Abstract
Background:
Gonorrhea treatment has been complicated by antimicrobial resistance in Neisseria gonorrhoeae. Gonococcal fluoroquinolone resistance emerged more rapidly among men who have sex with men (MSM) than among men who have sex exclusively with women (MSW).
Objective:
To determine whether N. gonorrhoeae urethral isolates from MSM were more likely than isolates from MSW to exhibit resistance to or elevated minimum inhibitory concentrations (MICs) of antimicrobials used to treat gonorrhea.
Design:
Six years of surveillance data from the Gonococcal Isolate Surveillance Project (GISP)
Setting:
Publicly-funded sexually transmitted disease clinics in 30 United States cities
Patients:
Men with a total of 34,600 episodes of symptomatic urethral gonorrhea
Measurements:
Primary outcomes included percentage of isolates exhibiting resistance or elevated MICs, and adjusted odds ratios for resistance or elevated MICs among isolates from MSM compared to isolates from MSW.
Funding Source:
GISP is funded by the CDC, an agency of the US Department of Health and Human Services.
Results:
Isolates from MSM were significantly more likely than isolates from MSW to exhibit elevated cephalosporin MICs (P <=0.028). Isolates from MSM had a high prevalence of resistance to ciprofloxacin, penicillin, and tetracycline and were significantly more likely to exhibit antimicrobial resistance than isolates from MSW (P <0.001).
Limitations:
Sentinel surveillance might not be representative of all patients with gonorrhea. HIV status, travel history, and antimicrobial use data were missing for some patients.
Conclusions:
MSM are vulnerable to the emerging threat of multidrug-resistant N. gonorrhoeae. Because antimicrobial susceptibility testing is not routinely performed in clinical practice, clinicians should monitor for treatment failures among MSM diagnosed with gonorrhea. Strengthened prevention strategies for MSM and new antimicrobial treatment options are needed.
Keywords: gonorrhea, Neisseria gonorrhoeae, resistance, men who have sex with men, GISP
Introduction
Gonorrhea, caused by Neisseria gonorrhoeae, is the second most commonly reported notifiable infection in the United States, with 309,341 cases reported in 2010. (1) Gonorrhea is associated with pelvic inflammatory disease, ectopic pregnancy, infertility, and epididymitis, and may facilitate HIV transmission. (2–5) Prevention of sequelae and control of disease transmission rely on prompt treatment with effective antimicrobial therapy.
The introduction of antimicrobial therapy in the 1930s ushered in an era of effective treatment options for gonorrhea. Yet N. gonorrhoeae rapidly developed resistance to sulfonamides and proved adept at developing resistance to each antimicrobial subsequently recommended for treatment: penicillin, tetracycline, and fluoroquinolones. Gonococcal resistance to penicillin and tetracycline developed both through the stepwise accumulation of chromosomal mutations and through acquisition of plasmids conferring high-level resistance.(6–9) Quinolone-resistant N. gonorrhoeae (QRNG) emerged in East Asia during the 1990s and subsequently spread to Hawaii, the Pacific Islands, and the US West Coast.(10) In the US, the prevalence of QRNG initially rose rapidly among men who have sex with men (MSM) and by 2004, fluoroquinolones were no longer recommended for gonorrhea treatment in MSM.(11) Three years later, the Centers for Disease Control and Prevention (CDC) no longer recommended fluoroquinolones for treatment of gonorrhea in anyone in the US; third-generation cephalosporins were the only remaining recommended antimicrobial class.(12) CDC now recommends that gonorrhea be treated with combination antimicrobial therapy with ceftriaxone, an injectable cephalosporin, plus either azithromycin or doxycycline as the only remaining first-line treatment options for gonorrhea.(13) Recent data indicating that cephalosporin (particularly cefixime) minimum inhibitory concentrations (MICs) for N. gonorrhoeae have increased in the US and are increasing rapidly among isolates from MSM are concerning.(13) The emergence of cephalosporin-resistant N. gonorrhoeae could greatly limit treatment options for gonorrhea.
In light of rapid emergence of QRNG among MSM and the current potential for emergence of cephalosporin-resistant N. gonorrhoeae, we investigated whether N. gonorrhoeae isolates from MSM were more likely than isolates from men who have sex exclusively with women (MSW) to exhibit elevated cephalosporin or azithromycin MICs or resistance to other antimicrobial classes previously recommended for treatment.
Methods
Data Source
We used data from the Gonococcal Isolate Surveillance Project (GISP), a national sentinel surveillance system that includes participating sexually transmitted disease (STD) clinics in US cities, reference laboratories, and the CDC. GISP was established in 1986 to monitor national trends in gonococcal antimicrobial susceptibilities. During 2005–2010, clinics in 30 cities participated in GISP (Figure). Each month, N. gonorrhoeae urethral isolates were collected from the first 25 men with symptomatic gonococcal urethritis attending participating STD clinics in each city and the isolates were submitted to reference laboratories for antimicrobial susceptibility testing. Specified epidemiological data elements (see Statistical Analysis section below) were abstracted from STD clinic notes. Data collection methods varied according to local clinic practices.
Figure 1.
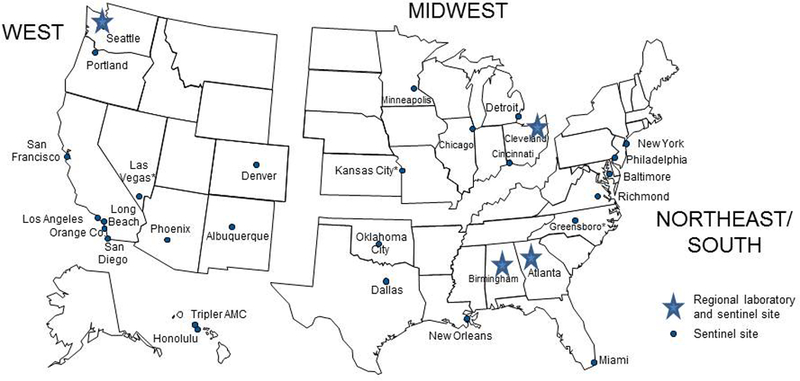
Gonococcal lsolate surveillance Project (GISP) —Location of Participating Sentinel Sites and Regional Laboratories,united states,2005–2010*
*Sites had continuous participation during 2005–2010 with the following exceptions (and years of participation): Kansas City (2007–2010); Long Beach (2005–2007); New York City (2006–2010); Richmond (2007–2010); Tripler AMC(2006, 2009–2010)
Human Subjects
As a disease control and surveillance activity, GISP was determined to be a non-research public health activity by CDC. Gonorrhea is a notifiable infection and health departments have authority to collect and transmit to CDC de-identified epidemiological data on patients with gonorrhea to assist with disease control. Antimicrobial and epidemiologic data from GISP are de-identified prior to transmission to CDC. Partner identification and notification are conducted as per local STD public health program policies.
Laboratory Methods
At the clinic laboratories, the isolates were sub-cultured on supplemented chocolate medium and frozen in trypticase soy broth with 20% glycerol. Isolates were shipped monthly to a participating reference laboratory where they were tested for ß-lactamase production and susceptibility by MICs to azithromycin, penicillin, tetracycline, ciprofloxacin, spectinomycin, cefixime, and ceftriaxone using the agar-dilution technique. Standardized bacterial suspensions were inoculated on Difco GC base medium supplemented with 1% IsoVitalex (Becton-Dickinson, Sparks, Maryland). Cefixime susceptibility testing was halted in 2007 due to lack of availability of cefixime in the United States and restarted in 2009. Control N. gonorrhoeae strains with known MICs of a variety of antimicrobials were included with each susceptibility run to ensure accuracy of the data. Twice yearly, CDC provided a panel of unidentified strains to each reference laboratory for testing; results were compared to assure inter-laboratory consistency.
Resistance criteria
We interpreted susceptibility results according to criteria for N. gonorrhoeae recommended by the Clinical and Laboratory Standards Institute (CLSI) when such criteria were available.(14) We used CLSI criteria to define resistance to penicillin (MIC ≥ 2 μg/ml), tetracycline (MIC ≥ 2 μg/ml), and ciprofloxacin, a quinolone antimicrobial (MIC ≥ 1 μg/ml). CLSI defines decreased susceptibility to cephalosporins ceftriaxone and cefixime (MICs ≥ 0.5 μg/ml) but does not define resistance. Increasing MICs can predict the emergence of resistance, so CDC uses lower MIC breakpoints, designated “elevated MICs”, to monitor trends in gonococcal susceptibility: ceftriaxone MICs ≥ 0.125 μg/ml and cefixime MICs ≥ 0.25 μg/ml. The breakpoints chosen for the 2 cephalosporins differ because ceftriaxone MICs in GISP isolates are generally 1–2 dilutions lower than cefixime MICs (1). CLSI does not define gonococcal susceptibility nor resistance breakpoints for azithromycin. We categorized isolates with azithromycin MICs ≥ 2.0 μg/ml as exhibiting elevated MICs of azithromycin. We defined penicillinase-producing N. gonorrhoeae by positive results on the nitrocefin β-lactamase test. Where not otherwise specified, we considered penicillin resistance to include either chromosomal resistance (MIC ≥ 2.0 μg/ml and β-lactamase-negative) or penicillinase-producing strains. We defined multidrug resistance as resistance to penicillin, tetracycline, and ciprofloxacin, and demonstration of elevated MICs of cefixime. We considered resistance phenotypes that have been prevalent in the US for ≥ 5 years, such as resistance to penicillin, tetracycline, and ciprofloxacin, to be “endemic,” and the other phenotypes to be “emerging”.
Statistical analysis
We included data from all cities that contributed to GISP during 2005–2010 and restricted the analytic sample to isolates for which we had data on gender of sex partner; we categorized men as either MSM or MSW. Gay and bisexual men were grouped together as MSM because we were interested in the possible association between resistance or elevated MICs and male same-sex sexual behavior, rather than self-identified sexual orientation. Clinical sites were categorized by US census region (Figure); the Northeast and South were combined due to the small number of sites in the Northeast and the history of similar timing of the emergence of resistance in the two regions. Gonococcal resistance in the United States tends to emerge initially in the West and spread eastward.(7, 10) Geographic region, age, race/ethnicity, HIV status, antimicrobial use in the past 60 days, prior gonococcal infection in the past 12 months, and travel outside of the state in which the isolate was collected in the past 60 days were pre-selected as potential confounders based on existing literature and biological plausibility. More detailed data about sexual behavior, such as the number of recent sex partners, are not routinely collected in GISP. To build a sustainable surveillance system, GISP attempts to minimize the data collection burden on sites and collect a small number of variables that can inform public health authorities about populations in which resistance may be emerging. We used the chi-square statistic to compare the frequency distributions of categorical variables. To evaluate the associations between antimicrobial resistance or elevated MICs and gender of sex partner after adjusting for potential confounders, we constructed separate multivariable logistic regression models, with antimicrobial resistance or elevated MICs as the dependent variable for each antimicrobial agent. In each multivariable model for the resistance phenotypes, we included gender of sex partner, other variables mentioned above as potential confounders, and the pre-specified interaction between gender of sex partner and geographic region. Missing values for HIV infection, travel history, antimicrobial use, and prior gonococcal infection were imputed using the logistic regression method in Proc MI from SAS 9.3. We generated 5 imputed datasets using this procedure and used the multivariable logistic regression method in Proc MIANALYZE to analyze these datasets. All statistical analyses were conducted using SAS, version 9.3 (SAS Institute, Cary, North Carolina).
Sensitivity Analyses
We performed sensitivity analyses in which missing values were handled two different ways. In the first method, we excluded observations with missing data and repeated the analyses. For the second method, we considered all missing values for HIV infection, travel history, antimicrobial use, and prior gonococcal infection to be negative and repeated the analyses. Results of these sensitivity analyses are available in the Appendix, Table B.
Because of small numbers of individuals with resistance or elevated MICs for azithromycin, cefixime, ceftriaxone, and multidrug resistance, we also constructed simple models to assess the relationship between gender of sex partner and emerging resistance phenotypes. In these models, we used antimicrobial resistance or elevated MICs as the dependent variable for each antimicrobial agent and only gender of sex partner, region, and the pre-specified interaction between gender of sex partner and geographic region as independent variables. Results of these sensitivity analyses are available in the Appendix, Table C.
Funding Source
GISP is funded by the CDC, an agency of the US Department of Health and Human Services. CDC staff were involved in the design and conduct of this surveillance activity and the collection, management, analysis, and interpretation of GISP data.
Results
During 2005–2010, 35,343 isolates were collected from men in 30 cities (range per year: 5,630–6,199). This represents approximately 4% of all reported male gonorrhea cases in the US. Gender of sex partner data were available for 34,600 (97.9%) isolates: 8,117 (23.5%) were from MSM and 26,483 (76.5%) were from MSW. MSM were older than MSW, and more likely to be white and from the Western region of the US (Table 1). Prior N. gonorrhoeae infection, antimicrobial use, HIV infection, and recent travel were more frequent among MSM than MSW (P < 0.001). After stratifying by HIV status, MSM were still more likely to report recent antimicrobial use (for HIV-infected men: 15.0% in MSM versus 9.0% in MSW, P=0.017; for HIV-uninfected: 6.9% in MSM versus 5.0% in MSW, P <0.001). Isolates from MSM exhibited significantly (P <0.001) higher prevalence of resistance to or elevated MICs of each antimicrobial class, including cephalosporins, than isolates from MSW (Table 1).
Table 1.
Characteristics of men from whom urethral Neisseria gonorrhoeae isolates were collected and antimicrobial susceptibility of isolates, Gonococcal Isolate Surveillance Project, 2005–2010
| Total | MSM | MSW | |||||
|---|---|---|---|---|---|---|---|
| Characteristic | n=34,600 | % | n=8,117 | % | n=26,483 | % | P value |
| Age > 24 years | 20,359/34,591 | 58.9 | 5,793/8,114 | 71.4 | 14,566/26,477 | 55.0 | <0.001 |
| Race/ethnicity | <0.001 | ||||||
| Black | 24,214/34,419 | 70.4 | 2,150/8,038 | 26.8 | 22,064/26,381 | 83.6 | |
| White | 5510/34,419 | 16.0 | 3,752/8,038 | 46.7 | 1,758/26,381 | 6.7 | |
| Other | 4,695/34,419 | 13.6 | 2,136/8,038 | 26.6 | 2,559/26,381 | 9.7 | |
| Region | <0.001 | ||||||
| Northeast/South | 13,588/34,600 | 39.3 | 1,600/8,117 | 19.7 | 11,988/26,483 | 45.3 | |
| Midwest | 8,114/34,600 | 23.5 | 909/8,117 | 11.2 | 7,205/26,483 | 27.2 | |
| West | 12,898/34,600 | 37.3 | 5,608/8,117 | 69.1 | 7,290/26,483 | 27.5 | |
| Prior gonorrhea infection | 16,101/33,092 | 48.7 | 4,303/7,799 | 55.2 | 11,798/25,293 | 46.7 | <0.001 |
| Antimicrobial use (past 60 days) | 1,488/26,537 | 5.6 | 491/5,768 | 8.4 | 997/19,772 | 4.8 | <0.001 |
| HIV-infected | 1,998/25,247 | 7.9 | 1,702/6,619 | 25.7 | 296/18,628 | 1.6 | <0.001 |
| Travel (past 60 days) | 1,832/19,165 | 9.6 | 654/4,535 | 14.4 | 1,178/14,630 | 8.1 | <0.001 |
| Resistance Phenotypes | |||||||
| Azithromycin DS* | 123/34,600 | 0.4 | 73/8,117 | 0.9 | 50/26,483 | 0.2 | <0.001 |
| Cefixime – elevated MICs† | 133/23,151 | 0.6 | 98/5,628 | 1.7 | 35/17,523 | 0.2 | <0.001 |
| Ceftriaxone – elevated MICs‡ | 57/34,600 | 0.2 | 29/8,117 | 0.4 | 28/26,483 | 0.1 | <0.001 |
| Ciprofloxacin resistance§ | 4,253/34,600 | 12.3 | 2,423/8,117 | 29.9 | 1,830/26,483 | 6.9 | <0.001 |
| Penicillin resistance | |||||||
| Chromosomal║ | 3,550/34,109 | 10.4 | 1,806/7,936 | 22.8 | 1,744/26,173 | 6.7 | <0.001 |
| PPNG¶ | 491/34,600 | 1.4 | 181/8,117 | 2.2 | 310/26,483 | 1.2 | <0.001 |
| Tetracycline resistance# | 6,529/34,600 | 18.9 | 3,033/8,177 | 37.4 | 3,496/26,483 | 13.2 | <0.001 |
| Multidrug resistance** | 88/34,600 | 0.3 | 66/8,117 | 0.8 | 22/26,483 | 0.1 | <0.001 |
MIC = minimum inhibitory concentration; MSM = Men who report sex with men; MSW = Men who report sex exclusively with women; PPNG = penicillinase-producing N. gonorrhoeae
Note: Denominators reflect the number of men for whom data are available. Differences in the denominators reflect missing data.
MIC ≥ 2 μg/ml
MIC ≥ 0.25 μg/ml
MIC ≥ 0.125 μg/ml
MIC ≥ 1 μg/ml
MIC ≥ 2 μg/ml and beta-lactamase negative
β-lactamase positive
MIC ≥ 2 μg/ml
Penicillin MICs ≥ 2 μg/ml or β-lactamase positive, tetracycline MICs ≥ 2 μg/ml, ciprofloxacin MICs ≥1 μg/ml, and cefixime MICs ≥ 0.25 μg/ml
Tables 2A and2B display adjusted odds ratios for resistance or elevated MICs among isolates from MSM compared to isolates from MSW, both for emerging resistance phenotypes (azithromycin, cefixime, ceftriaxone, and multidrug resistance) and endemic resistance phenotypes (ciprofloxacin, penicillin, and tetracycline). Interaction effects by region are shown and indicate significant differences by region in the magnitude of the association between resistance/elevated MICs and gender of sex partner. The displayed results are the adjusted odds ratios of elevated MICs or resistance among isolates from MSM compared to isolates from MSW, for each specific region. For example, isolates from MSM in the West had 1.4 times greater odds of elevated azithromycin MICs than isolates from MSW in the West (although the difference was non-significant), whereas isolates from MSM in the Midwest had 7.9 times greater odds of elevated azithromycin MICs than isolates from MSW in the Midwest. Isolates from MSM were significantly more likely than isolates from MSW to exhibit elevated cefixime MICs, antimicrobial resistance to penicillin, tetracycline, and ciprofloxacin, and multidrug resistance, after adjusting for other covariates. In the Midwestern and Northeastern/Southern regions of the United States (but not the Western region), isolates from MSM were significantly more likely than isolates from MSW to exhibit elevated MICs of azithromycin or ceftriaxone. Complete results of the models are shown in appendix Table A.
Table 2A.
Adjusted odds ratios of emerging Neisseria gonorrhoeae antibiotic resistance or elevated MICs among MSM compared to MSW, GISP, 2005–2010
| Emerging Resistance | ||
|---|---|---|
| Variable | aOR | 95% CI |
| Azithromycin, elevated MICs* | ||
| West | 1.4 | 0.8–2.2 |
| Midwest | 7.9 | 3.0–21.1 |
| Northeast/South | 3.7 | 1.3–10.5 |
| Cefixime, elevated MICs† | ||
| West | 2.7 | 1.7–4.4 |
| Midwest | 12.9 | 3.8–43.7 |
| Northeast/South | 33.1 | 3.8–286.4 |
| Ceftriaxone, elevated MICs‡ | ||
| West | 1.3 | 0.6–3.0 |
| Midwest | 6.8 | 2.2–20.6 |
| Northeast/South | 3.6 | 1.1–11.0 |
| Multidrug resistance§ | ||
| West | 2.6 | 1.5–4.7 |
| Midwest | 57.1 | 7.1–471.8 |
| Northeast/South | 36.4 | 4.2–315.5 |
aOR = adjusted odds ratio; CI = confidence interval;
GISP = the Gonococcal Isolate Surveillance Project;
MIC = minimum inhibitory concentration; MSM = men
who have sex with men; MSW = men who report
having sex exclusively with women
All models adjusted for age, region, race/ethnicity, antimicrobial use, travel history, HIV infection, prior gonococcal infection, and the interaction between gender of sex partner & region.
MIC ≥ 2 μg/ml
MIC ≥ 0.25 μg/ml
MIC ≥ 0.125 μg/ml
Penicillin MICs ≥ 2 μg/ml or β-lactamase positive, tetracycline MICs ≥ 2 μg/ml, ciprofloxacin MICs ≥1 μg/ml, and cefixime MICs ≥ 0.25 μg/ml
Table 2B.
Adjusted odds ratios of endemic Neisseria gonorrhoeae antibiotic resistance among MSM compared to MSW, GISP, 2005–2010
| Endemic Resistance | ||
|---|---|---|
| Variable | aOR | 95% CI |
| Ciprofloxacin, resistance║ | ||
| West | 2.6 | 2.4–2.9 |
| Midwest | 10.8 | 8.4–13.9 |
| Northeast/South | 2.5 | 2.2–2.9 |
| Penicillin, resistance¶ | ||
| West | 2.1 | 1.9–2.4 |
| Midwest | 4.0 | 3.2–5.0 |
| Northeast/South | 2.3 | 2.0–2.6 |
| Tetracycline, resistance# | ||
| West | 2.5 | 2.3–2.8 |
| Midwest | 5.4 | 4.5–6.4 |
| Northeast/South | 2.1 | 1.9–2.4 |
aOR = adjusted odds ratio; CI = confidence interval;
GISP = the Gonococcal Isolate Surveillance Project;
MIC = minimum inhibitory concentration; MSM = men
who have sex with men; MSW = men who report
having sex exclusively with women
All models adjusted for age, region, race/ethnicity, antimicrobial use, travel history, HIV infection, prior gonococcal infection, and the interaction between gender of sex partner & region.
MIC ≥ 1 μg/ml
MIC ≥ 2 μg/ml or β-lactamase positive
MIC ≥ 2 μg/ml
Sensitivity analyses were performed to evaluate the effect of different approaches for handling missing data on the results displayed in Table 2B. The results obtained by excluding missing data or considering missing data to be negative were consistent with the primary analysis (Appendix, Table B). Results of the simple models examining the association between elevated MICs of azithromycin, cefixime, or ceftriaxone, or multidrug resistance and gender of sex partner, adjusted for region and the interaction of gender of sex partner & region, were consistent with the results of the primary analysis (Appendix, Table C).
Discussion
During the past seventy years, N. gonorrhoeae has developed resistance over time to antimicrobial agents recommended for the treatment of gonorrhea. Combination therapy with ceftriaxone (a third-generation cephalosporin) and either azithromycin or doxycycline is now the only remaining first-line therapeutic option.(13) However, gonococcal susceptibility to cephalosporins, the cornerstone of treatment, is declining. Failures of treatment with oral cephalosporins have been reported in Asia and Europe in the past several years and ceftriaxone-resistant isolates were identified in Japan in 2009 and France in 2010.(15–20) In the US, MICs of cefixime for N. gonorrhoeae increased during 2006–2010, most notably in the West and among MSM.(13) In addition, gonococcal strains with high azithromycin MICs have been identified in the US (21, 22) and a patient unsuccessfully treated with azithromycin 2 g as a single oral dose was recently identified.(23) The introduction and spread of cephalosporin-resistant N. gonorrhoeae, particularly if also exhibiting azithromycin resistance, would greatly limit treatment options for gonorrhea and could render some cases of gonorrhea untreatable with currently recommended drug regimens.
MSM are particularly vulnerable to this emerging public health threat. In geographic areas participating in the STD Surveillance Network, approximately 22% of reported gonorrhea cases occur in MSM, although with substantial geographic variability (CDC, unpublished data). Previously published reports have described a higher prevalence of resistance to or elevated MICs of individual antimicrobials among isolates from MSM (11,13,24,25), but this is the first report to describe such findings across a range of antimicrobial classes either currently or previously recommended for gonorrhea treatment.
During the emergence of QRNG in the US, the prevalence of QRNG increased more rapidly among MSM than MSW: from 2002 to 2003, the prevalence of QRNG increased among MSM from 1.8% to 4.9%, but only from 0.2% to 0.4% among MSW.(11) By 2004, CDC no longer recommended fluoroquinolones for treatment of gonorrhea among MSM, three years before the same change in recommendation was made for heterosexuals.(12) The prevalence of QRNG remains high among MSM, despite the change in treatment recommendations and decline in fluoroquinolone use for gonorrhea.(26) A similar pattern seems to be emerging for cephalosporins, as MICs of cephalosporins are increasing more rapidly among MSM than MSW in the US and United Kingdom.(13,27)
Antimicrobial resistance in other clinically important microbes has also been described more often for MSM than for MSW. In a sample of recently diagnosed HIV-1 infected persons enrolled during 1997–2001, the prevalence of antiretroviral resistance associated mutations was significantly higher among MSM (11.6%) than among MSW (4.7%), possibly due to greater exposure to antiretroviral therapy.(28) MSM have been noted to be at elevated risk for community-associated methicillin-resistant Staphylococcus aureus, and an outbreak of ciprofloxacin-resistant Shigella sonnei among MSM has been described.(29,30)
The causes of the differences in gonococcal antimicrobial susceptibility between MSM and MSW are not fully understood, but there are several possible explanations. First, MSM might be more likely to travel internationally: a high proportion of newly HIV-infected MSM in San Francisco reported recent international travel or foreign-born sex partners.(31) This may be relevant because some cases of penicillinase-producing N. gonorrhoeae and QRNG appeared to have been imported into the US in the past by travelers from East Asia.(7, 32) Second, events such as circuit parties may provide a nexus for sexual interaction among MSM from different geographic regions (33) and potentially facilitate spread of resistant strains among MSM in different geographic regions. Third, we found that MSM with gonorrhea were more likely than MSW to report antimicrobial use in the past 60 days, possibly resulting in greater antimicrobial selection pressure. Although this might not explain the emergence of a resistance phenotype, which may be imported from other regions of the world, differential antimicrobial use might contribute to the selection and persistence of resistance phenotypes in the US. Fourth, N. gonorrhoeae infections of the rectum and/or pharynx might be more prone to develop antimicrobial resistance than urogenital isolates; resistant gonococcal strains may thus have a selective advantage for survival in and transmission to and from these sites in MSM. Rectal isolates have been noted to have higher geometric mean MICs of penicillin and erythromycin than genital isolates, possibly due to mutations in the mtr locus that result in reduced outer membrane permeability to hydrophobic molecules that allow the organism to survive in the rectum.(24,25,34–36) It has also been hypothesized that genetic re-assortment in pharyngeal infections might contribute to cephalosporin resistance: mosaic penA mutants found in many N. gonorrhoeae isolates with decreased susceptibility to cefixime include genetic material from commensal Neisseria species often found in the pharynx.(37) Under-treatment of pharyngeal gonorrhea, which is difficult to eradicate and often asymptomatic, could also select for resistance. It thus might not be a coincidence that the recently described ceftriaxone-resistant isolate from Japan was isolated from the pharynx of a female commercial sex worker.(19)
Cephalosporins MICs increased earlier and more steeply in the West than other regions (13). However, the adjusted odds ratios of elevated cephalosporins MICs among isolates from MSM compared to MSW are consistently lower than for other regions. This seeming contradiction is most likely due to the early increase in MICs in the West, which started in MSM and are now also observed in MSW, thus decreasing the magnitude of the association.
This analysis has several limitations. An increasing proportion of cases of gonorrhea are diagnosed and reported from clinical settings other than public STD clinics.(1) Thus, it is possible that our results may not be representative of all men with gonorrhea in the US. However, this is unlikely to alter the relative differences in resistance patterns between isolates from MSM and MSW. The analysis aggregated gay and bisexual men as MSM. Further work could investigate possible differences between isolates from gay and bisexual men. The aggregation of isolates from the Northeast and South may mask finer differences in susceptibility by geographic locations. However, as a sentinel surveillance system, GISP cannot and is not designed to provide full geographic coverage. The breakpoints for cephalosporin susceptibility that we used in this analysis do not necessarily represent “clinical” resistance. However, it is likely that increasing cephalosporin MICs will precede the emergence of resistance, and resistance would emerge first in the populations infected with strains exhibiting increasing MICs. GISP does not collect detailed behavioral data. Further work could investigate whether specific antimicrobial usage patterns or sexual behaviors, such as the number of recent partners or the type of sex in which men engaged (e.g. insertive versus receptive), influence gonococcal antimicrobial susceptibility. A substantial proportion of antimicrobial use, HIV, and travel history data were missing because some participating sites do not collect these data routinely. For instance, over 40% of travel data were missing. However, the results of the sensitivity analyses suggest that substantial bias was not introduced by missing data.
Strengthening prevention strategies for MSM is critical in this era of dwindling treatment options. The number of antimicrobials newly approved by the FDA has steadily declined,(38) and few new antimicrobials active against N. gonorrhoeae are being developed. New antimicrobials or antimicrobial combinations need to be developed and existing antimicrobials not yet used for gonorrhea should be evaluated for efficacy. The National Institute for Allergy and Infectious Diseases, in collaboration with CDC, has completed enrollment of a clinical trial of 2 combinations of existing drugs: azithromycin plus either gentamicin or gemifloxacin (NCT00926796). But additional antimicrobial agents should be studied. Clinicians are encouraged to screen sexually active MSM at all anatomic sites of exposure at least annually (39) and to treat those diagnosed with gonorrhea with ceftriaxone 250 mg as a single intramuscular dose plus either azithromycin 1 g orally or doxycycline 100 mg twice daily orally for 7 days.(13) Clinicians must remain vigilant for treatment failures, even among patients treated with recommended therapy, and should notify their local or state health department and CDC of possible treatment failures. Continued surveillance of N. gonorrhoeae antimicrobial susceptibility, particularly among MSM, is vital. Local surveillance can be enhanced by the maintenance or establishment of laboratory capacity to conduct culture for N. gonorrhoeae, a capacity lost in many places due to the widespread use of nucleic acid amplification testing. Sexually active MSM are encouraged to be in long-term mutually monogamous relationships with partners who have been tested and are known to be uninfected. Latex condoms, when used consistently and correctly, can reduce the risk of acquiring gonorrhea.(40)
The emergence of cephalosporin-resistant Neisseria gonorrhoeae would substantially complicate the ability to treat gonorrhea. MSM at risk for gonorrhea are particularly vulnerable to this public health threat.
Supplementary Material
Acknowledgements
Alesia Harvey, Tremeka Sanders, Kevin Pettus, Samera Bowers, Paula Dixon, Laura Doyle, Baderinwa Offut, and the GISP participating clinics
Funding information: The Gonococcal Isolate Surveillance Project (GISP) is funded by the CDC, an agency of the US Department of Health and Human Services. Representatives of the CDC were involved in the design and conduct of this surveillance activity and the collection, management, analysis, and interpretation of GISP data.
References
- 1.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2010. Atlanta: U.S. Department of Health and Human Services; 2011. [Google Scholar]
- 2.Braunstein SL, Ingabire CM, Kestelyn E, Uwizera AU, Mwamarangwe L, Ntirushwa J, et al. High human immunodeficiency virus incidence in a cohort of Rwandan female sex workers. Sex Transm Dis 2011;38(5):385–94. [DOI] [PubMed] [Google Scholar]
- 3.Johnson LF and Lewis DA. Effect of genital tract infections on HIV-1 shedding in the genital tract: a systematic review and meta-analysis. Sex Transm Dis 2008;35(11):946–59. [DOI] [PubMed] [Google Scholar]
- 4.Curran JW. Management of gonococcal pelvic inflammatory disease. Sex Transm Dis 1979;6(2 Suppl):174–80. [DOI] [PubMed] [Google Scholar]
- 5.Watson RA. Gonorrhea and acute epididymitis. Mil Med 1979;144(12):785–7. . [PubMed] [Google Scholar]
- 6.Martin JE, Lester A, Price EV, Schmale JD. Comparative study of gonococcal susceptibility to penicillin in the United States, 1955–1969. J Infect Dis 1970; 122(5):459–461 [DOI] [PubMed] [Google Scholar]
- 7.Perine PL, Morton RS, Piot P, Siegel MS, Antal GM. Epidemiology and treatment of penicillinase-producing Neisseria gonorrhoeae. Sex Transm Dis 1979; 6(2):152–158. [DOI] [PubMed] [Google Scholar]
- 8.Morse SA, Johnson SR, Biddle JW, Roberts MC. High-level tetracycline resistance in Neisseria gonorrhoeae is result of acquisition of streptococcal tetM determinant. Antimicrob Agents Chemother 1986;30(5):664–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knapp JS, Zenilman JM, Biddel JW, Perkins GH, DeWitt WE, Thomas ML, et al. Frequency and distribution in the United States of strains with Neisseria gonorrhoeae with plasmid-mediated, high-level resistance to tetracycline. J Infect Dis 1987; 155(4):819–822. [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Increases in fluoroquinolone-resistant Neisseria gonorrhoeae —Hawaii and California, 2001. MMWR 2002;51(46):1041–1044. [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. Increases in fluoroquinolone-resistant Neisseria gonorrhoeae among men who have sex with men —United States, 2003, and Revised recommendations for gonorrhea treatment, 2004. MMWR 2004;53(16):335–338. [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Update to CDC’s Sexually Transmitted Diseases Treatment Guidelines, 2006: Fluoroquinolones no longer recommended for treatment of gonococcal infections. MMWR 2007;56(14):332–336. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. Update to CDC’s Sexually Transmitted Diseases Treatment Guidelines, 2010: Oral cephalosporins no longer a recommended treatment for gonococcal infections. MMWR 2012; 61(31): 590–594. [PubMed] [Google Scholar]
- 14.Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; Twentieth Informational Supplement, M100-S20. National Committee for Clinical Laboratory Standards, 2010;29(3):84–86. [Google Scholar]
- 15.Akasaka S, Muratani T, Yamada T, Inatomi H, Takahashi K, Matsumoto T. Emergence of cephem- and aztreonam-high-resistant Neisseria gonorrhoeae that does not produce β-lactamase. J Infect Chemother 2001;7:49–50. [DOI] [PubMed] [Google Scholar]
- 16.Yokoi S, Deguchi T, Ozawa T, Yasuda M, Ito S, Kubota Y, et al. Threat to cefixime treatment for gonorrhea. Emerg Infect Dis 2007;13(8):1275–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Unemo M, Golparian D, Syversen G, Vestrheim DF, Moi H. Two cases of verified clinical failures using internationally recommended first-line cefixime for gonorrhoea treatment, Norway, 2010. Eurosurv 2010; 15(47). pii:19721. [DOI] [PubMed] [Google Scholar]
- 18.Ison CA, Hussey J, Sankar KN, Evans J, Alexander S. Gonorrhoea treatment failures to cefixime and azithromycin in England, 2010. Eurosurv 2011;16(14). p: 19833. [PubMed] [Google Scholar]
- 19.Ohnishi M, Golparian D, Shimuta K, Saika T, Hoshina S, Iwasaku K, et al. Is Neisseria gonorrhoeae initiating a future era of untreatable gonorrhea?: detailed characterization of the first strain with high-level resistance to ceftriaxone. Antimicrob Agents Chemother 2011;55(7):3538–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Unemo M, Golparian D, Nicholas R, Ohnishi M, Gallay A, Sednaoui P. High-level cefixime- and ceftriaxone-resistant Neisseria gonorrhoeae in Europe (France): novel penA mosaic allele in a successful international clone causes treatment failure. Antimicrob Agents Chemother 2012;56(3):1273–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. Neisseria gonorrhoeae with reduced susceptibility to azithromycin—San Diego County, California, 2009. MMWR 2011;60(18):579–581. [PubMed] [Google Scholar]
- 22.Katz AR, Komeya AY, Soge OO, et al. Neisseria gonorrhoeae with high-level resistance to azithromycin: case-report of the first isolate identified in the United States. Clin Infect Dis 2012; 54(6):841–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soge OO, Harger D, Schafer S, Toevs K, Raisler KA, Venator K, Holmes KK, Kirkcaldy RD. Emergence of increased azithromycin resistance among unsuccessful treatment of Neisseria gonorrhoeae infection with azithromycin (Portland, OR, 2011). Sex Transm Dis 2012;39(11):877–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Morse SA, Lysko PG, McFarland L, Knapp JS, Sandstrom E, Critchlow C, Holmes KK. Gonococcal strains from homosexual men have outer membranes with reduced permeability to hydrophobic molecules. Infect Immun 1982;37(2):432–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Handsfield HH, Knapp JS, Diehr PK, Holmes KK. Correlation of auxotype and penicillin susceptibility of Neisseria gonorrhoeae with sexual preference and clinical manifestations of gonorrhea. Sex Transm Dis 1980; 1–5. [DOI] [PubMed] [Google Scholar]
- 26.Dowell D, Tian LH, Stover JA, Donnelly JA, Martins S, Erbelding EJ, et al. Changes in fluoroquinolone use for gonorrhea following publication of revised treatment guidelines. Am J Public Health 2012;102(1):148–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gonococcal Resistance to Antimicrobials Surveillance Programme in England and Wales: GRASP 2010 Report. Health Protection Agency; 2011. London, United Kingdom. [Google Scholar]
- 28.Weinstock HS, Zaidi I, Heneine W, Bennett D, Garcia-Lerma JG, Douglas JM, et al. The epidemiology of antiretroviral drug resistance among drug naïve HIV-1–infected persons in 10 US cities. J Infect Dis 2004;189:2174–80. [DOI] [PubMed] [Google Scholar]
- 29.An Diep B, Chambers HF, Graber CJ, Szumowski JD, Miller LG, Han LL, et al. Emergence of multidrug-resistant community-associated, methicillin-resistant Staphylococcus aureus clone USA300 in men who have sex with men. Ann Intern Med 2008;148:249–257. [DOI] [PubMed] [Google Scholar]
- 30.Gaudreau C, Ratnayake R, Pilon PA, Gagnon S, Roger M, Lévesque S. Ciprofloxacin-resistant Shigella sonnei among men who have sex with men, Canada, 2010. Emerg Infect Dis 2011;17:1747–1750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Truong H-HM, Kellogg T, Schwarcz S, Delgado V, Grant RM, Louie B, Ngo H, McFarland W. Frequent international travel by men who have sex with men recently diagnosed with HIV-1: Potential for transmission of primary HIV-1 drug resistance. Intern J Travel Med 2008;15(6):454–456. [DOI] [PubMed] [Google Scholar]
- 32.Knapp JS, Ohye R, Neal SW, Parekh MC, Higa H, Rice RJ. Emerging in vitro resistance to quinolones in penicillinase-producing Neisseria gonorrhoeae strains in Hawaii. Antimicrob Agents Chemother 1994;38(9):2200–2203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mansergh G, Colfax GN, Marks G, Rader M, Guzman R, Buchbinder S. The circuit party men’s health survey: findings and implications for gay and bisexual men. Am J Public Health 2001;91(6):953–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fagan D Comparison of Neisseria gonorrhoeae isolates from homosexual and heterosexual men. Genitourin Med 1985;61:363–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McFarland L, Mietzner TA, Knapp JS, Sandstrom E, Holmes KK, Morse SA. Gonococcal sensitivity to fecal lipids can be mediated by an mtr-independent mechanism. J Clin Microbiol 1983;18:121–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shafer WM, Balthazar JT, Hagman KE, Morse SA. Missense mutations that alter the DNA-binding domain of the MtrR protein occur frequently in rectal isolates of Neisseria gonorrhoeae that are resistant to fecal lipids. Microbiol 1995;141:907–911. [DOI] [PubMed] [Google Scholar]
- 37.Ameyama S, Onodera S, Takahata M, Minami S, Maki N, Endo K, Goto H, Suzuki H, Oishi Y. Mosaic-like structure of penicillin-binding protein 2 gene (penA) in clinical isolates of Neisseria gonorrhoeae with reduced susceptibility to cefixime. Antimicrob Agents Chemother 2002; 46(12):3744–3749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Spellberg B, Powers JH, Brass EP, Miller LG, Edwards J. Trends in antimicrobial drug development: implications for the future. Clin Infect Dis 2004;38:1279–86. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Sexually Transmitted Diseases Treatment Guidelines, 2010. MMWR 2010; 59(No. RR-12):1–110. [PubMed] [Google Scholar]
- 40.Warner L, Stone KM, Macaluso M, Buehler JW, Austin HD Condom use and risk of gonorrhea and chlamydia: a systematic review of design and measurement factors assessed in epidemiologic studies. Sex Transm Dis 2006; 33(1):36–51. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


