Abstract
BACKGROUND:
In the 2014 PROtective Ventilation using High versus LOw positive end-expiratory pressure (PROVHILO) trial, intraoperative low tidal volume ventilation with high positive end-expiratory pressure (PEEP = 12 cm H2O) and lung recruitment maneuvers did not decrease postoperative pulmonary complications when compared to low PEEP (0–2 cm H2O) approach without recruitment breaths. However, effects of intraoperative PEEP on lung compliance remain poorly understood. We hypothesized that higher PEEP leads to a dominance of intratidal overdistension, whereas lower PEEP results in intratidal recruitment/derecruitment (R/D). To test our hypothesis, we used the volume-dependent elastance index %E2, a respiratory parameter that allows for noninvasive and radiation-free assessment of dominant overdistension and intratidal R/D. We compared the incidence of intratidal R/D, linear expansion, and overdistension by means of %E2 in a subset of the PROVHILO cohort.
METHODS:
In 36 patients from 2 participating centers of the PROVHILO trial, we calculated respiratory system elastance (E), resistance (R), and %E2, a surrogate parameter for intratidal overdistension (%E2 > 30%) and R/D (%E2 < 0%). To test the main hypothesis, we compared the incidence of intratidal overdistension (primary end point) and R/D in higher and lower PEEP groups, as measured by %E2.
RESULTS:
E was increased in the lower compared to higher PEEP group (18.6 [16...22] vs 13.4 [11.0…17.0] cm H2O-L−1; P < .01). %E2 was reduced in the lower PEEP group compared to higher PEEP (−15.4 [−28.0.6.5] vs 6.2 [−0.8.14.0] %; P < .05). Intratidal R/D was increased in the lower PEEP group (61% vs 22%; P = .037). The incidence of intratidal overdistension did not differ significantly between groups (6%).
CONCLUSIONS:
During mechanical ventilation with protective tidal volumes in patients undergoing open abdominal surgery, lung recruitment followed by PEEP of 12 cm H2O decreased the incidence of intratidal R/D and did not worsen overdistension, when compared to PEEP ≤2 cm H2O.
Mechanically ventilated patients are at risk for ventilator-induced lung injury.1,2 The use of small tidal volumes (VT) to avoid volutrauma and positive end-expiratory pressure (PEEP) to avoid atelectrauma are commonly accepted strategies to minimize ventilator-induced lung injury. In anesthetized patients without lung injury, low tidal volumes (VT = 6–8 mL∙kg−1 predicted body weight [PBW]) may reduce postoperative pulmonary complications (PPCs).3–5 However, the effect of intraoperative PEEP level on lung mechanics or outcome is incompletely understood.6,7
A 2014 multicenter trial on intraoperative mechanical ventilation, the PROtective Ventilation using High versus LOw PEEP (PROVHILO) trial,8,9 compared ventilation with high PEEP (12 cm H2O) with recruitment maneuvers (RMs) with low PEEP (2 cm H2O) without RM. PROVHILO found no difference in PPCs between high and low PEEP groups, although high PEEP increased intraoperative hemodynamic instability. Because low PEEP may increase intratidal recruitment/dere-cruitment (R/D), and high PEEP may increase overdistension of the lung, the effects of PEEP on respiratory system mechanics during intraoperative ventilation remain unclear.
Overdistension and intratidal R/D can be identified using computed tomography of the lung at end-inspiration and end-expiration. However, this approach is limited by exposure to ionizing radiation and prohibitive labor costs of image processing.10 An alternative method involves using airway pressure and flow waveforms obtained at the tracheal tube to derive nonlinear respiratory system mechanical parameters. In particular, the volume-dependent elastance index %E2 can quantify the nonlinearity of the lung pressure-volume curve during inspiration.11,12 Negative values of %E2 indicate decreasing lung stiffness during inflation and suggest lung recruitment, whereas large positive values of %E2 indicate increasing lung stiffness during inflation and imply overdistension.
The aim of this study was to investigate the effect of low and high PEEP on intratidal R/D and overdistension, as measured by the volume-dependent elastance index %E2 in a subgroup of the PROVHILO trial. We hypothesized that overdistension occurred more frequently in patients ventilated with the higher PEEP strategy, whereas intratidal R/D occurred more frequently in patients ventilated with the lower PEEP strategy.
METHODS
Design
This was a substudy of the prospective, double-blind, randomized controlled PROVHILO trial8 (registered at controlled-trials.gov as ISRCTN70332574), which included 900 patients. This substudy was conducted in 2 centers: the University Hospital Azienda Ospedaliero Universitaria–Ospedali Riuniti of Foggia, Italy, and the Massachusetts General Hospital in Boston, Massachusetts. Corresponding local ethics committees (119/CE/2011 and IRB: 2012P000062) approved the study protocol, and written informed consent for participation in PROVHILO study was obtained from each patient or their designated surrogate before enrollment. The primary end point was the percentage of volume-dependent elastance of the respiratory system, %E2, which was defined as the ratio of volume-dependent elastance to total elastance at end-inspiration.13 The secondary end point of the study was the resistance of the respiratory system (R).
Inclusion and exclusion criteria, randomization, intervention, and procedures were as previously described in the PROVHILO trial.8 Briefly, patients were considered eligible for participation if they met the following inclusion criteria: elective open abdominal surgery under general anesthesia, age >18 years, high or intermediate risk for PPCs following nonlaparoscopic abdominal surgery with general anesthesia according to the Assess Respiratory Risk in Surgical Patients in Catalonia (ARISCAT) risk score ;≥26.14,15 Exclusion criteria were body mass index >40 kg-m−2, pregnancy, consent for another interventional study, mechanical ventilation lasting longer than 30 minutes within last 30 days, severe cardiopulmonary comorbidities or other disorders that might compromise patient safety, or enrollment in another interventional study.
Patients were randomly allocated to receive intraoperative ventilation using either high PEEP (12 cm H2O) with RM (higher PEEP group) or low PEEP (≤2 cm H2O) without RM (lower PEEP group). Local investigators randomly allocated patients after enrollment, using a secure, central, Web-based system, according to the PROVHILO study protocol.16
In this substudy, data collected independently in 2 of the 30 PROVHILO centers were merged. The study procedure did not differ between centers and is summarized below.
Procedure
Anesthesia and postoperative care followed local standards in the respective centers. Intraoperative mechanical ventilation was performed as per the PROVHILO protocol.8 Briefly, all patients were ventilated in constant flow, volume-controlled mode. I:E ratio was set at 1:2, respiratory rate (RR) was titrated to achieve end-tidal carbon dioxide partial pressure of 35 to 45 mm Hg, inspiratory oxygen fraction adjusted to maintain the peripheric oxygen saturation >92%, and VT targeted to <8 mL∙kg−1 PBW.8 Patients were randomly allocated to the PEEP groups using a secure, central, web-based randomization system.16 In the higher PEEP group, RMs were performed (1) immediately after intubation; (2) after any disconnection from the mechanical ventilator; and (3) directly before tracheal extubation. RMs were conducted according to the following procedure: (1) setting PEEP = 12 cm H2O; reducing of RR to 6 to 8 minute−1, or lowest the ventilator allowed; (2) increasing in VT steps of 4 mL∙kg−1 PBW until a target plateau pressure of 30 to 35 cm H2O was reached; (3) administering 3 breaths with plateau pressure 30 to 35 cm H2O; and (4) returning RR and VT to values preceding the RM. In the lower PEEP group, RMs were allowed only as a rescue strategy due to hypoxemia, as described elsewhere.16
Measurements
In both centers, only measurements conducted at end of surgery, ie, under deep anesthesia and before reversal of muscle paralysis during the last 1 hour preceding extubation, were considered for analysis.
At the Foggia Center.
Airway flow () was measured with a heated pneumotachograph (Fleisch No. 2; Fleisch, Lausanne, Switzerland), connected to a differential pressure transducer (Diff-Cap; Special Instruments, Nördlingen, Germany) inserted between the Y-piece of the ventilator circuit and the endotracheal tube. Airway opening pressure (Paw) was measured proximal to the endotracheal tube with a pressure transducer (Digima-Clic ±100 cm H2O; Special Instruments). The transduced airway flow and pressure signals were sampled using a 12-bit analog-to-digital converter (DAQCard 700; National Instrument, Austin, TX) at a rate of 200 Hz (ICU Lab, KleisTEK Engineering, Bari, Italy).
At the Boston Center.
The and PAW signals were recorded with a combined sensor placed between the endotracheal tube and the respiratory circuit at a sampling rate of 100 Hz (NICO Monitor; Respironics Inc, Murrysville, PA).
Respiratory System Mechanics
Airway flow () and pressure (Paw) recordings demonstrating noticeable nonlinear artifacts that could not be compensated for, or otherwise corrected (eg, patient efforts, flow limitation, distortion from movement during surgical operation), were excluded from analysis.
Respiratory system mechanics were calculated identically for both study centers. Following respiratory cycle detection and identification (semiautomatically, based on flow and volume thresholds followed by manual correction), VT, mean airway pressure meanPaw, and peak airway pressure peakPaw were calculated. Respiratory mechanical parameters were derived by fitting the equation of motion (Equation 1) to the corresponding sampled flow signal and pressure signal Paw(t) for each respiratory cycle using a multiple linear regression technique. Volume-independent (E1), volume-dependent (E2), total elastance (E), resistance (R) of the respiratory system, and the end-expiratory pressure (P0) were estimated according to Equation 113:
| (1) |
whereby E was calculated according to Equation 2:
| (2) |
and %E2 was calculated as shown in Equation 313:
| (3) |
E2 represents, thus, the deviation from a linear relationship between volume and elastance, which can be due to increase (overdistension) or decrease (recruitment) of elastance with volume. Negative values of %E2 indicate concavity of the elastic airway pressure (Pel) versus volume curve and suggest intra-tidal R/D.11,13,17,18 A positive %E2 indicates a convex Pel-V curve, and values >30% suggested intratidal overdistension12,13 (Figure 1).
Figure 1.
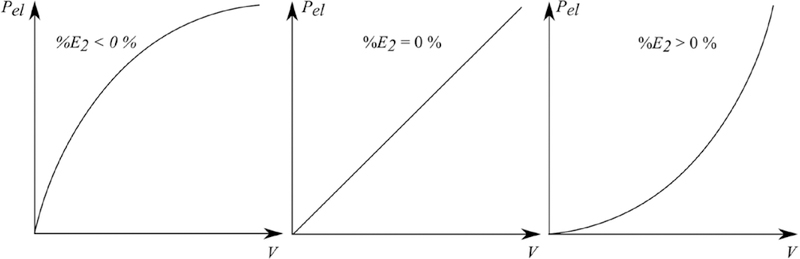
Qualitative elastic airway pressure (Pel) versus volume (V) curves and corresponding percentage of volume-dependent respiratory system elastance (%E2) values.
Current literature indicates that %E2 values between 0% and 30% correspond to linear expansion of the lung with increasing elastic pressure. In this range of %E2, changes in elastance due to intratidal recruitment and overdistension may be either equal and opposite, or both minimal.11–13,17,18 In a comparison between respiratory mechanics analysis and computer tomography (CT)-based measurement in healthy pigs, %E2 = 20% corresponded to overdistension in approximately 35% of total lung volume and 0% intratidal R/D, whereas %E2 = −26% corresponded to 9% total lung volume overdistension and 4% intratidal R/D.11
Statistical Analysis
Data are presented as mean ± standard deviation (SD) or as median (interquartile range), as appropriate. Between-group comparison for parameters measured at the end of surgery was performed using an unpaired nonparametric Wilcoxon-Mann-Whitney test. The incidence of overdistension, linear expansion, and intratidal R/D between both PEEP strategy groups were compared using the Fisher exact test (confidence interval 95%, 2000 Monte Carlo simulations) on a 2 × 2 contingence table, since incidence of over-distension was identical in both groups.
No formal sample size calculation was performed for this substudy. The number of patients included (N = 36) would provide approximately 80% power to detect a significant difference (α = .05, 2-tailed, Z test of proportions) between expected incidences of overdistension of 60% in the higher and 15% in the lower PEEP group. These values correspond to the lower and higher boundaries in the higher PEEP and the lower PEEP group, respectively. Accordingly, the lowest but still clinically relevant difference in incidence of over-distension we would have expected between groups was 45%.
P ≤ .05 was considered statistically significant. Sample size calculation was conducted with G*Power software (version 3.1.9.2).19 All other statistical analyses were performed using the R Statistical programming language.20
RESULTS
Study Population
The CONSORT diagram for this substudy is shown in Figure 2. Data from 36 patients were included in this sub-study (18 patients per group). Patient, surgery, and anesthesia characteristics did not differ between PEEP groups (Table 1).
Figure 2.
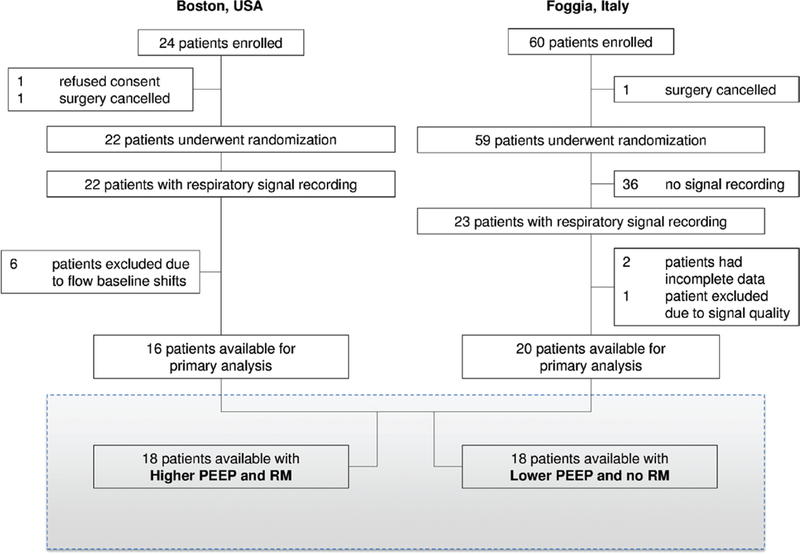
CONSORT diagram of the substudy. PEEP indicates positive end-expiratory pressure; RM, recruitment maneuver.
Table 1.
patient Characteristics
| Lower PEEP, N = 18 |
Higher PEEP, N = 18 |
P | |
|---|---|---|---|
| Age (y) | 65 (61–74) | 68.5 (63–72) | .987 |
| Female, N [%] | 5 [28] | 6 [33] | .804 |
| Body weight (kg) | 75 (65–86) | 77 (64–84) | .8 |
| Height (cm) | 168 (160–170) | 168 (170–180) | .751 |
| BMI (kg∙m−2) | 26.3 (24–30) | 26.2 (23–28) | .613 |
| PBW (kg∙m−2) | 63.5 (57–70) | 63.5 (57–71) | .787 |
| ARISCAT risk score | 41 (34–44) | 41.5 (34–44) | .772 |
| ASA score, N [%] | |||
| ASA I | 1 [6] | 0 [0] | 0 |
| ASA II | 12 [67] | 12 [67] | 1 |
| ASA III | 5 [28] | 6 [33] | .804 |
| ASA IV | 0 [0] | 0 [0] | 1 |
| ASA V | 0 [0] | 0 [0] | 1 |
| Type of surgery | |||
| Bladder | 1 [6] | 0 [0] | 0 |
| Colonic | 7 [39] | 9 [50] | .481 |
| Gastric | 1 [6] | 2 [11] | .713 |
| Pancreatic | 3 [17] | 1 [6] | .075 |
| Other | 6 [33] | 6 [33] | 1 |
| Duration of anesthesia (min) | 210 (180–290) | 188 (120–230) | .168 |
| Duration of surgical procedure (min) | 182 (150–240) | 152 (96–210) | .159 |
Values are median (first–third quartile) or absolute number [relative number in %]. Significance between groups was assessed by means of nonparametric, unpaired Wilcoxon test.
Abbreviations: ARISCAT, Assess Respiratory Risk in Surgical Patients in Catalonia; ASA, American Society of Anesthesiologists; BMI, body mass index; PBW, predicted body weight; PEEP positive end-expiratory pressure.
At end of surgery, Spo2 and hemodynamics did not differ between groups, while end-tidal carbon dioxide partial pressure was higher in higher PEEP (Supplemental Digital Content 1, Table 1, http://links.lww.com/AA/B799). The incidences of PPCs and intraoperative cardiocirculatory complications for both groups are shown in Supplemental Digital Content 2, Table 2, http://links.lww.com/AA/B800.
Respiratory Mechanics and Indices of Overdistension and Intratidal R/D
VT, RR, and minute ventilation did not differ between groups. Values for P0, meanPaw, and peakPaw were increased in higher versus lower PEEP groups (Table 2). Both E and R were significantly decreased, while E2 was significantly increased in higher versus lower PEEP groups. As shown in Figure 2, E1 decreased, while %E2 increased in higher versus lower PEEP groups.
Table 2.
Respiratory Variables at End of Surgery
| Variable | Lower PEEP, N = 18 |
Higher PEEP, N = 18 |
P |
|---|---|---|---|
| VT (mL∙kg−1) | 8.10 (6.6 to 9.6) | 7.73 (6.5 to 9.8) | .719 |
| RR (min−1) | 12.00 (10.0 to 12.0) | 12.00 (10.0 to 13.0) | .226 |
| MV (L∙min−1) | 6.59 (5.5 to 8.2) | 6.43 (5.6 to 7.7) | .743 |
| 0.42 (0.4 to 0.5) | 0.43 (0.4 to 0.5) | .963 | |
| meanPaw (cm H2O) | 6.24 (5.8 to 6.8) | 15.80 (15.0 to 16.0) | <.001 |
| peakPaw (cm H2O) | 16.30 (14.0 to 18.0) | 22.80 (22.0 to 24.0) | <.001 |
| ΔPaw, (cm H2O) | 14.50 (12.0 to 17.0) | 10.70 (10.0 to 12.0) | <.001 |
| P0 (cm H2O) | 2.08 (1.4 to 2.4) | 12.10 (12.0 to 12.0) | <.001 |
| E (cm H2O∙L−1) | 18.80 (16.0 to 22.0) | 13.30 (11.0 to 16.0) | .002 |
| E1 (cm H2O∙L−1) | 19.60 (15.0 to 24.0) | 12.60 (11.0 to 15.0) | .001 |
| E2 (cm H2O∙L−2) | −2.49 (−7.0 to 3.5) | 1.17 (0.2 to 4.9) | .047 |
| %E2 (%) | −12.70 (−26.0 to 6.7) | 6.59 (1.0 to 15.0) | .024 |
| R (cm H2O∙s∙L−1) | 8.62 (7.1 to 9.7) | 7.35 (6.2 to 8.4) | .019 |
Values are median (first-third quartile). Group differences were assessed using unpaired nonparametric Wilcoxon test.
Abbreviations: PEEP positive end-expiratory pressure; VT, tidal volume; RR, respiratory rate; MV, minute ventilation; airway flow during inspiration; meanPaw, mean airway pressure; peakPaw, peak airway pressure; ΔPaw, driving pressure; P0, airway pressure at end-expiration; E, respiratory system elastance; E1 volume independent respiratory system elastance; E2, volume-dependent respiratory system elastance; %E2, percentage of volume- dependent respiratory system elastance; R, respiratory system resistance.
Figure 3 shows typical Paw versus time curves, indicating overdistension (%E2 > 30%), linear expansion (0% < %E2 < 30%), and intratidal R/D (%E2 < 0%) in representative patients of the lower PEEP group.
Figure 3.
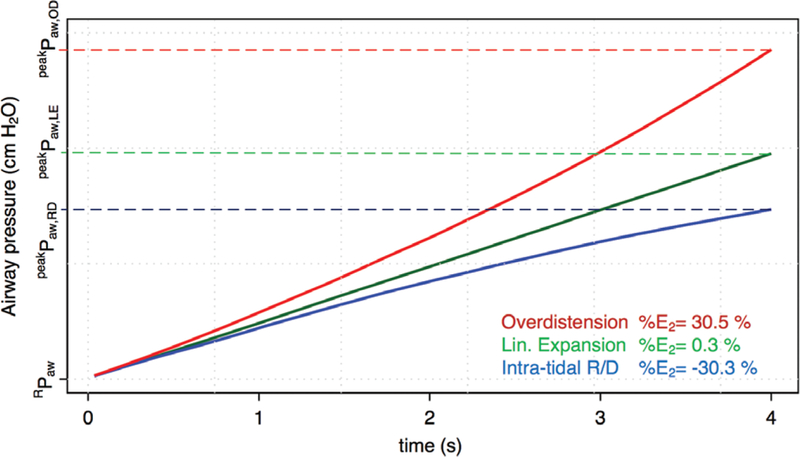
Airway pressure (Paw) versus time curves of 3 representative patients of the low positive end-expiratory pressure group showing the depicted %E2 values. Calculations of the percentage of volume-dependent elastance of the respiratory system (%E2) were performed to detect overdistension (%E2 > 30%), linear expansion (0% < %E2 < 30%), and intratidal recruitment/derecruitment (R/D) (%E2 < 0%); where RPaw denotes airway pressure due to resistance and peakPaw, the respective peak airway pressures in case of overdistension (OD), linear expansion (LE), and intratidal R/D.
Overdistension was observed in only one patient of each group (Figure 4 and Supplemental Digital Content 3, Table 3, http://links.lww.com/AA/B801). Intratidal R/D occurred more frequently in the lower PEEP group (61% vs 22%), whereas linear expansion was more frequent in the higher PEEP group (22% vs 72%; P = .037).
Figure 4.
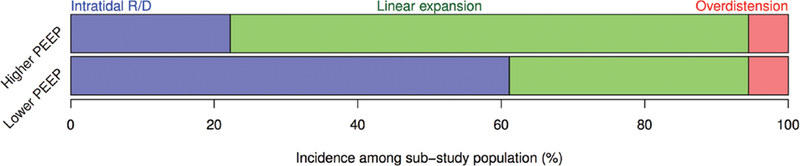
Incidences of overdistension, linear expansion of the respiratory system, and intratidal recruitment/derecruitment (R/D), in lower positive end-expiratory pressure (PEEP) and higher PEEP groups. While incidence of overdistension was not different between groups, incidence of linear expansion and intratidal R/D was significantly different (P = .037, Fisher exact test on a 2 × 2 contingency table).
DISCUSSION
In this substudy of the PROVHILO trial, we found that during mechanical ventilation for open abdominal surgery, a higher PEEP level was associated with (1) decreased E and R, but increased %E2; (2) no difference in incidence of over-distension; and (3) less intratidal R/D.
The present study clarifies the effect of high or low PEEP on lung mechanics during intraoperative mechanical ventilation. Our main findings are that a higher PEEP following lung recruitment does not worsen overdistension and decreases intratidal R/D.
Our results are consistent with prior data. In a 2008 study of healthy patients undergoing maxillofacial surgery, PEEP of 10 cm H2O following lung recruitment was associated with the highest compliance of the respiratory system and lowest dead space, suggesting that this level of PEEP did not lead to significant overdistension.21 Similarly, 2010 study of lung recruitment and PEEP = 10 cm H2O after anesthetic induction found improved respiratory system mechanics without increased dead space.22 In patients undergoing upper abdominal surgery and ventilated with a VT of 7 mL∙kg−1, PEEP of 10 cm H2O effectively maintained lung function and restored functional residual capacity to values prior to induction of anesthesia.23 More recently, in patients undergoing general anesthesia for reconstructive breast surgery, PEEP of 10 cm H2O was associated with %E2 values between 0% and 30%,12 suggesting no overdistension, whereas PEEP of 0 cm H2O resulted in detectable intratidal R/D. In the PROVHILO trial,16 the choice for a PEEP of 12 cm H2O was based on the rationale that a PEEP value slightly >10 cm H2O would be necessary to stabilize the lungs for longer time periods while still limiting overdistension. Our data support this assumption.
Despite the use of low VT, airway pressures were higher in patients ventilated with PEEP of 12 cm H2O. Thus, we cannot rule out that this increased static stress contributed to some degree of parenchymal injury. Recently, the role of static stress in promoting lung inflammation was demonstrated in experimental acute respiratory distress syndrome in pigs with PEEP levels >26 cm H2O.24 Although the specific causes of lung injury remain unclear, static stress in the higher PEEP group could be partly responsible for the observed incidence of PPCs in the PROVHILO study,16 whereas PPCs in the lower PEEP group may be attributed to the large incidence of intratidal R/D. Accordingly, we speculate that a ventilator strategy with high VT (10–12 mL∙kg−1 PBW) and PEEP of 0 cm H2O may promote both intratidal overdistension and R/D, yielding lung injury and increased postoperative complications. Such a hypothesis is supported by recent randomized clinical trials.25,26
LIMITATIONS
Several limitations of this study should be addressed. First, our measurement of respiratory mechanics was conducted in a relatively small subpopulation of the PROVHILO trial, and results cannot be directly extrapolated to the entire cohort of patients. However, our results are consistent with those observed in the original trial cohort. Second, overdistension and intratidal R/D were assessed indirectly and by the surrogate parameter %E2. Theoretically, the use of CT imaging and/or electrical impedance tomography may have been more accurate. However, CT imaging would require patient exposure to ionizing radiation, and neither CT imaging nor electrical impedance tomography can accurately assess intratidal overdistension and R/D with both high spatial and temporal resolution. Third, the comparison of multiple variables was not controlled for type I error at 5%, and we cannot exclude the possibility of false-positive results. Finally, we applied our analysis only to patients undergoing open abdominal surgery, and thus cannot extrapolate our results to other surgical procedures or clinical environments.
Conclusions
During mechanical ventilation with protective VT in patients undergoing open abdominal surgery, lung recruitment followed by PEEP of 12 cm H2O decreased intratidal R/D and did not increase the occurrence of overdistension, when compared to PEEP of ≤ 2 cm H2O.
Supplementary Material
ACKNOWLEDGMENTS
The Academic Medical Center (Amsterdam, the Netherlands) and the European Society of Anaesthesiology provided financial support from PROVHILO trial.
Funding: The PROtective Ventilation using HIgh versus LOw PEEP (PROVHILO) trial was partially funded by the Clinical Trial Network of the European Society of Anaesthesiology. Dr Vidal Melo was funded by the National Heart, Lung, and Blood Institute R34 Grant HL123438 and Dr Kaczka received partial salary support from National Institutes of Health UM1 HL108724.
Footnotes
DISCLOSURES
Name: Davide D’Antini, MD.
Contribution: This author helped collect the data, process the respiratory signals, draft the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: Robert Huhle, MSc.
Contribution: This author helped collect the data, process the respiratory signals, draft the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: Jacob Herrmann, MSc.
Contribution: This author helped collect the data, process the respiratory signals, draft the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: Mr. Herrmann is the cofounder and shareholder of OscillaVent, Inc.
Name: Demet S. Sulemanji, MD.
Contribution: This author helped analyze and interpret the data, revise the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: Jun Oto, MD.
Contribution: This author helped analyze and interpret the data, revise the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: Pasquale Raimondo, MD.
Contribution: This author helped analyze and interpret the data, revise the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: Lucia Mirabella, MD.
Contribution: This author helped analyze and interpret the data, revise the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: Sabrine N. T. Hemmes, MD, PhD.
Contribution: This author helped analyze and interpret the data, revise the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: Marcus J. Schultz, MD, PhD.
Contribution: This author helped conceive and design the work, analyze and interpret the data, draft the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: Paolo Pelosi, MD, FERS.
Contribution: This author helped conceive and design the work, analyze and interpret the data, draft the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: David W. Kaczka, MD, PhD.
Contribution: This author helped conceive and design the work, analyze and interpret the data, draft the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: Dr Kaczka is the cofounder and shareholder of OscillaVent, Inc.
Name: Marcos Francisco Vidal Melo, MD, PhD.
Contribution: This author helped conceive and design the work, analyze and interpret the data, draft the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: Marcelo Gama de Abreu, MD, MSc, PhD, DESA.
Contribution: This author helped conceive and design the work, analyze and interpret the data, draft the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
Name: Gilda Cinnella, MD.
Contribution: This author helped conceive and design the work, analyze and interpret the data, draft the manuscript, approve the manuscript, and is accountable for all aspects of the work.
Conflicts of Interest: None.
This manuscript was handled by: Avery Tung, MD, FCCM.
REFERENCES
- 1.Slutsky AS, Ranieri VM. Ventilator-induced lung injury. N Engl J Med. 2013;369:2126–2136. [DOI] [PubMed] [Google Scholar]
- 2.Sutherasan Y, D’Antini D, Pelosi P. Advances in ventilator-associated lung injury: prevention is the target. Expert Rev Respir Med. 2014;8:233–248. [DOI] [PubMed] [Google Scholar]
- 3.Serpa Neto A, Hemmes SN, Barbas CS, et al. ; PROVE Network investigators. Incidence of mortality and morbidity related to postoperative lung injury in patients who have undergone abdominal or thoracic surgery: a systematic review and meta-analysis. Lancet Respir Med. 2014;2:1007–1015. [DOI] [PubMed] [Google Scholar]
- 4.Serpa Neto A, Hemmes SN, Barbas CS, et al. ; PROVE Network Investigators. Protective versus conventional ventilation for surgery: a systematic review and individual patient data meta-analysis. Anesthesiology. 2015;123:66–78. [DOI] [PubMed] [Google Scholar]
- 5.Cinnella G, Grasso S, Spadaro S, et al. Effects of recruitment maneuver and positive end-expiratory pressure on respiratory mechanics and transpulmonary pressure during laparoscopic surgery. Anesthesiology. 2013;118:114–122. [DOI] [PubMed] [Google Scholar]
- 6.Futier E, Marret E, Jaber S. Perioperative positive pressure ventilation: an integrated approach to improve pulmonary care. Anesthesiology. 2014;121:400–408. [DOI] [PubMed] [Google Scholar]
- 7.Güldner A, Kiss T, Serpa Neto A, et al. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complications: a comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology. 2015;123:692–713. [DOI] [PubMed] [Google Scholar]
- 8.Hemmes SN, Severgnini P, Jaber S, et al. Rationale and study design of PROVHILO—a worldwide multicenter randomized controlled trial on protective ventilation during general anesthesia for open abdominal surgery. Trials. 2011;12:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cinnella G Enrolling patients into multiple trials: it is time for glasnost*. Crit Care Med. 2015;43:485–486. [DOI] [PubMed] [Google Scholar]
- 10.Puybasset L, Cluzel P, Gusman P, Grenier P, Preteux F, Rouby JJ. Regional distribution of gas and tissue in acute respiratory distress syndrome. I. Consequences for lung morphology. CT Scan ARDS Study Group. Intensive Care Med. 2000;26:857–869. [DOI] [PubMed] [Google Scholar]
- 11.Carvalho AR, Spieth PM, Pelosi P, et al. Ability of dynamic airway pressure curve profile and elastance for positive end-expiratory pressure titration. Intensive Care Med. 2008;34:2291–2299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carvalho AR, Pacheco SA, de Souza Rocha PV, et al. Detection of tidal recruitment/overdistension in lung-healthy mechanically ventilated patients under general anesthesia. Anesth Analg. 2013;116:677–684. [DOI] [PubMed] [Google Scholar]
- 13.Kano S, Lanteri CJ, Duncan AW, Sly PD. Influence of nonlinearities on estimates of respiratory mechanics using multilinear regression analysis. J Appl Physiol. 1994;77:1185–1197. [DOI] [PubMed] [Google Scholar]
- 14.Canet J, Gallart L, Gomar C, et al. ; ARlSCAT Group. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113:1338–1350. [DOI] [PubMed] [Google Scholar]
- 15.Mazo V, Sabaté S, Canet J, et al. Prospective external validation of a predictive score for postoperative pulmonary complications. Anesthesiology. 2014;121:219–231. [DOI] [PubMed] [Google Scholar]
- 16.The PROVE Network Investigators. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet. 2014;384:495–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bersten AD. Measurement of overinflation by multiple linear regression analysis in patients with acute lung injury. Eur Respir J. 1998;12:526–532. [DOI] [PubMed] [Google Scholar]
- 18.Jandre FC, Modesto FC, Carvalho AR, Giannella-Neto A. The endotracheal tube biases the estimates of pulmonary recruitment and overdistension. Med Biol Eng Comput. 2008;46:69–73. [DOI] [PubMed] [Google Scholar]
- 19.Faul F, Erdfelder E, Buchner A, Lang AG. Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods. 2009;41:1149–1160. [DOI] [PubMed] [Google Scholar]
- 20.The R Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2016. Available at: http://www.R-project.org/ Accessed May 23, 2017. [Google Scholar]
- 21.Maisch S, Reissmann H, Fuellekrug B, et al. Compliance and dead space fraction indicate an optimal level of positive end-expiratory pressure after recruitment in anesthetized patients. Anesth Analg. 2008;106:175–181. [DOI] [PubMed] [Google Scholar]
- 22.Futier E, Constantin JM, Petit A, et al. Positive end-expiratory pressure improves end-expiratory lung volume but not oxygenation after induction of anaesthesia. Eur J Anaesthesiol. 2010;27:508–513. [DOI] [PubMed] [Google Scholar]
- 23.Satoh D, Kurosawa S, Kirino W, et al. Impact of changes of positive end-expiratory pressure on functional residual capacity at low tidal volume ventilation during general anesthesia. J Anesth. 2012;26:664–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Güldner A, Braune A, Ball L, et al. Comparative effects of volutrauma and atelectrauma on lung inflammation in experimental acute respiratory distress syndrome. Crit Care Med. 2016;44:e854–e865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Severgnini P, Selmo G, Lanza C, et al. Protective mechanical ventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology. 2013;118:1307–1321. [DOI] [PubMed] [Google Scholar]
- 26.Futier E, Constantin JM, Paugam-Burtz C, et al. ; IMPROVE Study Group. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–437. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


