Abstract
Background
Lower socioeconomic status (SES) has been associated with higher rates of smoking. Few longitudinal studies have examined indicators of SES at both the neighborhood- and individual-level over time in conjunction with proximal risk factors of cigarette smoking.
Purpose
To examine associations of time-varying measures of SES, demographic factors, and proximal risk factors for smoking net of average trajectories of smoking behavior from ages 30 to 39 in a community sample.
Methods
Data from the Seattle Social Development Project (N = 752), a theory-driven longitudinal study originating in Seattle, WA, were used to estimate trajectories of smoking from age 30 to 39. Time-varying measures of neighborhood poverty, coworker smoking, partner smoking, depression, anxiety, education, income, marital status, and parenthood were associated with smoking over time using latent growth curve modeling.
Results
Results indicated that living in higher poverty neighborhoods was uniquely associated with a greater likelihood of smoking net of average trajectories of smoking from age 30 to 39, gender and race/ethnicity, time-varying measures of SES and demographics, and time-varying measures of proximal risk factors for smoking.
Conclusions
Living in higher poverty neighborhoods presents a unique risk for smoking among adults aged 30 to 39 above and beyond multiple aspects of SES and other potential mechanisms relating SES to smoking.
Keywords: Cigarette smoking, Neighborhood poverty, Risk factors, Latent growth curve
Adults living in higher poverty neighborhoods smoked more cigarettes over 9 years even after accounting for differences in smoking related to demographics, family socioeconomic status, mental health, and exposure to other smokers at home or work.
Each year in the USA, over 450,000 deaths and 300 billion dollars in economic losses are attributable to cigarette smoking-related disease and disability [1]. Despite reductions in smoking prevalence rates in the USA in recent years, disparities by socioeconomic status (SES) have widened over the last several decades [2, 3]. Explanations for maintenance in smoking or difficulties in quitting by lower SES groups have included greater exposure to smoking in work environments [4], low social or family support for quitting [2, 5], mental health problemsuo that often accompany financial strain or other life stressors [6] and may manifest in diagnoses of major depressive disorder or generalized anxiety disorder [7], and increased exposure to tobacco stores or prosmoking advertising [8]. SES, however, is a multifaceted construct that typically includes measures of individual-level income or education [9], but less often considers area-level measures of SES such as neighborhood poverty [10]. In addition, SES measures are typically assessed at a single point in time and static measurements may not adequately reflect changes related to income fluctuations, the benefits of increasing educational attainment, and residential mobility [9, 11]. Longitudinal analyses that consider time-varying measures of both neighborhood- and individual-level SES may improve our understanding of connections between SES and smoking. In addition, it is also important to consider time-varying measures of the mechanisms through which SES is hypothesized to impact smoking [6, 11].
Socioecological theories contend that human behavior is best understood embedded within social contexts such as neighborhood, family, and work environments [12]. Similarly, conceptual models of SES and health posit that the impact of neighborhood-level socioeconomic contexts on health should be assessed in concert with more proximal socioeconomic factors, immediate social contexts, and individual-level psychological factors [7, 13]. Further, there is broad agreement that the social contexts experienced by low SES populations can profoundly influence disparities in both health behaviors and health outcomes [5, 10]. While systematic reviews have consistently linked neighborhood poverty with physical health problems and diagnoses of mental health disorders [10], less consistent links have been shown for health risk behaviors such as heavy alcohol use and cigarette smoking [2, 14]. Neighborhood-focused scholars have suggested that the inconsistency of findings relating neighborhood poverty to health risk behaviors may result from insufficient individual-level controls for SES [10] or challenges in modeling changing individual- and neighborhood-level SES over time [11, 15]. Family and work social contexts also contain important factors related to health behavior and, in particular, smoking. For example, currently married individuals and higher income earners are less likely to smoke [16]. Multiple studies have also shown that exposure to family members or coworkers who smoke are key social context factors that increase risk for smoking [4, 17, 18]. Therefore, when examining risks connected to family or work, consideration of the smoking-specific social context is important.
The first goal of this study was to examine associations between multiple indicators of individual- and neighborhood-level SES, demographics, and cigarette smoking in a community sample of adults from age 30 to 39. National estimates have reported that smoking prevalence peaks among adults aged 26–34 and declines as individuals age [16]. As such, we sought to examine associations of SES and demographics with smoking during a period when we expect reductions in smoking. While indicators of SES such as education and income have well-established relationships with smoking, it remains unclear if neighborhood-level SES is independently associated with smoking after accounting for individual-level SES. The second goal of these analyses was to extend our initial model for SES and demographics to include proximal risk factors for smoking. Conceptual models linking SES and health behavior have suggested that proximal work and family social contexts and individual-level psychological factors such as depression and anxiety may operate as mechanisms connecting neighborhood-level SES and health behavior. Specifically, we sought to examine if associations between neighborhood-level SES and smoking changed upon inclusion of proximal risk factors.
Method
Participants
Data came from the Seattle Social Development Project (SSDP), a longitudinal, theory-driven study originating in 18 Seattle elementary schools over-representing high crime neighborhoods. SSDP conducted in-person interviews in 1985 with 808 students in the fifth grade when students were approximately 10 years old (M = 10.3, SD = 0.52). Of the 1,053 fifth-grade students invited into the study, 77% of the parents consented to participation. Since 1985, 15 waves of data have been collected with annual or bi-annual assessments for youth until 1993 and assessments approximately every 3–5 years for adults from 1996 to 2014. The history of the SSDP sample has been described elsewhere [19]. The analytic sample employed three waves of data gathered prospectively in 2005, 2008, and 2014 (N = 752) when both home address and cigarette smoking information were available for adult participants.
Measures
Cigarette smoking
At each wave, participants responded to one question describing their past month cigarette smoking with response options of none, less than one cigarette per day, one to five cigarettes per day, about a half a pack of cigarettes per day, and about a pack of cigarettes per day. Items were recoded as 0 = no past month smoking, 1 = 5 or less cigarettes per day, 2 = about half a pack of cigarettes or more per day.
Neighborhood poverty
Participant home addresses were geocoded and linked with census block group data from the American Community Survey (ACS). Census block groups, containing approximately 2,000–3,000 residents, are commonly employed as measures of neighborhood environment [20]. The ACS began publishing 5-year averages at the census block group level in 2010 and updates those averages annually. Participant addresses from 2005 and 2008 were linked with ACS 5-year averages from 2005 to 2010 and addresses from 2014 were linked with ACS 5-year averages from 2010 to 2014. Principal components analysis (PCA) was used to summarize four ACS variables at each year: the percent of individuals in the work force and unemployed, percent receiving public assistance, percent below the poverty line, and percent with less than a high school education. Results of the PCA are reported in Table 2.
Table 2.
Principal components analysis for census block group measures
| Variable | Neighborhood poverty | M | SD | Max | ||
|---|---|---|---|---|---|---|
| Age 30 | Age 33 | Age 39 | ||||
| Percent of individuals below the poverty line | 0.80 | 0.82 | 0.83 | 0.12 | 0.08 | 0.49 |
| Percent of individuals receiving public assistance income | 0.71 | 0.78 | 0.69 | 0.04 | 0.03 | 0.18 |
| Percent of adults without a high school diploma | 0.76 | 0.69 | 0.78 | 0.12 | 0.08 | 0.65 |
| Percent of individuals in the workforce and unemployed | 0.56 | 0.76 | 0.64 | 0.08 | 0.04 | 0.29 |
| Eigenvalue | 2.03 | 2.33 | 2.18 | |||
| Percent of Variance | 0.51 | 0.58 | 0.55 | |||
Note. M mean; SD standard deviation, M, SD, and Max are averaged across ages; average participants per block group ranged from 1.2 to 1.3 across ages.
Most coworkers smoke
At each wave, participants responded to one question describing how many of their coworkers smoke cigarettes with response options of none, some, most, and all. Items were coded as 1 to indicate that most or all coworkers who smoke and 0 to indicate that none or some coworkers smoke. Those reporting no formal employment skipped this question. At age 39, 70% (81 out of 116) of those reporting no formal employment also reported being a full-time homemaker or stay at home parent in the past year.
Partner smokes regularly
At each wave, participants responded to one yes or no question if their partner smoked cigarettes regularly. Those not reporting a current partner skipped this question.
Depression and anxiety
Probable diagnoses of major depressive episode (MDE) and generalized anxiety disorder (GAD) were assessed using a modified version of the Diagnostic Interview Schedule [21] completed by self-report at each wave. Fifteen diagnostic symptoms defined by the DSM-IV [22] were assessed. MDE was indicated by endorsement of at least five out of nine of the following symptoms for at least 2 weeks in the past year: changes in weight or appetite, sleep difficulties, moving or talking slowly, fatigue, difficulty concentrating or making decisions, guilt or worthlessness, and thoughts of suicide or death. GAD was indicated by endorsement of at least two out of six symptoms related to problems with irritability, recurrent worrying, and distractibility disrupting daily life for at least 2 weeks in the past year. Diagnoses of MDE and GAD based on the DIS have been uniquely associated with smoking in community samples [23].
SES and demographic factors
College degree was coded as 1 for attaining a 4-year college degree or higher and 0 for all others. For current marital status, 1 indicated married or currently living with a partner and 0 indicated not married or living with a partner. A six-category measure of household income was broken into $20,000 increments. Parenthood was indicated by self-reports of acting as a current biological or adoptive parent and coded with parenthood equal to 1. Education, income, marital status, and parenthood were assessed at each wave while gender and race/ethnicity remained static across waves.
Analytic Strategy
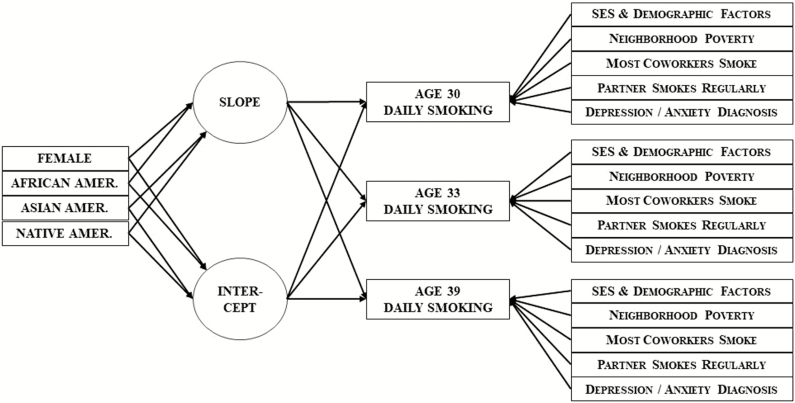
Latent growth curve modeling has been effectively used to estimate changes in substance using behavior over time while also allowing for individual differences in initial levels, rates of change over time, and deviation from average levels at each time point [24]. Deviation from average levels of smoking can be examined by estimating the growth curve and regressing the indicators that define the intercept and slope parameters of the curve on time-varying predictors [25]. Figure 1 presents a conceptual diagram of this strategy for an ordered logistic latent growth curve of smoking including both time-fixed and time-varying covariates. As expected, an initial unconditional growth model showed a significant negative slope for smoking and significant variance in both the intercept and slope for smoking across participants. Model 1 estimated the trajectory of smoking from age 30 to 39, included time-fixed covariates for gender and ethnicity, and included time-varying measures of educational attainment, marital status, household income, parenthood, and neighborhood poverty predicting the time-varying measure of smoking. Model 2 included coworker smoking, partner smoking, and diagnoses of depression and anxiety as time-varying predictors of smoking. Both models constrained the association of time-varying covariates with smoking to estimate their average association over time. Constrained models showed improved fit as indicated by a reduction in five or more in the sample-size adjusted bayesian information criterion (BIC) as compared to unconstrained models [24, 26]. Missing data were handled via multiple imputation [27] and data were present for 92% of possible data points (22,039 out of 24,064) across 32 variables in the analytic sample. Forty datasets were created and subsequently analyzed using the multiple imputation and latent growth modeling procedures in Mplus version 8.1 [28]. Model results employed the maximum likelihood estimator and are averaged across 40 datasets. Examination of the proportional odds assumption for ordered logistic regression showed similar magnitude and direction of coefficients across thresholds of smoking. Some SSDP participants received a social development intervention during elementary school [19]. Sensitivity tests controlling for intervention condition did not show substantive changes to the results of Model 2.
Fig. 1.
Path diagram for latent growth curve of daily smoking with time-varying measures of socioeconomic status (education and income), demographic factors (marriage and parenthood), neighborhood poverty, coworker smoking, partner smoking, and diagnoses of depression or anxiety.
Results
Table 1 provides descriptive statistics, Table 2 reports the results of the PCA for neighborhood poverty, and Table 3 reports the results of latent growth curves. Coefficients for ordinal regression can be interpreted such that a one unit increase in the predictor is associated with an increase in the ordered log odds of smoking at one higher level. The results of Model 1 indicated that having a college degree and being currently married were uniquely associated with reduced smoking after controlling for average growth in smoking from age 30 to 39, gender, and race/ethnicity. Living in a higher poverty neighborhood was uniquely associated with increased smoking. No differences were noted by household income or parenthood. Model 1 showed significant residual variance on the latent intercept and slope of the growth curve warranting inclusion of additional time-varying covariates to account for the residual variance.
Table 1.
Analytic sample descriptive statistics
| Age 30 | Age 33 | Age 39 | ||||||
|---|---|---|---|---|---|---|---|---|
| Min | Max | M | SD | M | SD | M | SD | |
| Past Month Smoking | 0 | 2 | 0.47 | 0.74 | 0.45 | 0.77 | 0.38 | 0.73 |
| No smoking | 68% | 72% | 76% | |||||
| Five or less cigarettes/day | 17% | 11% | 9% | |||||
| About half a pack or more/day | 15% | 17% | 15% | |||||
| College Degree | 0 | 1 | 26% | 28% | 30% | |||
| Married | 0 | 1 | 57% | 62% | 67% | |||
| Household Incomea | 1 | 6 | 3.17 | 1.60 | 3.70 | 1.68 | 3.74 | 1.84 |
| Parenthood | 0 | 1 | 60% | 69% | 81% | |||
| Neighborhood Poverty | −1.61 | 7.38 | 0 | 1 | 0 | 1 | 0 | 1 |
| Most Coworkers Smoke | 0 | 1 | 19% | 16% | 10% | |||
| Partner Smokes Regularly | 0 | 1 | 25% | 26% | 19% | |||
| Major Depressive Episode | 0 | 1 | 12% | 10% | 11% | |||
| Generalized Anxiety Disorder | 0 | 1 | 6% | 6% | 11% | |||
| Female | 0 | 1 | 49% | - | - | |||
| African American | 0 | 1 | 25% | - | - | |||
| Asian American | 0 | 1 | 21% | - | - | |||
| Native American | 0 | 1 | 5% | - | - | |||
| European American | 0 | 1 | 49% | - | - | |||
Note. N = 752, M mean; SD standard deviation.
a1 = less than $20,000, 6 = greater than $100,000 household income.
Table 3.
Results of latent growth curves for cigarette smoking from age 30 to 39
| Independent variable | Dependent variable | Model 1 | Model 2 |
|---|---|---|---|
| Time-varying Covariates | Est. (SE) | Est. (SE) | |
| College Degreea | Smoking | −4.16 (0.66)*** | −3.58 (0.60)*** |
| Marrieda | Smoking | −0.65 (0.29)* | −0.94 (0.29)** |
| Household Incomeb | Smoking | −0.15 (0.16) | −0.09 (0.15) |
| Parenthooda | Smoking | −0.46 (0.41) | −0.29 (0.38) |
| Neighborhood Povertyb | Smoking | 0.37 (0.13)** | 0.35 (0.13)** |
| Most Coworkers Smokea | Smoking | 0.73(0.30)* | |
| Partner Smokes Regularlya | Smoking | 1.63 (0.28)*** | |
| Major Depressive Episodea | Smoking | 0.82 (0.37)* | |
| Generalized Anxiety Disordera | Smoking | −0.06 (0.44) | |
| Time-fixed Covariates | |||
| Female | Intercept | −0.90 (0.51) | −1.00 (0.47)* |
| Slope | −0.07 (0.06) | −0.04 (0.06) | |
| African American | Intercept | −0.66 (0.61) | −0.91 (0.57) |
| Slope | −0.05 (0.07) | −0.04 (0.06) | |
| Asian American | Intercept | −0.51 (0.67) | −0.41 (0.61) |
| Slope | −0.08 (0.08) | −0.06 (0.07) | |
| Native American | Intercept | 1.00 (1.01) | 0.59 (0.93) |
| Slope | 0.14 (0.11) | 0.13 (0.10) | |
| Intercept and Slope | |||
| Smoking | Intercept | 0.00 (0.00) | 0.00 (0.00) |
| Slope | −0.09 (0.06) | −0.07 (0.06) | |
| Residual Variance | Intercept | 23.29 (5.28)*** | 18.25 (4.18)*** |
| Slope | 0.09 (0.04)* | 0.06 (0.03) | |
| BICc | 2,594 (2,608) | 2,549 (2,556) | |
Note. N = 752. Est. unstandardized estimate; SE standard error; all estimates are constrained to be equal from age 30 to 39, race/ethnicity variables are compared to European Americans.
aCoded as 0 | 1 with 1 indicating the variable name.
bStandardized with mean = 0 and SD = 1 prior to analysis.
cBIC in parentheses indicates fit with time-varying predictors unconstrained over time.
*p < .05, **p < .01, ***p < .001.
The substantive interpretation of coefficients for time-varying covariates in Model 1 remained consistent in Model 2 with the inclusion of proximal risk factors for smoking. Having a college degree (odds ratio [OR]: 0.03, 95% confidence interval [CI]: 0.01–0.05) and being married (OR: 0.39, 95% CI: 0.29–0.52) remained associated with reduced smoking while living in a higher poverty neighborhood remained associated with increased smoking (OR: 1.41, 95% CI: 1.24–1.61). Work environments characterized by coworker smoking (OR: 2.07, 95% CI: 1.54–2.80), having a partner who smokes regularly (OR: 5.10, 95% CI: 3.86–6.75), and a diagnosis of depression (OR: 2.37, 95% CI: 1.57–3.28) were uniquely associated with increased smoking net of growth in smoking from age 30 to 39 and differences by SES and demographics. The inclusion of proximal risk factors for smoking in Model 2 accounted for about 33% of the remaining variance in the slope parameter and rendered the residual variance of the slope parameter nonsignificant. Significant variance on the latent intercept persisted across models.
Discussion
Results of this study highlight neighborhood poverty as a unique risk factor for increased smoking from age 30 to 39 above and beyond other indicators of SES, demographic factors, smoking-specific work and family contexts, and diagnoses of depression and anxiety disorder. As expected, currently being married and having a college degree were independently associated with lower risk for smoking [2], while work environments characterized by coworker smoking, having a partner that smokes regularly, and depression were associated with increased risk of smoking [4, 6, 23]. Importantly, the inclusion of the proximal risk factors of coworker smoking, partner smoking, depression, and anxiety, which have been suggested as mechanisms linking neighborhood poverty to health behavior, did not account for the association between neighborhood poverty and smoking. Further research is needed to identify specific mechanisms uniquely connecting neighborhood poverty with increased smoking risk. This association in the SSDP sample may reflect greater exposure to tobacco retail shops and advertising as suggested by other studies [8].
Some limitations of the current study should be noted. First, our model was unable to fully explain residual variance in the intercept of the growth curve. This unexplained variance may reflect a long-standing nicotine addiction or other unmeasured factors contributing to smoking. Second, we did not include time-varying measures of alcohol use, peer smoking, or the percent of neighborhood residents who smoke cigarettes. It is possible that alcohol use and smoking are jointly associated with neighborhood poverty and/or reciprocally associated with one another over time [14]. Smoking-specific peer and neighborhood contexts were not available for the SSDP sample, but may also confer unmeasured risks for smoking. Third, it is important to consider that unemployed individuals, who would not report smoking coworkers in this study, are likely exposed to or experiencing additional risk factors for smoking [2]. Re-estimation of Model 2 removing unemployed participants from the analytic sample produced substantively identical results to those reported in Table 3. Further research should explicitly examine differences in social contexts associated with smoking across employment status.
The study has important strengths that contribute to the growing literature examining tobacco-related health disparities and low SES as a multifaceted risk factor for smoking. Time-varying measures of SES may improve our ability to detect associations with smoking and other health behaviors. Future studies should examine associations between changes in neighborhood living conditions and changes in smoking over time. For instance, individuals moving from higher to lower poverty areas may demonstrate different patterns of smoking when living in new neighborhoods. Similarly, changing neighborhood SES over time may be associated with different patterns of smoking among stationary residents.
Funding
Research reported in this publication was supported by the National Institute of Health through the National Institute on Drug Abuse under award number R01DA003721 and R01DA033956 and through the National Cancer Institute under award number F32CA232796. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Compliance with Ethical Standards
Conflicts of Interest The authors have no conflicts of interest to report.
Authors’ Contributions C. Cambron formulated the research questions, designed the study, analyzed the data and wrote the article. R. Kosterman reviewed the article and is the principal investigator on R01DA033956. J. D. Hawkins is the principal investigator on R01DA003721.
Ethical Approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the University of Washington and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1. Xu X, Bishop EE, Kennedy SM, Simpson SA, Pechacek TF.. Annual healthcare spending attributable to cigarette smoking: An update. Am J Prev Med. 2015;48:326–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hiscock R, Bauld L, Amos A, Fidler JA, Munafò M.. Socioeconomic status and smoking: A review. Ann N Y Acad Sci. 2012;1248:107–123. [DOI] [PubMed] [Google Scholar]
- 3. USDHHS: The Health Consequences of Smoking-50 Years of Progress. A Report of the Surgeon General. Atlanta, CA: US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 4. Fagan P, Moolchan ET, Lawrence D, Fernander A, Ponder PK.. Identifying health disparities across the tobacco continuum. Addiction. 2007;102(suppl 2):5–29. [DOI] [PubMed] [Google Scholar]
- 5. Fisher EB. The importance of context in understanding behavior and promoting health. Ann Behav Med. 2008;35:3–18. [DOI] [PubMed] [Google Scholar]
- 6. Businelle MS, Kendzor DE, Reitzel LR, et al. . Mechanisms linking socioeconomic status to smoking cessation: A structural equation modeling approach. Health Psychol. 2010;29:262–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gallo LC, Matthews KA.. Understanding the association between socioeconomic status and physical health: Do negative emotions play a role?Psychol Bull. 2003;129:10–51. [DOI] [PubMed] [Google Scholar]
- 8. Henriksen L, Schleicher NC, Feighery EC, Fortmann SP.. A longitudinal study of exposure to retail cigarette advertising and smoking initiation. Pediatrics. 2010;126:232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Braveman PA, Cubbin C, Egerter S, et al. . Socioeconomic status in health research: One size does not fit all. JAMA. 2005;294:2879–2888. [DOI] [PubMed] [Google Scholar]
- 10. Diez Roux AV, Mair C.. Neighborhoods and health. Ann N Y Acad Sci. 2010;1186:125–145. [DOI] [PubMed] [Google Scholar]
- 11. Wodtke GT, Harding DJ, Elwert F.. Neighborhood effects in temporal perspective. Am Sociol Rev. 2011;76:713–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bronfenbrenner U: Toward an experimental ecology of human development. Am Psychol. 1977, 32:513. [Google Scholar]
- 13. Adler NE, Newman K.. Socioeconomic disparities in health: Pathways and policies. Health Aff (Millwood). 2002;21:60–76. [DOI] [PubMed] [Google Scholar]
- 14. Karriker-Jaffe KJ. Areas of disadvantage: A systematic review of effects of area-level socioeconomic status on substance use outcomes. Drug Alcohol Rev. 2011;30:84–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kravitz-Wirtz N. A discrete-time analysis of the effects of more prolonged exposure to neighborhood poverty on the risk of smoking initiation by age 25. Soc Sci Med. 2016;148:79–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Garrett BE, Dube SR, Trosclair A, Caraballo RS, Pechacek TF; Centers for Disease Control and Prevention (CDC) Cigarette smoking - United States, 1965-2008. MMWR Suppl. 2011;60:109–113. [PubMed] [Google Scholar]
- 17. Hemsing N, Greaves L, O’Leary R, Chan K, Okoli C.. Partner support for smoking cessation during pregnancy: A systematic review. Nicotine Tob Res. 2012;14:767–776. [DOI] [PubMed] [Google Scholar]
- 18. Bailey JA, Hill KG, Meacham MC, Young SE, Hawkins JD.. Strategies for characterizing complex phenotypes and environments: General and specific family environmental predictors of young adult tobacco dependence, alcohol use disorder, and co-occurring problems. Drug Alcohol Depend. 2011;118:444–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Hill KG, Woodward D, Woelfel T, Hawkins JD, Green S.. Planning for long-term follow-up: Strategies learned from longitudinal studies. Prev Sci. 2016;17:806–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Elliott DS, Menard S, Rankin B, et al. . Good Kids from Bad Neighborhoods: Successful Development in Social Context. New York, NY: Cambridge University Press; 2006. [Google Scholar]
- 21. Robins LN, Helzer JE, Croughan J, Williams JB, Spitzer RL: NIMH Diagnostic Interview Schedule: Version III. Rockville, MD: National Institute of Mental Health; 1981. [DOI] [PubMed] [Google Scholar]
- 22. American Psychological Association: Diagnostic and Statistical Manual of Mental Disorders (DSM-IV). Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 23. Covey LS, Hughes DC, Glassman AH, Blazer DG, George LK: Ever-smoking, quitting, and psychiatric disorders: Evidence from the Durham, North Carolina, epidemiologic catchment area. Tob Control. 1994, 3:222. [Google Scholar]
- 24. Curran PJ, Hussong AM.. The use of latent trajectory models in psychopathology research. J Abnorm Psychol. 2003;112:526–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hussong AM, Curran PJ, Moffitt TE, Caspi A, Carrig MM.. Substance abuse hinders desistance in young adults’ antisocial behavior. Dev Psychopathol. 2004;16:1029–1046. [DOI] [PubMed] [Google Scholar]
- 26. Singer JD, Willett JB.. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York, NY: Oxford university press; 2003. [Google Scholar]
- 27. Graham JW. Missing data analysis: Making it work in the real world. Annu Rev Psychol. 2009;60:549–576. [DOI] [PubMed] [Google Scholar]
- 28. Muthen L, Muthen B: Mplus User’s Guide. 8th ed. Los Angeles, CA: Muthen & Muthen; 2017. [Google Scholar]