Abstract
Owing to their abilities to identify diseased conditions, to modulate biological process, and to control cellular activities, magnetic nanoparticles have become one of the most popular nanomaterials exploited in the biomedical field. Targeted drug delivery, controlled drug release, hyperthermia treatments, imaging, and stimulation of several biological entities are just some of the several tasks that can be accomplished by taking advantage of magnetic nanoparticles in tandem with magnetic fields. The huge interest towards this class of nanomaterials rises from the possibility to physically drive their spatiotemporal localization inside the body, and to deliver an externally applied stimulation at a target site. They in fact behave as actual nanotransducers, converting energy stemming from the external magnetic field into heat and mechanical forces, which act as signals for therapeutic processes as hyperthermia and controlled drug release. Magnetic nanoparticles result into a non-invasive tool that enables a remote activation of biological processes, besides behaving as formidable tracers for different imaging modalities, thus allowing to simultaneously carry out diagnosis and therapy. In view of all this, owing to their multifunctional and multitasking nature, magnetic nanoparticles are already one of the most important nanotechnological protagonists in medicine and biology, enabling an actual theranostic approach in many pathological conditions. In this Concept, we first provide a brief introduction on some physical properties of magnetic materials and on important features that determine the physical properties of magnetic nanoparticles; thereafter, we will consider some major biomedical applications: hyperthermia, drug delivery / release, and nanoparticle-mediated control of biological processes, even at subcellular level.
Keywords: Magnetic nanoparticles, Hyperthermia, Magnetic drug delivery systems, Magnetic cell control, Nanotransducers
Introduction
Magnetic nanoparticles represent an important class of inorganic materials with attractive properties for biomedical applications. Iron oxide nanoparticles have been for example exploited as contrast agents since many decades in magnetic resonance imaging, and several examples of products approved by regulatory bodies can be found in the clinical practice.[1] However, in the latest years, their intriguing physical properties have been explored for many other applications in biology and medicine, and in this Concept report we will focus on those examples that, in our opinion, make magnetic nanoparticles actual smart and active nanotranducers.
First of all, their physical features allow for a remote manipulation with external magnetic field gradients, thus enabling their positioning / targeting in desired sites. When envisioning drug delivery applications, this implies the possibility to physically transport a therapeutic molecule linked to the nanoparticle to the intended area, owing to a “wireless” guidance of the nanovectors following a system administration.[2] This strategy opens new perspectives in particular in the oncological field, offering the double advantage of reducing the aspecific systemic distribution of the compounds (in the most of the cases toxic also toward healthy tissues), and to instead increase their action at the target site, thus obtaining a more effective therapeutic treatment maintaining lower and safer drug doses.[2] Magnetic nanoparticles act moreover as transducers, able to convert a time-varying magnetic field into thermal and mechanical energy, suitable for inducing hyperthermia, drug release, and even for fostering specific cellular responses.[3]
Magnetic nanoparticles suitable for biomedical applications can be essentially classified as ferromagnetic or superparamagnetic. [4] Ferromagnetic nanoparticles are generally multi-domain particles with size > 10 nm, own a large spontaneous magnetization, and M-H curves present a consistent hysteresis loop; if properly functionalized to avoid agglomeration, they can be very useful for hyperthermia applications.[5]
Among the broad spectrum of magnetic nanomaterials investigated for biomedical purposes, those that exhibit superparamagnetic behavior at room temperature are however the most useful because of several favorable characteristics. Superparamagnetic nanoparticles own a magnetic moment that can be orientated upon the application of a remote magnetic field; following alignment of magnetic moments, resulting magnetization is different from zero and it increases proportionally to the applied field, but it is not preserved when magnetic field is removed.[6] In fact, in the case of mono-domain particles with size around 10 nm (like indeed the superparamagnetic ones), thermal fluctuations avoid establishment of a stable magnetization, and both the remanent magnetization (i.e., the value of the remaining magnetization when the applied magnetic field returns to zero) and the coercitivity (i.e., the magnitude of the field that must be applied to cancel the remanent magnetization) are zero after removing the magnetic field, indicating that the material is no longer magnetized.[6]
Owing to these peculiar features, superparamagnetic nanoparticles play an important role in biomedical applications, since a high magnetization value allows for a magnetic control in biological fluids, yet, however, the lack of a permanent magnetization avoids problems related to aggregation once the magnetic field is removed.[7]
Besides a high magnetization value, necessary for an effective remote manipulation, biocompatibility and colloidal stability are crucial aspects especially for in vivo applications. At this aim, several synthesis strategies have been elaborated in the recent years to achieve appropriate shape, size distribution, dispersibility, and magnetic behaviors.[8] Iron oxides, in particular magnetite (Fe3O4) and maghemite (γ-Fe2O3), are the most common used materials for the synthesis of magnetic nanoparticles[9]. Superparamagnetic iron oxide nanoparticles (SPIONs) are non-toxic, biodegradable, biocompatible, and the iron ions resulting from their degradation are efficiently regulated via the metabolic pathways of Fe and by the innate clearance mechanism of the body.[9],[10]
Since bare SPIONs can be chemically very reactive, in particular under the action of oxidizing agents that can provoke loss of dispersibility and alteration of the magnetic properties, their use usually requires biocompatible coatings, able to preserve them from the action of the surrounding environment.[8] The coating of magnetic nanoparticles plays an extremely important role, fundamental for their successful exploitation: it avoids flocculation, preserves magnetic properties, and can be even used as targeting agent toward specific biological structures. Polymers, surfactants, biomolecules, or inorganic layer such as silica, metal, metal sulfide, and metal oxide have been extensively proposed to provide appropriate coating or grafting to magnetic nanoparticles.[1]
Size, shape, and surface features of nanoparticles moreover determine their biological distribution:[11] in particular, nanovectors should be small enough to bypass body surveillance systems, thus avoiding removal from blood circulation,[12] overcoming several anatomic barriers,[13] and, finally, crossing the fenestrations of the blood capillaries in order to penetrate tissues.[14] Control of the surface characteristics is instead decisive to obtain a non-toxic and stable colloidal suspension in physiological solutions, and to ensure a well sustained cellular uptake.[11],[15] At this regard, several active targeting strategies have been proposed to facilitate the accumulation of magnetic complexes at a intended site with high specificity, that exploit surface functionalization with specific moieties able to selectively bind the intended cells and tissues.[15]
Magnetic Hyperthermia
Due to their capability to convert energy form alternating magnetic fields into heat, magnetic nanoparticles can be used to locally and precisely increase temperature (up to 42-45°C and even above) in hyperthermia treatments, particularly useful in the oncology field.[16] Literally, “hyperthermia” means increment of temperature, and it is an old technique that exploits the deleterious effects of the heat on the cellular structures, such as membranes, cytoskeleton and nuclei.[17] Because of the chaotic and disordered organization of the tumor blood vessels, heat is more difficultly dissipated in diseased sites with respect to healthy tissues, thus provoking a more consistent damage both in terms of cell apoptosis (programmed and active energy-dependent cell death following negative cues) and necrosis (passive cell death following fatal injuries).[18] Furthermore, hyperthermia can be mostly useful also as supporting treatment in traditional oncological approaches like chemotherapy and radiotherapy, since a mild, even sub-lethal, increment of temperature makes cells more sensitive to these therapeutic strategies[19],[20].
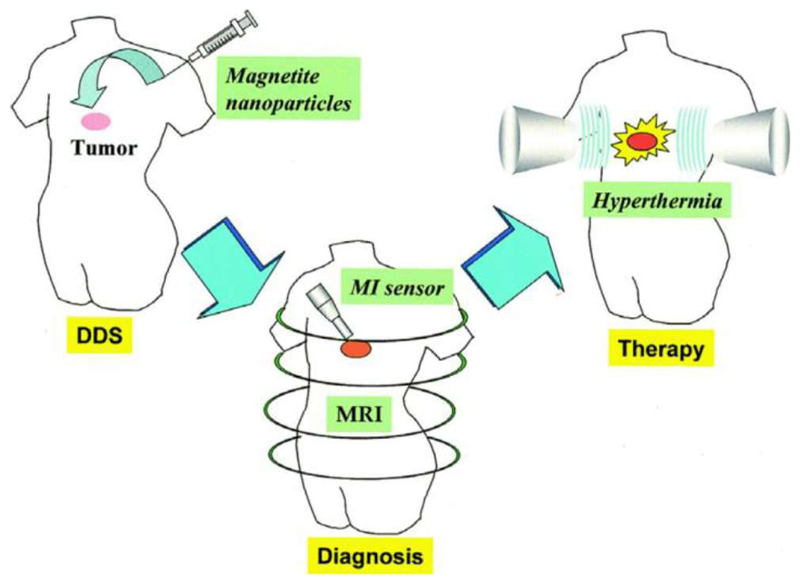
The approach consisting in the induction of a temperature increment through the use of magnetic nanoparticles is referred to as magnetic fluid hyperthermia (MFH);[16] with respect to other methods, MFH offers the advantage of a direct contact between heat source and tumor cells, thus ensuring a greater selectivity and efficacy.[21] MFH in fact relies on the local heating of the tumor tissue by using magnetic nanoparticles, selectively delivered to the tumor area through a local or systemic administration (Figure 1). Upon alternating, non-invasive, electromagnetic stimulation, heat production is thereafter associated to the rotation of the magnetic moment within each particle (Néel relaxation) and to the rotation of particles themselves within a viscos fluid (Brown relaxation)[22].
Figure 1.
Schematic representation of magnetic fluid hyperthermia in cancer therapy. Reprinted with permission from [16]. Copyright (2005) Elsevier.
After the first experimental studies about the use of magnetic nanoparticles for hyperthermia performed in 1957 by Gilchrist et al.,[23] twenty years later many works demonstrated hyperthermia effects obtained on several animal models with different types of magnetic nanoparticles,[24],[25],[26] and with several methods of encapsulation and delivery of the nanoparticles within the tumor.[27],[28] Most importantly, the feasibility and the efficacy of this approach were also confirmed by clinical trials,[29],[30],[31],[32] indeed receiving regulatory approval as a new clinical therapy in 2010.[33]
Currently, major efforts are addressed to optimize nanoparticle heating efficiency in order to obtain a therapeutic effect with an as lowest as possible amount of nanoparticles. Such approach would allow to achieve appropriate temperatures also in those areas where the magnetic material accumulation is poor due to the tumor anatomy and physiology.[21]
The amount of heat generated by colloidal suspension of magnetic nanoparticle is evaluated in terms of specific absorption rate (SAR), and such parameter depends on several properties of the nanovectors, including composition of magnetic material,[34] size,[35] shape,[36] magnetic anisotropy, and saturation magnetization,[37] and on the amplitude and frequency of the applied magnetic field.[36] Particles with high magnetization values, with an optimal anisotropy constant and highly monodispersed ensure high SAR values for an effective hyperthermia treatment.[34] Concerning magnetic field parameters, SAR is an increasing function of amplitude and frequency of the magnetic field. However, it is mandatory to work with frequencies capable to harmlessly pass through the body, and to generate heat just in the sites containing magnetic nanoparticles, without affecting healthy tissues:[38] the high penetrability of magnetic fields to human body without significant attenuation (at a frequency range of about 50-500 kHz) is the key point that makes hyperthermia a successful non-invasive therapeutic approach.[36]
Administration method of magnetic nanoparticles is also fundamental in order to achieve an efficient heat treatment. Magnetic fluid should be in fact accumulated and restricted to the tumor site in order to both limit adverse side effects and to allow repetition of several treatment cycles. Generally, magnetic nanoparticles are placed inside the tumor through direct injection,[39] or alternatively they reach the diseased area thanks to a targeting upon intravenous injection.[40]
Magnetic Drug Delivery
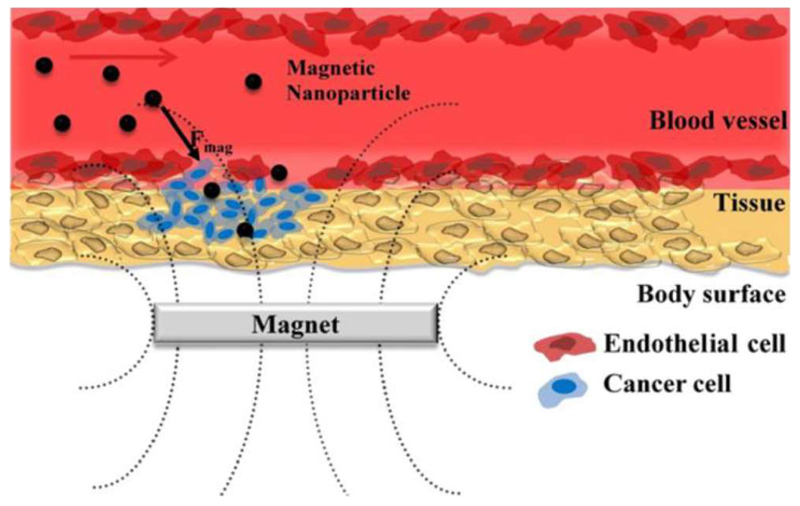
The idea of using magnetic nanoparticles for targeted drug delivery dates to 1970:[41] the rationale is the conjugation of a drug to a magnetically responsive carrier, in order to drive and concentrate its cytotoxic effect in a specific area by means of an external magnet, previously placed close to diseased tissue (Figure 2). The major advantage of a magnetic nanoparticle-mediated targeting with respect to other drug delivery strategies relies on the possibility to monitor the spatiotemporal movement of the carrier through magnetic resonance imaging, by exploiting contrast properties of the magnetic nanoparticles.[2] The multifunctional nature of the nanovector allows the obtainment of a real “theranostic” platform, owing to the combination into a single nanodevice of a therapeutic treatment, by increasing the delivery of a cytotoxic compound at the target site, and of diagnosis, by monitoring the response to the therapy through non-invasive imaging techniques.[42] Over the years such approach has been thus used for the targeted delivery of chemotherapeutic drugs,[43] radionuclides,[44] and genes,[45] by exploiting several strategies of synthesis of magnetic nanoparticles and by designing magnetic drug delivery systems (MDDS) with specific biological, chemical and physical properties.[8]
Figure 2.
Schematic representation of magnetic drug targeting. Reprinted with permission from [43]. Copyright (2011) Elsevier.
Therapeutic compounds can be directly linked to the surface of the magnetic nanoparticles or encapsulated into magnetic nanocarriers having a core-shell structure, where magnetic iron oxide nanoparticles are surrounded by polymers, metals, or lipids.[2],[11],[46] Generally, such approach is used in anticancer therapies, and first clinical trials were reported by Lübbe et al., that exploited epidoxorubicin-coated magnetic nanoparticles for the treatment of inoperable solid tumors.[47] Since then, many examples of magnetic drug delivery systems have been reported by using different animal models.[48],[49] Very interesting, as an example, is the work of Kubo et al.,[50] where a permanent magnet was implanted at the tumor site in hamsters to increase accumulation of magnetic liposomes containing a cytotoxic compound. These encouraging results pushed Pulfer et al. to use a similar approach to target drugs to a rat glioma.[51]
To date, no MDDS has been yet approved for clinical use, however some of them entered into clinical trials, with important promising outcomes.[47],[52] Among the many difficulties that these new nanoplatforms experience in the clinical fields, the most important ones are related to the possibility of reaching the intended site, that often is represented by a depth tumor tissue.[53] Moreover, during their “travel” in the human body, magnetic nanoparticles experience interactions with vessel walls, anatomical barriers, and penetration through various tissue types, and their behavior under the action of a magnetic field is influenced by several physiological variables (first of all the blood flow) so that size, shape, and geometry of the particles as well as strength of the magnetic field are just some of the features we have to consider when designing a MDDS.[53]
Once that the nanoparticles are concentrated at the target site and are internalized by tumor cells, the following step is represented by the release of the encapsulated drug from the carrier, with an appropriate rate compatible with the therapeutic goals. Dealing with MDDSs, the application of an appropriate external magnetic stimulus has been demonstrated to be a suitable trigger of drug release.[54],[55] Such approach exploits the combination of magnetic nanoparticles with stimuli-responsive materials (as an example polymers or lipids), able to change their conformation and structure in response to an external cue, like an increment of temperature or mechanical stresses.[56] Magnetic nanoparticles integrated in thermally- or mechanically-responsive structures result able to induce conformational changes following heat or vibrations generated by exposure to magnetic fields,[57] thus inducing a release of the drug in a well-controlled and sustained manner.
Magnetic nanoparticles for cell activities control
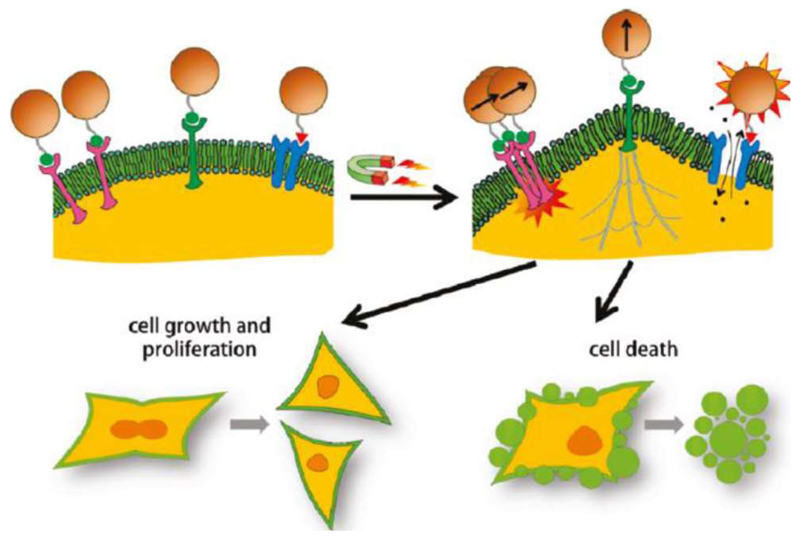
Another potential intriguing application of magnetic nanoparticles is represented by the possibility to modulate cell functions and responses by activating signal transduction mechanisms through stimulation of cells or sub-cellular entities. Cellular receptors can be in fact activated by simultaneous binding of multi-valent signaling molecules; such multi-valent signaling molecules can be mimicked by appropriately targeted magnetic nanoparticles that, in the presence of external magnetic fields, act as nanotransducers by fostering cell behaviors and, at the same time, by preventing non-specific activation.[3]
Cell functions are regulated by macromolecules able to perceive and to respond to stimuli and changes from the surrounding environment. Generally, a signal molecule recognizes and binds a membrane or intracellular receptor, which in turn activates a particular metabolic pathway. The final outcome is the fostering of a well-defined behavior, like variation of the cytoskeleton organization, gene transcription activation, changes of membrane permeability, etc.[58]. Magnetic nanoparticles can be used as actual “switchers” for the manipulation of cell functions and of molecular pathways: following an appropriate functionalization with specific ligands, the nanovectors are able to bind biological receptors in cells, owing to their small size.[58] Thereafter, the application of a remote magnetic field produces mechanical or thermal stimulation able to alter the receptor functionalities[56] (Figure 3).
Figure 3.
Schematic representation of magnetic nanoparticle-mediated activation of cell signaling. Reprinted with permission from [58]. Copyright (2011) American Chemical Society.
In this regard, magnetically generated mechanical stimuli have been for example exploited for the activation of integrin receptors bound to magnetic particles.[59] Authors demonstrated that, if the magnetic field is strong enough to generate a twist of the nanoparticles, or to pull them towards the magnetic field source, receptors perceive the mechanical cue and subsequently activate a cellular signaling pathway.[59] El Haj et al. focused instead their work on the use of magnetic nanoparticles for a selective and precise activation of mechanosensitive ion channels, without interfering with the normal functions of other channels on the cell membrane.[60]
Mannix and colleagues demonstrated that a similar strategy can be used to modulate the spatial organization of membrane receptors.[61] Authors exploited a magnetic needle to concentrate magnetic forces on a small area, in order to induce an aggregation of nanoparticles previously coated with ligands for binding specific transmembrane receptors. Aggregation of the magnetic nanoparticles induced the clustering of the receptors, thus activating a cellular response.[61] Magnetically-driven clustering of receptors represents a new and impressive opportunity to regulate a plenty of cellular and biological processes that are activated by the clustering of membrane receptors. As an example, some groups exploited this strategy for the control of the metabolic pathways involved in angiogenesis (i.e., the development of new blood vessels during the tumor formation),[62] and for fostering programmed cell death.[63]
As a final remark, magnetic nanoparticles constitute a valid tool for cell signaling transduction control through selective heat generation at the level of specific heat-sensitive cellular component, such as some classes of ion channels. Huang et al. succeeded in triggering action potentials in cultured neurons previously treated with superparamagnetic ferrite nanoparticles able to target temperature-sensitive ion channel TRPV1.[64] Application of alternating magnetic fields induced the heating of the nanoparticles, provoking the opening of the TRPV1 channels with a consequent influx of calcium ions, thus inducing the generation of action potentials.[64]
Conclusions
Magnetic nanoparticles are an interesting class of nanomaterials with extraordinary potentials in biological and medical fields. They represent one of the first and few examples of nanotechnological products already approved in the clinical practice, as contrast agents in magnetic resonance imaging.[65] However, just considering magnetic nanovectors as a diagnostic tool is extremely limiting: as summarized in this Concept paper, magnetic nanoparticles are actual theranostic, multifunctional, and multistage nanoplatforms, that offer unprecedented aid in drug delivery, drug targeting and thermal therapy, besides more traditional imaging applications. Although the obtained findings are overall promising, many questions are however still open, including long-term fate, bioaccumulation, and biodegradability issues, that should be adequately addressed before a wide spreading of magnetic nanovectors in the future clinical practice, and in the development of innovative subcellular nanotransducers.
Acknowledgements
This research has received funding from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (grant agreement N°709613, SLaMM).
References
- [1].Wu W, He Q, Jiang C. Nanoscale Research Letters. 2008;3:397–415. doi: 10.1007/s11671-008-9174-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Rui H, Xing R, Xu Z, Hou Y, Goo S, Sun S. Advanced Materials. 2010;22:2729–2742. doi: 10.1002/adma.201000260. [DOI] [PubMed] [Google Scholar]
- [3].Shin TH, Cheon J. Accounts of Chemical Research. 2017;50:567–572. doi: 10.1021/acs.accounts.6b00559. [DOI] [PubMed] [Google Scholar]
- [4].Akbarzadeh A, Samiei M, Davaran S. Nanoscale Research Letters. 2012;7:1–13. doi: 10.1186/1556-276X-7-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kita E, Oda T, Kayano T, Sato S, Minagawa M, Yanagihara H, Kishimoto M, Mitsumata C, Hashimoto S, Yamada K, Ohkohchi N. Journal of Physics D: Applied Physics. 2010;43:474011–474020. [Google Scholar]
- [6].Polyak B, Friedman G. Expert opinion on drug delivery. 2009;6:53–70. doi: 10.1517/17425240802662795. [DOI] [PubMed] [Google Scholar]
- [7].Neuberger T, Schöpf B, Hofmann H, Hofmann M, Von Rechenberg B. Journal of Magnetism and Magnetic Materials. 2005;293:483–496. [Google Scholar]
- [8].Ali A, Zafar H, Zia M, Haq I, Phull AR, Ali JS, Hussain A. Nanotechnology, Science and Applications. 2016;9:49–67. doi: 10.2147/NSA.S99986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Arami H, Khandhar A, Liggitt D, Krishnan KM. Chem Soc Rev. 2015;42:4906. doi: 10.1039/c5cs00541h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Richter GW. The Journal of experimental medicine. 1959;109:197–216. doi: 10.1084/jem.109.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Wu W, Jiang C, Roy VAL. Nanoscale. 2016;8:19421–19474. doi: 10.1039/c6nr07542h. [DOI] [PubMed] [Google Scholar]
- [12].Tartaj P, del Morales MPM, Veintemillas-Verdaguer S, González-Carreño T, Serna CJ. Journal of Physics D: Applied Physics. 2003;36:182–197. [Google Scholar]
- [13].Liu H, Zhang J, Chen X, Du X-S, Zhang J-L, Liu G, Zhang W-G. Nanoscale. 2016;8:7808–26. doi: 10.1039/c6nr00147e. [DOI] [PubMed] [Google Scholar]
- [14].Barua S, Mitragotri S. Nano Todat. 2014;2:223–243. doi: 10.1016/j.nantod.2014.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Frey NA, Peng S, Cheng K, Sun S. Chemical Society Reviews. 2009;38:2532–2542. doi: 10.1039/b815548h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ito A, Shinkai M, Honda H, Kobayashi T. Journal of bioscience and bioengineering. 2005;100:1–11. doi: 10.1263/jbb.100.1. [DOI] [PubMed] [Google Scholar]
- [17].Hildebrandt B, Wust P, Ahlers O, Dieing A, Sreenivasa G, Kerner T, Felix R, Riess H. Critical Reviews in Oncology/Hematology. 2002;43:33–56. doi: 10.1016/s1040-8428(01)00179-2. [DOI] [PubMed] [Google Scholar]
- [18].Song CW, Lokshina A, Rhee JG, Patten M, Levitt SH. IEEE Transactions on Biomedical Engineering. 1984;BME-31:9–16. doi: 10.1109/TBME.1984.325364. [DOI] [PubMed] [Google Scholar]
- [19].Bull JM. Cancer research. 1984;44:4853s–4856s. [PubMed] [Google Scholar]
- [20].Kaur P, Hurwitz MD, Krishnan S, Asea A. Cancers. 2011;3:3799–3823. doi: 10.3390/cancers3043799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Dutz S, Hergt R. Nanotechnology. 2014;25 doi: 10.1088/0957-4484/25/45/452001. 452001. [DOI] [PubMed] [Google Scholar]
- [22].Pankhurst QA, Connolly J, J SK, Dobson J. Journal of physics D: Applied Physics. 2003;36:R167–R181. [Google Scholar]
- [23].Gilchrist RK, Medal R, Shorey WD, Hanselman RC, Parrott JC, Taylor CB. Annals of surgery. 1957;146:596–606. doi: 10.1097/00000658-195710000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Gordon RT, Hines JR, Gordon D. Medical Hypotheses. 1979;5:83–102. doi: 10.1016/0306-9877(79)90063-x. [DOI] [PubMed] [Google Scholar]
- [25].Rand RW, Snow HD, Brown WJ. Journal of Surgical Research. 1982;33:177–183. doi: 10.1016/0022-4804(82)90026-9. [DOI] [PubMed] [Google Scholar]
- [26].Jordan A, Scholz R, Wust P, Fähling H, Krause J, Wlodarczyk W, Sander B, Vogl T, Felix R. International journal of hyperthermia : the official journal of European Society for Hyperthermic Oncology, North American Hyperthermia Group. 1997;13:587–605. doi: 10.3109/02656739709023559. [DOI] [PubMed] [Google Scholar]
- [27].Yanase M, Shinkai M, Honda H, Wakabayashi T, Yoshida J, Kobayashi T. Japanese journal of cancer research : Gann. 1998;89:775–82. doi: 10.1111/j.1349-7006.1998.tb03283.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Le B, Shinkai M, Kitade T, Honda H, Yoshida J, Wakabayashi T, Kobayashi T. Journal of Chemical Engineering of Japan. 2001;34:66–72. [Google Scholar]
- [29].Maier-Hauff K, Rothe R, Scholz R, Gneveckow U, Wust P, Thiesen B, Feussner A, Deimling A, Waldoefner N, Felix R, et al. Journal of Neuro-Oncology. 2007;81:53–60. doi: 10.1007/s11060-006-9195-0. [DOI] [PubMed] [Google Scholar]
- [30].Johannsen M, Gneveckow U, Eckelt L, Feussner A, Waldöfner N, Scholz R, Deger S, Wust P, Loening Sa, Jordan A. International journal of hyperthermia : the official journal of European Society for Hyperthermic Oncology, North American Hyperthermia Group. 2005;21:637–647. doi: 10.1080/02656730500158360. [DOI] [PubMed] [Google Scholar]
- [31].Johannsen M, Gneveckow U, Thiesen B, Taymoorian K, Cho CH, Waldöfner N, Scholz R, Jordan A, Loening SA, Wust P. European Urology. 2007;52:1653–1662. doi: 10.1016/j.eururo.2006.11.023. [DOI] [PubMed] [Google Scholar]
- [32].Johannsen M, Gneveckow U, Taymoorian K, Thiesen B, Waldöfner N, Scholz R, Jung K, Jordan A, Wust P, Loening Sa. International journal of hyperthermia. 2007;23:315–323. doi: 10.1080/02656730601175479. [DOI] [PubMed] [Google Scholar]
- [33].Asín L, Ibarra MR, Tres A, Goya GF. Pharmaceutical Research. 2012;29:1319–1327. doi: 10.1007/s11095-012-0710-z. [DOI] [PubMed] [Google Scholar]
- [34].Jang JT, Nah H, Lee JH, Moon SH, Kim MG, Cheon J. Angewandte Chemie - International Edition. 2009;48:1234–1238. doi: 10.1002/anie.200805149. [DOI] [PubMed] [Google Scholar]
- [35].Hergt R, Dutz S, Roder M. Journal of Physics: Condensed Matter. 2008;20:385214–385226. doi: 10.1088/0953-8984/20/38/385214. [DOI] [PubMed] [Google Scholar]
- [36].Guardia P, Di Corato R, Lartigue L, Wilhelm C, Espinosa A, Garcia-Hernandez M, Gazeau F, Manna L, Pellegrino T. ACS Nano. 2012;6:3080–3091. doi: 10.1021/nn2048137. [DOI] [PubMed] [Google Scholar]
- [37].Di Corato R, Espinosa A, Lartigue L, Tharaud M, Chat S, Pellegrino T, Ménager C, Gazeau F, Wilhelm C. Biomaterials. 2014;35:6400–6411. doi: 10.1016/j.biomaterials.2014.04.036. [DOI] [PubMed] [Google Scholar]
- [38].Reilly JP. Annals of the New York Academy of Sciences. 1992;649:96–117. doi: 10.1111/j.1749-6632.1992.tb49600.x. [DOI] [PubMed] [Google Scholar]
- [39].Jordan A, Scholz R, Maier-Hauff K, van Landeghem FKH, Waldoefner N, Teichgraeber U, Pinkernelle J, Bruhn H, Neumann F, Thiesen B, et al. Journal of Neuro-Oncology. 2006;78:7–14. doi: 10.1007/s11060-005-9059-z. [DOI] [PubMed] [Google Scholar]
- [40].Huang HS, Hainfeld JF. International Journal of Nanomedicine. 2013;8:2521–2532. doi: 10.2147/IJN.S43770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Widder KJ, Senyei AE, Scarpelli DG. Experimental Biology and Medicine. 1978;158:141–146. doi: 10.3181/00379727-158-40158. [DOI] [PubMed] [Google Scholar]
- [42].Bao G, Mitragotri S, Tong S. Annual review of biomedical engineering. 2013;15:253–82. doi: 10.1146/annurev-bioeng-071812-152409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Park JH, Saravanakumar G, Kim K, Kwon IC. Advanced Drug Delivery Reviews. 2010;62:28–41. doi: 10.1016/j.addr.2009.10.003. [DOI] [PubMed] [Google Scholar]
- [44].Häfeli UO, Sweeney SM, Beresford BA, Humm JL, Macklis RM. Nuclear Medicine and Biology. 1995;22:147–155. doi: 10.1016/0969-8051(94)00124-3. [DOI] [PubMed] [Google Scholar]
- [45].Mah C, Fraites TJ, Zolotukhin I, Song S, Flotte TR, Dobson J, Batich C, Byrne BJ. Molecular therapy. 2002;6:106–112. doi: 10.1006/mthe.2001.0636. [DOI] [PubMed] [Google Scholar]
- [46].Ulbrich K, Holá K, Šubr V, Balandritsos A, Tuček J, Zbořil R. Chemical Reviews. 2016;116:5338–5431. doi: 10.1021/acs.chemrev.5b00589. [DOI] [PubMed] [Google Scholar]
- [47].Lübbe AS, Bergemann C, Riess H, Lãbbe AS, Schriever F, Reichardt P, Possinger K, Matthias M, Dã B, Herrinann F, Gurtler R, et al. Cancer Research. 1996;56:4686–4693. [PubMed] [Google Scholar]
- [48].Goodwin S, Peterson C, Hoh C, Bittner C. Journal of Magnetism and Magnetic Materials. 1999;194:132–139. [Google Scholar]
- [49].Alexiou C, Arnold W, Klein RJ, Parak FG, Hulin P, Bergemann C, Erhardt W, Wagenpfeil S, Lu AS. 2000:6641–6648. [PubMed] [Google Scholar]
- [50].Kubo T, Sugita T, Shimose S, Nitta Y, Ikuta Y, Murakami T. International journal of oncology. 2000;17:309–315. doi: 10.3892/ijo.17.2.309. [DOI] [PubMed] [Google Scholar]
- [51].Pulfer SK, Gallo JM. Journal of Drug Targeting. 1998;6:215–227. doi: 10.3109/10611869808997896. [DOI] [PubMed] [Google Scholar]
- [52].Kharlamov AN, Tyurnina AE, Veselova VS, Kovtun OP, Shur VY, Gabinsky JL. Nanoscale. 2015;7:8003–8015. doi: 10.1039/c5nr01050k. [DOI] [PubMed] [Google Scholar]
- [53].Shapiro B, Kulkarni S, Nacev A, Muro S, Stepanov PY, Weinberg IN. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology. 2015;7:446–457. doi: 10.1002/wnan.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Kost J, Wolfrum J, Langer R. Journal of Biomedical Materials Research. 1987;21:1367–1373. doi: 10.1002/jbm.820211202. [DOI] [PubMed] [Google Scholar]
- [55].Edelman ER, Kost J, Bobeck H, Langer R. Journal of Biomedical Materials Research. 1985;19:67–83. doi: 10.1002/jbm.820190107. [DOI] [PubMed] [Google Scholar]
- [56].Brazel CS. Pharmaceutical Research. 2009;26:644–656. doi: 10.1007/s11095-008-9773-2. [DOI] [PubMed] [Google Scholar]
- [57].Kumar CSSR, Mohammad F. Advanced Drug Delivery Reviews. 2011;63:789–808. doi: 10.1016/j.addr.2011.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Yoo D, Lee J, Shin T, Cheon J. Accounts of Chemical Research. 2011;44:863–874. doi: 10.1021/ar200085c. [DOI] [PubMed] [Google Scholar]
- [59].Dobson J. Nat Nano. 2008;3:139–143. doi: 10.1038/nnano.2008.39. [DOI] [PubMed] [Google Scholar]
- [60].El Haj AJ, Hughes S, Dobson J. Comparative Biochemistry and Physiology Part A. 2003;134 [Google Scholar]
- [61].Mannix RJ, Kumar S, Cassiola F, Montoya-Zavala M, Feinstein E, Prentiss M, Ingber DE. Nature Nanotechnology. 2008;3:36–40. doi: 10.1038/nnano.2007.418. [DOI] [PubMed] [Google Scholar]
- [62].Lee J-H, Kim ES, Cho MH, Son M, Yeon S-I, Shin J-S, Cheon J. Angewandte Chemie - International Edition. 2010;49:5698–5702. doi: 10.1002/anie.201001149. [DOI] [PubMed] [Google Scholar]
- [63].Cho MH, Lee EJ, Son M, Lee J-H, Yoo D, Kim J, Park SW, Shin J-S, Cheon J. Nature Materials. 2012;11:1038–1043. doi: 10.1038/nmat3430. [DOI] [PubMed] [Google Scholar]
- [64].Huang H, Delikanli S, Zeng H, Ferkey DM, Pralle A. Nature Nanotechnology. 2010;5:602–606. doi: 10.1038/nnano.2010.125. [DOI] [PubMed] [Google Scholar]
- [65].Shen Z, Wu A, Chen X. Molecular Pharmaceutics. 2017;14:1352–1364. doi: 10.1021/acs.molpharmaceut.6b00839. [DOI] [PubMed] [Google Scholar]