Abstract
Background:
Precision health calls for collecting and analyzing large amounts of data to capture an individual’s unique behavior, lifestyle, genetics, and environmental context. The diffusion of digital tools has led to a significant growth of patient generated health data (PGHD), defined as health-related data created, gathered or inferred by or from patients and for which the patient controls data collection and data sharing.
Purpose:
We assessed the current evidence of the impact of PGHD use in clinical practice and provide recommendations for the formal integration of PGHD in clinical care.
Methods:
We searched PubMed, Ovid, Embase, CINAHL, Web of Science, and Scopus up to May 2018. Inclusion criteria were applied and four reviewers screened titles and abstracts and consequently full articles.
Findings:
Our systematic literature review identified 21 studies that examined the use of PGHD in clinical settings. Integration of PGHD into electronic records was extremely limited, and decision support capabilities were for the most part basic.
Discussion:
PGHD and other types of patient-reported data will be part of the health care system narrative and we must continue efforts to understand its impact on health outcomes, costs, and patient satisfaction. Nursing scientists need to lead the process of defining the role of PGHD in the era of precision health.
INTRODUCTION
Precision health calls for collecting and analyzing large amounts of data to capture an individual’s unique behavior, lifestyle, genetics, and environmental context to inform tailored and personalized delivery of health services (Akdis & Ballas, 2016). The growth of consumer technologies including smartphone apps and wearables has led to the design and use of tools that allow individual consumers to collect their own health related data. Such data pertain to their well-being and behavioral patterns as well as the environment in which they find themselves. In the US, 46% of consumers in 2016 were considered active digital health adopters, having used 3 or more categories of digital health tools (A. Adams, Shankar, & Tecco, 2016). Nearly a third of people who downloaded a health app did so because the app was recommended by their doctor and nearly a quarter of Americans owned a wearable device such as an activity tracker in 2016, up from 12% in 2015 (A. Adams et al., 2016).
The implementation of digital tools has led to a significant growth of so-called patient generated health data (PGHD). PGHD are defined by the Office of the National Coordinator for Health Information Technology (ONC) as “health-related data including health history, symptoms, biometric data, treatment history, lifestyle choices, and other information-created, recorded, gathered or inferred by or from patients or their designees” (Shapiro, Johnston, Wald, & Mon, 2012). This definition emphasizes that patients, not providers, are primarily responsible for capturing or recording these data and it is patients who direct the sharing or distributing of the data to stakeholders (Shapiro et al., 2012). PGHD from self-tracking has been envisioned as a means to bridge a gap, supplementing data from clinical visits, with a rich picture of a person’s daily behaviors, environment and lifestyle. This approach has the potential to inform better clinical decision making, with patients engaged in the decision-making process (Shapiro et al., 2012). PGHD tools are perceived as ways to capture and even “amplify” the patient voice in the health care system and strengthen the patient-provider relationship, increasing patient safety and information access (National eHealth Collaborative, 2013).
Patients may utilize a broad spectrum of platforms to capture such data (ranging from paper-based tools to wearable or implantable devices). Similarly, such platforms may have varying degrees of sophistication in how data are handled and analyzed. For example, the platforms may include alerts for individual data points, predictive analytics, natural language processing or artificial intelligence. The data may also be communicated and shared in numerous ways including integration into the patient’s record, graphical, text- or audio-based summaries that can be shared with clinicians and others. The use of information technology for capturing and transmitting PGHD allows for the generation of new types of data that can now be generated outside of a clinical setting without sole reliance on self-report. These might include data related to overall physical activity, mobility, sleep quality, nutrition, social interactions, water and air quality. Table 1 showcases the breadth of PGHD types and sources as well as potential tools to capture such data.
Table 1.
Range of PGHD types and sources
| Data Type | Data Element Examples | Modality for Data Capturing Examples |
|---|---|---|
| Personal profile | Life goals, values | Online/patient portal (Kneale, Choi, & Demiris, 2016) |
| Preferences | Notifications | |
| Communication | ||
| Delegation or identification of proxy | ||
| Health data review | Edits/ updates to health record data (e.g. list of allergies) | |
| Health and family history | Updates to personal and family health history and health events | |
| Medication information | Updates to over the counter medication | |
| Medication adherence | Connected medication dispensing unit (Brath et al., 2013; Forni Ogna et al., 2013) | |
| Biometric tracking | Blood pressure | Wireless blood pressure cuff/Bluetooth to Smartphone application (Ciemins et al., 2018; Evans et al., 2016) |
| Weight | Digital weight scale (Demiris et al., 2013) | |
| Body temperature | Digital thermometer (Ask, Ekstrand, Hult, Lindén, & Pettersson, 2012) | |
| Oxygen saturation | Wireless pulse oximeter (Velardo et al., 2017) | |
| Blood glucose level | Digital glucose monitor (Lee et al., 2017) | |
| Lung function | Digital spirometer (Shakkottai, Kaciroti, Kasmikha, & Nasr, 2018) | |
| Heart rate | Wrist-worn activity tracking device (Thiebaud et al., 2018) | |
| Behavioral tracking | Activity level | Pedometer watch/Accelerometer (Actigraph) (Hooke, Gilchrist, Tanner, Hart, & Withycombe, 2016; Joseph, Stromback, Hagstromer, & Conradsson, 2018) |
| Calorie burning | Fitness tracker with calorie burning calculator (Franco, Fallaize, Lovegrove, & Hwang, 2016) | |
| Sleep quality | Bed sensor strip with ballistocardiography sensor (Kortelainen, van Gils, & Pärkkä, 2012) | |
| Daily hygiene routine | Water sensors, motion sensors (J. Chung et al., 2017) | |
| Environmental tracking | Room temperature | Temperature sensor (Bock et al., 2016) |
| Noise | Indoor sound level sensor (Risojević , Rozman, Pilipović, Češnovar, & Bulić, 2018) | |
| Luminosity | Home digital luminosity sensor (Bock et al., 2016) | |
| Humidity | Indoor air quality sensor (Bock et al., 2016) | |
| Social interactions tracking | Number of visitors | Door sensor (Skubic, Guevara, & Rantz, 2015) |
| Time spent outside the home | ||
| Number of calls | Phone usage summary app (Deave et al., 2018) | |
| Time spent online | Online monitoring app (Chen & Schulz, 2016) | |
| Genetic information | Predictive and pre-symptomatic testing | Direct to consumer genetic testing kit |
| Mental health assessment | Screening for depression | Online/patient portal (Leveille, Huang, Tsai, Weingart, & Iezzoni, 2008) |
| Anxiety assessment | Smartphone app (Alyami, Giri, Alyami, & Sundram, 2017) | |
| Symptom tracking | Symptom frequency, intensity, side effects | Online/patient portal (Kneale et al., 2016) |
| Patient reported outcomes | Condition-specific outcomes, quality of life | Online/patient-portal (Kneale et al., 2016) |
| Multimedia observations | Video- or photo-recordings | Telehealth video-camera (Gunter et al., 2016) |
| Care goals | Patient review of healthcare team goals | Personal health record (Lum et al., 2019) |
| Patient experience | Patient satisfaction | Online/patient-portal (Kneale et al., 2016) |
| Legal documentation | Advanced directive | Paper-based/ online (Lum et al., 2019) |
| Ad hoc requests | Request for health data amendment | Online/patient-portal (Kneale et al., 2016) |
| Administrative data | Contact information, caregiver(s) |
The use of PGHD can have utility for patients across the lifespan and in various conditions. PGHD systems have been designed for pediatric patients (W. Adams et al., 2003; Barrett et al., 2018; Johansen et al., 2004; Miller et al., 2016), students (Lau et al., 2013), adults, and older adult patients (Quinn et al., 2008b). In regards to age and gender, researchers in one study found significantly greater use of an app that supported the upload of continuous health data for health management (e.g., blood pressure, blood glucose, weight) among older users (P<.001) and men (P<.001) (Y. Park et al., 2018). Similarly, PGHD have been used to monitor and manage a spectrum of diseases and conditions. For example, PGHD have been used for cancer (Basch et al., 2007; A. E. Chung & Basch, 2015a; Holch et al., 2017), stress and sleep in physically active adults (Peake, Kerr, & Sullivan, 2018a), CVD and metabolic syndrome (Y. Park et al., 2018), asthma (W. Adams et al., 2003; Barrett et al., 2018), diabetes (Albisser, En Chao, Parson, & Sperlich, 2001), depression and anxiety (Bauer et al., 2018), lung transplant care (Jiang, Sereika, DeVito Dabbs, Handler, & Schlenk, 2016), and uncontrolled blood pressure (Lv et al., 2017).
While opportunities have been identified in integrating PGHD into clinical workflow and care management, there are also identified concerns. Health care providers have expressed concerns over the potential added burden of reviewing PGHD outweighing any potential for added efficiencies (Shapiro et al., 2012). In a simulation study to understand changes to a health system with adding PGHD, researchers identified indirect consequences of additional time and cognitive demand, increase in labor cost with additional time required to assimilate PGHD (D. A. Steward, R.A. Hofler, C. Thaldorf, & D. E. Milov, 2010). Specifically, workday and patient visits were extended in duration and became less predictable to schedule, with nurse utilization rates of the PGHD system increasing over time while physicians’ utilization rates remained relatively unchanged. Authors concluded that the impact of PGHD is nontrivial and would cause longer workdays or mandate sacrifice of other activities. Other concerns include whether the data will be usable and of high enough quality to support decision making, what the financial impact may be, and whether there may be potential liability concerns (A. E. Chung & Basch, 2015a). For individuals unable to track PGHD based on disease make-up, access to devices, or medical coverage, for example, there are concerns about creating or contributing to inequities. Furthermore, questions remain about determining content and frequency that would be most helpful. Concerns of accuracy and completeness of PGHD have been identified (Weissmann, Mueller, Messinger, Parkin, & Amann-Zalan, 2016). Clinicians may have reservations in utilizing PGHD in their clinical decision making as such data sets may be new and unfamiliar source of information. In one study many patients who shared self-tracking data with their providers expressed their dissatisfaction with the level of provider engagement with these data (C. Chung et al., 2016).
Despite these concerns, some health systems are moving forward with efforts to use PGHD to improve care. For example, the US Department of Veterans Affairs is striving to implement the enterprise-wide capability to collect and use PGHD in order to improve the patient healthcare experience, and promote shared decision making (S. Woods, N. Evans, & K. Frisbee, 2016). To date evidence of the effectiveness of integrating PGHD into clinical settings may be limited and many questions still remain, such as: How can we integrate patient generated data into the electronic health record? What strategies can be pursued to effectively mine and analyze these data to support clinical decision-making? What are the barriers and challenges in the integration of patient generated data into health information systems? How can we facilitate patient engagement and empowerment while addressing ethical concerns associated with the use of pervasive and ubiquitous monitoring? The purpose of this paper is to assess the current evidence of the impact of PGHD use in clinical practice and/or the use of PGHD for clinical decision making (e.g., for diagnosis, treatment, monitoring, or management) and discuss opportunities and challenges associated with the formal integration of PGHD in clinical care.
METHODS
We conducted a systematic literature review to examine the use of PGHD in clinical practice. We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009).
Search Strategy
We searched PubMed, Ovid, Embase, CINAHL, Web of Science, and Scopus. We started to search the MeSH term, “Patient Generated Health Data.” Because it was newly introduced in 2018 as MeSH, only few articles were identified. To identify all relevant studies, we added several keywords and those synonyms. First of all, we entered keywords such as “patient”, “person”, “peer”, and “caregiver” to expand targets who can create, record, and gather data. Also, we put common data capturing modalities (e.g. self-tracking, wearable, mobile health, and m-health). Moreover, we included “patient reported outcome (PRO) as a common form of PGHD. All keywords and synonyms related to patient-generated health data and decision making were searched in May 2018. Table 2 outlines our search strategy which was finalized after review by a Health Sciences librarian. We were broadly inclusive of digital or paper as the means of self-tracking, but limited to articles in English, human participants, and articles in which full-text was available (but not constrained to free article access). We augmented this search with 11 papers known to us but not returned by keyword search.
Table 2.
Search strategy outline
| Search Terms | Combination | |||
|---|---|---|---|---|
| Search Terms | Combination | |||
| “patient generated health data”[Mesh] | OR | OR | OR | |
| “patient generated health data” | ||||
| “patient-generated health data” | ||||
| “patient generated health information” | OR | |||
| “patient-generated health information” | ||||
| “patient generated data” | OR | |||
| “patient-generated data” | ||||
| “patient generated” | OR | OR | AND | |
| “patient-generated” | ||||
| “person generated” | OR | |||
| “person-generated” | ||||
| “caregiver generated” | OR | |||
| “caregiver-generated” | ||||
| “peer generated” | OR | |||
| “peer-generated” | ||||
| “data” or “information” | ||||
| “patient reported outcome measures”[Mesh] | OR | |||
| “patient reported” | ||||
| “patient-reported” | ||||
| “self tracking” | OR | |||
| “self-tracking” | ||||
| “body-worn sensor*” | ||||
| wearable | ||||
| smartphone* | OR | |||
| mhealth | ||||
| “mobile health” | ||||
| “personal health record” | ||||
| Combine all above and below with “AND” | ||||
| “clinical decision making” | OR | |||
| “clinical decision-making” | ||||
| “medical decision making” | ||||
| “medical decision-making” | ||||
Selection Criteria
Given the focus of this review on actual PGHD use for clinical decision making in a clinical setting (unlike use of PGHD for the sole purpose of collecting data for a research protocol or without involvement of clinicians), inclusion was based on three main criteria: (1) The article must have been peer reviewed, and represent empirical work (data, whether qualitative or quantitative, collected as part of the study and reported in the article). This excluded opinion papers, vision statements, literature surveys, and similar pieces. It also excluded a number of papers discussing PGHD issues, and papers describing the architecture of particular systems or apps. Articles in which the data were simulated or fabricated for test purposes were also excluded. (2) We adhered to the ONC definition of PGHD, requiring that the patient initiate data collection and control data sharing. This excluded clinician-initiated data collection such as clinical tele-monitoring and most implantable devices, because in those cases the patient did not control data collection or data sharing. Patient-reported outcomes were commonly reported but most were excluded from this review because the data were retrospective and gathered at a fixed schedule mandated by the research study protocol (patients did not control the “self-monitoring” process). (3) The self-monitoring data had to have been used for clinical decision making or during a patient-clinician encounter. This excluded social media groups and online discussion forums, which typically focused on peer-to-peer interactions, and platforms for self-improvement or self-reflection.
We used the Covidence systematic review software (Veritas Health Innovation LtD, Melbourne, Australia) to manage the review process. The software automatically removed duplicates. We required that at least two people from our team review the title and abstract for each article. When there were conflicts, we resolved those by a third person vote or, if the third person was also uncertain, used group discussion to reconcile the conflicts. We used a similar process for full text screening, allowing one person to vote to retain an article but requiring at least two for article exclusion, with group discussion to resolve conflicts.
Analysis
Papers were read in full by members of the research team to identify and tabulate features of the studies (such as design and sample). All papers were read by at least two team members. Two team members derived themes to describe the tabulated findings. The themes were reviewed and refined by all team members.
RESULTS
The original keyword search returned 7994 articles and screening and review of text resulted in a final 21 articles that were included in the review. Figure 1 shows our PRISMA diagram and includes the primary reason for exclusion for the articles in which full text was reviewed. In the larger set of articles, we eliminated 1256 duplicates. Most of the articles in the abstract/title search were excluded because of not meeting the PGHD definition used in this study, including more than 200 articles that included formal or informal patient-reported outcomes (but missing some element, most commonly not meeting the requirement that patient/participant controlled the timing of data collection or the decision about whether to share the data). Similarly, the most common reason for excluding studies of sensors was lack of information about whether the patient had any control over the data collection or sharing. Other common reasons for exclusion were that the study did not include actual participant data (e.g., fabricated data sets, or description of architecture without actual data collection). There was only 1 article excluded for not being English-language, however the English-language abstract for that article appeared not to meet the PGHD definition. There were no articles that were excluded on the basis of full-text being unavailable.
Figure 1.
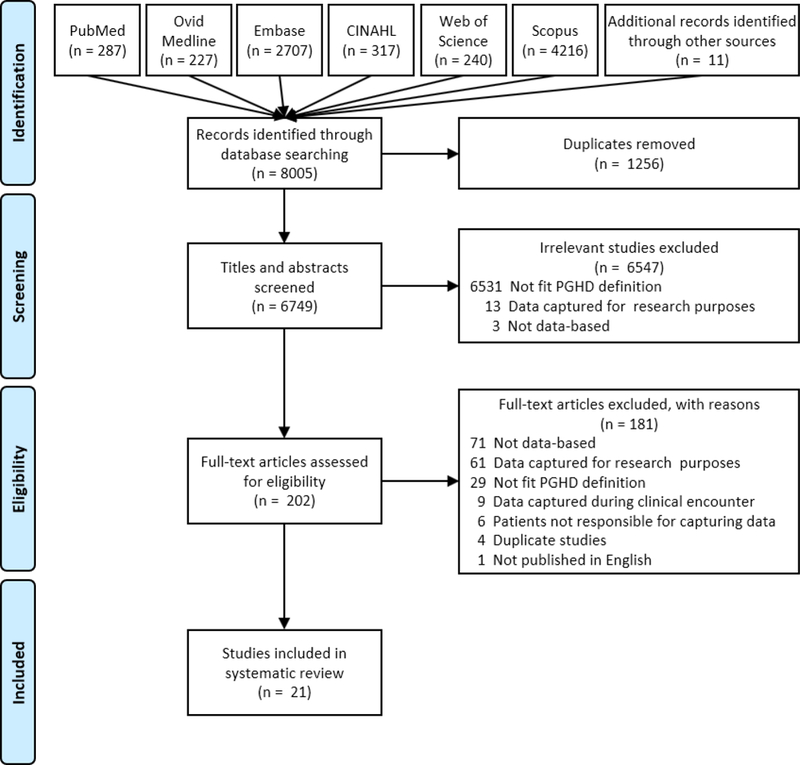
PRISMA diagram
We found that, while there are articles discussing the vision or need for PGHD in clinical care (at least 40), and more than 200 articles describing data collected from patients or caregivers, empirical research meeting the ONC definition of PGHD was scarce. Table 3 summarizes the final 21 articles. Publication dates for the articles ranged from 2001 to 2018. An initial slow start (less than 1 article per year) was followed by increasing number of articles starting in 2016. As shown in Table 3, study locations included USA, UK/Europe, Australia, and Asia, with location not specified for 2 studies. Participant ages covered the lifespan from pediatrics to older adults. Studies examined a wide variety of conditions and symptom foci (see Table 3).
Table 3.
Description of the included studies
| Reference | Overview | Study/System | Findings |
|---|---|---|---|
| Adams et al. (2003) | Model information system that integrates patient health information to support monitoring and care of children with persistent asthma Focus: asthma Location: USA |
Study: Feasibility/proof of concept. Ages: children and adults (parents) N = unreported System: telephone-linked communication (TLC-Asthma) with symptom monitoring and automated phone-based education, web-based alert and nurse case-management, EHR (Epic) communications |
Monitoring includes severity-treatment mismatch, use of peak flow meter, changes in symptom frequency or severity. Level 1 alerts: patient advised to seek care immediately, fax sent to dedicated line and phone call to clinic personnel. Level 2 alerts recorded to a log and reviewed by nurse |
| Albisser et al. (2001) | Glucose clamping algorithm for patient use (clamping defined as efforts to maintain glucose in a specified range through glucose or insulin administration). Focus: diabetes Location: unspecified |
Study: described by authors as “system beta testing” Ages: not specified, presumably adult N = 142 patients for 1 year (approx. 100,000 messages) System: Data entry via touch tone phone/voice response hardware (HumaLink). |
Clinical outcomes improved (rate of hyperglycemia, hypoglycemia, or symptoms; and Hemoglobin A1c level). |
| Andy et al. (2012) | Personal health record for diabetes care, based on American Association of Diabetes Educators guidelines. Focus: diabetes Location: Asia (Taiwan) |
Study: developmental evaluation. (Described as randomized but not reported as such) Data collected are application feedback, outcomes monitoring, usage Ages: not specified, presumably adult N= 61 (36 intervention, 25 control) System: Un-named; Web based app + unspecified interaction with care managers. Generates HL7 Continuity of Care Document (CCD). |
Decreased HbA1C in intervention group (66% of patients vs 40% in control group) |
| Barrett et al. (2018) | Study of AIR Louisville, a public health collaboration to improve asthma Focus: asthma Location: USA |
Study: Pragmatic single arm, interventional (CBPR) Ages: adults and children N=497 Electronic sensors to monitor medication usage (Propeller Health). FDA-approved system includes inhaler sensors, digital health platform. Also did environmental monitoring. |
78 percent reduction in rescue inhaler use and a 48 percent improvement in symptom-free days |
| Basch et al. (2007) | Monitoring symptoms of chemo toxicity in lung cancer patients (eRapid; study-specific system) Focus: cancer Location: USA |
Study: Prospective observational study. Ages: adults N= 124 enrolled. Interviews with 13 patients, 9 advocates, 19 staff. System was self-reported via questionnaires and based on NCI Common Terminology Criteria for Adverse Events (CTCAE), mandated reporting for NCI-funded studies |
Targeted advice based on national guidelines. Self-reporting found to be feasible. Patients could use system on their own but seldom used system between visits, unless prompted by explicit reminders or clinician feedback. |
| Bauer et al. (2018) | Testing the feasibility and acceptability of a mobile health platform (patient-facing smartphone application) supporting collaborative care for patients with depressive and anxiety disorder. Focus: depression/anxiety Location: USA |
Study: mixed method pilot study (4-week study period) Ages: adult N = 17. System: The platform supports the transmission of patient data to care manager via an online dashboard. Smartphone sensor data were also collected, mainly about patients’ movement and communication. The dashboard offered providers an overview of patient basic information and graphing of patients’ report of their mood and symptoms. |
Only 6 participants retained in the study, 15 completed weekly reports with a lower response rate on daily measures (i.e. medication use). |
| Holch et al. (2017) | Describing the development of eRAPID (electronic patient self-Reporting of Adverse-events: Patient Information and aDvice) for cancer patients to self-report and manage significant adverse events during and after cancer treatment. Focus: cancer Location: UK |
Study: Usability and functionality Ages: adult N = 13 patients, 9 advocates, 19 staff System: the eRAPID system. Algorithms imbedded in the system allows patients to receive tailored advice for low to moderate adverse events or contact hospital for severe adverse events. Integrated with electronic record at Leeds Teaching Hospital |
The eRAPID system allows patients to report adverse events and guide patients to better manage these events. |
| Hsu et al. (2016) | Examining the effects of a cloud based diabetes management system on glycemic control as compared to control group receiving standard care among patients with type 2 diabetes. Focus: diabetes Location: USA |
Study: Randomized controlled trial Ages: adult N = 40 System: Patients with type 2 diabetes starting basal insulin therapy, who were in the intervention group, received a cloud-based diabetes management program for communication, collaboration and decision making between patients and healthcare providers. Control group = usual care |
Patients in the intervention group achieved a better hemoglobin A1c control and satisfaction than those in the control group. |
| Jiang et al. (2016) | Describing factors associated with usage of advice from a mobile health application among lung transplant patients. Focus: transplant Location: USA |
Study: cross-sectional study examining app usage, extent to which recommendations are followed, as well as predictors of usage and following recommendations. Ages: adult N = 96 System: mobile health app called Pocket PATH for daily health self-monitoring; system generated suggestions. |
Patients with moderate use of Pocket PATH were less likely to follow system recommendations than high or low users. Usage of recommendations from system were associated with gender, past experience with technology, income, hospital stay, and self-monitoring frequency among lung transplant patients. |
| Johansen et al. (2004) | Parents of burns patients are involved in patient care by capturing suitable pictures without intensive training and cost. Focus: burns Location: Australia |
Study: Feasibility study Ages: pediatric burn patients, study enrolled parents N=4 System: email, cell phone camera. Study examined extent to which parents of burns patients can take clinically suitable pictures for follow-up communication with healthcare providers via email. |
Low-resolution images were satisfactory for diagnosis and email messages from parents were adequate for clinical decision making. Parents reported the easiness and convenience of taking photographs. |
| Lau et al. (2013) | Personally controlled health management systems (PCHMSs) with social and self-reflective features were designed to support self-maintaining and self-management of physical and emotional well-being. Focus: physical and emotional well-being Location: Australia |
Study: single-group pre/post study over 4 months Ages: university students and staff N= 709 System: Personally controlled health management systems (PCHMSs) with social and self-reflective features. Study examined how students used the features. |
Social features were considered most engaging. Self-reflective feature (i.e. diary) was associated with higher levels of professional health seeking behaviors. |
| Lindroth et al. (2018) | Describing how patient generated data via mobile apps were used by nurses and how these data transformed patient care. Focus: cancer Location: Europe (Sweden) |
Study: case study Ages: adult N = 10 System: mobile app developed for the study |
Patient generated data introduces changes in communication and decision-making between patients and nurses by providing more precise descriptions of health problems. |
| Lv et al. (2017) | EMPOWER-H that enables capture of home blood pressure (BP) data via a smartphone. Focus: hypertension Location: USA |
Study: pre-post study Ages: adult N = 149 EMPOWER-H is an interactive Web-based disease management system integrated with the electronic health record. Study explored how home BP data gendered by patients with uncontrolled BP influenced clinical decision making. |
EMPOWER-H significantly improved the usage of patients’ office-measured and home-monitored BP in patient care. |
| Marceau et al. (2010) | Describing the experiences of using electronic diaries with summary feedback in the care of patients with chronic pain. Focus: pain Location: USA |
Study: described as 10-month follow up study Ages: adult N = 134 Study: electronic diaries with feedback or paper diaries without feedback- to monitor and manage pain. |
About 23% of patients reported electronic diaries improved care. About 77% of participants reported satisfaction with the app. |
| Martinez et al. (2017) | Describing diabetic patients’ and clinicians’ experiences of using the CONDUIT-HID for the management of BP. Focus: diabetes, hypertension Location: unspecified |
Study: qualitative interview Ages: presumably adult N = 21 patients, 5 clinicians System: CONDUIT-HID Patients can upload BP data into HealthVault (personal health record) via internet; Patients have choices to allow HealthVault to send their data to Reliant Medical Group’s EHR via HL7; protocol driven feedback loop was used to adjust medications if BP was not controlled; nurses can schedule phone calls with patients between office visits when alerts were triggered. |
System that supports users’ workflow and minimizes users’ cognitive efforts is important for the successful adoption. |
| Miller et al. (2016) | Describing the use of digital images captured by parents of pediatric patients receiving ambulatory surgery. Focus: post surgical wound healing Location: USA |
Study: retrospective chart review Ages: pediatric patients age 0 – 17years (parents enrolled) N = 166 enrolled, 129 included System: cell phone camera, email A structured review of the electronic health record was conducted to explore how the digital images of post-operative wounds taken by parents of pediatric patients were used in the patient care. |
Of 166 participants who reported sending digital images to the clinician, 121 participants’ images were documented, and corresponding changes in patient care were noted. |
| Peleg et al. (2017a) | Evaluating whether the MobiGuide (mobile decision-support system) facilitated the compliance to system’s recommendations, satisfaction, and quality of life among patients with AF or GDM and their HCPs. Focus: atrial fibrillation (AF), Gestational diabetes (GDM) Location: Europe (Italy/Spain) |
Study: developmental / feasibility study Ages: older adults, adults N = 10 AF; 20 GDM System: MobiGuide is a chronic patient management system that has, patient-empowering innovative functionalities based on the interaction of patients’ activity and clinical guidelines. Incorporates data from mobile sensors via Bluetooth, self-report of symptoms, computer interpretable clinical guidelines, compliance-checking functions Data from electronic health records can be pulled into the PGHD system (semantic data integration) |
A high compliance to system recommendations was noted. Quality of life for patients was uncertain. |
| Peleg et al. (2017b) | Describing MobiGuide users’ experiences in terms of sustainable usage, patients’ perceptions of usage, and HCP’s views of patient data. Focus: atrial fibrillation (AF), Gestational diabetes (GDM) Location: Europe (Italy/Spain) |
Study: developmental / feasibility study Ages: older adults, adults N = 10 AF; 20 GDM MobiGuide, a personalized evidence-based decision-support system. |
Hypothesis of sustainable usage of MobiGuide, positive perceptions of MobiGuide usage, and clinician usage of patient data were supported. |
| Quinn et al. (2008) | Adult patients with type 2 diabetes can benefit from the use of WellDoc™. Focus: diabetes Location: USA |
Study: feasibility and usability, randomized to intervention and control Ages: adult ages 18–70 N = 30 The feasibility of using WellDoc™, a mobile diabetes management system in conjunction with web-based analytics to manage A1C by patients and HCPs. |
Better A1C control among patients who used WellDoc™. HCPs reported the system facilitated clinical decision making. The majority of patients and physicians were satisfied with the system. |
| Smith et al. (2012) | Reporting mHealth-based EMA and two-way interactive text messaging for providing treatment feedback for the care of veterans with mTBI and/or PTSD. Focus: mild traumatic brain injury (mTBI), post traumatic stress disorder (PTSD) Location: USA |
Study: pilot study to assess feasibility, potential utility Ages: adult N = 27 System: un-named. described as an electronic survey tool that supports data collection from personal digital assistants, commercial SMS text messaging Study examined ecological momentary assessment (EMA) and two-way interactive text messaging as communication modes in the care of veterans with mTBI and/or PTSD. |
mHealth-based support in conjunction with traditional mental treatment are feasible for the treatment of veterans with mental health concerns. Users’ prior mobile experiences and clear data presentation are important for the design of such a system. |
| Weissman et al. (2016) | Study of information management system, Accu-Chek Smart Pix system to improve the self-monitoring of blood glucose for patients with type 1 and type 2 diabetes in outpatient settings. Focus: diabetes Location: Europe (Denmark/ Germany) |
Study: observational prospective study Ages: adult N = 965 System: information management system, Accu-Chek Smart Pix system |
Significant reductions in HbA1c from baseline were noted, and reports from the information management system were used for therapy adjustment. |
Notes. CONDUIT-HID= CONtrolling Disease Using Inexpensive Technology-Hypertension in Diabetes; BP=blood pressure; AF=atrial fibrillation; GDM=gestational diabetes Mellitus; EMA=ecological momentary assessment; mTBI =mild traumatic brain injury; PTSD= post-traumatic stress disorder
Most of the studies were at exploratory or developmental stages. Two studies were randomized controlled trials (RCT), with sample sizes of 40 (Hsu et al., 2016) and 96 (Jiang et al., 2016). A third (Andy et al., 2012) described their 61-patient study as a randomized trial but did not provide information about the groups and reported the results like as an observational study. Six studies were observational or cross-sectional designs (Barrett et al., 2018; Lau et al., 2013; Lv et al., 2017; Marcau et al., 2010; Miller et al., 2017; Weissmann et al., 2016). More than half (12/21, 57%) described the study as beta test, pilot, feasibility or case study (Adams, et al., 2003; Albisser, et al., 2001; Basch et al., 2007; Bauer et al., 2018; Johansen et al., 2004; Lindroth et al., 2018; Martinez et al., 2017; Peleg et al., 2017a, 2017b; Quinn et al., 2008; Smith et al., 2012). Sample sizes for these early stage exploratory studies ranged from 4 (Johansen et al., 2004) to 142 (Albisser et al., 2001), with most having 30 or fewer participants (Table 3).
Article Quality
We were not reporting the effects of PGHD per se, and most of the studies reported very early stage projects, with less than half of the articles as RCT or prospective observational studies. Because of the preponderance of early, developmental, and pilot studies we did not use a standard appraisal tool to formally evaluate study quality. However, we qualitatively examined article quality. Some of the articles met traditional quality metrics. For example the observational study by Weissman et al. (2016) had a fairly large sample, well-described participant characteristics, and provided detail about their study processes.
We also noted several limitations on study quality in some of the studies. Participant characteristics were largely unreported. The study by Adams et al. (2003), a striking example, did not report any participant characteristics including the number of participants. As shown in Table 3, in multiple studies the age range was not specified but presumed to be adult based on the study description. Most were single center, and often single unit within a center, with only the study by Weissmann et al. (2016) explicitly described as multi-center. Some effects were reported but not actually measured; for example, in the study by Barrett et al. (2018), potential clinical effects were only hypothesized. The PGHD systems were evolving and undergoing iterative refinement (particularly for studies described as pilot or beta-testing). The study by Albisser et al. (2001) for example, explicitly noted the system was being actively refined during the time the study was being conducted. Refinement is a natural part of tool development processes but can be a challenge to reproducibility. We noted other design and methodology issues, some reported by the authors, including high attrition (Marceau et al., 2010), recall bias and ascertainment bias (Peleg et al.,2017a).
Types of Data Collected
We extracted descriptions of the wide variety of data collected in the studies and grouped them by data elements. Not surprisingly, almost all the PGHD systems collected data about symptoms, physiological measurements, and behaviors, with the exception of the study by Hsu et al. (2016); the PGHD system Hsu evaluated focused on blood glucose values and medication adherence although the patients also participated in virtual visits with their health care provider via videoconferencing. Some of the system didn’t just ask if symptoms were present but also included extent of symptom interference or quality of life metrics. The study by Basch et al. (2007) included formal PRO measures as well as study-specific questionnaires to measure symptoms, and used validated measures of quality of life. The study by Bauer et al. (2018) included the validated instruments PHQ-9 to measure depression and GAD-7 to measure anxiety. As shown in Table 3, most studies were focused on condition-specific topics, and consequently data collected in the systems focused on the condition-specific symptoms. Also commonly reported were lifestyle and health behaviors such as activity/exercise and diet, risk behaviors (such as smoking) and preventive measures (like foot or eye exam). Medication usage or adherence was examined in several PGHD systems (Adams et al., 2003; Andy et al., 2012; Barrett et al., 2018; Hsu et al., 2016; Marceau et al., 2017; Peleg et al., 2017a, 2017b; Quinn et al., 2008).
Many of the studies included physiologic measurements from a device, such as a blood glucose monitor (Albisser et al., 2001; Andy et al., 2012; Hsu et al., 2016; Peleg et al., 2017a, 2017b; Quinn et al., 2008; Weissman et al., 2016), vital signs such as blood pressure or heart rate (Andy et al., 2012, Jiang et al., 2016; Peleg et al., 2017a, 2017b), body weight (Lv et al., 2017), or spirometry or peak flow (Adams et al., 2003, Jiang et al., 2016). The device data in some studies was manually entered by the patient into the PGHD system with notable exceptions being the report by Andy et al. (2012) and the reports by Peleg et al. (2017a, 2017b) which explicitly noted the sytem allowed data to upload from commercial blood glucose monitors; the Weissmann et al. (2016) report also included a device reader that could pull data from blood glucose monitors. The paper by Martinez et al. (2017) used an automated blood pressure cuff that uploaded data to the Microsoft HealthVault personal health record.
Less commonly seen data element categories were contextual data, goals/preferences, and miscellaneous. Contextual elements included patient demographics and events such as illness or pre-defined psychosocial contexts such as being at work (Albisser et al., 2001; Andy et al., 2012; . Goals or preferences were occasionally reported in the PGHD system (Barret et al., 2018; Peleg et al., 2017b). Miscellaneous data included problem-solving activities or journal functions in which the patient could choose what to document (Andy et al., 2012).
Usability and Satisfaction
Some of the studies reported that the PGHD system/app included built in surveys or questionnaires evaluating the application itself, reactions to using the system, or issue tracking. However, despite the clearly formative nature of most of these evaluations, few of the developmental studies reported formal usability evaluations and reported satisfaction or reactions in broad terms. Some assessed usability or satisfaction externally to the PGHD system. The study by Andy et al. (2012) for example, predominantly reported what functions were used, and noted in the conclusions that they received “user feedback including either device problems or browser compatibility problems” (p. 6 of 6). Jiang et al. (2016) used a satisfaction survey but then noted that the distribution of scores was highly skewed so dichotomized to fully satisfied or less than fully satisfied (p.6). Johansen et al. (2004) noted that families were “happy to participate” and found it “easy and convenient” (p. S1:55) but also provided qualitative comments to illustrate responses. Despite having ease of use in the title, the study by Martinez et al. (2017) did not report any ease of use or usability metrics. Similarly, Quinn et al. (2008) had satisfaction in their study title but what they evaluated was satisfaction with the clinical outcome rather than satisfaction with the PGHD system. Smith et al. (2012) did not describe their survey other than to note it was a brief, forced-choice questionnaire, and reported broadly “participants generally found the messaging program useful” (p. 300), with percentages of respondents who found selected features of the system “helpful” (p. 301).
A few of the studies were more informative. Barrett et al. (2018) described their study as a crowdsourced application, and although not describing a formal evaluation in detail, they reported participant experiences from 57 patients, noting 80% were satisfied with the sensor and found it easy to use, 81% reporting feeling more confident in being to avoid an asthma attack. Bausch et al. (2007) noted that they used a satisfaction survey with items adapted from measures used in similar research, and reported “Satisfaction with the system was high (90%), but only 51% felt communication was improved” (p. 5375). Bauer et al. (2018) reported “the app was easy to use and the amount of time was reasonable” but added detail including a table with responses to individual items on their questionnaire. Hsu et al. (2016) conducted a qualitative exit interview and reported example user comments organized around themes of reduced anxiety, empowerment, and connecting glucose level to behavior (p.63–64). Marceau et al. (2010) noted satisfaction as a main study outcome, and described their questionnaires as adapted for the study from previously published questionnaires and reported not only questionnaire results, but also qualitative comments, both positive and negative. Peleg et al. (2017b) reported in detail the results of a usability survey with detailed responses in a table. Weissmann et al. (2016) reported high levels of physician satisfaction (“satisfied or perfectly satisfied”) along a number of domains such as time for decision making, quality of patient interactions, speed of report generation, clarity of records, and other domains (p. 81).
PGHD Systems/Apps
Most of the PGHD systems were study-specific. A few (5) used commercial systems or included off-the-shelf components (Albessier et al., 2001; Barrett et al., 2018; Miller et al., 2016; Quinn et al., 2008; Weissmann et al., 2016). Data were predominantly manually entered. In many of the studies, patients had to manually record even device data into the PGHD system. There were 5 studies (Andy et al., 2012; Hsu et al, 2016; Martinez et al., 2017; Quinn et al., 2008; Weissmann et al., 2016) that indicated they pulled data from a limited number of very specific devices, such as specified glucometers. Voice or phone touch-tone was used for data entry in 2 studies (Adams et al., 2003; Albisser et al., 2001). Digital images were used in the studies by Johansen (2004) and Miller (2016), and as an option for recording food intake in the study by Andy (2012). Bauer et al. (2018) included data from sensors built into the phone or tablet, such as location, movement, phone usage, and app usage data.
Data storage was predominantly not reported. A few studies discussed a study or app-specific survey, or integrated with REDCap or similar data collection tools. Data transfer methods included Bluetooth (for those that captured data from devices to phone) and Wi-Fi (phone to server). Web portals were reported in multiple studies. Some had no data transfer (data were entered and viewed directly on a central server). Data transfer methods were sometimes unspecified (“secure data transfer” or “patients could upload”).
Electronic Health Record (EHR) integration
Interestingly, 2 of the studies used paper (printed reports) for sharing data with the clinicians (Albisser et al., 2001; Basch et al., 2007). Only 4 studies claimed electronic health record (EHR) integration of PGHD data Adams et al., 2003; Holch et al, 2017; Lv et al, 2017; Martinez et al., 2017). The system examined by Peleg et al. (2017a, 2017b) interacted with EHR data in the other direction, pulling clinical data into the PGHD system. Integration with electronic health records was discussed as a potential for future development using terms such as HL7 compatible (Martinez 2017) or formatted to support semantic integration (Peleg 2017a, 2017b)). Andy et al. (2012) created a report formatted as an HL7 Continuity of Care Document (CCD), which is a national standard accepted by the U.S. Department of Health and Human Services for sharing clinical information (HL7 International).
Decision Support
The articles in this review used mostly very simple forms of decision support. The predominant form of decision support was information presentation, in a variety of summaries, reports, or status dashboards. This included progress reports stored centrally (Albisser et al., 2001), visualizations of patient data viewed the nurse and used to adjust interview questions for face to face consultations (Lindroth et al., 2018), and weekly summaries correlating medication adherence and blood glucose values with reminders to also consider diet and exercise effects and links to communications tools (Hsu et al, 2017). Blood glucose profiles, statistics, graphs and other visualizations were also provided in reports by Weissman et al. (2018). Johansen et al. (2004) asked families to email a summary to the burn team. Well constructed reports and information displays are known to support communication between patients and providers and facilitate collaborative decision making. Weissman et al. (2018) for example, explicitly noted that the reports were used during clinic visits to guide collaborative decision making, as did Hsu et al. (2017). Marceau et al. (2010) used direct patient and healthcare provider communications as the primary means of decision support. Similarly, Smith et al. (2012) used data shared with the treatment team as a primary form of decision support. Some of the reports and information presentation features targeted specifically the patient or provider. Miller et al. (2016) presented wound images to the providers, leaving it to the provider to interpret. Lau et al (2013) specifically designed their electronic diary to support participant self-reflection, with llinks to communications portals that would allow people to choose to communicate with clinicians.
Also commonly reported were a variety of unspecified feedback or reminders, or simple alerts based on thresholds (like a blood pressure that was above guideline thresholds). Patients were generally advised to consult with their clinician, rather than being offered specific actionable advice. A few systems included automatically generated emails that could be sent to the providers for certain alert conditions. Examples of these alerts and feedback include:
symptom-treatment mismatch notice to the patient, with alerts sent to a clinician (Adams et al., 2003)
out of range vital signs (Andy et al., 2012)
dashboard showing asthma control, medication adherence, as well as notification of local air pollution levels (Barrett et al., 2018)
patient alerted to contact clinician if symptom severity of grade 3 or higher was reported (Basch et al., 2007). This study had no automated reporting to clinicians.
app (for patients) plus dashboard (for care managers) that include ability to graph findings over time; dashboard flagged patients with specified alerts such as persistent symptoms or isolation based on movement/communication, or if patient response indicated thoughts of self-harm. Care managers and clinicians responded to patient by phone (Bauer et al., 2018)
alerts for symptoms that passed critical thresholds, with feedback message about when and what to report to the transplant coordinator (Jiang et al., 2016)
dashboard alert for nurse case manager if individual blood pressure measurements cross a specified critical level (Lv et al., 2017)
feedback about how entered blood glucose value compared to patient-specific target (Quinn et al., 2008)
Patient education was specifically called out as a form of feedback or advice in some of the studies. Albisser et al (2001) provided self-management instructions, and Andy et al. (2012) provided standardized educational messages. Similarly the system evaluated by Quinn et al. 2008) provided patient feedback/education about nutrition, lifesyle, stage of change, and self-management skills. Sometimes the messages were somewhat tailored. Adams et al. (2003) provided behavioral reinforcement education tailored to the patient data. Barrett et al. (2018) tailored education based on guidelines.
Three of the more recent studies provided actionable advice, coupled with clinician notifications. The sytem evaluated by Holch et al. (2017) provided immediate targeted advice based on local and national guidelines for low to moderate severity events. For severe events, the system provided advice to contact the hospital and email was sent to clinicians. The system evaluated by Martinez et al. (2017) used a protocol to evaluate data and provided feedback to adjust medications if blood pressure was not controlled, along with alerts sent to diabetes care nurses. The system evaluated by Peleg et al. (2017a, 2017b) included a formal clinical decision support system that provided feedback based on patient data and clinical guidelines, but gave patients control over how to use the system.
A care manager (often a nurse care manager) or other intermediary was an important part of the decision support workflow for several studies. Adams et al. (2003) triaged alerts into level 1 (high priority) with alerts sent directly to a care manager, and level 2 (lower priority) alerts which were reported into a document that could be reviewed by the care manager at their convenience. The care manager determined when to contact the primary care provider. In the system used by Albisser et al. (2001), the case worker was the primary day to day reviewer of data in the system and providers reviewed printed reports biweekly or monthly. The system examined by Andy et al. (2012) gave the patient the ability to initate a message with a case manager. In the study by Basch et al. (2007), the primary intermediary was the nurse at a clinic visit. However, only 1 in 7 of the nurses reported that they discussed PGHD findings with patients “frequently”, with time as the biggest barrier to discussing the data with patients. In the study by Johansen et al. (2004), research staff acted as the intermediary. Patients were asked to send emails to the burn team, but those emails were delivered to the research staff and then collated and forwarded by research staff to the burn team. The collated emails added a checklist for the burn team to use in evaluated the image quality. Responses from the burn team were sent to the research staff, who then forwarded messages back to the family. The importance of nurses as an intermediary continued into more recent studies. In the study by Lv et al. (2017) nurse case managers and registered dieticians actively accessed the dashboard, contacting patients as needed using system-supported bi-directional secure messaging. IN the study by Martinez et al. (2017), diabetes care nurses phoned patients between office visits and when alert was generated.
DISCUSSION
In this review we examined scientific literature to attempt to understand the extent to which the vision of using PGHD to inform clinical decision-making has been realized. We found literature that showed predominantly developmental and feasibility studies, and studies that look at impact or outcomes are just emerging. The PGHD systems were highly diverse in terms of what data were collected, and how data were collected, stored, and shared. Despite the rapid growth in personal sensors (such as activity trackers) and general positive attitudes about “quantified self” in popular literature, we found only limited usage of these devices in the studies. This slow start and gradual growth aligns with the PGHD adoption curve projected by the Office of the National Coordinator for Health IT (Cortez, Hsii, Mitchell, Riehl, & Smith, 2018), which suggested that we are currently in an early adopter stage for PGHD in clinical care and research.
The scarcity of empirical research that included both PGHD and clinical processes was similar to that reported in a recent synthesis looking at PGHD information quality (Peter West, Max Van Kleek, Richard Giordano, Mark Weal, & Nigel Shadbolt, 2017). Because of our narrow focus and the scarcity of literature that met our review criteria we also examined the excluded studies, at a high level, to try to evaluate why these studies returned on the keyword search but were excluded. We saw that people sometimes used PGHD keywords to represent data collection methods, such as interviews or questionnaires that are aimed at the patients or caregivers (A. E. Chung & Basch, 2015b; Peeples, Iyer, & Cohen, 2013). In many cases, papers were excluded that included study protocols, a number of scale or instrument development or validation studies, and system architecture descriptions. Some used only fabricated or synthetic data and lab testing. We also excluded a number of drug studies or intervention evaluations, in which the “patient-reported information” was limited to intervention effects or “reportable” drug adverse effects.
In terms of clinical decision support features for PGHD data, we identified in most cases a very basic level of decision support. This rudimentary form of clinical decision support may be a reflection of the emergent state of PGHD systems (Shameer et al., 2017). It may also be that developers could be intentionally avoiding giving actionable recommendations because such usage might place the devices into the realm of being a “medical device” per FDA definitions and therefore subject to additional oversight, which can be prohibitive for devices that are still in developmental process (Tung et al., 2018). Personal devices that are low-cost enough for widespread use (consumer-grade devices) are in some cases known to have issues with accuracy and precision (P. West, M. Van Kleek, R. Giordano, M. Weal, & N. Shadbolt, 2017). Finally, data from these devices can be difficult to use in rigorous research studies, with no standard formats defined (as yet) and data from many devices are often stored in a manner that is proprietary to the system developer (Quinn et al., 2008a).
Our findings highlight that efforts to integrate PGHD to support clinical decision making are growing in recent years, however, further work is needed to allow for its broader application and use. Our recommendations fall under the following categories: research; policy; system design, EMR integration, regulating hardware and software; engaging the clinical workforce, and consumer education.
Research
Findings from our systematic review highlight the need to further explore several areas to ensure clinical decisions can be made appropriately when PGHD are used. Research using rigorous methods and larger sample sizes are needed to evaluate the impact of PGHD on, for example, health outcomes, or cost of care. Further research should address quality, accuracy, and reliability of the data produced in various settings and case scenarios. Data accuracy and reliability will be increasingly important as more individuals decide to share their data and providers use it to guide their care (Sitapati et al., 2017; Tung et al., 2018). Researchers have described an anticipated enhanced patient engagement using these technologies, however, this assumption should be directly assessed (Y. R. Park et al., 2018). Unintended consequences have also been suggested, such as the potential for increased patient anxiety due to a heightened awareness of health decline (Harrison, Koppel, & Bar-Lev, 2007; D. A. Steward, R. A. Hofler, C. Thaldorf, & D. E. Milov, 2010). The unanticipated consequences need to be closely monitored and further described to help mitigate poor outcomes or to identify who may benefit most using PGHD. Other areas of further exploration include how PGHD influences shared decision making, care coordination, new models of patient-centered care delivery, healthcare utilization, and workflow and provider efficiencies. Usability studies will help to integrate the patient voice and elucidate user issues and satisfaction with the mobile and sensing tools and determine how to meaningfully provide feedback to patients and families (S. S. Woods, N. C. Evans, & K. L. Frisbee, 2016).
The analytic processes for assessing PGHD is another area primed for further development. As we move from historically aggregated, population-based data to individual, longitudinal data more advanced methodologies need to be applied to identify an individual’s patterns, changes in patterns and outliers. Advanced methodologies for interpreting PGHD include, for example, predictive analytics (the branch of analytics that uses various techniques to predict future events based on existing large data sets), machine learning (the use of algorithms by computer systems to complete tasks relying on inferences over time), deep learning (that focuses on learning data representations rather than tasks), artificial intelligence, and other complex analysis (Bhavnani et al., 2017; Peake, Kerr, & Sullivan, 2018b; Shameer et al., 2017). We also recommend being proactive in making patients and families part of the analytic team to make better sense of the data.
In the included studies we found variability in the data that were presented. We recommend authors use and journals require a standardized reporting framework to assess the quality of the produced data. For example, the Mobile Health Evidence Reporting and Assessment (mERA) reporting framework has been adapted to support health system evaluation of technology promoting the capture and use of PGHD to deliver patient-centered care (Agarwal et al., 2016).
Policy
Policy will help to guide and determine the future of digitally enabled healthcare. Based on our findings, there are several areas where policy development is important to further examine and provide guidance for the use of PGHD in health care delivery. Policy areas include, but are not limited to, guiding interoperability of devices and systems; establishing standards around tracking modalities; addressing issues of liability and privacy; and to help inform reimbursement structures. Tracking modality issues may include, for example, determining the frequency or intervals of tracking and analysis, methods of measuring, and how providers should manage the data. When technological advances occur too quickly for existing healthcare practices to keep up a mismatch between development and preparedness of the system to effectively integrate and utilize the data can occur (Bhavnani et al., 2017). Liability issues include determining who is responsible for analyzing the data – the provider, the vendor of the digital tool, to whom can the data analysis be delegated. Potenial liability may be reduced or mitigated by establishing policies and proceedures for handling PGHD and maintaining transparency about the used of the patient’s information (HIMSS, 2014). It will be important to determine the delegation of responsibilities for review of certain types of PGHD, for example, to designees such as a nurse, care manager or other staff and guidelines for responding to alerts or concerning data. Despite the value of PGHD to extend or expand care for individuals, there is a tension that this approach to care management/delivery is not yet reimbursed by the current payment structures limiting the integration of PGHD in practice. There is a need for the innovations to align with institutional objectives and for business cases that incorporate payment models and value based reimbursements (Bhavnani et al., 2017). Establishing a reimbursement structure could promote broader use or more rapid uptake. With clinical measures increasingly tied to performance and payment metrics, ensuring that data accurately reflects the health status of patient population is critical (P. West et al., 2017).
System Design, EHR integration, Regulating hardware and software
As PGHD tools become more widely available to become formally integrated to standard processes of care, applying principles of user-centered design can facilitate the implementation of systems that more effectively address stakeholder and workflow needs (Poole, 2013). The integration of PGHD into the Electronic Health Record systems is not fully examined and efforts to date highlight the need for wide adoption of interoperability standards in the industry (Mandel, Kreda, Mandl, Kohane, & Ramoni, 2016). When considering regulating PGHD related hardware and software, several challenges have been identified. Many mobile applications or sensors on the market are considered “lifestyle devices” and do not undergo FDA approval. The FDA has adapted new strategies to address the growing concern for regulation (U.S. Food and Drug Administration, 2013, 2015). Although FDA reviews medical devices, it does not require that the device has been rigorously tested to show if it has had an impact on health outcomes (IMS Institute for Healthcare Informatics, 2015).
Engaging the Clinical Workforce
In addition to integrating data into EHRs, there is a need for clinical workforce training on interpretation of PGHD. Establishing best practices for integration into clinical workflow is essential. For example, real-time alert systems that align with the health systems’ workflow can help providers and staff quickly sift through a large quantity of data to identify when follow-up action is needed (National eHealth Collaborative, 2013). W. Adams et al. (2003) established protocols and built algorithms to determine responses to alerts, e.g., level 1 required immediate response, whereby a nurse was alerted and and patient/parent was notified to seek medical care, while Level 2 alerts were reviewed by a study nurse. All alerts and their corresponding responses were entered into the Electronic Health Record. Providers will also need guidance for identifying tools to recommend to their patients when they choose to take advantage of self-tracking options. For example, a framework has been developed to assist healthcare professionals in recommending quality applications to match patients needs for diabetes self-management (Hale, Capra, & Bauer, 2015).
Implications for Nursing Science
As nurse scientists frequently examine biological underpinnings of symptoms that are inherently self-reported or captured by patients outside clinical settings, PGHD systems can become powerful tools in capturing or predicting vulnerability to changes in health. As Hickey et al. (2019) point out nurse scientists can integrate precision health to better understand disease burden and facilitate symptom management and improvement of quality of life. Given the comprehensive focus on health and well-being in different settings, nurses are uniquely poised to assist patients in capturing information about their physiological, mental and cognitive well-being as well as exposure to environmental parameters (aspects of what is referred to as “phenotypic characterization” in the Nursing Science Precision Health Model (Hickey et al., 2019)). Nursing scientists can use their holistic lense as reflected in the Nursing Science Precision Health Model to lead the process of defining the role of PGHD in the era of precision health.
Consumer Education
Health consumers will need education in how to select accurate and reliable tools, interpret their data, discuss and understand expectations of how their data will inform clinical decision making or lifestyle choices. In this context, we must remain aware of the potential for widening health disparities and be proactive in identifying strategies to mitigate this potential unwanted outcome, such as actively seeking to reduce digital divides and developing novel ways to assure digital data privacy for small populations (Zhang et al., 2017). Challenges include not only the level of access to digital tools and necessary infrastructure but also challenges of health literacy and also “data literacy”, the extent to which users understand the meaning of their data, how they are stored and transmitted and who has or may have access to them (Lor, Koleck, Bakken, Yoon, & Dunn Navarra, 2019; van der Vaart & Drossaert, 2017).
Limitations of our Review
In this review we pursued a narrow focus, requiring that the study include interaction with clinicians for decision making, but that data collection and sharing be patient-initiated. Requiring that there be a clinician-patient decision-making interaction excluded social media platforms and similar emerging forms of patient initiated health data. We tightly adhered to the ONC definition of PGHD, but the use of this term has clearly evolved over time in addition to other, broader definitions. Because of our tight adherence to this specific definition, we excluded many studies where patient generated data were facilitated for the purposes of a research study without actual use in clinical practice; however, the findings of these studies may inform the next step of actual translation of this work into clinical settings. In particular, we excluded many studies that used patient reported outcomes but didn’t meet the nuances of the selected PGHD definition, most often because the data were collected only at investigator-specified intervals or only at the prompting of a clinician during a clinic visit. Our choice of search terms may have also limited our findings. We chose many synonyms for “patient generated health data” but we still found surprisingly few articles that included sensors or monitoring technologies, for example. It is possible that had we searched for specific types of sensors (such as actigraph or activity tracking) without looking for PGHD phrasing, we might have found more relevant literature.
CONCLUSION
Our systematic literature review found few studies that implement the full scope and intent of the ONC definition of PGHD. Integration of PGHD into electronic records was extremely limited, and decision support capabilities were for the most part basic/rudimentary. PGHD will be part of the health care system narrative and we must continue efforts to understand its impact on health outcomes, costs, efficiency, and patient satisfaction. This will require an iterative design and implementation process with patients, health care providers, and researchers. To accomplish the integration of use of PGHD in daily practice, policies and guidelines will be needed to accommodate the vast arrange of data types and use case scenarios to be able to use PGHD in daily practice effectively. We conclude that the use of PGHD in clinical practice is in the promising stage and inevitable but needs further work for widespread adaption and seamless integration into healthcare systems. Nursing scientists need to be at the forefront of this research and lead the process of defining the role of PGHD in the era of precision health.
Footnotes
Declarations of interest: none
References
- Adams A, Shankar M, & Tecco H (2016). 50 things we now know about digital health consumers: 2016 digital health consumer adoption survey results. Retrieved from https://rockhealth.com/reports/digital-health-consumer-adoption-2016/
- Adams W, Fuhlbrigge A, Miller C, Panek C, Gi Y, Loane K, … Friedman R (2003). TLC-Asthma: an integrated information system for patient-centered monitoring, case management, and point-of-care decision support. AMIA Annual Symposium proceedings, 1–5. [PMC free article] [PubMed] [Google Scholar]
- Agarwal S, LeFevre A, Lee J, L’Engle K, Mehl G, Sinha C, & Labrique A (2016). WHO mHealth Technical Evidence Review Group. Guidelines for reporting of health interventions using mobile phones: mobile health (mHealth) evidence reporting and assessment (mERA) checklist. BMJ, 352(8049), i1174. [DOI] [PubMed] [Google Scholar]
- Akdis C, & Ballas Z (2016). Precision medicine and precision health: Building blocks to foster a revolutionary health care model. Journal of Allergy and Clinical Immunology, 137(5), 1359–1361. doi: 10.1016/j.jaci.2016.03.020 [DOI] [PubMed] [Google Scholar]
- Albisser AM, En Chao SC, Parson ID, & Sperlich M (2001). Information technology and home glucose clamping. Diabetes Technology and Therapeutics, 3(3), 377–386. [DOI] [PubMed] [Google Scholar]
- Alyami M, Giri B, Alyami H, & Sundram F (2017). Social anxiety apps: a systematic review and assessment of app descriptors across mobile store platforms. Evidence-based mental health, 20(3), 65–70. doi: 10.1136/eb-2017-102664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andy YYL, Shen CP, Lin YS, Chen HJ, Chen AC, Cheng LC, … Lai F (2012). Continuous, personalized healthcare integrated platform C3 - IEEE Region 10 Annual International Conference, Proceedings/TENCON. [Google Scholar]
- Ask P, Ekstrand K, Hult P, Lindén M, & Pettersson N (2012). NovaMedTech - A regional program for supporting new medical technologies in personalized health care. Paper presented at the 9th International Conference on Wearable Micro and Nano Technologies for Personalized Health, Porto, Portugal. [PubMed] [Google Scholar]
- Barrett M, Combs V, Su JG, Henderson K, Tuffli M, & The AIR Louisville Collaborative. (2018). AIR Louisville: Addressing Asthma With Technology, Crowdsourcing, Cross-Sector Collaboration, And Policy. Health Affairs, 37(4), 525–534. doi: 10.1377/hlthaff.2017.1315 [DOI] [PubMed] [Google Scholar]
- Basch E, Iasonos A, Barz A, Culkin A, Kris MG, Artz D, … Schrag D (2007). Long-term toxicity monitoring via electronic patient-reported outcomes in patients receiving chemotherapy. Journal of Clinical Oncology, 25(34), 5374–5380. doi: 10.1200/JCO.2007.11.2243 [DOI] [PubMed] [Google Scholar]
- Bauer AM, Iles-Shih M, Ghomi RH, Rue T, Grover T, Kincler N, … Katon WJ (2018). Acceptability of mHealth augmentation of Collaborative Care: A mixed methods pilot study. General Hospital Psychiatry, 51, 22–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhavnani SP, Parakh K, Atreja A, Druz R, Graham GN, Hayek SS, … Shah BR (2017). 2017 Roadmap for Innovation-ACC Health Policy Statement on Healthcare Transformation in the Era of Digital Health, Big Data, and Precision Health: A Report of the American College of Cardiology Task Force on Health Policy Statements and Systems of Care. Journal of the American College of Cardiology, 70(21), 2696–2718. doi: 10.1016/j.jacc.2017.10.018 [DOI] [PubMed] [Google Scholar]
- Bock C, Demiris G, Choi Y, Le T, Thompson HJ, Samuel A, & Huang D (2016). Engaging older adults in the visualization of sensor data facilitated by an open platform for connected devices. Technology and Health Care, 24(4), 541–550. doi: 10.3233/THC-161150 [DOI] [PubMed] [Google Scholar]
- Brath H, Morak J, Kästenbauer T, Modre-Osprian R, Strohner-Kästenbauer H, Schwarz M, … Schreier G (2013). Mobile health (mHealth) based medication adherence measurement - a pilot trial using electronic blisters in diabetes patients. British Journal of Clinical Pharmacology, 76(1), 47–55. doi: 10.1111/bcp.12184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen YR, & Schulz PJ (2016). The Effect of Information Communication Technology Interventions on Reducing Social Isolation in the Elderly: A Systematic Review. Journal of Medical Internet Research, 18(1), E18. doi: 10.2196/jmir.4596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung AE, & Basch EM (2015a). Potential and challenges of patient-generated health data for high-quality cancer care. Journal of Oncology Practice, 11(3), 195–197. doi: 10.1200/JOP.2015.003715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung AE, & Basch EM (2015b). Potential and challenges of patient-generated health data for high-quality cancer care. J Oncol Pract, 11(3), 195–197. doi: 10.1200/JOP.2015.003715 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung C, Dew K, Cole A, Zia J. e., Fogarty J, & Julie A (2016). Boundary Negotiating Artifacts in Personal Informatics: Patient-Provider Collaboration with Patient-Generated Data. Paper presented at the Computer-Supported Cooperative Work. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung J, Demiris G, Thompson HJ, Chen K-Y, Burr R, Patel S, & Fogarty J (2017). Feasibility testing of a home-based sensor system to monitor mobility and daily activities in Korean American older adults. International Journal of Older People Nursing, 12(1), e12127. doi: 10.1111/opn.12127 [DOI] [PubMed] [Google Scholar]
- Ciemins EL, Arora A, Coombs NC, Holloway B, Mullette EJ, Garland R, … Coon PJ (2018). Improving Blood Pressure Control Using Smart Technology. Telemedicine and e-Health, 24(3), 222–228. doi: 10.1089/tmj.2017.0028 [DOI] [PubMed] [Google Scholar]
- Cortez A, Hsii P, Mitchell E, Riehl V, & Smith P (2018). Conceptualizing a Data Infrastructure for the Capture, Use, and Sharing of Patient-Generated Health Data in Care Delivery and Research through 2024: White Paper. Retrieved from https://www.healthit.gov/sites/default/files/onc_pghd_final_white_paper.pdf
- Deave T, Kendal S, Lingam R, Day C, Goodenough T, Bailey E, … Coad J (2018). A study to evaluate the effectiveness of Best Beginnings’ Baby Buddy phone app in England: a protocol paper. Primary health care research & development, 1–6. doi: 10.1017/S1463423618000294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demiris G, Thompson H, Boquet J, Le T, Chaudhuri S, & Chung J (2013). Older adults’ acceptance of a community-based telehealth wellness system. Informatics for Health and Social Care, 38(1), 27–36. doi: 10.3109/17538157.2011.647938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans J, Papadopoulos A, Silvers CT, Charness N, Boot WR, Schlachta-Fairchild L, … Ent CB (2016). Remote Health Monitoring for Older Adults and Those with Heart Failure: Adherence and System Usability. Telemedicine and e-Health, 22(6), 480–488. doi: 10.1089/tmj.2015.0140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forni Ogna V, Pruijm M, Zweiacker C, Wuerzner G, Tousset E, & Burnier M (2013). Clinical benefits of an adherence monitoring program in the management of secondary hyperparathyroidism with cinacalcet: Results of a prospective randomized controlled study. BioMed Research International, 2013. doi: 10.1155/2013/104892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franco RZ, Fallaize R, Lovegrove JA, & Hwang F (2016). Popular Nutrition-Related Mobile Apps: A Feature Assessment. Jmir Mhealth and Uhealth, 4(3), e85. doi: 10.2196/mhealth.5846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunter R, Fernandes-Taylor S, Mahnke A, Awoyinka L, Schroeder C, Wiseman J, … Kent KC (2016). Evaluating Patient Usability of an Image-Based Mobile Health Platform for Postoperative Wound Monitoring. Jmir Mhealth and Uhealth, 4(3), e113. doi: 10.2196/mhealth.6023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hale K, Capra S, & Bauer J (2015). A Framework to Assist Health Professionals in Recommending High-Quality Apps for Supporting Chronic Disease Self-Management: Illustrative Assessment of Type 2 Diabetes Apps. JMIR MHealth and UHealth, 3(3), e87. doi: 10.2196/mhealth.4532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison MI, Koppel R, & Bar-Lev S (2007). Unintended consequences of information technologies in health care--an interactive sociotechnical analysis. J Am Med Inform Assoc, 14(5), 542–549. doi:M2384 [pii] 10.1197/jamia.M2384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hickey KT, Bakken S, Byrne MW, Bailey DCE, Demiris G, Docherty SL, … Grady PA (2019). Precision health: Advancing symptom and self-management science. Nursing Outlook, In Pree, 1–14. doi: 10.1016/j.outlook.2019.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- HIMSS. (2014). Value of Patient-Generated Health Data. Retrieved from https://www.himss.org/value-patient-generated-health-data-pghd?ItemNumber=36962
- HL7 International. Get the HL7 Standards Referenced in US Regulations. Retrieved from http://www.hl7.org/implement/standards/hhsifr.cfm?ref=nav
- Holch P, Warrington L, Bamforth LCA, Keding A, Ziegler LE, Absolom K, … Velikova G (2017). Development of an integrated electronic platform for patient self-report and management of adverse events during cancer treatment. Annals of Oncology, 28(9), 2305–2311. doi: 10.1093/annonc/mdx317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooke MC, Gilchrist L, Tanner L, Hart N, & Withycombe JS (2016). Use of a Fitness Tracker to Promote Physical Activity in Children With Acute Lymphoblastic Leukemia. Pediatric Blood & Cancer, 63(4), 684–689. doi: 10.1002/pbc.25860 [DOI] [PubMed] [Google Scholar]
- Hsu WC, Lau KH, Huang R, Ghiloni S, Le H, Gilroy S, … Moore J (2016). Utilization of a Cloud-Based Diabetes Management Program for Insulin Initiation and Titration Enables Collaborative Decision Making Between Healthcare Providers and Patients. Diabetes Technol Ther, 18(2), 59–67. doi: 10.1089/dia.2015.0160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- IMS Institute for Healthcare Informatics. (2015). Patient Adoption of mHealth. Use, Evidence and Remaining Barriers to Mainstream Acceptance. Retrieved from http://www.imshealth.com/portal/site/imshealth/menuitem.762a961826aad98f53c753c71ad8c22a/?vgnextoid=365656f1603bf410VgnVCM1000000e2e2ca2RCRD&vgnextchannel=a64de5fda6370410VgnVCM10000076192ca2RCRD [Google Scholar]
- Jiang Y, Sereika SM, DeVito Dabbs A, Handler SM, & Schlenk EA (2016). Using mobile health technology to deliver decision support for self-monitoring after lung transplantation. International Journal of Medical Informatics, 94, 164–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansen MA, Wootton R, Kimble R, Mill J, Smith A, & Hockey A (2004). A feasibility study of email communication between the patient’s family and the specialist burns team. J Telemed Telecare, 10 Suppl 1, 53–56. doi: 10.1258/1357633042614302 [DOI] [PubMed] [Google Scholar]
- Joseph C, Stromback B, Hagstromer M, & Conradsson D (2018). ACCELEROMETRY: A FEASIBLE METHOD TO MONITOR PHYSICAL ACTIVITY DURING SUB-ACUTE REHABILITATION OF PERSONS WITH STROKE. JOURNAL OF REHABILITATION MEDICINE, 50(5), 429–434. doi: 10.2340/16501977-2326 [DOI] [PubMed] [Google Scholar]
- Kneale L, Choi Y, & Demiris G (2016). Assessing commercially available personal health records for home health: Recommendations for design. APPLIED CLINICAL INFORMATICS, 7(2), 355–367. doi: 10.4338/ACI-2015-11-RA-0156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kortelainen JM, van Gils M, & Pärkkä J (2012, 2012). Multichannel bed pressure sensor for sleep monitoring. Paper presented at the Computing in Cardiology. [Google Scholar]
- Lau AYS, Dunn AG, Mortimer N, Gallagher A, Proudfoot J, Andrews A, … Coiera E (2013). Social and self-Reflective use of a web-Based personally controlled health management system. Journal of Medical Internet Research, 15(9), 170–185. doi: 10.2196/jmir.2682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JM, Newman MW, Gebremariam A, Choi P, Lewis D, Nordgren W, … Hirschfeld E (2017). Real-World Use and Self-Reported Health Outcomes of a Patient-Designed Do-it-Yourself Mobile Technology System for Diabetes: Lessons for Mobile Health. Diabetes Technology & Therapeutics, 19(4), 209–219. doi: 10.1089/dia.2016.0312 [DOI] [PubMed] [Google Scholar]
- Leveille SG, Huang A, Tsai SB, Weingart SN, & Iezzoni LI (2008). Screening for Chronic Conditions Using a Patient Internet Portal: Recruitment for an Internet-based Primary Care Intervention. Journal of General Internal Medicine, 23(4), 472–475. doi: 10.1007/s11606-007-0443-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindroth T, Islind AS, Steineck G, & Lundin J (2018). From narratives to numbers: Data work and patient-generated health data in consultations C3 - Studies in Health Technology and Informatics. 247, 491–495. [PubMed] [Google Scholar]
- Lor M, Koleck TA, Bakken S, Yoon S, & Dunn Navarra AM (2019). Association Between Health Literacy and Medication Adherence Among Hispanics with Hypertension. J Racial Ethn Health Disparities. doi: 10.1007/s40615-018-00550-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lum HD, Brungardt A, Jordan SR, Phimphasone-Brady P, Schilling LM, Lin C-T, & Kutner JS (2019). Design and Implementation of Patient Portal–Based Advance Care Planning Tools. Journal of Pain and Symptom Management, 57(1), 112–117.e112. doi: 10.1016/j.jpainsymman.2018.10.500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lv N, Xiao L, Simmons ML, Rosas LG, Chan A, & Entwistle M (2017). Personalized Hypertension Management Using Patient-Generated Health Data Integrated With Electronic Health Records (EMPOWER-H): Six-Month Pre-Post Study. 19. doi: 10.2196/jmir.7831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandel JC, Kreda DA, Mandl KD, Kohane IS, & Ramoni RB (2016). SMART on FHIR: a standards-based, interoperable apps platform for electronic health records. J Am Med Inform Assoc, 23(5), 899–908. doi: 10.1093/jamia/ocv189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marceau LD, Link CL, Smith LD, Carolan SJ, & Jamison RN (2010). In-clinic use of electronic pain diaries: Barriers of implementation among pain physicians. Journal of Pain and Symptom Management, 40(3), 391–404. doi: 10.1016/j.jpainsymman.2009.12.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez VI, Marquard JL, Saver B, Garber L, & Preusse P (2017). Consumer Health Informatics Interventions Must Support User Workflows, Be Easy-To-Use, and Improve Cognition: Applying the SEIPS 2.0 Model to Evaluate Patients’ and Clinicians’ Experiences with the CONDUIT-HID Intervention. International Journal of Human-Computer Interaction, 33(4), 333–343. [Google Scholar]
- Miller MW, Ross RK, Voight C, Brouwer H, Karavite DJ, Gerber JS, … Coffin SE (2016). Patient-generated Digital Images after Pediatric Ambulatory Surgery. Appl Clin Inform, 7(3), 646–652. doi: 10.4338/aci-2015-12-cr-0168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, … The, P. G. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Medicine, 6(7), e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National eHealth Collaborative. (2013). Patient-Generated Health Information Technical Expert Panel Final Report. Retrieved from https://www.healthit.gov/sites/default/files/pghi_tep_finalreport121713.pdf
- Park Y, Lee Y, Kim J, Kim J, Kim H, Kim Y, … Lee J (2018). Managing Patient-Generated Health Data Through Mobile Personal Health Records: Analysis of Usage Data. Jmir Mhealth and Uhealth, 6(4), e89. doi: 10.2196/mhealth.9620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park YR, Lee Y, Kim JY, Kim J, Kim HR, Kim YH, … Lee JH (2018). Managing Patient-Generated Health Data Through Mobile Personal Health Records: Analysis of Usage Data. JMIR MHealth and UHealth, 6(4), e89. doi: 10.2196/mhealth.9620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peake JM, Kerr G, & Sullivan JP (2018a). A Critical Review of Consumer Wearables, Mobile Applications, and Equipment for Providing Biofeedback, Monitoring Stress, and Sleep in Physically Active Populations. FRONTIERS IN PHYSIOLOGY, 9. doi: 10.3389/fphys.2018.00743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peake JM, Kerr G, & Sullivan JP (2018b). A Critical Review of Consumer Wearables, Mobile Applications, and Equipment for Providing Biofeedback, Monitoring Stress, and Sleep in Physically Active Populations. Front Physiol, 9, 743. doi: 10.3389/fphys.2018.00743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeples MM, Iyer AK, & Cohen JL (2013). Integration of a mobile-integrated therapy with electronic health records: lessons learned. J Diabetes Sci Technol, 7(3), 602–611. doi: 10.1177/193229681300700304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peleg M, Shahar Y, Quaglini S, Broens T, Budasu R, Fung N, … van Schooten B (2017). Assessment of a personalized and distributed patient guidance system. International Journal of Medical Informatics, 101, 108–130. [DOI] [PubMed] [Google Scholar]
- Peleg M, Shahar Y, Quaglini S, Fux A, García-Sáez G, Goldstein A, … Soffer P (2017). MobiGuide: a personalized and patient-centric decision-support system and its evaluation in the atrial fibrillation and gestational diabetes domains. User Modeling and User-Adapted Interaction, 27(2), 159–213. [Google Scholar]
- Poole ES (2013). HCI and mobile health interventions: How human-computer interaction can contribute to successful mobile health interventions. Transl Behav Med, 3(4), 402–405. doi: 10.1007/s13142-013-0214-3214 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn CC, Clough SS, Minor JM, Lender D, Okafor MC, & Gruber-Baldini A (2008a). WellDoc mobile diabetes management randomized controlled trial: change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technol Ther, 10(3), 160–168. doi: 10.1089/dia.2008.0283 [DOI] [PubMed] [Google Scholar]
- Quinn CC, Clough SS, Minor JM, Lender D, Okafor MC, & Gruber-Baldini A (2008b). WellDoc™ mobile diabetes management randomized controlled trial: Change in clinical and behavioral outcomes and patient and physician satisfaction. Diabetes Technology and Therapeutics, 10(3), 160–168. [DOI] [PubMed] [Google Scholar]
- Risojević V, Rozman R, Pilipović R, Češnovar R, & Bulić P (2018). Accurate Indoor Sound Level Measurement on A Low-Power and Low-Cost Wireless Sensor Node. SENSORS, 18(7), 2351. doi: 10.3390/s18072351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakkottai A, Kaciroti N, Kasmikha L, & Nasr SZ (2018). Impact of home spirometry on medication adherence among adolescents with cystic fibrosis. Pediatric Pulmonology, 53(4), 431–436. doi: 10.1002/ppul.23950 [DOI] [PubMed] [Google Scholar]
- Shameer K, Badgeley MA, Miotto R, Glicksberg BS, Morgan JW, & Dudley JT (2017). Translational bioinformatics in the era of real-time biomedical, health care and wellness data streams. Brief Bioinform, 18(1), 105–124. doi: 10.1093/bib/bbv118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro M, Johnston D, Wald J, & Mon D (2012). Patient Generated Health Data: White Paper. Retrieved from Research Traiangle Park, NC: https://www.healthit.gov/sites/default/files/rti_pghd_whitepaper_april_2012.pdf [Google Scholar]
- Sitapati A, Kim H, Berkovich B, Marmor R, Singh S, El-Kareh R, … Ohno-Machado L (2017). Integrated precision medicine: the role of electronic health records in delivering personalized treatment. Wiley Interdiscip Rev Syst Biol Med, 9(3). doi: 10.1002/wsbm.1378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skubic M, Guevara RD, & Rantz M (2015). Automated Health Alerts Using In-Home Sensor Data for Embedded Health Assessment. IEEE Journal of Translational Engineering in Health And Medicine, 3, 2700111. doi: 10.1109/JTEHM.2015.2421499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B, Harms WD, Burres S, Korda H, Rosen H, & Davis J (2012). Enhancing behavioral health treatment and crisis management through mobile ecological momentary assessment and SMS messaging. Health Informatics Journal, 18(4), 294–308. [DOI] [PubMed] [Google Scholar]
- Steward DA, Hofler RA, Thaldorf C, & Milov DE (2010). A Method for Understanding Some Consequences of Bringing Patient-Generated Data into Health Care Delivery. Medical Decision Making, 30(4), E1–E13. doi: 10.1177/0272989X10371829 [DOI] [PubMed] [Google Scholar]
- Steward DA, Hofler RA, Thaldorf C, & Milov DE (2010). A method for understanding some consequences of bringing patient-generated data into health care delivery. Medical Decision Making, 30(4), E1–E13. doi: 10.1177/0272989X10371829 [DOI] [PubMed] [Google Scholar]
- Thiebaud RS, Funk MD, Patton JC, Massey BL, Shay TE, Schmidt MG, & Giovannitti N (2018). Validity of wrist-worn consumer products to measure heart rate and energy expenditure. Digital Health, 4, 2055207618770322. doi: 10.1177/2055207618770322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung JY, Shaw RJ, Hagenkord JM, Hackmann M, Muller M, Beachy SH, … Ginsburg GS (2018). Accelerating Precision Health by Applying the Lessons Learned from Direct-to-Consumer Genomics to Digital Health Technologies. Paper presented at the NAM Perspectives. [Google Scholar]
- U.S. Food and Drug Administration. (2013). FDA issues final guidance on mobile medical apps. Retrieved from http://www.webcitation.org/6ai9uTZex; http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm369431.htm
- U.S. Food and Drug Administration. (2015). Mobile Medical Applications. Guidance for Industry and Food and Drug Administration Staff. Retrieved from Rockville, MD: http://www.fda.gov/downloads/MedicalDevices/.../UCM263366.pdf [Google Scholar]
- van der Vaart R, & Drossaert C (2017). Development of the Digital Health Literacy Instrument: Measuring a Broad Spectrum of Health 1.0 and Health 2.0 Skills. J Med Internet Res, 19(1), e27. doi: 10.2196/jmir.6709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velardo C, Shah SA, Gibson O, Clifford G, Heneghan C, Rutter H, … on behalf of the, E. C. T. (2017). Digital health system for personalised COPD long-term management. BMC Medical Informatics and Decision Making, 17(1). doi: 10.1186/s12911-017-0414-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weissmann J, Mueller A, Messinger D, Parkin CG, & Amann-Zalan I (2016). Improving the Quality of Outpatient Diabetes Care Using an Information Management System: Results from the Observational VISION Study. Journal of Diabetes Science and Technology, 10(1), 76–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West P, Van Kleek M, Giordano R, Weal M, & Shadbolt N (2017). Information Quality Challenges of Patient-Generated Data in Clinical Practice. Frontiers in public health, 5, 284. doi: 10.3389/fpubh.2017.00284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- West P, Van Kleek M, Giordano R, Weal M, & Shadbolt N (2017). Information Quality Challenges of Patient-Generated Data in Clinical Practice. Front Public Health, 5, 284. doi: 10.3389/fpubh.2017.00284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woods S, Evans N, & Frisbee K (2016). Integrating patient voices into health information for self-care and patient-clinician partnerships: Veterans Affairs design recommendations for patient-generated data applications. Journal of the American Medical Informatics Association, 23(3), 491–495. doi: 10.1093/jamia/ocv199 [DOI] [PubMed] [Google Scholar]
- Woods SS, Evans NC, & Frisbee KL (2016). Integrating patient voices into health information for self-care and patient-clinician partnerships: Veterans Affairs design recommendations for patient-generated data applications. J Am Med Inform Assoc, 23(3), 491–495. doi: 10.1093/jamia/ocv199 [DOI] [PubMed] [Google Scholar]
- Zhang X, Perez-Stable EJ, Bourne PE, Peprah E, Duru OK, Breen N, … Denny J (2017). Big Data Science: Opportunities and Challenges to Address Minority Health and Health Disparities in the 21st Century. Ethn Dis, 27(2), 95–106. doi: 10.18865/ed.27.2.95 [DOI] [PMC free article] [PubMed] [Google Scholar]


