Abstract
Background
More than 100 studies document disparities in patient portal use among vulnerable populations. Developing and testing strategies to reduce disparities in use is essential to ensure portals benefit all populations.
Objective
To systematically review the impact of interventions designed to: (1) increase portal use or predictors of use in vulnerable patient populations, or (2) reduce disparities in use.
Materials and Methods
A librarian searched Ovid MEDLINE, EMBASE, CINAHL, and Cochrane Reviews for studies published before September 1, 2018. Two reviewers independently selected English-language research articles that evaluated any interventions designed to impact an eligible outcome. One reviewer extracted data and categorized interventions, then another assessed accuracy. Two reviewers independently assessed risk of bias.
Results
Out of 18 included studies, 15 (83%) assessed an intervention's impact on portal use, 7 (39%) on predictors of use, and 1 (6%) on disparities in use. Most interventions studied focused on the individual (13 out of 26, 50%), as opposed to facilitating conditions, such as the tool, task, environment, or organization (SEIPS model). Twelve studies (67%) reported a statistically significant increase in portal use or predictors of use, or reduced disparities. Five studies (28%) had high or unclear risk of bias.
Conclusion
Individually focused interventions have the most evidence for increasing portal use in vulnerable populations. Interventions affecting other system elements (tool, task, environment, organization) have not been sufficiently studied to draw conclusions. Given the well-established evidence for disparities in use and the limited research on effective interventions, research should move beyond identifying disparities to systematically addressing them at multiple levels.
Keywords: personal health records, patient portals, patient access to records, consumer health information, healthcare disparities, vulnerable populations
INTRODUCTION
Last year, millions of Americans accessed their own health records online, more than ever before.1–4 Secure websites called patient portals offer convenient, 24-hour access to records, as well as appointment scheduling, medication monitoring, and other health management features.5 Portals provide patients with unprecedented transparency into health information, which evidence suggests can prevent medical errors,6–11 increase shared decision-making,12–17 and improve health outcomes.18,19 As such, transparency has been hailed as the next “blockbuster drug” and “healthcare revolution” by prominent media outlets.20–22
Patient portals have only recently gained popularity. The percentage of healthcare organizations offering portals rose from 43% in 2013 to 92% in 2015.4,23,24 As availability has increased, more patients have used portals.25–28 In the United States (US), self-reported use rose from 17% in 2014 to 28% in 2017.29,30 Multiple factors have contributed to the increase in portal availability, including the perceived impact on outcomes,31 consumers' desire for transparency,32 and the federal Meaningful Use program, which requires that organizations allow patients to view, download, and transmit their health records.33,34
Some researchers initially hoped that portals could reduce health inequities,35,36 a highly significant and refractory problem in the US.37 Health inequities lead to poor health management and outcomes, which contribute to rising healthcare costs.38 Vulnerable populations often demonstrate lower health literacy and experience significant barriers to care, such as inflexible job hours, cost, and insurance status.39 Portal features such as messaging, online education, and automatic medication refills might increase convenience, improve health literacy, and overcome at least some barriers to care, thereby reducing health inequities.
Unfortunately, more than 100 studies now show substantial health-equity–relevant disparities in portal use (additional citations available upon request).28,40–56 Vulnerable populations use portals less often, including elderly persons,44,46–48,56 racial minorities,43,46–50 as well as persons with low socioeconomic status,28,43,54 low health literacy,44,49,51–53 chronic illness,41,46,50,56 or disabilities.44,49,55 Relatively low portal use in vulnerable populations may lead to intervention-generated inequity, a phenomena where well-intentioned solutions worsen existing health inequities rather than reduce them.57–59 Developing, implementing, and evaluating strategies to reduce disparities in portal use is critical to ensure portals benefit all populations as originally intended.
In this systematic review, we explore how researchers have confronted differential use of patient portals. Our review focuses on two critical questions: (1) what interventions impact portal use or predictors of portal use in vulnerable populations? (2) what interventions impact disparities in portal use?
MATERIALS AND METHODS
We conducted and reported this systematic review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).60 A technical protocol that details our eligibility criteria, includes the complete search strategies, and contains additional results tables is available as Supplementary Material.
Eligibility criteria
We developed eligibility criteria with respect to publication characteristics (type, language, year, and status) and study characteristics (participants, interventions, comparisons, outcomes, study design [PICOS], and technology), as described in Supplementary Table 1. Publication Characteristics: We included English-language research articles published or in press. Participants: We required that the interventions occur in 1 or more vulnerable populations. To define vulnerable populations, we used the PROGRESS-Plus framework developed by Campbell and Cochrane Equity Methods Group.61–63 The PROGRESS-Plus framework identifies characteristics that stratify health opportunities and outcomes, including Place of residence, Race/ethnicity/culture/language, Occupation, Gender/sex, Religion, Education, Socioeconomic status, and Social capital. “Plus” considers additional characteristics associated with social disadvantage, including age, disability, and illness status. Additionally, we included characteristics known to disadvantage portal users: (1) chronic, critical, or psychiatric illness;40,64–66 (2) low functional, health, or technology literacy;40,66,67 (3) low numeracy or graph literacy;40,68,69 (4) low patient engagement, activation, or participation.40,66Interventions: We included any intervention designed to impact an eligible outcome. Comparisons: Studies had to include a comparison to evaluate the effect of the intervention. Comparisons could involve measurements before and after implementation, or the intervention could be compared with some concurrent control condition or group. Outcomes: Studies had to include at least 1 outcome measure that captured portal use (such as rate of portal registration or number of logins), a predictor of portal use (such as usability or intended use), or a health-equity–relevant disparity in portal use (such as the difference between enrollment rates among white and non-white patients). We included studies regardless of whether this outcome measure was the primary outcome or a secondary outcome. Study Design: We included any study design as long as an eligible comparison occurred. Technology: We excluded consumer health technologies other than patient portals, such as telehealth, mobile health (mHealth), or electronic visit (eVisit) platforms.
Data sources and searches
We searched Ovid MEDLINE, EMBASE, CINAHL, and Cochrane Reviews for English-language studies published before September 1, 2018. The Supplementary Materials include the full electronic database names, search dates, and search strategies. First, 3 authors (LVG, RMC, JSA) identified relevant Medical Subject Headings (MeSH) and free-text search terms based on the eligibility criteria, potentially relevant studies, and personal expertise. Then, an experienced librarian (DW) developed and conducted all searches. A second librarian reviewed the searches for completeness and accuracy. Additionally, we manually searched our personal reference libraries, reference lists of included studies, and pertinent reviews to identify potentially relevant citations our search might have missed. Finally, we searched tables of contents of pertinent scientific journals between May 1, 2018 and December 1, 2018 to identify recently published citations. When necessary, we directly communicated with study authors to ensure we had included all relevant citations and to obtain any manuscripts in press.
Study selection
We used Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia; available at www.covidence.org) for citation screening, as recommended by Cochrane.70 Initially, 2 researchers independently evaluated each citation for eligibility based on the title and abstract. For all potentially eligible studies identified in the initial screening, at least 2 researchers reviewed the full text to determine final eligibility. Conflicts were resolved by discussion with the study team.
Data extraction
The study team developed the data extraction form based on an initial review of included studies. Information extracted included the study objective, setting, population, design, eligibility criteria, intervention category, and findings. One team member extracted relevant data from each article, and a second team member reviewed all data extractions for completeness and accuracy.
Risk of bias assessment
To assess risk of bias (internal validity), we used predefined criteria from the AHRQ Methods Guide for Effectiveness and Comparative Effectiveness Reviews to rate studies as low, medium, high, or unclear risk of bias.71 The criteria evaluate common sources of selection, performance, attrition, detection, and reporting bias. The guide specifies which criteria apply to different study designs, which was important because we included multiple study designs in this review. Two reviewers independently assessed risk of bias for each study, and differences were resolved by discussion with the study team.
Data analysis and synthesis
Descriptive analysis of study characteristics was conducted in Microsoft Excel. When relevant estimates could not be extracted directly from the article, we computed or estimated them based on published data (see footnotes to Tables 1, 2, and 4 for details). We assessed intensity of intervention as per the Cochrane Handbook for Systematic Reviews of Interventions.72 Given the heterogeneity of included interventions, we could not apply 1 single measure of intensity to all interventions. In general, we defined low intensity as 1 mode of delivery or episode of patient contact, medium as 2 or 3, and high as more than 3.
Table 1.
Studies included in the systematic review
| Study | Portal-Relevant Objective | Study Design | Intervention (Category)a | Main Finding(s) |
|---|---|---|---|---|
| Ali et al. 201877 | Identify usability challenges in a portal, and evaluate whether recommended solutions improved its usability |
|
Improve usability (B7) | System usability score (81.9 after vs 69.2 before, p=.049) and task completion (87% after vs 55% before) improved after recommended solutions were appliedb |
| Ancker et al. 201778 | Estimate the effect of a universal access policy on socioeconomic disparities in use of the portal |
|
|
Significant disparities in portal use by age, race, and ethnicity vanished after replacing an opt-in policy with a universal access policy (among other interventions), but disparities on the basis of income did not disappear |
| Casey 201679 | Evaluate the effectiveness of a hands-on technology education intervention in improving portal use |
|
Technology education (A1) | The intervention group sent significantly more messages (54 vs 12 control, p<.001) than the matched control group in the month post-intervention |
| Graetz et al. 201880 | Assess if mobile access increases the frequency and timeliness of portal use by diabetes patients |
|
Mobile access (B8) | Mobile access increases frequency in all patients (0.78 days more per month [0.74-0.83]) and timeliness in non-White patients (64% after vs 59% before, p<.001) |
| Greysen et al. 201881 | Evaluate the efficacy of a bedside education intervention to increase portal use by inpatients |
|
|
The intervention was feasible, however, a significant increase in mean number of logins (3.48 vs 2.94 control, p=.60) and use of key portal functions was not observed |
| Kim et al. 200582 | Determine the impact of technical help from nurses on portal information updates by patients |
|
|
Information update events occurred primarily on days when technical help was available (58%) or the day afterward (23%)b |
| Leisy et al. 201783 | Assess the effect of an iBooks-based tutorial on comfort with portal features |
|
iBooks-based tutorial (A1) | The tutorial increased comfort levels with portal features by 20%-80%, and most patients (86%) agreed the tutorial would increase their future portal use |
| Leveille et al. 201684 | Investigate the impact of OpenNotes on use of the portal and its functions* |
|
OpenNotes (B5) | Overall frequency of portal use did not change, but the proportion of login days dedicated to record viewing increased from 24% to 35%b |
| Lyles et al. 201885 | Evaluate an in-person vs online self-paced training program on portal use |
|
Portal training (A1) | Training of either type increased portal use compared to usual care (21% vs 9% logins, p<.001), but no differences existed between in-person and online training |
| Mafi et al. 201686 | Assess the impact of email alerts on whether patients viewed their doctor's notes through portals |
|
Email alerts (E12) | Note viewing declined substantially and immediately beginning when email alerts ceased (RR 0.29 [0.26-0.32]) and persisting until the study's end (RR 0.20 [0.17-0.23]) |
| McInnes et al. 201387 | Evaluate group training to increase portal skills in vulnerable populations with limited computer experience |
|
Group training (A1) | Portal use increased directly after training (use score of 2.00 vs 0.36 baseline, p<.001), and remained elevated 3 months later (1.36 vs 0.36 baseline, p=.01) |
| Navaneethan et al. 201788 | Assess the effect of an enhanced portal and navigator program on portal use in CKD patients* |
|
|
The patient navigator group reported more logins than other groups (estimated median 49 vs 37 usual care, 36 portal only, 41 navigator and portal, p=.04)b |
| Phelps et al. 201489 | Investigate characteristics that impact persistence of portal use over time |
|
Assistance with first login (A1) | Provision of assistance with first login is associated with higher odds of completing the initial login (OR 3.22[2.17-4.76])b |
| Ramsey et al. 201790 | Determine effectiveness of dedicating staff (MyChart Geniuses) to assist adolescents with portal sign-up |
|
MyChart Geniuses (A1) | MyChart Geniuses sign up more patients (86% vs 59% general population, p<.001), but those patients were less likely to activate their accounts (20% vs 77%, p<.001)b,c |
| Shaw et al. 201791 | Increase portal utilization through nurse navigators and assignment of health education videos to patients |
|
|
2 of 19 participants reported portal use in the 6 months prior to intervention, whereas 4 of 19 participants reported portal use within 30 days post-intervention |
| Stein et al. 201892 | Assess an intervention to teach vulnerable inpatients to access their discharge summaries using a portal |
|
|
Hospitalized patients who received training and email reminders were more likely to register for the portal (48% vs 11% control, p<.01) |
| Turvey et al. 201693 | Investigate the impact of training veterans to use the Blue Button feature in the VA portal |
|
|
Training increased health record sharing with outside providers (90% vs 17% control, p<.001) |
| Weisner et al. 201694 | Assess effect of a patient engagement intervention (LINKAGE) on portal use* |
|
Portal training (A1) | LINKAGE significantly increased mean number of portal login-days (IRR 1.53, p=.001) and mean number of messages sent by a provider (IRR 1.45, p=.02) |
Abbreviations: RCT, randomized controlled trial; CT, clinical trial; CKD, chronic kidney disease; VA, veterans affairs; RR, relative risk; OR, odds ratio; IRR, incidence rate ratio.
Denotes an objective that is secondary to the study's primary objective.
See Table 3 for descriptions of intervention categories.
Estimates calculated from published data by systematic review authors.
Chi-squared test performed by systematic review authors.
We categorized interventions according to the components described in the System Engineering Initiative for Patient Safety (SEIPS) model.73–75 The SEIPS model segments work systems into 5 tightly coupled components. Per the model, a person (component 1) performs a range of tasks (component 2) using various tools and technologies (component 3). Performance of tasks occurs within a physical environment (component 4) under specific organization conditions (component 5). Interventions may be made on work system processes to impact outcomes, which may target 1 or more of the 5 components. We categorized interventions based on which component(s) were addressed. One team member categorized the interventions, and a second team member with experience applying the SEIPS model (NCB) reviewed the categorizations. Using the SEIPS model allowed us to determine gaps in the targets of current interventions and shortcomings related to considering the interaction among components of the work system.
In our protocol, we initially planned to conduct a meta-analysis and grade strength of evidence as per the Evidence-Based Practice Center program guidelines.76 Unfortunately, the paucity of literature and lack of directly comparable outcomes limited us to the systematic review component only.
RESULTS
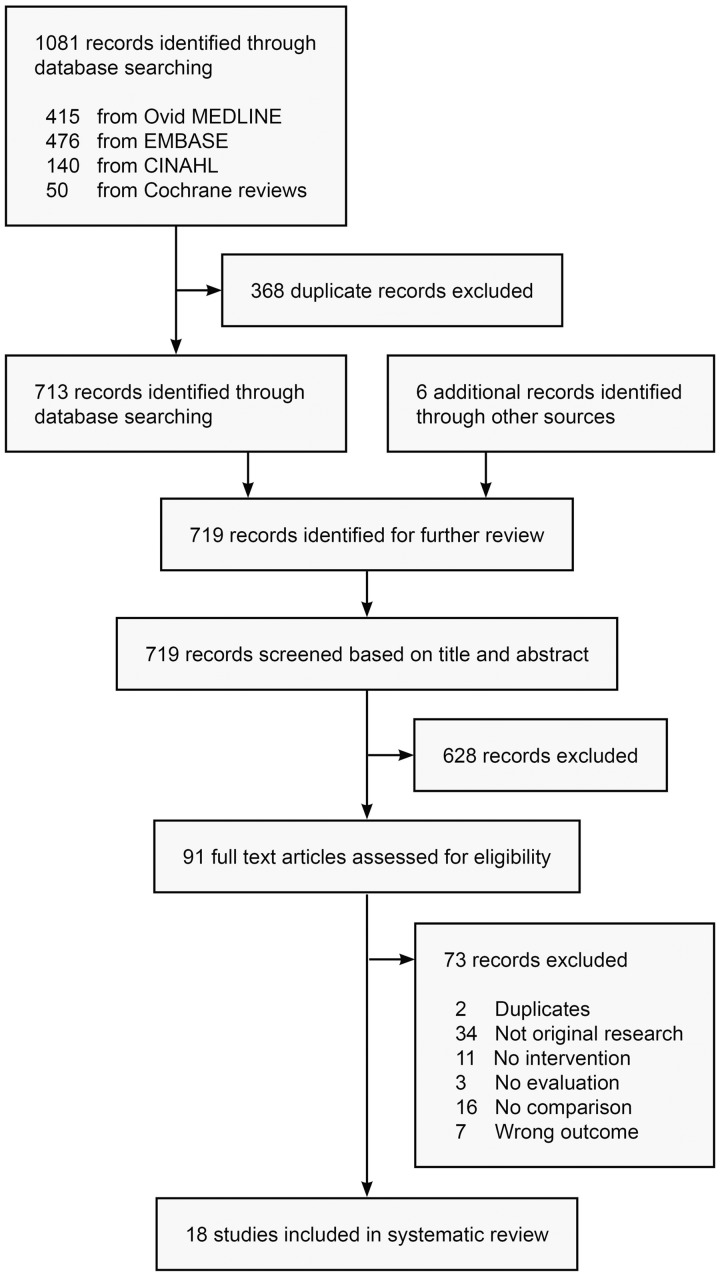
Literature searches identified 719 potentially relevant citations. Of those, 91 studies were deemed eligible for full text review, and 18 studies fulfilled the inclusion criteria for this systematic review (Figure 1).77–94
Figure 1.
Flow diagram for study selection
Study characteristics
Table 1 summarizes the objective, design, intervention, and main finding(s) of included studies. Most included studies were published between 2016 and 2018, with 1 study published in 2014, 1 in 2013, and 1 in 2005. Designs included 5 randomized controlled trials (28%), 1 non-randomized clinical trial (6%), 5 time series (28%), 1 pre-test post-test with concurrent controls (6%), 4 pre-test post-test without concurrent controls (22%), and 2 post-test only (11%). Studies employed a broad variety of outcome measures (Supplementary Table 2) over varied time periods, limiting their comparability. For example, when reporting portal use, studies variably reported login-days, total logins, activation, or another measure, and time periods varied from “per month” to “per 2 years.”
Table 2 reports the study demographics, eligibility criteria, setting, risk of bias, and intensity of intervention. Sample sizes of prospective studies ranged from 14 to 503 participants. Because retrospective studies often relied on portal system use data, their sample sizes included more than 10 000 or even 100 000 participants. Four out of 18 studies (22%) did not report on participants' race, and 8 (44%) did not report on ethnicity. One study (6%) included English- and Spanish-speakers, 8 (44%) included only English-speakers, and 9 (50%) did not report on language. All studies excluded pediatric populations except 1 study of adolescents. All interventions were limited to the outpatient setting except 3 that included inpatients. Intensity of intervention varied widely across studies. An example of a low-intensity intervention was one-time assistance with credentialing,89 whereas an example of a high-intensity intervention was training participants across 4 weekly 2-hour sessions.87
Table 2.
Characteristics of included studies
| Variable | Ali et al. 201877 | Ancker et al. 201778 | Casey 201679 | Graetz et al. 201880 | Greysen et al. 201881 | Kim et al. 200582 | Leisy et al. 201783 | Leveille et al. 201684 | Lyles et al. 201885 |
|---|---|---|---|---|---|---|---|---|---|
| Study Population | |||||||||
| Total sample size | 23 | 129 738 | 100 | 135 153 | 97 | 24 | 70 | 44 951 | 93 |
| Age (mean) | 41a | 42a | 65 | 61a | 46a | 65 | 61a | 51 | 54 |
| Female (%) | 83 | 62 | 66 | 47 | 55 | − | 56 | 62 | 52 |
| Race (%) | |||||||||
| White | 60 | 38 | 92 | 52 | 55 | − | − | − | 39 |
| Black | 5 | 23 | 2 | 8 | 20 | − | − | − | 29 |
| Other | 35 | 38 | 6 | 40 | 25 | − | − | − | 32 |
| Latino ethnicity (%) | 25 | 27 | 4 | 16 | 9 | − | − | − | 12 |
| Eligibility Criteria | |||||||||
| Illness status | ≥ 1 chronic condition | Any | ≥ 1 chronic condition | Diabetes | Hospitalized | Any | Ophthalmic | Any | ≥ 1 chronic condition |
| Age range | 18-95 | >18 | 40-85 | >18 | >18 | Adult | Adult | >18 | >18 |
| Primary language | English only | English or Spanish | English only | − | English only | − | English only | − | English only |
| Study Setting | |||||||||
| Level of care | Primary or specialist | Primary | Primary | Primary or specialist | Tertiary | Primary or specialist | Specialist | Primary | Primary |
| Clinical setting | Outpatient | Outpatient | Outpatient | Outpatient | Inpatient | Outpatient | Outpatient | Outpatient | Outpatient |
| Other details | Academic | Safety net | − | − | Academic | Residential | Academic | Two sites | Safety net |
| Quality Assessment | |||||||||
| Risk of bias | Medium | Low | Unclear | Low | Medium | High | Medium | Medium | Medium |
| Intensity of intervention | Medium | High | Unclear | Low | Medium | High | Medium | Low | Medium |
| Variable |
Mafi et al. 201686 | McInnes et al. 201387 | Navaneethan et al. 201788 | Phelps et al. 201489 | Ramsey et al. 201790 | Shaw et al. 201791 | Stein et al. 201892 | Turvey et al. 201693 | Weisner et al. 201694 |
|---|---|---|---|---|---|---|---|---|---|
| Study Population | |||||||||
| Total sample size | 14 360 | 14 | 209 | 11 352 | 96 | 19 | 70 | 52 | 503 |
| Age (mean) | 52 | 57 | 68 | 53a | 19 | 60 | 56 | 68 | 42 |
| Female (%) | 58 | 7 | 56 | 40 | 59 | 63 | 36 | 12 | 31 |
| Race (%) | |||||||||
| White | 75b | 57 | 75 | − | 0 | 73 | 76 | 92 | 61 |
| Black | 5 | 21 | 22 | − | 87 | 16 | 10 | − | 7 |
| Other | 20 | 21 | 3 | − | 13 | 11 | 14 | − | 32 |
| Latino ethnicity (%) | − | 14 | − | − | 5 | − | 11 | − | 20 |
| Eligibility Criteria | |||||||||
| Illness status | Any | HIV or HCV | CKD | CKD | Any | Cardiac | Any | ≥ 1 chronic condition | Addiction |
| Age range | Adult | Adult | 18-80 | Any | 13-25 | 18-75 | >18 | Adult | >18 |
| Primary language | − | − | English only | − | − | English only | English only | − | − |
| Study Setting | |||||||||
| Level of care | Primary | Primary | Primary or specialist | Specialist | Primary | Specialist | Tertiary | Primary or specialist | Specialist |
| Clinical setting | Outpatient | Outpatient | Outpatient | Outpatient or inpatient | Outpatient | Outpatient | Inpatient | Outpatient | Outpatient |
| Other details | Academic | Veterans | Academic | − | Academic | − | Safety net | Veterans | − |
| Quality Assessment | |||||||||
| Risk of bias | Medium | Medium | Low | High | Medium | High | Medium | Unclear | Low |
| Intensity of intervention | Medium | High | High | Low | Low | Medium | Medium | Low | High |
|
| |||||||||
Abbreviations: HIV, human immunodeficiency virus; HCV, hepatitis C virus; CKD, chronic kidney disease.
Mean age estimated from categorical data.
Race reported for only 1 of 2 study sites; the second unreported study site is described as “predominantly white.”
–Not reported or not applicable.
Risk of bias assessment
Four out of 18 studies (22%) had low risk of bias, 9 studies (50%) had medium, 3 studies (17%) had high, and 2 studies (11%) were unclear (Table 2). The most common sources of bias included: (1) failure in design or analysis to account for important confounding and modifying variables through matching, stratification, multivariable analysis, or other approaches [10 studies, 56%]; (2) differential length of follow-up between comparison groups [5 studies, 28%]; (3) if attrition was a concern, failure to handle missing data appropriately through intention-to-treat analysis, imputation, or other approaches [4 studies, 22%]; (4) failure to rule out impact from a concurrent intervention or an unintended exposure that might bias results [3 studies, 17%]; (5) failure to blind outcome assessors to the intervention or exposure status of participants [3 studies, 17%].
Intervention categorization using the SEIPS model
Figure 2 presents the SEIPS system components intervened on in each study. Out of 18 studies, 13 (72%) intervened on the individual (person) component, 5 (28%) on the tool component (ie, patient portal), 1 (6%) on the task component (eg, prescribing portal content), 2 (11%) on the environment component, and 4 (22%) on the organization component. Seven studies (39%) intervened on 2 components, but no study intervened on more than 2. Table 3 more deeply explores the different interventions and their relationships with the SEIPS system components. In the included studies, 13 out of 26 interventions (50%) involved training or assisting patients with portal use (person component).79,81–83,85,87–94 Out of 26 interventions 6 (23%) involved enhancing portal content,84,88 providing mobile access,78,80 Spanish translation,78 or improving usability (tool component).77 The remaining interventions involved prescribing portal use (task component),91 offering devices or internet connectivity (environment component),81,82 increasing portal reminders (organization component),86,92,93 or modifying organizational policy (organization component).78
Figure 2.
SEIPS system components intervened on in included studies
Table 3.
Categories of interventions to increase patient portal use
| No. | Intervention | Description | Included Studies | Additional Examples from the Literaturea |
|---|---|---|---|---|
| Category A. Person-based Interventions | ||||
| A1 | Assist patients | Training, technical assistance, or motivation for patients, from a physician, nurse, educator, or other professional | Casey79Greysen et al.8111 more82,83,85,87–94 | |
| A2 | Engage informal care providers | Portal co-access or assistance from an informal care provider, like healthcare proxies, family members, or peers | No studies | |
| A3 | Engage formal care providers | Training, assistance, or motivation for providers, to encourage them to engage their patients in portals | No studies | |
| Category B. Tool-based Interventions | ||||
| B4 | Simplify content | Define complex terms, simplify readability of medical text, or offer education around clinical content | No studies | |
| B5 | Enhance content | Include novel content, improve utility of existing content, or more transparency of existing medical record information | Leveille et al.84 Navaneethan et al.88 | |
| B6 | Portal translation | Translation of portal text into the user's preferred language, in part or in entirety | Ancker et al.78 | |
| B7 | Improve usability | Use heuristic evaluation, participatory or user-centered design to create interfaces | Ali et al.77 | |
| B8 | Better accessibility | Provide portal interfaces for users with disabilities, or limited literacy, technology experience, or broadband access | Ancker et al.78 Graetz et al.80 | |
| Category C. Task-based Interventions | ||||
| C9 | Prescribe tasks | Assign patients tasks within the portal to improve understanding of care | Shaw et al.91 |
|
| Category D. Environment-based Interventions | ||||
| D10 | Provide technology | Offer devices or internet connectivity for patients to access their portals | Greysen et al.81 Kim et al.82 |
|
| Category E. Organization-based Interventions | ||||
| E11 | Modify policy | Implement policy strategies to ensure all patients receive portal access | Ancker et al.78 |
|
| E12 | Increase exposure | Increase exposure to reminders and information about portal use | Mafi et al.86 Turvey et al.93 Stein et al.92 |
|
Includes studies that did not meet our eligibility criteria as additional examples.
Findings of individual studies
Table 4 summarizes the key findings of included studies. Supplementary Table 2 defines each outcome measure and reports how frequently it is used.
Table 4.
Summary of key findings for included studies
| Outcomes |
Findings |
|||||
|---|---|---|---|---|---|---|
| Study | Main Comparison | Category | Description / Timing | Intervention group | Comparison group | P value |
| Portal Use | ||||||
| Casey 201679 | Received education vs did not | Messages | Number of messages sent in the 4 weeks post-intervention | 54 messages | 12 messages | <.001 |
| Graetz et al. 201880 | After mobile access vs before | Login-days | Mean days user logged in per month over a one-year period | 2.86 days/month | 2.00 days/month | <.001b |
| Timeliness | Percent of lab test results viewed within 7 days over a one-year period | 63.8% (Non-white race) | 58.8% (Non-white race) | <.001 | ||
| 72.6% (White race) | 72.3% (White race) | .439 | ||||
| Greysen et al. 201881 | Received education vs did not | Logins | Percent of patients able to login without any assistance, the same day or 7 days after training | 64% (same day) | 60% (same day) | .65 |
| 58% (7 days) | 55% (7 days) | .86 | ||||
| Mean number of logins within 7 days post-discharge | 3.48 logins | 2.94 logins | .60 | |||
| Messages | Percent of patients able to view messages without any assistance, the same day or 7 days after training | 92% (same day) | 77% (same day) | .04 | ||
| 48% (7 days) | 38% (7 days) | .55 | ||||
| Mean number of message clicks within 7 days post-discharge | 5.98 clicks | 3.98 clicks | .33 | |||
| Test results | Percent of patients able to view test results without any assistance, the same day or 7 days after training | 86% (same day) | 77% (same day) | .23 | ||
| 44% (7 days) | 38% (7 days) | .59 | ||||
| Mean number of test result clicks within 7 days post-discharge | 5.68 clicks | 4.36 clicks | .49 | |||
| Kim et al. 200582 | Technical help vs none | Updates | Percent of user-made information updates occurring when help is available | 58% of updates | 42% of updates | Not reported |
| Leveille et al. 201684 | After OpenNotes vs before | Binary use | Percent of patients using the portal 6-12 months before and after OpenNotes | 78% used portala | 84% used portal | <.001b |
| Login-days | Percent of login-days for record seeking6-12 months before and after OpenNotes | 35% record seekinga | 24% record seeking | <.001b | ||
| Lyles et al. 201885 | In-person vs online training | Activation | Percent of patients who enrolled within 3-6 months of training | 19% enrolled | 20% enrolled | .9 |
| Logins | Percent of enrolled patients who logged in once or more within 3-6 months of training | 21% logged in | 20% logged in | .8 | ||
| Any training vs none | Activation | Percent of patients who enrolled within 3-6 months after training | 20% enrolled | 8% enrolled | <.001 | |
| Logins | Percent of enrolled patients who logged in once or more within 3-6 months of training | 21% logged in | 9% logged in | <.001 | ||
| Mafi et al. 201686 | Email reminders vs none | Notes | Effect of discontinuing reminders on viewing Visit Notes within 30 days | 1.00 (reference group) | 0.20 (risk ratio) | <.001b |
| McInnes et al. 201387 | Received education vs did not | Overall use | Mean score on a self-reported 4-item portal use scale directly after training, and again 3 months after training | 2.00 (end of training) | 0.36 (before training) | <.001 |
| 1.36 (3 months later) | 0.36 (before training) | .01 | ||||
| Navaneethan et al. 201888 | Patient navigator vs none | Login-days | Mean total number of days user logged over the 2-year study period | 70 days /2 years | 45 days /2 years | .10 |
| Logins | Percent with more than 48 logins over the 2-year study period | 70% (>48 logins) | 46% (>48 logins) | .04 | ||
| Clicks | Median number of clicks on the portal over the 2-year study period | 427 clicks | 269 clicks | .08 | ||
| Phelps et al. 201489 | Help with credentialing vs none | Initial login | Effect of provision of assistance with credentialing on completing an initial login | 3.22 (odds ratio)a | 1.00 (reference group) | <.001b |
| Ramsey et al. 201790 | MyChart Geniuses vs none | Sign up | Percent of patients who signed up for the portal during the 8-month study period | 86% signed upa | 59% signed up | <.001b |
| Activation | Percent of signed-up patients activating their account in the 8-month study period | 20% activateda | 77% activated | <.001b | ||
| Shaw et al. 201791 | Received education plus video assignment vs did not | Binary use | Number reporting use 30 days after intervention vs 6 months before | 4 out of 19 | 2 out of 19 | Not reported |
| Stein et al. 201892 | Received education plus reminder emails vs did not | Activation | Percent of inpatients who registered an account ≥2 weeks post-discharge | 48% enrolled | 11% enrolled | <.01 |
| Logins | Percent who self-reported an attempt to login ≥2 weeks post-discharge | 60% logged in | 35% logged in | .05 | ||
| Turvey et al. 201693 | Received education vs did not | Blue Buttonc | Percent who gave outside providers content generated with Blue Button | 90% | 17% | <.001 |
| Weisner et al. 201694 | Received education vs did not | Login-days | Mean days user logged in per month in the 6 months post-intervention | 1.7 days/month | 1.1 days/month | .001 |
| Messages | Mean messages from provider per month in the 6 months post-intervention | 0.6 messages/month | 0.4 messages/month | .02 | ||
| Test results | Mean login-days per month for test results in the 6 months post-intervention | 0.3 days/month | 0.2 days/month | <.001 | ||
| Predictors of Portal Use | ||||||
| Ali et al. 201877 | Portal version 2 vs version 1 | Usability | Mean System Usability Scale score | 81.9 out of 100 | 69.2 out of 100 | .049 |
| Greysen et al. 201881 | Received education vs did not | Satisfaction | Percent satisfied with using the tablet to access and navigate the portal | 88% (same day) | 83% (same day) | .48 |
| Leisy et al. 201783 | After tutorial vs before | Comfort | Self-reported percent increase in comfort with login in previously unenrolled patients | 77% (after) | Not reported (baseline) | Not reported |
| Lyles et al. 201885 | After any training vs before | Intended use | Percent with intention to use the portal 3–6 months after training | 53% intend to use | 72% intend to use | .01 |
| Confidence | Percent with high confidence in their ability to use the portal without help, 3–6 months after training | 77% confident | 67% confident | .53 | ||
| Skills | Percent with self-reported skill in portal use, 3-6 months after training | 78% skilled | 63% skilled | .03 | ||
| Disparities in Portal Use | ||||||
| Ancker et al. 201778 | After new policy vs before | Age | Percent of patients >65 years old who received an offer or who repeatedly used the portal in 2014 (after) vs 2011 (before) | 97% received offers | 27% received offers | <.001b |
| 11% repeated use | 9% repeated use | <.001b | ||||
| Race | Difference in percent of non-black vs black patients who received an offer or who repeatedly used the portal in 2014 (after) vs 2011 (before) | 0.0% difference in offers | 2.1% difference in offers | <.001b | ||
| 1.5% difference in use | 2.9% difference in use | <.001b | ||||
Estimates calculated from published data by systematic review authors.
P value calculated by systematic review authors.
Blue Button is a system for patients to download their own health records.
Patient portal use
Fifteen out of 18 studies (83%) addressed an outcome related to portal use, including portal enrollment (aka activation, credentialing, or initiation), logins, timely use, clicks, persistent use, and use of features. Commonly reported outcome measures included login-days, portal activation, binary portal use [yes/no], total portal logins, portal features viewed, and secure messages sent. Supplementary Table 2 contains definitions of each measure.
Ten out of 18 studies (56%) reported on how technical training or assistance for patients impacted portal use.79,81,85,87–92,94 Eight of the 10 reported or permitted calculation of statistical significance, of which 6 demonstrated benefit (the intervention increased portal use), 1 demonstrated neutrality (ie, the intervention did not impact portal use), and 1 demonstrated mixed results (ie, the intervention both increased and decreased aspects of portal use). Lyles et al.85 found that any type of technical training increased activation (20% vs 8% control, p < .001) and binary use (21% vs 9% control, p < .001), but found no differences between in-person and online training. McInnes et al.87 reported that training increased patients' scores on a self-reported 4-item portal use scale (mean of 2.00 after vs 0.36 before, p < .001). The increase persisted 3 months after training (mean of 1.36 at 3 months vs 0.36 before, p = .01). Navaneethan et al.88 found that logins significantly increased when patient navigators146 offered portal training and ongoing technical support (estimated median of 49 vs 37 usual care, 36 portal only, 41 navigator and portal, p = .04). Phelps et al.89 reported that patients from health centers providing credentialing assistance had higher odds of completing an initial login (odds ratio 3.22, 95% CI: 2.17–4.76), although risk of bias was high. Stein et al.92 found that 1 education session for hospitalized patients, along with 2 follow-up email reminders, increased portal registration (48% vs 11% control, p < .01) but not attempted logins (60% vs 33% control, p = .05). Weisner et al.94 reported that login-days per month significantly increased after 6 group education sessions on patient engagement and health information technology resources (mean of 1.7 vs 1.1 control, p < .001). Greysen et al.81 found that 1 individual education session for hospitalized patients did not significantly increase same-day ability to login (64% vs 60% control, p = .65) or logins within 1 week post-discharge (mean of 3.48 vs 2.94 control, p = .60). Ramsey et al.90 reported that trained portal educators (MyChart Geniuses) signed up significantly more patients (86% vs 59% general population, p < .001), but significantly fewer patients that signed up activated their portal accounts (20% vs 77% general population, p < .001).
Five out of 18 studies (28%) observed how technical training or assistance for patients impacts use of specific features.79,81,82,93,94 Four of the 5 reported statistical significance, 3 for benefit (ie, increased use of features) and 1 neutral (ie, no impact on use of features). Casey79 reported that patients sent more secure messages in the month after education (frequency of 54 vs 12 control, p < .001), although risk of bias was unclear. Turvey et al.93 studied Blue Button, a portal-based system for patients to download their health records, including their continuity of care document, although risk of bias was unclear. Patients shared their continuity of care document significantly more frequently with outside providers after Blue Button training (90% vs 17% control, p < .001). Weisner et al.94 found that 6 education sessions significantly increased secure messages per month (mean of 0.6 vs 0.4 control, p = .02) and login-days per month for laboratory test results (mean of 0.3 vs 0.2 control, p < .001). Greysen et al.81 found that 1 education session did not significantly increase clicks on secure messages (mean of 5.98 vs 3.98 control, p = .33) or clicks on laboratory test results (mean of 5.68 vs 4.36 control, p = .49) within 1 week post-discharge.
Three studies of interventions besides patient education reported or permitted calculation of statistical significance, 2 for benefit and 1 mixed. Graetz et al.80 studied the impact of adding mobile access to computer-only access. Adding mobile access increased login-days per month (0.78 login-days more [adjusted], 95% CI: 0.74–0.83). Adding mobile access also increased timeliness, defined as percent of test results viewed within 1 week, among non-whites (63.8% vs 58.8% control, p < .001) but not among whites (72.6% vs 72.3% control, p = .439). Mafi et al.86 studied the effect of email reminders on patients viewing their doctor's notes. Note-viewing declined substantially at 1 institution when email alerts ceased (relative risk 0.20, 95% CI: 0.17–0.23), but persisted at another institution where alerts continued (relative risk 0.94, 95% CI: 0.89–1.00). Leveille et al.84 found that portal use decreased after OpenNotes (78% after vs 84% before, p < .001), although the statistical significance may have resulted from the large sample size and may not indicate any meaningful clinical difference. However, the percentage of login-days dedicated to record-seeking increased after OpenNotes (35% after vs 24% before, p < .001).
Predictors of patient portal use
Seven out of 18 studies (39%) reported on predictors of portal use, including offers of enrollment, patient-assessed usability, patient perceptions, and patient intended use.77,79,81,83,85,90,93 Three of the 7 studies reported statistical significance, 1 for benefit, 1 neutral, and 1 mixed. Ali et al.77 found that an iterative user evaluation improved portal usability (mean System Usability Score 81.9/100 after vs 69.2/100 before, p = .049). Greysen et al.81 reported that an education session for hospitalized patients did not significantly improve satisfaction with portal access through hospital-provided tablets (88% vs 83% control, p = .48). Lyles et al.85 found that technical training significantly increased self-reported skill in portal use (78% after vs 63% before, p = .03), but not self-reported confidence (77% after vs 67% before, p = .53). Furthermore, technical training significantly decreased intention to use the portal (53% after vs 72% before, p = .01).
Disparities in patient portal use
Only 1 study reported on how an intervention impacted health-equity–related disparities in portal use. Ancker et al.78 studied a universal access policy, or policy declaring that all patients must be offered portal enrollment. Before the policy's implementation, vulnerable groups were less likely to receive offers of portal enrollment and subsequently use the portal. The vulnerable groups included the elderly, racial minorities, and the uninsured or publicly insured. Three years post-intervention, only insurance status remained a significant predictor in multivariate models.
DISCUSSION
A growing body of literature suggests that patient portals can prevent medical errors,6–11 increase shared decision-making,12–17 and improve at least certain health outcomes.18,19 Unfortunately, more than 100 studies document disparities in portal use,28,40–56 and interventions will be critical to ensure portals do not disproportionately benefit more advantaged populations. Despite this, our results suggest that few studies have evaluated interventions to reduce disparities in portal use. Due to the strong evidence of disparities in use, the limited research on addressing them, and the need to ensure all populations benefit from portals, we recommend that researchers shift from identifying disparities in portal use to systematically addressing them. Additionally, we recommend that future studies measure interventions' impact on disparities in use directly, as most studies to date have not. Finally, categorization using the SEIPS model demonstrated that most interventions to date addressed only the individual (person) component, and lacked coverage of the other components as well as combinations of components. To enhance impact, we recommend that future interventions affect, or at least consider the repercussions on, multiple components.
Out of 18 included studies, 15 assessed the intervention's impact on portal use and 7 on predictors of use. Surprisingly, only 1 study78 assessed impact on disparities in use. To generate the best evidence on how interventions impact disparities in portal use, future studies should measure these disparities directly. This may include disparities on age, sex, race, ethnicity, preferred language, insurance status, income, level of education, technology access, technology experience, health literacy, numeracy, functional literacy, illness status, and disability status. Surprisingly, almost half of included studies did not report participants' race and ethnicity. At minimum, studies should report participants' age, sex, race, and ethnicity, which will enable readers to better interpret results and determine generalizability.
Technical training and assistance programs for patients currently have the best evidence for increasing portal use in vulnerable populations. Other interventions have not been sufficiently studied to draw conclusions. Thirteen out of 18 studies focused on patient education, either alone (7 studies) or in combination with other interventions (6 studies). In other research domains such as patient safety, training is considered a weak action because it affects 1 individual at a time without reducing the systemic drivers of error147 or, in this case, the systemic drivers of inequity. In contrast, strong actions eliminate potential sources of error (or inequity) from a system. For example, a weak action may involve training a patient to mitigate issues related to portal usability, whereas a strong action would involve re-designing the interface to eliminate usability issues. Additional examples of strong actions may include: (1) free or low-cost internet access via smartphone or broadband, (2) data delivery through 2G and 3G networks in addition to 4G, (3) creating accessible and easily understandable policies, and (4) ensuring software adheres to accessibility, legibility, and readability standards for persons with disabilities and elderly persons.148 Importantly, strong actions have been demonstrated to be more sustainable as they facilitate system-wide impact,149 as opposed to impact on an individual-by-individual basis. Strength of action frameworks designed for patient safety do, however, acknowledge that weak actions may be necessary stopgap solutions while stronger actions are implemented.147
The interventions we reviewed were heterogeneous in type and intensity, and could be categorized using various approaches. Categorization based on the SEIPS model was not meant to be an all-encompassing approach, but was meant to inform concerned researchers, clinicians, and administrators on the gaps in the current literature. Interestingly, few studies intervened on multiple components of the work system (person, tool, task, environment, and organization) or combined multiple intervention types. The SEIPS model stresses the importance of considering the tightly coupled, interactive nature of system components.73–75 Future work should explore composite approaches that address multiple components and leverage multiple types of interventions to maximize impact. As an example, the recent PRISM (Personal Reminder Information and Social Management) randomized controlled trial evaluated a multi-component intervention to improve social support for older adults.150,151 Participants received computers (technology component) with iteratively designed programs (task component), and received internet access (environment component), computer use training (individual component), and organizational support (organization component) as needed. The intervention demonstrated efficacy for improving social support. The efficacy of similar multi-component interventions for improving portal use remains to be studied.
The included studies reported several unintended consequences of interventions. Ramsey et al.90 found that fewer patients signed up by MyChart Geniuses activated their portal accounts. One potential reason is that MyChart Geniuses target patients with lower technology literacy than the general population, and the intervention is insufficient to overcome technology-literacy–based barriers to activation. This hypothesis is consistent with previous research suggesting that technical assistance with activation is insufficient to overcome barriers to subsequent use.143 Leveille et al.84 reported that portal use decreased after OpenNotes, and Lyles et al.85 found technical training significantly decreased intention to use the portal. Reasons for these unintended consequences remain to be explored.
In the included studies, measures of portal use varied greatly in definition and in timing. To create comparable evidence, the field will need to develop standardized measures or metrics of portal use. Single measures many not provide the best overall picture of portal use, and composite metrics may be needed. For example, logins may not accurately reflect use in situations where patients login infrequently, but spend hours browsing after each login. Common metrics from the web analytics domain include downloads, installations, acquisition, user growth rate, retention rate, churn rate, stickiness, session length, and daily or monthly active use.152 Commonly used web and mobile analytics software may help researchers record additional metrics of portal use.
The included studies almost always excluded non-English speakers and hospitalized patients. Therefore, results may not apply to these populations. The studies we examined were conducted in various outpatient settings in the US, including academic, safety net, and veterans hospitals. Therefore, the findings are more likely to apply to the outpatient setting. Five out of 18 studies had high or unclear risk of bias. In a recent review, Showell40 identified common sources of selection bias in studies of portal users, including: (1) exclusion of participants with critical illness, (2) exclusion of non-English speakers, and (3) exclusion of participants with limited technology experience. Recruiting these populations is resource-intensive and time-consuming,153 but necessary to reduce selection bias and ensure generalizability.
Limitations
A potential limitation of our review is incomplete retrieval of relevant research. Because we included a broad variety of study designs, intervention types, and outcome measures, developing an inclusive search strategy proved difficult. Occasionally, Medical Subject Headings did not include relevant terms (for example, no term for “patient portal use” exists). We mitigated these limitations by collaborating with an experienced librarian and incorporating supplemental search strategies such as table-of-contents review of pertinent journals. However, we cannot exclude the possibility that we missed potentially eligible studies. Another potential limitation is publication bias and selective reporting. We do not have information about unpublished studies or outcomes, limiting our certainty about the potential for publication bias. Several studies did not report statistical significance for outcomes, limiting what we could extract from the literature. In 3 included studies, the primary outcome differed from the portal-related outcome, meaning the portal-related outcome was potentially underpowered, less detailed, or analyzed in a post-hoc manner.
CONCLUSION
Disparities in patient portal use may worsen existing health inequities and prevent portals from benefiting all populations. More than 100 studies have described disparities in portal use, however, our review suggests that far fewer have evaluated interventions to overcome disparities. We found that most interventions focused on the individual, rather than including the portal-, task-, environment-, or organization-based components, which could increase their effectiveness. Additional research is urgently needed to identify effective, cross-cutting interventions that reduce disparities in portal use.
FUNDING
This work was supported by the National Library of Medicine (R01LM012964, PI: Ancker; T15LM007079, trainee: Grossman), the National Institute of Nursing Research (R00NR016275, PI: Masterson Creber), and the Agency for Healthcare Research and Quality (R01HS21816, PI: Vawdrey).
CONTRIBUTORS
LVG, DKV, and JSA collaboratively conceptualized this review. DW conducted the literature searches. LVG, RMC, and JSA conducted the initial and full-text screening. LVG, RMC, NCB, and JSA performed the data extraction, risk of bias assessment, and analyses. LVG drafted the manuscript, and all authors contributed to refining all sections and critically editing the paper.
SUPPLEMENTARY MATERIAL
Supplementary material is available online at Journal of the American Medical Informatics Association.
CONFLICT OF INTEREST STATEMENT
None declared.
Supplementary Material
REFERENCES
- 1. Delbanco T, Walker J, Darer JD, et al. Open notes: doctors and patients signing on. Ann Intern Med 2010; 153 (2): 121–5. [DOI] [PubMed] [Google Scholar]
- 2. Delbanco T, Walker J, Bell SK, et al. Inviting patients to read their doctors’ notes: a quasi-experimental study and a look ahead. Ann Intern Med 2012; 157 (7): 461–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Walker J, Leveille SG, Ngo L, et al. Inviting patients to read their doctors’ notes: patients and doctors look ahead. Ann Intern Med 2011; 155 (12): 811.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. American Hospital Association. Individuals’ Ability to Electronically Access Their Hospital Medical Records, Perform Key Tasks Is Growing. 2016. http://www.aha.org/research/reports/tw/16jul-tw-healthIT.pdf. Accessed February 8, 2017.
- 5. HealthIT.gov. What is a patient portal? https://www.healthit.gov/providers-professionals/faqs/what-patient-portal. Accessed August 8, 2017.
- 6. Weingart SN, Toth M, Eneman J, et al. Lessons from a patient partnership intervention to prevent adverse drug events. Int J Qual Heal Care 2004; 16 (6): 499–507. [DOI] [PubMed] [Google Scholar]
- 7. Weingart SN, Hamrick HE, Tutkus S, et al. Medication safety messages for patients via the web portal: the MedCheck intervention. Int J Med Inform 2008; 77 (3): 161–8. [DOI] [PubMed] [Google Scholar]
- 8. Heyworth L, Paquin AM, Clark J, et al. Engaging patients in medication reconciliation via a patient portal following hospital discharge. J Am Med Inform Assoc 2014; 21 (e1): e157–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Schnipper JL, Gandhi TK, Wald JS, et al. Effects of an online personal health record on medication accuracy and safety: a cluster-randomized trial. J Am Med Inform Assoc 2012; 19 (5): 728–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Dullabh PM, Sondheimer NK, Katsh E, Evans MA.. How patients can improve the accuracy of their medical records. EGEMS (Wash DC) 2014; 2 (3): 1080.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Staroselsky M, Volk LA, Tsurikova R, et al. Improving electronic health record (EHR) accuracy and increasing compliance with health maintenance clinical guidelines through patient access and input. Int J Med Inform 2006; 75 (10–11): 693–700. [DOI] [PubMed] [Google Scholar]
- 12. Caligtan CA, Carroll DL, Hurley AC, Gersh-Zaremski R, Dykes PC.. Bedside information technology to support patient-centered care. Int J Med Inform 2012; 81 (7): 442–51. [DOI] [PubMed] [Google Scholar]
- 13. Dalal AK, Dykes PC, Collins S, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: a preliminary evaluation. J Am Med Inform Assoc 2016; 23 (1): 80–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stade D, Dykes P.. Nursing leadership in development and implementation of a patient-centered plan of care toolkit in the acute care setting. Comput Inform Nurs 2015; 33 (3): 90–2. [DOI] [PubMed] [Google Scholar]
- 15. Maher M, Hanauer DA, Kaziunas E, et al. A novel health information technology communication system to increase caregiver activation in the context of hospital-based pediatric hematopoietic cell transplantation: a pilot study. JMIR Res Protoc 2015; 4 (4): e119.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Maher M, Kaziunas E, Ackerman M, et al. User-centered design groups to engage patients and caregivers with a personalized health information technology tool. Biol Blood Marrow Transplant 2016; 22 (2): 349–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dykes PC, Carroll DL, Hurley AC, et al. Building and testing a patient-centric electronic bedside communication center. J Gerontol Nurs 2013; 39 (1): 15–9. [DOI] [PubMed] [Google Scholar]
- 18. Kruse CS, Bolton K, Freriks G.. The effect of patient portals on quality outcomes and its implications to meaningful use: a systematic review. J Med Internet Res 2015; 17 (2): e44.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mold F, De Lusignan S, Sheikh A, et al. Patients’ online access to their electronic health records and linked online services: a systematic review in primary care. Br J Gen Pract 2015; 65 (632): e141–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chase D. Patient engagement is the blockbuster drug of the century. Forbes, 2012. [Google Scholar]
- 21. Landro L. How to get patients to take more control of their medical decisions. The Wall Street Journal, 2017. [Google Scholar]
- 22. Chen P. Letting patients read the doctor’s notes. New York Times, 2012. [Google Scholar]
- 23. Adler-Milstein J, DesRoches CM, Kralovec P, et al. Electronic health record adoption in US hospitals: progress continues, but challenges persist. Health Aff 2015; 34 (12): 2174–80. [DOI] [PubMed] [Google Scholar]
- 24. Adler-Milstein J, DesRoches CM, Furukawa MF, et al. More than half of US hospitals have at least a basic EHR, but stage 2 criteria remain challenging for most. Health Aff 2014; 33 (9): 1664–71. [DOI] [PubMed] [Google Scholar]
- 25. Ancker JS, Silver M, Kaushal R.. Rapid growth in use of personal health records in New York, 2012-2013. J Gen Intern Med 2014; 29 (6): 850–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Undem T. Consumers and Health Information Technology: A National Survey. Oakland, CA; 2010. http://scholar.google.com/scholar? hl=en&btnG=Search&q=intitle: Consumers+and+Health+Information+Technology+:+A+National+Survey#0. Accessed November 10, 2018. [Google Scholar]
- 27. Halamka JD, Mandl KD, Tang PC. Early experiences with personal health records. J Am Med Inform Assoc 2008; 15 (1): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ancker JS, Hafeez B, Kaushal R.. Socioeconomic disparities in adoption of personal health records over time. Am J Manag Care 2016; 22 (8): 539–40. [PMC free article] [PubMed] [Google Scholar]
- 29. Patel V, Barker W, Siminerio E. ONC Data Brief No. 30: Trends in Consumer Access and Use of Electronic Health Information. 2015. https://dashboard.healthit.gov/evaluations/data-briefs/trends-consumer-access-use-electronic-health-information.php. Accessed November 10, 2018.
- 30. Patel V, Johnson C. ONC Data Brief No. 40: Individuals’ Use of Online Medical Records and Technology for Health Needs. 2017. https://www.healthit.gov/sites/default/files/page/2018-03/HINTS-2017-Consumer-Data-Brief-3.21.18.pdf. Accessed November 10, 2018.
- 31. Volpp KG, Mohta NS. Patient Engagement Survey: Far to Go to Meaningful Participation. NEJM Catal. 2016. http://catalyst.nejm.org/patient-engagement-initiatives-survey-meaningful-participation/. Accessed November 10, 2018.
- 32. Walker J, Darer JD, Elmore JG, Delbanco T.. The road toward fully transparent medical records. N Engl J Med 2014; 370 (1): 6–8. [DOI] [PubMed] [Google Scholar]
- 33. Bitton A, Poku M, Bates D.. Policy context and considerations for patient engagement with health information technology In: Grando M, Rozenblum R, Bates D, eds. Information Technology for Patient Empowerment in Healthcare. Berlin: Walter de Gruyter Inc.; 2015: 75–90. [Google Scholar]
- 34.2014 Edition EHR Certification Criteria Grid Mapped to Meaningful Use Stage 2. https://www.healthit.gov/sites/default/files/2014editionehrcertificationcriteria_mustage2.pdf. Accessed November 10, 2018.
- 35. Apter AJ. Can patient portals reduce health disparities? A perspective from asthma. Ann ATS 2014; 11 (4): 608–12. [DOI] [PubMed] [Google Scholar]
- 36. Gibbons MC, Casale CR.. Reducing disparities in health care quality: the role of health IT in underresourced settings. Med Care Res Rev 2010; 67 (5_suppl): 155S–62S. [DOI] [PubMed] [Google Scholar]
- 37. Braveman PA, Kumanyika S, Fielding J, et al. Health disparities and health equity: the issue is justice. Am J Public Health 2011; 101 (Suppl 1): S149–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. LaVeist TA, Gaskin D, Richard P.. Estimating the economic burden of racial health inequalities in the United States. Int J Health Serv 2011; 41 (2): 231–8. [DOI] [PubMed] [Google Scholar]
- 39. Devoe JE, Baez A, Angier H, Krois L, Edlund C, Carney PA.. Insurance + access not equal to health care: typology of barriers to health care access for low-income families. Ann Fam Med 2007; 5 (6): 511–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Showell C. Barriers to the use of personal health records by patients: a structured review. PeerJ 2017; 5: e3268.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Logue MD, Effken JA.. An exploratory study of the personal health records adoption model in the older adult with chronic illness. Inform Prim Care 20 (3): 151–69. [DOI] [PubMed] [Google Scholar]
- 42. Chrischilles EA, Hourcade JP, Doucette W, et al. Personal health records: a randomized trial of effects on elder medication safety. J Am Med Inform Assoc 2014; 21 (4): 679–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yamin CK, Emani S, Williams DH, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med 2011; 171 (6): 568–74. [DOI] [PubMed] [Google Scholar]
- 44. Lober WB, Zierler B, Herbaugh A, et al. Barriers to the use of a personal health record by an elderly population. AMIA Annu Symp Proc 2006; 2006:514–518. [PMC free article] [PubMed] [Google Scholar]
- 45. Gordon P, Camhi E, Hesse R, et al. Processes and outcomes of developing a continuity of care document for use as a personal health record by people living with HIV/AIDS in New York City. Int J Med Inform 2012; 81 (10): 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Emani S, Yamin CK, Peters E, et al. Patient perceptions of a personal health record: a test of the diffusion of innovation model. J Med Internet Res 2012; 14 (6): e150.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW.. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med 2011; 26 (10): 1112–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc 2011; 18 (3): 318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Kim E-H, Stolyar A, Lober WB, et al. Challenges to using an electronic personal health record by a low-income elderly population. J Med Internet Res 2009; 11 (4): e44.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Roblin DW, Houston TK, Allison JJ, Joski PJ, Becker ER.. Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc 2009; 16 (5): 683–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Taha J, Czaja SJ, Sharit J, Morrow DG.. Factors affecting usage of a personal health record (PHR) to manage health. Psychol Aging 2013; 28 (4): 1124–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Taha J, Sharit J, Czaja SJ.. The impact of numeracy ability and technology skills on older adults’ performance of health management tasks using a patient portal. J Appl Gerontol 2014; 33 (4): 416–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Sarkar U, Karter AJ, Liu JY, et al. The literacy divide: health literacy and the use of an internet-based patient portal in an integrated health system—results from the diabetes study of northern California (DISTANCE). J Health Commun 2010; 15 (Suppl 2): 183–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ancker JS, Mauer E, Hauser D, Calman N.. Expanding access to high-quality plain-language patient education information through context-specific hyperlinks. AMIA Annu Symp Proc 2016; 17: 277–84. [PMC free article] [PubMed] [Google Scholar]
- 55. Atreja A, Mehta N, Miller D, et al. One size does not fit all: using qualitative methods to inform the development of an internet portal for multiple sclerosis patients. AMIA Annu Symp Proc 2005; 2005:16–20. [PMC free article] [PubMed] [Google Scholar]
- 56. Kruse RL, Koopman RJ, Wakefield BJ, et al. Internet use by primary care patients: where is the digital divide? Fam Med 2012; 44 (5): 342–7. [PubMed] [Google Scholar]
- 57. Veinot TC, Mitchell H, Ancker JS.. Good intentions are not enough: how informatics interventions can worsen inequality. J Am Med Inform Assoc 2018; 25 (8): 1080–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lorenc T, Petticrew M, Welch V, Tugwell P.. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health 2013; 67 (2): 190–3. [DOI] [PubMed] [Google Scholar]
- 59. Hart JT. The inverse care law. Lancet 1971; 1 (7696): 405–12. [DOI] [PubMed] [Google Scholar]
- 60. Moher D, Liberati A, Tetzlaff J, Altman DG, Prisma G.. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009; 151 (4): 264–9. W64. [DOI] [PubMed] [Google Scholar]
- 61. O’Neill J, Tabish H, Welch V, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J Clin Epidemiol 2014; 67 (1): 56–64. [DOI] [PubMed] [Google Scholar]
- 62. Oliver S, Kavanagh J, Caird J, et al. Health promotion, inequalities and young people’s health: a systematic review of research. 2008. London: EPPI-Centre, Social Science Research Unit, Institute of Education, University of London.
- 63. Oliver S, Dickson K, Newman M.. Getting started with a review In: Gough D, Oliver S, Thomas J, eds. An Introduction to Systematic Reviews. Los Angeles, CA: SAGE Publications; 2012: 71–92. [Google Scholar]
- 64. Prey JE, Woollen J, Wilcox L, et al. Patient engagement in the inpatient setting: a systematic review. J Am Med Inform Assoc 2014; 21 (4): 742–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Ennis L, Rose D, Callard F, Denis M, Wykes T.. Rapid progress or lengthy process? Electronic personal health records in mental health. BMC Psychiatry 2011; 11: 117.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Irizarry T, De Vito Dabbs A, Curran CR.. Patient portals and patient engagement: a state of the science review. J Med Internet Res 2015; 17 (6): e148.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Wildenbos GA, Peute L, Jaspers M.. Facilitators and barriers of electronic health record patient portal adoption by older adults: a literature study. Stud Health Technol Inform 2017; 235: 308–12. [PubMed] [Google Scholar]
- 68. Sharit J, Lisigurski M, Andrade AD, et al. The roles of health literacy, numeracy, and graph literacy on the usability of the VA’s personal health record by veterans. J Usability Stud 2014; 9 (4): 173–93. [Google Scholar]
- 69. Ruiz JG, Andrade AD, Hogue C, et al. The association of graph literacy with use of and skills using an online personal health record in outpatient veterans. J Health Commun 2016; 21 (sup2): 83–90. [DOI] [PubMed] [Google Scholar]
- 70. Cochrane C. Covidence. https://community.cochrane.org/help/tools-and-software/covidence. Accessed December 9, 2018.
- 71. Agency for Healthcare Research and Quality. Methods Guide for Effectiveness and Comparative Effectiveness Reviews. Rockville, MD: US Department of Health and Human Services; 2012. http://www.effectivehealthcare.ahrq.gov/ehc/products/60/318/CER-Methods-Guide-140109.pdf. [PubMed] [Google Scholar]
- 72. Higgins, JPT, Green, S. The Cochrane Collaboration. In: Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions 5.1.0. 2011.
- 73. Carayon P, Schoofs Hundt A, Karsh B-T, et al. Work system design for patient safety: the SEIPS model. Qual Saf Health Care 2006; 15 (Suppl_1): i50–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Carayon P, Wooldridge A, Hose BZ, Salwei M, Benneyan J.. Challenges and opportunities for improving patient safety through human factors and systems engineering. Health Aff (Millwood) 2018; 37 (11): 1862–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 2013; 56 (11): 1669–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Owens DK, Lohr KN, Atkins D, et al. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions-agency for healthcare research and quality and the effective health-care program. J Clin Epidemiol 2010; 63 (5): 513–23. [DOI] [PubMed] [Google Scholar]
- 77. Ali S, Romero J, Morrison K, Hafeez B, Ancker J.. Focus section health IT usability: applying a task-technology fit model to adapt an electronic patient portal for patient work. Appl Clin Inform 2018; 09 (01): 174–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Ancker JS, Nosal S, Hauser D, Way C, Calman N.. Access policy and the digital divide in patient access to medical records. Health Policy Technol 2017; 6 (1): 3–11. [Google Scholar]
- 79. Casey I. The effect of education on portal personal health record use. Online J Nurs Informatics 2016; 20 (2): 9. [Google Scholar]
- 80. Graetz I, Huang J, Brand R, Hsu J, Reed ME.. Mobile-accessible personal health records increase the frequency and timeliness of PHR use for patients with diabetes. J Am Med Inform Assoc 2019; 26 (1): 50–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Greysen SR, Harrison JD, Rareshide C, et al. A randomized controlled trial to improve engagement of hospitalized patients with their patient portals. J Am Med Inform Assoc 2018; 25 (12): 1626–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Kim E, Mayani A, Modi S, Kim Y, Soh C.. Evaluation of patient-centered electronic health record to overcome digital divide. Conf Proc IEEE Eng Med Biol Soc 2005; 2: 1091–4. [DOI] [PubMed] [Google Scholar]
- 83. Leisy H, Ahmad M, Guevara G, Smith RT.. Engaging patients through an iBooks-based patient portal tutorial. BMJ Innov 2017; 3 (3): 152–6. [Google Scholar]
- 84. Leveille SG, Mejilla R, Ngo L, et al. Do patients who access clinical information on patient internet portals have more primary care visits? Med Care 2016; 54 (1): 17–23. [DOI] [PubMed] [Google Scholar]
- 85. Lyles CR, Tieu L, Sarkar U, et al. A randomized trial to train vulnerable primary care patients to use an online patient portal website. J Am Board Fam Med 2019; 32 (2): 248–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Mafi JN, Mejilla R, Feldman H, et al. Patients learning to read their doctors’ notes: the importance of reminders. J Am Med Inform Assoc 2016; 23 (5): 951–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. McInnes DK, Solomon JL, Shimada SL, et al. Development and evaluation of an internet and personal health record training program for low-income patients with HIV or hepatitis C. Med Care 2013; 51: S62–6. [DOI] [PubMed] [Google Scholar]
- 88. Navaneethan SD, Jolly SE, Schold JD, et al. Pragmatic randomized, controlled trial of patient navigators and enhanced personal health records in CKD. CJASN 2017; 12 (9): 1418–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Phelps RG, Taylor J, Simpson K, Samuel J, Turner AN.. Patients’ continuing use of an online health record: a quantitative evaluation of 14,000 patient years of access data. J Med Internet Res 2014; 16 (10): e241.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Ramsey A, Lanzo E, Huston-Paterson H, Tomaszewski K, Trent M.. Increasing patient portal usage: preliminary outcomes from the MyChart genius project. J Adolesc Health 2018; 62 (1): 29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Shaw CL, Casterline GL, Taylor D, Fogle M, Granger B.. Increasing health portal utilization in cardiac ambulatory patients: a pilot project. Comput Inform Nurs 2017; 35 (10): 512–9. [DOI] [PubMed] [Google Scholar]
- 92. Stein JN, Klein JW, Payne TH, et al. Communicating with vulnerable patient populations: a randomized intervention to teach inpatients to use the electronic patient portal. Appl Clin Inform 2018; 09 (04): 875–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Turvey CL, Klein DM, Witry M, et al. Patient education for consumer-mediated HIE: a pilot randomized controlled trial of the department of veterans affairs Blue Button. Appl Clin Inform 2016; 7(3): 765–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Weisner CM, Chi FW, Lu Y, et al. Examination of the effects of an intervention aiming to link patients receiving addiction treatment with health care: the LINKAGE clinical trial. JAMA Psychiatry 2016; 73 (8): 804–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Greenhalgh T, Wood GW, Bratan T, Stramer K, Hinder S.. Patients’ attitudes to the summary care record and HealthSpace: qualitative study. BMJ 2008; 336 (7656): 1290–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Hemsley B, Georgiou A, Balandin S, et al. The personally controlled electronic health record (PCEHR) for adults with severe communication impairments: findings of pilot research. Stud Health Technol Inform 2015; 214: 100–6. [PubMed] [Google Scholar]
- 97. Robotham D, Mayhew M, Rose D, Wykes T.. Electronic personal health records for people with severe mental illness: a feasibility study. BMC Psychiatry 2015; 15 (1): 192.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Hilton JF, Barkoff L, Chang O, et al. A cross-sectional study of barriers to personal health record use among patients attending a safety-net clinic. PLoS One 2012; 7 (2): 24–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Barron J, Bedra M, Wood J, Finkelstein J.. Exploring three perspectives on feasibility of a patient portal for older adults. Stud Health Technol Inform 2014; 202: 181–4. [PubMed] [Google Scholar]
- 100. Latulipe C, Gatto A, Nguyen HT, et al. Design considerations for patient portal adoption by low-income, older adults. Proc SIGCHI Conf Hum Factor Comput Syst 2015; 3859–68. doi:10.1145/2702123.2702392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Crotty BH, Walker J, Dierks M, et al. Information sharing preferences of older patients and their families. JAMA Intern Med 2015; 175 (9): 1492.. [DOI] [PubMed] [Google Scholar]
- 102. Haverhals LM, Lee CA, Siek KA, et al. Older adults with multi-morbidity: medication management processes and design implications for personal health applications. J Med Internet Res 2011; 13 (2): 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Lee LH, Chou YT, Huang EW, Liou DM.. Design of a personal health record and health knowledge sharing system using IHE-XDS and OWL. J Med Syst 2013; 37 (2): 9921.. [DOI] [PubMed] [Google Scholar]
- 104. Mayberry LS, Kripalani S, Rothman RL, Osborn CY.. Bridging the digital divide in diabetes: family support and implications for health literacy. Diabetes Technol Ther 2011; 13 (10): 1005–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Mishuris RG, Stewart M, Fix GM, et al. Barriers to patient portal access among veterans receiving home-based primary care: a qualitative study. Health Expect 2015; 18 (6): 2296–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Wolff JL, Berger A, Clarke D, et al. Patients, care partners, and shared access to the patient portal: online practices at an integrated health system. J Am Med Inform Assoc 2016; 23 (6): 1150–8. [DOI] [PubMed] [Google Scholar]
- 107. Butler JM, Carter M, Hayden C, et al. Understanding adoption of a personal health record in rural health care clinics: revealing barriers and facilitators of adoption including attributions about potential patient portal users and self-reported characteristics of early adopting users. AMIA Annu Symp Proc 2013; 2013: 152–61. [PMC free article] [PubMed] [Google Scholar]
- 108. Ronda MC, Dijkhorst-Oei L-T, Rutten GE.. Reasons and barriers for using a patient portal: survey among patients with diabetes mellitus. J Med Internet Res 2014; 16 (11): e263.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Lyles CR, Sarkar U, Ralston JD, et al. Patient–provider communication and trust in relation to use of an online patient portal among diabetes patients: the diabetes and aging study. J Am Med Inform Assoc 2013; 20 (6): 1128–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Borbolla D, Del Fiol G, Taliercio V, et al. Integrating personalized health information from medlineplus in a patient portal. Stud Health Technol Inform 2014; 205: 348–52. [PubMed] [Google Scholar]
- 111. Polepalli Ramesh B, Houston T, Brandt C, Fang H, Yu H.. Improving patients’ electronic health record comprehension with NoteAid. Stud Health Technol Inform 2013; 192 (1–2): 714–8. [PubMed] [Google Scholar]
- 112. Chen J, Yu H.. Unsupervised ensemble ranking of terms in electronic health record notes based on their importance to patients. J Biomed Inform 2017; 68: 121–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Zeng-Treitler Q, Goryachev S, Kim H, Keselman A, Rosendale D.. Making texts in electronic health records comprehensible to consumers: a prototype translator. AMIA Annu Symp Proc 2007; 2007:846–50. [PMC free article] [PubMed] [Google Scholar]
- 114. Schillinger D, McNamara D, Crossley S, et al. The next frontier in communication and the ECLIPPSE study: bridging the linguistic divide in secure messaging. J Diabetes Res 2017; 2017: Article ID: 1348242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Tieu L, Sarkar U, Schillinger D, et al. Barriers and facilitators to online portal use among patients and caregivers in a safety net health care system: a qualitative study. J Med Internet Res 2015; 17 (12): e275.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Tieu L, Schillinger D, Sarkar U, et al. Online patient websites for electronic health record access among vulnerable populations: portals to nowhere? J Am Med Inform Assoc 2017; 24 (e1): e47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Grossman LV, Masterson Creber R, Restaino S, Vawdrey DK.. Sharing clinical notes with hospitalized patients via an acute care portal. AMIA Annu Symp Proc 2017; 2017: 800–9. [PMC free article] [PubMed] [Google Scholar]
- 118. Essex B, Doig R, Renshaw J.. Pilot study of records of shared care for people with mental illnesses. BMJ 1990; 300 (6737): 1442–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Schnipper JL, Gandhi TK, Wald JS, et al. Design and implementation of a web-based patient portal linked to an electronic health record designed to improve medication safety: the Patient Gateway medications module. Inform Prim Care 2008; 16 (2): 147–55. [DOI] [PubMed] [Google Scholar]
- 120. Zarcadoolas C, Vaughon WL, Czaja SJ, Levy J, Rockoff ML.. Consumers’ perceptions of patient-accessible electronic medical records. J Med Internet Res 2013; 15 (8): e168.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Schickedanz A, Huang D, Lopez A, et al. Access, interest, and attitudes toward electronic communication for health care among patients in the medical safety net. J Gen Intern Med 2013; 28 (7): 914–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Oster NV, Jackson SL, Dhanireddy S, et al. Patient access to online visit notes. J Int Assoc Provid AIDS Care 2015; 14 (4): 306–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Parrott J, Strathdee G, Brown P.. Patient access to psychiatric records: the patients’ view. J R Soc Med 1988; 81 (9): 520–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Morrow D, Hasegawa-Johnson M, Huang T, et al. A multidisciplinary approach to designing and evaluating Electronic Medical Record portal messages that support patient self-care. J Biomed Inform 2017; 69: 63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Zikmund-Fisher BJ, Exe NL, Witteman HO.. Numeracy and literacy independently predict patients’ ability to identify out-of-range test results. J Med Internet Res 2014; 16 (8): e187.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Zikmund-Fisher BJ, Scherer AM, Witteman HO, et al. Graphics help patients distinguish between urgent and non-urgent deviations in laboratory test results. J Am Med Inform Assoc 2017; 24 (3): 520–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Tao D, Yuan J, Qu X.. Presenting self-monitoring test results for consumers: the effects of graphical formats and age. J Am Med Inform Assoc 2018; 25 (8): 1036–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Zeng-Treitler Q, Kim H, Rosemblat G, Keselman A.. Can multilingual machine translation help make medical record content more comprehensible to patients? Stud Health Technol Inform 2010; 160 (Pt 1): 73–7. [PubMed] [Google Scholar]
- 129. Alpert JM, Krist AH, Aycock RA, Kreps GL.. Applying multiple methods to comprehensively evaluate a patient portal’s effectiveness to convey information to patients. J Med Internet Res 2016; 18 (5): e112.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. McDougald Scott AM, Jackson GP, Ho Y-X, Yan Z, Davison C, Rosenbloom ST.. Adapting comparative effectiveness research summaries for delivery to patients and providers through a patient portal. AMIA Annu Symp Proc 2013; 2013: 959–68. [PMC free article] [PubMed] [Google Scholar]
- 131. Chan CV, Kaufman DR.. A framework for characterizing ehealth literacy demands and barriers. J Med Internet Res 2011; 13 (4): 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Czaja SJ, Zarcadoolas C, Vaughon WL, Lee CC, Rockoff ML, Levy J.. The usability of electronic personal health record systems for an underserved adult population. Hum Factors 2015; 57 (3): 491–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Alpert JM, Desens L, Krist AH, Aycock RA, Kreps GL.. Measuring health literacy levels of a patient portal using the CDC’s clear communication index. Health Promot Pract 2017; 18 (1): 140–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Keselman A, Slaughter L, Arnott-Smith C, et al. Towards consumer-friendly PHRs: patients’ experience with reviewing their health records. AMIA Annu Symp Proc 2007; 2007: 399–403. [PMC free article] [PubMed] [Google Scholar]
- 135. Keselman A, Smith CA.. A classification of errors in lay comprehension of medical documents. J Biomed Inform 2012; 45 (6): 1151–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Odlum M, Gordon P, Camhi E, Valdez E, Bakken S.. Exploring factors related to the adoption and acceptance of an internet-based electronic personal health management tool (EPHMT) in a low income, special needs population of people living with HIV and AIDS in New York City. Stud Health Technol Inform 2014; 201: 145–52. [PubMed] [Google Scholar]
- 137. Smith SG, O’Conor R, Aitken W, Curtis LM, Wolf MS, Goel MS. A.. Disparities in registration and use of an online patient portal among older adults: findings from the LitCog cohort. J Am Med Inform Assoc 2015; 22 (4): 888–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Fernandez N, Copenhaver DJ, Vawdrey DK, Kotchoubey H, Stockwell MS.. Smartphone use among postpartum women and implications for personal health record utilization. Clin Pediatr (Phila) 2017; 56 (4): 376–81. [DOI] [PubMed] [Google Scholar]
- 139. Forchuk C, Reiss JP, O’Regan T, Ethridge P, Donelle L, Rudnick A.. Client perceptions of the mental health engagement network: a qualitative analysis of an electronic personal health record. BMC Psychiatry 2015; 15 (1): 250.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Kim E-H, Stolyar A, Lober WB, et al. Usage patterns of a personal health record by elderly and disabled users. AMIA Annu Symp Proc 2007; 04: 409–13. [PMC free article] [PubMed] [Google Scholar]
- 141. Grossman LV, Feiner SK, Mitchell EG, Masterson Creber RM.. Leveraging patient-reported outcomes using data visualization. Appl Clin Inform 2018; 9 (3): 565–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Masterson Creber RM, Grossman LV, Ryan B, et al. Engaging hospitalized patients with personalized health information: a randomized trial of an inpatient portal. J Am Med Inform Assoc 2019; 26 (2): 115–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Ancker JS, Barrón Y, Rockoff ML, et al. Use of an electronic patient portal among disadvantaged populations. J Gen Intern Med 2011; 26 (10): 1117–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Davis SE, Osborn CY, Kripalani S, Goggins KM, Jackson GP.. Health literacy, education levels, and patient portal usage during hospitalizations. AMIA Annu Symp Proc 2015; 2015: 1871–80. [PMC free article] [PubMed] [Google Scholar]
- 145. Ancker JS, Osorio SN, Cheriff A, Cole CL, Silver M, Kaushal R.. Patient activation and use of an electronic patient portal. Inform Health Soc Care 2015; 40 (3): 254–66. [DOI] [PubMed] [Google Scholar]
- 146. Jolly SE, Navaneethan SD, Schold JD, et al. Development of a chronic kidney disease patient navigator program. BMC Nephrol 2015; 16 (1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. US Department of Veterans Affairs: National Center for Patient Safety. Root Cause Analysis Tools, 2015. https://www.patientsafety.va.gov/docs/RCA_Step_By_Step_Guide_REV7_1_16_FINAL.pdf. Accessed November 10, 2018.
- 148. National Patient Safety Foundation. RCA2: Improving Root Cause Analyses and Actions to Prevent Harm 2015. http://c.ymcdn.com/sites/www.npsf.org/resource/resmgr/PDF/RCA2_first-online-pub_061615.pdf. Accessed November 10, 2018.
- 149. Hettinger AZ, Fairbanks RJ, Hegde S, et al. An evidence-based toolkit for the development of effective and sustainable root cause analysis system safety solutions. J Healthc Risk Manag 2013; 33 (2): 11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Czaja SJ, Boot WR, Charness N, et al. The personalized reminder information and social management system (PRISM) trial: rationale, methods and baseline characteristics. Contemp Clin Trials 2015; 40: 35–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Czaja SJ, Boot WR, Charness N, Rogers WA, Sharit J.. Improving social support for older adults through technology: findings from the PRISM randomized controlled trial. Gerontologist 2018; 58 (3): 467–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Kaushik A. Web Analytics 2.0: the Art of Online Accountability and Science of Customer Centricity. Indianapolis, IN: Wiley; 2009. [Google Scholar]
- 153. UyBico SJ, Pavel S, Gross CP.. Recruiting vulnerable populations into research: a systematic review of recruitment interventions. J Gen Intern Med 2007; 22 (6): 852–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.