Abstract
Objective:
This study was designed to examine the feasibility of immersive virtual reality (VR) mirror therapy for upper limb paresis after stroke using a head-mounted display, and provide preliminary evidence of efficacy.
Design:
Ten outpatients with chronic stroke, upper limb hemiparesis, and a low predisposition for motion sickness completed a 12-session program of 30 minutes each of immersive VR mirror therapy. The VR system provided the illusion of movement in the hemiparetic upper limb while suppressing the visual representation of the non-paretic side. Feasibility was assessed via patient compliance, adverse event tracking, the System Usability Scale, and the Simulator Sickness Questionnaire. Preliminary efficacy was evaluated using the Fugl-Meyer Upper Extremity (FM-UE) and Action Research Arm Test.
Results:
Immersive VR mirror therapy for patients with chronic stroke was safe, well-tolerated, and without adverse events, such as simulator sickness. Motor outcomes revealed a small improvement for the FM-UE from 21.7 (SD= 8.68) to 22.8 (SD= 9.19) that did not achieve statistical significance (p=0.084).
Conclusion:
Four weeks of immersive virtual reality mirror therapy was well-tolerated by chronic stroke patients. Our findings support further clinical trials of immersive VR technologies and visually-enhanced mirror therapies for stroke survivors.
Keywords: Stroke, Rehabilitation, Virtual Reality, Occupational Therapy
BACKGROUND:
Stroke is a leading cause of acquired disability in the United States. According to the American Stroke Association, nearly 800,000 new cases are reported each year1, with approximately 80% of survivors experiencing motor impairment2. Motor impairments of the upper limb are particularly common and enduring3,4. Approximately 50% of individuals who experience upper limb paralysis following stroke continue to face functional deficits four years after injury5.
Mirror therapy is a low-cost intervention that utilizes visual illusion to promote motor recovery. In this therapy, a mirror or mirror box (a mirror mounted on the side of a lightweight enclosure that surrounds the affected arm) is positioned at the mid-sagittal plane, obstructing the impaired extremity from a stroke survivor’s view. Subjects are instructed to focus their visual attention on the mirror image of the unimpaired extremity during movement, which creates the illusion of two limbs moving synchronously and symmetrically without deficit6. A 2018 Cochrane Review examining 62 studies (comprising 1982 participants) found moderate-quality evidence that mirror therapy has a significant beneficial effect on motor function and motor impairment following stroke, and may improve activities of daily living7.
While the simplicity of mirror box therapy offers an appealing low-cost and portable option for stroke patients, there are important limitations to this treatment. Therapeutic activities are limited by the physical confines of the modality, with exercises largely restricted to distal movements and simple functional activities. While free-standing mirrors enable a more extensive range of motion for therapeutic activities, they provide less protection from environmental distractions.
Virtual reality (VR) is a technology that may allow the application of this modality beyond the physical and creative bounds of the mirror box. While other virtual reality interventions to date have not shown efficacy for upper limb training when used in isolation, a recent meta-analysis suggests a statistically significant benefit (considering low-quality evidence) when provided in addition to usual care8. VR interventions provide enriched opportunities for the integration of goal-oriented tasks and repetition of movement, increasingly considered critical components for neurological recovery9,10. The modality is also an appealing option for patients, who perceive virtual tasks to be interesting and motivating11.
Early virtual reality systems were expensive, complex to operate and lacked the technological capabilities required to emulate natural movement, calling into question their value for the provision of mirror therapy6. These technologies have since progressed considerably. Virtual reality systems differ significantly in their level of immersion or “presence” in the virtual environment, with systems ranging from standard computer monitors, to “interface devices” (e.g. gloves, joysticks) with haptic feedback, to fully isolating head-mounted systems12.
Many clinical trials have avoided the use of head-mounted goggles and visually immersive VR due to concerns regarding safety and cybersickness12. For the purposes of mirror therapy, however, we propose that a more visually immersive environment would provide a more convincing illusion. Moreover, the use of immersive VR with head mounted goggles allows the option of providing the illusion that only the paretic arm is moving, which is not feasible with conventional mirror therapy. To our knowledge, patient tolerance of immersive virtual reality has not been studied in the chronic stroke population. This pilot study sought to demonstrate the feasibility and preliminary efficacy of a fully immersive virtual reality system using head-mounted goggles for the provision of mirror therapy in the chronic stroke population.
METHODS:
This study was registered with clinicaltrials.gov and has been assigned the following identifier: NCT03582397.
Subjects
Eleven community-dwelling individuals with chronic stroke (5 women, 6 men) met inclusion criteria and volunteered to participate in this study. Inclusion criteria were (1) adults between the ages of 18 and 85, six months or more following an ischemic or hemorrhagic stroke (2) reduced motor control of the upper limb as defined by a score of 10–50 on the Fugl-Meyer Test of Upper Extremity Function (3) ability to follow two-step commands (4) ability to provide informed consent. Exclusion criteria included (1) significant visual or visual-perceptual deficits, neuropsychological impairments or orthopedic conditions limiting participation in the protocol, as determined by the treatment team (2) concurrent participation in another study protocol related to motor function after stroke (3) high susceptibility to motion sickness, as evidenced by a score of 26 or greater on the Motion Sickness Susceptibility Questionnaire - Short Form (MSSQ-Short), corresponding to the 90th percentile for this test (4) concurrent participation in occupational or physical therapy for upper limb motor retraining. All subjects screened for this study were deemed eligible to participate. Ten of eleven subjects completed the full protocol and are described in Table 1.
Table 1:
Summary of subject characteristicsTable
| Subject | Gender | Age (Years) | Time since Stroke (In months) | MSSQ-Short Score, Raw | MOCA | Baseline Fugl-Meyer Score |
|---|---|---|---|---|---|---|
| 1 | Female | 64 | 160 | 0 | 23 | 22 |
| 2 | Male | 42 | 48 | 0 | 26 | 27 |
| 3 | Male | 25 | 132 | 0 | 27 | 32 |
| 4 | Male | 45 | 12 | 0 | 18 | 11 |
| 5 | Female | 63 | 36 | 1 | 23 | 11 |
| 6 | Female | 64 | 102 | 0 | 27 | 24 |
| 7 | Male | 62 | 51 | 2 | 18 | 34 |
| 8 | Male | 62 | 109 | 0.2 | 28 | 14 |
| 10 | Female | 67 | 142 | 0 | 20 | 28 |
| 11 | Male | 47 | 27 | 0 | 24 | 14 |
| Total: 10 Subjects | 4 Female/6 Male | Range: 25–67 Mean: 54.1, (SD 13.0), Median 62 |
Range: 12–160 months, Mean: 81.9 (SD 50.5), Median 76.5 | Range: 0–2/54 | Range: 18–28, Mean: 23.4 (SD 3.5), Median 23.5 | Range: 11–34, Mean: 21.7 (SD 8.2), Median 23 |
Participants ranged in age from 25 to 68 years of age, with duration post-stroke ranging from 1–13 years (mean 81.9 months, SD 50.46, median 76.7). Six patients reported hemorrhagic stroke and four reported ischemic stroke. Six patients had a right hemiparesis and four had left hemiparesis.
The patient population exhibited a range of cognitive and motor performance, with Montreal Cognitive Assessment scores ranging from 18–28, with scores above 26 indicating normal cognitive function and Fugl-Meyer Upper Extremity scores ranging from 11–34, corresponding to classifications of No/Poor to Limited Capacity13,14. All subjects completed the Motion Sickness Susceptibility Questionnaire Short Form to assess risk of cyber-sickness from immersive virtual reality therapy. The scale combines childhood and adult responses to motion into a composite value, with 100 representing maximum susceptibility15. Seven of ten subjects reported no adverse experiences related to motion either as children or adults. Three of ten subjects reported mild responses to motion, scoring 1–2 on the MSSQ-Short. These scores are considerably lower than the mean score of 12.4 (SD 9.4) established through normative sampling for this tool16. Three of ten subjects reported prior experience with conventional mirror therapy.
All subjects provided written informed consent to participate in this study. The experimental protocol was approved by the Institutional Review Board at Columbia University Medical Center, where all study appointments were conducted.
Measures
The upper extremity (UE) motor section of the Fugl-Meyer Assessment (FMA)17 served as a baseline measure of motor performance. The FMA is a widely-used metric of motor recovery and well-established research tool in the stroke population18. The UE-FMA consists of 33 items. Each item is rated on a 3-point ordinal scale ranging from 0 (no movement) to 3 (normal movement). A score of 66 indicates normal UE movement. Subjects also completed the Action Research Arm Test19 (ARAT), a performance-based measure that assesses UE activity limitations. The ARAT consists of 19 items arranged in four subscales: grasp, grip, pinch and gross arm movement. Each item is rated on a 4-point ordinal scale ranging from 0 (unable to perform) to 3 (normal performance). Scores range from 0–57, with higher scores indicating greater UE capacity20. Both clinical motor assessments were conducted prior to and following the intervention by a single, independent assessor who was not present during therapy sessions.
The Star Cancellation Test was added to baseline testing after the protocol had already begun to assess acceptability of the intervention for individuals with perceptual deficits and to detect possible improvement with use of the virtual reality system21. The measure was performed for eight of ten subjects. None of the subjects who completed Star Cancellation screening tested positive for unilateral hemi-spatial neglect in the near extra-personal space.
Adherence to the protocol was tracked via patient attendance and any adverse events were recorded. The feasibility of the system was measured using the System Usability Scale, a ten-item patient questionnaire, and the Simulator Sickness Questionnaire, a checklist designed to assess physical symptoms following high-fidelity simulator training22,23. These measures were completed by subjects following their initial and final treatment sessions.
Patient observation was used to track progression through the virtual reality training. A subjective observation scale was also integrated to record the frequency of movement in the impaired extremity, which subjects were instructed not to move during treatment.
Intervention
Treatment sessions utilized WiseMind Software® developed by Realiteer (Redwood City, CA). Gaming environments and tasks were conceptualized or augmented by the study team and engineered by Realiteer to optimize usability and fidelity to the intended form of mirror therapy. This intervention represents a novel iteration of existing WiseMind embodiment and mirroring technology. The software was run on a laptop computer and utilized a commercially-available virtual reality technology, Oculus Rift (Oculus VR, Menlo Park, CA). The virtual reality system is comprised of head-mounted goggles which provide positional tracking, stereoscopic 3D imaging and integrated audio, two tabletop infrared LED sensors and two hand controllers, which capture motion and house action buttons, thumb-sticks, and triggers for gameplay.
Patients were positioned in an armless chair in the center of a private treatment room, with adequate space for safe movement. Treatment sessions were supervised by an occupational therapist or a trained assistant. Patients engaged in treatment by embodying a first-person view of a virtual avatar, represented by a man or woman wearing a short-sleeved shirt. Prior to donning the headset, virtual parameters were set to best match the patient’s physical characteristics including sex, height, weight, and skin tone. One patient with extensive tattoos on his upper extremities utilized a custom avatar wearing a tight-fitting long-sleeved shirt to ensure his physical form within the system provided a realistic representation of his upper limbs.
Subjects utilized one Touch controller positioned in their intact hand and fastened to their wrist for safety. Within the headset, subjects visualized a mirrored representation of their movements superimposed on the impaired upper extremity and a stationary representation of their intact limb. Subjects were instructed to complete all treatment activities using their unaffected upper extremity and to maintain their affected arm in a relaxed state throughout treatment. The system was capable of capturing and portraying movement at the shoulder, elbow and wrist. Digit movement was limited to gross grasp and release controlled by trigger squeeze.
Patients completed twelve virtual reality sessions, incorporating three five-minute treatment blocks performed twice per session for a total of thirty minutes of direct training. Treatment frequency and dose were selected to mimic typical amounts of practice provided in conventional occupational therapy.
While the software did not include adjustable difficulty levels, the therapist adjusted the difficulty of the tasks selected within the virtual environment to provide a challenging but achievable set of tasks to optimize patient performance. For example, in the dining room scenario, the therapist might advance a participant from the simple task of moving a dinner plate (an inherently stable object) from one location to another, to the more challenging task of placing a wine glass (a less stable object) in the correct location without tipping it over. Patients unable to complete items independently were provided with fading verbal cues to aid problem solving, motor planning or use of hardware. Items were presented in a uniform sequence and were considered complete when they were performed correctly for a set number of repetitions. An optional rest break was offered at the midpoint of training. Treatment blocks were designed to emulate best practice in conventional mirror therapy and are described below.
Segment I: Exercise (5 minutes)
In this treatment block, patients completed basic range of motion exercises demonstrated and described by a human avatar. Exercises included shoulder flexion/extension, abduction/adduction, elbow flexion/extension, forearm pronation/supination, wrist flexion/extension, grasp/release and composite motions such as punching. Patients completed each exercise for 10 repetitions before moving onto the next exercise.
Segment II: Rock Stacking (5 minutes)
In this treatment block, patients were asked to pick up rocks of various shapes and sizes positioned on a virtual tabletop. Patients were asked to stack as many rocks as possible without knocking any over.
Segment III: Functional Task (5 minutes)
In this treatment block, patients engaged in various functional tasks in the context of a dining room. Subjects were asked to stack plates, set up a tea set, right upturned objects such as a wine bottle or goblet, move fruit from one plate to another, and unset and reset a table. Patients completed tasks in the same sequence each time, moving onto the next after successfully demonstrating the prior task.
RESULTS:
Feasibility
Ten of eleven subjects who began the protocol completed all study visits. One subject withdrew from the study following treatment session seven of twelve due to worsening shoulder pain in the non-paretic upper extremity, a pre-existing condition that was not disclosed by the patient during study screening.
Subjects completed the Simulator Sickness Questionnaire directly following treatment after the first and final session to assess initial tolerance of the intervention and change over time. Total Simulator Sickness scores averaged ¼8 following the initial treatment session and 1.6 following the final treatment session, indicating little to no cyber sickness. Four subjects scored equivalently at sessions one and twelve, three reported worsening symptoms and three reported symptom improvement. All ten subjects completed the entire twelve-session treatment protocol with no requests for additional rest breaks and no adverse events reported.
Subject perceptions of system usability were recorded immediately following the final treatment session using the System Usability Scale, with higher scores reflecting enhanced perceptions of usability. Scores ranged from 40–100, with a mean of 76 and a median of 80. Scores beyond 68 on this scale are classified as above average24.
Informally, patients appeared to enjoy using the system, stating that the sessions passed by quickly and were entertaining. Several commented on the novelty of seeing their paretic arm move normally within the system, particularly into positions typically restricted by contracture. Four patients spontaneously reported a change in sensation with treatment, with one noting, “For a second, I really felt my arm moving…it’s like this arm is alive…My whole arm is there again. Before it wasn’t there.”
Subjects were prompted to maintain their affected extremity in a relaxed position during gameplay and not to attempt the exercises with it. However, many demonstrated involuntary movements mirroring the actions of the intact extremity to varying degrees. To capture this phenomenon more objectively, frequency of movement of the affected extremity was tracked for each five-minute segment using a simple observation scale ranging from absent to maximal movement (67–100% of the time). While physical demands on the intact extremity were highest during the Physical Exercise level, “maximal” involuntary movements of the affected arm were most frequent during task-based segments (Rock Stacking and Dining) as compared to the Physical Exercise segment.
Due to the exploratory nature of this study, subjects were not excluded on the basis of cognitive limitations. All subjects (MoCA range 18–28) were able to learn to use the system, with varied degrees of assistance in the form of verbal cues. Intermittent cues were provided to maintain visual attention to the affected arm and acclimate to the mirrored movements represented in the headset. Subjects with lower cognitive scores required occasional cues for problem solving and to simplify tasks for optimal success. One subject was noted to “lose” objects in his left visual field during gameplay, but was able to complete the intervention with fading cues and practice. Subjects with impaired sitting balance benefitted from verbal cues to maintain a safe seated position and utilize upper extremity movements, rather than trunk movements, to complete reaching tasks.
Motor Outcomes
Statistical analyses were completed using Microsoft® Excel® 2013 and SPSS for Mac, Version 24. A paired-samples t-test was conducted to compare Fugl Meyer Upper Extremity Scores from baseline to post-test. A normal distribution was confirmed using the Shapiro-Wilk test (p > .05 for both pre and post test data). There was a small improvement in mean Fugl Meyer scores that did not achieve statistical significance from baseline (M=21.7, SD= 8.68) to post-test (M=22.8, SD= 9.19); p=0.084. A paired-samples t-test was also utilized to compare Action Research Arm Test Scores from baseline to post-test. No significant difference was seen from baseline (M=9.1, SD=8.05) to post-test (M=9.8, SD=9.08); p=0.33). Because assumptions of normality were violated as assessed by the Shapiro-Wilk for both pre (p=.014) and post (p=.008) data, a secondary analysis was performed using the Wilcoxon signed rank test, which also failed to demonstrate any statistically significant difference from pre- to post- (p=0.461).
DISCUSSION
The results of this pilot study suggest that immersive virtual reality mirror therapy is feasible for patients with chronic stroke with respect to safety, adherence and tolerance. As with all pilot studies with a limited sample size, these results should be interpreted with caution and may not be generalizable to the stroke population at-large. While some patients did report mild symptoms of simulator sickness following treatment, complaints were relatively mild, did not necessitate intervention, and did not impede completion of the study protocol. Of note, our population was unusually low scoring on the motion sickness susceptibility test at baseline, which could give an optimistic impression of tolerability in the general population. While we did not explicitly state that patients with high scores would be excluded from the study, it is possible that our subjects understated their susceptibility during screening in the interest of gaining entry. Nonetheless, it is clear that many, if perhaps not all, stroke survivors are able to tolerate this type of therapy without cybersickness as a complication.
While improvements on measures of motor performance did not achieve statistical significance, this may be due to a variety of factors. The small sample size is likely a contributing factor, and the favorable trend the UEFM may achieve statistical significance in a larger study. Another factor may have been the relatively severely impaired population studied, who may be less capable of achieving motor improvements with exercise therapy. Intensity of treatment may also have been insufficient. A recent meta-analysis of VR interventions for stroke identified a trend suggesting that a higher dose (upwards of 15 hours, as compared to our 6 hours) may be more efficacious8. Lastly, interventions in the chronic phase of stroke recovery generally provide only modest benefits in motor performance, and testing this therapy earlier post-stroke may yield larger benefits.
The successful application of a fully immersive virtual reality system may lay the groundwork for additional treatment options for stroke rehabilitation. Virtual reality platforms provide a richness of experience and credibility that cannot be achieved by semi-immersive modalities. They also enable the provision of treatment in alternative environments that aid relaxation, more closely approximate the home, or build safety awareness without jeopardizing patient safety. Immersive therapy also provides the unique benefit of occluding the hospital or clinic environment, minimizing auditory and visual distractions while highlighting preferred stimuli (in this case, the affected extremity).
Virtual mirror therapy and other forms of immersive VR allow the creation of a variety of visual distortions for therapeutic purposes. In our study, we used this capability to provide the illusion that the non-paretic arm was motionless, and transposed this movement to the visual representation of the impaired arm. This is not feasible with conventional mirror therapy. In future studies, this treatment paradigm could be compared with virtual mirror therapy that shows both arms moving in symmetric fashion to determine relative efficacy. Other distortions with potential therapeutic value could include a non-mirrored therapy providing a representation of the paretic arm with smaller movements than are actually performed to explore whether this might encourage the user to increase their active arc of movement to accomplish an assigned task.
With respect to mirror therapy itself, virtual reality allows us to convert simple movements into functional tasks, perhaps providing more meaningful, engaging treatment for patients. Functional tasks also provide additional opportunities for cognitive and perceptual training and may generalize more readily to real-life environments. This implementation of mirror therapy could allow patients with injuries or movement precautions to engage in some form of therapy without risking injury.
While this form of mirror therapy is more expensive than conventional mirror box treatment, it does represent a more accessible and self-directed alternative to existing rehabilitation technologies. Stand-alone VR headsets are now commercially available for as low as $200 (e.g. Oculus Go®), and wider availability and adoption of lower-cost consumer versions of these devices is likely in the near future. Therefore, virtual mirror therapy may function as useful preparatory activity/primer prior to treatment or adjunct treatment to increase engagement during hospital downtime. The coupling of virtual reality mirror therapy with conventional treatment may also increase its efficacy, as has been demonstrated in traditional mirror therapy paradigms8.
Of note, many subjects who participated in this pilot demonstrated non-volitional movements of the impaired upper extremity with treatment, despite explicit instruction to maintain their arm in a relaxed state. This phenomenon may carry a range of implications, perhaps corresponding to a patient’s level of virtual presence within the system or responsiveness to treatment. Also of note, patients appeared to demonstrate an increased in non-volitional movements during activity-based levels, perhaps suggesting additional benefit as compared to rote exercise. Future studies should incorporate more objective data collection using movement tracking technologies to better understand this observation.
Future studies should also explore the use of virtual reality mirror therapy as an adjunct to conventional treatment, the effect of encouraging the paretic arm to move during treatment, and the addition of haptic feedback to the system.
In summary, immersive virtual reality mirror therapy appears safe and feasible in individuals with chronic hemiparesis after stroke. Further studies are needed to determine optimal parameters for training, and to determine efficacy.
Figure 1:

System setup for individual with left hemiplegia including laptop computer, tabletop sensors, headset and controller.
Figure 2:
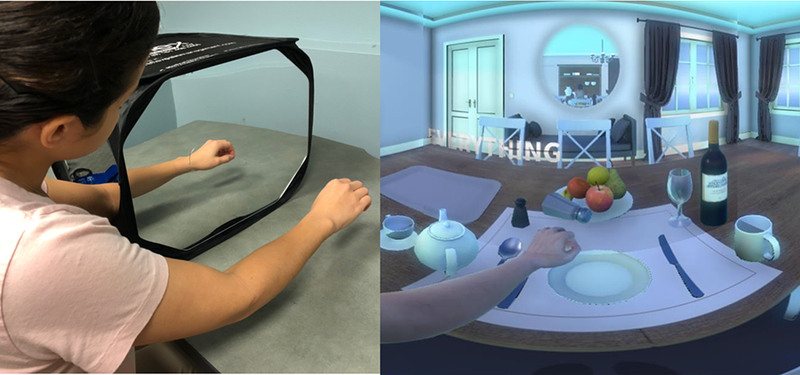
Comparison of conventional mirror box therapy with immersive virtual reality mirror therapy. Note suppression of the non-paretic upper limb within the enriched virtual environment.
Figure 3:

Screenshot of shoulder flexion exercise guided by avatar therapist, as seen through virtual reality headset.
Figure 4:
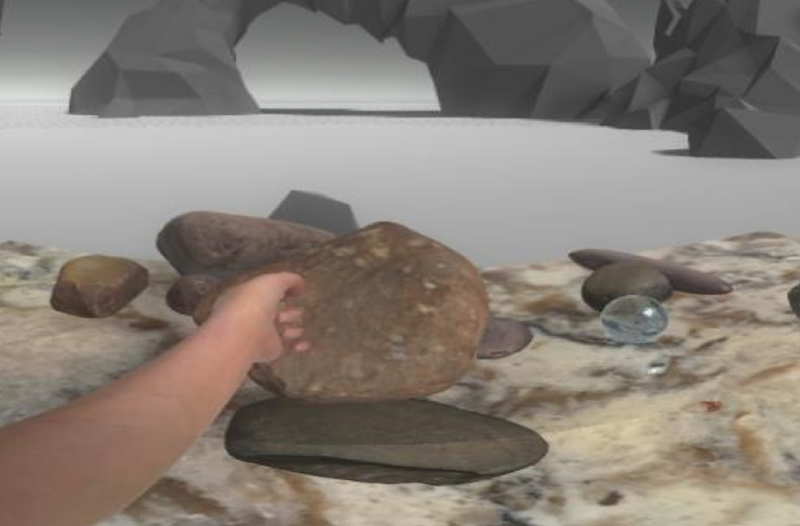
Screenshot of rock stacking activity, as seen through virtual reality headset.
Table 2:
Summary of motor outcome data
| Subject | Baseline Fugl-Meyer | Post Fugl-Meyer | % Change | Baseline ARAT | Post ARAT | % Change |
|---|---|---|---|---|---|---|
| 1 | 22 | 23 | 4.5% | 4 | 4 | 0.0% |
| 2 | 27 | 27 | 0.0% | 11 | 10 | −9.1% |
| 3 | 32 | 37 | 15.6% | 18 | 24 | 33.3% |
| 4 | 11 | 10 | −9.1% | 3 | 3 | 0.0% |
| 5 | 11 | 14 | 27.3% | 3 | 3 | 0.0% |
| 6 | 24 | 26 | 8.3% | 8 | 7 | −12.5% |
| 7 | 34 | 34 | 0.0% | 27 | 27 | 0.0% |
| 8 | 14 | 14 | 0% | 3 | 3 | 0.0% |
| 10 | 28 | 28 | 0% | 11 | 14 | 27.3% |
| 11 | 14 | 15 | 7.10% | 3 | 3 | 0.0% |
Acknowledgments:
The authors would like to acknowledge Lauri Bishop, PhD, DPT and Adam Blanchard, Exercise Physiologist for their guidance and assistance with this project.
Author disclosures: Realiteer, Inc. – Loan of research equipment; Grant funding: T35 AG044303. Related Presentations: “Virtual Reality Mirror Therapy for Stroke: Let’s Turn it Around!” American Academy of Physical Medicine and Rehabilitation Annual Assembly, October 2018.
Contributor Information
Lynne M. Weber, Department of Rehabilitation and Regenerative Medicine, Columbia University Medical Center.
Dawn M. Nilsen, Associate Professor of Rehabilitation and Regenerative Medicine at Columbia University Medical Center.
Glen Gillen, Professor and Director, Programs in Occupational Therapy, Vice Chair, Department of Rehabilitation and Regenerative Medicine, Assistant Dean, Vagelos College of Physicians and Surgeons, Columbia University.
Jin Yoon, Columbia University Vagelos College of Physicians and Surgeons.
Joel Stein, Simon Baruch Professor and Chair Department of Rehabilitation and Regenerative Medicine, Columbia University College of Physicians and Surgeons, Chair, Department of Rehabilitation Medicine, Weill Cornell Medical College, Physiatrist-in-Chief, New York Presbyterian Hospital.
References:
- 1.Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics-2017 Update: A Report From the American Heart Association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Langhorne P, Coupar F, Pollock A. Motor recovery after stroke: a systematic review. Lancet Neurol. 2009;8(8):741–754. doi: 10.1016/S1474-4422(09)70150-4 [DOI] [PubMed] [Google Scholar]
- 3.Lai S-M, Studenski S, Duncan PW, Perera S. Persisting Consequences of Stroke Measured by the Stroke Impact Scale. 2002. doi: 10.1161/01.STR.0000019289.15440.F2 [DOI] [PubMed] [Google Scholar]
- 4.Kwakkel G, Kollen BJ, van der Grond J, Prevo AJH. Probability of Regaining Dexterity in the Flaccid Upper Limb. Stroke. 2003;34(9):2181–2186. doi: 10.1161/01.STR.0000087172.16305.CD [DOI] [PubMed] [Google Scholar]
- 5.Broeks JG, Lankhorst GJ, Rumping K, Prevo AJ. The long-term outcome of arm function after stroke: results of a follow-up study. Disabil Rehabil. 1999;21(8):357–364. http://www.ncbi.nlm.nih.gov/pubmed/10503976. Accessed October 3, 2018. [DOI] [PubMed] [Google Scholar]
- 6.Ramachandran VS, Altschuler EL. The use of visual feedback, in particular mirror visual feedback, in restoring brain function. Brain. 2009;132(7):1693–1710. doi: 10.1093/brain/awp135 [DOI] [PubMed] [Google Scholar]
- 7.Thieme H, Morkisch N, Mehrholz J, et al. Mirror therapy for improving motor function after stroke (Review). Cochrane Database Syst Rev. 2018;(7). doi: 10.1002/14651858.CD008449.pub3.www.cochranelibrary.com [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laver K, Lange B, George S, Deutsch J, Saposnik G, Crotty M. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev. 2017;(11):CD008349. doi: 10.1002/14651858.CD008349.pub4.www.cochranelibrary.com [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet. 2011;377(9778):1693–1702. doi: 10.1016/S0140-6736(11)60325-5 [DOI] [PubMed] [Google Scholar]
- 10.Veerbeek JM, van Wegen E, van Peppen R, et al. What Is the Evidence for Physical Therapy Poststroke? A Systematic Review and Meta-Analysis. Quinn TJ, ed. PLoS One. 2014;9(2):e87987. doi: 10.1371/journal.pone.0087987 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewis GN, Rosie JA. Virtual reality games for movement rehabilitation in neurological conditions: how do we meet the needs and expectations of the users? Disabil Rehabil. 2012;34(22):1880–1886. doi: 10.3109/09638288.2012.670036 [DOI] [PubMed] [Google Scholar]
- 12.Henderson A, Korner-Bitensky N, Levin M. Topics in Stroke Rehabilitation Virtual Reality in Stroke Rehabilitation: A Systematic Review of its Effectiveness for Upper Limb Motor Recovery. 2014. doi: 10.1310/tsr1402-52 [DOI] [PubMed] [Google Scholar]
- 13.Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: A Brief Screening Tool For Mild Cognitive Impairment. J Am Geriatr Soc. 2005;53(4):695–699. doi: 10.1111/j.1532-5415.2005.53221.x [DOI] [PubMed] [Google Scholar]
- 14.Singer B, Garcia-Vega J. The Fugl-Meyer Upper Extremity Scale. 2017. doi: 10.1016/j.jphys.2016.08.010 [DOI] [PubMed] [Google Scholar]
- 15.Golding JF. Predicting individual differences in motion sickness susceptibility by questionnaire. Pers Individ Dif. 2006;41:237–248. doi: 10.1016/j.paid.2006.01.012 [DOI] [Google Scholar]
- 16.Golding JF. Predicting individual differences in motion sickness susceptibility by questionnaire. 2006. doi: 10.1016/j.paid.2006.01.012 [DOI] [Google Scholar]
- 17.Fugl-Meyer AR, Jääskö L, Leyman I, Olsson S, Steglind S. The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand J Rehabil Med. 1975;7(1):13–31. http://www.ncbi.nlm.nih.gov/pubmed/1135616. Accessed October 3, 2018. [PubMed] [Google Scholar]
- 18.Gladstone DJ, Danells CJ, Black SE, Article R. The Fugl-Meyer Assessment of Motor Recovery after Stroke: A Critical Review of Its Measurement Properties. Neurorehabil Neural Repair. 2002;16(3):232–240. http://journals.sagepub.com/doi/pdf/10.1177/154596802401105171. Accessed July 20, 2018. [DOI] [PubMed] [Google Scholar]
- 19.Lyle RC. A performance test for assessment of upper limb function in physical rehabilitation treatment and research. Int J Rehabil Res. 1981;4(4):483–492. http://www.ncbi.nlm.nih.gov/pubmed/7333761. Accessed October 3, 2018. [DOI] [PubMed] [Google Scholar]
- 20.Lang CE, Bland MD, Bailey RR, Schaefer SY, Birkenmeier RL. Assessment of upper extremity impairment, function, and activity after stroke: foundations for clinical decision making. J Hand Ther. 2013;26(2):104–115. doi: 10.1016/j.jht.2012.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Friedman PJ. The Star Cancellation Test in acute stroke. Clin Rehabil. 1992;6:23–30. http://journals.sagepub.com/doi/pdf/10.1177/026921559200600104. Accessed September 21, 2018. [Google Scholar]
- 22.Brooke J SUS: a “quick and dirty” usability scale In: Jordan PW Thomas B Weerdmeester B, McClelland I, eds. Usability Evaluation in Industry. London: Taylor & Francis; 1996:189–194. [Google Scholar]
- 23.Kennedy RS, Lane NE, Berbaum KS, Lilienthal MG. Simulator Sickness Questionnaire: An Enhanced Method for Quantifying Simulator Sickness. Int J Aviat Psychol. 1993;3(3):203–220. doi:10.1207/ [Google Scholar]
- 24.Brooke J SUS: A Retrospective. J Usability Stud. 2013;8(2):29–40. http://delivery.acm.org/10.1145/2820000/2817913/p29-brooke.pdf?ip=156.111.104.191&id=2817913&acc=ACTIVESERVICE&key=7777116298C9657D.CCAFA7F43E96773E.4D4702B0C3E38B35.4D4702B0C3E38B35&__acm__=1537557115_d30c95d905aeca27cfefcd457e536203. Accessed September 21, 2018. [Google Scholar]


