Abstract
Objective
The study sought to develop the necessary elements for a personalized health record (PHR) for youth emancipating from child protective custody (eg, foster care) by collecting thoughts and ideas from current and former foster youth and community stakeholders who have a significant amount of experience working with emancipating young people.
Materials and Methods
We employed a mixed methods, participatory research design using concept mapping to identify key features for PHR across stakeholders.
Results
In the clusters, common themes for necessary elements for a PHR included health education, health tips, medication instructions, diagnoses including severity, and website resources that could be trusted to provide reliable information, and addressed data privacy issues such as the primary user being able to choose what diagnoses to share with their trusted adult and the ability to assign a trusted adult to view a part of the record.
Discussion
By directly involving youth in the design of the PHR, we are able to ensure we included the necessary health and life skills elements that they require. As a PHR is created for foster youth, it is important to consider the multiple uses that the data may have for emancipated youth.
Conclusion
A PHR for foster youth needs to include an appropriate combination of information and education for a vulnerable population. In addition to providing some of their basic health and custody information, a PHR provides an opportunity to give them information that can be trusted to explain common diagnoses, medications, and family health history risks.
Keywords: medical informatics applications, child, foster, concept mapping, pediatrics
INTRODUCTION
There are 479 000 children1 in the custody of child protective services (eg, foster care) in the United States. Children remain in custody an average 19 months, with 26% of children in foster care for more than 2 years. Approximately 24 000 youth emancipate from foster care between the ages of 18 and 20 years old annually.2 Children often enter foster care traumatized by maltreatment and are placed in foster or group homes with unfamiliar caregivers who do not know their health histories. Children in foster care are significantly more likely to suffer from emotional, behavioral, medical, and dental problems3–7 that require healthcare services at higher rates than children in the general population.8 Despite their needs, foster youth fail to receive appropriate health care,9 in part due to the lack of access to health information for foster youth or their caseworkers. Records are lost and health care is disrupted when children enter foster care or change placements.10 To address this issue, our study team developed IDENTITY (Integrated Data Environment to eNhance ouTcomes In cusTody Youth),11,12 a data hub that shares merged child welfare administrative records and electronic health records (EHRs) with caseworkers and clinicians. IDENTITY allows near real-time information exchange of pertinent custody data and vital medical history data with medical providers and county caseworkers. Unfortunately, adolescents in foster care are a particularly vulnerable group and are unable to also access this information for themselves.
While adolescents are in custody, access to their medical records is managed by their caseworker; adolescents report limited access to health information13 and caseworkers and caregivers report not having sufficient health information for the children in their care.10,14 Adolescents experience an average of 7 placement changes during their time in foster care, disrupting their relationships to the adults who can provide health information to them. This lack of health information results in foster youth reporting no knowledge of how to access primary care,15,16 poor management of chronic conditions,16–18 and increased preventable disease.6,19 Foster youth aging out of custody have poor health outcomes,20 including being more likely to define their health as poor and identify as having a disability.21
Only 15% of youth receive transition planning assistance while they are in foster care, and those with chronic conditions are particularly vulnerable.22 Those youth with chronic conditions are vulnerable and are more likely to have medical complications because they lack proper information and a transition plan.22 Foster youth who emancipate are also faced with transitioning from pediatric to adult care. Transitioning to adult care includes self-management, a need for caregiver support, and effective communication.22 The transition planning elements can be important components of a personalized health record (PHR).
Adolescent privacy is a major concern to considering when sharing their medical data in EHRs and PHRs. To protect their privacy and confidentiality, additional education and training is needed for providers, families, and adolescents. The American Academy of Pediatrics has endorsed that “confidentiality protection is an essential component of adolescent health care.”23,24 For children in protective custody, data access is more complex. While caseworkers have legal access to the health data and a limited amount is available for families of origin, foster caregivers are not afforded access to the record. For adolescents, certain elements of their data are protected, such as sexually transmitted infection testing results, and it is important to pay special attention to sharing these when developing an electronic means of sharing data.23
Providing health data from the EHR, including basic information on prescribed medications, major diagnoses, and mental health services could improve health knowledge, care coordination, and patient outcomes in this vulnerable population. We employed concept mapping to include foster and recently emancipated youth and key stakeholders in the area of foster care in the design of the PHR. Concept mapping employs a 4-step procedure of data collection using idea generation, unstructured sorting, feasibility, and importance ratings.25 We followed the concept mapping methodology laid out by Kane and Trochim.26,27 The purpose of our study was to develop the necessary elements for a PHR for youth emancipating out of care by collecting thoughts and ideas from foster youth and community stakeholders, to inform the future development of a PHR for foster youth emancipating out of care.
MATERIALS AND METHODS
We employed a mixed methods, participatory research design using concept mapping to identify key features across all stakeholders. We worked with stakeholders and youth to conduct a concept mapping project that generated and prioritized specific strategies to address PHR data and display. Through brainstorming and sorting steps followed by multidimensional scaling and hierarchical cluster analysis, concept mapping resulted in a structured, data-driven visual representation of thoughts or ideas of these stakeholders group.26 Concept mapping has been used to address substantive issues in health care improvement,28 culturally competent intervention services,29 and health disparities.30 Extensive work has demonstrated both the validity and utility of concept mapping methodology.31,32 Through this process, a diverse perspective of stakeholders was able to emerge. This study was approved by our institutional review board.
Concept mapping procedure
The stakeholders and foster youth collaborated with the research team to conduct the concept mapping project and identify stakeholders divided among: (1) caseworkers, (2) community members and other foster youth, and (3) healthcare providers. Snowball sampling,33,34 whereby initial participants recommend other participants with similar characteristics, was used.
Concept mapping involves 3 main steps. Before beginning, the participant categories are chosen (foster youth and community members) and focus prompts are developed to guide what should be answered. In step 1, idea generation, the participants respond to the prompts. These responses are combined to remove redundancies and then in step 2 are provided to a set of participants for unstructured sorting of the ideas. From here, the third and final step involves applying multidimensional scaling and hierarchical cluster analysis to create a concept map of the ideas grouped by clusters. Last, the maps are interpreted and utilized to inform the next step of the research, which in this case was the create of a web-based PHR for foster youth.
Study participants
We created a foster youth council (FYC) who met and provided input throughout the design process. Without the voice of youth, research can miss the contextual input necessary to represent the unique youth experience, lowering the potential impact and sustainability. As the intended users of the PHR, we involved current and former foster youth in the research design and creation of the PHR prompts. We worked directly with foster youth who were recruited from existing FYCs and caseworker recommendations with additional youth identified peer to peer. The FYC was asked to share opinions and thoughts on health care, their access, the foster system, and what they feel is missing in their current health education.
We also reached out to community stakeholders to advise the research team in the design and development of the elements in the PHR. Guardians ad litem, court-appointed special advocates, case workers, foster caregivers, and community healthcare providers were invited to participate.
Step 1: idea generation
A purposeful sample of diverse community stakeholders and foster youth were asked to generate statements that complete 4 open-ended prompts relevant to providing foster youth PHR access (eg, “To improve health outcomes and promote healthy behaviors in foster youth, I believe we need to…”; “A successful and user-friendly personal health record for foster youth will include…”; “The medical information foster youth need is…”; “A successful and easy-to-use personal health record for foster youth should NOT include…”). Prior to starting the questions, PHR was defined for the participants. This step was conducted via an interactive website, via a telephone discussion, or through email. Statements were captured verbatim. If on paper, the participants filled out the forms on their own in their own language. The results of this step were a diverse set of statements from multiple perspectives relevant to the issue of providing coordinated PHRs to foster youth and helping promote long-term healthy behaviors and help provide tools necessary to transition from pediatric to adult care. Responding to prompts took a few minutes of each participant’s time and could be done during a FYC meeting, online, through email, in person, or over the phone. The goal was to get input about how best to approach and engage foster youth transitioning to adulthood, what factors are most relevant, and the format that will be most helpful for sharing and understanding the PHRs. All statements generated were combined regardless of which participant group initiated them and then were reviewed by three members of the research team to ensure that they were at a similar level of detail, responsive to the focus prompt, and not redundant. In condensing the responses, we combined the 4 prompts into 2 main focus areas, given the similarity of stakeholder responses: (1) primary information included in a PHR and (2) additional information necessary to help the PHR be useful. The final responses were edited for grammar and clarity of expression without altering the original response meaning.
Step 2: unstructured sorting
Foster youth individually sorted the 2 sets of statements into groups of similar ideas or concepts.35,36 The youth sorters received 2 decks of cards representing responses from each of the 2 focus areas. Each card contained 1 item generated in response to the focus
areas along with an identification number. The sorters were asked to individually sort cards into
groups based on their perception of similar ideas. Next, the sorters were directed to place each group of cards into separate envelopes. On the front of the envelope, the sorters were asked to provide a label or name for each group of cards.
Step 3: concept mapping data analysis
We combined the 4 prompts into 2 main themes for analysis. The 2 key themes that emerged were primary information for the PHR, including data elements that should be included in a PHR, and additional information for the PHR, which were items necessary to help make a PHR useful. These 2 themes were used to sort the individual statements and redundancies were removed.
Using open source software in R,37 multidimensional scaling and cluster analysis of the sorting results for each focus area created concept maps to illustrate the conceptual similarity of specific ideas and the aggregation of these ideas into clusters.27,38 Statistical analysis included creation of a summed matrix of responses. Each participant sorted N cards, and for each participant, an NxN matrix was created. If a given participant sorted 2 cards together, the cell representing the intersection of those 2 cards was scored as 1. If a given participant sorted 2 cards separately, the cell of their intersection was scored a 0. The matrices were summed across all participants. In the resulting matrix, the higher the number in any given cell, the more often those 2 items (ie, the items whose row and column intersect at the given cell) were sorted together. Higher numbers were represented on the concept map by closer points on the map (closer x, y coordinates), while lower numbers were represented by larger distances between points on the concept map. This resulted in a 2-dimensional visual representation of the data wherein points close together represent ideas that were closely linked in the minds of the sorters, and points farther apart represent less similar ideas.
Subsequently, the x, y coordinates were analyzed using cluster analysis. Cluster analysis provides a framework to segregate the data points into clusters of similar ideas. Cluster analysis results in as many cluster as sorted responses so a judgement must be made about the appropriate number of total clusters. The goal is to have the fewest clusters possible but express sufficient detail throughout the interpretive process. The final cluster solutions chosen balanced detail with restraint. In the concept map results, a “stress value” for each cluster solution is chosen to best fit the relationship strength of ideas. The stress value helps determine if the map of ideas represents the data and the strength of relationship between distances on the map.27,39 A value of 0.27 (focus area 1) and 0.22 (focus area 2) indicates a good fit which is defined as less than 1% chance that the arrangement of ideas were random. The research team reviewed multiple cluster solutions before determining the appropriate number of clusters. A label for each cluster was created that succinctly expressed the theme and allowed a clear meaning. The research team used labels created by the youth in the sorting process as a guide for creating final names for the clusters.40
RESULTS
Data collection during idea generation included a sample of relevant stakeholders and foster youth (n = 76). Of the participants that shared demographic information, 31 were current and former foster youth (41%), 10 were foster parents or caregivers (13%), 10 were community stakeholders (13%), 12 were health care professionals (16%), and 13 were social service workers (17%). Fourteen youth completed the sorting for focus area 1, and 9 completed the sorting for focus area 2. Unfortunately, data for 2 sorts had to be excluded because all the cards were not sorted. We analyzed 13 sorts for focus area 1 and 8 for focus area 2. It is common within concept mapping to have different samples for each step of the process.40
Stakeholders generated a total of 493 ideas for all the prompts (Table 1). After combining the prompts into 2 main focus areas (primary information included in a PHR and additional information necessary to help the PHR be useful) and removing redundancies, there were 368 unique ideas to be included. The overall responses were represented by 66 unique statements for focus area 1 (primary information included in a PHR) and 53 for focus area 2 (additional information necessary to help the PHR be useful).
Table 1.
Initial responses from all stakeholder and foster youth prompts
| Prompt | Initial responses |
|---|---|
| To improve health outcomes and promote healthy behaviors in foster youth, I believe we need to… | 77 |
| A successful and user-friendly personal health record for foster youth will include…. | 280 |
| The medical information foster youth need is… | 88 |
| A successful and easy-to-use personal health record for foster youth should NOT include… | 48 |
Concept maps
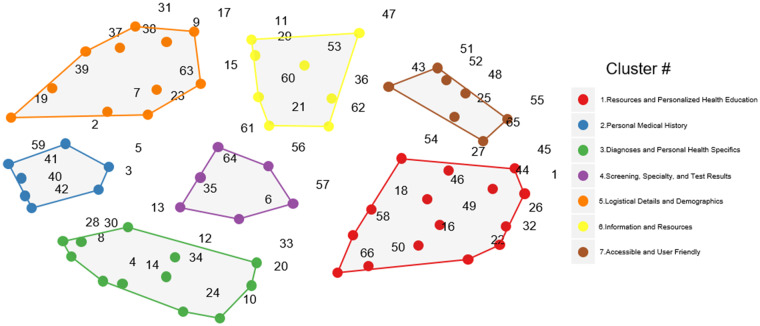
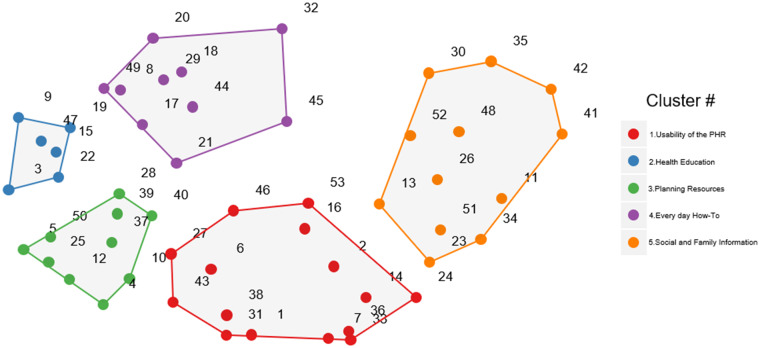
Sorting of the responses for focus area 1 (primary information included in a PHR) was completed by 13 foster youth. The research team chose a 7-cluster solution (stress value = .27) for the focus area 1 (primary information included in a PHR) as the combination of related themes for each of the sorting response categories (Figure 1). The second focus area (additional information necessary to help the PHR be useful) was completed by 8 foster youth. The research team chose a 5-cluster solution (stress value = 0.22) as the combination of related themes for each of the sorting response categories (Figure 2). The concept maps are shown in the figures. Tables 2 and 3 shows example responses in each cluster for the prompts.
Figure 1.
Primary information concept map.
Figure 2.
Additional information concept map. PHR: personalized health record.
Table 2.
Example responses for each cluster for the personalized health record focus area
| Cluster Title | |
|---|---|
| 1. Resources and personalized health education |
|
| 2. Personal medical history |
|
| 3. Diagnoses and personal health specifics |
|
| 4. Screening, specialty, and test results |
|
| 5. Logistical details and demographics |
|
| 6. Information and resources |
|
| 7. Accessible and user friendly |
|
DNR: Do Not Rescucitate; HIV: human immunodeficiency virus; JFS: Job and Family Services.
Table 3.
Example responses for the additional information for the PHR focus area
| Cluster Title | |
|---|---|
| 1. Usability of the PHR |
|
| 2. Health education |
|
| 3. Planning resources |
|
| 4. Every day how-to |
|
| 5. Social and family information |
|
PHR: personalized health record; STI: sexually transmitted infection.
Primary information included in a PHR
Table 2 lists cluster titles and example responses for each of the 7 clusters. Resources and personalized health education included common responses of health education, health tips, medication instructions, and website resources that could be trusted to provide reliable information. Clusters 2 and 3 are heavily related. In Cluster 2 (personal medical history), responses included past medical history specifically prior visits, and past injuries or mental illness diagnoses. In Cluster 3 (diagnoses and personal health specifics), specific items such as blood type, allergies, and immunization records were mentioned. Cluster 4 (specialty and test results), included any laboratory results that could be shared, active subspecialist visits, and discharge summaries. Cluster 5 (logistical details), included next of kin and birth certificates, while cluster 6 (information and resources) also included items such as their health insurance information and their most recently listed pharmacy. Finally, cluster 7 (accessible and user-friendly), addressed the actual look and feel of the data, including that it be internet accessible, easily understandable, and have clear print with good organization.
Additional information necessary to help the PHR be useful
Table 3 lists cluster titles and example responses for the 5 clusters in focus area 2. In additional information, the first cluster (elements of the PHR) addressed data privacy issues such as the primary user being able to choose what diagnoses to share with their trusted adult, the ability to assign a trusted adult to view a part of the record, and sharing the severity of their own diagnoses (eg, bipolar diagnosis compared to strep throat). Cluster 2 (health education and information) included how to manage a healthy lifestyle and promote responsible mental health as well as basic health information and education. Cluster 3 (health planning resources) is closely related to cluster 2 including celebrating health successes, exercise, management plans for common diagnoses, and parenting resources for the youth themselves. Cluster 4 (everyday how-to) focuses on the life skills that are frequently taught at home including how to make a doctor’s appointment, how insurance works, and other independent living skills such as how to set up gas and electric. Last, cluster 5 (social and family information) focused on data from the county that the youth do not readily have access to including placement information, emancipation information, and siblings and where they are located.
DISCUSSION
PHRs currently exist in multiple forms, however, creating a PHR for youth in foster care presents a unique opportunity to provide not just basic medical information, but limited custody information as well as health education and coaching. Concept mapping is an important user-involved tool to employ across stakeholder groups. These concept maps will inform the future design and building of the PHR.
Common elements available in PHRs include demographics, allergies, medications, major diagnoses, and immunizations.41,42 All of these elements were listed by our participants to be included and additional elements included health planning resources (eg, what does a given diagnosis mean?), every day how-to (eg, how to make a doctor appointment), and the social information that can be provided by the county (eg, number of custody placements, birth certificate, social security number). Many of the attributes suggested for the ideal PHR were also identified by the participants, including being electronic, continuously updated, able to include paper documents (such as from outside providers), and private and controlled by the individual. While the participants did suggest common data elements, the vital elements to the adoption and use of the PHR will be in the additional information section (Table 3). The foster youth expressed an interest in having trusted sources to obtain medical information, encourage a healthy lifestyle, and have step-based walk-throughs of life tasks so they could be easily completed the first time.
The foster youth were interested in including their social and medical histories, their immunizations, life skills, and how to restrict access to their data to either a trusted adult or to themselves. A common theme was found that while the youth may have been given a diagnosis, it was not adequately explained or they did not believe it was accurate. The community stakeholders and healthcare professionals were more focused on including how to promote healthy lifestyles, how to encourage exercise, and teach health and behavior to a receptive audience. The foster youth are more focused on the privacy of their medical data than anticipated. The youth in custody may have experienced a lot of perceived invasion of privacy due to the many nonfamilial adults in their lives with legal rights to their personal data, such as caseworkers, guardians ad litem, court-appointed special advocates, etc. The community stakeholders were more focused on anticipatory guidance (eg, how to promote a healthy lifestyle) than originally thought. This may be because they see more of a need of including related to efforts to improve overall health status and know that this education is lacking in these adolescents. These 2 themes highlight the importance of including all stakeholders in the design of a new system. All the initial responses generated were from all stakeholders but then the sorters were foster youth only because we wanted them to drive the design of the EHR.
In our concept mapping, we included foster youth who were 18 years of age or older. In Hamilton county, youth can remain in protective custody until 21 years of age. Data privacy was not provided as a prompt; however, it was addressed in the usability of the PHR (Table 3), where it was requested for adolescents to be able to control which data elements they shared with a trusted adult and how they could provide or revoke that access. Privacy issues will need to be continually addressed while building and ultimately with dissemination of the PHR.43 There is an additional need to empirically evaluate this in future work, and as a start, this will be addressed with the end users in the design of the application.
For the sorting task, all concepts were combined and not separated based on who initiated it. Across the 2 focus areas, much of the information in the clusters overlapped. For example, medications appeared in personal medical history and diagnoses and personal health specifics. While these 2 concepts were named differently in sorting, fundamentally, they represented the same type of information to be provided in the PHR. All of the youth and community stakeholders wanted to be able to access the information electronically and have it be clear and easy to read, and printable so that the information could be easily shared when transitioning to a new care team.
Many of the novel topics in the additional information to be included in the PHR are skills that might have been taught in a more traditional family setup (eg, living with 1 or more parents). These topics included crisis and safety planning, how insurance works, what the diagnosis actually means, and even how to set up electric or gas in order to be independent. A consistent theme heard from the foster youth for including additional information was a need for accurate and timely contraception information that could be trusted. Along with this, foster youth frequently requested parenting resources for helping with their own children.
Concept map results will set the stage to ensure that key areas are considered for inclusion. Not all data elements requested will be able to be displayed or shared for the foster youth. For example, while it may be relatively easy to provide medication history or vital signs, a comprehensive guide to common diagnoses will be difficult and will need to link to an outside resource. The data merging and sharing for the application have already been performed with IDENTITY, but no outside resources have been identified.
There are existing hospital-based and vendor PHR systems.41,44–47 The hospital-based systems may not contain data outside their network and by having a modifiable PHR, we are allowing the users to update their record. And vendor systems may not be integrated with any hospital and therefore force the user to enter in all of their own data. Neither of these solutions is ideal for foster youth as they may be seen in different hospitals, but they also may not have any of their past history as a basis for a PHR.
As a PHR is created for foster youth, it is important to consider the multiple uses that the data may have for the emancipated youth. These uses may include transition to adult care and learning skills that would normally have been taught at home. Through the user-centric design, the PHR aims to help address 2 major issues, the first being the lack of access to available health and custody information and the second being the eventual transition to adult care. It is important that both of these roles are addressed as well as information necessary for the youth, their caseworkers, and their providers.
Youth-driven development is key to having a successful PHR application, but is also vital to having a sustainable and engaged population. Youths are frequently not involved in the development and analysis of research involving themselves48 and using concept mapping allows us to ensure they are active participants in the research. Foster youth must frequently learn to live independently without external adult assistance.49 They often must learn everyday life skills as well as how to take care of their own health. By directly involving youth in the design of the PHR, we are able to ensure we included the necessary health and links to trusted educational elements that they requested and currently lack. This is a difficult to study population as, when emancipated, they can be difficult to track down or unwilling to work within the system. It is of vital importance to keep them involved in the design and ultimate implementation of the PHR so that a truly useful and user-friendly system results from the collaboration.
Our concept mapping did have limitations. The foster youth are more transient population than other adolescents and may not be as willing to be involved in research. We approached as many adolescents as possible and sought volunteers at existing foster youth meetings. We found a core group of about 5 youth that attended the majority of monthly FYC meetings but many others only participated sporadically as work schedules and transportation permitted. Previous work in concept mapping has shown that there is minimal variation in the final maps after approximately 20 sorts26; we used a purposeful sample of foster youth that were available to participate in the sorting activity and recruited from several venues to ensure a more diverse sample. The stakeholders and healthcare providers represented a convenience sample of those who attended community meetings, were available during the study period, and had an interest in helping the foster youth population. The youth who participated in our study may also present a bias. The ones who participated are likely more engaged and higher functioning than others are. Those facing more challenges were less likely to participate and may have reported different needs from a PHR.
With the number of children and adolescents in foster care throughout the United States, we foresee difficulties for most youth emancipating from care with identification and coordination of their own data. These youth are frequently seen in many different settings and may not know all of their past medical history. A PHR created for this population could help to serve the foster youth but also eventually may help foster care providers have a record of the child’s care to better understand their history. This coordination of knowledge sharing could help foster parents, caseworkers, and even future providers allowing the PHR to benefit more than just 1 population.
In the next steps of building the user interface for the PHR, we will continue to evaluate whether the information requested from the youth can be extracted and displayed from the existing databases. We will also work with 3-4 foster youth, community stakeholders, and the LiveWell Collaborative to design a user interface that is intuitive and clear. The foster youth must be involved in the design steps to ensure their voice continues to be heard, included, and evaluated in the design and ultimate implementation of the PHR.
CONCLUSION
Concept mapping allowed us to take disparate thoughts and have a motivated team of individuals help to identify important elements to be included in a PHR for foster youth. A PHR for foster youth is an appropriate combination of information and education for a vulnerable population. While the youth lack access to some of their basic health and custody information, this also provided an opportunity to give them information to explain common diagnoses, medications, and family health history risks. At the same time, these youth may be lacking in “home-taught” skills, from contraception to how to set up a gas and electric line for independent living. By providing this information, we will ensure that the youth receive the information they want in a format that is user-friendly and helps them to feel comfortable trusting and learning all of the information.
FUNDING
This work was supported by internal grant funding from Cincinnati Children’s Hospital Medical Center, National Institutes of Health grant number R01LM012816-01, and National Institute on Drug Abuse grant number 1K01DA041620-01A1.
AUTHOR CONTRIBUTORS
All authors contributed materially to the production of this manuscript. JWD conducted and coordinated the study, conceptualized the work, and wrote the manuscript. MVG participated in the conception of the project, drafting of the manuscript, and critical revisions. SJB participated in the conception of the project, drafting of the manuscript, and critical revisions. DJ participated in acquisition of data, manuscript review, design, and revisions. AK participated in acquisition of data, manuscript review, design, and revisions. LMV designed and organized the concept mapping, analyzed the results, and created the tables and figures.
ACKNOWLEDGMENTS
The authors would like to thank Kristine Flinchum at Hamilton County Jobs and Family Services.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. AFCARS Report. Preliminary FY 2015 estimates as of June 2016. Washington, DC. https://www.acf.hhs.gov/sites/default/files/cb/afcarsreport23.pdf. Accessed March 23, 2017.
- 2. Gardner D. Youth Aging Out of Foster Care: Identifying Strategies and Best Practices, 2007-08 Presidential Initiative. Washington, DC: National Associate of Counties (NACo; ); 2008. http://www.naco.org/sites/default/files/documents/Youth%20Aging%20Out%20of%20Foster%20Care.pdf. Accessed 2019. [Google Scholar]
- 3. Halfon N, Mendonca A, Berkowitz G.. Health status of children in foster care. The experience of the Center for the Vulnerable Child. Arch Pediatr Adolesc Med 1995; 149 (4): 386–92. [DOI] [PubMed] [Google Scholar]
- 4. Melbye ML, Chi DL, Milgrom P, et al. Washington state foster care: dental utilization and expenditures. J Public Health Dent 2014; 74 (2): 93–101. [DOI] [PubMed] [Google Scholar]
- 5. Ringeisen H, Casanueva C, Urato M, et al. Special health care needs among children in the child welfare system. Pediatrics 2008; 122 (1): e232–41. [DOI] [PubMed] [Google Scholar]
- 6. Simms MD, Dubowitz H, Szilagyi MA.. Health care needs of children in the foster care system. Pediatrics 2000; 106 (Suppl 4): 909–18. [PubMed] [Google Scholar]
- 7. Turney K, Wildeman C.. Mental and physical health of children in foster care. Pediatrics 2016; 138 (5): e20161118. [DOI] [PubMed] [Google Scholar]
- 8. Chernoff R, Combs-Orme T, Risley-Curtiss C, et al. Assessing the health status of children entering foster care. Pediatrics 1994; 93 (4): 594–601. [PubMed] [Google Scholar]
- 9. Sullivan DJ, van Zyl MA.. The well-being of children in foster care: exploring physical and mental health needs. Child Youth Serv Rev 2008; 30 (7): 774–86. [Google Scholar]
- 10. Greiner MV, Ross J, Brown CM, et al. Foster caregivers’ perspectives on the medical challenges of children placed in their care: Implications for pediatricians caring for children in foster care. Clin Pediatr (Phila) 2015; 54 (9): 853–61. [DOI] [PubMed] [Google Scholar]
- 11. Cincinnati Children's Hospital Medical Center. 2016 Research Annual Report. Internal Funding: Academic and Research Committee (ARC) Awards. 2016. https://www.cincinnatichildrens.org/research/cincinnati/annual-report/2016/by-the-numbers/internal#1. Accessed 26 May 2019.
- 12. Dexheimer JW, Beal SJ, Hall ES, et al. Automated patient matching for electronic health record and child welfare databases [abstract]. Pediatrics 2018; 142 (1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kushel MB, Yen IH, Gee L, et al. Homelessness and health care access after emancipation: Results from the midwest evaluation of adult functioning of former foster youth. Arch Pediatr Adolesc Med 2007; 161 (10): 986–93. [DOI] [PubMed] [Google Scholar]
- 14. Risley-Curtiss C, Kronenfeld JJ.. Health care policies for children in out-of-home care. Child Welfare 2001; 80 (3): 325–50. [PubMed] [Google Scholar]
- 15. Courtney ME, Dworsky AL, Brown A, et al. Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 26. Chicago, IL: Chapin Hall at the University of Chicago; 2011. [Google Scholar]
- 16. Christian CW, Schwarz DF.. Child maltreatment and the transition to adult-based medical and mental health care. Pediatrics 2011; 127 (1): 139–45. [DOI] [PubMed] [Google Scholar]
- 17. Ahrens KR, Dubois DL, Garrison M, et al. Qualitative exporation of relationships with important non-parental adults in the lives of youth in foster care. Child Youth Serv Rev 2011; 33 (6): 1012–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Lopez P, Allen PJ.. Addressing the health needs of adolescents transitioning out of foster care. Pediatr Nurs 2007; 33 (4): 345–55. [PubMed] [Google Scholar]
- 19. Ahrens KR, Richardson LP, Courtney ME, et al. Laboratory-diagnosed sexually transmitted infections in former foster youth compared with peers. Pediatrics 2010; 126 (1): e97–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dworsky A, Courtney ME, Ruth G, et al. Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 19. Chicago, IL: Chapin Hall at the University of Chicago; 2005. [Google Scholar]
- 21. Courtney ME, Dworsky A, Ruth G, et al. Midwest Evaluation of the Adult Functioning of Former Foster Youth: Outcomes at Age 21. Chicago, IL: Chapin Hall at the University of Chicago; 2007. [Google Scholar]
- 22. White PH, Cooley WC.. Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics 2018; 142 (5) [DOI] [PubMed] [Google Scholar]
- 23. Gray SH, Pasternak RH, Gooding HC, et al. Recommendations for electronic health record use for delivery of adolescent health care. J Adolesc Health 2014; 54 (4): 487–90. [DOI] [PubMed] [Google Scholar]
- 24. Ford C, English A, Sigman G.. Confidential health care for adolescents: position paper for the society for adolescent medicine. J Adolesc Health 2004; 35 (2): 160–7. [PubMed] [Google Scholar]
- 25. Vaughn LM, Jacquez F, McLinden D.. The use of concept mapping to identify community-driven intervention strategies for physical and mental health. Health Promot Pract 2013; 14 (5): 675–85. [DOI] [PubMed] [Google Scholar]
- 26. Trochim W, Kane M.. Concept mapping: an introduction to structured conceptualization in health care. Int J Qual Health Care 2005; 17 (3): 187–91. [DOI] [PubMed] [Google Scholar]
- 27. Kane M, Trochim WMK.. Concept Mapping for Planning and Evaluation. Thousand Oaks, CA: Sage; 2007. [Google Scholar]
- 28. Behar LB, Hydaker WM.. Defining community readiness for the implementation of a system of care. Adm Policy Ment Health 2009; 36 (6): 381–92. [DOI] [PubMed] [Google Scholar]
- 29. Shorkey C, Windsor LC, Spence R.. Assessing culturally competent chemical dependence treatment services for Mexican Americans. J Behav Health Serv Res 2009; 36 (1): 61–74. [DOI] [PubMed] [Google Scholar]
- 30. Risisky D, Hogan VK, Kane M, et al. Concept mapping as a tool to engage a community in health disparity identification. Ethn Dis 2008; 18 (1): 77–83. [PubMed] [Google Scholar]
- 31. Davis JE. Construct validity in measurement. Eval Program Plann 1989; 12 (1): 31–6. [Google Scholar]
- 32. Jackson KM, Trochim W.. Concept mapping as an alternative approach for the analysis of open-ended survey responses. Organ Res Methods 2002; 5 (4): 307–36. [Google Scholar]
- 33. Goodman LA. Snowball sampling. Ann Math Stat 1961; 32 (1): 148–70. [Google Scholar]
- 34. Seale C. Qualitative Research Practice. Thousand Oaks, CA: Sage; 2004. [Google Scholar]
- 35. Rosenberg S, Park Kim M.. The method of sorting as a data-gathering procedure in multivariate research. Multivariate Behav Res 1975; 10 (4): 489–502. [DOI] [PubMed] [Google Scholar]
- 36. Weller SC, Romney AK.. Systematic Data Collection. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 37.McLinden D. Concept maps as network data: analysis of a concept map using the methods of social network analysis. Eval Program Plann. 2013; 36(1): 40–8. [DOI] [PubMed]
- 38. de Leeuw J, Mair P.. Multidimensional scaling using majorization: SMACOF in R. J Stat Softw 2009; 31 (3): 1–30. [Google Scholar]
- 39. Sturrock K, Rocha J.. A multidimensional scaling stress evaluation table. Field Methods 2000; 12 (1): 49–60. [Google Scholar]
- 40. Vaughn L., McLinden D. Concept mapping In: Leonard J, Glenwick D, eds. Handbook of Methodological Approaches to Community-Based Research: Qualitative, Quantitative, and Mixed Methods. New York, NY: Oxford University Press; 2016: 305–14. [Google Scholar]
- 41. Tang PC, Ash JS, Bates DW, et al. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption. J Am Med Inform Assoc 2006; 13 (2): 121–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. American Health Information Management Association (AHIMA). How to create a personal health record. http://www.myphr.com/StartaPHR/Create_a_PHR.aspx. Accessed April 19, 2017.
- 43. Blythe MJ, Del Beccaro MA.. Standards for health information technology to ensure adolescent privacy. Pediatrics 2012; 130 (5): 987–90. [DOI] [PubMed] [Google Scholar]
- 44. Bourgeois FC, Nigrin DJ, Harper MB.. Preserving patient privacy and confidentiality in the era of personal health records. Pediatrics 2015; 135 (5): e1125–7. [DOI] [PubMed] [Google Scholar]
- 45. Woollen J, Prey J, Wilcox L, et al. Patient experiences using an inpatient personal health record. Appl Clin Inform 2016; 7 (2): 446–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Halamka JD, Mandl KD, Tang PC.. Early experiences with personal health records. J Am Med Inform Assoc 2008; 15 (1): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Microsoft HealthVault. HealthVault. US 2019. https://international.healthvault.com/us/en. Accessed March 7, 2019.
- 48. Arunkumar K, Bowman DD, Coen SE, et al. Conceptualizing youth participation in children's health research: insights from a youth-driven process for developing a youth advisory council. Children (Basel )2018; 6 (1): E3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Allen M, Nixon R.. Gautreaux and Chicago's public housing crisis. J Poverty Law Policy 2000; 34 (3–4). [Google Scholar]