (18 years of age and older) outpatients to a tobacco treatment quit line.
Setting
Two not-for-profit integrated healthcare delivery systems in southern Wisconsin participated. At study inception, system A comprised 19 primary care clinics while system B comprised 53 primary care clinics. Both systems used an Epic-licensed EHR (Epic Systems, Verona, WI).
Clinic Randomization and Masking
Eligibility requirements included provision of clinic based primary care (general internal medicine, family practice), ≥3 primary care clinicians (physicians or nurse practitioners or physician assistants who see patients independently of a physician), volume >60 patients/week; prior training in F2Q to the Wisconsin Tobacco Quitline (WTQL), and willingness to accept random assignment. A Multiattribute Utility Measurement randomization strategy was used to randomize eligible clinics to conditions, balancing number of primary care providers, smoking prevalence, and rate of F2Q referral during a 1-year baseline period. Clinic personnel were not blinded as to their experimental condition.
Overview of F2Q and eReferral Workflows
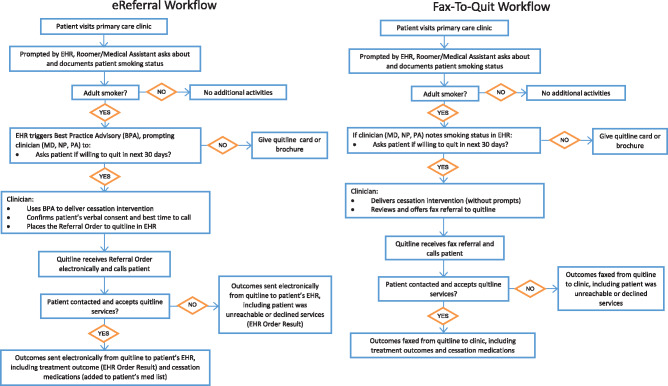
Workflows for both conditions began with documenting the patient’s smoking status or tobacco use during vital signs assessment (the existing standard) and ended with the quitline returning service receipt information to the clinic (Figure 1).
Figure 1.
Clinic workflows for electronic health record (EHR)–based referral (eReferral) and fax-based referral of patients to the Wisconsin Tobacco Quit Line. MD: medical doctor; NP: nurse practitioner; PA: physician’s assistant.
F2Q Workflow
The EHR prompted the roomer (typically medical assistants) to ask and document smoking status for all adult patients. This EHR documentation was available to clinicians, possibly prompting them to advise smokers to quit and to ask about interest in treatment, including WTQL referral. Patients accepting referral received a quitline information sheet and completed a paper consent-referral form, which was faxed to the quitline.
After contacting the patient or exhausting 5 call attempts, the quitline sent a return fax to a clinic liaison detailing services provided: ie, patient reached or not, accepted or declined treatment services, quit date if set, medications mailed or not (2-week supply of nicotine replacement therapy [NRT]). The clinic liaison was instructed to scan the quitline report into the EHR and distribute it as per clinic practice.
eReferral Workflow
The CDS for referral to the WTQL was built into the EHR using both an alert and a prefilled referral order template. First, the EHR prompted roomers (typically medical assistants) to ask about and document the smoking status of all patients. The EHR automatically then triggered an alert for adult smokers, which appeared when the clinician opened the patient encounter. The alert included a recommended script for encouraging the patient to quit smoking and assessing interest in quitting via the WTQL, and gave the clinicians the option to open the order template or note that the patient declined referral. For interested patients, the order entry template was prefilled with patient contact information and prompted clinicians to ask about (1) best time to call (to enhance patient acceptance of WTQL calls) and (2) confirmation of the patient’s verbal referral consent. Closing this order template pended the order. Approving the order triggered immediate electronic transmission of the referral to the WTQL, which provided standard protocol services as in F2Q.
The WTQL then electronically transmitted a service use outcome report that populated the patient’s EHR as a referral order result. These reports included the same outcome information as in F2Q (ie, patient reached or not reached, accepted or declined treatment, quit date, NRT provided or not).
Intervention components
Health System eReferral EHR Customization
Following Adsit et al,28 base functionality for quitline eReferral was programmed and openly available as an Epic foundational component beginning in 2016. However, implementation requires the health system’s information technology department to activate this functionality using technical specifications provided by Epic and the WTQL vendor (Optum, Inc, Eden Prairie, MN) and facilitated by an Epic build guide. This customizes the health systems’ EHR configuration, including secure interface connections for message transmission.
Alert functionality differed in the 2 health systems: clinicians in healthcare system A had to document an alert response to end the encounter (“hard stop”) while healthcare system B clinicians could override (bypass) the alert. The visual display of the alert also differed in the 2 healthcare systems. It was a vividly colored alert tab in healthcare system A and a “pop-up” in healthcare system B. While healthcare system A alerts targeted “tobacco use,” healthcare system B alerts targeted “smoking.” Data in the current article concern only patients identified as smokers.
Implementation and training
Quitline eReferral was tested in 1 pilot site from each health system; this included training, implementation, and troubleshooting over 1-2 months. Data from the pilot clinics are not included in the results reported.
Rollout in the 23 experimental clinics began with 30- to 60-minute on-site training for all clinic staff led by study personnel and a University of Wisconsin Center for Tobacco Research and Intervention regional outreach specialist. For F2Q clinics, this emphasized the importance of tobacco treatment, WTQL services, and staff and clinician roles in the F2Q clinics. For eReferral clinics, sessions were similar but included overviews of the eReferral process including a demonstration of the new EHR screenshots and functionality (by healthcare system information technology trainers). The regional outreach specialist contacted each clinic manager 1 week later to respond to questions. A second educational session occurred approximately 30 days after the intervention was launched at each clinic and reviewed the clinic workflow, elicited feedback, and engaged in problem solving if needed.
For all clinic sites, the WTQL emailed monthly quitline referral summary reports to clinic managers to permit performance feedback to clinicians. The first randomized clinic was launched in October 2016; the last postintervention data collection occurred on October 2017.
Target population, data collection, and study measures
For all clinic sites, data on referral rates were extracted from the WTQL databases (indicating referring clinics) because faxed referrals were not tracked systematically by healthcare systems.
Data were extracted from each health system’s EHR for 6 months before and 6 months after each clinic’s intervention implementation date. These data pulls and WTQL data revealed the proportion of adult smokers visiting the clinics who were referred to the WTQL.
Statistical methods
Power for the primary aim was calculated a priori for a 2-group cluster-randomized design with clinic as the unit of randomization (n = 6 clinics per condition for each health system) with an estimated 90 smokers seen in each clinic per month. A difference between conditions for the postintervention proportion of referrals per month of 2% vs 7% (standard deviation for mean proportion/month = 2.5%) was assumed. Power exceeded .80 (α = .05, 2-tailed). Chi-square tests were used to test for proportions and t statistics were used to test for differences in continuous variables.
RESULTS
Healthcare system A
Demographics
Demographic data for all F2Q and eReferral adult clinic patients are presented in Table 1 for the 6-month pre- and postimplementation periods. Detailed demographic characteristics for referred patients are available for only eReferred patients; faxed referral could not be linked accurately with demographic data.
Table 1.
Demographic variables for the F2Q and eRef clinics before and after implementation: healthcare system A
|
6 Months Preimplementation
|
6 Months Postimplementation
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Adult Patients |
Patients Who Smoke |
Patients Who Smoke |
eReferred
a
|
|||||||||
| F2Q (n = 18 984) | eRef (n = 23 295) | t/χ2 | F2Q (n = 3060) | eRef (n = 3387) | t/χ2 | F2Q (n = 3020) | eRef (n = 3415) | t/χ2 | Yes (n = 610) | No (n = 2805) | t/χ2 | |
| Age, y | 52.2 ± 2.7b | 58.0 ± 3.6b | 181.6** | 46.1 ± 2.1b | 49.8 ± 3.7b | 48.3** | 46.7 ± 1.8b | 49.8± 3.7b | 42.1** | 49.8 ± 3.7 | 50.1 ± 3.4b | −0.1 |
| Male | 7846 (41.3) | 10 656 (45.7) | 498.4** | 1251 (40.9) | 1616 (47.7) | 30.1** | 1300 (43.1) | 1633 (47.8) | 14.5** | 267 (43.8) | 1366 (48.7) | 4.7* |
| Female | 11 138 (58.7) | 12 639 (54.3) | 1809 (59.1) | 1771 (52.3) | 1720 (57.0) | 1782 (52.2) | 343 (56.2) | 1439 (51.3) | ||||
| White | 18 303 (96.4) | 22 830 (98.0) | 101.3** | 2921 (95.5) | 3281 (96.9) | 7.8* | 2800 (95.4) | 3290 (96.3) | 3.8 | 582 (95.4) | 2708 (97.6) | 2.0 |
| African American | 162 (0.9) | 204 (0.9) | 0.04 | 58 (1.9) | 76 (2.2) | 0.8 | 67 (2.2) | 82 (2.4) | 0.1 | 21 (3.4) | 61 (2.2) | 2.9 |
| Asian, Native American/American Indian, Native Hawaiian or Pacific Islander | 492 (2.6) | 234 (1.0) | 155.3** | 76 (2.5) | 27 (0.8) | 28.1** | 66 (2.2) | 39 (1.1) | 11.2* | 7 (1.1) | 32 (1.1) | 0.0 |
| Commercial insurance | 10 016 (52.8) | 9346 (40.1) | 672.7** | 1287 (42.1) | 1284 (37.9) | 11.2* | 1322 (43.8) | 1341 (39.3) | 13.2* | 211 (34.6) | 1130 (40.3) | 6.6* |
| Medicaid | 2013 (10.6) | 1659 (7.1) | 159.5** | 793 (25.9) | 785 (23.2) | 6.4* | 785 (26.0) | 828 (24.3) | 2.5 | 182 (29.8) | 646 (23.0) | 12.3** |
| Medicare | 6153 (32.4) | 11 595 (49.8) | 1293.7** | 702 (22.9) | 1083 (32.0) | 65.1** | 689 (22.8) | 1023 (30.0) | 41.5** | 176 (28.9) | 847 (30.2) | 0.4 |
| Uninsured | 802 (4.2) | 695 (3.0) | 46.8** | 278 (9.1) | 235 (6.9) | 9.8* | 223 (7.4) | 223 (6.5) | 1.7 | 41 (6.7) | 182 (6.5) | 0.0 |
Values are mean ± SD or n (%).
eRef = electronic health record–based referral; FTQ: fax-to-quit.
Demographics are unavailable for fax-referred patients because faxed referrals were not consistently documented in the electronic health record.
Standard deviation is standard deviation across mean aggregate patient age in clinics, not patients; aggregate age for smokers not eReferred was not gathered from the electronic health record.
P < .05.
P < .0001.
As shown in Table 1, among smokers from eReferral clinics, those eReferred to the quitline were more likely to be Medicaid recipients than were those not referred, and were less likely to have private insurance. eReferred and non-eReferred smokers did not differ significantly in racial composition, but women were overrepresented among those eReferred, relative to those not eReferred.
Patient-Level Data Pre- and Postimplementation
The following represent patient-level data (they pertain to individual patients’ outcomes and not visit outcomes). Documented ask rates regarding tobacco use were quite high (>95%) for both conditions during pre- and postimplementation (Table 2; Supplementary Table 1). Rates of documented current smoking across clinics ranged from about 9%-24% preimplementation and 9%-23% postimplementation. Mean smoking prevalence was slightly higher in F2Q clinics than in eReferral clinics both pre- and postlaunch (Table 2; Supplementary Table 1).
Table 2.
Summary data on rates of smoking documentation and quit line referral for both healthcare systems
|
6 Months Preimplementation
|
6 Months Postimplementation
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Adult Patient Volume | Asked About Tobacco | Current Smokers | Adult Patient Volume | Asked About Tobacco | Current Smokers | Smokers Referred to Quitline | Referred Connecting With Quitlinea | |||
| Healthcare System A | ||||||||||
| F2Q | 19 915 | 18 268 (96.2) | 3060 (16.1) | 18 917 | 18 434 (97.5) | 3020 (16.0) | 115 (3.8) | 39 (33.9) | ||
| eRef | 23 295 | 23 197 (99.6) | 3387 (14.5) | 23 241 | 23 183 (99.8) | 3415 (14.7) | 610 (17.9) | 184 (30.2) | ||
| F2Q vs eRef χ2 | 1075.0** | 5.7* | 435.1** | 12.9* | 315.3** | 0.5 | ||||
| Healthcare System B | ||||||||||
| F2Q | 30 320 | 29 889 (98.6) | 4703 (15.5) | 28 030 | 2761 (98.5) | 4135 (14.8) | 216 (5.2) | 82 (38.0) | ||
| eRef | 30 206 | 29 705 (98.3) | 4737 (15.7) | 27 030 | 26 455 (97.9) | 4066 (15.0) | 770 (18.9) | 216 (28.1) | ||
| F2Q vs eRef χ2 | 14.2* | 0.3 | 32.6* | 0.9 | 363.2** | 7.4* | ||||
Values are n (%).
eRef = electronic health record–based referral; FTQ: fax-to-quit.
Rate of connecting with the quitline reflects the proportion of patients who accepted a quitline call and at least started quitline registration. It does not necessarily reflect engaging in treatment.
P < .05.
P < .0001.
Averaged postimplementation referral rates were more than 4 times higher in the eReferral condition than in the F2Q condition (17.9% [n = 610 of 3415] vs 3.8% [n = 115 of 3020], respectively) (Table 2; Supplementary Table 1). Clinic-specific preimplementation referral rates are not available. However, a WTQL report shows that WTQL received a total of 6 F2Q referrals from all of the 53 healthcare system A clinics over a 20-month period ending on August 31, 2016. This rate is much lower than the F2Q and eReferral postimplementation rates (Table 2; Supplementary Table 1).
Rates of quitline connection (accepting a quitline call and at least starting quitline registration) were determined as a percentage of all smokers seen in each clinic over the postimplementation period. In F2Q clinics, 39 patients connected with the quitline of 3020 smokers (1.3%) seen in the first 6 months postimplementation. In eReferral clinics, 184 patients connected with the quitline of 3415 smokers seen over the same time period (5.4%), a significantly higher rate (χ21,6435 = 79.18, P < .001) compared with F2Q patients (Figure 2).
Figure 2.
Rates of quitline (QL) referral, connection, and treatment delivered among fax-to-quit and electronic health record–based referral (eReferral) primary care clinics (by healthcare systems A and B).
Rates of connecting with the quitline among those referred to it were quite variable across clinics (range, 6%-55%), but were similar on average in the F2Q and eReferral conditions (39 of 115 [33.9%] vs 184 of 610 [30.2%]) (Table 2; Supplementary Table 1). As such, eReferral appears to increase referral volume without decreasing referral quality (ie, quitline connection).
WTQL data for patients connecting with it indicated that fax-referred and eReferred patients received similar levels of treatment. For instance, for F2Q and eReferral, respectively, 95 of 196 (48.5%) and 17 of 43 (39.5%) were sent NRT (χ21,239 = 1.13, P = .29), and had means of 0.63 ±.054 and 0.69 ± 0.55) for coaching calls completed (t237 = −0.67, P = .51) and 0.23 ± 0.81 and 0.13 ± 0.60 for web coaching logins (t237 = 1.01, P = .31).
Healthcare system B
Demographics
Table 3 presents demographics for the 6-month pre- and postimplementation periods for eReferral and F2Q clinic patients. System B had a far higher proportion of African American patients than did system A (19.2% vs 1%).
Table 3.
Demographic variables for the F2Q and eRef clinics before and after implementation: healthcare system B
|
6 Months Preimplementation
|
6 Months Postimplementation
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All Adult Patients |
Patients Who Smoke |
Patients Who Smoke |
eReferred
a
|
|||||||||
| F2Q (n = 29 710) | eRef (n = 30 816) | t/χ2 | F2Q (n = 4517) | eRef (n = 4923) | t/χ2 | F2Q (n = 4072) | eRef (n = 4129) | t/χ2 | Yes (n = 789) | No (n = 3340) | t/χ2 | |
| Age, y | 56.3 ± 18.1 | 53.8 ± 18.1 | 17.1** | 50.0 ± 14.8 | 49.3 ± 14.8 | 2.5* | 50.3 ± 14.8 | 50.2 ± 14.8 | 0.6 | 50.2 (13.6) | 50.2 (15.1) | 0.1 |
| Male | 13 892 (46.8) | 11 362 (36.9) | 608.3** | 2247 (49.8) | 2128 (43.2) | 40.3** | 2047 (50.3) | 1743 (42.2) | 53.5** | 318 (40.3) | 1425 (42.7) | 1.4 |
| Female | 15 818 (53.2) | 19 454 (63.1) | 2270 (50.3) | 2795 (56.8) | 2025 (49.7) | 2386 (57.8) | 471 (59.7) | 1915 (57.3) | ||||
| White | 24 161 (81.3) | 22 070 (71.6) | 796.7** | 3140 (69.5) | 2943 (59.8) | 94.8** | 2882 (70.8) | 2422 (58.7) | 122.1** | 405 (51.3) | 2017 (62.2) | 22.5** |
| African American | 4389 (14.8) | 7236 (23.5) | 804.6** | 1235 (27.3) | 1813 (36.8) | 100.9** | 1075 (26.4) | 1549 (37.5) | 124.6** | 354 (44.9) | 1195 (36.9) | 22.3** |
| Asian, Native American/American Indian, Native Hawaiian or Pacific Islander | 515 (1.7) | 614 (2.0) | 5.7* | 49 (1.1) | 42 (0.9) | 1.0 | 40 (1.0) | 39 (0.9) | 0 | 8 (1.0) | 31 (1.0) | 0.0 |
| Commercial insurance b | 15 030 (50.6) | 16 317 (53.0) | 33.8** | 2002 (44.3) | 2091 (42.5) | 3.3 | 1772 (43.5) | 1726 (41.8) | 2.5 | 303 (38.4) | 1423 (42.6) | 4.5* |
| Medicaid b | 3397 (11.4) | 4566 (14.8) | 151.5** | 1341 (29.7) | 1670 (33.9) | 19.5** | 1142 (28.1) | 1298 (31.4) | 11.3* | 281 (35.6) | 1017 (30.5) | 7.7* |
| Medicare b | 11 249 (37.9) | 9956 (32.3) | 205.1** | 1162 (25.7) | 1173 (23.8) | 4.6* | 1108 (27.2) | 1068 (25.9) | 1.9 | 205 (26.0) | 863 (25.8) | 0.0 |
| Uninsured b | 365 (1.2) | 337 (1.1) | 2.4 | 108 (2.4) | 83 (1.7) | 5.9* | 104 (2.6) | 100 (2.4) | 0.2 | 17 (2.2%) | 83 (2.5%) | 0.2 |
Values are mean ± SD or n (%).
eRef = electronic health record–based referral; FTQ: fax-to-quit.
Demographics are unavailable for fax-referred patients because faxed referrals were not consistently documented in electronic health record.
The total number of people insured in each category can exceed the total number in some columns due to changes in insurance during the period in question (eg, patients may have gone from having Medicaid to having no insurance).
P < .05.
P < .0001.
Demographic characteristics for referred patients are available for only eReferred patients. As shown in Table 3, among smokers from eReferral clinics, those referred were more likely to be Medicaid-insured than were those not referred, and were less likely to have private or commercial insurance. African-American patients were overrepresented among eReferred patients, and White patients were underrepresented among eReferred patients, relative to those not referred.
Patient-Level Data Pre- and PostImplementation
The following are patient-level data (they pertain to outcomes for individual patients and not per visit outcomes) (Table 2; Supplementary Table 2). Documented ask rates regarding tobacco use exceeded 95% across all clinics during both the 6-month pre- and postimplementation periods. Smoking prevalence was very similar across eReferral and F2Q clinics both pre- and postlaunch (15%). The average referral rate among the eReferral clinics (18.9%) was more than 3 times that of the F2Q clinics (5.2%) (Figure 2). In all of 2016 (preimplementation), the 19 healthcare system B primary care clinics made only 37 fax referrals; thus, the 6-month postimplementation F2Q and eReferral referral rates far exceeded the preimplementation rate.
Rates of connection with the quitline (acceptance of a quitline call and at least starting quitline registration), among all smokers seen in the 6-month postimplementation period were significantly greater with eReferral (216 of 4066 [5.3%]) than with F2Q (82 of 4135 [2.0%] of smokers connected [χ21,8201 = 63.95, P < .001]).
Table 2 and Supplementary Table 2 present rates of connecting with the quitline as a percentage of smokers referred to it. Quitline connection among those referred was significantly higher with F2Q (82 of 216 [38.0%]) than with eReferral (216 of 770 [28.1%]) (P < .05); this became nonsignificant when an outlier F2Q clinic with a 68.4% service acceptance rate was omitted (56 of 178 [31.5%]) (χ21,948 = 0.7, P = .42).
WTQL data for patients connecting with it indicated that fax-referred and eReferred patients received similar levels of treatment. For instance, for F2Q and eReferral, respectively, 55 of 115 (47.8%) and 128 of 233 (54.9%) were sent NRT (χ21,348 = 1.6, P = .21) and had means of 0.68 ± 0.57) and 0.76 ± 0.48 for coaching calls made (t346 = −1.3, P = .19), and means of 0.08 ± 0.38 and 0.11 ± 0.59 web coaching logins (t346 = −0.48, P = .63).
DISCUSSION
Twenty-three primary care clinics in 2 different healthcare systems were randomized to either a F2Q or an eReferral CDS strategy for engaging smokers in evidence based quitline smoking cessation treatment. The F2Q strategy used paper faxes to refer patients to the quitline and to report treatment service outcomes. In contrast, eReferral CDS used the EHR to facilitate secure electronic transmission of referrals to the quitline with outcomes of the referrals electronically returned to the patients’ EHR, thereby achieving both secure interoperability and “closed-loop” functionality. Across both healthcare systems, eReferral produced referral rates that were 3-4 times higher than those produced by F2Q. This, plus examination of treatment connection data, showed that eReferral meaningfully increased the reach of evidence-based tobacco quitline services in primary care, consistent with systematic reviews of CDS systems showing that they improve provision of preventive care.25,26
eReferral achieved especially great reach among Medicaid recipients. Thus, eReferral may address key smoking treatment access disparities.31,32 eReferral could significantly benefit public health if widely adopted because quitline treatment has been shown to increase a smoker’s likelihood of becoming abstinent by 20%-25%.1,33 Adoption of the eReferral strategy is feasible because the tested resources were incorporated into Epic functionality in 2016, making it potentially available Epic users worldwide (eg, more than 200 million Americans have Epic EHR access).34
While previous studies of eReferral yielded promising results, they were all observational (pre-post).28–30 The current research is the first randomized controlled trial to compare eReferral and F2Q in primary care and shows that eReferral reliably increases quitline referral rates relative to fax referral and does so across multiple clinics in 2 different health systems with different patient demographics.
eReferral EHR enhancements included EHR-guided smoker identification as in the F2Q clinics, but also prompted assessment of interest in quitline treatment, populated fields in the eReferral form, permitted simple and secure electronic referral to the quitline, and provided closed-loop feedback on quitline service delivery, with quitline outcomes entered into a patient’s EHR.28 As such, this EHR resource can provide sound data related to quality improvement initiatives and external performance standards.
In F2Q, the EHR did not specifically prompt offering quitline treatment (although staff were trained to do so). Also, clinic staff had to complete referral sheets by hand and fax them to the quitline. The quitline provided feedback to the clinic via another paper fax, but this had to be manually scanned into the EHR.
One limitation of the eReferral strategy is that its implementation requires effort by healthcare system information technology and other staff28,35 to customize it. Also, as with any quitline referral strategy, a high proportion of referred patients never actually engage in quitline treatment.8,29,36–38 In the present research, only about one-third of patients who were fax or eReferred actually connected with the quitline. Clearly more needs to be done to increase both referral and treatment engagement rates for smokers making primary care visits. An additional limitation of this research is that we do not present data on long-term abstinence; however, substantial evidence does document the long-term effectiveness of quitline treatment.1,33 It may also be that eReferral was used more heavily by clinic staff in this research because it was a newer strategy for the clinics than was F2Q (ie, reflecting a Hawthorne effect). In addition, the current study documents marked variance in referral and connection rates across clinics, but does not examine patient, clinic, or system characteristics associated with these rates. Hierarchical modeling approaches could identify multilevel factors associated with referral reach, equity, and service connection yield in the future. Strengths of this research included an experimental design with random assignment of clinics, replication across 2 healthcare systems, and use of quitline (vs clinic) data for the referral outcome.
This research shows that an EHR eReferral strategy resulted in rates of quitline referral that were 3-4 times higher than for paper fax referral, and demonstrated impressive reach among certain underserved demographic groups, particularly Medicaid patients. Further, it achieves secure interoperability between healthcare systems and an external treatment resource and it populates the patients’ EHR records with treatment delivery and outcome data. Future researchers should explore methods to increase treatment acceptance by referred smokers and determine the long-term effects of this strategy on smoking prevalence.
FUNDING
This work was supported by National Cancer Institute Grant No. R35 CA197573 awarded to Dr. Michael Fiore.
AUTHOR CONTRIBUTORS
Author contributions were grant development/funding (RA, TB, MF); experimental design (TB, MF); methods development and execution (RA, TB, MF, AG, PH, SL, TM, DM, AS, MZ); data analysis (DM), data interpretation (RA, TB, MF, AG, PH, SL, TM, DM, AS, MZ), writing and manuscript development (RA, TB, MF, AG, PH, SL, TM, DM, AS, MZ).
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGEMENTS
We acknowledge the cooperation and support for this research by the 2 participating healthcare systems Gundersen Health System and Ascension Healthcare. We acknowledge the cooperation of Epic Systems Cooperation including Brad Fox, MD, Thanos Tsiolis, and Aaron Beal. We acknowledge the contributions of Wendy Theobald, Ph.D., at the Center for Tobacco Research and Intervention, University of Wisconsin and Public Health, who provided great assistance with manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Fiore MC, Jaen CR, Baker TB, et al. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services, U.S. Public Health Service; 2008. [Google Scholar]
- 2. Stead LF, Perera R, Bullen C, et al. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev 2012; 11: CD000146. [DOI] [PubMed] [Google Scholar]
- 3. U.S. Department of Health and Human Services. The health consequences of smoking - 50 years of progress: A report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 4. U.S. National Cancer Institute, World Health Organization. The economics of tobacco and tobacco control. National Cancer Institute Tobacco Control Monograph 21, NIH Pub No> 16-CA-8029A; 2016. https://cancercontrol.cancer.gov/brp/tcrb/monographs/21/docs/m21_exec_sum.pdf. Accessed May 21, 2018.
- 5. Centers for Disease Control and Prevention. Quitting smoking among adults - United States 2001-2010. MMWR Morb Mortal Wkly Rep 2011; 60 (44): 1513–9. [PubMed] [Google Scholar]
- 6. Papadakis S, McDonald P, Mullen KA, Reid R, Skulsky K, Pipe A.. Strategies to increase the delivery of smoking cessation treatments in primary care settings: a systematic review and meta-analysis. Prev Med 2010; 51 (3–4): 199–213. [DOI] [PubMed] [Google Scholar]
- 7. Thomas D, Abramson MJ, Bonevski B, George J.. System change interventions for smoking cessation. Cochrane Database Syst Rev 2017; 2: CD010742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Willett JG, Hood NE, Burns EK, et al. Clinical faxed referrals to a tobacco quitline: reach, enrollment, and participant characteristics. Am J Prev Med 2009; 36 (4): 337–40. [DOI] [PubMed] [Google Scholar]
- 9. Milch CE, Edmunson JM, Beshansky JR, Griffith JL, Selker HP.. Smoking cessation in primary care: a clinical effectiveness trial of 2 simple interventions. Prev Med 2004; 38 (3): 284–94. [DOI] [PubMed] [Google Scholar]
- 10. Piper ME, Fiore MC, Smith SS, et al. Use of the vital sign stamp as a systematic screening tool to promote smoking cessation. Mayo Clin Proc 2003; 78 (6): 716–22. [DOI] [PubMed] [Google Scholar]
- 11. Rothemich SF, Woolf SH, Johnson RE, et al. Effect on cessation counseling of documenting smoking status as a routine vital sign: an ACORN study. Ann Fam Med 2008; 6 (1): 60–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Siu AL. U. S. Preventive Services Task Force. Behavioral and pharmacotherapy interventions for tobacco smoking cessation in adults, including pregnant women: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 2015; 163 (8): 622–34. [DOI] [PubMed] [Google Scholar]
- 13. Schroeder SA. What to do with a patient who smokes. JAMA 2005; 294 (4): 482–7. [DOI] [PubMed] [Google Scholar]
- 14. Meredith LS, Yano EM, Hickey SC, Sherman SE.. Primary care provider attitudes are associated with smoking cessation counseling and referral. Med Care 2005; 43 (9): 929–34. [DOI] [PubMed] [Google Scholar]
- 15. Holtrop JS, Malouin R, Weismantel D, Wadland WC.. Clinician perceptions of factors influencing referrals to a smoking cessation program. BMC Fam Pract 2008; 9: 18.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Landrine H, Corral I, Campbell KM.. Racial disparities in healthcare provider advice to quit smoking. Prev Med Rep 2018; 10: 172–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cokkinides VE, Halpern MT, Barbeau EM, Ward E, Thun MJ.. Racial and ethnic disparities in smoking-cessation interventions: analysis of the 2005 National Health Interview Survey . Am J Prev Med 2008; 34 (5): 404–12. [DOI] [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Smoking rates for uninsured and adults on Medicaid more than twice those for adults with private health insurance; 2015. https://www.cdc.gov/media/releases/2015/p1112-smoking-rates.html. Accessed May 29, 2018.
- 19. Clegg LX, Reichman ME, Miller BA, et al. Impact of socioeconomic status on cancer incidence and stage at diagnosis: selected findings from the surveillance, epidemiology, and end results: National Longitudinal Mortality Study. Cancer Causes Control 2009; 20 (4): 417–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Solberg LI, Quinn VP, Stevens VJ, et al. Tobacco control efforts in managed care: what do the doctors think? Am J Manag Care 2004; 10 (3): 193–8. [PubMed] [Google Scholar]
- 21. Bentz CJ, Bayley BK, Bonin KE, et al. Provider feedback to improve 5A's tobacco cessation in primary care: a cluster randomized clinical trial. Nicotine Tob Res 2007; 9 (3): 341–9. [DOI] [PubMed] [Google Scholar]
- 22. Linder JA, Rigotti NA, Schneider LI, Kelley JH, Brawarsky P, Haas JS.. An electronic health record-based intervention to improve tobacco treatment in primary care: a cluster-randomized controlled trial. Arch Intern Med 2009; 169 (8): 781–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Garg AX, Adhikari NK, McDonald H, et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA 2005; 293 (10): 1223–38. [DOI] [PubMed] [Google Scholar]
- 24. Kawamoto K, Houlihan CA, Balas EA, Lobach DF.. Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ 2005; 330 (7494): 765.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Murphy EV. Clinical decision support: effectiveness in improving quality processes and clinical outcomes and factors that may influence success. Yale J Biol Med 2014; 87 (2): 187–97. [PMC free article] [PubMed] [Google Scholar]
- 26. Moja L, Kwag KH, Lytras T, et al. Effectiveness of computerized decision support systems linked to electronic health records: a systematic review and meta-analysis. Am J Public Health 2014; 104 (12): e12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lancet. Making sense of our digital medicine babel. Lancet 2018; 392: 1487.. [DOI] [PubMed] [Google Scholar]
- 28. Adsit RT, Fox BM, Tsiolis T, et al. Using the electronic health record to connect primary care patients to evidence-based telephonic tobacco quitline services: a closed-loop demonstration project. Behav Med Pract Policy Res 2014; 4 (3): 324–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tindle HA, Daigh R, Reddy VK, et al. eReferral between hospitals and quitlines: an emerging tobacco control strategy . Am J Prev Med 2016; 51 (4): 522–6. [DOI] [PubMed] [Google Scholar]
- 30. Warner DD, Land TG, Rodgers AB, Keithly L.. Integrating tobacco cessation quitlines into health care: Massachusetts, 2002-2011. Prev Chronic Dis 2012; 9: E133.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Varghese M, Sheffer C, Stitzer M, Landes R, Brackman SL, Munn T.. Socioeconomic disparities in telephone-based treatment of tobacco dependence. Am J Public Health 2014; 104 (8): e76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bandi P, Cokkinides VE, Virgo KS, Ward EM.. The receipt and utilization of effective clinical smoking cessation services in subgroups of the insured and uninsured populations in the USA. J Behav Health Serv Res 2012; 39 (2): 202–13. [DOI] [PubMed] [Google Scholar]
- 33. Stead LF, Hartmann-Boyce J, Perera R, Lancaster T.. Telephone counselling for smoking cessation. Cochrane Database Syst Rev 2013; 8: CD002850. [DOI] [PubMed] [Google Scholar]
- 34. Epic. In a nutshell; 2017. https://www.epic.com/about. Accessed July 1, 2018.
- 35. Fraser D, Christiansen BA, Adsit R, Baker TB, Fiore MC.. Electronic health records as a tool for recruitment of participants' clinical effectiveness research: lessons learned from tobacco cessation. Behav Med Pract Policy Res 2013; 3 (3): 244–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bentz CJ, Bayley KB, Bonin KE, Fleming L, Hollis JF, McAfee T.. The feasibility of connecting physician offices to a state-level tobacco quit line. Am J Prev Med 2006; 30 (1): 31–7. [DOI] [PubMed] [Google Scholar]
- 37. Piper ME, Baker TB, Mermelstein R, et al. Recruiting and engaging smokers in treatment in a primary care setting: developing a chronic care model implemented through a modified electronic health record. Behav Med Pract Policy Res 2013; 3 (3): 253–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wadland WC, Holtrop JS, Weismantel D, Pathak PK, Fadel H, Powell J.. Practice-based referrals to a tobacco cessation quit line: assessing the impact of comparative feedback vs general reminders. Ann Fam Med 2007; 5 (2): 135–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.