Abstract
The prevalence of intimate partner violence (IPV) is alarmingly high among South African adolescent girls and young women (AGYW). Limited data exist exploring how IPV prevalence and its risk factors differ by age. Study data were from the baseline visit of HPTN 068, a randomized controlled trial (RCT) conducted from 2011 to 2015 in Mpumalanga, South Africa. A cohort of 2,533 AGYW, aged 13 years to 20 years, answered survey questions on demographics and behaviors, including their experiences of physical and sexual violence ever and in the past 12 months. We calculated the prevalence of IPV and related risk factors, as well as prevalence ratios with 95% confidence intervals, stratified by age. Nearly one quarter (19.5%, 95% CI = [18.0, 21.2]) of AGYW experienced any IPV ever (physical or sexual) by a partner. The prevalence of any IPV ever among AGYW aged 13 years to 14 years, 15 years to 16 years, and 17 years to 20 years was 10.8%, 17.7%, and 32.1%, respectively. Key variables significantly associated with any IPV ever across all age groups included borrowing money from someone outside the home in the past 12 months, ever having had vaginal sex, ever having had anal sex, and consuming any alcohol. Few statistically significant associations were unique to specific age groups. The history of IPV among the youngest AGYW is a critical finding and should be a focus of prevention efforts.
Keywords: Africa, data processing and interpretation, research methods, social sciences
Background
Global Intimate Partner Violence (IPV)
Women’s experience of IPV is a global concern, and intervention efforts to decrease the burden of IPV are vital. A 2013 World Health Organization (WHO) report indicated that globally, close to one third of women who reported ever having been in a relationship experienced IPV, and nearly 30% of women in southern sub-Saharan Africa report experiencing it (García-Moreno et al., 2013). In South Africa, approximately one fifth of adult women report ever experiencing violence by a partner (Statistics South Africa, 2017).
South African Adolescent Girls and Young Women (AGYW) and IPV
IPV prevalence estimates are also alarmingly high among South African AGYW. A multicountry study published in 2014 found that among 15-year to 19-year-old adolescent young women in Johannesburg, prevalence in the past year of physical IPV was 30.9% and sexual IPV was 18.3% (Decker et al., 2014). Similarly, a 2015 study in a peri-urban area of South Africa found that 16-year to 24-year-old AGYW who reported multiple partnerships also reported a high burden of IPV; 80% reported physical IPV and 67% reported sexual IPV in the past 12 months (Zembe, Townsend, Thorson, Silberschmidt, & Ekstrom, 2015). Furthermore, a study in urban South Africa found that among Grade 8 AGYW, lifetime experience of physical and sexual IPV was 24.1% and 13.8%, respectively; and 30.9% of AGYW reported either physical or sexual IPV. The prevalence was also delineated by age group (12–13 years vs. 14–19 years), and the prevalence of sexual or physical IPV was higher among the older age group (46.8% vs. 53.2%; Shamu et al., 2016). A Cape Town study of Grade 8 AGYW found that 39% reported physical IPV by a partner in the past 3 months (Russell et al., 2014).
Risk Factors and IPV
Several factors are associated with IPV in South Africa, including violence as the acceptable social norm (Jewkes, 2002), childhood experiences of abuse (Shamu et al., 2016), alcohol and substance use (Decker et al., 2014; Shamu et al., 2016), multiple partnerships (Decker et al., 2014), transactional sex (Decker et al., 2014; Zembe et al., 2015), lack of condom use (Decker et al., 2014), and mental health problems, such as depression (Decker et al., 2014).
Adolescent Development
Although there are several prevalence studies with reported risk factors for IPV among South African AGYW, most studies aggregate ages and do not provide information separated into the three stages of adolescence—early adolescence, middle adolescence, and later adolescence entering young adulthood. Key life events are transpiring at different ages (e.g., beginning of romantic and sexual relationships in middle adolescence), which may influence external exposures as well as the behaviors of the AGYW. Early adolescence is marked by the start of puberty (Rosenfield, Lipton, & Drum, 2009), budding sexual attraction, the preparation for or entry into secondary school, and wanting to fit in closely with peers (Teipel, 2003a). This may be the time when the adolescent is introduced to her first partnership. In middle adolescence, AGYW often begin to have sex and conflict with parental figures may escalate as they attempt to establish their autonomy (e.g., spending more of their free time with partners). During this period, peer acceptance on partner choice and emulating the behaviors they perceive their peers to be engaging in is important (Teipel, 2003c). In older adolescence, AGYW are preparing for the adult stage of life. This may include graduation from secondary school and/or preparing for tertiary education, a full-time job, and raising a family. At this stage, much of the physical growth from the earlier stages of adolescence begins slowing down. Another key component to this developmental stage is the transition from predominantly peer-oriented relationships to more intimate and serious relationships. During this stage, the AGYW are beginning to solidify characteristics they are looking for in a partner (Teipel, 2003b).
In the early 2000s, Arnett coined the term “emerging adulthood,” conceptualizing adolescence as a period that could extend through the 20s (Arnett, 2000). Many resource-rich settings can support an extended period of adolescent development and exploration, but AGYW living in regions with particular economic and social expectations may take on more traditional adult roles, such as parenting, at a younger age, limiting their opportunities (Sawyer, Azzopardi, Wickremarathne, & Patton, 2018). A rural Mpumalanga, South African study, found adult women identified puberty, socializing with the opposite sex, having a child (regardless of marital status), and behaving in a socially respectable and feminine manner as important components to a successful transition to womanhood (Sennott & Mojola, 2017). Biologically, changes in social-affective processing during adolescence may position the AGYW to be more adaptive to changing contexts, therefore, more willing to consider and enact new ideas and behaviors when presented with them (Crone & Dahl, 2012). This transitional time period could mark an uptick in risky behaviors associated with IPV, but just as important, both adolescent women and men may show an increased preparedness, motivation and flexibility to engage in interventions that help prevent IPV, if presented with them.
IPV Prevalence and Stages of Adolescence
In this paper, we provide prevalence estimates of IPV and explore potentially related factors, such as individual, partner, and economic characteristics, disaggregated by age group (13–14, 15–16, 17–20; all in years) among AGYW in rural Mpumalanga Province, South Africa. Our cohort ranged in age from 13 years to 20 years, with a median age of 15 years. The defined age range for each developmental stage differs across studies (Curtis, 2015), which can make cross-study comparisons challenging. The disaggregation we chose closely matches the typical ranges for the three stages of adolescence, while considering the data available in our study. We contribute to the existing body of evidence by highlighting these differences by age strata.
Method
Study Overview
This secondary analysis uses baseline data from HPTN 068, an RCT conducted in Mpumalanga, South Africa. The HIV Prevention Trials Network (HPTN) conducts global clinical trials focused on HIV prevention. The purpose of HPTN 068 was to assess if receiving cash transfers, conditional on school attendance, reduced HIV incidence in South African AGYW. Each AGYW randomized to the intervention arm and her parent/legal guardian received approximately US$30 per month, in total, if she successfully attended 80% of school the month prior. Baseline study data were collected from March 2011 through December 2012 (Pettifor, MacPhail, Selin, et al., 2016). This pre-intervention data set provided a unique opportunity to analyze IPV among a large sample of South African AGYW, including young AGYW, disaggregated by age.
Enrollment
The Agincourt Health and Socio-Demographic Surveillance System (AHDSS) follows the local population through an annual census to monitor health and social factors. This census served as the platform for recruitment of the study sample (Kahn et al., 2012). The AHDSS has a strong relationship with the communities engaged in the research, and prior to study start, each study is formally introduced to the participating communities. The community also receives summarized study results upon analysis completion.
To be enrolled in the study, participants needed to be female and between 13 years and 20 years of age at baseline, planning to reside in the AHDSS catchment area for the next 3 years, a student in Grades 8 to 11 at one of the local 26 public high schools, able to consent or assent to participate in the study, be able to read, have either a bank account or the proper paperwork to open a bank account to receive the cash transfer (if randomized to the intervention arm), and not be pregnant or married at baseline. An HIV positive status at baseline was not an exclusion criterion for study participation. A parent/legal guardian also needed to consent to the AGYW’s participation (if she was below 18 years), as well as consent to her or his own participation. In addition, the parent/legal guardian needed to also either have a bank account, have proper paperwork to open a bank account, or be able to identify someone who could receive the money. There were 2,533 AGYW and their parents/legal guardians enrolled in the study, 25% of the total number of families screened (Pettifor, MacPhail, Hughes, et al., 2016); all participants enrolled provided informed consent and assent.
Data Collection and Baseline Measures
Data for this analysis were acquired from two surveys and from laboratory data. The surveys included a baseline household survey on family economic assets conducted with the parent/guardian of the AGYW and then the AGYW baseline survey, from which most of the data for the analysis originates.
Baseline household survey.
Parents/legal guardians of the AGYW completed a fieldworker led computer survey at home using Computer-Assisted Personal Interview (CAPI) software. The household survey included a roster of characteristics of those living in the home, agricultural and water resources, durable assets, and monetary transfers in and out of the home.
Young women’s survey and laboratory testing.
To maintain privacy for sensitive questions, most of the data collection process involved use of Audio Computer-Assisted Self-Interview (ACASI), which allowed young women to read and hear the questions through headphones and complete the survey on their own, potentially minimizing response bias. Survey questions included IPV experience, alcohol use, views toward gender norms, number of sexual partners, coital debut, and number of self-reported sex acts in the past 3 months, among others. A majority of the predictor variables were analyzed with a dichotomous response of yes/no. Age at sexual debut (15 years and younger vs. older than 15 years), number of lifetime partners (two or more vs. zero or one), and orphan status (one or both parents deceased vs. none) are examples of the different variable categorizations. The gender norms scale focused on sexual relationship domains, household chores and daily life, and reproductive health and disease prevention. There were 13 questions asked, ranging from, “It is the man who decides what type of sex to have” to “A woman should obey her husband in all things.” AGYW could respond with “agree a lot,” “somewhat agree,” or “do not agree.” Final scores were calculated, with the most equitable gender norms being a score of 13 and the least being a score of 0. Pretest counseling for HIV occurred after the survey, followed by HIV testing, posttest counseling, and finally randomization for the overall trial. Participants received HIV rapid test results on the same day the testing was performed.
Definition and measurement of IPV in the young women’s baseline survey.
IPV was defined as physical and/or sexual violence occurring between an AGYW and a partner, with partnership defined as a “current boyfriend or partner or any other partner in [a young woman’s] past.” There were a total of eight IPV questions asked, designed by the WHO (García-Moreno, Jansen, Ellsberg, Heise, & Watt, 2005), including six physical violence questions and two sexual violence questions. The severity of the physical violence ranged from “Has a partner ever slapped you or threw something at you that could hurt?” to “Has a partner ever threatened to use or used a gun, knife, or other weapon against you?”
Both physical and sexual violence questions assessed whether that form of violence had “ever” happened, and if yes, whether it had happened “in the last 12 months.” Physical violence questions specifically mentioned a partner as the perpetrator. Sexual violence questions asked about several kinds of perpetrators: a boyfriend/partner, a family member, or someone else outside the family (not including a boyfriend or partner). For this analysis, we only focused on sexual violence experienced by a partner.
Study Response to Reports of Violence
During the post-test HIV counseling session, the counselor followed up with AGYW who reported violence in their surveys and provided them with rights and safety planning, which included information on health and sexual rights, strategies to stay safe, and how to handle situations that are physically or sexually unsafe. Following South African Health Department Guidelines, all reports of violence by AGYW below the age of 18 years were referred to a local social worker. AGYW and their parents/legal guardians were made aware of this procedure during the time of assent/consent, and again for the AGYW at time of survey completion. Social workers then contacted the AGYW to determine next steps, and the study team facilitated initial meetings between the AGYW and the social workers after triaging cases. AGYW 18 years and above who reported violence and wanted support from the social workers were also referred.
Analysis
Data were analyzed in SAS v9.3. Prevalence and prevalence ratios with 95% confidence intervals were calculated using log binomial regression. Data were coded in the following manner: any IPV (responding yes to at least one physical or sexual IPV question), any physical IPV (answering yes to one or more physical IPV questions), any sexual IPV (answering yes to one or more sexual IPV questions), and both IPV (responding yes to at least one physical IPV question and yes to at least one sexual IPV question). If data on one or more questions within each type (i.e., any IPV) were missing, the constructed variable value was set to missing. Following this approach may have led to a slight underestimate of IPV reported.
Results
Study Population Characteristics
The 2,533 participants ranged in age from 13 years to 20 years, with a median age of 15 years. The 15- to 16-year olds were the largest age group, at 42.4%. Over one third of the participants reported being worried about having enough food for themselves or their family in the past 12 months, and 25% currently had savings for the future. Over one fifth needed to borrow money from outside the home during the past 12 months, and over one quarter had at least one parent who had died.
Just over one quarter (26.6%) of the sample reported ever having had vaginal sex, with a median sexual debut age of 16 years. As expected, a much lower number reported ever having had anal sex (4.8%). Among those who reported ever having had vaginal or anal sex, the median number of lifetime sexual partners was one. Among those who reported ever having had vaginal or anal sex, the majority (94.3%) also reported having had one or more partners in the past 12 months, indicating that while partnership number was low, it was recent. Over one quarter reported unprotected sex in the past 3 months and a large majority of participants who reported ever having had sex indicated that one or more of their sexual partners was a main partner/boyfriend (74%). Moreover, 14.1% of AGYW reported having had transactional sex—defined as sex in exchange for money or goods.
Approximately 9% of the young women in the total sample reported ever being pregnant, 25.8% reported currently using birth control, 3.2% were found HIV+ at baseline, and 4.7% were found HSV-2+ at baseline. Low substance abuse was also reported in our sample, with only 8.9% reporting any alcohol consumption (whether frequent or infrequent use), and 4.8% reporting ever having used drugs (Table 1).
Table 1.
Characteristics of South African AGYW Participating in HPTN 068 Baseline, March 2011-December 2012 (n = 2,533).
| Characteristics | Yes, n (%) | Median (IQR) |
|---|---|---|
| Age in years (n = 2,533) | 15 (14–17) | |
| 17–20a | 685 (27.0) | |
| 15–16 | 1,075 (42.4) | |
| 13–14 | 773 (30.5) | |
| Orphan status (n = 2,406) | ||
| One or both parents dead | 683 (28.4) | |
| Past 12 months, worried about food for self or family (n = 2,511) | 862 (34.3) | |
| Past 12 months, borrowed money from someone outside the home (n = 2,511) | 563 (22.4) | |
| Currently has savings for the future (cash, assets; n = 2,520) | 630 (25.0) | |
| Assets (number of durable goods in the home; n = 2,528)b | 13 (9–18) | |
| Assets (AGYW with ≤ 13 durable goods in the home) | 1,317 (52.10) | |
| Ever had vaginal sex (n = 2,523) | 672 (26.6) | |
| Age at vaginal sexual debut (among those who reported ever having vaginal sex; n = 631)c | 16 (15–16) | |
| 15 years or younger | 290 (46.0) | |
| Ever had anal sex (n = 2,528) | 120 (4.8) | |
| Number of lifetime sexual partners (n = 676)d | 1 (1–2) | |
| Two or more | 323 (47.8) | |
| One | 353 (52.2) | |
| Number of sexual partners in past 12 months (n = 665)d | ||
| One or more | 627 (94.3) | |
| Zero | 38 (5.7) | |
| Had unprotected sex with a partner in the past 3 months (n = 677)d | 204 (30.1) | |
| One or more of the three most recent sexual partners is/was a main partner/boyfriend (n = 678)d | 499 (73.6) | |
| One or more of the three most recent sexual partners is/was a regular, casual sex partner (n = 678)d | 200 (29.5) | |
| One or more of the three most recent sexual partners is/was a nonregular casual sex partner (n = 678)d | 94 (13.9) | |
| One or more of the three most recent sexual partners is/was a sex work client (n = 678)d | 16 (2.4) | |
| Currently lives with one or more (up to three) of the three most recent sexual partners (n = 679)d | 84 (12.4) | |
| Had transactional sex (sex because $ or gifts given; n = 689)d | 97 (14.1) | |
| HIV+ (n = 2,529) | 81 (3.2) | |
| HSV-2+ (n = 2,529) | 120 (4.7) | |
| Had an older partner (≥5 years, sexual or nonsexual; n = 985) | 153 (15.5) | |
| Gender equitable norms (GEMS; n = 2,530)e | 4 (2–6) | |
| Score of 0–4 | 1,447 (57.2) | |
| Score >4, up to 13 | 1,083 (42.8) | |
| Ever pregnant (n = 2,502) | 223 (8.9) | |
| Currently using birth control (n = 2,520) | 651 (25.8) | |
| Consumes any alcohol (n = 2,526) | 225 (8.9) | |
| Ever used drugs (n = 2,527) | 120 (4.8) |
Note. AGYW = adolescent girls and young women; HPTN = HIV Prevention Trials Network; HSV = herpes simplex virus; GEMS = gender equitable measurement scale; IQR = interquartile range.
One participant turned 21 years on her date of randomization.
Durable assets include items such as radios, televisions, cell phones, and so on.
Vaginal sexual debut of ≤5 was considered unlikely and not included (n = 31).
Among those who reported ever having vaginal or anal sex.
The range of GEMS scores is from 0 to 13 with a higher score representing more equitable gender norms views.
Prevalence of Experiencing IPV
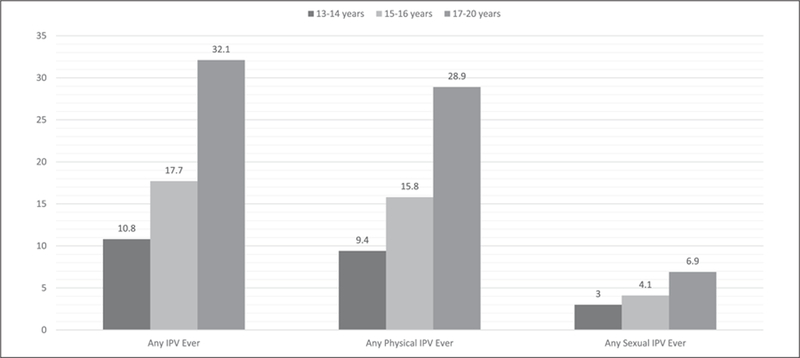
Close to 20% of our study population (19.5%, 95% CI = [18.0, 21.2]) ever experienced any IPV (physical or sexual) by a partner (Table 2). In addition, prevalence of experiencing any IPV increases with age (Figure 1). The prevalence of any IPV ever among AGYW aged 13 years to 14 years, 15 years to 16 years, and 17 years to 20 years was 10.8%, 17.7%, and 32.1%, respectively. The prevalence of any physical IPV and any sexual IPV was highest among the 17- to 20-year olds at 28.9% and 6.9%, respectively.
Table 2.
Prevalence of Experiencing IPV Among South African AGYW Participating in HPTN 068 Baseline, March 2011-December 2012 (n = 2,533).
| Characteristics | Ever experienced, total study population (n = 2,533) |
Ever experienced, among those who reported ever being sexually active (vaginal or anal sex; n = 693) |
Experienced in past 12 months, total study population (n = 2,533) |
Experienced in past 12 months, among those reporting greater than one sexual partner in the past 12 months (n = 683) |
||||
|---|---|---|---|---|---|---|---|---|
| Numerator/denominator | Prevalence (95% CI) | Numerator/denominator | Prevalence (95% CI) | Numerator/denominator | Prevalence (95% CI) | Numerator/denominator | Prevalence (95% CI) | |
| Any violence (physical or sexual) by a partner (any IPV) | 479/2,451 | 19.5 [18.0, 21.2] | 256/684 | 37.4 [34.0, 41.2] | ||||
| Any physical violence by a partner | 431/2,474 | 17.4 [16.0, 19.0] | 239/689 | 34.7 [31.3, 38.4] | 266/2,474 | 10.8 (9.6, 12.0) | 159/681 | 23.4 [20.4, 26.8] |
| Partner slapped you or threw something at you that could hurt | 291/2,485 | 11.7 [10.5, 13.1] | 193/690 | 28.0 [24.8, 31.5] | 179/2,484 | 7.2 (6.3, 8.3) | 116/681 | 17.0 [14.4, 20.1] |
| Partner ever pushed or shoved | 218/2,482 | 8.8 [7.7, 10.0] | 116/690 | 16.8 [14.2, 19.9] | 128/2,481 | 5.2 (4.4, 6.1) | 81/681 | 11.9 [9.7, 14.6] |
| Partner ever hit you with his fist or with something else that could hurt you | 78/2,482 | 3.1 [2.5, 3.9] | 45/689 | 6.5 [4.9, 8.7] | 53/2,482 | 2.1 (1.6, 2.8) | 35/681 | 5.1 [3.7, 7.1] |
| Partner ever kicked you, dragged you, or beat you up | 138/2,483 | 5.6 [4.7, 6.5] | 77/689 | 11.2 [9.1, 13.8] | 92/2,483 | 3.7 (3.0, 4.5) | 61/681 | 9.0 [7.1, 11.4] |
| Partner ever choked or burned you on purpose | 36/2,481 | 1.5 [1.1, 2.0] | 22/689 | 3.2 [2.1, 4.8] | 28/2,481 | 1.1 (0.8, 1.6) | 20/681 | 2.9 [1.9, 4.5] |
| Partner ever threatened to use or used a gun, knife, or other weapon against you | 37/2,484 | 1.5 [1.1, 2.1] | 26/689 | 3.8 [2.6, 5.5] | 25/2,484 | 1.0 (0.7, 1.5) | 18/681 | 2.6 [1.7, 4.2] |
| Any sexual violence by a partnera | 113b/2,490 | 4.5 [3.8, 5.4] | 57/685 | 8.3 [6.5, 10.7] | ||||
| Ever physically forced to have sex when you did not want | 76/2,498 | 3.0 [2.4, 3.8] | 42/686 | 6.1 [4.6, 8.2] | ||||
| Ever had sex that you did not want because you were afraid of what the other person might do | 66/2,503 | 2.6 [2.1, 3.4] | 37/687 | 5.4 [3.9, 7.4] | ||||
| Both physical and sexual violence by a partner (both IPV)a | 62/2,451 | 2.5 [2.0, 3.2] | 39/684 | 5.7 [4.2, 7.7] | ||||
Note. IPV = intimate partner violence; HPTN = HIV Prevention Trials Network; ACASI = Audio Computer-Assisted Self-Interview; AGYW = adolescent girls and young women.
Question on sexual IPV experienced in the past 12 months could not be analyzed given ACASI construction.
56/113 girls said yes to sexual violence by a partner, but no to any vaginal or anal sex ever.
Figure 1.
IPV prevalence by type and age group at HPTN 068 baseline.
Note. IPV = intimate partner violence; HPTN = HIV Prevention Trials Network.
Factors Associated With IPV
The prevalence of any IPV ever among AGYW with exposed status for selected characteristics is presented in Table 3. AGYW of all ages who had experienced IPV had a higher prevalence of worrying about food for self or family in the past 12 months, borrowing money outside the home in the past 12 months, having had vaginal sex, having had anal sex, and having consumed any alcohol (Table 4).
Table 3.
Prevalence of Any Physical or Sexual IPV (Any IPV) Ever Among Those With Selected Characteristics, South African AGYW Participating in HPTN 068 Baseline, March 2011-December 2012—Total Study Population (n = 2,533).
| Among 17- to 20-year olds |
Among 15- to 16-year olds |
Among 13- to 14-year olds |
||||
|---|---|---|---|---|---|---|
| Characteristic (exposed status presented) | Number of any IPV/total n exposed status | Prevalence of any IPV ever among exposed status (95% CI) | Number of any IPV/total n exposed status | Prevalence of any IPV ever among exposed status (95% CI) | Number of any IPV/total n exposed status | Prevalence of any IPV ever among exposed status (95% CI) |
| Orphan (both/one parent dead) | 75/207 | 36.2 [30.2, 43.4] | 52/274 | 19.0 [14.9, 24.2] | 20/191 | 10.5 [6.9, 15.9] |
| In past 12 months, worried about food for self or family | 100/276 | 36.2 [31.0, 42.4] | 83/359 | 23.1 [19.2, 27.9] | 32/206 | 15.5 [11.3, 21.4] |
| In past 12 months, borrowed money from someone outside home | 91/185 | 49.2 [42.5, 57.0] | 55/234 | 23.5 [18.7, 29.6] | 24/131 | 18.3 [12.8, 26.3] |
| Currently has savings for the future (cash, assets) | 60/147 | 40.8 [33.6, 49.6] | 53/260 | 20.4 [16.0, 25.9] | 27/211 | 12.8 [9.0, 18.2] |
| Assets (AGYW with ≤13 durable goods in the home) | 119/373 | 31.9 [27.5, 37.0] | 100/547 | 18.3 [15.3, 21.8] | 41/361 | 11.4 [8.5, 15.2] |
| Ever had vaginal sex | 163/366 | 44.5 [39.7, 49.9] | 72/254 | 28.4 [23.3, 34.5] | 12/45 | 26.7 [16.4, 43.3] |
| Age at vaginal sexual debuta (15 years or younger)b | 47/87 | 54.0 [44.5, 65.6] | NCc | NCc | NCc | NCc |
| Ever had anal sex | 30/52 | 57.7 [45.7, 72.8] | 16/55 | 29.1 [19.3, 44.0] | 3/8 | 37.5 [15.3, 91.7] |
| Number of lifetime sexual partners (two or more partners)d | 101/203 | 50.0 [43.3, 57.1] | 35/104 | 33.7 [25.7, 44.1] | 6/11 | 54.6 [31.8, 93.6] |
| Number of sex partners in the past 12 months (one or more)d | 159/348 | 45.7 [40.7, 51.2] | 71/234 | 30.3 [25.0, 36.8] | 9/40 | 22.5 [12.7, 40.0] |
| Unprotected sex with a partner in the past 3 monthsd | 68/125 | 54.4 [46.3, 63.9] | 26/71 | 36.6 [27.0, 49.7] | 4/7 | CUe |
| One or more of the three most recent sexual partners is/was a main partner/boyfriendd | 123/274 | 44.9 [39.4, 51.2] | 54/190 | 28.4 [22.7, 35.6] | 10/31 | 32.3 [19.4, 53.7] |
| One or more of the three most recent sexual partners is/was a regular, casual sex partnerd | 58/117 | 49.6 [41.3, 59.5] | 28/73 | 38.4 [28.7, 51.3] | 2/8 | 25.0 [7.5, 83.0] |
| One or more of the three most recent sexual partners is/was a nonregular casual sex partnerd | 22/49 | 44.9 [32.9, 61.2] | 11/38 | 29.0 [17.6, 47.6] | 2/7 | 28.6 [8.9, 92.2] |
| One or more of the three most recent sexual partners is/was a sex work clientd | 7/11 | 63.6 [40.7, 99.5] | 1/2 | CUe | 1/3 | CUe |
| Currently lives with one or more (up to three) of the three most recent sexual partnersd | 28/53 | 52.8 [41.0, 68.1] | 12/26 | 46.2 [30.5, 69.9] | 1/5 | CUe |
| Had transactional sex (sex because given in US$ or gifts)d | 37/57 | 64.9 [53.6, 78.6] | 13/34 | 38.2 [24.9, 58.6] | 1/6 | 16.7 [2.8, 100.0] |
| HIV+ | 15/39 | 38.5 [25.9, 57.2] | 5/24 | 20.8 [9.6, 45.4] | 2/17 | 11.8 [3.2, 43.3] |
| HSV-2+ | 29/74 | 39.2 [29.5, 52.1] | 7/39 | 18.0 [9.2, 35.1] | 1/5 | CUe |
| Older partner (≥5 years, sexual or nonsexual) | 33/74 | 44.6 [34.6, 57.5] | 21/66 | 31.8 [22.4, 45.3] | 4/12 | 33.3 [15.0, 74.2] |
| GEMS score of 0–4f | 149/387 | 38.5 [34.0, 43.7] | 125/588 | 21.3 [18.2, 24.8] | 48/425 | 11.3 [8.7, 14.7] |
| Ever pregnant | 85/166 | 51.2 [44.1, 59.4] | 21/50 | 42.0 [30.3, 58.2] | CUe | CUe |
| Currently using birth control | 133/310 | 42.9 [37.7, 48.8] | 73/254 | 28.7 [23.7, 34.9] | 12/79 | 15.2 [9.0, 25.6] |
| Consumes any alcohol | 46/81 | 56.8 [47.0, 68.7] | 42/97 | 43.3 [34.5, 54.4] | 11/45 | 24.4 [14.6, 40.9] |
| Ever used drugs | 26/40 | 65.0 [51.8, 81.6] | 12/47 | 25.5 [15.7, 41.6] | 5/33 | 15.2 [6.8, 34.0] |
Note. IPV = intimate partner violence; AGYW = adolescent girls and young women; HPTN = HIV Prevention Trials Network; HSV = herpes simplex virus; GEMS = gender equitable measurement scale.
Vaginal sexual debut of ≤5 was considered unlikely and not included (n = 31).
Among those who reported ever having vaginal sex.
NC = not calculated as adolescent girls would not have a chance to experience later debut.
Among those who reported ever having vaginal or anal sex.
CU = numbers not large enough—estimate unstable or could not be calculated correctly.
The range of GEMS scores is from 0 to 13 with a higher score representing more equitable gender norms views; median of 4.
Table 4.
Baseline Associations of Selected Characteristics and Any Physical or Sexual IPV (Any IPV) Ever Among South African AGYW Participating in HPTN 068 Baseline, March 2011-December 2012—Total Study Population (n = 2,533).
| Among 17–20 year olds |
Among 15–16 year olds |
Among 13–14 year olds |
|
|---|---|---|---|
| Characteristics | Prevalence ratio (95% CI) | Prevalence ratio (95% CI) | Prevalence ratio (95% CI) |
| Orphan (both/one parent dead vs. both alive) | 1.2 [1.0, 1.5] | 1.1 [0.9, 1.5] | 1.0 [0.6, 1.6] |
| In past 12 months, worried about food for self or family vs. did not worry | 1.2 [1.0, 1.5] | 1.6 [1.2, 2.0] | 1.7 [1.1, 2.6] |
| In past 12 months, borrowed money from someone outside home vs. did not | 1.9 [1.6, 2.4] | 1.5 [1.1, 2.0] | 2.0 [1.3, 3.1] |
| Currently has savings for the future (cash, assets) vs. currently does not | 1.4 [1.1, 1.7] | 1.2 [0.9, 1.6] | 1.3 [0.8, 2.0] |
| Assets (AGYW with ≤13 durable goods in the home vs. not) | 1.0 [0.8, 1.2] | 1.1 [0.8, 1.4] | 1.1 [0.7, 1.7] |
| Ever vaginal sex vs. never vaginal sex | 2.5 [1.9, 3.3] | 2.0 [1.5, 2.6] | 2.7 [1.6, 4.6] |
| Age at vaginal sexual debuta (15 years or younger vs. 16 years or older)b | 1.3 [1.0, 1.7] | NCc | NCc |
| Ever anal sex vs. never anal sex | 1.9 [1.5, 2.5] | 1.7 [1.1, 2.6] | 3.6 [1.4, 8.9] |
| Number of lifetime sexual partners (two or more partners vs. one)d | 1.3 [1.0, 1.6] | 1.3 [0.9, 1.9] | 3.1 [1.3, 7.6] |
| Number of sex partners in the past 12 months (one or more vs. zero)d | 1.1 [0.6, 2.1] | 1.8 [0.6, 5.2] | 0.5 [0.1, 1.4] |
| Unprotected sex with a partner in the past 3 months vs. no unprotected sex in past 3 monthsd | 1.4 [1.1, 1.7] | 1.4 [0.9, 2.0] | CUe |
| One or more of the three most recent sexual partners is/was a main partner/boyfriend vs. notd | 1.0 [0.8, 1.3] | 0.9 [0.6, 1.3] | 2.4 [0.6, 9.7] |
| One or more of the three most recent sexual partners is/was a regular, casual sex partner vs. notd | 1.2 [0.9, 1.5] | 1.5 [1.0, 2.2] | 1.0 [0.3, 3.5] |
| One or more of the three most recent sexual partners is/was a nonregular casual sex partner vs. notd | 1.0 [0.7, 1.4] | 1.0 [0.6, 1.7] | 1.1 [0.3, 4.0] |
| One or more of the three most recent sexual partners is/was a sex work client vs. notd | 1.4 [0.9, 2.3] | 1.7 [0.4, 6.9] | 1.3 [0.2, 7.0] |
| Currently lives with one or more (up to three) of the three most recent sexual partners vs. does notd | 1.2 [0.9, 1.6] | 1.7 [1.1, 2.7] | 0.7 [0.1, 4.4] |
| Had transactional sex (sex because given US$ or gifts) vs. did notd | 1.6 [1.3, 2.0] | 1.4 [0.9, 2.2] | 0.6 [0.1, 3.7] |
| HIV+ vs. HIV− | 1.2 [0.8, 1.8] | 1.2 [0.5, 2.6] | 1.1 [0.3, 4.1] |
| HSV-2+ vs. HSV-2− | 1.3 [0.9, 1.7] | 1.0 [0.5, 2.0] | 1.9 [0.3, 10.9] |
| Older partner (≥5 years, sexual or nonsexual) | 1.1 [0.8, 1.4] | 1.2 [0.8, 1.8] | 1.4 [0.6, 3.3] |
| Gender equitable norms score of 0–4f | 1.6 [1.3, 2.1] | 1.6 [1.2, 2.2] | 1.1 [0.7, 1.7] |
| Ever pregnant vs. never pregnant | 2.0 [1.6, 2.5] | 2.6 [1.8, 3.7] | CUe |
| Currently using birth control vs. not | 1.9 [1.5, 2.4] | 2.0 [1.6, 2.6] | 1.5 [0.8, 2.6] |
| Consumes any alcohol vs. none | 2.0 [1.6, 2.5] | 2.9 [2.2, 3.8] | 2.5 [1.4, 4.3] |
| Ever used drugs vs. never used drugs | 2.2 [1.7, 2.8] | 1.5 [0.9, 2.5] | 1.4 [0.6, 3.3] |
Note. IPV = intimate partner violence; AGYW = adolescent girls and young women; HPTN = HIV Prevention Trials Network; HSV = herpes simplex virus; GEMS = gender equitable measurement scale.
Vaginal sexual debut of ≤5 was considered unlikely and not included (n = 31).
Among those who reported ever having vaginal sex.
NC = not calculated as adolescent girls would not have a chance to experience later debut.
Among those who reported ever having vaginal or anal sex.
CU = numbers not large enough—estimate unstable and could not be calculated, or the prevalence in Table 3 was not able to be calculated.
The range of GEMS scores is from 0 to 13 with a higher score representing more equitable gender norms views; median of 4.
In addition, among both the 17- to 20-year olds and 15- to 16-year olds, ever being pregnant, currently using birth control, and having lower gender equitable norm scores were associated with experiencing any IPV ever (Table 4).
Furthermore, among the 17- to 20-year olds alone, currently having savings for the future, having unprotected sex with a partner in the past 3 months, having had transactional sex (among those who had ever had vaginal or anal sex), and ever using drugs were all factors significantly associated with experiencing IPV. Among the 15- to 16-year olds alone, currently living with a sex partner and having a casual sex partner had a significant association with IPV (Table 4).
Discussion
In this study, among AGYW in rural South Africa, we found that the prevalence of sexual or physical IPV experienced was close to 20%. Given that 15 was the mean age of the sample and 26.6% reported ever having had vaginal sex, this is very high. Our study is the only study, of which we are aware, that describes the prevalence and associated factors of IPV among South African AGYW, disaggregated by age.
Physical violence is very common among AGYW who have had sex, whereas sexual violence from a partner is less common. Milder types of physical IPV are more prevalent compared with more severe types, reported both in their lifetime as well as in the past 12 months. Physical IPV (10.7%) was reported among AGYW who said they had never had sex (data not shown). This is not unexpected given AGYW may form partnerships not involving sex, especially during early adolescence, and thus, IPV interventions should be tailored accordingly. In addition, AGYW may have chosen not to report their sexual history in the survey.
Although our data suggest that age matters when having ever experienced any IPV, we did not see a great difference, by age, in risk factors for IPV. Rather, a common set of risk factors emerged for experiencing any IPV. This included borrowing money from someone outside the home in the past 12 months (a marker of experiencing poverty or insufficient resources for perceived needs), ever having had vaginal sex, ever having had anal sex, and consuming any alcohol.
In our study, borrowing money was associated with increased reporting of IPV among all age groups. Research in Kenya showed that working versus not working, among married female adolescents who did not have any savings, was associated with increased IPV, but male partner trust of the adolescent with money was associated with reduced IPV (Muthengi, Gitau, & Austrian, 2016). This supports the role of traditional gender roles (women not working) as well as male-centered decision making (his level of trust) in the experience of IPV. Among the 17- to 20-year olds in our study, having personal assets (i.e., personal savings for the future) was associated with IPV. A meta-analysis of global demographic and health surveys did not find a clear directional relationship between asset ownership and IPV (Peterman, Pereira, Bleck, Palermo, & Yount, 2017).
A minority of our sample reported ever having vaginal sex, ever having anal sex, and two or more lifetime partners. National data on South African adolescent sexual behavior (Shisana et al., 2014) supports this. Reporting ever having vaginal sex and ever having anal sex was associated with IPV among all age groups. Engaging in sex, particularly with multiple partners, introduces, as well as reinforces, social norms within relationships, that could be beneficial (e.g., trust and companionship), but also harmful (e.g., low support of gender equity, sexual expectations and roles). Consumption of alcohol was also associated with IPV among all age groups, and is established in the literature (Davis, Rotheram-Borus, Weichle, Rezai, & Tomlinson, 2017). Consuming alcohol may encourage attendance to alcohol venues (e.g., shebeens), which has been found to be associated with risky behavior (Rosenberg et al., 2015).
Transactional sex and drug use was associated with IPV among the 17- to 20-year olds. The association between transactional sex and IPV is known (Dunkle et al., 2007), but many research findings on the relationship between drug use and IPV report on drug use by the perpetrator rather than the victim. Among the middle and oldest adolescent age groups (ages 15–16, 17–20; in years), using birth control, ever being pregnant, and low support for gender equity were associated with IPV, as noted in the literature, respectively (Alio, Daley, Nana, Duan, & Salihu, 2009; Decker et al., 2014; Mpondo, Ruiter, van den Borne, & Reddy, 2016). Median sexual debut age is 16 years; therefore, the use of birth control and pregnancy could be reflecting sexual activity as the AGYW enter middle adolescence. Among AGYW aged 15 to 16 years, currently living with one or more (up to three) recent sex partners was associated with IPV, suggesting that cohabiting with a partner could place AGYW at an increased risk of IPV.
Our analyses show a low prevalence of IPV risk factors (e.g., ever sex, alcohol use, ever pregnant), but AGYW who experience IPV are more likely to report them. A comprehensive intervention package that addresses multiple risk factors of IPV is needed. To have lasting impact, interventions should be rooted in theories of behavior change and address the social norms that encourage male perpetration of violence (Jewkes, Flood, & Lang, 2015). A review of interventions targeting the reduction of IPV perpetration found that interventions were successful when they were delivered in multiple settings (e.g., both community and with parents), included adults who played a significant role in the life of the adolescent, had a longer duration, and addressed multiple types of violence (De Koker, Mathews, Zuch, Bastien, & Mason-Jones, 2014). As our analysis has shown, physical (both minor and major types) and sexual IPV are experienced by AGYW across the adolescent age spectrum.
Including parental figures in IPV prevention could help both adults and adolescents navigate some of the challenges faced during this time. The innovative U.S.-based intervention, Families for Safe Dates, positively impacted factors related to parental engagement around dating violence issues, showed lower acceptance of dating violence by the adolescent, and a smaller number of adolescents reported dating abuse onset, compared with the control group (Foshee et al., 2012). Exposure to familial violence as a child is a known risk factor for perpetration of IPV as an adult (Abrahams & Jewkes, 2005); therefore, interventions that also address exposure to violence at home may be protective. AGYW just entering adolescence are already experiencing alarming rates of IPV, and interventions with a particular focus on pre- and early adolescence may be beneficial. A recent school-based intervention with early and middle-aged adolescent boys and girls in Kenya demonstrated a reduction in IPV risk among the girls, at the school level. The program utilized a multicomponent curriculum that focused on promoting gender equitable behavior with the boys and empowerment, gender relations, and self-defense training for the girls. There was also a significant increase in reported self-efficacy among the girls, which could have longer lasting positive effects as they build more relationships throughout adolescence and adulthood (Baiocchi et al., 2017).
Limitations
We acknowledge some limitations regarding our study. The data presented in this analysis are cross-sectional; therefore, we cannot make causal conclusions. Our IPV measures do not allow us to pinpoint exact time frames for when the violence occurred in the lifetime of the AGYW. However, we did use a common WHO multicountry study survey tool with standard time periods of measurement (ever and the past 12 months) in our study to best ascertain IPV experienced. Underreporting of IPV is possible and has been noted elsewhere (Palermo, Bleck, & Peterman, 2014). In our study, this could be due to both social desirability and knowing that, if below 18 years, participant-confirmed reports of IPV would be reported to a social worker. However, we attempted to minimize underreporting to the extent possible by the use of the ACASI survey tool in private. To note, some of the AGYW aged 18 years and older were interested in seeking services, even though referral was not mandatory.
Conclusion
The key findings in this study are important as we look to the future of IPV prevention. Intervention efforts should address the experience of IPV among AGYW of all ages, but of note, among younger AGYW in their first relationships. Although our results showed some characteristics were associated with IPV across all age groups, a few, such as drug use, were found to only be significantly associated with certain age groups (in this case, within the oldest AGYW). More research, including longitudinal analysis on IPV among South African AGYW, disaggregated by age, would further elucidate the risk factors and age-specific findings of the current study. Researchers should consider that AGYW as young as 13 years, prior to the median age of sexual debut, are experiencing IPV. Partnering with adolescents and executing theory- and evidence-driven IPV prevention efforts must be considered a top priority.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research and/or authorship of this article: This work was supported by Award Numbers UM1AI068619 (HPTN Leadership and Operations Center), UM1AI068617 (HPTN Statistical and Data Management Center), and UM1AI068613 (HPTN Laboratory Center) from the National Institute of Allergy and Infectious Diseases, the National Institute of Mental Health and the National Institute on Drug Abuse of the National Institutes of Health. This work was also supported by NIMH R01 (R01MH087118), the Carolina Population Center and its NIH Center grant (P2C HD050924) and the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number T32-AI007001 (Stephanie M. DeLong). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Author Biographies
Amanda Selin is a clinical research manager in the Cancer Clinical Trials Office at Stanford University. As project manager for HPTN 068 she led the data acquisition, data collection, and study management of the parent study, and led the conception, data interpretation and writing of this manuscript.
Stephanie M. DeLong is a doctoral candidate in the Department of Epidemiology at the University of North Carolina at Chapel Hill. Her research focuses on gender-based violence experienced by adolescents and young adults both internationally and domestically.
Aimée Julien is a Public Health researcher formerly affiliated with the University of North Carolina and the MRC/Wits Rural Public Health and Health Transitions Research Unit (Agincourt) as the Monitoring & Evaluation Manager for the HPT068 trial. She was involved in data acquisition, data collection, and study management of HPTN 068, and contributed to the conception, data interpretation and writing of this manuscript. She is currently pursuing PhD studies in Epidemiology at the University of Antwerp in Belgium.
Catherine MacPhail is a senior lecturer in the School of Health and Society, University of Wollongong, NSW, Australia. She is a qualitative researcher interested in understanding the impact of social structures and contexts on health. In particular, she is interested in the social determinants of health and how factors such as poverty, education, race/ethnicity and gender impact on health and access to health care, particularly for marginalised populations. MacPhail has expertise in HIV prevention and interventions focused on structural determinants of HIV risk among adolescents in sub-Saharan Africa and domestic violence in Australia.
Rhian Twine has worked for 30 years in rural areas in South Africa, specifically 13 years working in the field of community engagement in research. During this time she has been involved in projects that required her to work in the community, rather than in an institution, allowing her a deep understanding of this society, its organisation, its challenges and its progress over the past 25 years. She has worked for the MRC/Wits Rural Public Health and Health Transitions Research Unit (Agincourt) since 2004, focusing on developing strong links with the host community since a relationship of trust, respect and mutual fair benefit is essential to conducting longitudinal research in any one community.
James P. Hughes received an MS in Biomath in 1980 and a PhD in Statistics in 1993, both from UW. He joined the UW Biostatistics department in 1993 and is currently a Professor of Biostatistics at the UW and Full Member of the FHCRC Vaccine and Infectious Diseases Division. Hughes works primarily in the area of HIV/AIDS and sexually transmitted infections and is the principle investigator of the UW based Statistical Methods in AIDS Research grant. He is lead statistician on several HIV prevention trials through the HIV Prevention Trials Network.
Yaw Agyei is a senior International Laboratory Coordinator with more than twenty years’ experience in the field of clinical laboratory medicine. The past fifteen years have been spent in sub-Saharan Africa to assist labs in building capacity to perform HIV related prevention and treatment research.
Erica L. Hamilton has provided programmatic and technical support for clinical research protocols with FHI 360 for more than seven years. Currently, she is a Clinical Research Manager with the HIV Prevention Trials Network (HPTN), where she is a valued team member on various clinical research trials and manages the HPTN Scholars Program, a mentored scholarship for early-career domestic and international investigators interested in HIV prevention research. Ms. Hamilton earned her MPH in Maternal and Child Health and completed the Global Health Certificate at the University of North Carolina at Chapel Hill.
Kathleen Kahn is a professor in the School of Public Health, University of the Witwatersrand. She is a medical doctor with a PhD in public health and epidemiology, and a senior public and population health scientist with 25 years working in rural South Africa. Kahn has jointly led the MRC/Wits Rural Public Health and Health Transitions Research Unit (Agincourt), an internationally recognized research centre, and its health and socio-demographic surveillance system, since its inception in 1992. She is site-PI of the NIH R01/HPTN 068 trial, an RCT to determine the effect on HIV incidence of cash transfers to young women and their families conditional on school attendance.
Audrey Pettifor is a professor of epidemiology at the University of North Carolina at Chapel Hill. Her research focuses on sexual behavior and determinants of HIV/STI infection in sub-Saharan Africa. Pettifor has expertise in sexual behavior, HIV prevention, HIV testing and structural interventions among adolescents and young adults in sub-Saharan Africa, and has published extensively in the area of HIV and sexual behavior among youth in sub-Saharan Africa.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abrahams N, & Jewkes R (2005). Effects of South African men’s having witnessed abuse of their mothers during childhood on their levels of violence in adulthood. American Journal of Public Health, 95, 1811–1816. doi: 10.2105/AJPH.2003.035006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alio AP, Daley EM, Nana PN, Duan J, & Salihu HM (2009). Intimate partner violence and contraception use among women in sub-Saharan Africa. International Journal of Gynecology & Obstetrics, 107, 35–38. doi: 10.1016/j.ijgo.2009.05.002 [DOI] [PubMed] [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55, 469–480. [PubMed] [Google Scholar]
- Baiocchi M, Omondi B, Langat N, Boothroyd DB, Sinclair J, Pavia L, … Sarnquist C (2017). A behavior-based intervention that prevents sexual assault: The results of a matchedpairs, cluster-randomized study in Nairobi, Kenya. Prevention Science, 18, 818–827. doi: 10.1007/s11121-016-0701-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crone EA, & Dahl RE (2012). Understanding adolescence as a period of social-affective engagement and goal flexibility. Nature Reviews Neuroscience, 13, 636–650. doi: 10.1038/nrn3313 [DOI] [PubMed] [Google Scholar]
- Curtis AC (2015). Defining adolescence. Journal of Adolescent and Family Health, 7(2), Article 2. [Google Scholar]
- Davis EC, Rotheram-Borus MJ, Weichle TW, Rezai R, & Tomlinson M (2017). Patterns of alcohol abuse, depression, and intimate partner violence among township mothers in South Africa over 5 years. AIDS and Behavior, 21(Suppl. 2), 174–182. doi: 10.1007/s10461-017-1927-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker MR, Peitzmeier S, Olumide A, Acharya R, Ojengbede O, Covarrubias L, … Brahmbhatt H (2014). Prevalence and health impact of intimate partner violence and non-partner sexual violence among female adolescents aged 15–19 years in vulnerable urban environments: A multi-country study. Journal of Adolescent Health, 55(Suppl. 6), S58–S67. doi: 10.1016/j.jadohealth.2014.08.022 [DOI] [PubMed] [Google Scholar]
- De Koker P, Mathews C, Zuch M, Bastien S, & Mason-Jones AJ (2014). A systematic review of interventions for preventing adolescent intimate partner violence. Journal of Adolescent Health, 54, 3–13. doi: 10.1016/j.jadohealth.2013.08.008 [DOI] [PubMed] [Google Scholar]
- Dunkle KL, Jewkes R, Nduna M, Jama N, Levin J, Sikweyiya Y, & Koss MP (2007). Transactional sex with casual and main partners among young South African men in the rural Eastern Cape: Prevalence, predictors, and associations with gender-based violence. Social Science & Medicine, 65, 1235–1248. doi: 10.1016/j.socscimed.2007.04.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foshee VA, McNaughton Reyes HL, Ennett ST, Cance JD, Bauman KE, & Bowling JM (2012). Assessing the effects of families for safe dates, a family-based teen dating abuse prevention program. Journal of Adolescent Health, 51, 349–356. doi: 10.1016/j.jadohealth.2011.12.029 [DOI] [PubMed] [Google Scholar]
- García-Moreno C, Jansen HAFM, Ellsberg M, Heise L, & Watt C (2005). WHO multi-country study on women’s health and domestic violence against women: Summary report of initial results on prevalence, health outcomes and women’s responses Geneva: World Health Organization. [Google Scholar]
- García-Moreno C, Pallitto C, Devries K, Stöckl H, Watts C, & Abrahams N (2013). Global and regional estimates of violence against women: Prevalence and health effects of intimate partner violence and non-partner sexual violence Geneva: World Health Organization. [Google Scholar]
- Jewkes R (2002). Intimate partner violence: Causes and prevention. The Lancet, 359, 1423–1429. doi: 10.1016/S0140-6736(02)08357-5 [DOI] [PubMed] [Google Scholar]
- Jewkes R, Flood M, & Lang J (2015). From work with men and boys to changes of social norms and reduction of inequities in gender relations: A conceptual shift in prevention of violence against women and girls. The Lancet, 385, 1580–1589. doi: 10.1016/S0140-6736(14)61683-4 [DOI] [PubMed] [Google Scholar]
- Kahn K, Collinson MA, Gomez-Olive FX, Mokoena O, Twine R, Mee P, …Tollman SM (2012). Profile: Agincourt health and socio-demographic surveillance system. International Journal of Epidemiology, 41, 988–1001. doi: 10.1093/ije/dys115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mpondo F, Ruiter RA, van den Borne B, & Reddy PS (2016). Intimate partner violence and its association with self-determination needs and gender-power constructs among rural South African women. Journal of Interpersonal Violence Advance online publication. doi: 10.1177/0886260516664316 [DOI] [PubMed]
- Muthengi E, Gitau T, & Austrian K (2016). Is working risky or protective for married adolescent girls in urban slums in Kenya? Understanding the association between working status, savings and intimate partner violence. PLoS ONE, 11(5), e0155988. doi: 10.1371/journal.pone.0155988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T, Bleck J, & Peterman A (2014). Tip of the iceberg: Reporting and gender-based violence in developing countries. American Journal of Epidemiology, 179, 602–612. doi: 10.1093/aje/kwt295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterman A, Pereira A, Bleck J, Palermo TM, & Yount KM (2017). Women’s individual asset ownership and experience of intimate partner violence: Evidence from 28 international surveys. American Journal of Public Health, 107, 747–755. doi: 10.2105/AJPH.2017.303694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettifor A, MacPhail C, Hughes JP, Selin A, Wang J, Gomez-Olive FX, … Kahn K (2016). The effect of a conditional cash transfer on HIV incidence in young women in rural South Africa (HPTN 068): A Phase 3, randomised controlled trial. The Lancet Global Health, 4(12), e978–e988. doi: 10.1016/S2214-109X(16)30253-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettifor A, MacPhail C, Selin A, Gomez-Olive FX, Rosenberg M, Wagner RG, … The HPTN 068 Protocol Team. (2016). HPTN 068: A randomized control trial of a conditional cash transfer to reduce HIV infection in young women in South Africa—Study design and baseline results. AIDS and Behavior, 20, 1863–1882. doi: 10.1007/s10461-015-1270-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M, Pettifor A, Van Rie A, Thirumurthy H, Emch M, Miller WC, … Kahn K (2015). The relationship between alcohol outlets, HIV risk behavior, and HSV-2 infection among South African young women: A cross-sectional study. PLoS ONE, 10(5), e0125510. doi: 10.1371/journal.pone.0125510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfield RL, Lipton RB, & Drum ML (2009). Thelarche, pubarche, and menarche attainment in children with normal and elevated body mass index. Pediatrics, 123, 84–88. doi: 10.1542/peds.2008-0146 [DOI] [PubMed] [Google Scholar]
- Russell M, Cupp PK, Jewkes RK, Gevers A, Mathews C, LeFleur-Bellerose C, & Small J (2014). Intimate partner violence among adolescents in Cape Town, South Africa. Prevention Science, 15, 283–295. doi: 10.1007/s11121-013-0405-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer SM, Azzopardi PS, Wickremarathne D, & Patton GC (2018). The age of adolescence. Lancet Child & Adolescent Health, 2, 223–228. doi: 10.1016/S2352-4642(18)30022-1 [DOI] [PubMed] [Google Scholar]
- Sennott C, & Mojola SA (2017). “Behaving well”: The transition to respectable womanhood in rural South Africa. Culture, Health & Sexuality, 19, 781–795. doi: 10.1080/13691058.2016.1262062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shamu S, Gevers A, Mahlangu BP, Jama Shai PN, Chirwa ED, & Jewkes RK (2016). Prevalence and risk factors for intimate partner violence among Grade 8 learners in urban South Africa: Baseline analysis from the Skhokho Supporting Success cluster randomised controlled trial. International Health, 8, 18–26. doi: 10.1093/inthealth/ihv068 [DOI] [PubMed] [Google Scholar]
- Shisana O, Rehle T, Simbayi LC, Zuma K, Jooste S, Zungu N, … Onoya D (2014). South African national HIV prevalence, incidence and behaviour survey, 2012 Retrieved from http://www.hsrc.ac.za/en/research-data/view/6871 [DOI] [PubMed]
- Statistics South Africa. (2017). South Africa demographic and health survey 2016: Key indicator report Retrieved from https://dhsprogram.com/pubs/pdf/PR84/PR84.pdf
- Teipel K (2003a). Understanding adolescence: Early adolescence Minneapolis: Konopka Institute, University of Minnesota. [Google Scholar]
- Teipel K (2003b). Understanding adolescence: Late adolescence Minneapolis: Konopka Institute, University of Minnesota. [Google Scholar]
- Teipel K (2003c). Understanding adolescence: Middle adolescence Minneapolis: Konopka Institute, University of Minnesota. [Google Scholar]
- Zembe YZ, Townsend L, Thorson A, Silberschmidt M, & Ekstrom AM (2015). Intimate partner violence, relationship power inequity and the role of sexual and social risk factors in the production of violence among young women who have multiple sexual partners in a peri-urban setting in South Africa. PLoS ONE, 10(11), e0139430. doi: 10.1371/journal.pone.0139430 [DOI] [PMC free article] [PubMed] [Google Scholar]