Abstract
OBJECTIVES:
Optimistic expectations about prognosis by surrogate decision-makers in ICUs are common, but there are few data about the causes and clinical consequences. Our objective was to determine the causes of optimistic expectations about prognosis among surrogates and whether it is associated with more use of life support at the end of life.
DESIGN:
Prospective, multicenter cohort study from 2009–2012.
SETTING:
Twelve ICUs from multiple regions of the United States.
PARTICIPANTS:
The surrogates and physicians of 275 incapacitated ICU patients at high risk of death.
MEASUREMENTS & MAIN RESULTS:
Surrogates and physicians completed a validated instrument assessing their prognostic expectations for hospital survival. We determined the proportion of surrogates with optimistic expectations, defined as a prognostic estimate that was at least 20% more optimistic than the physician’s, then determined how frequently this arose from surrogates miscomprehending the physicians’ prognosis versus holding more hopeful beliefs compared to the physician. We used multivariable regression to examine whether optimistic expectations were associated with length of stay, stratified by survival status, and time to withdrawal of life support among nonsurvivors.
Overall, 45% of surrogates (95% CI 38–51%) held optimistic expectations about prognosis, which arose from a combination of misunderstanding the physician’s prognostic expectations and from holding more hopeful beliefs compared to the physician. Optimistic expectations by surrogates were associated with significantly longer duration of ICU treatment among nonsurvivors before death (β-coefficient= 0.44; 95% CI: 0.05–0.83; p=0.027), corresponding to a 56% longer ICU stay. This difference was associated with a significantly longer time to withdrawal of life support among dying patients whose surrogates had optimistic prognostic expectations compared to this who did not (β coefficient= 0.61; 95% CI: 0.16–1.07; p=0.009).
CONCLUSIONS:
The prevalent optimism about prognosis among surrogates in ICUs arises both from surrogates’ miscomprehension of physicians’ prognostications and from surrogates holding more hopeful beliefs. This optimism is associated with longer duration of life support at the end of life.
Keywords: Prognosis, Decision making, Communication, Critical Illness, End of life
summary:
In a multicenter study, optimism about prognosis by surrogates was common & associated with more use of life support in dying patients.
BACKGROUND
Hundreds of thousands of patients annually die in or shortly after an ICU admission, generally after decisions to forego life-sustaining treatments.1–3 In most cases, patients are too ill to participate in these decisions and clinicians therefore turn to patients’ surrogate decision-makers to help make end-of-life decisions that align with the patient’s values and preferences.3,4 In order to be informed participants in decision-making, surrogates need a clear understanding of the patient’s prognosis with intensive treatment. However, numerous studies suggest that surrogates of patients with advanced illness often have overly optimistic expectations about prognosis.5–8 Although there is inherent uncertainty in physicians’ predications for individual patients, physicians’ survival predictions are significantly more accurate than surrogates’ in the setting of critical illness.8 ICU physicians’ discriminant accuracy is also superior to existing risk prediction models.9,10 Physicians’ judgments of a poor prognosis are independently predictive of patient outcomes among patients who died receiving full life support, lessening concerns that physicians’ prognostic accuracy is solely a result of a self-fulfilling prophecy.11 Despite the imperfect accuracy of physicians’ prognostications, surrogate decision-makers highly value physicians’ predications, and the vast majority of surrogates wish to hear physicians’ prognostications despite this uncertainty.12
Although clinicians cite unrealistic expectations about prognosis by surrogates as a barrier to good decision-making in advanced illness13, there are two important gaps in knowledge about this issue. First, there is a paucity of empirical data about the causes of surrogates’ optimistic expectations. The prevailing assumption is that surrogates’ optimistic expectations arise from miscomprehension of physicians’ prognostications. However, insights from decision science14 as well as single-center studies in ICUs8,15–18 suggest that cognitive biases-rather than solely misunderstandings-may also contribute. One such bias that may be relevant, termed the better-than-average effect, is the tendency of individuals to rate themselves as more likely to have better outcomes than their peers.14 Lack of knowledge of the causes of surrogates’ misperceptions about prognosis makes it difficult to know how to best intervene to improve communication about prognosis.
Second, it is uncertain whether surrogates’ optimistic expectations about prognosis contribute to more intensive treatment at the end of life. According to traditional decision theory (e.g., expected utility theory), individuals will be less willing to authorize intensive treatment as the likelihood of a good outcome diminishes.19 However, modern decision theory suggests that individuals do not behave in purely rational ways and instead that decisions may be influenced by strong emotions and a variety of cognitive biases.20 For example, some have argued that the emotional difficulty of authorizing treatment withdrawal for another person may make surrogates continue life support in the face of a poor prognosis.21 Using hypothetical vignettes with ICU surrogates, Zier and colleagues found that 25% of surrogates were unwilling to withdraw life support when informed that the treating physician judged there to be a <1% chance of survival to hospital discharge.22 Therefore, it remains uncertain whether improving the effectiveness of communication about prognosis should be expected to change end-of-life treatment decisions.
We therefore conducted this prospective, multi-center cohort study to determine the prevalence and causes of optimistic expectations about prognosis among surrogates of ICU patients and whether surrogates’ optimistic expectations are associated with health care utilization at the end of life.
METHODS
Study Design:
From October 2009 through October 2012, we conducted a prospective multi-center cohort study in 12 ICUs in the NHLBI ARDS Clinical Trials Network. The medical centers were located in California, Massachusetts, North Carolina, Pennsylvania, and Washington.
Patients and Procedures
We enrolled incapacitated, mechanically ventilated, adult patients at high risk of death or severe, long-term functional impairment, their surrogate decision-makers, and their attending physician. Patient inclusion criteria included lack of decision making capacity, a diagnosis of ARDS using traditional clinical criteria23, an APACHE II score ≥ 25 or ≥ 50% chance of severe long-term functional impairment as judged by their attending physician (defined as requiring ongoing assistance with at least two activities of daily living). Decisional incapacity was determined by clinical assessment by the patient’s treating physician. We excluded patients who were awaiting organ transplantation, actively dying, or had no surrogate available. We enrolled the patient’s legally designated surrogate decision-maker. If there was no legally designated surrogate, we enrolled the individual acting as the patient’s decision maker for clinical care decisions. We excluded individuals who were not able to complete study procedures in English. We enrolled the patient’s attending physician of record or his/her designee, defined as a physician directly supervised by the attending physician. This study was approved by the Institutional Review Board of each participating institution. All participants provided written consent for all study procedures; the patient’s surrogate provided proxy consent for review of the patient’s medical record.
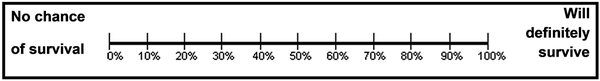
On patients’ fifth day of mechanical ventilation and within one hour of each other, surrogates and physicians independently estimated the likelihood that the patient would survive the hospitalization using a previously validated question: “What do you think are the chances that your loved one/the patient will survive this hospitalization if the current plan of care stays the same?”18,24 Figure 1 illustrates the probability scale used to record subject’s prognostic estimates. To minimize the chance of response errors among participants with limited numeracy, the anchors on the response scale contained non-numeric expressions of risk (i.e., “No chance of survival” and “Will definitely survive”). Such scales are well validated to assess risk perceptions and may be less affected by limited numeracy than other methods to elicit quantitative risk estimates.25–27 Surrogates and physicians were blinded to the other’s response. Surrogates also recorded what they perceived to be the physician’s prognostic expectation with the following question: “If you had to guess, what do you think the doctor thinks is the chance that your loved one will survive this hospitalization if the current plan of care stays the same?” All data was collected after at least one family meeting had occurred.
FIGURE 1. Outcome Measure to Assess Surrogates’ Perceptions of Prognosis.
What do you think are the chances that your family member will survive this hospitalization if the current plan of care stays the same? Place a mark on the line to indicate your estimate.
Appendix C describes other covariates recorded from surrogate decision-makers and physicians, including surrogates’ trust in physicians, health literacy, religiosity, quality of communication with physicians, and symptoms of depression.
Outcome Measures
We quantified the proportion of surrogates with optimistic expectations about prognosis compared to the treating physicians, defined as the surrogate’s prognostic estimate being at least 20% more optimistic than the physician’s. The rationale for choosing a 20% difference as clinically significant is that prior studies using hypothetical cases suggest that changes in prognostic expectations of roughly this magnitude are associated with changes in patients’ willingness to accept life support.28,29
To determine how often surrogates’ optimistic expectations about prognosis arose from misunderstanding the physician’s prognostic expectations, we determined the proportion of cases in which there was a difference between the physician’s estimate and the surrogate’s best guess of the physicians’ prognostic expectations, which indicated misunderstanding. To determine the frequency with which prognostic discordance arose from different beliefs about prognosis by surrogates and physicians, we determined the proportion of cases in which there was a difference between the surrogate’s perception of the physicians’ prognostic expectations and the surrogate’s own prognostic estimate.
At the time of hospital discharge, we abstracted from the medical record the ICU and hospital length of stay, the duration of mechanical ventilation, the incidence and timing of withdrawal of life support, and patients’ vital status.
Statistical Analyses
We calculated that a sample size of 275 patients with APACHE II score ≥ 25 would result in a sample with 105 patients who died, which would yield 80% power to detect a correlation of at least 0.26 between optimistic expectations by surrogates and length of stay on a two-sided 0.05 level test. This sample size also gives 80% power to detect a multiple R-squared as small as 0.11, equivalent to multiple correlation of 0.33, in a multiple linear regression with 5 predictors using a two-sided alpha error of 0.05.
We performed linear regressions to evaluate the relationship between optimistic expectations by surrogates and 1) duration of ICU stay, 2) duration of mechanical ventilation, and 3) time to withdrawal of life support. These variables were right-skewed using the Shapiro–Wilk test; therefore log-transformation of the outcome variables was required to normalize the variables before fitting them into linear regression models. We also performed multilevel modeling to assess for physician-level clustering, which did not reveal significant clustering. To assess for clustering by study site, we performed likelihood ratio tests, which showed no statistical difference in using ordinary least square regression as opposed to multilevel regression clustering by sites. We therefore present results of standard linear regressions. We identified confounding variables at the patient, clinician, and surrogate level using significance test methods.30 We first identified factors associated with length of stay in the univariate analyses with a p-value < 0.20 (Appendix A). Then we used stepwise regression to select the subset of factors to be incorporated into the multivariable model. We performed similar linear regressions for patients who survived to hospital discharge.
We used logistic regression and the variable selection strategy described above to examine whether optimistic expectations by surrogates were associated with higher odds of patient survival to hospital discharge. All analyses were performed with Stata version 14.0 (College Station, TX).
RESULTS
Among 405 eligible patients, surrogate decision makers for 275 agreed to participate, for an overall enrollment rate of 68%. All 150 physicians who treated these patients agreed to participate in the study. There were no differences in the demographic characteristics of enrolled vs non-enrolled patients (Supplemental materials- appendix B). Tables 1, 2, and 3 list characteristics of the enrolled patients, surrogates and physicians. The in-hospital mortality rate was 44% (122 of 275; 95% CI 39–50%)
TABLE 1.
CHARACTERISTICS OF THE ENROLLED PATIENTS
| Characteristic |
Total N=275* |
Surrogate does not have optimistic prognostic expectations (N=124) |
Surrogate has optimistic prognostic expectations (N=121) |
pa | |
|---|---|---|---|---|---|
| Age, year | Mean 58.2, SD 16.5 |
Mean 57.7, SD 16.3 |
Mean 59.4, SD 16.5 |
0.434 | |
| Sex (male) | 152 (55.3) | 62 (50.0) | 69 (57.0) | 0.306 | |
| Hispanic | 21 (9.0) | 10 (9.2) | 11 (10.6) | 0.820 | |
| Race White Black Asian Native American Multiethnic |
222 (81.9) 31 (11.4) 13 (4.8) 2 (0.7) 3 (1.1) |
107 (87.7) 10 (8.2) 3 (2.5) 1 (0.8) 1 (0.8) |
91 (76.5) 18 (15.1) 8 (6.7) 0 2 (1.7) |
0.084 | |
| Admission source Home Acute care facility/Outside hospital Long-term acute care facility Skilled nursing facility Rehabilitation center Other |
142 (51.8) 113 (41.2) 4 (1.5) 11 (4.0) 2 (0.7) 2 (0.7) |
61 (49.2) 53 (42.7) 4 (3.2) 4 (3.2) 1 (0.8) 1 (0.8) |
67 (55.4) 45 (37.2) 0 7 (5.8) 1 (0.8) 1 (0.8) |
0.280 | |
| Admission diagnosisb Respiratory failure Cardiovascular Genitourinary Gastrointestinal Trauma Neurologic failure Hematologic Metabolic |
134 (36.1) 105 (28.3) 36 (9.7) 34 (9.2) 28 (7.5) 20 (5.4) 10 (2.7) 4 (1.1) |
64 (37.2) 48 (27.9) 20 (11.6) 13 (7.6) 11 (6.4) 11 (6.4) 3 (1.7) 2 (1.2) |
61 (38.9) 45 (28.7) 11 (7.0) 16 (10.2) 12 (7.6) 5 (3.2) 5 (3.2) 2 (1.3) |
0.636 | |
| APACHE II score at enrollment | Mean 31.6, SD (5.2) |
Mean 30.9, SD 5.3 |
Mean 32.2, SD 5.0 |
0.042 | |
| APACHE II score on the patient’s fifth day on mechanical ventilation | Mean 26.6, SD (6.7) |
Mean 25.6, SD (7.0) |
Mean 27.3, SD (6.0) |
0.043 | |
| Full code at enrollment | 245 (89.1) | 114 (91.9) | 104 (86.0) | 0.156 | |
| Survival estimate by the surrogate, % | Mean 71.4, SD 32.4 |
Mean 59.5, SD 36.8 |
Mean 82.9, SD 22.2 |
<0.001 | |
| Survival prognostication by the clinician, % | Mean 55.2, SD 29.7 |
Mean 63.7, SD 30.9 |
Mean 47.3, SD 26.0 |
<0.001 | |
| In-hospital mortality | 122 (44.4) | 55 (44.4) | 52 (43.0) | 0.898 | |
| Length of ICU stay from enrollment, day | Mean 16.3, SD 19.7 |
Mean 14.5, SD 15.4 |
Mean 18.2, SD 23.6 |
0.150 |
Physician-surrogate discordance score can be determined only in 245 patients due to missing data on physicians’ or surrogates’ prognostications in 30 cases
Comparison tests used were t-test and Fisher’s exact test, comparing surrogates with optimistic prognostic expectations to those without optimistic prognostic expectations.
A patient may have more than one admission diagnoses. Total number of listed diagnoses is 371.
Definition of abbreviations: APACHE II = Acute Physiology and Chronic Health Evaluation II; ICU = intensive care unit.
Data are presented as no. (%) unless otherwise noted.
TABLE 2.
CHARACTERISTICS OF THE ENROLLED SURROGATES
| Characteristic |
Total (N=271) |
Without optimistic prognostic expectations (N=124) |
With optimistic prognostic expectations (N=121) |
pa | |
|---|---|---|---|---|---|
| Age, year | Mean 52.6, SD 13.2 | Mean 52.0, SD 13.2 |
Mean 52.9, SD 13.0 |
0.566 | |
| Sex (male) | 85 (31.4) | 38 (31.2) | 37 (30.8) | 0.999 | |
| Hispanic | 23 (8.5) | 9 (7.4) | 14 (11.7) | 0.280 | |
| Race White Black Asian Native American Multiracial |
210 (79.6) 28 (10.6) 15 (5.7) 2 (0.8) 9 (3.4) |
102 (85.7) 7 (5.9) 4 (3.4) 2 (1.7) 4 (3.4) |
84 (71.8) 19 (16.2) 9 (7.7) 0 5 (4.3) |
0.018 | |
| Education Some high school or less than high school High school graduate Some college College graduate Post graduate, graduate, professional education |
19 (7.0) 73 (26.9) 68 (25.1) 58 (21.4) 53 (19.6) |
7 (5.7) 29 (23.8) 30 (24.6) 28 (23.0) 28 (23.0) |
10 (8.3) 35 (29.1) 31 (25.8) 25 (20.8) 19 (15.8) |
0.567 | |
| Main Language English Other language |
249 (92.2) 21 (7.8) |
114 (93.4) 8 (6.6) |
108 (90.8) 11 (9.2) |
0.481 | |
| Religion Catholic Other Christian Other Atheist/None/No affiliation |
77 (30.4) 126 (49.8) 11 (4.4) 39 (15.4) |
34 (29.6) 57 (49.6) 3 (2.6) 21 (18.3) |
35 (31.8) 56 (50.9) 6 (5.5) 13 (11.8) |
0.448 | |
| Importance of religion Very important Fairly important Somewhat important Not at all important |
132 (48.9) 86 (31.9) 32 (11.9) 20 (7.4) |
54 (44.3) 39 (32.0) 16 (13.1) 13 (10.7) |
68 (57.1) 34 (28.6) 13 (10.9) 4 (3.4) |
0.072 | |
| Relationship to patient Spouse/partner Child Sibling Parent Other |
106 (39.1) 86 (31.7) 25 (9.2) 41 (15.1) 13 (4.8) |
42 (34.4) 38 (31.2) 16 (13.1) 19 (15.6) 7 (5.7) |
55 (45.8) 40 (33.3) 6 (5.0) 15 (12.5) 4 (3.3) |
0.106 | |
| Lipkus numeracy scale (score 0–11, higher score indicates better understanding of math and probability) | Mean 6.6, SD 3.2 | Mean 7.1, SD 2.9 |
Mean 6.2, SD 3.3 |
0.020 | |
| STOFHLA (score 0–36, higher score indicates more health literacy) | Mean 33.4, SD 6.1 | Mean 33.7, SD 5.4 |
Mean 33.1, SD 6.7 |
0.460 | |
| LOTR (score 0–24, higher score indicates more optimistic) | Mean 16.8, SD 3.9 | Mean 16.5, SD 3.8 |
Mean 17.2, SD 3.9 |
0.162 | |
| PHQ9 (score 0–27, higher score indicates more severe depression) | Mean 7.3, SD 4.9 | Mean 8.0, SD 4.8 |
Mean 6.0, SD 4.7 |
0.002 | |
| GAD7 (score 0–21, higher score indicates more anxiety) | Mean 8.3, SD 5.3 | Mean 8.9, SD 5.3 |
Mean 7.2, SD 5.0 |
0.012 | |
| Had prior conversation with the patient about advance care planning | 191 (70.7) | 80 (65.6) | 91 (76.5) | 0.067 | |
| Has past experience as a surrogate decision-maker | 145 (53.7) | 66 (54.6) | 64 (53.3) | 0.897 | |
| Self-rating in knowing what the patient wants (score 0–10, higher score indicates knowing the patient’s wants very well) | Mean 8.3, SD 2.3 | Mean 8.2, SD 2.4 |
Mean 8.6, SD 2.2 |
0.255 | |
| Wake Forest Physician Trust Scale | Mean 21.7, SD 3.6 |
Mean 21.8, SD 3.7 |
Mean 21.5, SD 3.6 |
0.542 |
271 surrogate completed baseline questionnaire. Physician-surrogate discordance score cannot be determined in 30 surrogates (4 of which did not complete the baseline questionnaire).
Definitions of abbreviations: STOFHLA = Short Test of Functional Health Literacy in Adults; LOTR = Revised Life Orientation Test; PHQ9 = Patient Health Questionnaire-9; GAD7 = Generalized Anxiety Disorder 7-item; SER= Survival Expectancy Ratio
Data are presented as no. (%) unless otherwise noted.
Comparison tests used were t-test and Fisher’s exact test, comparing surrogates with optimistic prognostic expectations to those without optimistic prognostic expectations.
TABLE 3.
CHARACTERISTICS OF THE ENROLLED CLINICIANS
| Characteristic |
Total (N=149)a |
Surrogate does not have optimistic prognostic expectations (N=124)b |
Surrogate has optimistic prognostic expectations (N=121)b |
Pc | |
|---|---|---|---|---|---|
| Age, year | Mean 38.9, SD 10.0 |
Mean 40.8, SD 9.7 |
Mean 40.4, SD 10.9 |
0.750 | |
| Sex (male) | 103 (69.1) | 94 (75.8) | 86 (71.1) | 0.470 | |
| Hispanic | 8 (5.4) | 10 (8.1) | 6 (5.0) | 0.439 | |
| Race White Black Asian Pacific Islander Multiethnic |
110 (76.9) 5 (3.5) 25 (17.5) 1 (0.7) 2 (1.4) |
95 (79.2) 3 (2.5) 21 (17.5) 1 (0.8) 0 |
94 (79.0) 3 (2.5) 20 (16.8) 0 2 (1.7) |
0.734 | |
| Medical practice duration, year | Mean 8.7, SD 9.6 |
Mean 10.5, SD 9.8 |
Mean 10.4, SD 10.0 |
0.928 | |
| Training level Attending Fellow Resident Nurse practitioner |
77 (51.3) 41 (27.3) 30 (20.0) 2 (1.3) |
79 (63.7) 28 (22.6) 15 (12.1) 2 (1.6) |
72 (59.5) 35 (28.9) 14 (11.6) 0 |
0.427 | |
| Specialtyd Internal medicine Anesthesiology Surgery Neurology Other |
83 (67.5) 9 (7.3) 26 (21.1) 1 (0.8) 4 (3.3) |
79 (73.8) 3 (2.8) 21 (19.6) 1 (0.9) 3 (2.8) |
85 (78.0) 8 (7.3) 13 (11.9) 0 3 (2.8) |
0.220 | |
| Self-rating of skillfulness in discussing prognosis (score 0–10, 10 indicates extremely skilled) | Mean 7.7, SD 1.4 |
Mean 7.9, SD 1.4 |
Mean 8.0, SD 1.4 |
0.933 | |
| Self-rating of skillfulness in guiding surrogates through making decisions about life support (score 0–10, 10 indicates extremely skilled) | Mean 7.8, SD 1.3 |
Mean 8.0, SD 1.3 |
Mean 8.0, SD 1.3 |
0.805 |
There are 150 clinicians in the study but 149 completed the questionnaire
Due to the nature of the division, a clinician may be represented more than once
Comparison tests used were t-test and Fisher’s exact test, comparing surrogates with optimistic prognostic expectations to those without optimistic prognostic expectations.
Applicable among attendings and fellows only (n=118). Total number exceeds 118 due to some physicians have more than one specialties.
Data are presented as no. (%) unless otherwise noted.
Prevalence of Optimistic Prognostic Expectations by Surrogates
Overall, 45% of surrogate decision makers (109 of 245; 95% CI 38–51%) held prognostic expectations that were at least 20% more optimistic that the physician’s. Among these patients, the average prognostic estimates for hospital survival among surrogates and physicians were 86% (±19) and 48% (±26), respectively. Among the 107 patients who died, optimistic expectations by surrogates were present in 42% (45 of 107; 95% CI 33–51%) of surrogates. Among these cases, the mean ± SD prognostic estimates for hospital survival from surrogates and physicians were 79.4% ± 21.0 and 36.4% ± 26.5, respectively. Appendix C contains a summary of the discriminant accuracy and calibration of physicians’ and surrogates’ predictions.
Sources of Optimistic Prognostic Expectations by Surrogates
In 52 of 109 cases (48%), the discordance arose from the surrogate misunderstanding the physician’s prognostic expectations. In 49 (45%) cases, the discordance arose from both surrogates misunderstanding physicians’ prognostic expectations and from surrogates holding systematically more hopeful beliefs about the patient’s prognosis compared to what they heard from the physicians. In 7 (6%) cases, the prognostic discordance was caused only by surrogates holding more hopeful beliefs about the patient’s prognosis compared to what they heard from the physician. Data were missing from 1 surrogate who did not respond to the question eliciting what they thought the physicians’ prognosis estimate was.
Optimism by Surrogates and Patient Survival
In a multivariable model adjusted for patient age and APACHE II, there was no significant association between higher levels of optimism by surrogates and patients’ odds of survival to hospital discharge (OR 1.39 (95% CI 0.80–2.41); p=0.25).
Association between Optimistic Prognostic Expectations and Healthcare Utilization
Among patients who died in the hospital, the median unadjusted ICU length of stay and duration of mechanical ventilation were 8 days (IQR 4–15) and 8 days (IQR 3–15); 75% (91 of 122) of deaths occurred after life support was withdrawn and an additional 13% (16 of 122) occurred after life support was withheld (Appendix D). In a multivariable model after log-transformation and adjustment for severity of illness (APACHE II), surrogate race, and relationship to the patient, optimistic expectations by surrogates were associated with a significantly longer ICU stay (β coefficient= 0.44; 95% CI: 0.05–0.83; p=0.027), corresponding to a 56% longer hospital stay before death (Table 4). Optimistic expectations were also associated with a significantly longer time to withdrawal of life support among dying patients (β coefficient= 0.61; 95% CI: 0.16–1.07; p=0.009), corresponding to on average 6.5 more days of life support before death. Among patients who survived their hospitalization, optimistic expectations by surrogates were not associated with longer hospital ICU stay (p=0.78). (Appendix E).
TABLE 4.
MULTIPLE VARIABLE ANALYSIS SHOWING ADJUSTED ASSOCIATION BETWEEN OPTIMISTIC EXPECTATIONS BY SURROGATES AND DURATION OF ICU TREATMENT AT THE END OF LIFE
| Outcome of regression model | Regression Coefficient for Surrogates with Optimistic Prognostic Expectations* (95% CI) |
Change from the Meana,b (% change) |
p |
|---|---|---|---|
| ICU length of stay | 0.44 (0.05– 0.83)d | +7.7 days | 0.027 |
| Length of mechanical ventilation | 0.30 (-0.10–0.71)c | +5.4 days | 0.139 |
| Time to withdrawal of life support | 0.61 (0.16–1.07)e | +6.5 days | 0.009 |
Optimistic prognostic expectations by surrogates is defined as when the surrogate’s prediction of the chance of hospital survival is at least 20% greater than the physician’s.
Among the patients who died, the mean (median) ICU length of stay is=13.9 days (8 days), the mean (median) length of mechanical ventilation is=15.1 days (8 days), and the mean (median) time to withdrawal of life support is 14.5 days (8 days).
The % change from the mean is computed by exponentiating the coefficient (beta) from the regression with log-transformed outcome
Adjusted for the following factors: the patient’s APACHE II score on the fifth day on mechanical ventilation (the same day prognostic estimates were taken), and surrogate’s relationship to the patient
Adjusted for the following factors: the patient’s APACHE II score on the fifth day on mechanical ventilation (the same day prognostic estimates were taken), surrogate’s relationship to the patient, and surrogate’s race (non-Hispanic black vs. other)
Adjusted for the following factors: the patient’s age and APACHE II score on the fifth day on mechanical ventilation (the same day prognostic estimates were taken)
Definition of abbreviations: ICU = intensive care unit; APACHE II = Acute Physiology and Chronic Health Evaluation II.
We conducted two sensitivity analyses to verify that the relationship between optimistic expectations and duration of intensive treatment at the end of life is robust to different analytic approaches. Both yielded qualitatively similar conclusions to those from the main analysis (Appendix F).
First, we used an alternative definition of optimistic expectations: a survival expectancy ratio (SER) exceeding 1.2. The SER is the ratio of the surrogate’s prognostic expectations to the physician’s expectations. The use of such ratios has previously been used to quantify discrepancies between physicians’ and patients’ prognostic estimates.(24) A potential advantage of the SER compared to a choosing a single absolute difference to signify prognostic discordance is that it may better account for the possibility that as the patient’s prognosis worsens smaller difference between clinician’s and surrogate’s expectations may be important.
Second, we maintained the original definition of optimistic expectations and excluded patients for whom the treating physician judged that the patient had >80% chance of survival; the rationale for this analysis is that the lack of optimistic expectations in these cases arises because the physician’s expectations of survival are so high in these patients that surrogates cannot be 20% more optimistic.
DISCUSSION
We found that nearly half of surrogate decision-makers for incapacitated ICU patients at high risk of death or severe disability held substantially more optimistic expectations about prognosis compared to the treating physicians. These expectations arose from both misunderstandings by surrogates of physicians’ prognoses as well as from surrogates holding more optimistic beliefs about the patient’s prognosis compared to what they heard from the physician. Optimistic expectations by surrogates were associated with significantly longer duration of intensive treatment at the end of life without an increase in survival.
Our results suggest that problems persist with clinician-family communication in ICUs, despite substantial efforts in the last two decades to improve this aspect of ICU care. The prevalence of misperceptions about prognosis observed in our study was similar to that documented by Azoulay et al. in 20005 and also similar to those observed in more recent single-center studies.6,8 The lack of improvement in this particular aspect of end-of-life care is consistent with published reports that patients’ and families’ perceptions of the quality of end-of-life care have not improved in the last decade.31
The results of the present study suggest that the findings from prior single-center8 and simulation-based studies16–18 on this topic are broadly generalizable. Specifically, our data indicate that surrogates’ optimism about prognosis arises from both miscomprehension by surrogates of physicians’ expectations as well as from surrogates holding systematically more optimistic beliefs than what they heard from the physicians. These findings fit with insights from decision psychology about optimism bias, which is the tendency of individuals to view themselves as more likely to have good outcomes compared to others.14 Taken together, these studies suggest that interventions to improve communication about prognosis need to address both the comprehensibility of prognostic information, and also attend to the psychological and affective complexity for surrogates coming to terms with news of a poor prognosis.15–17,32–34
It is uncertain how to intervene to improve the accuracy of surrogates’ prognostic expectations. In fact, expert clinicians such as palliative care consultants often avoid direct attempts to change surrogates’ prognostic expectations, and instead align with surrogates’ optimism, attend to their emotions, and gently help them move in the direction of acceptance.35 A recent trial testing the effect of trained interventionists providing clear prognostic information to surrogates in ICUs found no impact on treatment decisions, but more psychological distress among surrogates in the intervention arm.36 One possible explanation for these findings is that the protocolized intervention did not allow the interventionists to longitudinally support surrogates through the emotional difficulty of receiving news of a loved one’s poor prognosis.
The finding that optimism about prognosis by surrogates is associated with more invasive treatment at the end of life highlights the potential clinical and economic consequences of ineffective communication in ICUs. Our results may partially explain the results of the SUPPORT trial, which showed no effect on health care utilization near the end of life from an intervention in which physicians were provided with model-derived prognostic estimates for patients with serious illness.37 In the SUPPORT trial physicians rarely shared the prognostic estimates with patients/surrogates, yet our data suggest that surrogates’ prognostic expectations-which differ from physicians’- may substantially influence utilization. Our results are consistent with studies of nursing home residents and elderly outpatients, which reported that individuals’ were less willing to authorize intensive treatment when they had accurate expectations about prognosis.29,38
This study has several limitations. First, all study ICUs had academic affiliations, and therefore it is uncertain whether our findings can be generalized to non-academic settings and regions of the U.S. not represented in the trial sites. Second, the cohort was predominantly Caucasian, and these results may not generalize to other racial and ethnic groups. Third, the cohort study design does not allow us to make causal inferences from the observed associations. Fourth, due to the logistical challenges of studying surrogate decision-makers in crisis situations, we did not make serial measurements of prognostic estimates and therefore were not able to quantify the natural history of surrogates’ prognostic expectations during a terminal hospitalization and how this relates to decisions about life support.
Conclusion
This multicenter study shows that optimistic expectations about prognosis are prevalent among surrogates of patients with advanced critical illness, arise from both misunderstandings by surrogates and from surrogates holding more hopeful beliefs than what they heard from physicians, and are associated with a longer duration of intensive treatment at the end of life. These findings underscore the need to develop strategies to improve the comprehensibility of physicians’ prognostications, and also to attend to the emotional and psychological challenges surrogates face when confronted with news of a poor prognosis.
Supplementary Material
Key points:
We conducted a multicenter prospective cohort study to determine the causes of optimistic expectations about prognosis among surrogates in ICUs and whether they are associated with more use of life support at the end of life. We found that optimism about prognosis is prevalent among surrogates and arises both from surrogates’ miscomprehension of physicians’ prognostications and from surrogates holding more hopeful beliefs. This optimism is associated with longer duration of life support at the end of life.
Funding Source:
National Institutes of Health; National Heart, Lung, and Blood Institute grant R01HL094553.
Copyright form disclosure: Dr. White, Steingrub, Buddadhumaruk, Weissfeld, and Hough’s institution received funding from National Institutes of Health (NIH). Drs. White and Bird’s institutions received funding from National Heart, Lung, and Blood Institute (NHLBI) grant R01HL094553. Dr. White received funding from UptoDate. Drs. White, Carson, Anderson, Steingrub, Bird, Buddadhumaruk, Shields, Ernecoff, Weissfeld, Chang, and Hough received support for article research from the NIH. Drs. Carson, Anderson, Shields, and Ernecoff’s institutions received funding from the NHLBI. Dr. Carson’s institution received funding from Biomarck Pharmaceuticals. Dr. Bird received funding from Forrest Pharmaceuticals (speakers fees). Dr. Matthay’s institution received funding from Bayer Pharmaceuticals (Observational Study of ARDS grant), GlaxoSmithKline (Observational Studies of Sepsis), and he received funding from CS Behring (consultation on ARDS). The remaining authors have disclosed that they do not have any potential conflicts of interest.
Contributor Information
Douglas B. White, University of Pittsburgh School of Medicine.
Shannon Carson, UNC-Chapel Hill School of Medicine.
Wendy Anderson, UCSF School of Medicine.
Jay Steingrub, Baystate Medical Center, U Mass School of Medicine.
Garrett Bird, UCSF-Fresno School of Medicine.
J Randall Curtis, University of Washington School of Medicine.
Michael Matthay, UCSF School of Medicine.
Michael Peterson, UCSF-Fresno School of Medicine.
Praewpannarai Buddadhumaruk, University of Pittsburgh School of Medicine.
Anne-Marie Shields, University of Pittsburgh School of Medicine.
Natalie Ernecoff, UNC-Chapel Hill School of Medicine.
Kaitlin Shotsberger, University of Pittsburgh School of Medicine.
Lisa Weissfeld, University of Pittsburgh School of Medicine.
Chung-Chou H. Chang, University of Pittsburgh School of Medicine.
Francis Pike, University of Pittsburgh School of Medicine.
Bernard Lo, UCSF School of Medicine.
Catherine L. Hough, University of Washington School of Medicine.
REFERENCES
- 1.Sprung CL, Cohen SL, Sjokvist P, et al. End-of-life practices in European intensive care units: the Ethicus Study. Jama. 2003;290(6):790–797. [DOI] [PubMed] [Google Scholar]
- 2.Angus DC, Barnato AE, Linde-Zwirble WT, et al. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32(3):638–643. [DOI] [PubMed] [Google Scholar]
- 3.Prendergast TJ, Claessens MT, Luce JM. A national survey of end-of-life care for critically ill patients. Am J Respir Crit Care Med. 1998;158(4):1163–1167. [DOI] [PubMed] [Google Scholar]
- 4.Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. N Engl J Med. 2010;362(13):1211–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Azoulay E, Chevret S, Leleu G, et al. Half the families of intensive care unit patients experience inadequate communication with physicians. Crit Care Med. 2000;28(8):3044–3049. [DOI] [PubMed] [Google Scholar]
- 6.Cox CE, Martinu T, Sathy SJ, et al. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med. 2009;37(11):2888–2894; quiz 2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Teno JM, Fisher E, Hamel MB, et al. Decision-making and outcomes of prolonged ICU stays in seriously ill patients. J Am Geriatr Soc. 2000;48(5 Suppl):S70–74. [DOI] [PubMed] [Google Scholar]
- 8.White DB, Ernecoff N, Buddadhumaruk P, et al. Prevalence of and Factors Related to Discordance About Prognosis Between Physicians and Surrogate Decision Makers of Critically Ill Patients. JAMA. 2016;315(19):2086–2094. [DOI] [PubMed] [Google Scholar]
- 9.Sinuff T, Adhikari NK, Cook DJ, et al. Mortality predictions in the intensive care unit: comparing physicians with scoring systems. Crit Care Med. 2006;34(3):878–885. [DOI] [PubMed] [Google Scholar]
- 10.Detsky ME, Harhay MO, Bayard DF, et al. Discriminative Accuracy of Physician and Nurse Predictions for Survival and Functional Outcomes 6 Months After an ICU Admission. JAMA. 2017;317(21):2187–2195. doi: 2110.1001/jama.2017.4078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rocker G, Cook D, Sjokvist P, et al. Clinician predictions of intensive care unit mortality. Crit Care Med. 2004;32(5):1149–1154. [DOI] [PubMed] [Google Scholar]
- 12.Evans LR, Boyd EA, Malvar G, et al. Surrogate decision-makers’ perspectives on discussing prognosis in the face of uncertainty. Am J Respir Crit Care Med. 2009;179(1):48–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.You JJ, Downar J, Fowler RA, et al. Barriers to goals of care discussions with seriously ill hospitalized patients and their families: a multicenter survey of clinicians. JAMA internal medicine. 2015;175(4):549–556. [DOI] [PubMed] [Google Scholar]
- 14.Alicke MD, Klotz ML, Breitenbecher DL, Yurak TJ, Vredenburg DS. Personal contact, individuation, and the better-than-average effect. J Pers Soc Psychol 1995;68(5):804. [Google Scholar]
- 15.Schenker Y, White DB, Crowley-Matoka M, Dohan D, Tiver GA, Arnold RM. “It hurts to know... and it helps”: exploring how surrogates in the ICU cope with prognostic information. J Palliat Med. 2013;16(3):243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zier LS, Burack JH, Micco G, et al. Doubt and belief in physicians’ ability to prognosticate during critical illness: the perspective of surrogate decision makers. Crit Care Med. 2008;36(8):2341–2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zier LS, Sottile PD, Hong SY, Weissfield LA, White DB. Surrogate decision makers’ interpretation of prognostic information: a mixed-methods study. Ann Intern Med. 2012;156(5):360–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee Char SJ, Evans LR, Malvar GL, White DB. A randomized trial of two methods to disclose prognosis to surrogate decision makers in intensive care units. Am J Respir Crit Care Med. 2010;182(7):905–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.von Neumann John and Morgenstern Oskar. Theory of Games and Economic Behavior. Princeton, NJ: Princeton University Press, 2004. [Google Scholar]
- 20.Kahneman Daniel. A Perspective on Judgment and Choice: Mapping Bounded Rationality. American Pyschologist. 2003; 58: 697–720. [DOI] [PubMed] [Google Scholar]
- 21.Rubenfeld GD, Elliott M. Evidence-based ethics? Curr Opin Crit Care. 2005;11(6):598–599. [DOI] [PubMed] [Google Scholar]
- 22.Zier LS, Burack JH, Micco G, Chipman AK, Frank JA, White DB. Surrogate decision makers’ responses to physicians’ predictions of medical futility. Chest. 2009;136(1):110–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bernard GR, Artigas A, Brigham KL, et al. The American-European Consensus Conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am J Respir Crit Care Med. 1994;149(3 Pt 1):818–824. [DOI] [PubMed] [Google Scholar]
- 24.Cox CE, Carson SS. Medical and economic implications of prolonged mechanical ventilation and expedited post-acute care. Seminars in respiratory and critical care medicine. 2012;33(4):357–361. [DOI] [PubMed] [Google Scholar]
- 25.Gigerenzer G, Edwards A. Simple tools for understanding risks: from innumeracy to insight. BMJ: British Medical Journal. 2003;327(7417):741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Huskisson E Measurement of pain. The Lancet. 1974;304(7889):1127–1131. [DOI] [PubMed] [Google Scholar]
- 27.Holland JC. Now we tell--but how well? Journal of Clinical Oncology. 1989;7(5):557–559. [DOI] [PubMed] [Google Scholar]
- 28.Lloyd CB, Nietert PJ, Silvestri GA. Intensive care decision making in the seriously ill and elderly. Crit Care Med. 2004;32(3):649–654. [DOI] [PubMed] [Google Scholar]
- 29.Fried TR, Bradley EH, Towle VR, Allore H. Understanding the treatment preferences of seriously ill patients. N Engl J Med. 2002;346(14):1061–1066. [DOI] [PubMed] [Google Scholar]
- 30.Maldonado G, Greenland S. Simulation study of confounder-selection strategies. Am J Epidemiol. 1993. December 1;138(11):923–36. [DOI] [PubMed] [Google Scholar]
- 31.Teno JM, Freedman VA, Kasper JD, Gozalo P, Mor V. Is Care for the Dying Improving in the United States? J Palliat Med. 2015;18(8):662–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Apatira L, Boyd EA, Malvar G, et al. Hope, truth, and preparing for death: perspectives of surrogate decision makers. Ann Intern Med. 2008;149(12):861–868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schenker Y, Crowley-Matoka M, Dohan D, Tiver GA, Arnold RM, White DB. I don’t want to be the one saying ‘we should just let him die’: intrapersonal tensions experienced by surrogate decision makers in the ICU. J Gen Intern Med. 2012;27(12):1657–1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cox CE, Lewis CL, Hanson LC, et al. Development and pilot testing of a decision aid for surrogates of patients with prolonged mechanical ventilation. Crit Care Med. 2012;40(8):2327–2334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jackson VA, Jacobsen J, Greer JA, Pirl WF, Temel JS, Back AL. The cultivation of prognostic awareness through the provision of early palliative care in the ambulatory setting: a communication guide. J Palliat Med. 2013;16(8):894–900. [DOI] [PubMed] [Google Scholar]
- 36.Carson SS, Cox CE, Wallenstein S, et al. Effect of Palliative Care-Led Meetings for Families of Patients With Chronic Critical Illness: A Randomized Clinical Trial. JAMA. 2016;316(1):51–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.SUPPORT. A Controlled Trial to Improve Care for Seriously Ill Hospitalized Patients. JAMA. 1995;274(20):1591–1598. [PubMed] [Google Scholar]
- 38.Mitchell SL, Teno JM, Kiely DK, et al. The clinical course of advanced dementia. N Engl J Med. 2009;361(16):1529–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.